COVID-19 Vaccine Information Exposure: The Effect of Online Authority vs. Non-Authority Sources on Beliefs, Emotions and Information Engagement Behaviors
Abstract
1. Introduction
1.1. Vaccine-Related Information Engagement
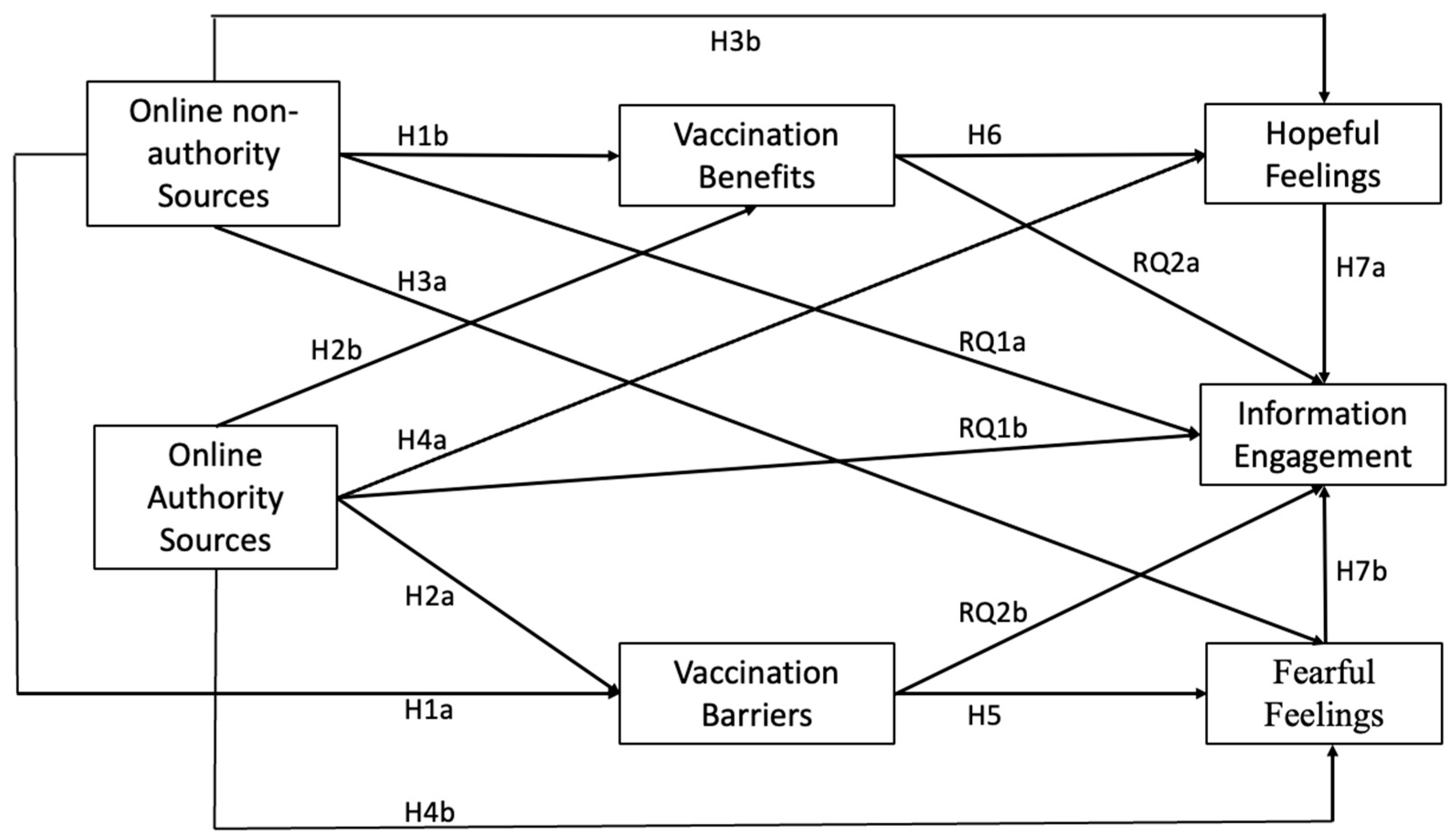
1.2. Stimulus–Organism–Response (S-O-R) Paradigm
1.3. Information Sources and Vaccination Beliefs
1.4. Information Sources, Fear, and Hope
1.5. Health Beliefs, Fear, and Hope
1.6. Information Exposure, Beliefs, Emotions and Information Engagement
2. Materials and Methods
2.1. Method
2.2. Measures
2.3. Statistical Analyses
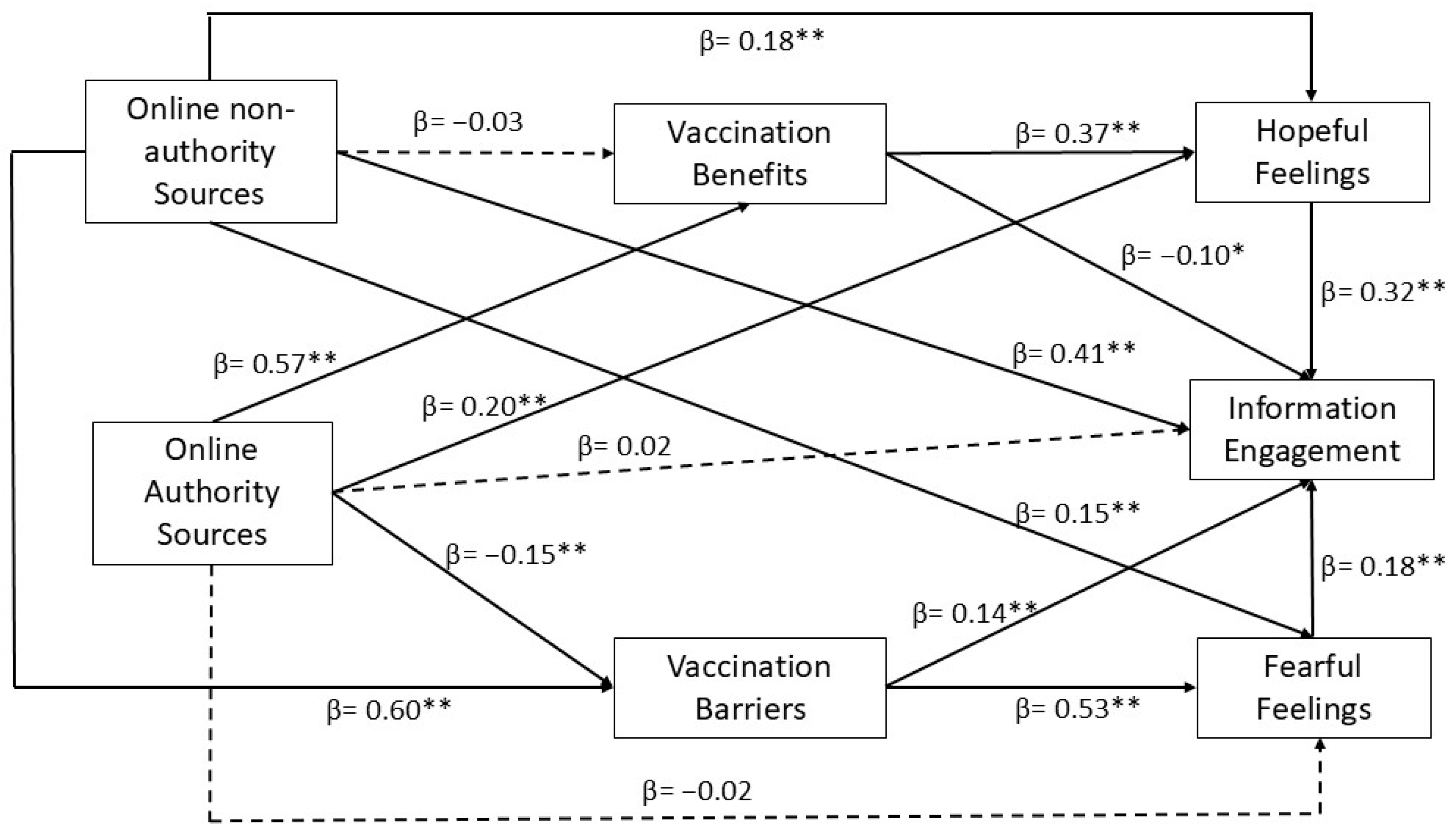
3. Results
3.1. Descriptive Results
3.2. Hypotheses Testing
4. Discussion
4.1. Practical Implications
4.2. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ali, K.; Zain-ul-abdin, K.; Li, C.; Johns, L.; Ali, A.A.; Carcioppolo, N. Viruses Going Viral: Impact of Fear-Arousing Sensationalist Social Media Messages on User Engagement. Sci. Commun. 2019, 41, 314–338. [Google Scholar] [CrossRef]
- Nielsen, R.K.; Fletcher, R.; Newman, N.; Brennen, J.S. Navigating the ‘Infodemic’: How People in Six Countries Access and Rate News and Information about Coronavirus. Available online: https://reutersinstitute.politics.ox.ac.uk/infodemic-how-people-six-countries-access-and-rate-news-and-information-about-coronavirus#footnote-02 (accessed on 8 August 2023).
- Pierri, F.; Perry, B.L.; DeVerna, M.R.; Yang, K.-C.; Flammini, A.; Menczer, F.; Bryden, J. Online Misinformation Is Linked to Early COVID-19 Vaccination Hesitancy and Refusal. Sci. Rep. 2022, 12, 5966. [Google Scholar] [CrossRef] [PubMed]
- Machado Vieira, L.; Cordeiro, D.F. Lado Obscuro Da Antivacinação: Análise de Um Grupo Brasileiro Antivacina No Facebook. Rev. FAMECOS (Online) 2023, 30, e43710. [Google Scholar] [CrossRef]
- Pellegrino, R.; Pellino, G.; Selvaggi, L.; Selvaggi, F.; Federico, A.; Romano, M.; Gravina, A.G. BNT162b2 mRNA COVID-19 Vaccine Is Safe in a Setting of Patients on Biologic Therapy with Inflammatory Bowel Diseases: A Monocentric Real-Life Study. Expert. Rev. Clin. Pharmacol. 2022, 15, 1243–1252. [Google Scholar] [CrossRef]
- Hudhud, D.; Caldera, F.; Cross, R.K. Addressing COVID-19 Vaccine Hesitancy in Patients with IBD. Inflamm. Bowel Dis. 2022, 28, 492–493. [Google Scholar] [CrossRef]
- Lin, L.; Jung, M.; McCloud, R.F.; Viswanath, K. Media Use and Communication Inequalities in a Public Health Emergency: A Case Study of 2009–2010 Pandemic Influenza a Virus Subtype H1n1. Public Health Rep. 2014, 129, 49–60. [Google Scholar] [CrossRef] [PubMed]
- Mohammed, F.; Al-Kumaim, N.H.; Alzahrani, A.I.; Fazea, Y. The Impact of Social Media Shared Health Content on Protective Behavior against COVID-19. Int. J. Environ. Res. Public Health 2023, 20, 1775. [Google Scholar] [CrossRef]
- Zhao, X.; Tsang, S.J. Self-Protection by Fact-Checking: How Pandemic Information Seeking and Verifying Affect Preventive Behaviours. J. Contingencies Crisis Manag. 2021, 30, 171–184. [Google Scholar] [CrossRef]
- Xu, X.; Lin, C.A.; Chen, H. Exploring COVID-19 Vaccine Misinformation Exposure, Beliefs, Fear, and Information Avoidance via the Stimulus–Organism–Response Framework. Sci. Commun. 2023, 45, 824–850. [Google Scholar] [CrossRef]
- Chen, S.; Xiao, L.; Kumar, A. Spread of Misinformation on Social Media: What Contributes to It and How to Combat It. Comput. Hum. Behav. 2023, 141, 107643. [Google Scholar] [CrossRef]
- Fredrickson, B.L.; Branigan, C. Positive Emotions Broaden the Scope of Attention and Thought-action Repertoires. Cogn. Emot. 2005, 19, 313–332. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.L.; Idris, I.K. Recognise Misinformation and Verify before Sharing: A Reasoned Action and Information Literacy Perspective. Behav. Inf. Technol. 2019, 38, 1194–1212. [Google Scholar] [CrossRef]
- Kovach, B.; Rosenstiel, T. The Elements of Journalism: What Newspeople Should Know and the Public Should Expect; Three Rivers Press: New York, NY, USA, 2014; ISBN 978-0-8041-3678-5. [Google Scholar]
- Wu, L.; Morstatter, F.; Hu, X.; Liu, H. Mining Misinformation in Social Media. In Big Data in Complex and Social Networks; Chapman and Hall/CRC: Boca Raton, FL, USA, 2016; ISBN 978-1-315-39670-5. [Google Scholar]
- Obi-Ani, N.A.; Anikwenze, C.; Isiani, M.C. Social Media and the COVID-19 Pandemic: Observations from Nigeria. Cogent Arts Humanit. 2020, 7, 1799483. [Google Scholar] [CrossRef]
- Saud, M.; Mashud, M.; Ida, R. Usage of Social Media during the Pandemic: Seeking Support and Awareness about COVID-19 through Social Media Platforms. J. Public Aff. 2020, 20, e2417. [Google Scholar] [CrossRef]
- Rosenstock, I.M. Historical Origins of the Health Belief Model. Health Educ. Monogr. 1974, 2, 328–335. [Google Scholar] [CrossRef]
- Gavilanes, J.M.; Flatten, T.C.; Brettel, M. Content Strategies for Digital Consumer Engagement in Social Networks: Why Advertising Is an Antecedent of Engagement. J. Advert. 2018, 47, 4–23. [Google Scholar] [CrossRef]
- van Doorn, J.; Lemon, K.N.; Mittal, V.; Nass, S.; Pick, D.; Pirner, P.; Verhoef, P.C. Customer Engagement Behavior: Theoretical Foundations and Research Directions. J. Serv. Res. 2010, 13, 253–266. [Google Scholar] [CrossRef]
- Schachter, S. The Psychology of Affiliation: Experimental Studies of the Sources of Gregariousness; The psychology of affiliation: Experimental studies of the sources of gregariousness; Stanford Univer. Press: Palo Alto, CA, USA, 1959; p. 141. [Google Scholar]
- Ngai, C.S.B.; Singh, R.G.; Lu, W.; Yao, L.; Koon, A.C. Exploring the Relationship Between Trust-Building Strategies and Public Engagement on Social Media During the COVID-19 Outbreak. Health Commun. 2023, 38, 2141–2157. [Google Scholar] [CrossRef]
- Zhang, W.; Yuan, H.; Zhu, C.; Chen, Q.; Evans, R.D.; Min, C. Factors Influencing Public Engagement in Government TikTok during the COVID-19 Crisis. Electron. Libr. 2023, 42, 210–229. [Google Scholar] [CrossRef]
- Mehrabian, A.; Russell, J.A. An Approach to Environmental Psychology; The MIT Press: Cambridge, MA, USA, 1974; ISBN 978-0-262-13090-5. [Google Scholar]
- Russell, J.; Pratt, G. A Description of the Affective Quality Attributed to Environments. J. Personal. Soc. Psychol. 1980, 38, 311–322. [Google Scholar] [CrossRef]
- Song, S.; Yao, X.; Wen, N. What Motivates Chinese Consumers to Avoid Information about the COVID-19 Pandemic?: The Perspective of the Stimulus-Organism-Response Model. Inf. Process. Manag. 2021, 58, 102407. [Google Scholar] [CrossRef] [PubMed]
- Soroya, S.H.; Farooq, A.; Mahmood, K.; Isoaho, J.; Zara, S. From Information Seeking to Information Avoidance: Understanding the Health Information Behavior during a Global Health Crisis. Inf. Process. Manag. 2021, 58, 102440. [Google Scholar] [CrossRef] [PubMed]
- Laato, S.; Islam, A.K.M.N.; Islam, M.N.; Whelan, E. Why Do People Share Misinformation during the COVID-19 Pandemic? Eur. J. Inf. Syst. 2020, 29, 288–305. [Google Scholar] [CrossRef]
- Skarpa, P.E.; Garoufallou, E. Information Seeking Behavior and COVID-19 Pandemic: A Snapshot of Young, Middle Aged and Senior Individuals in Greece. Int. J. Med. Inform. 2021, 150, 104465. [Google Scholar] [CrossRef] [PubMed]
- Zampetakis, L.A.; Melas, C. The Health Belief Model Predicts Vaccination Intentions against COVID-19: A Survey Experiment Approach. Appl. Psych. Health Well 2021, 13, 469–484. [Google Scholar] [CrossRef]
- Ali, S.H.; Foreman, J.; Tozan, Y.; Capasso, A.; Jones, A.M.; DiClemente, R.J. Trends and Predictors of COVID-19 Information Sources and Their Relationship With Knowledge and Beliefs Related to the Pandemic: Nationwide Cross-Sectional Study. JMIR Public Health Surveill. 2020, 6, e21071. [Google Scholar] [CrossRef]
- Zhao, S.; Wu, X. From Information Exposure to Protective Behaviors: Investigating the Underlying Mechanism in COVID-19 Outbreak Using Social Amplification Theory and Extended Parallel Process Model. Front. Psychol. 2021, 12, 631116. [Google Scholar] [CrossRef]
- Lee, J.J.; Kang, K.-A.; Wang, M.P.; Zhao, S.Z.; Wong, J.Y.H.; O’Connor, S.; Yang, S.C.; Shin, S. Associations Between COVID-19 Misinformation Exposure and Belief with COVID-19 Knowledge and Preventive Behaviors: Cross-Sectional Online Study. J. Med. Internet Res. 2020, 22, e22205. [Google Scholar] [CrossRef]
- Lin, C.A. A Year like No Other: A Call to Curb the Infodemic and Depoliticize a Pandemic Crisis. J. Broadcast. Electron. Media 2021, 64, 661–671. [Google Scholar] [CrossRef]
- Ahmed, N.; Quinn, S.C.; Hancock, G.R.; Freimuth, V.S.; Jamison, A. Social Media Use and Influenza Vaccine Uptake among White and African American Adults. Vaccine 2018, 36, 7556–7561. [Google Scholar] [CrossRef]
- Lu, H.; APPC 2018–2019 ASK Group; Winneg, K.; Jamieson, K.H.; Albarracín, D. Intentions to Seek Information About the Influenza Vaccine: The Role of Informational Subjective Norms, Anticipated and Experienced Affect, and Information Insufficiency Among Vaccinated and Unvaccinated People. Risk Anal. 2020, 40, 2040–2056. [Google Scholar] [CrossRef] [PubMed]
- Hyer, R.N.; Covello, V.T. Effective Media Communication during Public Health Emergencies: A WHO Field Guide; World Health Organization: Geneva, Switzerland, 2005. [Google Scholar]
- Chou, W.-Y.S.; Gaysynsky, A.; Cappella, J.N. Where We Go From Here: Health Misinformation on Social Media. Am. J. Public Health 2020, 110, S273–S275. [Google Scholar] [CrossRef] [PubMed]
- Loomba, S.; de Figueiredo, A.; Piatek, S.J.; de Graaf, K.; Larson, H.J. Measuring the Impact of Exposure to COVID-19 Vaccine Misinformation on Vaccine Intent in the UK and US. Nat. Hum. Behav. 2020, 5, 407. [Google Scholar] [CrossRef]
- Trent, M.; Seale, H.; Chughtai, A.A.; Salmon, D.; MacIntyre, C.R. Trust in Government, Intention to Vaccinate and COVID-19 Vaccine Hesitancy: A Comparative Survey of Five Large Cities in the United States, United Kingdom, and Australia. Vaccine 2022, 40, 2498–2505. [Google Scholar] [CrossRef]
- Viskupič, F.; Wiltse, D.L.; Meyer, B.A. Trust in Physicians and Trust in Government Predict COVID-19 Vaccine Uptake. Soc. Sci. Q. 2022, 103, 509–520. [Google Scholar] [CrossRef]
- Zimand-Sheiner, D.; Kol, O.; Frydman, S.; Levy, S. To Be (Vaccinated) or Not to Be: The Effect of Media Exposure, Institutional Trust, and Incentives on Attitudes toward COVID-19 Vaccination. Int. J. Environ. Res. Public Health 2021, 18, 12894. [Google Scholar] [CrossRef]
- Lazarus, R.S. Emotion and Adaptation; Oxford University Press: Oxford, UK, 1991; ISBN 978-0-19-028178-6. [Google Scholar]
- Kim, K.; Lee, C.; Ihm, J.; Kim, Y. A Comprehensive Examination of Association between Belief in Vaccine Misinformation and Vaccination Intention in the COVID-19 Context. J. Health Commun. 2022, 27, 495–509. [Google Scholar] [CrossRef]
- Zhou, L.; Ampon-Wireko, S.; Xu, X.; Quansah, P.E.; Larnyo, E. Media Attention and Vaccine Hesitancy: Examining the Mediating Effects of Fear of COVID-19 and the Moderating Role of Trust in Leadership. PLoS ONE 2022, 17, e0263610. [Google Scholar] [CrossRef]
- Smith, C.A.; Lazarus, R.S. Appraisal Components, Core Relational Themes, and the Emotions. Cogn. Emot. 1993, 7, 233–269. [Google Scholar] [CrossRef]
- Tan, A.S.L.; Lee, C.; Chae, J. Exposure to Health (Mis)Information: Lagged Effects on Young Adults’ Health Behaviors and Potential Pathways. J. Commun. 2015, 65, 674–698. [Google Scholar] [CrossRef]
- van der Meer, T.G.L.A.; Jin, Y. Seeking Formula for Misinformation Treatment in Public Health Crises: The Effects of Corrective Information Type and Source. Health Commun. 2020, 35, 560–575. [Google Scholar] [CrossRef]
- Lee, J.; Kim, S.; Ham, C.-D. A Double-Edged Sword? Predicting Consumers’ Attitudes Toward and Sharing Intention of Native Advertising on Social Media. Am. Behav. Sci. 2016, 60, 1425–1441. [Google Scholar] [CrossRef]
- Lades, L.K.; Laffan, K.; Daly, M.; Delaney, L. Daily Emotional Well-Being during the COVID-19 Pandemic. Br. J. Health Psychol. 2020, 25, 902–911. [Google Scholar] [CrossRef]
- Ni, M.Y.; Yang, L.; Leung, C.M.C.; Li, N.; Yao, X.I.; Wang, Y.; Leung, G.M.; Cowling, B.J.; Liao, Q. Mental Health, Risk Factors, and Social Media Use During the COVID-19 Epidemic and Cordon Sanitaire Among the Community and Health Professionals in Wuhan, China: Cross-Sectional Survey. JMIR Ment. Health 2020, 7, e19009. [Google Scholar] [CrossRef]
- Nan, X.; Wang, Y.; Thier, K. Health Misinformation. In The Routledge Handbook of Health Communication; Routledge: London, UK, 2022; ISBN 9780367487447. [Google Scholar]
- Nabi, R.L. Exploring the Framing Effects of Emotion: Do Discrete Emotions Differentially Influence Information Accessibility, Information Seeking, and Policy Preference? Commun. Res. 2003, 30, 224–247. [Google Scholar] [CrossRef]
- Nabi, R.L. Emotion and Persuasion: A Social Cognitive Perspective. In Communication and Social Cognition: Theories and Methods; LEA’s communication series; Lawrence Erlbaum Associates Publishers: Mahwah, NJ, USA, 2007; pp. 377–398. ISBN 978-0-8058-5355-1. [Google Scholar]
- Nabi, R.L.; Prestin, A. Unrealistic Hope and Unnecessary Fear: Exploring How Sensationalistic News Stories Influence Health Behavior Motivation. Health Commun. 2016, 31, 1115–1126. [Google Scholar] [CrossRef]
- Frijda, N.H.; Kuipers, P.; ter Schure, E. Relations among Emotion, Appraisal, and Emotional Action Readiness. J. Personal. Soc. Psychol. 1989, 57, 212–228. [Google Scholar] [CrossRef]
- Nabi, R.L. A Cognitive-Functional Model for the Effects of Discrete Negative Emotions on Information Processing, Attitude Change, and Recall. Commun. Theory 1999, 9, 292–320. [Google Scholar] [CrossRef]
- Champion, V.L.; Skinner, C.S.; Menon, U.; Rawl, S.; Giesler, R.B.; Monahan, P.; Daggy, J. A Breast Cancer Fear Scale: Psychometric Development. J. Health Psychol. 2004, 9, 753–762. [Google Scholar] [CrossRef]
- Champion, V.L.; Skinner, C.S. The Health Belief Model. Health Behav. Health Educ. Theory Res. Pract. 2008, 4, 45–65. [Google Scholar]
- Ahn, J.; Kim, H.K.; Kahlor, L.A.; Atkinson, L.; Noh, G.-Y. The Impact of Emotion and Government Trust on Individuals’ Risk Information Seeking and Avoidance during the COVID-19 Pandemic: A Cross-Country Comparison. J. Health Commun. 2021, 26, 728–741. [Google Scholar] [CrossRef] [PubMed]
- Catellier, J.R.A.; Yang, Z.J. Trust and Affect: How Do They Impact Risk Information Seeking in a Health Context? J. Risk Res. 2012, 15, 897–911. [Google Scholar] [CrossRef]
- Wang, X. Putting Emotions in the Health Belief Model: The Role of Hope and Anticipated Guilt on the Chinese’s Intentions to Get COVID-19 Vaccination. Health Commun. 2023, 38, 2491–2500. [Google Scholar] [CrossRef]
- Yang, Z.J.; Kahlor, L.A.; Griffin, D.J. I Share, Therefore I Am: A U.S.−China Comparison of College Students’ Motivations to Share Information about Climate Change. Hum. Commun. Res. 2014, 40, 112–135. [Google Scholar] [CrossRef]
- Alkuwari, M.G.; Aziz, N.A.; Nazzal, Z.A.S.; Al-Nuaimi, S.A. Pandemic Influenza A/H1N1 Vaccination Uptake among Health Care Workers in Qatar: Motivators and Barriers. Vaccine 2011, 29, 2206–2211. [Google Scholar] [CrossRef]
- Burns, V.E.; Ring, C.; Carroll, D. Factors Influencing Influenza Vaccination Uptake in an Elderly, Community-Based Sample. Vaccine 2005, 23, 3604–3608. [Google Scholar] [CrossRef] [PubMed]
- Adam, M.; Mohan, D.; Forster, S.; Chen, S.; Gates, J.; Yu, F.; Bärnighausen, T. Hope as a Predictor for COVID-19 Vaccine Uptake in the US: A Cross-Sectional Survey of 11,955 Adults. Hum. Vaccines Immunother. 2022, 18, 2072138. [Google Scholar] [CrossRef]
- Mayer, Y.; Etgar, S.; Shiffman, N.; Bloch, Y.; Mendlovic, S.; Lurie, I. Hope as a Predictor for COVID-19 Vaccine Uptake. Hum. Vaccines Immunother. 2021, 17, 4941–4945. [Google Scholar] [CrossRef] [PubMed]
- Dillard, J.P.; Li, R.; Yang, C. Fear of Zika: Information Seeking as Cause and Consequence. Health Commun. 2021, 36, 1785–1795. [Google Scholar] [CrossRef] [PubMed]
- Myrick, J.G. The Role of Emotions and Social Cognitive Variables in Online Health Information Seeking Processes and Effects. Comput. Hum. Behav. 2017, 68, 422–433. [Google Scholar] [CrossRef]
- Yang, J.Z. Whose Risk? Why Did the U.S. Public Ignore Information About the Ebola Outbreak? Risk Anal. 2019, 39, 1708–1722. [Google Scholar] [CrossRef] [PubMed]
- Berger, J. Arousal Increases Social Transmission of Information. Psychol. Sci. 2011, 22, 891–893. [Google Scholar] [CrossRef] [PubMed]
- Berger, J.; Milkman, K.L. What Makes Online Content Viral? J. Mark. Res. 2012, 49, 192–205. [Google Scholar] [CrossRef]
- Duffy, A.; Tandoc, E.; Ling, R. Too Good to Be True, Too Good Not to Share: The Social Utility of Fake News. Inf. Commun. Soc. 2020, 23, 1965–1979. [Google Scholar] [CrossRef]
- Han, J.; Cha, M.; Lee, W. Anger Contributes to the Spread of COVID-19 Misinformation. Harv. Kennedy Sch. Misinf. Rev. 2020, 1–14. [Google Scholar] [CrossRef]
- Tsang, S.J.; Zhao, X.; Chen, Y.-R.R. Assessing Mechanisms Underlying the Sharing of Official and Unofficial Information during a Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 13298. [Google Scholar] [CrossRef] [PubMed]
- Huang, Q.; Lei, S.; Ni, B. Perceived Information Overload and Unverified Information Sharing on WeChat Amid the COVID-19 Pandemic: A Moderated Mediation Model of Anxiety and Perceived Herd. Front. Psychol. 2022, 13, 837820. [Google Scholar] [CrossRef]
- Kongkauroptham, W.; Ractham, P.; Kaewkitipong, L.; Chiu, E.M.P. Health-Related Misinformation Sharing on Social Media in Thailand: A Case Study during the COVID-19 Pandemic. In Proceedings of the ICEB 2022, Bangkok, Thailand, 13–17 October 2022. [Google Scholar]
- Volkman, J.E.; Day, A.M.; McManus, T.G.; Hokeness, K.L.; Morse, C.R. PRISM and Emotions: Understanding the Role of Fear and Hope toward Vaccine Information Seeking Intentions. Health Commun. 2022, 38, 2806–2817. [Google Scholar] [CrossRef]
- Lin, C.A.; Xu, X.; Dam, L. Information Source Dependence, Presumed Media Influence, Risk Knowledge, and Vaccination Intention. Atl. J. Commun. 2021, 29, 53–64. [Google Scholar] [CrossRef]
- Sherman, S.M.; Smith, L.E.; Sim, J.; Amlôt, R.; Cutts, M.; Dasch, H.; Rubin, G.J.; Sevdalis, N. COVID-19 Vaccination Intention in the UK: Results from the COVID-19 Vaccination Acceptability Study (CoVAccS), a Nationally Representative Cross-Sectional Survey. Hum. Vaccines Immunother. 2021, 17, 1612–1621. [Google Scholar] [CrossRef]
- Hornik, R.; Kikut, A.; Jesch, E.; Woko, C.; Siegel, L.; Kim, K. Association of COVID-19 Misinformation with Face Mask Wearing and Social Distancing in a Nationally Representative US Sample. Health Commun. 2021, 36, 6–14. [Google Scholar] [CrossRef]
- Lin, Y.; Hu, Z.; Zhao, Q.; Alias, H.; Danaee, M.; Wong, L.P. Understanding COVID-19 Vaccine Demand and Hesitancy: A Nationwide Online Survey in China. PLoS Negl. Trop. Dis. 2020, 14, e0008961. [Google Scholar] [CrossRef] [PubMed]
- Forster, A.S.; McBride, K.A.; Davies, C.; Stoney, T.; Marshall, H.; McGeechan, K.; Cooper, S.C.; Skinner, S.R. Development and Validation of Measures to Evaluate Adolescents’ Knowledge about Human Papillomavirus (HPV), Involvement in HPV Vaccine Decision-Making, Self-Efficacy to Receive the Vaccine and Fear and Anxiety. Public Health 2017, 147, 77–83. [Google Scholar] [CrossRef] [PubMed]
- Strekalova, Y.A.; Krieger, J.L. Beyond Words: Amplification of Cancer Risk Communication on Social Media. J. Health Commun. 2017, 22, 849–857. [Google Scholar] [CrossRef] [PubMed]
- Deaths by Select Demographic and Geographic Characteristics: Provisional Death Counts for COVID-19. Center for Disease Control. Available online: https://www.cdc.gov/nchs/nvss/vsrr/covid_weekly/index.htm#SexAndAge (accessed on 17 September 2024).
- Woo-Hoo, P.J. Going to Be a Beautiful Day out! And I’m Getting My COVID Vaccine Today! #COVIDVaccination @ptatom1709. X (Twitter). 2021. Available online: https://x.com/ptatom1709/status/1367099848936284164?s=46 (accessed on 23 September 2024).
- Robin. Just Got My First Shot! #CovidVaccine #GetTheShot @rob0349 2021.89. X (Twitter). 2021. Available online: https://x.com/rob0349/status/1375182640790319110?s=46 (accessed on 23 September 2024).
- Sun, Y. Verification Upon Exposure to COVID-19 Misinformation: Predictors, Outcomes, and the Mediating Role of Verification. Sci. Commun. 2022, 44, 261–291. [Google Scholar] [CrossRef]
- Tello, M. My COVID-19 Vaccine Story––And What Happened Next. Available online: https://www.health.harvard.edu/blog/my-covid-19-vaccine-story-and-what-happened-next-2021030422082 (accessed on 31 August 2024).
- COVID Vaccinations Problems and Injuries|Shiner Law Group. Available online: https://shinerlawgroup.com/covid-vaccinations-problems-and-injuries/ (accessed on 31 August 2024).
- Gabarda, A.; Butterworth, S.W. Using Best Practices to Address COVID-19 Vaccine Hesitancy: The Case for the Motivational Interviewing Approach. Health Promot. Pract. 2021, 22, 611–615. [Google Scholar] [CrossRef]
- Kim, H.K.; Ahn, J.; Atkinson, L.; Kahlor, L.A. Effects of COVID-19 Misinformation on Information Seeking, Avoidance, and Processing: A Multicountry Comparative Study. Sci. Commun. 2020, 42, 586–615. [Google Scholar] [CrossRef]
- Zaki, J.; Williams, W.C. Interpersonal Emotion Regulation. Emotion 2013, 13, 803–810. [Google Scholar] [CrossRef]
- Malthouse, E. Confirmation Bias and Vaccine-Related Beliefs in the Time of COVID-19. J. Public Health 2023, 45, 523–528. [Google Scholar] [CrossRef]
- Lu, J. Two Large-Scale Global Studies on COVID-19 Vaccine Hesitancy over Time: Culture, Uncertainty Avoidance, and Vaccine Side-Effect Concerns. J. Personal. Soc. Psychol. 2022, 124, 683–706. [Google Scholar] [CrossRef]
- Dam, L.; Basaran, A.-M.B.; Lin, C.A.; Rogers, D. Exploring the Influence of Cultural and Health Beliefs on Intentions to Adopt COVID-19 Prevention Measures. Atl. J. Commun. 2023, 31, 189–206. [Google Scholar] [CrossRef]
- Chou, W.-Y.S.; Budenz, A. Considering Emotion in COVID-19 Vaccine Communication: Addressing Vaccine Hesitancy and Fostering Vaccine Confidence. Health Commun. 2020, 35, 1718–1722. [Google Scholar] [CrossRef] [PubMed]
- Verpaalen, I.A.M.; Ritter, S.M.; van Hooff, M.L.M.; van Stekelenburg, A.; Fransen, M.L.; Holland, R.W. Psychological Reactance and Vaccine Uptake: A Longitudinal Study. Psychol. Health 2023, 38, 1–21. [Google Scholar] [CrossRef]
- Sprengholz, P.; Betsch, C.; Böhm, R. Reactance Revisited: Consequences of Mandatory and Scarce Vaccination in the Case of COVID-19. Appl. Psychol. Health Well-Being 2021, 13, 986–995. [Google Scholar] [CrossRef] [PubMed]

| 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
|---|---|---|---|---|---|---|---|
| 1. Non-Authority Source Exposure | |||||||
| 2. Authority Source Exposure | 0.37 ** | ||||||
| 3. Information Engagement | 0.67 ** | 0.30 ** | |||||
| 4. Fear Connected to Vaccination | 0.44 ** | 0.08 | 0.50 ** | ||||
| 5. Hope Connected to Vaccination | 0.32 ** | 0.48 ** | 0.44 ** | 0.14 ** | |||
| 6. Perceived Vaccination Benefits | 0.18 ** | 0.56 ** | 0.13 * | −0.04 | 0.52 ** | ||
| 7. Perceived Vaccination Barriers | 0.54 ** | 0.07 | 0.50 ** | 0.61 ** | 0.02 | −0.11 ** | |
| M | 3.02 | 3.64 | 2.28 | 2.47 | 3.16 | 3.62 | 2.80 |
| SD | 1.17 | 1.04 | 0.92 | 1.25 | 1.30 | 1.03 | 1.06 |
| Dependent Variables | df (between-Group) | F | p |
|---|---|---|---|
| Exposure to Non-Authority Sources | 3 | 29.18 | *** |
| Exposure to Authority Sources | 3 | 4.13 | 0.007 |
| Perceived Vaccination Benefits | 3 | 16.20 | *** |
| Perceived Vaccination Barriers | 3 | 23.61 | *** |
| Fear Connected to Vaccination | 3 | 19.30 | *** |
| Hope Connected to Vaccination | 3 | 2.66 | 0.048 |
| Information Engagement | 3 | 30.88 | *** |
| Group 1 | Group 2 | Group 3 | Group 4 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 18–29 N = 176 | 30–39 N = 212 | 40–49 N = 83 | 50 and up N = 156 | Group Comparisons * | |||||
| M | SD | M | SD | M | SD | M | SD | ||
| Exposure to Non-Authority Sources | 3.16 | 0.98 | 3.19 | 1.16 | 3.53 | 1.16 | 2.33 | 1.10 | G1 > G4; G2 > G4; G3 > G4 |
| Exposure to Authority Sources | 3.41 | 1.10 | 3.73 | 1.03 | 3.70 | 1.04 | 3.74 | 0.95 | G1 < G2; G1 < G4 |
| Perceived Vaccination Benefits | 3.27 | 0.89 | 3.60 | 1.09 | 3.75 | .93 | 4.01 | 0.99 | G1 < G2; G1 < G3; G1 < G4; G2 < G4 |
| Perceived Vaccination Barriers | 2.98 | 0.88 | 2.90 | 1.10 | 3.21 | 1.06 | 2.23 | 0.98 | G1 > G4; G2 > G4; G3 > G4 |
| Fear Connected to Vaccination | 2.81 | 1.13 | 2.50 | 1.28 | 2.78 | 1.33 | 1.88 | 1.09 | G1 > G4; G2 > G4; G3 > G4 |
| Hope Connected to Vaccination | 3.08 | 1.15 | 3.06 | 1.37 | 3.50 | 1.26 | 3.21 | 1.39 | G2 < G3 |
| Information Engagement | 2.54 | 0.78 | 2.35 | 0.97 | 2.56 | 0.95 | 1.72 | 0.72 | G1 > G4; G2 > G4; G3 > G4 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Xu, X.; Lin, C.A. COVID-19 Vaccine Information Exposure: The Effect of Online Authority vs. Non-Authority Sources on Beliefs, Emotions and Information Engagement Behaviors. Vaccines 2024, 12, 1096. https://doi.org/10.3390/vaccines12101096
Xu X, Lin CA. COVID-19 Vaccine Information Exposure: The Effect of Online Authority vs. Non-Authority Sources on Beliefs, Emotions and Information Engagement Behaviors. Vaccines. 2024; 12(10):1096. https://doi.org/10.3390/vaccines12101096
Chicago/Turabian StyleXu, Xiaowen, and Carolyn A. Lin. 2024. "COVID-19 Vaccine Information Exposure: The Effect of Online Authority vs. Non-Authority Sources on Beliefs, Emotions and Information Engagement Behaviors" Vaccines 12, no. 10: 1096. https://doi.org/10.3390/vaccines12101096
APA StyleXu, X., & Lin, C. A. (2024). COVID-19 Vaccine Information Exposure: The Effect of Online Authority vs. Non-Authority Sources on Beliefs, Emotions and Information Engagement Behaviors. Vaccines, 12(10), 1096. https://doi.org/10.3390/vaccines12101096






