Abstract
Background: men who have sex with men (MSM) are a high-risk group for human papillomavirus (HPV) infection, and the HPV vaccine is effective in preventing it. However, according to risk compensation theory, people may increase sexual risk behaviors after receiving HPV vaccination. Based on the Health Action Process Approach (HAPA), this study investigated the influencing factors to predict intention to reduce condom use (risk compensation intention) among MSM after taking HPV vaccination in southwest China. Methods: we conducted a cross-sectional study among 948 MSM in southwest China using a non-probability sampling method and an electronic questionnaire including sociodemographic characteristics, sexual risk behavior characteristics, HPV-related prevention behavior, and the HAPA scale. Confirmatory factor analysis was performed using a structural equation model. Results: among 948 MSM, the incidence rate of reducing the frequency of condom use was 14.1%. The structural equation model showed that self-efficacy (β = −0.378, p = 0.020) and positive outcome expectancy (β = 0.366, p < 0.05) had greater effects on behavioral intention, followed by negative outcome expectancy (β = −0.296, p < 0.05) and risk perception (β = −0.232, p < 0.05). Conclusions: risk compensation may not be a major barrier to receiving HPV vaccination among MSM. Nevertheless, the recognition of possible risk compensation is necessary to implement appropriate interventions to reduce the occurrence of risk compensation.
1. Introduction
Human papillomavirus (HPV) is one of the most common sexually transmitted diseases (STD) worldwide. At present, more than 200 types of HPV have been identified [1]. Almost all cervical cancers, 90% of anal cancers, and 30% of oropharyngeal cancers worldwide are caused by HPV [2]. HPV infection is common among men who have sex with men (MSM). MSM have significantly higher rates of HPV infection compared to heterosexual men and women [3,4,5]. Meta-analysis showed that the prevalence of HPV infection was very high among MSM internationally (63.9% for HIV-negative MSM and 92.6% for HIV-positive MSM) [6], and the overall HPV prevalence in China was 66.3% [7]. HPV infection can cause genital warts, penile, anal, and oropharyngeal cancers in men [8,9,10]. MSM are at high risk of HPV infection and persistence, carrying multiple HPV types and HPV-related diseases with rapid progression to malignancies [11].
The HPV vaccine is effective in preventing HPV infection and the diseases it causes. The Advisory Committee on Immunization Practices (ACIP) recommends either nine-valent HPV or four-valent HPV vaccines for MSM [12]. Numerous studies have shown that nine-valent HPV or four-valent HPV vaccines are both effective and cost-effective in preventing HPV-related diseases among males [13,14,15]. In 2011, the United States became the first country to incorporate regular HPV vaccination for men, including MSM under the age of 26, into its national vaccination program [16]. By March 2017, 11 countries had provided male vaccination [17]. In China, males are still excluded from the HPV vaccination program [18]. Previous studies have found that MSM had a high willingness for HPV vaccination in China, and more than 80% of MSM were willing to vaccinate; thus, they could be considered for inclusion in the HPV vaccination program [19,20].
However, HPV vaccination has the potential to increase sexual risk behavior while providing benefits to MSM. This phenomenon is called risk compensation. Risk compensation theory refers to the concern that those who undergo a preventive intervention (e.g., HPV vaccination) may engage in behaviors that put them at risk (e.g., reducing condom use) because they feel protected [21]. It has been used to study the sexual behaviors of people at high risk of sexually transmitted infections (STIs) and HIV infection. For example, the introduction of HIV pre-exposure prophylaxis (PrEP), though significantly reducing the risk of HIV transmission, was associated with a decrease in the willingness to use condoms and an increase in the number of sexual partners [22,23]. Therefore, some studies have been concerned with HPV vaccination encouraging sexual risk behaviors, leading to the occurrence of risk compensation [24,25]. At present, studies on risk compensation after taking HPV vaccination mainly focus on women. As an intervention to reduce the risk of STD among MSM, there are few studies on the behavioral intention and influencing factors of risk compensation among MSM after receiving HPV vaccination.
The theoretical framework of this study is the Health Action Process Approach (HAPA) proposed by German psychologist Schwarzer, which is often applied to predict various health behaviors [26,27]. The HAPA is a dual-phase model that distinguishes pre-intentional motivational and post-intentional volitional phases involved in behavior formulation [28]. In the pre-intentional motivational phase, intention is regarded as a primary predictor of behavior. Outcome expectancy (i.e., the belief that the target behavior will lead to effective outcomes for the individual) and self-efficacy (i.e., beliefs in one’s personal capacity to perform the target behavior) are posited as the main factors influencing intention. Risk perception (i.e., the belief in the severity and susceptibility that may result from not performing the target behavior) is posited as a remote antecedent of intention formation. In the volitional phase, there are mainly two parts: (1) action planning and coping plan, and (2) maintenance and recovery self-efficacy. The volitional phase could not be used for this study because MSM do not receive HPV vaccination. It is appropriate to apply the pre-intentional motivational phase of HAPA as the theoretical framework of this study. Some research has also only focused on it [29,30,31]. Previous studies have consistently supported the use of HAPA for vaccination, as all structures of the model predict subsequent vaccination behavior. It has also been applied to explore intentions for influenza vaccination [32], HPV vaccination [24], and COVID-19 vaccination [33].
As more and more countries include males in the HPV vaccination program, it is worth paying attention to whether the psychological cognition and sexual behavior of individuals among MSM will change after receiving HPV vaccination. Therefore, this study investigates the influencing factors to predict risk compensation intention among MSM after taking HPV vaccination in southwest China, and provides evidence for subsequent risk coping strategies of such prevention measures.
2. Materials and Methods
2.1. Participants and Recruitment
From October to November 2022, a non-probability sampling method (including collaboration with non-governmental organizations (NGOs), peer recommendations, and core members (“snowball”)) was used to recruit participants in two cities in Chongqing and Sichuan, China. The inclusion criteria for MSM were as follows: (1) between the ages of 18 and 65 years; (2) self-reported anal sex with one or more male partners in the last year; (3) no serious mental illness or intellectual defect. This study was conducted in an anonymous cross-sectional online survey. Some participants were recruited from the MSM cohort established in the previous study (a cohort study of the National Science and Technology Major Project, registration number: 2018ZX10721102-005), whereas others were recruited from other NGOs. The investigators distributed electronic questionnaires to participants after acquiring their informed consent. If participants did not agree to continue, they had the right to terminate the survey at any time. After completing the questionnaire and passing the review, each participant received a reward of 5 RMB (approximately $0.73). This study was approved by the Ethics Committee of Chongqing Medical University (2019001, 28 May 2019). A total of 1342 participants were recruited for the study. A total of 394 MSM (29.4%) were excluded for the reasons displayed in Figure 1, and the remaining 948 participants met the study criteria.
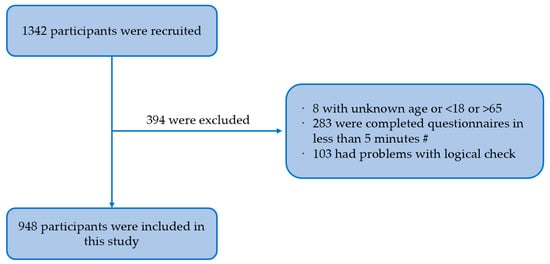
Figure 1.
Flow chart of participants selection. Note: #—after testing, we assessed that participants should have completed the questionnaire in at least 5 min.
2.2. Measurements
2.2.1. Background Characteristics
The information collected included the following four parts: (1) sociodemographic characteristics (i.e., age, household registration, ethnicity, educational level, employment status); (2) characteristics of sexual risk behaviors in the past six months (i.e., number of male partners, condom use during anal sex with male partners); (3) HPV-related preventive behavior (HPV counseling); (4) HPV vaccine-related intentions.
2.2.2. HAPA Scale
Based on the HAPA model, MSM were asked about their views on condom use in a hypothetical situation of having received HPV vaccination. On the basis of the previous literature, this scale consisted of 14 items, including four constructs (risk perception, positive outcome expectancy, negative outcome expectancy, and self-efficacy). The scale was scored according to the Likert five-point scoring method (Table 1).

Table 1.
The HAPA scale and value assignment.
The risk perception consisted of four items, with a higher score indicating a perceived greater increase in the risk of HPV infection. There were two items that made up the positive outcome expectancy, wherein a higher score meant that the perception of reducing condom use after HPV vaccination would result in a more positive outcome. The negative outcome expectancy consisted of three items, with a higher score suggesting that the perceived outcome of reducing condom use after getting HPV vaccine would lead to a more negative impact. The self-efficacy part comprised four items, with a higher score indicating greater confidence in consistently using condoms after receiving the HPV vaccine. Behavioral intention was measured by asking “How condom use may change when you have anal sex with your male sex partner after receiving HPV vaccination”. (1 = very likely to increase, 2 = likely to increase, 3 = remain the same, 4 = likely to reduce, 5 = very likely to reduce). The answers “likely to reduce” and “very likely to reduce” were regarded as the behavioral intention to generate risk compensation. The initial structural equation model of HAPA is displayed in Figure 2.
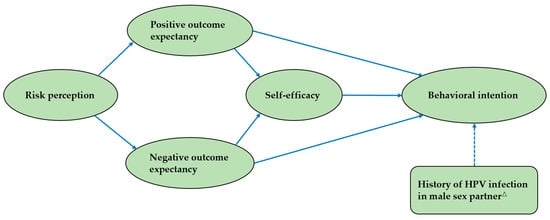
Figure 2.
The initial structural equation model of HAPA. Note: the solid line indicates the theoretical model. The dotted line indicates the added path for this study. △ indicates whether a male partner has been infected with HPV in the last six months.
2.3. Statistical Analysis
SAS version 9.4 was used for data collation and descriptive analysis. Categorical data were described in frequencies and percentages. Structural equation modeling was performed to construct HAPA models using a weighted least squares mean and variance adjusted estimator. Mplus version 8.3 (Los Angeles, LA, USA: Asparouhov & Muthén, 2019) was used to evaluate the factor structure and the relationship of relative variables. Cronbach’s alpha and composite reliability (CR) were used to measure reliability, both of which needed to be greater than 0.70, indicating good internal consistency. The average variance extracted (AVE) was used to measure the convergent validity, and a value greater than 0.50 indicated good convergence. The discriminant validity was considered acceptable if the correlation coefficient between structures was lower than the square root of the corresponding structure. Model fit was assessed using the chi-squared and degree of freedom ratio (χ2/df), comparative fit index (CFI), Tucker Lewis index (TLI), standardized root mean square residual (SRMR), and root mean square error of approximation (RMSEA). The model fitting was acceptable when χ2/df < 5, CFI > 0.90, TLI > 0.90, SRMR < 0.08, and RMSEA < 0.08. Statistical significance was considered at p < 0.05.
3. Results
3.1. Background Characteristics
A total of 948 MSM were included in this study, of which 59.8% were aged 18–27, 59.7% were urban, 95.7% were Han, 54.6% had a bachelor’s degree or above, 55.1% were employed, 83.5% were married, and 72.7% had a monthly salary of less than 5000 RMB. In terms of the characteristics of sexual risk behaviors in the past six months, 33.3% of MSM had two or more male sex partners, whereas only 48.5% had used condoms every time when having anal sex with their male partners. A total of 2.1% had a male partner who had been infected with HPV, and 3.4% had a history of STD. In terms of HPV-related preventive behavior, 41.5% had HPV counseling. In addition, 87.6% indicated that they were very willing or willing to receive HPV vaccination. If receiving HPV vaccination, 14.1% of MSM said they were very likely or likely to reduce condom use (risk compensation intention) (Table 2).

Table 2.
Background characteristics of MSM in southwest China (N = 948).
3.2. Measurement Model
The initial measurement model was tested. Table 3 describes the mean, standard deviation, factor loading, CR, AVE, and Cronbach’s alpha of each construct. The factor loading of each item was greater than 0.5, which was at an acceptable level and statistically significant (p < 0.001). CR and Cronbach’s alpha were greater than 0.7, indicating good internal consistency of the data. AVE was greater than 0.5, indicating good convergence validity. At the same time, the square root of AVE was greater than other correlation coefficients, indicating that the discriminant validity was acceptable (Table 4). Confirmatory factor analysis was performed using a structural equation model. The model fit indices were as follows: χ2/df = 4.686, CFI = 0.990, TLI = 0.988, SRMR = 0.042, and RMSEA = 0.062. These fit indices met the recommended values and indicated that the model was acceptable. Therefore, the model established could be considered acceptable.

Table 3.
Descriptive statistics, factor loading, convergent validity, and reliability analysis.

Table 4.
Discriminant validity.
3.3. Structural Model
Structural model analysis showed (Figure 3) that self-efficacy and positive outcome expectancy had a greater effect on risk compensation intention, followed by negative outcome expectancy and risk perception. Positive outcome expectancy (β = 0.256, p < 0.001), self-efficacy (β = −0.378, p = 0.020), and history of HPV infection in male sex partner (β = 0.101, p = 0.038) had direct effects on behavioral intention, whereas negative outcome expectancy (β = −0.296, p < 0.05) and risk perception (β = −0.232, p < 0.05) had indirect effects on it. What is inconsistent with the hypothesized model is that negative outcome expectancy had no direct effect on behavioral intention (p = 0.242). Positive outcome expectancy was positively correlated with behavioral intention, whereas self-efficacy, risk perception, and negative outcome expectancy were negatively correlated with it.
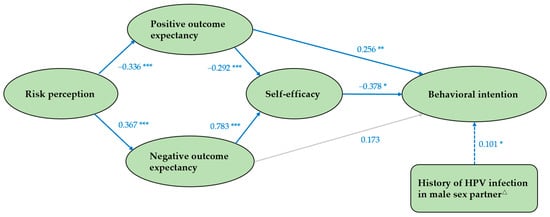
Figure 3.
The path diagram of structural model. Note: the solid line indicates the theoretical model. The dotted line indicates the added path for this study. The gray line indicates that the coefficient is not statistically significant and the pathway is not valid. △ indicates whether a male partner has been infected with HPV in the last six months. * p < 0.05, ** p < 0.01, *** p < 0.001.
Our study found that self-efficacy played an indirect role in the relationship between positive outcome expectancy and behavioral intention. The direct effect of positive outcome expectancy on behavioral intention was 0.256 (p = 0.001), and the indirect effect was 0.110 (p < 0.05) and the total effect was 0.366 (p < 0.05), in which 30.1% of the effect of positive outcome expectancy on behavioral intention was caused by self-efficacy. The significant standardized path coefficients of the structural equation model are depicted in Table 5.

Table 5.
Standardized direct, indirect, and total effects of the final structural equation model.
4. Discussion
HPV is one of the most common sexually transmitted diseases worldwide. It is strongly associated with a variety of human cancers, including cervical, penile, anal, and oral cancers. Co-factors (e.g., environmental carcinogens, cigarette smoking, immunosuppression) are deemed to have an effect on contributing to HPV-related carcinogenesis recognized by the International Agency for Research on Cancer (IARC) [35,36,37]. In males, the development of precancerous lesions is a growing problem, especially among MSM. HPV vaccination is an important measure to reduce the precancerous and cancerous lesions associated with HPV infection [38]. It has a good immune response and can play a direct protective role in men. Current vaccines are able to cover most viral subtypes of HPV-related diseases.
However, risk compensation theory predicts that the emergence of biomedical prevention strategies may be accompanied by an increase in sexual risk behaviors. There were some direct links between risk compensation and vaccines [39,40,41]. The potential risk compensation after receiving HPV vaccination, as an intervention to reduce the risk of STD among MSM, is a topic of concern. Based on the HAPA, this study investigated the influencing factors to predict risk compensation intention among MSM after taking HPV vaccination in southwest China. The structural equation model was used for confirmatory factor analysis. Overall, the model fits well.
This study found that 87.6% of MSM were willing to receive HPV vaccination, which is similar to the results of previous studies in China (86.2% and 82.8%) [19,20]. It can be seen that MSM had a high willingness to receive HPV vaccination. Risk compensation intention was investigated among all participants in a hypothetical situation of having received HPV vaccination. We only studied one form of risk compensation (changes in condom use intention). Theoretically, MSM might increase the number of sex partners while reducing the frequency of condom use. Such cases may just be rare occurrences [42]. The results showed that 14.1% of MSM would reduce their intention to use condoms after taking HPV vaccination. The incidence rate of risk compensation intention investigated in our study was higher than the previous study among MSM in Hong Kong (8.0%) [24], but lower than those related to some other biomedical prevention measures among men who have sex with men, such as voluntary medical male circumcision (15.9%) [43] and HIV vaccines (34.6%) [44]. This study suggests that risk compensation may not be a major barrier to receiving HPV vaccination among MSM. Nevertheless, the recognition of possible risk compensation is necessary to implement appropriate interventions for reducing the occurrence of risk compensation after HPV vaccination.
Structural equation model analysis showed that self-efficacy and positive outcome expectancy had a greater effect on behavioral intention, followed by negative outcome expectancy and risk perception. Risk perception was negatively correlated with risk compensation intention, that is, the reduced risk perception of HPV in MSM may lead to an increased willingness to risk compensation after taking HPV vaccination, which is similar to the results of previous studies on risk compensation behavior [42,45]. Our finding on the relationship between risk perception and risk compensation intention also confirmed the risk compensation theory. After taking HPV vaccination, MSM’s perceived risk may decrease, thereby increasing sexual risk behavior and generating risk compensation. Therefore, when promoting HPV vaccination, we should take care to remind MSM that the protective effect of the HPV vaccine is limited and it should not be used as a substitute for condom use, but rather as a complementary strategy to prevent STDs.
Positive outcome expectancy was one of the main influencing factors of risk compensation intention and was positively correlated with it. After receiving HPV vaccination, MSM believed that condomless anal intercourse would increase intimacy and trust between them and their male sex partners. Such a positive outcome expectancy was related to a higher intention to conduct risk compensation behavior. Several studies have also paid attention to the effect of intimacy and trust on sexual risk behavior among MSM. Condomless anal intercourse was seen by MSM as a bond to build a trusting relationship, and more than half of the participants cited it as a reason for not using condoms [46]. A quantitative study on MSM found that there was a relationship between relationship length, trust, and condom use. If the relationship lasted longer, the increase of trust would lead to a decrease in condom use [47]. Negative outcome expectancy had a negative effect on behavioral intention, and increasing it might reduce risk compensation. Based on this, future interventions should emphasize negative outcomes (e.g., condomless anal intercourse can give you HPV/other STDs.) and should improve the negative outcome expectancy of MSM to prevent the occurrence of risk compensation after HPV vaccination in this population.
Self-efficacy had a direct negative effect on risk compensation intention, and increasing self-efficacy may reduce risk compensation. Self-efficacy of condom use refers to how confident people are in their ability to use condoms. Previous studies have shown that lower self-efficacy of condom use was strongly associated with higher sexual risk behaviors [48,49,50], and our study confirmed this relationship. This finding highlights the importance of finding creative, effective ways to improve self-efficacy of condom use among MSM and suggests that achieving this goal may help reduce the likelihood of risk compensation after receiving HPV vaccination among MSM. Combined with the above negative correlation results, it is suggested that when promoting HPV vaccination to MSM, we should enhance the risk awareness of MSM, emphasize the negative outcome expectancy of condom use reduction, improve the self-efficacy of condom use, and decrease the positive outcome expectancy of condom use reduction to reduce the occurrence of risk compensation.
There are some limitations to the current study. First, our study is a cross-sectional survey, which limited causal inference. Cohort studies are needed to confirm these findings in the future. Second, MSM do not receive HPV vaccination. We investigated the risk compensation intention in a hypothetical situation of having received HPV vaccination. Although behavioral intention is deemed to be a major factor affecting actual behavior, some differences occur between actual behavior and intention. Third, due to the obscuring nature of the MSM, a non-probabilistic sampling method was used in this study. The results may be biased, which may limit the generalization of our findings to other MSM populations.
5. Conclusions
The HAPA model could be used to predict the risk compensation intention after taking HPV vaccination among MSM in southwest China, in which self-efficacy and positive outcome expectancy are the important predictor factors. Risk compensation may not be a major barrier to receiving HPV vaccination among MSM. Nevertheless, it is necessary to acknowledge possible risk compensation. Future research should focus on improving MSM’s risk perception of HPV, emphasize the negative outcome expectancy of condom use reduction, decrease the positive outcome expectancy of condom use reduction, and find effective ways to improve the self-efficacy of condom use among MSM, aiming to reduce the occurrence of risk compensation after HPV vaccination and providing interventions for subsequent risk coping strategies of such prevention measures.
Author Contributions
Conceptualization, Z.C.; methodology, Z.C. and H.J.; software, W.H. and H.P.; validation, Z.C., W.H. and H.P.; formal analysis, Z.C.; investigation, Z.C. and H.J.; resources, X.Z.; data curation, Z.C. and H.J.; writing—original draft preparation, Z.C. and C.Z.; supervision, X.Z.; project administration, X.Z.; funding acquisition, X.Z. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the National Key Project for Infectious Diseases of the Ministry of Science and Technology of China, grant number 2018ZX10721102-005.
Institutional Review Board Statement
This study was approved by the Ethics Committee of Chongqing Medical University (2019001, 28 May 2019).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data involved in the current study are available from the corresponding author on reasonable request.
Acknowledgments
The authors thank all the participants and investigators for their help. Furthermore, the authors express their gratitude to Bing Lin, Guiqian Shi, Hui Liu, and Guichuan Lai for comments and suggestions in the process of writing this manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Tian, T.; Wang, D.; Papamichael, C.; Yan, Z.; Guoyao, S.; Zhanlin, Z.; Mahan, Y.; Xiaoqing, T.; Zheng, G.; Jianghong, D. HPV vaccination acceptability among men who have sex with men in Urumqi, China. Hum. Vaccin. Immunother. 2019, 15, 1005–1012. [Google Scholar] [CrossRef]
- de Martel, C.; Plummer, M.; Vignat, J.; Franceschi, S. Worldwide burden of cancer attributable to HPV by site, country and HPV type. Int. J. Cancer 2017, 141, 664–670. [Google Scholar] [CrossRef] [PubMed]
- Marra, E.; Lin, C.; Clifford, G.M. Type-Specific Anal Human Papillomavirus Prevalence Among Men, According to Sexual Preference and HIV Status: A Systematic Literature Review and Meta-Analysis. J. Infect. Dis. 2019, 219, 590–598. [Google Scholar] [CrossRef] [PubMed]
- Ma, X.; Wang, Q.; Ong, J.J.; Fairley, C.K.; Su, S.; Peng, P.; Jing, J.; Wang, L.; Soe, N.N.; Cheng, F.; et al. Prevalence of human papillomavirus by geographical regions, sexual orientation and HIV status in China: A systematic review and meta-analysis. Sex. Transm. Infect. 2018, 94, 434–442. [Google Scholar] [CrossRef]
- Zhou, Y.; Lin, Y.F.; Gao, L.; Dai, J.; Luo, G.; Li, L.; Yuan, T.; Li, P.; Zhan, Y.; Gao, Y.; et al. Human papillomavirus prevalence among men who have sex with men in China: A systematic review and meta-analysis. Eur. J. Clin. Microbiol. Infect. Dis. Off. Publ. Eur. Soc. Clin. Microbiol. 2021, 40, 1357–1367. [Google Scholar] [CrossRef] [PubMed]
- Machalek, D.A.; Poynten, M.; Jin, F.; Fairley, C.K.; Farnsworth, A.; Garland, S.M.; Hillman, R.J.; Petoumenos, K.; Roberts, J.; Tabrizi, S.N.; et al. Anal human papillomavirus infection and associated neoplastic lesions in men who have sex with men: A systematic review and meta-analysis. Lancet Oncol. 2012, 13, 487–500. [Google Scholar] [CrossRef] [PubMed]
- Chow, E.P.; Tucker, J.D.; Wong, F.Y.; Nehl, E.J.; Wang, Y.; Zhuang, X.; Zhang, L. Disparities and risks of sexually transmissible infections among men who have sex with men in China: A meta-analysis and data synthesis. PLoS ONE 2014, 9, e89959. [Google Scholar] [CrossRef] [PubMed]
- Lacey, C.J.; Lowndes, C.M.; Shah, K.V. Chapter 4: Burden and management of non-cancerous HPV-related conditions: HPV-6/11 disease. Vaccine 2006, 24 (Suppl. S3), S35–S41. [Google Scholar] [CrossRef] [PubMed]
- Gillison, M.L.; Chaturvedi, A.K.; Lowy, D.R. HPV prophylactic vaccines and the potential prevention of noncervical cancers in both men and women. Cancer 2008, 113, 3036–3046. [Google Scholar] [CrossRef] [PubMed]
- Olesen, T.B.; Sand, F.L.; Rasmussen, C.L.; Albieri, V.; Toft, B.G.; Norrild, B.; Munk, C.; Kjær, S.K. Prevalence of human papillomavirus DNA and p16(INK4a) in penile cancer and penile intraepithelial neoplasia: A systematic review and meta-analysis. Lancet Oncol. 2019, 20, 145–158. [Google Scholar] [CrossRef]
- Ren, X.; Qiu, L.; Ke, W.; Zou, H.; Liu, A.; Wu, T. Awareness and acceptance of HPV vaccination for condyloma acuminata among men who have sex with men in China. Hum. Vaccin. Immunother. 2022, 18, 2115267. [Google Scholar] [CrossRef]
- Petrosky, E.; Bocchini, J.A., Jr.; Hariri, S.; Chesson, H.; Curtis, C.R.; Saraiya, M.; Unger, E.R.; Markowitz, L.E. Use of 9-valent human papillomavirus (HPV) vaccine: Updated HPV vaccination recommendations of the advisory committee on immunization practices. MMWR Morb. Mortal. Wkly. Rep. 2015, 64, 300–304. [Google Scholar] [PubMed]
- Zhang, L.; Regan, D.G.; Ong, J.J.; Gambhir, M.; Chow, E.P.F.; Zou, H.; Law, M.; Hocking, J.; Fairley, C.K. Targeted human papillomavirus vaccination for young men who have sex with men in Australia yields significant population benefits and is cost-effective. Vaccine 2017, 35, 4923–4929. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.J. Targeted human papillomavirus vaccination of men who have sex with men in the USA: A cost-effectiveness modelling analysis. Lancet Infect. Dis. 2010, 10, 845–852. [Google Scholar] [CrossRef]
- Ben Hadj Yahia, M.B.; Jouin-Bortolotti, A.; Dervaux, B. Extending the Human Papillomavirus Vaccination Programme to Include Males in High-Income Countries: A Systematic Review of the Cost-Effectiveness Studies. Clin. Drug Investig. 2015, 35, 471–485. [Google Scholar] [CrossRef]
- Markowitz, L.E.; Dunne, E.F.; Saraiya, M.; Chesson, H.W.; Curtis, C.R.; Gee, J.; Bocchini, J.A., Jr.; Unger, E.R. Human papillomavirus vaccination: Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm. Rep. Morb. Mortal. Wkly. Rep. Recomm. Rep. 2014, 63, 1–30. [Google Scholar]
- Human papillomavirus vaccines: WHO position paper, May 2017-Recommendations. Vaccine 2017, 35, 5753–5755. [CrossRef] [PubMed]
- Huang, R.; Wang, Z.; Yuan, T.; Nadarzynski, T.; Qian, H.Z.; Li, P.; Meng, X.; Wang, G.; Zhou, Y.; Luo, D.; et al. Using protection motivation theory to explain the intention to initiate human papillomavirus vaccination among men who have sex with men in China. Tumour Virus Res. 2021, 12, 200222. [Google Scholar] [CrossRef] [PubMed]
- He, W.; Pan, H.; Lin, B.; Zhong, X. Analysis of HPV Vaccination Willingness amongst HIV-Negative Men Who Have Sex with Men in China. Vaccines 2021, 9, 1069. [Google Scholar] [CrossRef] [PubMed]
- Pan, H.; He, W.; Lin, B.; Zhong, X. Factors influencing HPV vaccination willingness among men who have sex with men in China: A structural equation modeling analysis. Hum. Vaccin. Immunother. 2022, 18, 2038504. [Google Scholar] [CrossRef]
- Wilde, G.J. Risk homeostasis theory: An overview. Inj. Prev. J. Int. Soc. Child Adolesc. Inj. Prev. 1998, 4, 89–91. [Google Scholar] [CrossRef]
- Traeger, M.W.; Cornelisse, V.J.; Asselin, J.; Price, B.; Roth, N.J.; Willcox, J.; Tee, B.K.; Fairley, C.K.; Chang, C.C.; Armishaw, J.; et al. Association of HIV Preexposure Prophylaxis With Incidence of Sexually Transmitted Infections Among Individuals at High Risk of HIV Infection. JAMA 2019, 321, 1380–1390. [Google Scholar] [CrossRef] [PubMed]
- Golub, S.A.; Kowalczyk, W.; Weinberger, C.L.; Parsons, J.T. Preexposure prophylaxis and predicted condom use among high-risk men who have sex with men. J. Acquir. Immune Defic. Syndr. 2010, 54, 548–555. [Google Scholar] [CrossRef] [PubMed]
- Wu, T.; Qu, S.; Fang, Y.; Ip, M.; Wang, Z. Behavioral intention to perform risk compensation behaviors after receiving HPV vaccination among men who have sex with men in China. Hum. Vaccin. Immunother. 2019, 15, 1737–1744. [Google Scholar] [CrossRef]
- Hansen, B.T. No evidence that HPV vaccination leads to sexual risk compensation. Hum. Vaccin. Immunother. 2016, 12, 1451–1453. [Google Scholar] [CrossRef]
- Schwarzer, R.; Schuz, B.; Ziegelmann, J.P.; Lippke, S.; Luszczynska, A.; Scholz, U. Adoption and maintenance of four health behaviors: Theory-guided longitudinal studies on dental flossing, seat belt use, dietary behavior, and physical activity. Ann. Behav. Med. Publ. Soc. Behav. Med. 2007, 33, 156–166. [Google Scholar] [CrossRef] [PubMed]
- Schwarzer, R.; Lippke, S.; Luszczynska, A. Mechanisms of health behavior change in persons with chronic illness or disability: The Health Action Process Approach (HAPA). Rehabil. Psychol. 2011, 56, 161–170. [Google Scholar] [CrossRef] [PubMed]
- Smith, S.R.; Kroon, J.; Schwarzer, R.; Hamilton, K. Social-cognitive predictors of parental supervised toothbrushing: An application of the health action process approach. Br. J. Health Psychol. 2021, 26, 995–1015. [Google Scholar] [CrossRef] [PubMed]
- Tsui, H.Y.; Lau, J.T.; Wang, Z.; Gross, D.L.; Wu, A.M.; Cao, W.; Gu, J.; Li, S. Applying the pre-intentional phase of the Health Action Process Approach (HAPA) Model to investigate factors associated with intention on consistent condom use with various types of female sex partners among males who inject drugs in China. AIDS Care 2016, 28, 1079–1088. [Google Scholar] [CrossRef]
- Williams, R.J.; Herzog, T.A.; Simmons, V.N. Risk perception and motivation to quit smoking: A partial test of the Health Action Process Approach. Addict. Behav. 2011, 36, 789–791. [Google Scholar] [CrossRef] [PubMed]
- Scholz, U.; Keller, R.; Perren, S. Predicting behavioral intentions and physical exercise: A test of the health action process approach at the intrapersonal level. Health Psychol. Off. J. Div. Health Psychol. Am. Psychol. Assoc. 2009, 28, 702–708. [Google Scholar] [CrossRef]
- Payaprom, Y.; Bennett, P.; Alabaster, E.; Tantipong, H. Using the Health Action Process Approach and implementation intentions to increase flu vaccine uptake in high risk Thai individuals: A controlled before-after trial. Health Psychol. Off. J. Div. Health Psychol. Am. Psychol. Assoc. 2011, 30, 492–500. [Google Scholar] [CrossRef]
- Yu, Y.; Jia, W.; Lau, M.M.C.; Lau, J.T.F. Levels and factors derived from the Health Action Process Approach of behavioral intentions to take up COVID-19 vaccination: A random population-based study. Vaccine 2022, 40, 612–620. [Google Scholar] [CrossRef] [PubMed]
- Ni, Y.; Lu, Y.; He, X.; Li, Y.; Li, Y.; Guo, S.; Ong, J.J.; Xu, C.; Wang, X.; Yan, X.; et al. Self-sampled specimens demonstrate comparable accuracy and consistency to clinician-sampled specimens for HPV detection among men who have sex with men in China. Sex. Transm. Infect. 2022, 99, 104–109. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Luo, Y.; Zhong, R.; Law, P.T.Y.; Boon, S.S.; Chen, Z.; Wong, C.H.; Chan, P.K.S. Role of polycyclic aromatic hydrocarbons as a co-factor in human papillomavirus-mediated carcinogenesis. BMC Cancer 2019, 19, 138. [Google Scholar] [CrossRef]
- Vawda, N.; Banerjee, R.N.; Debenham, B.J. Impact of Smoking on Outcomes of HPV-related Oropharyngeal Cancer Treated with Primary Radiation or Surgery. Int. J. Radiat. Oncol. Biol. Phys. 2019, 103, 1125–1131. [Google Scholar] [CrossRef] [PubMed]
- Camargo, M.; Del Río-Ospina, L.; Soto-De León, S.C.; Sánchez, R.; Pineda-Peña, A.C.; Sussmann, O.; Patarroyo, M.E.; Patarroyo, M.A. Association of HIV status with infection by multiple HPV types. Trop. Med. Int. Health TM IH 2018, 23, 1259–1268. [Google Scholar] [CrossRef]
- Giannini, A.; Di Donato, V.; Sopracordevole, F.; Ciavattini, A.; Ghelardi, A.; Vizza, E.; D’Oria, O.; Simoncini, T.; Plotti, F.; Casarin, J.; et al. Outcomes of High-Grade Cervical Dysplasia with Positive Margins and HPV Persistence after Cervical Conization. Vaccines 2023, 11, 698. [Google Scholar] [CrossRef]
- Newman, P.A.; Lee, S.J.; Duan, N.; Rudy, E.; Nakazono, T.K.; Boscardin, J.; Kakinami, L.; Shoptaw, S.; Diamant, A.; Cunningham, W.E. Preventive HIV vaccine acceptability and behavioral risk compensation among a random sample of high-risk adults in Los Angeles (LA VOICES). Health Serv. Res. 2009, 44, 2167–2179. [Google Scholar] [CrossRef]
- Marlow, L.A.; Forster, A.S.; Wardle, J.; Waller, J. Mothers’ and adolescents’ beliefs about risk compensation following HPV vaccination. J. Adolesc. Health Off. Publ. Soc. Adolesc. Med. 2009, 44, 446–451. [Google Scholar] [CrossRef] [PubMed]
- Sun, L.X.; Chen, L.L.; Chen, W.Y.; Zhang, M.X.; Yang, M.G.; Mo, L.C.; Zhu, J.J.; Tung, T.H.; Li, F.P. Association between health behaviours and the COVID-19 vaccination: Risk compensation among healthcare workers in Taizhou, China. Hum. Vaccin. Immunother. 2022, 18, 2029257. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Lau, J.T.; Gu, J. Acceptability of circumcision among clients of female sex worker in Hong Kong. AIDS Behav. 2012, 16, 1836–1845. [Google Scholar] [CrossRef] [PubMed]
- Lau, J.T.; Zhang, J.; Yan, H.; Lin, C.; Choi, K.C.; Wang, Z.; Hao, C.; Huan, X.; Yang, H. Acceptability of circumcision as a means of HIV prevention among men who have sex with men in China. AIDS Care 2011, 23, 1472–1482. [Google Scholar] [CrossRef]
- Newman, P.A.; Roungprakhon, S.; Tepjan, S.; Yim, S. Preventive HIV vaccine acceptability and behavioral risk compensation among high-risk men who have sex with men and transgenders in Thailand. Vaccine 2010, 28, 958–964. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Feng, T.; Lau, J.T. Prevalence and associated factors of behavioral intention for risk compensation following voluntary medical male circumcision among male sexually transmitted diseases patients in China. AIDS Care 2016, 28, 1332–1337. [Google Scholar] [CrossRef] [PubMed]
- Giano, Z.; Kavanaugh, K.E.; Durham, A.R.; Currin, J.M.; Wheeler, D.L.; Croff, J.M.; Hubach, R.D. Factors Associated with Condom Use among a Sample of Men Who Have Sex with Men (MSM) Residing in Rural Oklahoma. J. Homosex. 2020, 67, 1881–1901. [Google Scholar] [CrossRef]
- Hoff, C.C.; Chakravarty, D.; Beougher, S.C.; Neilands, T.B.; Darbes, L.A. Relationship characteristics associated with sexual risk behavior among MSM in committed relationships. AIDS Patient Care STDs 2012, 26, 738–745. [Google Scholar] [CrossRef] [PubMed]
- Klein, H. Condom use self-efficacy and HIV risk practices among men who use the internet to find male partners for unprotected sex. Am. J. Men’s Health 2014, 8, 190–204. [Google Scholar] [CrossRef]
- Tucker, J.S.; Elliott, M.N.; Wenzel, S.L.; Hambarsoomian, K. Relationship commitment and its implications for unprotected sex among impoverished women living in shelters and low-income housing in Los Angeles County. Health Psychol. Off. J. Div. Health Psychol. Am. Psychol. Assoc. 2007, 26, 644–649. [Google Scholar] [CrossRef] [PubMed]
- O’Leary, A.; Jemmott, L.S.; Jemmott, J.B. Mediation analysis of an effective sexual risk-reduction intervention for women: The importance of self-efficacy. Health Psychol. Off. J. Div. Health Psychol. Am. Psychol. Assoc. 2008, 27, S180–S184. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).