The Impact of SARS-CoV-2 Immune Status and Societal Restrictions in Controlling COVID-19 across the World
Abstract
:1. Introduction
2. Methods
2.1. Government Stringency Index
2.2. Statistical Analysis
3. Results
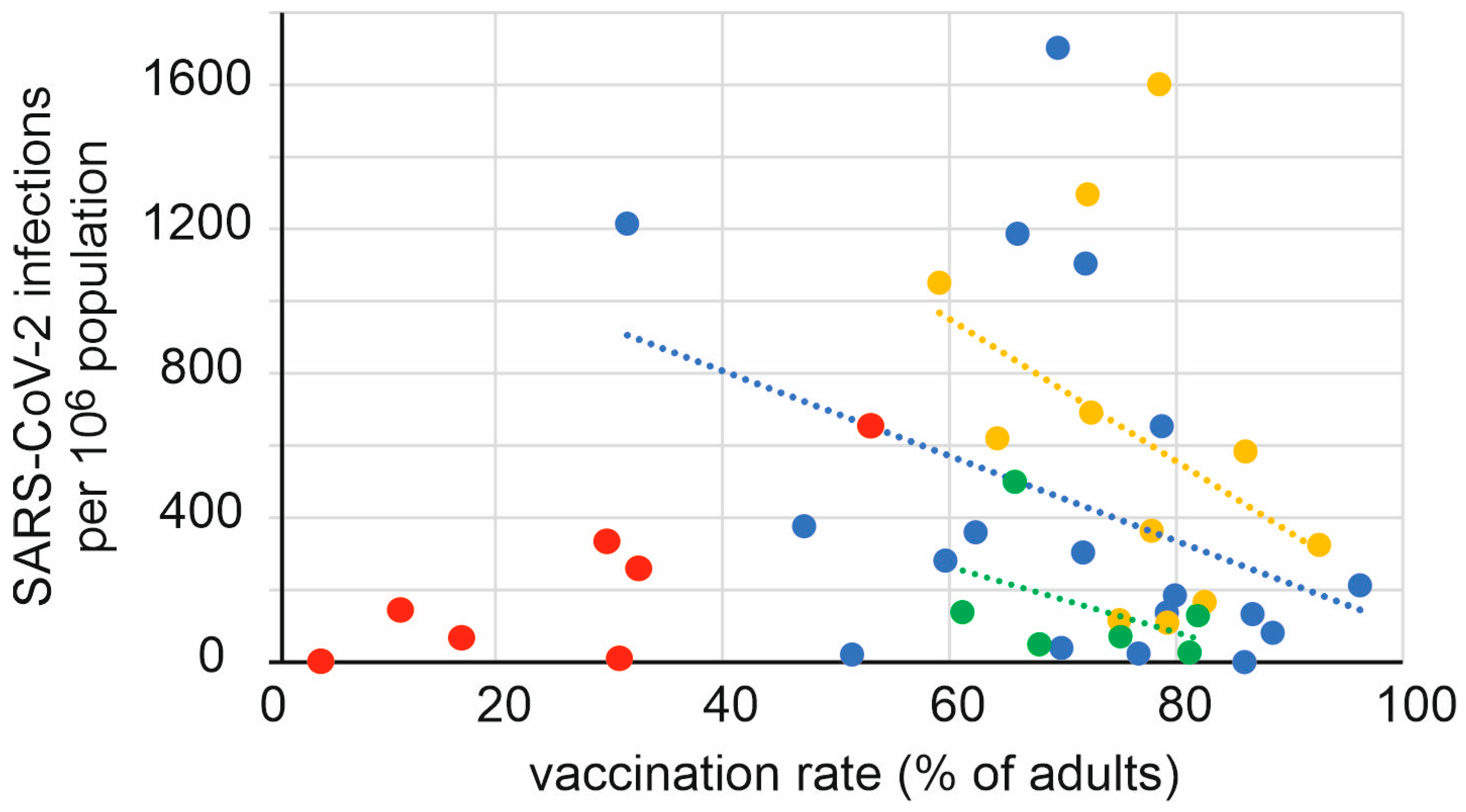
3.1. Prevention of SARS-CoV-2 Infection by Vaccination
3.2. Societal Restrictions
3.3. Introduction and Effect of a COVID Pass
4. Discussion
5. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zhu, N.; Zhang, D.; Wang, W.; Li, X.; Yang, B.; Song, J.; Zhao, X.; Huang, B.; Shi, W.; Lu, R.; et al. China Novel Coronavirus Investigating and Research Team. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N. Engl. J. Med. 2020, 382, 727–733. [Google Scholar] [CrossRef]
- Cucinotta, D.; Vanelli, M. WHO Declares COVID-19 a Pandemic. Acta Biomed. 2020, 91, 157–160. [Google Scholar] [CrossRef] [PubMed]
- Sohrabi, C.; Alsafi, Z.; O’Neill, N.; Khan, M.; Kerwan, A.; Al-Jabir, A.; Iosifidis, C.; Agha, R. World Health Organization declares global emergency: A review of the 2019 novel coronavirus (COVID-19). Int. J. Surg. 2020, 76, 71–76. [Google Scholar] [CrossRef] [PubMed]
- Hiscott, J.; Alexandridi, M.; Muscolini, M.; Tassone, E.; Palermo, E.; Soultsioti, M.; Zevini, A. The global impact of the coronavirus pandemic. Cytokine Growth Factor Rev. 2020, 53, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Shah, S.G.S.; Farrow, A. A commentary on “World Health Organization declares global emergency: A review of the 2019 novel Coronavirus (COVID-19)”. Int. J. Surg. 2020, 76, 128–129. [Google Scholar] [CrossRef]
- WHO Coronavirus (COVID-19) Dashboard. (n.d.). WHO.int. 2022. Available online: https://covid19.who.int/ (accessed on 31 March 2022).
- Ritchie, H.; Mathieu, E.; Rodés-Guirao, L.; Appel, C.; Giattino, C.; Ortiz-Ospina, E.; Hasell, J.; Macdonald, B.; Beltekian, D.; Max Roser, M. Coronavirus Pandemic (COVID-19). 2020. Available online: https://ourworldindata.org/coronavirus (accessed on 22 October 2022).
- Greer, S.L.; King, E.J.; da Fonseca, E.M.; Peralta-Santos, A. The comparative politics of COVID-19: The need to understand government responses. Glob. Public Health 2020, 15, 1413–1416. [Google Scholar] [CrossRef]
- Khailany, R.A.; Safdar, M.; Ozaslan, M. Genomic characterization of a novel SARS-CoV-2. Gene Rep. 2020, 19, 100682. [Google Scholar] [CrossRef]
- Golob, J.L.; Lugogo, N.; Lauring, A.S.; Lok, A.S. SARS-CoV-2 vaccines: A triumph of science and collaboration. JCI Insight 2021, 6, e149187. [Google Scholar] [CrossRef]
- Rijkers, G.T.; Weterings, N.; Obregon-Henao, A.; Lepolder, M.; Dutt, T.S.; van Overveld, F.J.; Henao-Tamayo, M. Antigen Presentation of mRNA-Based and Virus-Vectored SARS-CoV-2 Vaccines. Vaccines 2021, 9, 848. [Google Scholar] [CrossRef]
- Chen, L.H.; Petersen, E.; Blumberg, L.; Piyaphanee, W.; Steffen, R. COVID-19 health passes: Current status and prospects for a global approach. J. Travel Med. 2021, 28, taab118. [Google Scholar] [CrossRef]
- Ward, J.K.; Gauna, F.; Gagneux-Brunon, A.; Botelho-Nevers, E.; Cracowski, J.L.; Khouri, C.; Launay, O.; Verger, P.; Peretti-Watel, P. The French health pass holds lessons for manda-tory COVID-19 vaccination. Nat. Med. 2022, 28, 232–235. [Google Scholar] [CrossRef] [PubMed]
- Wang, B.; Ping, Y. A comparative analysis of COVID-19 vaccination certificates in 12 countries/regions around the world: Rationalising health policies for international travel and domestic social activities during the pandemic. Health Policy 2022, 126, 755–762. [Google Scholar] [CrossRef] [PubMed]
- Hale, T.; Angrist, N.; Goldszmidt, R.; Kira, B.; Petherick, A.; Phillips, T.; Webster, S.; Cameron-Blake, E.; Hallas, L.; Majumdar, S.; et al. A global panel database of pandemic policies (Oxford COVID-19 Government Response Tracker). Nat. Hum. Behav. 2021, 5, 529–538. [Google Scholar] [CrossRef]
- Human Development Reports. Available online: https://hdr.undp.org/data-center/human-development-index (accessed on 23 June 2023).
- The World Bank. Available online: https://data.worldbank.org/ (accessed on 23 June 2023).
- Stobart, A.; Duckett, S. Australia’s Response to COVID-19. Health Econ. Policy Law 2022, 17, 95–106. [Google Scholar] [CrossRef]
- Alshammari, T.M.; Alenzi, K.A.; Alnofal, F.A.; Fradees, G.; Altebainawi, A.F. Are countries’ precautionary actions against COVID-19 effective? An assessment study of 175 countries worldwide. Saudi Pharm. J. 2021, 29, 391–409. [Google Scholar] [CrossRef] [PubMed]
- Cao, X.; Li, Y.; Zi, Y.; Zhu, Y. The shift of percent excess mortality from zero-COVID policy to living-with-COVID policy in Singapore, South Korea, Australia, New Zealand and Hong Kong SAR. Front. Public Health 2023, 11, 1085451. [Google Scholar] [CrossRef]
- Pardhan, S.; Drydakis, N. Associating the Change in New COVID-19 Cases to GDP per Capita in 38 European Countries in the First Wave of the Pandemic. Front. Public Health 2021, 8, 582140. [Google Scholar] [CrossRef]
- Pettit, S.D.; Jerome, K.R.; Rouquié, D.; Mari, B.; Barbry, P.; Kanda, Y.; Matsumoto, M.; Hester, S.; Wehmas, L.; Botten, J.W.; et al. ‘All In’: A pragmatic framework for COVID-19 testing and action on a global scale. EMBO Mol. Med. 2020, 12, e12634. [Google Scholar] [CrossRef]
- Gupta, M.; Wahl, B.; Adhikari, B.; Bar-Zeev, N.; Bhandari, S.; Coria, A.; Erchick, D.J.; Gupta, N.; Hariyani, S.; Kagucia, E.W.; et al. The need for COVID-19 research in low- and middle-income countries. Glob. Health Res. Policy 2020, 5, 33. [Google Scholar] [CrossRef]
- Dzinamarira, T.; Dzobo, M.; Chitungo, I. COVID-19: A perspective on Africa’s capacity and response. J. Med. Virol. 2020, 92, 2465–2472. [Google Scholar] [CrossRef]
- Burki, T.K. Undetected COVID-19 cases in Africa. Lancet Respir. Med. 2021, 9, e121. [Google Scholar] [CrossRef] [PubMed]
- Català, M.; Pino, D.; Marchena, M.; Palacios, P.; Urdiales, T.; Cardona, P.J.; Alonso, S.; López-Codina, D.; Prats, C.; Alvarez-Lacalle, E. Robust estimation of diagnostic rate and real incidence of COVID-19 for European policymakers. PLoS ONE 2021, 16, e0243701. [Google Scholar] [CrossRef] [PubMed]
- Msemburi, W.; Karlinsky, A.; Knutson, V.; Aleshin-Guendel, S.; Chatterji, S.; Wakefield, J. The WHO estimates of excess mortality associated with the COVID-19 pandemic. Nature 2023, 613, 130–137. [Google Scholar] [CrossRef] [PubMed]
- Vandrevala, T.; Montague, A.; Terry, P.; Fielder, M.D. Willingness of the UK public to volunteer for testing in relation to the COVID-19 pandemic. BMC Public Health 2022, 22, 565. [Google Scholar] [CrossRef] [PubMed]
- Taylor, L. COVID-19: Omicron drives weekly record high in global infections. BMJ 2022, 376, o66. [Google Scholar] [CrossRef] [PubMed]
- Willyard, C. What the Omicron wave is revealing about human immunity. Nature 2022, 602, 22–25. [Google Scholar] [CrossRef]
- Kishore, K.; Jaswal, V.; Pandey, A.K.; Verma, M.; Koushal, V. Utility of the Comprehensive Health and Stringency Indexes in Evaluating Government Responses for Containing the Spread of COVID-19 in India: Ecological Time-Series Study. JMIR Public Health Surveill. 2023, 9, e38371. [Google Scholar] [CrossRef]
- Liu, Y.; Rocklöv, J. The effective reproductive number of the Omicron variant of SARS-CoV-2 is several times relative to Delta. J. Travel Med. 2022, 29, taac037. [Google Scholar] [CrossRef]
- Ren, S.Y.; Wang, W.B.; Gao, R.D.; Zhou, A.M. Omicron variant (B.1.1.529) of SARS-CoV-2: Mutation, infectivity, transmission, and vaccine resistance. World J. Clin. Cases 2022, 10, 1–11. [Google Scholar] [CrossRef]
- Sharun, K.; Tiwari, R.; Dhama, K.; Rabaan, A.A.; Alhumaid, S. COVID-19 vaccination passport: Prospects, scientific feasibility, and ethical concerns. Hum. Vaccin. Immunother. 2021, 17, 4108–4111. [Google Scholar] [CrossRef]
- Hall, M.A.; Studdert, D.M. Privileges and Immunity Certification During the COVID-19 Pandemic. JAMA 2020, 323, 2243–2244. [Google Scholar] [CrossRef]
- Andeweg, S.P.; de Gier, B.; Eggink, D.; van den Ende, C.; van Maarseveen, N.; Ali, L.; Vlaemynck, B.; Schepers, R.; Hahné, S.J.M.; Reusken, C.B.E.M.; et al. Protection of COVID-19 vaccination and previous infection against Omicron BA.1, BA.2 and Delta SARS-CoV-2 infections. Nat. Commun. 2022, 13, 4738. [Google Scholar] [CrossRef] [PubMed]
- Keyel, A.C.; Russell, A.; Plitnick, J.; Rowlands, J.V.; Lamson, D.M.; Rosenberg, E.; St George, K. SARS-CoV-2 Vaccine Breakthrough by Omicron and Delta Variants, New York, USA. Emerg. Infect. Dis. 2022, 28, 1990–1998. [Google Scholar] [CrossRef] [PubMed]
- Du, Z.; Hong, H.; Wang, S.; Ma, L.; Liu, C.; Bai, Y.; Adam, D.C.; Tian, L.; Wang, L.; Lau, E.H.Y.; et al. Reproduction Number of the Omicron Variant Triples That of the Delta Variant. Viruses 2022, 14, 821. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Liu, B.; Zhang, S.; Huang, N.; Zhao, T.; Lu, Q.B.; Cui, F. Differences in incidence and fatality of COVID-19 by SARS-CoV-2 Omicron variant versus Delta variant in relation to vaccine coverage: A world-wide review. J. Med. Virol. 2023, 95, e28118. [Google Scholar] [CrossRef] [PubMed]
- Ward, I.L.; Bermingham, C.; Ayoubkhani, D.; Gethings, O.J.; Pouwels, K.B.; Yates, T.; Khunti, K.; Hippisley-Cox, J.; Banerjee, A.; Walker, A.S.; et al. Risk of covid-19 related deaths for SARS-CoV-2 omicron (B.1.1.529) compared with delta (B.1.617.2): Retrospective cohort study. BMJ 2022, 378, e070695. [Google Scholar] [CrossRef]
- Lorenzo-Redondo, R.; Ozer, E.A.; Hultquist, J.F. COVID-19: Is omicron less lethal than delta? BMJ 2022, 378, o1806. [Google Scholar] [CrossRef]
- Kim, Y.Y.; Choe, Y.J.; Kim, J.; Kim, R.K.; Jang, E.J.; Lee, H.; Yi, S.; Lee, S.; Park, Y.J. Vaccine Effectiveness Against Severe Disease and Death for Patients With COVID-19 During the Delta-Dominant and Omicron-Emerging Periods: A K-COVE Study. J. Korean Med. Sci. 2023, 38, e87. [Google Scholar] [CrossRef]
- Dobrowolska, K.; Brzdęk, M.; Zarębska-Michaluk, D.; Rzymski, P.; Rogalska, M.; Moniuszko-Malinowska, A.; Szymanek-Pasternak, A.; Jaroszewicz, J.; Dutkiewicz, E.; Kowalska, J.; et al. Differences between the course of SARS-CoV-2 infections in the periods of the Delta and Omicron variants dominance in Poland. Pol. Arch. Intern. Med. 2023, 16403. [Google Scholar] [CrossRef]
- Intawong, K.; Chariyalertsak, S.; Chalom, K.; Wonghirundecha, T.; Kowatcharakul, W.; Ayood, P.; Thongprachum, A.; Chotirosniramit, N.; Noppakun, K.; Khwanngern, K.; et al. Reduction in severity and mortality in COVID-19 patients owing to heterologous third and fourth-dose vaccines during the periods of delta and omicron predominance in Thailand. Int. J. Infect. Dis. 2023, 126, 31–38. [Google Scholar] [CrossRef]
- Mahmoudi, J.; Xiong, C. How social distancing, mobility, and preventive policies affect COVID-19 outcomes: Big data-driven evidence from the District of Columbia-Maryland-Virginia (DMV) megaregion. PLoS ONE 2022, 17, e0263820. [Google Scholar] [CrossRef] [PubMed]
- Gambau, B.; Palomino, J.C.; Rodríguez, J.G.; Sebastian, R. COVID-19 restrictions in the US: Wage vulnerability by education, race and gender. Appl. Econ. 2022, 54, 2900–2915. [Google Scholar] [CrossRef]
- World Health Organization. Virtual Press Conference on COVID-19 & Other Global Health Emergencies. Available online: https://www.who.int/publications/m/item/virtual-press-conference-on-covid-19---other-global-health-emergencies (accessed on 17 March 2023).
- Harris, E. WHO Declares End of COVID-19 Global Health Emergency. JAMA 2023, 329, 1817. [Google Scholar] [CrossRef] [PubMed]
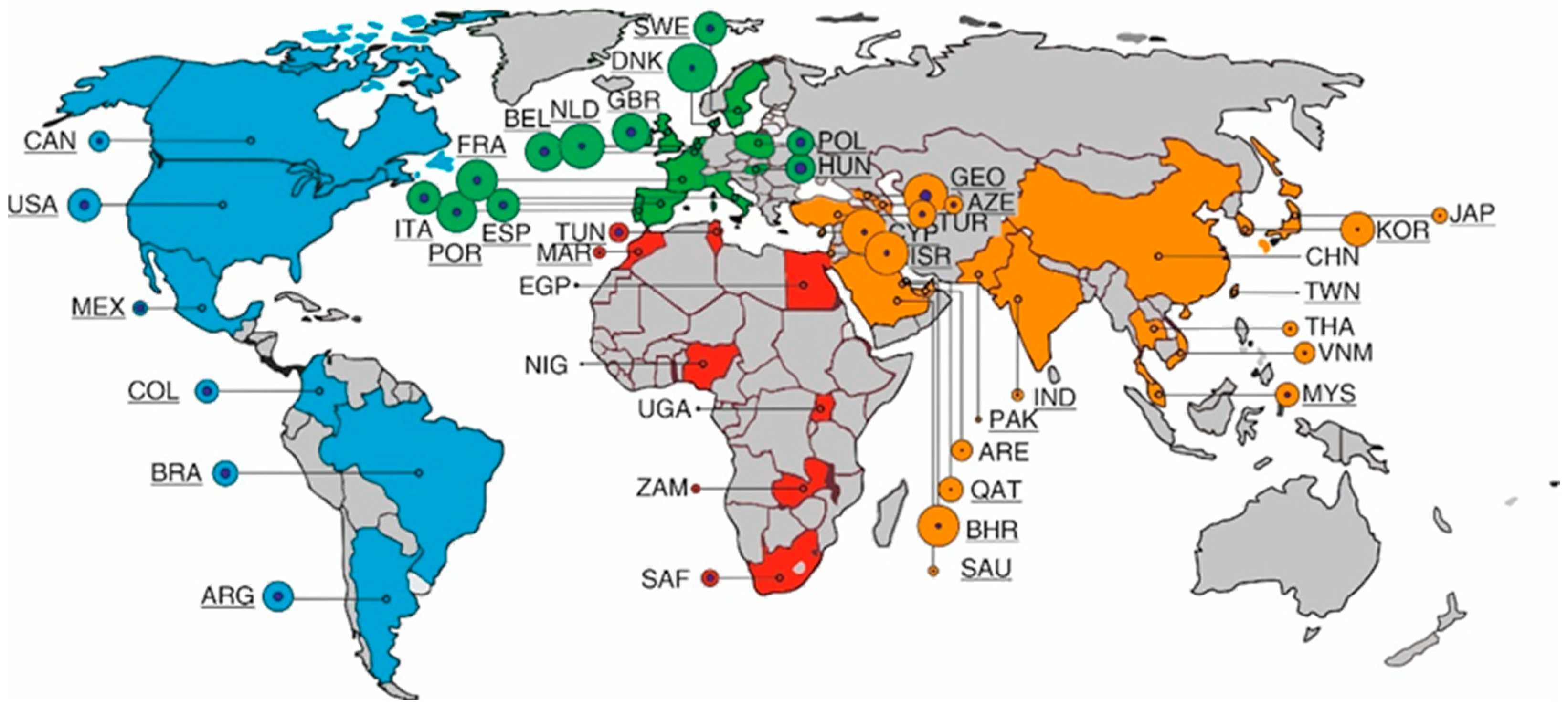



| Continent and Country or Territory | Population (as of 2020) [16,17] | Cases (Cumulative per Million People; 31 March 2022) | Deaths (Cumulative per Million People; 31 March 2022) | Vaccination Rate (per 31 March 2022) in Percentage | GDP per Capita (US$) 2020 | HDI |
|---|---|---|---|---|---|---|
| Asia | ||||||
| Azerbaijan | 10,139,177 | 76,450 | 935 | 47.19 | 5083 | 756 |
| Bahrain | 1,701,575 | 376,128 | 998 | 69.56 | 19,514 | 852 |
| China | 1,439,323,776 | 155 | 3 | 86.02 | 10,370 | 761 |
| Cyprus | 1,207,359 | 475,863 | 1046 | 72.02 | 26,372 | 887 |
| Georgia | 3,989,167 | 440,071 | 4470 | 31.59 | 4447 | 812 |
| India | 1,396,378,127 | 30,360 | 367 | 59.66 | 1811 | 645 |
| Israel | 8,655,535 | 413,196 | 1109 | 65.99 | 37,488 | 919 |
| Japan | 126,476,461 | 52,547 | 226 | 79.86 | 34,813 | 919 |
| Malaysia | 32,365,999 | 123,263 | 1029 | 78.74 | 10,631 | 810 |
| Pakistan | 220,892,340 | 20,618 | 129 | 51.41 | 1446 | 557 |
| Qatar | 2,881,053 | 134,050 | 251 | 88.5 | 56,026 | 848 |
| Saudi Arabia | 34,813,871 | 29,563 | 248 | 69.88 | 18,691 | 854 |
| South Korea | 51,269,185 | 252,734 | 313 | 86.73 | 31,327 | 916 |
| Taiwan | 23,816,775 | 969 | 36 | 76.66 | 28,306 | 949 |
| Thailand | 69,799,978 | 50,222 | 349 | 71.8 | 6198 | 777 |
| Turkey | 84,339,067 | 173,963 | 1148 | 62.3 | 12,038 | 820 |
| United Arab Emirates | 9,890,402 | 94,372 | 243 | 96.22 | 40,438 | 890 |
| Vietnam | 97,338,579 | 96,471 | 423 | 79.15 | 2655 | 704 |
| Africa | ||||||
| Egypt | 102,334,404 | 4,552 | 220 | 30.89 | 4028 | 707 |
| Morocco | 36,910,560 | 31,053 | 428 | 32.56 | 2818 | 686 |
| Nigeria | 206,139,589 | 1,168 | 14 | 4.52 | 2396 | 539 |
| South Africa | 59,308,690 | 62,060 | 1669 | 29.81 | 5659 | 709 |
| Tunisia | 11,818,619 | 83,835 | 2292 | 53.2 | 3780 | 740 |
| Uganda | 45,741,007 | 3468 | 76 | 17.01 | 891 | 544 |
| Zambia | 18,383,955 | 15,813 | 198 | 11.62 | 1273 | 584 |
| Europe | ||||||
| Belgium | 11,589,623 | 326,663 | 2638 | 78.52 | 45,189 | 931 |
| Denmark | 5,792,202 | 519,331 | 963 | 82.5 | 56,202 | 940 |
| France | 65,273,511 | 376,011 | 2097 | 77.84 | 35,785 | 901 |
| Hungary | 9,660,351 | 185,528 | 4558 | 59.13 | 14,368 | 854 |
| Italy | 60,461,826 | 246,758 | 2697 | 79.23 | 29,359 | 892 |
| Netherlands | 17,134,872 | 446,569 | 1255 | 72.17 | 46,345 | 944 |
| Poland | 37,846,611 | 149,482 | 2886 | 64.23 | 14,660 | 880 |
| Portugal | 10,196,709 | 362,778 | 2097 | 92.6 | 19,771 | 864 |
| Spain | 46,754,778 | 241,981 | 2149 | 86.09 | 24,939 | 904 |
| Sweden | 10,099,265 | 235,250 | 1724 | 74.98 | 51,539 | 945 |
| United Kingdom | 67,886,011 | 313,253 | 2846 | 72.49 | 43,020 | 932 |
| America | ||||||
| United States | 331,002,651 | 237,189 | 2905 | 65.77 | 58,203 | 926 |
| Canada | 37,742,154 | 90,526 | 977 | 81.92 | 42,258 | 929 |
| Colombia | 50,882,891 | 117,294 | 2691 | 67.93 | 5892 | 767 |
| Brazil | 212,559,417 | 138,962 | 3064 | 75.1 | 8228 | 765 |
| Argentina | 45,195,774 | 198,529 | 2812 | 81.18 | 11,334 | 845 |
| Mexico | 128,932,753 | 44,346 | 2532 | 61.19 | 8909 | 779 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stroo, J.; Lepolder, M.; Murk, J.-L.; Rijkers, G.T. The Impact of SARS-CoV-2 Immune Status and Societal Restrictions in Controlling COVID-19 across the World. Vaccines 2023, 11, 1407. https://doi.org/10.3390/vaccines11091407
Stroo J, Lepolder M, Murk J-L, Rijkers GT. The Impact of SARS-CoV-2 Immune Status and Societal Restrictions in Controlling COVID-19 across the World. Vaccines. 2023; 11(9):1407. https://doi.org/10.3390/vaccines11091407
Chicago/Turabian StyleStroo, Jasmijn, Michaëla Lepolder, Jean-Luc Murk, and Ger T. Rijkers. 2023. "The Impact of SARS-CoV-2 Immune Status and Societal Restrictions in Controlling COVID-19 across the World" Vaccines 11, no. 9: 1407. https://doi.org/10.3390/vaccines11091407
APA StyleStroo, J., Lepolder, M., Murk, J.-L., & Rijkers, G. T. (2023). The Impact of SARS-CoV-2 Immune Status and Societal Restrictions in Controlling COVID-19 across the World. Vaccines, 11(9), 1407. https://doi.org/10.3390/vaccines11091407







