Influenza Vaccination Uptake and Prognostic Factors among Health Professionals in Italy: Results from the Nationwide Surveillance PASSI 2015–2018
Abstract
1. Introduction
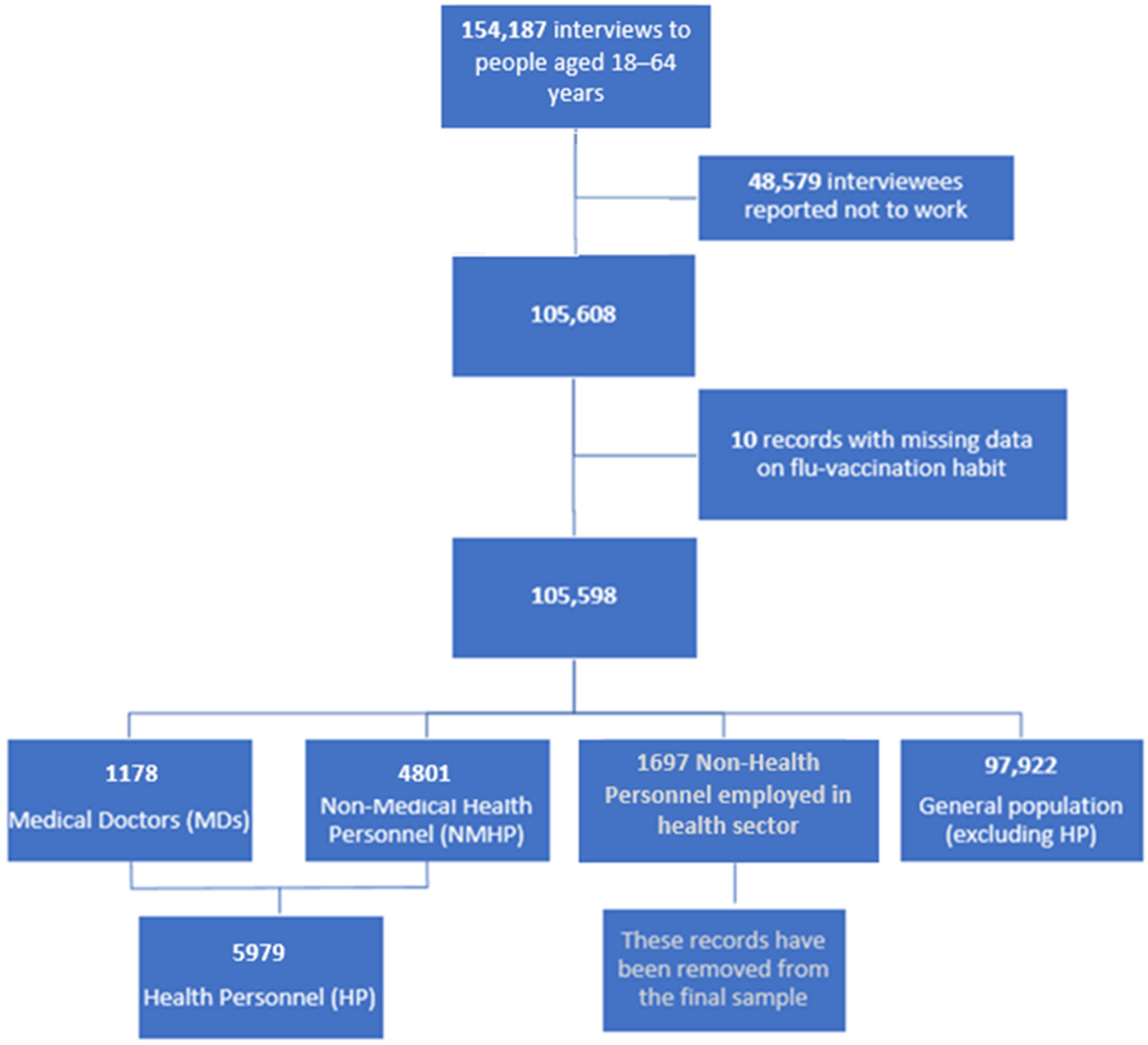
2. Materials and Methods
2.1. Study Design and Data Source
Sampling Procedure
2.2. Outcome and Covariate Variables
2.3. Statistical Analysis
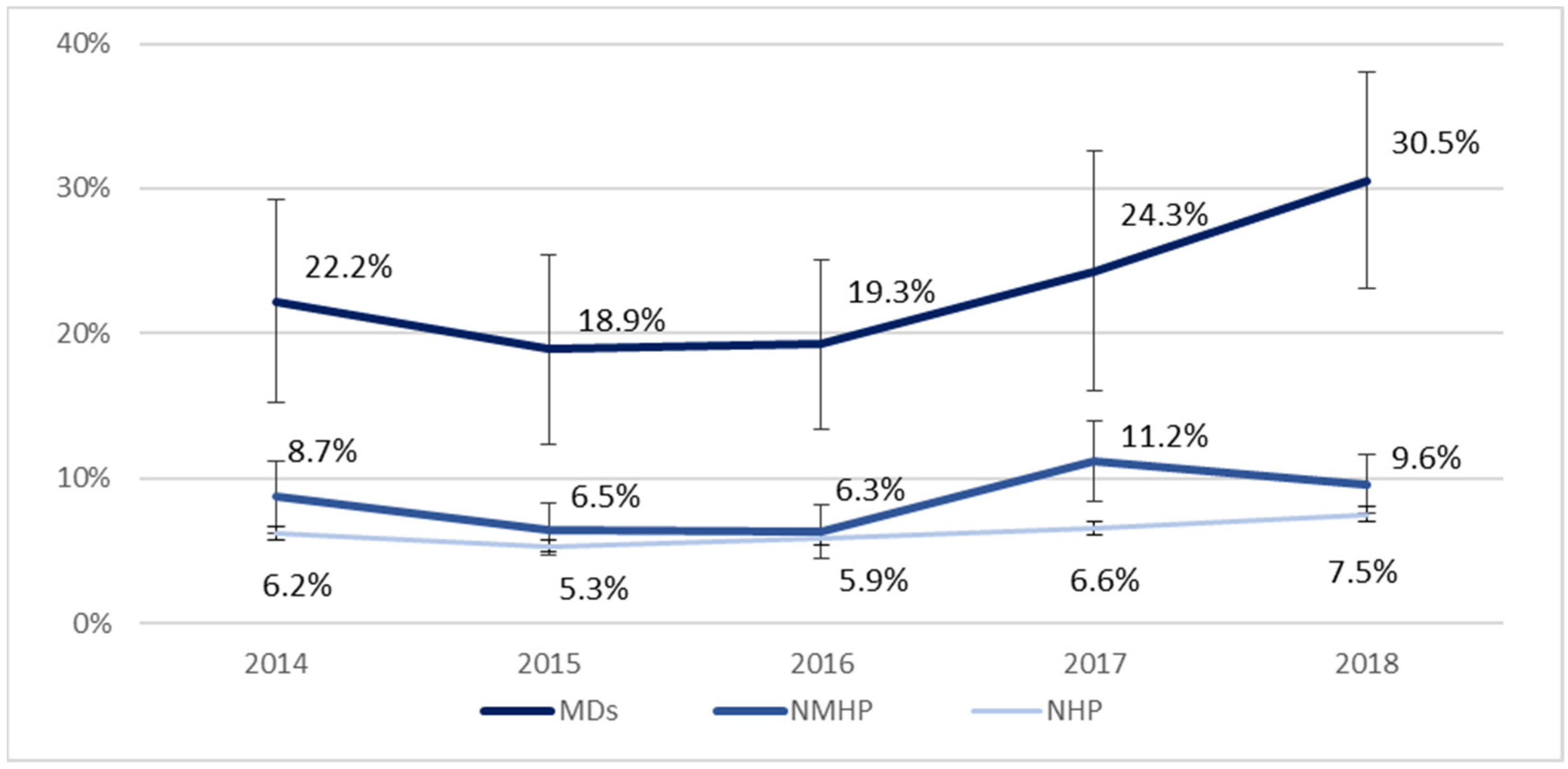
3. Results
3.1. Socio-Demographic Characteristics and Health Conditions
- Among NMHP, females were more represented (73.9%) than in the other two groups [MDs (47.1%) and NHP (42.7%)].
- Almost half of the MDs were between 50–64 years and had the highest education level compared to the other groups (89.9% of NMHP vs. 71.5% of NHP had a university or high school diploma), holding at least a university degree. They also reported fewer economic difficulties.
- Most respondents resided in municipalities with an intermediate urbanization degree. MDs lived more frequently in municipalities with high population density (48.9%) than NMHP (35.1%) or NHP (33.7%).
- MDs were less likely to smoke (16.4%) compared with other categories (25.4% of NMHP and 28.7% of NHP).
- The general population (9.4%) was more likely to have obesity than NMHP (7.9%) or MDs (6.4%).
3.2. Adherence to the Flu Vaccination Campaign by Socio-Demographic Characteristics and Health Conditions
4. Discussion
4.1. Critical Reading of the Results
4.1.1. The Literature Appraisal on Influenza Vaccination Uptake and Its Main Determinants
4.1.2. Interventions and Application of Proven Effective Policies
4.1.3. Impact of Pandemics
4.2. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Influenza (Seasonal). Available online: https://www.who.int/news-room/fact-sheets/detail/influenza-(seasonal) (accessed on 31 March 2023).
- Siriwardena, A.N.; Gwini, S.M.; Coupland, C.A. Influenza vaccination, pneumococcal vaccination and risk of acute myocardial infarction: Matched case-control study. CMAJ 2010, 182, 1617–1623. [Google Scholar] [CrossRef]
- Amodio, E.; Restivo, V.; Firenze, A.; Mammina, C.; Tramuto, F.; Vitale, F. Can influenza vaccination coverage among healthcare workers influence the risk of nosocomial influenza-like illness in hospitalized patients? J. Hosp. Infect. 2014, 86, 182–187. [Google Scholar] [CrossRef] [PubMed]
- Barchitta, M.; Basile, G.; Lopalco, P.L.; Agodi, A. Vaccine-preventable diseases and vaccination among Italian healthcare workers: A review of current literature. Future Microbiol. 2019, 14, 15–19. [Google Scholar] [CrossRef] [PubMed]
- Maltezou, H.C.; Theodoridou, K.; Ledda, C.; Rapisarda, V.; Theodoridou, M. Vaccination of healthcare workers: Is mandatory vaccination needed? Expert Rev. Vaccines 2019, 18, 5–13. [Google Scholar] [CrossRef] [PubMed]
- Leone Roberti Maggiore, U.; Scala, C.; Toletone, A.; Debarbieri, N.; Perria, M.; D’Amico, B.; Montecucco, A.; Martini, M.; Dini, G.; Durando, P. Susceptibility to vaccine-preventable diseases and vaccination adherence among healthcare workers in Italy: A cross-sectional survey at a regional acute-care university hospital and a systematic review. Hum. Vaccines Immunother. 2017, 13, 470–476. [Google Scholar] [CrossRef]
- Squeri, R.; Di Pietro, A.; La Fauci, V.; Genovese, C. Healthcare workers’ vaccination at European and Italian level: A narrative review. Acta Biomed. 2019, 13, 45–53. [Google Scholar] [CrossRef]
- Dini, G.; Toletone, A.; Sticchi, L.; Orsi, A.; Bragazzi, N.L.; Durando, P. Influenza vaccination in healthcare workers: A comprehensive critical appraisal of the literature. Hum. Vaccines Immunother. 2018, 14, 772–789. [Google Scholar] [CrossRef]
- Ministero Della Salute. National Immunization Prevention Plans (PNPV) 2017–2019. Available online: https://www.salute.gov.it/portale/documentazione/p6_2_2_1.jsp?id=2571 (accessed on 31 March 2023).
- Prato, R.; Tafuri, S.; Fortunato, F.; Martinelli, D. Vaccination in healthcare workers: An Italian perspective. Expert Rev. Vaccines 2010, 9, 277–283. [Google Scholar] [CrossRef]
- Di Pietro, A.; Visalli, G.; Antonuccio, G.M.; Facciolà, A. Today’s vaccination policies in Italy: The National Plan for Vaccine Prevention 2017–2019 and the Law 119/2017 on the mandatory vaccinations. Ann. Ig. 2019, 31 (Suppl. S1), 54–64. [Google Scholar] [CrossRef]
- Sassano, M.; Barbara, A.; Grossi, A.; Poscia, A.; Cimini, D.; Spadea, A.; Zaffina, S.; Villari, P.; Ricciardi, W.; Laurenti, P.; et al. La vaccinazione negli operatori sanitari in Italia: Una revisione narrativa di letteratura [Vaccination among healthcare workers in Italy: A narrative review]. Ig. Sanita Pubblica 2019, 75, 158–173. (In Italian) [Google Scholar]
- Decree of the President of the Council of Ministers of 3 March 2017. In Identification of Surveillance Systems and Registers of Mortality, Cancer and Other Diseases; (17A03142) (OJ General Series No.109 of 12-05-2017); Decree of the President of the Council of Ministers: Rome, Italy, 2017.
- Ministero Della Salute. National Prevention Plan (PNP) 2020–2025. Available online: https://www.salute.gov.it/portale/prevenzione/dettaglioContenutiPrevenzione.jsp?id=5772&area=prevenzione&menu=vuoto#:~:text=Adottato%20il%206%20agosto%202020%20con%20Intesa%20in,vita%2C%20nei%20luoghi%20in%20cui%20vive%20e%20lavora (accessed on 31 March 2023).
- Baldissera, S.; Campostrini, S.; Binkin, N.; Minardi, V.; Minelli, G.; Ferrante, G.; Salmaso, S. Features and initial assessment of the Italian behavioral risk factor surveillance system (PASSI), 2007–2008. Prev. Chronic Dis. 2011, 8, A24. [Google Scholar] [PubMed]
- Baldissera, S.; Ferrante, G.; Quarchioni, E.; Minardi, V.; Possenti, V.; Carrozzi, G.; Masocco, M.; Salmaso, S. Field substitution of nonresponders can maintain sample size and structure without altering survey estimates-the experience of the Italian behavioral risk factors surveillance system (PASSI). Ann. Epidemiol. 2014, 24, 241–245. [Google Scholar] [CrossRef] [PubMed]
- Principali Statistiche Geografiche Sui Comuni. Available online: https://www.istat.it/it/archivio/156224 (accessed on 31 March 2023).
- de Figueiredo, A.; Eagan, R.L.; Hendrickx, G.; Karafillakis, E.; van Damme, P.; Larson, H.J. State of Vaccine Confidence in the European Union, 2022; Publications Office of the European Union: Luxembourg, 2022; pp. 31–32. [Google Scholar]
- Guillari, A.; Polito, F.; Pucciarelli, G.; Serra, N.; Gargiulo, G.; Esposito, M.R.; Botti, S.; Rea, T.; Simeone, S. Influenza vaccination and healthcare workers: Barriers and predisposing factors. Acta Biomed. 2021, 92 (Suppl. S2), e2021004. [Google Scholar] [CrossRef]
- Bianchi, F.P.; Tafuri, S.; Spinelli, G.; Carlucci, M.; Migliore, G.; Calabrese, G.; Daleno, A.; Melpignano, L.; Vimercati, L.; Stefanizzi, P. Two years of on-site influenza vaccination strategy in an Italian university hospital: Main results and lessons learned. Hum. Vaccines Immunother. 2022, 18, 1993039. [Google Scholar] [CrossRef]
- Vimercati, L.; Bianchi, F.P.; Mansi, F.; Ranieri, B.; Stefanizzi, P.; De Nitto, S.; Tafuri, S. Influenza vaccination in health-care workers: An evaluation of an on-site vaccination strategy to increase vaccination uptake in health professionals of a South Italy Hospital. Hum. Vaccines Immunother. 2019, 15, 2927–2932. [Google Scholar] [CrossRef] [PubMed]
- Tafuri, S.S.; Martinelli, D.D.; Caputi, G.G.; Arbore, A.A.; Germinario, C.C.; Prato, R.R. Italian healthcare workers’ views on mandatory vaccination. BMC Health Serv. Res. 2009, 9, 100. [Google Scholar] [CrossRef] [PubMed]
- Lytras, T.; Kopsachilis, F.; Mouratidou, E.; Papamichail, D.; Bonovas, S. Interventions to increase seasonal influenza vaccine coverage in healthcare workers: A systematic review and meta-regression analysis. Hum. Vaccines Immunother. 2016, 12, 671–681. [Google Scholar] [CrossRef]
- Costantino, C.; Restivo, V.; Gaglio, V.; Lanza, G.L.M.; Marotta, C.; Maida, C.M.; Mazzucco, W.; Casuccio, A.; Torregrossa, M.V.; Vitale, F. Effectiveness of an educational intervention on seasonal influenza vaccination campaign adherence among healthcare workers of the Palermo University Hospital, Italy. Ann. Ig. 2019, 31, 35–44. [Google Scholar] [CrossRef]
- Corsaro, A.; Poscia, A.; de Waure, C.; De Meo, C.; Berloco, F.; Ricciardi, W.; Damiani, G.; Laurenti, P.; Group, C. Fostering Flu Vaccination in Healthcare Workers: Forum Theatre in a University Hospital. Med. Sci. Monit. 2017, 24, 4574–4578. [Google Scholar] [CrossRef]
- Ogliastro, M.; Borghesi, R.; Costa, E.; Fiorano, A.; Massaro, E.; Sticchi, L.; Domnich, A.; Tisa, V.; Durando, P.; Icardi, G.; et al. Monitoring influenza vaccination coverage among healthcare workers during the COVID-19 pandemic: A three-year survey in a large university hospital in North-Western Italy. J. Prev. Med. Hyg. 2022, 63, E405–E414. [Google Scholar] [CrossRef]
- State of Vaccine Confidence in the European Union, 2022. Country Factsheets. Italy. Available online: https://health.ec.europa.eu/publications/state-vaccine-confidence-eu-2022_en#factsheets-by-country (accessed on 31 March 2023).
- EpiCentro. PASSI d’Argento. Seasonal Influenza Vaccination. Available online: https://www.epicentro.iss.it/passi-argento/dati/VaccinazioneAntinfluenzale (accessed on 31 March 2023).
- PASSI and PASSI d’Argento National Working Group. PASSI and PASSI d’Argento and COVID-19 Pandemic. First National Report on Results from the COVID Module, 1st ed.; Istituto Superiore di Sanità: Rome, Italy, 2020; Available online: https://www.epicentro.iss.it/passi-argento/pdf2020/PASSI-PdA-COVID19-first-national-report-december-2020.pdf (accessed on 23 February 2023).
- Nelson, D.E.; Holtzman, D.; Bolen, J.; Stanwyck, C.A.; Mack, K.A. Reliability and validity of measures from the Behavioral Risk Factor Surveillance System (BRFSS). Soz. Praventivmed. 2001, 46, S3-42. [Google Scholar] [PubMed]
- Belli, R.F.; Winkielman, P.; Read, J.D.; Schwarz, N.; Lynn, S.J. Recalling more childhood events leads to judgments of poorer memory: Implications for the recovered/false memory debate. Psychon. Bull. Rev. 1998, 5, 318–323. [Google Scholar] [CrossRef]
- Minardi, V.; D’Argenio, P.; Gallo, R.; Possenti, V.; Contoli, B.; Carrozzi, G.; Cattaruzza, M.S.; Masocco, M.; Gorini, G. Smoking prevalence among healthcare workers in Italy, PASSI surveillance system data, 2014–2018. Ann. Dell’Istituto Super. Sanità 2021, 57, 151–160. [Google Scholar] [CrossRef]
- Albano, L.; Matuozzo, A.; Marinelli, P.; Di Giuseppe, G. Knowledge, attitudes and behaviour of hospital health-care workers regarding influenza A/H1N1: A cross sectional survey. BMC Infect. Dis. 2014, 14, 208. [Google Scholar] [CrossRef]
- Alicino, C.; Iudici, R.; Barberis, I.; Paganino, C.; Cacciani, R.; Zacconi, M.; Battistini, A.; Bellina, D.; Di Bella, A.M.; Talamini, A.; et al. Influenza vaccination among healthcare workers in Italy. Hum. Vaccines Immunother. 2014, 11, 95–100. [Google Scholar] [CrossRef]
- Amodio, E.; Tramuto, F.; Maringhini, G.; Asciutto, R.; Firenze, A.; Vitale, F.; Costantino, C.; Calamusa, G. Are medical residents a “core group” for future improvement of influenza vaccination coverage in health-care workers? A study among medical residents at the University Hospital of Palermo (Sicily). Vaccine 2011, 29, 8113–8117. [Google Scholar] [CrossRef]
- Amodio, E.; Anastasi, G.; Marsala, M.G.L.; Torregrossa, M.V.; Romano, N.; Firenze, A. Vaccination against the 2009 pandemic influenza A (H1N1) among healthcare workers in the major teaching hospital of Sicily (Italy). Vaccine 2011, 29, 1408–1412. [Google Scholar] [CrossRef]
- Amodio, E.; Di Pasquale, M.; Anastasi, G.; Gelsomino, V.; Morici, M.; Romano, N.; Torregrossa, M.V.; Cannova, L.; Calamusa, G.; Firenze, A. Influenza vaccination among healthcare workers and absenteeism from work due to influenza-like illness in a teaching hospital in Palermo. Ital. J. Public Health 2010, 7. [Google Scholar] [CrossRef]
- Arghittu, A.; Dettori, M.; Azara, A.; Gentili, D.; Serra, A.; Contu, B.; Castiglia, P. Flu Vaccination Attitudes, Behaviours, and Knowledge among Health Workers. Int. J. Environ. Res. Public Health 2020, 17, 3185. [Google Scholar] [CrossRef]
- Ballada, D.; Biasio, L.R.; Cascio, G.; D’Alessandro, D.; Donatelli, I.; Fara, G.M.; Pozzi, T.; Profeta, M.L.; Squarcione, S.; Riccò, D.; et al. Attitudes and behavior of health care personnel regarding influenza vaccination. Eur. J. Epidemiol. 1994, 10, 63–68. [Google Scholar] [CrossRef]
- Barbara, A.; La Milia, D.I.; Di Pumpo, M.; Tognetto, A.; Tamburrano, A.; Vallone, D.; Viora, C.; Cavalieri, S.; Cambieri, A.; Moscato, U.; et al. Strategies to Increase Flu Vaccination Coverage among Healthcare Workers: A 4 Years Study in a Large Italian Teaching Hospital. Vaccines 2020, 8, 85. [Google Scholar] [CrossRef] [PubMed]
- Barbadoro, P.; Brighenti, A.; Acquaviva, G.; Catalini, A.; Diotallevi, F.; Masiero, A.L.; Montagna, V.; D’errico, M.M. Gender, Socioeconomic, and Health Characteristics Associated with Influenza Vaccination Coverage (VC) among Italian Healthcare Workers: Secondary Analysis of a National Cross-Sectional Survey. Healthcare 2020, 8, 298. [Google Scholar] [CrossRef] [PubMed]
- Bonaccorsi, G.; Lorini, C.; Santomauro, F.; Guarducci, S.; Pellegrino, E.; Puggelli, F.; Balli, M.; Bonanni, P. Predictive factors associated with the acceptance of pandemic and seasonal influenza vaccination in health care workers and students in Tuscany, Central Italy. Hum. Vaccines Immunother. 2013, 9, 2603–2612. [Google Scholar] [CrossRef] [PubMed]
- Bonaccorsi, G.; Santomauro, F.; Porchia, B.R.; Niccolai, G.; Pellegrino, E.; Bonanni, P.; Lorini, C. Beliefs and Opinions of Health Care Workers and Students Regarding Influenza and Influenza Vaccination in Tuscany, Central Italy. Vaccines 2015, 3, 137–147. [Google Scholar] [CrossRef] [PubMed]
- Brunelli, L.; Antinolfi, F.; Malacarne, F.; Cocconi, R.; Brusaferro, S. A Wide Range of Strategies to Cope with Healthcare Workers’ Vaccine Hesitancy in A North-Eastern Italian Region: Are They Enough? Healthcare 2020, 9, 4. [Google Scholar] [CrossRef]
- Campagna, M.; Argiolas, F.; Soggiu, B.; Mereu, N.M.; Lai, A.; Galletta, M.; Coppola, R.C. Current preventive policies and practices against Vaccine-Preventable Diseases and tuberculosis targeted for workers from hospitals of the Sardinia Region, Italy. J. Prev. Med. Hyg. 2016, 57, E69–E74. [Google Scholar]
- Castella, A.; Argentero, P.A.; Lanszweert, A. Factors influencing uptake of influenza vaccination in healthcare workers. Findings from a study in a general hospital. Ann. Ig. Med. Prev. Comunita 2009, 21, 35–40. [Google Scholar]
- Congedo, E.C.; Paladino, M.E.; Riva, M.A.; Belingheri, M. Adherence, Perception of, and Attitude toward Influenza and Flu Vaccination: A Cross-Sectional Study among a Population of Future Healthcare Workers. Int. J. Environ. Res. Public Health 2021, 18, 13086. [Google Scholar] [CrossRef]
- Costantino, C.; Mazzucco, W.; Azzolini, E.; Baldini, C.; Bergomi, M.; Biafiore, A.D.; Bianco, M.; Borsari, L.; Cacciari, P.; Cadeddu, C.; et al. Influenza vaccination coverage among medical residents. Hum. Vaccines Immunother. 2014, 10, 1204–1210. [Google Scholar] [CrossRef]
- Costantino, C.; Amodio, E.; Vitale, F.; Maida, C.; Meringhini, G.; Asciutto, R.; Tramuto, F.; Calamusa, G. Attitudes, behaviours and perceptions of Italian General Practitioner trainees towards influenza vac-cination in Western Sicily (Italy). Ital. J. Public Health 2012, 9. [Google Scholar] [CrossRef]
- Franchino, G.; Costantino, C.; Asta, M.D.; Furnari, R. Knowledge, attitudes and behaviors regarding influenza vaccination among hygiene and preventive medicine residents in Calabria and sicily. EuroMediterranean Biomed. J. 2012, 7, 77–83. [Google Scholar]
- Cozza, V.; Alfonsi, V.; Rota, M.C.; Paolini, V.; Degli Atti, M.L.C. Promotion of influenza vaccination among health care workers: Findings from a tertiary care children’s hospital in Italy. BMC Public Health 2015, 15, 697. [Google Scholar] [CrossRef] [PubMed]
- Desiante, F.; Caputi, G.; Cipriani, R.; Nanula, C.; Aprile, I.; Pesare, A.; Conversano, M. Assessment of coverage and analysis of the determinants of adherence to influenza vaccination in the general practitioners of Taranto. Ann. Ig. 2017, 29, 256–263. [Google Scholar] [CrossRef] [PubMed]
- Durando, P.; Alicino, C.; Dini, G.; Barberis, I.; Bagnasco, A.; Iudici, R.; Zanini, M.; Martini, M.; Toletone, A.; Paganino, C.; et al. Determinants of adherence to seasonal influenza vaccination among healthcare workers from an Italian region: Results from a cross-sectional study. BMJ Open 2016, 6, e010779. [Google Scholar] [CrossRef]
- Festini, F.; Biermann, K.P.; Neri, S.; Reali, M.F.; de Martino, M. Influenza vaccination of nurses in an Italian pediatric hospi-tal: Effects on absenteeism and on costs, factors associated with vaccine uptake and analysis of personal motivations. A pro-spective cohort study. Assist. Inferm. E Ric. 2007, 26, 5–13. [Google Scholar]
- Fortunato, F.; Tafuri, S.; Cozza, V.; Martinelli, D.; Prato, R. Low vaccination coverage among italian healthcare workers in 2013. Hum. Vaccines Immunother. 2014, 11, 133–139. [Google Scholar] [CrossRef] [PubMed]
- Gallone, M.F.; Cappelli, M.G.; Fortunato, F.; Martinelli, D.; Quarto, M.; Prato, R.; Tafuri, S. Medical students’ attitude toward influenza vaccination: Results of a survey in the University of Bari (Italy). Hum. Vaccines Immunother. 2017, 13, 1937–1941. [Google Scholar] [CrossRef] [PubMed]
- Gianino, M.M.; Kakaa, O.; Politano, G.; Scarmozzino, A.; Benso, A.; Zotti, C.M. Severe and moderate seasonal influenza epidemics among Italian healthcare workers: A comparison of the excess of absenteeism. Influ. Other Respir. Viruses 2020, 15, 81–90. [Google Scholar] [CrossRef]
- Karnaki, P.; Baka, A.; Petralias, A.; Veloudaki, A.; Zota, D.; Linos, A.; HProImmune Partnership. Immunization related behaviour among healthcare workers in Europe: Results of the HProImmune survey. Cent. Eur. J. Public Health 2019, 27, 204–211. [Google Scholar] [CrossRef]
- Keske, Ş.; Mutters, N.T.; Tsioutis, C.; Ergönül, Ö.; EUCIC Influenza Vaccination Survey Team. Influenza vaccination among infection control teams: A EUCIC survey prior to COVID-19 pandemic. Vaccine 2020, 38, 8357–8361. [Google Scholar] [CrossRef]
- Lorini, C.; Collini, F.; Gasparini, F.; Paolini, D.; Grazzini, M.; Ierardi, F.; Galletti, G.; Zanobini, P.; Gemmi, F.; Bonaccorsi, G. Health Literacy, Vaccine Confidence and Influenza Vaccination Uptake among Nursing Home Staff: A Cross-Sectional Study Conducted in Tuscany. Vaccines 2020, 8, 154. [Google Scholar] [CrossRef] [PubMed]
- Lorini, C.; Ierardi, F.; Gatteschi, C.; Galletti, G.; Collini, F.; Peracca, L.; Zanobini, P.; Gemmi, F.; Bonaccorsi, G. Promoting Influenza Vaccination among Staff of Nursing Homes According to Behavioral Insights: Analyzing the Choice Architecture during a Nudge-Based Intervention. Vaccines 2020, 8, 600. [Google Scholar] [CrossRef] [PubMed]
- Maffeo, M.; Luconi, E.; Castrofino, A.; Campagnoli, E.M.; Cinnirella, A.; Fornaro, F.; Gallana, C.; Perrone, P.M.; Shishmintseva, V.; Pariani, E.; et al. 2019 Influenza Vaccination Campaign in an Italian Research and Teaching Hospital: Analysis of the Reasons for Its Failure. Int. J. Environ. Res. Public Health 2020, 17, 3881. [Google Scholar] [CrossRef]
- Mellucci, C.; Tamburrano, A.; Cassano, F.; Galletti, C.; Sguera, A.; Damiani, G.; Laurenti, P. Vaccine Hesitancy among Master’s Degree Students in Nursing and Midwifery: Attitude and Knowledge about Influenza Vaccination. Int. J. Environ. Res. Public Health 2020, 17, 7191. [Google Scholar] [CrossRef] [PubMed]
- Napolitano, F.; Bianco, A.; D’Alessandro, A.; Papadopoli, R.; Angelillo, I.F. Healthcare workers’ knowledge, beliefs, and coverage regarding vaccinations in critical care units in Italy. Vaccine 2019, 37, 6900–6906. [Google Scholar] [CrossRef] [PubMed]
- Paoli, S.; Lorini, C.; Puggelli, F.; Sala, A.; Grazzini, M.; Paolini, D.; Bonanni, P.; Bonaccorsi, G. Assessing Vaccine Hesitancy among Healthcare Workers: A Cross-Sectional Study at an Italian Paediatric Hospital and the Development of a Healthcare Worker’s Vaccination Compliance Index. Vaccines 2019, 7, 201. [Google Scholar] [CrossRef]
- Perrone, P.M.; Biganzoli, G.; Lecce, M.; Campagnoli, E.M.; Castrofino, A.; Cinnirella, A.; Fornaro, F.; Gallana, C.; Grosso, F.M.; Maffeo, M.; et al. Influenza Vaccination Campaign during the COVID-19 Pandemic: The Experience of a Research and Teaching Hospital in Milan. Int. J. Environ. Res. Public Health 2021, 18, 5874. [Google Scholar] [CrossRef]
- Rabensteiner, A.; Buja, A.; Regele, D.; Fischer, M.; Baldo, V. Healthcare worker’s attitude to seasonal influenza vaccination in the South Tyrolean province of Italy: Barriers and facilitators. Vaccine 2018, 36, 535–544. [Google Scholar] [CrossRef]
- Riccò, M.; Cattani, S.; Casagranda, F.; Gualerzi, G.; Signorelli, C. Knowledge, attitudes, beliefs and practices of Occupational Physicians towards seasonal influenza vaccination: A cross-sectional study from North-Eastern Italy. J. Prev. Med. Hyg. 2017, 58, E141–E154. [Google Scholar]
- Santangelo, O.E.; Provenzano, S.; Firenze, A. Factors influencing flu vaccination in nursing students at Palermo University. J. Prev. Med. Hyg. 2021, 61, E563–E567. [Google Scholar] [CrossRef]
- Squeri, R.; La Fauci, V.; Picerno, I.A.M.; Trimarchi, G.; Cannavò, G.; Egitto, G.; Cosenza, B.; Merlina, V.; Genovese, C. Evalu-ation of Vaccination Coverages in the Health Care Workers of a University Hospital in Southern Italy. Ann. Ig. 2019, 31, 13–24. [Google Scholar] [CrossRef] [PubMed]
- Tognetto, A.; Zorzoli, E.; Franco, E.; Gervasi, G.; Paglione, L.; Di Ninno, F.; De Soccio, P.; Barbara, A.; Orsi, G.B.; De Vito, C.; et al. Seasonal influenza vaccination among health-care workers: The impact of different tailored programs in four University hospitals in Rome. Hum. Vaccines Immunother. 2019, 16, 81–85. [Google Scholar] [CrossRef] [PubMed]
- Tomboloni, C.; Tersigni, C.; De Martino, M.; Dini, D.; González-López, J.R.; Festini, F.; Neri, S.; Ciofi, D. Knowledge, attitude and disinformation regarding vaccination and immunization practices among healthcare workers of a third-level paediatric hospital. Ital. J. Pediatr. 2019, 45, 104. [Google Scholar] [CrossRef]
| Healthcare Personnel (HP) | General Population (Excluding HP) (n = 97,922) | |||||
|---|---|---|---|---|---|---|
| Medical Doctors (MDs) (n = 1178) | Non-Medical Health Personnel (NMHP) (n = 4801) | |||||
| % | (IC 95%) | % | IC 95% | % | IC 95% | |
| Total | 1.1 | – | 4.6 | – | 94.3 | – |
| Gender | ||||||
| Men | 52.9 | (50.0–55.7) | 26.1 | (24.9–27.4) | 57.3 | (57.0–57.6) |
| Women | 47.1 | (44.3–50.0) | 73.9 | (72.6–75.1) | 42.7 | (42.4–43.0) |
| Age group | ||||||
| 18–34 | 17.7 | (15.7–20.0) | 21.5 | (20.4–22.7) | 24.9 | (24.6–25.1) |
| 35–49 | 31.3 | (28.7–34.0) | 45.2 | (43.8–46.6) | 44.4 | (44.1–44.7) |
| 50–64 | 50.9 | (48.1–53.8) | 33.3 | (32.0–34.7) | 30.7 | (30.4–31.0) |
| Economic difficulties | ||||||
| Some or many | 10.5 | (8.5–13.0) | 42.2 | (40.4–44.1) | 49.8 | (49.3–50.1) |
| None | 89.5 | (87.0–91.6) | 57.8 | (55.9–59.6) | 50.3 | (49.9–50.7) |
| Educational level | ||||||
| Low | – | (–) | 10.1 | (9.0–11.2) | 28.5 | (28.2–28.9) |
| High | 100.0 | (–) | 89.9 | (88.8–91.0) | 71.5 | (71.1–71.8) |
| Geographical area | ||||||
| North | 39.3 | (35.8–42.9) | 43.4 | (41.7–45.1) | 41.6 | (41.5–41.8) |
| Center | 22.4 | (19.9–25.1) | 21.7 | (20.4–23.0) | 23.9 | (23.7–24.0) |
| South and Islands | 38.3 | (34.5–42.3) | 34.9 | (33.1–36.8) | 34.5 | (34.4–34.6) |
| Urbanization Degree (population density) | ||||||
| High | 48.9 | (45.2–52.7) | 35.1 | (33.3–37.0) | 33.7 | (33.4–34.0) |
| Intermediate | 41.8 | (38.1–45.6) | 47.6 | (45.8–49.3) | 47.6 | (47.2–47.9) |
| Low | 9.3 | (7.7–11.0) | 17.3 | (16.2–18.5) | 18.7 | (18.5–19.0) |
| Marital status | ||||||
| Married | 62.3 | (58.6–65.8) | 57.7 | (55.9–59.5) | 58.2 | (57.8–58.6) |
| Not married | 37.7 | (34.2–41.4) | 42.3 | (40.5–44.1) | 41.8 | (41.4–42.2) |
| Nationality | ||||||
| Italian | 99.2 | (98.3–99.6) | 97.3 | (96.8–97.8) | 94.8 | (94.6–95.0) |
| Others | 0.8 | (0.4–1.7) | 2.7 | (2.2–3.2) | 5.2 | (5.0–5.4) |
| Chronic diseases * | ||||||
| None | 86.9 | (84.4–89.0) | 84.7 | (83.3–85.8) | 86.1 | (85.8–86.4) |
| At least one | 13.1 | (11.0–15.6) | 15.4 | (14.2–16.7) | 13.9 | (13.6–14.2) |
| Obesity | ||||||
| Yes | 6.4 | (4.8–8.6) | 7.9 | (7.0–8.9) | 9.4 | (9.1–9.6) |
| No | 93.6 | (91.4–95.2) | 92.1 | (91.1–93.0) | 90.6 | (90.4–90.9) |
| Tobacco smoking | ||||||
| Yes | 16.4 | (13.5–19.8) | 25.4 | (23.8–27.0) | 28.7 | (28.3–29.1) |
| No | 83.6 | (80.2–86.5) | 74.6 | (73.0–76.2) | 71.3 | (70.9–71.7) |
| Self-perceived health status | ||||||
| Good or very good | 79.3 | (75.8–82.4) | 74.4 | (72.8–75.9) | 75.7 | (75.3–76.0) |
| Fair, bad, and very bad | 20.7 | (17.6–24.2) | 25.6 | (24.1–27.2) | 24.3 | (24.0–24.7) |
| Healthcare Personnel (HP) | ||||||
|---|---|---|---|---|---|---|
| Medical Doctors (MDs) (n = 1178) | Non-Medical Health Personnel (NMHP) (n = 4801) | General Population (Excluding HP) (NHP) (n = 97,922) | ||||
| % (IC 95%) | Crude OR (IC 95%) | % (IC 95%) | Crude OR (IC 95%) | % (IC 95%) | Crude OR (IC 95%) | |
| Total | 22.8 (19.8–26.1) | – | 8.5 (7.5–9.5) | – | 6.3 (6.1–6.5) | – |
| Gender | ||||||
| Men | 24.1 (20.0–28.8) | – | 10.2 (8.3–12.4) | – | 6.8 (6.5–7.0) | – |
| Women | 21.3 (17.1–26.1) | 0.852 (0.581–1.249) | 7.8 (6.7–9.0) | 0.742 * (0.566–0.974) | 5.6 (5.3–5.9) | 0.818 * (0.764–0.876) |
| Age group | ||||||
| 18–34 | 9.9 (6.2–15.3) | 4.4 (3.2–5.9) | 3.4 (3.1–3.8) | – | ||
| 35–49 | 20.3 (15.6–26.1) | 2.317 * (1.262–4.254) | 6.4 (5.3–7.8) | 1.507 * (1.09–2.209) | 4.9 (4.6–5.2) | 1.451 * (1.300–1.626) |
| 50–64 | 28.4 (23.8–33.4) | 3.596 * (2.019–6.404) | 13.9 (11.8–16.3) | 3.534 * (2.437–5.125) | 10.6 (10.1–11.0) | 3.336 * (2.991–3.720) |
| Economic difficulties | ||||||
| Some or many | 20.5 (13.2–30.6) | – | 8.5 (6.9–10.4) | – | 6.4 (6.1–6.7) | – |
| None | 23.0 (19.8–26.6) | 1.157 (0.664–2.015) | 8.4 (7.3–9.6) | 0.989 (0.755–1.295) | 6.2 (5.9–6.5) | 0.969 (0.905–1.038) |
| Educational level ** | ||||||
| Low | – | – | 7.7 (5.4–10.9) | 7.0 (6.6–7.4) | – | |
| High | 22.8 (19.8–26.1) | – | 8.5 (7.5–9.7) | 1.122 (0.750–1.679) | 6.0 (5.7–6.2) | 0.840 * (0.780–0.904) |
| Geographic area | ||||||
| North | 25.7 (21.2–30.8) | 7.9 (6.7–9.2) | 5.7 (5.5–6.0) | – | ||
| Center | 17.9 (13.6–23.1) | 0.629 * (0.417–0.948) | 7.8 (6.1–9.8) | 0.987 (0.731–1.333) | 6.3 (6.0–6.7) | 1.108 * (1.028–1.194) |
| South and Islands | 22.7 (17.3–29.2) | 0.848 (0.538–1.335) | 9.6 (7.7–12.0) | 1.248 (0.929–1.676) | 6.9 (6.5–7.4) | 1.227 * (1.131–1.331) |
| Urbanization Degree (population density) | ||||||
| High | 19.2 (15.3–23.9) | – | 8.8 (7.1–10.7) | – | 6.7 (6.4–7.1) | – |
| Intermediate | 26.2 (21.2–31.9) | 1.493 * (1.006–2.216) | 7.8 (6.6–9.2) | 0.883 (0.669–1.165) | 6.0 (5.8–6.3) | 0.891 * (0.824–0.964) |
| Low | 26.2 (19.3–34.5) | 1.494 (0.934–2.388) | 8.7 (6.9–11.0) | 0.994 (0.711–1.388) | 6.1 (5.7–6.5) | 0.901 * (0.821–0.988) |
| Marital status | ||||||
| Married | 25.0 (21.1–29.3) | – | 9.1 (7.8–10.6) | 6.9 (6.7–7.2) | – | |
| Not married | 19.1 (14.7–24.5) | 0.709 (0.493–1.020) | 7.6 (6.3–9.2) | 0.826 (0.635–1.073) | 5.4 (5.1–5.6) | 0.759 * (0.707–0.815) |
| Nationality | ||||||
| Italian | 22.8 (20.0–26.4) | – | 8.6 (7.6–9.7) | – | 6.3 (6.1–6.5) | – |
| Others | – | – | 4.9 (1.9–11.6) | 0.543 (0.209–1.411) | 5.5 (4.8–6.2) | 0.862 * (0.754–0.986) |
| Healthcare Personnel (HP) | ||||||
|---|---|---|---|---|---|---|
| Medical Doctors (MDs) (n = 1178) | Non-Medical Health Personnel (NMHP) (n = 4801) | General Population (Excluding HP) (NHP) (n = 97,922) | ||||
| % (IC 95%) | Crude OR (IC 95%) | % (IC 95%) | Crude OR (IC 95%) | % (IC 95%) | Crude OR (IC 95%) | |
| Total | 22.8 (19.8–26.1) | – | 8.5 (7.5–9.5) | – | 6.3 (6.1–6.5) | – |
| Chronic disease ** | ||||||
| None | 20.8 (17.6–24.3) | – | 7.5 (6.5–8.6) | 4.4 (4.3–4.6) | – | |
| At least one | 36.3 (27.9–45.7) | 2.180 * (1.407–3.377) | 13.9 (11.0–17.3) | 1.996 * (1.481–2.691) | 17.6 (16.8–18.5) | 4.601 * (4.275–4.953) |
| Obesity | ||||||
| Yes | 30.0 (15.9–44.1) | 1.493 (0.741–3.009) | 10.6 (7.0–14.2) | 1.312 (0.878–1.962) | 9.2 (8.4–10.0) | 1.586 * (1.428–1.762) |
| No | 22.3 (19.1–25.5) | – | 8.3 (7.2–9.3) | – | 6.0 (5.8–6.2) | – |
| Tobacco smoking | ||||||
| Yes | 20.0 (13.9–27.9) | 0.814 (0.505–1.311) | 8.0 (6.2–10.3) | 0.935 (0.682–1.281) | 5.2 (4.9–5.6) | 0.764 * (0.705–0.828) |
| No | 23.5 (20.2–27.2) | – | 8.6 (7.5–9.8) | – | 6.7 (6.5–7.0) | – |
| Self–perceived health status | ||||||
| Good or very good | 21.3 (18.2–24.7) | 0.672 (0.423–1.66) | 7.6 (6.6–8.9) | 0.691 * (0.524–0.910) | 4.8 (4.6–5.0) | 0.418 * (0.389–0.449) |
| Fair, bad, and very bad | 28.7 (20.9–37.9) | – | 10.7 (8.8–13.0) | – | 10.8 (10.3–11.4) | |
| Healthcare Personnel (HP) | ||||||
|---|---|---|---|---|---|---|
| Medical Doctors (MDs) (n = 1178) | Non-Medical Health Personnel (NMHP) (n = 4801) | General Population (excluding HP) (NHP) (n = 97,922) | ||||
| AdjOR | (IC 95%) | AdjOR | (IC 95%) | AdjOR | (IC 95%) | |
| Gender | ||||||
| Men | – | – | – | – | – | – |
| Women | 1.014 | (0.662–1.554) | 0.741 * | (0.557–0.986) | 0.808 * | (0.752–0.867) |
| Age group | ||||||
| 18–34 | – | – | – | – | – | – |
| 35–49 | 2.223 * | (1.195–4.138) | 1.518 * | (1.020–2.261) | 1.358 * | (1.210–1.524) |
| 50–64 | 3.135 * | (1.681–5.846) | 3.299 * | (2.216–4.912) | 2.473 * | (2.196–2.785) |
| Educational level ** | ||||||
| Low | – | – | ||||
| High | 1.069 | (0.988–1.158) | ||||
| Geographic area | ||||||
| North | – | – | – | – | – | – |
| Center | 0.644 * | (0.422–0.983) | 0.967 | (0.707–1.321) | 1.097 * | (1.014–1.187) |
| South and Islands | 0.792 | (0.492–1.276) | 1.197 | (0.885–1.620) | 1.229 * | (1.129–1.338) |
| Urbanization Degree (population density) | ||||||
| High | – | – | – | – | ||
| Intermediate | 1.415 | (0.954–2.097) | 0.907 * | (0.835–0.984) | ||
| Low | 1.428 | (0.882–2.313) | 0.899 * | (0.816–0.991) | ||
| Marital status | ||||||
| Married | – | – | – | – | – | – |
| Not married | 0.951 | (0.636–1.422) | 1.039 | (0.794–1.360) | 1.108 * | (1.026–1.196) |
| Nationality | ||||||
| Italian | – | – | ||||
| Others | 1.092 | (0.949–1.256) | ||||
| Chronic disease ** | ||||||
| None | – | – | – | – | – | – |
| At least one | 1.852 * | (1.169–2.934) | 1.729 * | (1.268–2.357) | 3.490 * | (3.225–3.775) |
| Obesity | ||||||
| Yes | 1.115 | (0.737–1.688) | 1.096 | (0.980–1.227) | ||
| No | – | – | – | – | ||
| Tobacco smoking | ||||||
| Yes | 0.768 * | (0.706–0.834) | ||||
| No | – | – | ||||
| Self–perceived health status | ||||||
| Good or very good | 0.859 | (0.529–1.394) | 0.982 | (0.726–1.330) | 0.685 * | (0.633–0.742) |
| Fair, bad, and very bad | – | – | – | – | – | – |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Minardi, V.; Gallo, R.; Possenti, V.; Contoli, B.; Di Fonzo, D.; D’Andrea, E.; Masocco, M. Influenza Vaccination Uptake and Prognostic Factors among Health Professionals in Italy: Results from the Nationwide Surveillance PASSI 2015–2018. Vaccines 2023, 11, 1223. https://doi.org/10.3390/vaccines11071223
Minardi V, Gallo R, Possenti V, Contoli B, Di Fonzo D, D’Andrea E, Masocco M. Influenza Vaccination Uptake and Prognostic Factors among Health Professionals in Italy: Results from the Nationwide Surveillance PASSI 2015–2018. Vaccines. 2023; 11(7):1223. https://doi.org/10.3390/vaccines11071223
Chicago/Turabian StyleMinardi, Valentina, Rosaria Gallo, Valentina Possenti, Benedetta Contoli, Davide Di Fonzo, Elvira D’Andrea, and Maria Masocco. 2023. "Influenza Vaccination Uptake and Prognostic Factors among Health Professionals in Italy: Results from the Nationwide Surveillance PASSI 2015–2018" Vaccines 11, no. 7: 1223. https://doi.org/10.3390/vaccines11071223
APA StyleMinardi, V., Gallo, R., Possenti, V., Contoli, B., Di Fonzo, D., D’Andrea, E., & Masocco, M. (2023). Influenza Vaccination Uptake and Prognostic Factors among Health Professionals in Italy: Results from the Nationwide Surveillance PASSI 2015–2018. Vaccines, 11(7), 1223. https://doi.org/10.3390/vaccines11071223





