Exploring Knowledge and Perceptions of Polio Disease and Its Immunization in Polio High-Risk Areas of Pakistan
Abstract
1. Introduction
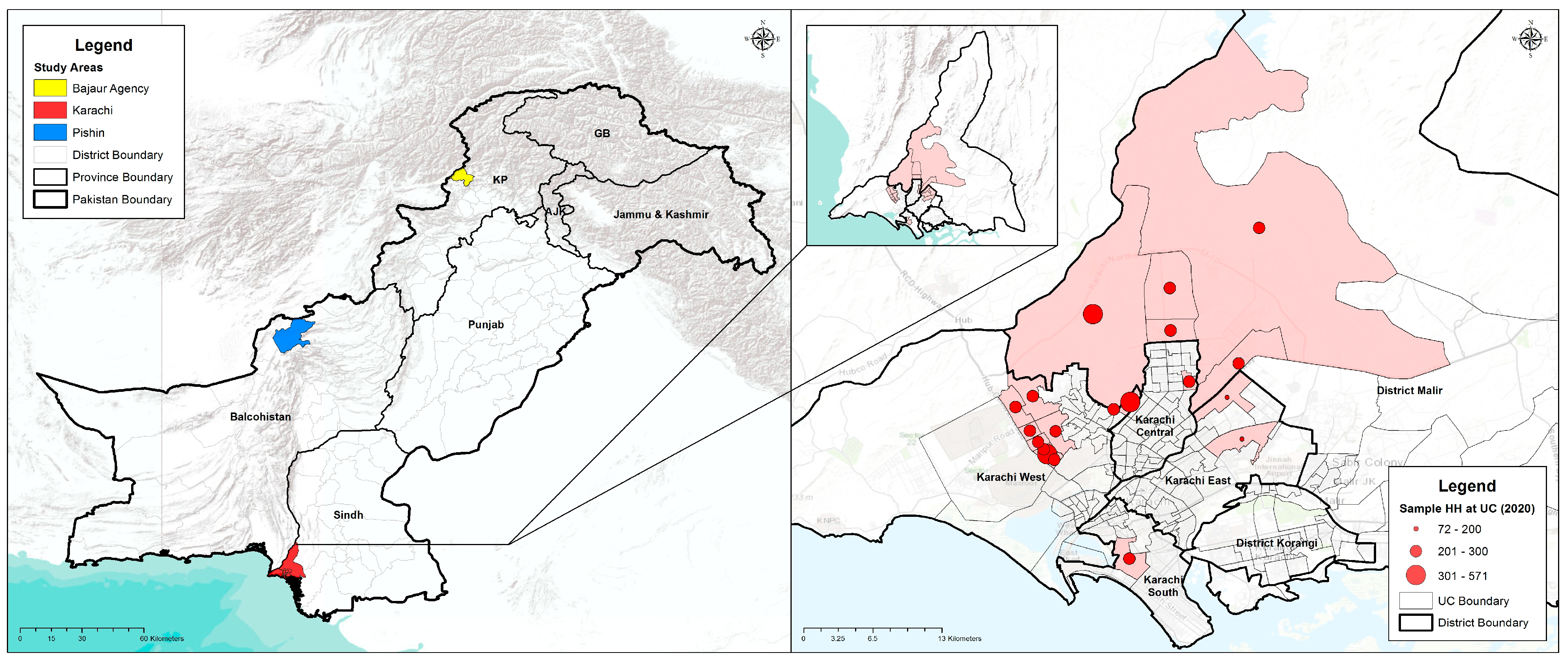
2. Methodology
3. Data Analysis
4. Results
4.1. Quantitative Component
4.2. Comparison with a Previous Similar Survey Conducted in 2012
4.3. Qualitative Component
“Grandmothers guide our daughters-in-laws about child-rearing and caring, counsel what to feed if the child has fever or pain, what type is food is good in hot and cold weather to keep the child healthy.”
“Health of our children is not good, as most children don’t get a vaccination, they don’t get proper nutrition, and live in unhygienic conditions. Nowadays, the diet of mothers is also not good that’s why children are weak.”
“Polio workers give knowledge and guide us about health and vaccine, we are thankful to them that they visit our households repeatedly for the sake of community health.”
“People believe that these vaccines are for family planning, cause infertility to decrease their generation.”
“Only legs are not affected by polio disease but it may cause many other problems like weakness, low immunity, heart disease, indigestion, weakens of an arm or leg and it can also lead to death.”
“My niece got affected by polio disease because her mother never gave her polio drops. When she took her to the doctor, he told them that she got infected by poliovirus. Now, she is 18 years old but disabled. After this incident, my sister gave polio drops to every child to prevent them from polio virus.”
“Water testing from drainage was done to identify the polio virus in our area and it has been proven that this is one of the main reasons for spreading this disease. Unfortunately, no vaccine and medicine can save children, until and unless the environment can be cleaned.”
“I have seen that there was one girl who was 18 months old, and she got polio attack and she became disabled. So, her family took her to the Syed family (the direct descendants of the Prophet Muhammad), and within 5 days she became normal. Another child was in the last stage, and they took the child to the Maulvi and then the child became normal.”
“Mostly people refuse to give polio drops to their male child. When asked about the reason for refusal during the polio campaign, and said we have an only male child in our family and these drops cause impotence.”
5. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Global Polio Eradication Initiative. Available online: https://polioeradication.org/who-we-are/our-mission/ (accessed on 20 February 2023).
- Pakistan Polio Eradication Programme. Available online: https://www.endpolio.com.pk/polioin-pakistan (accessed on 20 February 2022).
- World Health Organization. Available online: https://www.emro.who.int/pak/programmes/polio-eradication-initiative.html (accessed on 21 February 2022).
- Global Polio Eradication Initiative. Available online: https://polioeradication.org/where-we-work/ (accessed on 21 February 2022).
- Khowaja, A.R.; Zaman, U.; Feroze, A.; Rizvi, A.; Zaidi, A.K. Routine EPI coverage: Subdistrict inequalities and reasons for immunization failure in a rural setting in Pakistan. Asia Pac. J. Public Health 2015, 27, NP1050–NP1059. [Google Scholar] [CrossRef] [PubMed]
- Ministry of National Health Services. National EPI Policy and Strategic Guidlines Pakistan 2015. Available online: https://phkh.nhsrc.pk/sites/default/files/2019-06/National%20EPI%20Policy%20and%20Strategic%20Guidlines%20Revised%202015.pdf (accessed on 21 February 2022).
- World Health Organization. Global Emergency Action Plan 2012–2013. Available online: https://terrance.who.int/mediacentre/data/sage/SAGE_Docs_Ppt_Feb2012/2_session_polio/Feb2012_session2_Outline_Polio_EAP.pdf (accessed on 21 February 2022).
- Kew, O. Reaching the last one percent: Progress and challenges in global polio eradication. Curr. Opin. Virol. 2012, 2, 188–198. [Google Scholar] [CrossRef] [PubMed]
- Obregón, R.; Chitnis, K.; Morry, C.; Feek, W.; Bates, J.; Galway, M.; Ogden, E. Achieving polio eradication: A review of health communication evidence and lessons learned in India and Pakistan. Bull. World Health Organ. 2009, 87, 624–630. [Google Scholar] [CrossRef] [PubMed]
- Khan, T.; Qazi, J. Hurdles to the global antipolio campaign in Pakistan: An outline of the current status and future prospects to achieve a polio free world. J. Epidemiol. Community Health 2013, 67, 696–702. [Google Scholar] [CrossRef] [PubMed]
- Habib, M.A.; Soofi, S.B.; Ali, N.; Hussain, I.; Tabassum, F.; Suhag, Z.; Anwar, S.; Ahmed, I.; Bhutta, Z.A. Knowledge and perceptions of polio and polio immunization in polio high-risk areas of Pakistan. J. Public Health Policy 2017, 38, 16–36. [Google Scholar] [CrossRef] [PubMed]
- Shah, S.Z.; Saad, M.; Khattak, M.H.R.; Rizwan, M.; Haidari, A.; Idrees, F. Why We Could Not Eradicate Polio from Pakistan and How Can We? J. Ayub Med. Coll. Abbottabad 2016, 28, 423–425. [Google Scholar] [PubMed]
- Khan, T.M.; Chiau, L.M. Polio vaccination in Pakistan: By force or by volition? Lancet 2015, 386, 1733. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.U.; Ahmad, A.; Salman, S.; Ayub, M.; Aqeel, T.; Haq, N.-u.; Saleem, F.; Khan, M.U. Muslim scholars’ knowledge, attitudes and perceived barriers towards polio immunization in Pakistan. J. Relig. Health 2017, 56, 635–648. [Google Scholar] [CrossRef] [PubMed]
- Jin, Q.; Raza, S.H.; Yousaf, M.; Munawar, R.; Shah, A.A.; Hassan, S.; Shaikh, R.S.; Ogadimma, E.C. Ingraining Polio Vaccine Acceptance through Public Service Advertisements in the Digital Era: The Moderating Role of Misinformation, Disinformation, Fake News, and Religious Fatalism. Vaccines 2022, 10, 1733. [Google Scholar] [CrossRef] [PubMed]
- Lemeshow, S.; Stroh, G. Sampling Techniques for Evaluating Health Parameters in Developing Countries; National Academy Press: Washington, DC, USA, 1988. [Google Scholar]
- Nath, D.; Patowari, B. Estimation and comparison of immunization coverage under different sampling methods for health surveys. Int. J. Popul. Res. 2014, 2014, 850479. [Google Scholar] [CrossRef]
- Khan, M.U.; Ahmad, A.; Aqeel, T.; Salman, S.; Ibrahim, Q.; Idrees, J.; Khan, M.U. Knowledge, attitudes and perceptions towards polio immunization among residents of two highly affected regions of Pakistan. BMC Public Health 2015, 15, 1100. [Google Scholar] [CrossRef] [PubMed]
- Ogwumike, O.O.; Kaka, B.; Adeniyi, A.F. Children with paralytic poliomyelitis: A cross-sectional study of knowledge, attitudes and beliefs of parents in Zamfara state, Nigeria. BMC Public Health 2012, 12, 800. [Google Scholar] [CrossRef] [PubMed]
- Knowledge, Attitudes and Practices (KAPs) Polls in Pakistan and Nigeria|The Polio Network. 1 July 2014. Available online: https://www.comminit.com/polio/content/knowledge-attitudes-and-practices-kaps-polls-pakistan-and-nigeria (accessed on 20 February 2023).
- Shawn, D.H.; Gold, R. Survey of parents’ attitudes to the recommended Haemophilus influenzae type b vaccine program. CMAJ Can. Med. Assoc. J. 1987, 136, 1038. [Google Scholar]
- Baumgaertner, B.; Carlisle, J.E.; Justwan, F. The influence of political ideology and trust on willingness to vaccinate. PLoS ONE 2018, 13, e0191728. [Google Scholar] [CrossRef] [PubMed]
- Bhutta, Z.A. Infectious disease: Polio eradication hinges on child health in Pakistan. Nature 2014, 511, 285–287. [Google Scholar] [CrossRef] [PubMed]
- Loevinsohn, B.; Hong, R.; Gauri, V. Will more inputs improve the delivery of health services?: Analysis of district vaccination coverage in Pakistan. Int. J. Health Plan. Manag. 2006, 21, 45–54. [Google Scholar] [CrossRef]
- Edwards, K.M.; Hackell, J.M.; Committee on Infectious Diseases; The Committee on Practice and Ambulatory Medicine. Countering vaccine hesitancy. Pediatrics 2016, 138, e20162146. [Google Scholar] [CrossRef]
- Khowaja, A.R.; Khan, S.A.; Nizam, N.; Omer, S.B.; Zaidi, A. Parental perceptions surrounding polio and self-reported non-participation in polio supplementary immunization activities in Karachi, Pakistan: A mixed methods study. Bull. World Health Organ. 2012, 90, 822–830. [Google Scholar] [CrossRef] [PubMed]
- Nasir, S.-G.; Aliyu, G.; Ya’u, I.; Gadanya, M.; Mohammad, M.; Zubair, M.; El-Kamary, S.S. From intense rejection to advocacy: How Muslim clerics were engaged in a polio eradication initiative in Northern Nigeria. PLoS Med. 2014, 11, e1001687. [Google Scholar] [CrossRef] [PubMed]
- Dotto, C. Vaccine case study: Understanding the impact of polio vaccine disinformation in Pakistan. First Draft, 19 February 2020. [Google Scholar]
- Pakistan Polio Eradication Programme. National Emergency Action Plan for Polio Eradication 2020; National Emergency Operations Centre: Islamabad, Pakistan, 2020. Available online: https://polioeradication.org/wp-content/uploads/2020/11/Pakistan-NEAP-2020.pdf (accessed on 20 February 2023).
- Habib, M.A.; Soofi, S.; Cousens, S.; Anwar, S.; ul Haque, N.; Ahmed, I.; Ali, N.; Tahir, R.; Bhutta, Z.A. Community engagement and integrated health and polio immunization campaigns in conflict-affected areas of Pakistan: A cluster randomised controlled trial. Lancet Glob. Health 2017, 5, e593–e603. [Google Scholar] [CrossRef] [PubMed]
| Karachi (18 UCs~210 HH/UC) | Bajaur (6 UCs~210 HH/UC) | Pishin (10 UCs~210 HH/UC) |
|---|---|---|
| Gujro, Songal, Maymarabad, Yousaf Goth, Mangopir, Godhra, Gulshan-e-Ghazi, Itehad Town, Islam Nagar, Nai Abbadi, Saeedabad, Muslim Mujahid Colony, Muhajir Camp, Islamia Colony, Pehlwan Goth, Metrovile Colony, Hijrat Colony, Baloch Goth | Khar, Mamund, Salarzai, Nawagai, Uttamkhel, Barang | Bazar Kona, Muchan, Bazar Pishin, Karbala, Batazai, Khanozai, Bostan, Dilsora, Malikyar, Kaza Villa |
| Karachi | Bajaur | Pishin | ||||
|---|---|---|---|---|---|---|
| FGDs | IDIs | FGDs | IDIs | FGDs | IDIs | |
| Mothers | 4 | - | 2 | - | 2 | - |
| Fathers | 4 | - | 2 | - | 2 | - |
| Mothers-in-Law | 4 | - | 2 | - | 2 | - |
| Community influencers | - | 8 | - | 4 | - | 4 |
| Healthcare Providers | - | 8 | - | 4 | - | 4 |
| 12 | 16 | 6 | 8 | 6 | 8 | |
| Karachi | Bajaur | Pishin | |
|---|---|---|---|
| Indicators | |||
| Union councils | 18 | 6 | 10 |
| Households surveyed | 3780 | 1258 | 2099 |
| HH density | 7.8 | 9.1 | 12.5 |
| Total population | 29,381 | 11,507 | 26,223 |
| Male (%) | 50.8 | 51 | 49.8 |
| Total children under 5 years of age | 6181 | 2144 | 4774 |
| Male (%) | 51.73 | 53.26 | 49.79 |
| Illiteracy rate (among respondents) | 44.1 | 74.7 | 84.2 |
| Ownership of household (owned households) | 61.3 | 92.6 | 81.6 |
| Hand-washing practice (after defecation) | 99.7 | 96.5 | 92.3 |
| Water treatment (% treats water) | 45.3 | 31.2 | 42.3 |
| Karachi | Bajaur | Pishin | |
|---|---|---|---|
| Indicators | (n = 3766) | (n = 1258) | (n = 2099) |
| Knowledge about Polio | n (%) | n (%) | n (%) |
| Yes | 3748 (99.5) | 1229 (97.7) | 2036 (97) |
| No | 18 (0.5) | 29 (2.3) | 63 (3) |
| Source of knowledge about Polio | |||
| TV | 2199 (47.1) | 199 (15.8) | 822 (39.2) |
| Radio | 23 (0.5) | 905 (71.9) | 561 (26.7) |
| Newspaper | 49 (1.1) | 31 (2.5) | 139 (6.6) |
| Posters | 388 (8.3) | 49 (3.9) | 416 (19.8) |
| Masjid Imam | 10 (0.2) | 64 (5.1) | 274 (13.1) |
| Local leaders | 24 (0.5) | 79 (6.3) | 19 (0.9) |
| Elders | 1231 (26.4) | 330 (26.2) | 526 (25.1) |
| Neighbors | 368 (7.9) | 169 (13.4) | 445 (21.2) |
| Friends | 131 (2.8) | 66 (5.3) | 264 (12.6) |
| Relatives | 682 (14.6) | 235 (18.7) | 348 (16.6) |
| Doctor | 592 (12.7) | 629 (50) | 451 (21.5) |
| Hakeem | 0 (0) | 1 (0.1) | 29 (1.4) |
| Homeopathic doctor | 0 (0) | 0 (0) | 14 (0.7) |
| Quack | 0 (0) | 0 (0) | 16 (0.8) |
| LHV | 13 (0.3) | 28 (2.2) | 26 (1.2) |
| Nurse | 0 (0) | 2 (0.2) | 27 (1.3) |
| Traditional healer | 0 (0) | 0 (0) | 8 (0.4) |
| LHWs | 58 (1.2) | 339 (27) | 822 (39.2) |
| Vaccinators | 36 (0.8) | 364 (28.9) | 83 (4) |
| Others | 37 (0.8) | 8 (0.6) | 29 (1.4) |
| Consider Polio as a health problem | |||
| Yes | 3482 (92.5) | 1088 (86.5) | 1267 (60.4) |
| No | 90 (2.4) | 69 (5.5) | 231 (11) |
| Don’t know | 194 (5.2) | 101 (8) | 601 (28.6) |
| Knowledge about preventing a child from getting polio | |||
| By proper disposal of waste/sewage | 487 (10.4) | 245 (19.5) | 607 (28.9) |
| By vaccinating a child/person or polio drops | 2643 (56.6) | 811 (64.5) | 1066 (50.8) |
| Avoiding contact with an infected child/person | 86 (1.8) | 96 (7.6) | 305 (14.5) |
| Washing hands with soap and water | 204 (4.4) | 69 (5.5) | 196 (9.3) |
| Others | 997 (21.4) | 6 (0.5) | 9 (0.4) |
| Don’t know | 426 (9.1) | 139 (11.1) | 438 (20.9) |
| Knowledge about how a child gets polio disease | |||
| By drinking dirty water | 602 (12.9) | 246 (19.6) | 701 (33.4) |
| By eating dirty food | 624 (13.4) | 318 (25.3) | 543 (25.9) |
| Through sewage contamination of food/water | 372 (8) | 300 (23.9) | 441 (21) |
| By air/breathing | 34 (0.7) | 117 (9.3) | 452 (21.5) |
| By evil eye | 48 (1) | 212 (16.9) | 442 (21.1) |
| Don’t know | 1626 (34.8) | 73 (5.8) | 367 (17.5) |
| Allah’s will | 793 (17) | 452 (35.9) | 842 (40.1) |
| Other | 403 (8.6) | 4 (0.3) | 3 (0.1) |
| Knowledge about polio transmission | |||
| By air/breathing | 262 (5.6) | 596 (47.4) | 855 (40.7) |
| By evil eye | 28 (0.6) | 152 (12.1) | 359 (17.1) |
| By contaminated water | 389 (8.3) | 183 (14.6) | 496 (23.6) |
| By sewage contamination | 707 (15.2) | 191 (15.2) | 697 (33.2) |
| Through polio vaccines | 43 (0.9) | 258 (20.5) | 160 (7.6) |
| Don’t know | 2543 (54.5) | 334 (26.6) | 773 (36.8) |
| Other | 228 (4.9) | 0 (0) | 8 (0.4) |
| Knowledge about preventive measures for polio | |||
| Completing routine EPI immunization | 2485 (53.3) | 900 (71.5) | 1365 (65) |
| Completing routine EPI immunization plus getting your child vaccinated in NIDs | 1327 (28.4) | 248 (19.7) | 473 (22.5) |
| Proper nutrition of the child | 847 (18.2) | 116 (9.2) | 561 (26.7) |
| Proper hygiene | 1331 (28.5) | 288 (22.9) | 226 (10.8) |
| Proper care | 510 (10.9) | 138 (11) | 138 (6.6) |
| Keeping child away from a sick child | 147 (3.2) | 302 (24) | 651 (31) |
| Proper sewage disposal and sanitation | 99 (2.1) | 75 (6) | 178 (8.5) |
| Other | 429 (9.2) | 0 (0) | 7 (0.3) |
| Do not know | 282 (6) | 57 (4.5) | 247 (11.8) |
| Karachi | Bajaur | Pishin | |
|---|---|---|---|
| Indicators | (n = 3766) | (n = 1258) | (n = 2099) |
| Knowledge about oral polio vaccine | n (%) | n (%) | n (%) |
| Yes | 3759 (99.8) | 1253 (99.6) | 2044 (97.4) |
| No | 7 (0.2) | 5 (0.4) | 55 (2.6) |
| Knowledge about OPV protecting against polio | |||
| Yes | 3347 (88.9) | 1186 (94.3) | 1445 (68.8) |
| No | 55 (1.5) | 21 (1.7) | 25 (1.2) |
| Don’t know | 71 (1.9) | 30 (2.4) | 342 (16.3) |
| Not sure | 293 (7.8) | 21 (1.7) | 287 (13.7) |
| Knowledge about the consequences of not giving OPV | |||
| Child gets polio | 2419 (64.2) | 669 (53.2) | 1208 (57.6) |
| Child will not get polio | 919 (24.4) | 359 (28.5) | 492 (23.4) |
| Polio would not be eradicated from Pakistan | 172 (4.6) | 111 (8.8) | 191 (9.1) |
| Don’t know | 256 (6.8) | 119 (9.5) | 208 (9.9) |
| Perceptions about the safety of OPV | |||
| Completely safe | 2891 (76.8) | 791 (62.9) | 880 (41.9) |
| Reasonably safe | 517 (13.7) | 353 (28.1) | 405 (19.3) |
| Not safe at all | 179 (4.8) | 16 (1.3) | 199 (9.5) |
| Other | 4 (0.1) | 0 (0) | 0 (0) |
| Don’t Know | 175 (4.7) | 97 (7.7) | 615 (29.3) |
| Ever refused to give polio drops to your child? | |||
| Never | 2897 (76.9) | 943 (75) | 1689 (80.5) |
| Once | 294 (7.8) | 209 (16.6) | 111 (5.3) |
| More than once | 420 (11.2) | 92 (7.3) | 290 (13.8) |
| Always | 137 (3.6) | 14 (1.1) | 5 (0.2) |
| Other | 18 (0.5) | 0 (0) | 4 (0.2) |
| Are all your children immunized with OPV? | |||
| Yes | 3543 (94.1) | 1162 (92.4) | 1996 (95.1) |
| No | 95 (2.5) | 16 (1.3) | 33 (1.6) |
| Partially | 99 (2.6) | 32 (2.5) | 42 (2) |
| Not at all | 20 (0.5) | 3 (0.2) | 2 (0.1) |
| Don’t know | 9 (0.2) | 45 (3.6) | 26 (1.2) |
| Did your child/children receive OPV during the recent campaign | |||
| Yes | 3526 (93.6) | 1241 (98.7) | 2067 (98.5) |
| No | 238 (6.3) | 14 (1.1) | 18 (0.9) |
| Don’t know | 2 (0.1) | 3 (0.2) | 14 (0.7) |
| Decision-maker regarding the health matters of the children? | |||
| Mother-in-law | 419 (9) | 353 (28.1) | 769 (36.6) |
| Father-in-law | 136 (2.9) | 359 (28.5) | 633 (30.2) |
| Husband | 2304 (49.4) | 763 (60.7) | 1812 (86.3) |
| Mother/Myself | 2212 (47.4) | 259 (20.6) | 363 (17.3) |
| Other | 65 (1.4) | 0 (0) | 1 (0.1) |
| Decision-maker regarding immunization of the children? | |||
| Mother-in-law | 336 (8.9) | 158 (12.6) | 201 (9.6) |
| Father-in-law | 92 (2.4) | 256 (20.4) | 244 (11.6) |
| Husband | 1562 (41.5) | 703 (55.9) | 1593 (75.9) |
| Mother/Myself | 1717 (45.6) | 139 (11.1) | 59 (2.8) |
| Others | 59 (1.6) | 2 (0.2) | 1 (0.1) |
| Karachi | Bajaur | Pishin | |
|---|---|---|---|
| Reasons | |||
| Reasons for refusing polio drops to child? | n (%) | n (%) | n (%) |
| Vaccine is not halal | 21 (2.4) | 10 (3.2) | 187 (45.6) |
| Vaccine can cause sterility | 163 (18.8) | 62 (19.7) | 280 (68.3) |
| Vaccine is not safe | 162 (18.6) | 11 (3.5) | 161 (39.3) |
| Child has received polio drops too many times | 31 (3.6) | 67 (21.3) | 93 (22.7) |
| Prohibited by community/local leaders | 0 (0) | 0 (0) | 4 (1) |
| Against my religious belief | 6 (0.7) | 0 (0) | 19 (4.6) |
| Other | 227 (26.1) | 42 (13.3) | 13 (3.2) |
| Total | 869 | 315 | 410 |
| Reasons for not giving OPV in the last polio campaign | |||
| Polio team did not visit the house | 86 (26.5) | 90 (86.5) | 92 (83.6) |
| Did not know about OPV | 53 (16.3) | 6 (5.8) | 5 (4.6) |
| Went, but the distribution point had run out of OPV | 3 (0.9) | 1 (1) | 4 (3.6) |
| Child was not at home at the time of the visit | 2 (0.6) | 0 (0) | 1 (0.9) |
| Child was sick | 13 (4) | 2 (1.9) | 1 (0.9) |
| Distribution site is far away | 24 (7.4) | 0 (0) | 1 (0.9) |
| Family members/elders did not allow the child to get OPV | 99 (30.5) | 5 (4.8) | 5 (4.6) |
| Other | 45 (13.9) | 0 (0) | 1 (0.9) |
| Don’t Know | 86 (26.5) | 90 (86.5) | 92 (83.6) |
| Total | 223 | 96 | 103 |
| Karachi | Bajaur | Pishin | ||||
|---|---|---|---|---|---|---|
| Indicators | 2012 | 2020 | 2012 | 2020 | 2012 | 2020 |
| Respondent’s knowledge about polio | 94.1 | 99.5 * | 97.5 | 97.7 | 98.4 | 97.0 |
| Respondent considers polio to be a health problem | 92.2 | 92.5 | 85.6 | 86.5 | 77.6 | 60.4 * |
| Respondents having knowledge about OPV | 99.3 | 99.8 | 96.8 | 99.6 | 97.8 | 97.4 |
| Perceptions about the safety of OPV | ||||||
| Completely safe | 76.5 | 76.8 | 61.6 | 62.9 | 49.7 | 41.9 |
| Reasonably safe | 11.2 | 13.7 | 11 | 28.1 | 28.9 | 19.3 |
| Not safe at all | 1.1 | 4.8 | 2.7 | 1.3 | 1.4 | 9.5 |
| Don’t Know | 11.2 | 4.7 | 24.7 | 7.7 | 19.7 | 29.3 |
| Ever refused OPV | 5.0 | 23.1 * | 17.4 | 25.0 * | 20.0 | 19.5 |
| Immunization card available | 26.4 | 47.7 | 12.9 | 78.1 | 6.9 | 44.5 |
| Immunization status | ||||||
| Fully immunized | 52.3 | 55.5 * | 28.3 | 67.8 * | 56.5 | 68.6 * |
| Partially immunized | 27.9 | 35.1 | 35.4 | 27.3 | 17.2 | 18.0 |
| Unimmunized | 19.8 | 9.4 * | 35.1 | 5.0 * | 25.6 * | 13.4 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Habib, M.A.; Tabassum, F.; Hussain, I.; Khan, T.J.; Syed, N.; Shaheen, F.; Soofi, S.B.; Bhutta, Z.A. Exploring Knowledge and Perceptions of Polio Disease and Its Immunization in Polio High-Risk Areas of Pakistan. Vaccines 2023, 11, 1206. https://doi.org/10.3390/vaccines11071206
Habib MA, Tabassum F, Hussain I, Khan TJ, Syed N, Shaheen F, Soofi SB, Bhutta ZA. Exploring Knowledge and Perceptions of Polio Disease and Its Immunization in Polio High-Risk Areas of Pakistan. Vaccines. 2023; 11(7):1206. https://doi.org/10.3390/vaccines11071206
Chicago/Turabian StyleHabib, Muhammad Atif, Farhana Tabassum, Imtiaz Hussain, Tooba Jawed Khan, Nazia Syed, Fariha Shaheen, Sajid Bashir Soofi, and Zulfiqar A. Bhutta. 2023. "Exploring Knowledge and Perceptions of Polio Disease and Its Immunization in Polio High-Risk Areas of Pakistan" Vaccines 11, no. 7: 1206. https://doi.org/10.3390/vaccines11071206
APA StyleHabib, M. A., Tabassum, F., Hussain, I., Khan, T. J., Syed, N., Shaheen, F., Soofi, S. B., & Bhutta, Z. A. (2023). Exploring Knowledge and Perceptions of Polio Disease and Its Immunization in Polio High-Risk Areas of Pakistan. Vaccines, 11(7), 1206. https://doi.org/10.3390/vaccines11071206







