General Practitioners’ Awareness and Perception of Current Pneumococcal Vaccination for Adult Patients with Known Risk Factors in Switzerland: Evidence from a Survey
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population and Design
2.2. Measures
2.2.1. Self-Reported Awareness of the Recommendations for Vaccinating Adult Patients at Known Risks
2.2.2. Perception of the Recommendations and Pneumococcal Vaccination
2.2.3. Perception of Pneumococcal Disease
2.2.4. Perceived Barriers to Pneumococcal Vaccination
2.2.5. GPs’ Demographic and Professional Characteristics
2.2.6. Previous Experience Vaccinating Adult Patients with Known Risks
2.3. Sample Size and Statistical Analysis
3. Results
3.1. Population Characteristics
3.2. Awareness of the Recommendations for Vaccinating Adult Patients at Known Risks
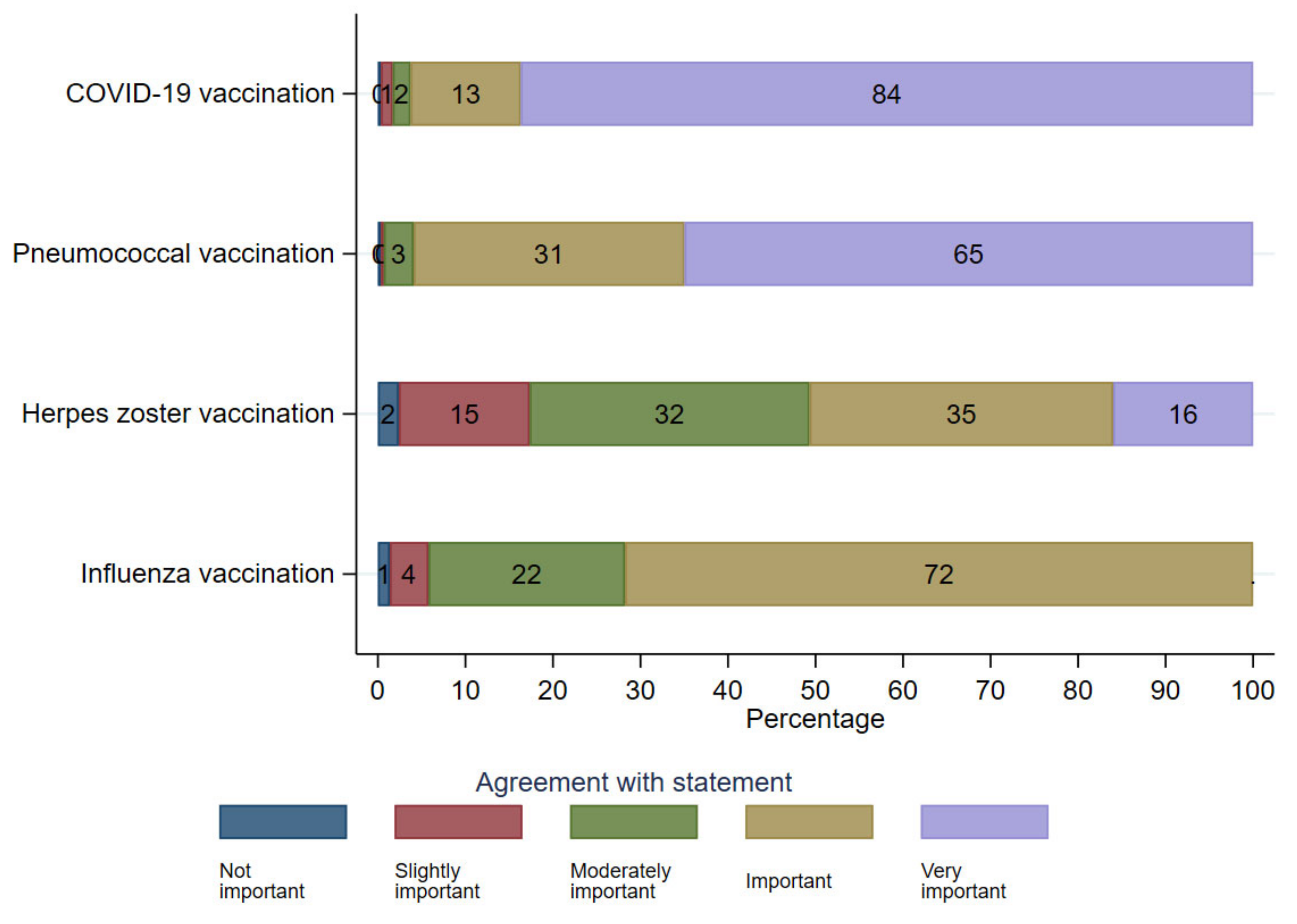
3.3. Agreement and Perception of the Current Vaccination Recommendation
3.4. Perception of Pneumococcal Vaccination
3.5. Attitudes towards Pneumococcal Disease and Vaccination
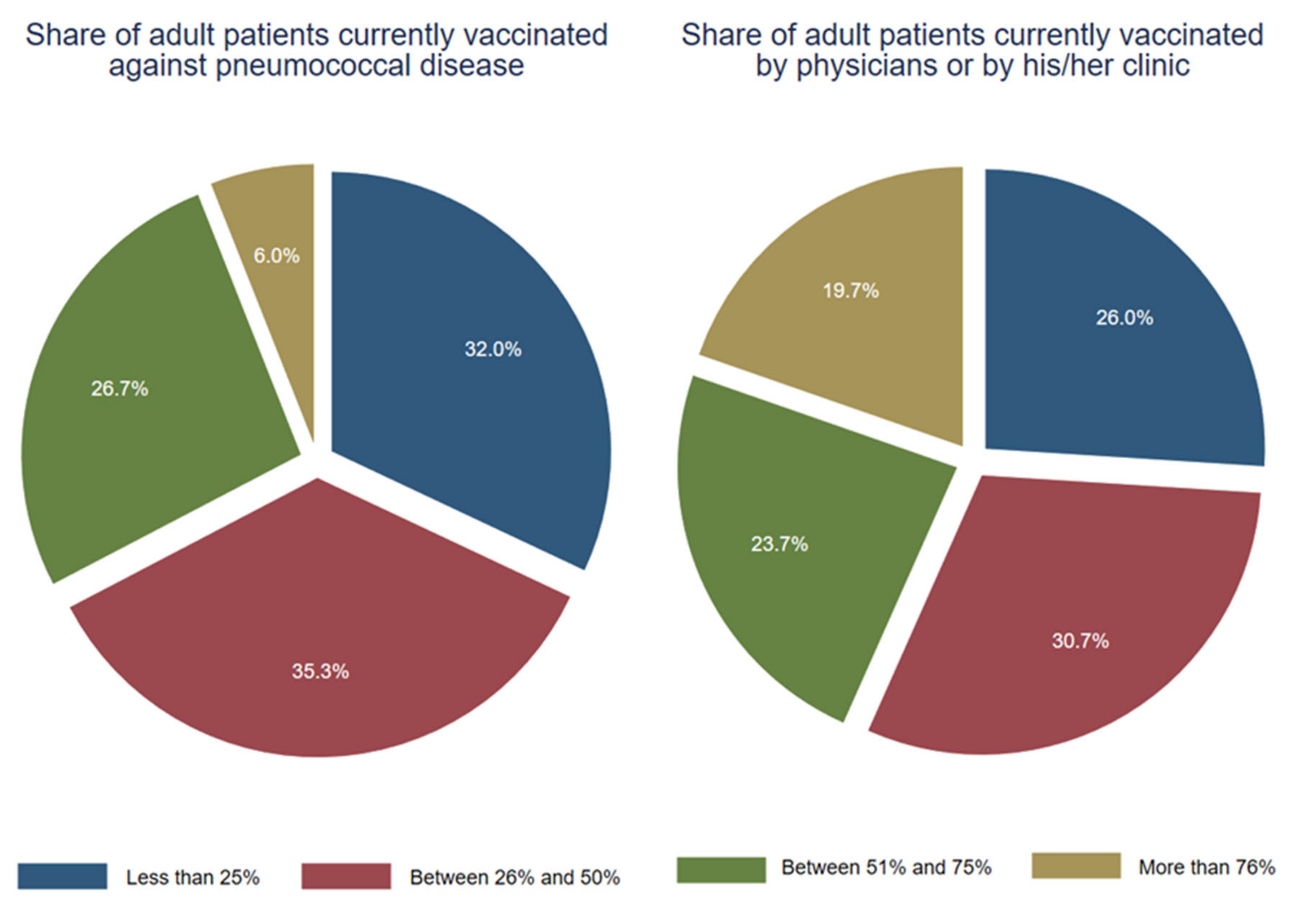
3.6. Current Pneumococcal Vaccination Practice
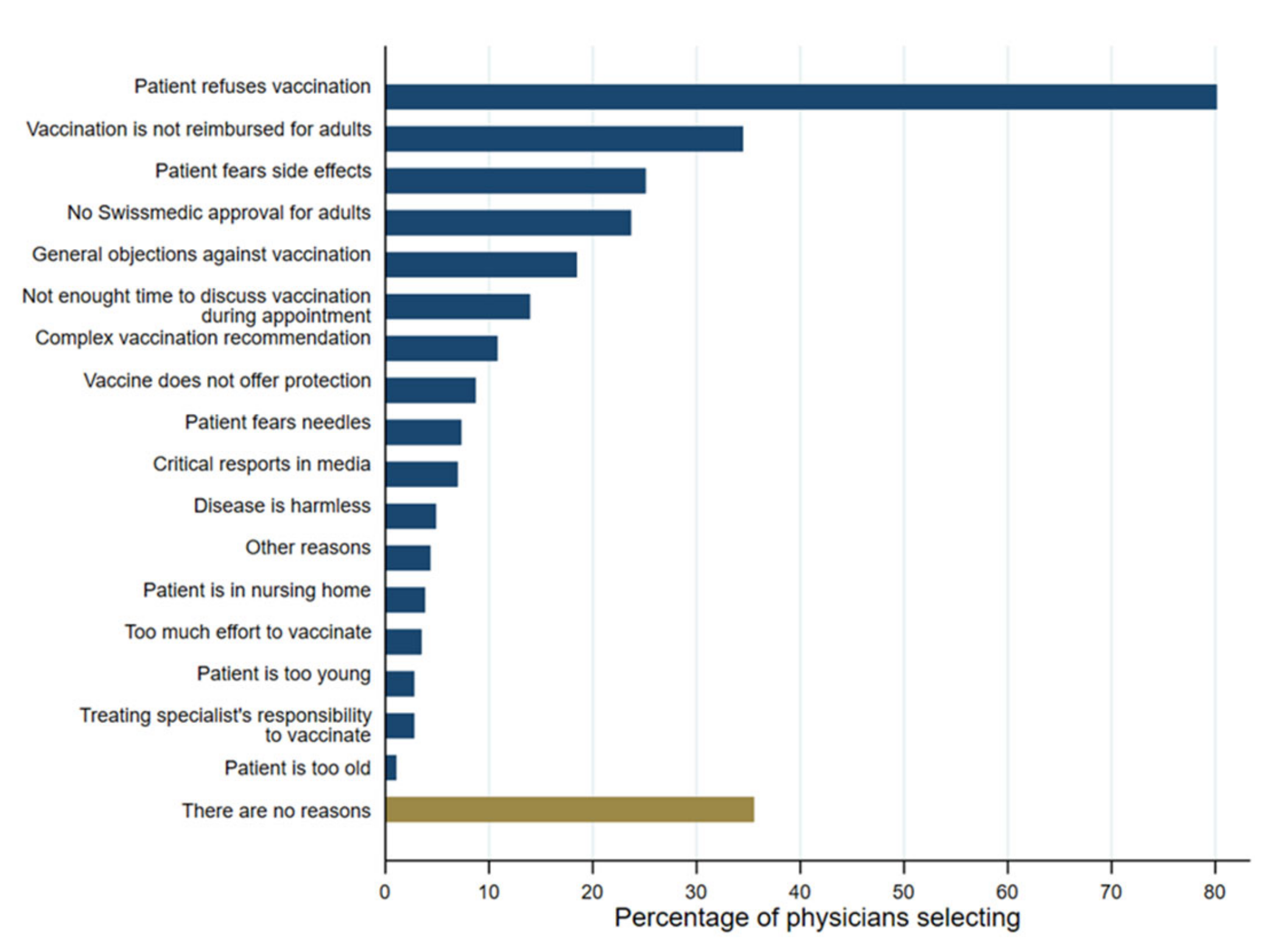
3.7. Reasons for Not Vaccinating
4. Discussion
4.1. Summary
4.2. Comparison with Existing Literature
4.3. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hamborsky, J.; Kroger, A. (Eds.) Epidemiology and Prevention of Vaccine-Preventable Diseases, E-Book: The Pink Book; Public Health Foundation: Washington, DC, USA, 2015. [Google Scholar]
- Cillóniz, C.; Amaro, R.; Torres, A. Pneumococcal vaccination. Curr. Opin. Infect. Dis. 2016, 29, 187–196. [Google Scholar] [CrossRef] [PubMed]
- Feldman, C.; Anderson, R. New insights into pneumococcal disease. Respirology 2009, 14, 167–179. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Liceras, F.C.; Flasche, S.; Sidharta, S.; Yoong, J.; Sundaram, N.; Jit, M. Effect and cost-effectiveness of pneumococcal conjugate vaccination: A global modelling analysis. Lancet Glob. Health 2019, 7, e58–e67. [Google Scholar] [CrossRef]
- Ray, G.T.; Whitney, C.G.; Fireman, B.H.; Ciuryla, V.; Black, S.B. Cost-effectiveness of pneumococcal conjugate vaccine: Evidence from the first 5 years of use in the United States incorporating herd effects. Pediatr. Infect. Dis. J. 2006, 25, 494–501. [Google Scholar] [CrossRef] [PubMed]
- Bundesamt für Gesundheit. Schweizerischer Impfplan 2021. 2021. Available online: https://www.bag.admin.ch/dam/bag/de/dokumente/mt/i-und-b/richtlinien-empfehlungen/allgemeine-empfehlungen/schweizerischer-impfplan.pdf.download.pdf/schweizerischer-impfplan-de.pdf (accessed on 25 April 2023).
- Bundesamt für Gesundheit. Durchimpfung von 2-, 8- und 16-Jährigen Kindern in der Schweiz, 1999–2019. 2020. Available online: https://www.bag.admin.ch/dam/bag/de/dokumente/mt/i-und-b/durchimpfung/tabelle-durchimpfung.xlsx.download.xlsx/tabelle-durchimpfung-200731-de.xlsx (accessed on 25 April 2023).
- Pittet, L.F.; Verolet, C.M.; Michetti, P.; Girardin, M.; Juillerat, P.; Mottet, C.; Maillard, M.H.; Siegrist, C.A.; Posfay-Barbe, K.M.; Swiss Inflammatory Bowel Disease Cohort Study Group. High immunogenicity of the pneumococcal conjugated vaccine in immunocompromised adults with inflammatory bowel disease. Off. J. Am. Coll. Gastroenterol. ACG 2019, 114, 1130–1141. [Google Scholar] [CrossRef]
- Zens, K.D.; Baroutsou, V.; Fehr, J.S.; Lang, P. Pneumococcal vaccination coverage and uptake among adults in Switzerland: A nationwide cross-sectional study of vaccination records. Front. Public Health 2022, 9, 2347. [Google Scholar] [CrossRef]
- Stoffel, S.T.; Colaninno, A.; Bräm, R.; Schwenkglenks, M. Pneumococcal vaccination among adult risk patient with axial spondyloarthritis in Switzerland: Data from the survey of the ankylosing spondylitis association of Switzerland (SVMB). Vaccine 2022, 40, 6206–6210. [Google Scholar] [CrossRef]
- Costello, R.; Winthrop, K.L.; Pye, S.R.; Brown, B.; Dixon, W.G. Influenza and pneumococcal vaccination uptake in patients with rheumatoid arthritis treated with immunosuppressive therapy in the UK: A retrospective cohort study using data from the clinical practice research datalink. PLoS ONE 2016, 11, e0153848. [Google Scholar] [CrossRef]
- Hmamouchi, I.; Winthrop, K.; Launay, O.; Dougados, M. Low rate of influenza and pneumococcal vaccine coverage in rheumatoid arthritis: Data from the international COMORA cohort. Vaccine 2015, 33, 1446–1452. [Google Scholar] [CrossRef]
- Nguyen, M.T.; Lindegaard, H.; Hendricks, O.; Friis-Møller, N. Factors associated with influenza and pneumococcal vaccine uptake among rheumatoid arthritis patients in Denmark invited to participate in a pneumococcal vaccine trial (Immunovax_RA). Scand. J. Rheumatol. 2017, 46, 446–453. [Google Scholar] [CrossRef]
- Schmedt, N.; Schiffner-Rohe, J.; Sprenger, R.; Walker, J.; von Eiff, C.; Häckl, D. Pneumococcal vaccination rates in immunocompromised patients—A cohort study based on claims data from more than 200,000 patients in Germany. PLoS ONE 2019, 14, e0220848. [Google Scholar] [CrossRef] [PubMed]
- Sprenger, R.; Häckl, D.; Kossack, N.; Schiffner-Rohe, J.; Wohlleben, J.; von Eiff, C. Pneumococcal vaccination rates in immunocompromised patients in Germany: A retrospective cohort study to assess sequential vaccination rates and changes over time. PLoS ONE 2022, 17, e0265433. [Google Scholar] [CrossRef]
- Wyplosz, B.; Fernandes, J.; Sultan, A.; Roche, N.; Roubille, F.; Loubet, P.; Fougère, B.; Moulin, B.; Duhot, D.; Vainchtock, A.; et al. Pneumococcal and influenza vaccination coverage among at-risk adults: A 5-year French national observational study. Vaccine 2022, 40, 4911–4921. [Google Scholar] [CrossRef]
- Kopp, A.; Mangin, O.; Gantzer, L.; Lekens, B.; Simoneau, G.; Ravelomanantsoa, M.; Evans, J.; Bergmann, J.F.; Sellier, P. Pneumococcal vaccination coverage in France by general practitioners in adults with a high risk of pneumococcal disease. Hum. Vaccines Immunother. 2021, 17, 162–169. [Google Scholar] [CrossRef]
- Loubet, P.; Verger, P.; Abitbol, V.; Peyrin-Biroulet, L.; Launay, O. Pneumococcal and influenza vaccine uptake in adults with inflammatory bowel disease in France: Results from a web-based study. Dig. Liver Dis. 2018, 50, 563–567. [Google Scholar] [CrossRef]
- Poethko-Muller, C.; Schmitz, R. Vaccination coverage in German adults: Results of the German Health Interview and Examination Survey for Adults (DEGS1). Bundesgesundheitsblatt Gesundh. Gesundh. 2013, 56, 845–857. [Google Scholar]
- Lejri-El Euchi, H.; Chirpaz, E.; Foucher, A.; Sultan-Bichat, N.; Randrianjohany, A.; Poubeau, P.; Gamon, E.; Roussin, C.; Osdoit, S.; Raffray, L. Vaccination against influenza and pneumococcal infections in patients with autoimmune disorders under biological therapy: Coverage and attitudes in patients and physicians. Eur. J. Intern. Med. 2019, 69, 25–31. [Google Scholar] [CrossRef]
- Hurley, L.P.; Allison, M.A.; Pilishvili, T.; O’Leary, S.T.; Crane, L.A.; Brtnikova, M.; Beaty, B.L.; Lindley, M.C.; Bridges, C.B.; Kempe, A. Primary care physicians’ struggle with current adult pneumococcal vaccine recommendations. J. Am. Board Fam. Med. 2018, 31, 94–104. [Google Scholar] [CrossRef]
- Lode, H.; Ludwig, E.; Kassianos, G. Pneumococcal infection—Low awareness as a potential barrier to vaccination: Results of a European survey. Adv. Ther. 2013, 30, 387–405. [Google Scholar] [CrossRef] [PubMed]
- Klett-Tammen, C.J.; Krause, G.; von Lengerke, T.; Castell, S. Advising vaccinations for the elderly: A cross-sectional survey on differences between general practitioners and physician assistants in Germany. BMC Fam. Pract. 2016, 17, 98. [Google Scholar] [CrossRef] [PubMed]
- Romani, M.H.; Musharrafieh, U.M.; Lakkis, N.A.; Hamadeh, G.N. Family physicians beliefs and attitudes regarding adult pneumococcal and influenza immunization in Lebanon. Fam. Pract. 2011, 28, 632–637. [Google Scholar] [CrossRef] [PubMed]
- Von Wagner, C.; Stoffel, S.T.; Freeman, M.; Laszlo, H.E.; Nicholson, B.D.; Sheringham, J.; Szinay, D.; Hirst, Y. General practitioners’ awareness of the recommendations for faecal immunochemical tests (FITs) for suspected lower gastrointestinal cancers: A national survey. BMJ Open 2019, 9, e025737. [Google Scholar] [CrossRef]
- Lienert, F.; Weiss, O.; Schmitt, K.; Heininger, U.; Guggisberg, P. Acceptance of universal varicella vaccination among Swiss pediatricians and general practitioners who treat pediatric patients. BMC Infect. Dis. 2021, 21, 12. [Google Scholar] [CrossRef]
- Betsch, C.; Schmid, P.; Heinemeier, D.; Korn, L.; Holtmann, C.; Böhm, R. Beyond confidence: Development of a measure assessing the 5C psychological antecedents of vaccination. PLoS ONE 2018, 13, e0208601. [Google Scholar] [CrossRef]
- Bundesamt für Raumenwicklung. Die Sieben Grossregionen der Schweiz: Die Schweiz im Europäischen Regionalsystem. 1999. Available online: https://www.admin.ch/gov/de/start/dokumentation/medienmitteilungen.msg-id-10585.html (accessed on 25 April 2023).
- Mui, L.W.; Chan, A.Y.; Lee, A.; Lee, J. Cross-sectional study on attitudes among general practitioners towards pneumococcal vaccination for middle-aged and elderly population in Hong Kong. PLoS ONE 2013, 8, e78210. [Google Scholar] [CrossRef] [PubMed]
- Badertscher, N.; Morell, S.; Rosemann, T.; Tandjung, R. General practitioners’ experiences, attitudes, and opinions regarding the pneumococcal vaccination for adults: A qualitative study. Int. J. Gen. Med. 2012, 5, 967–974. [Google Scholar]
- Mieczkowski, T.A.; Wilson, S.A. Adult pneumococcal vaccination: A review of physician and patient barriers. Vaccine 2002, 20, 1383–1392. [Google Scholar] [CrossRef] [PubMed]
- Davis, D.A.; Mazmanian, P.E.; Fordis, M.; Van Harrison, R.T.K.E.; Thorpe, K.E.; Perrier, L. Accuracy of physician self-assessment compared with observed measures of competence: A systematic review. JAMA 2006, 296, 1094–1102. [Google Scholar] [CrossRef]
- Neeley, S.M.; Cronley, M.L. When research participants don’t tell it like it is: Pinpointing the effects of social desirability bias using self vs. indirect-questioning. ACR N. Am. Adv. 2004, 31, 432–433. [Google Scholar]
- Stöcker, A.; Hoffmann, J.; Mause, L.; Neufeind, J.; Ohnhäuser, T.; Scholten, N. What impact does the attitude toward COVID-19 vaccination have on physicians as vaccine providers? A cross sectional study from the German outpatient sector. Vaccine 2023, 41, 263–273. [Google Scholar] [CrossRef]
- Kawczak, S.; Mooney, M.; Mitchner, N.; Senatore, V.; Stoller, J.K. The impact of a quality improvement continuing medical education intervention on physicians’ vaccination practice: A controlled study. Hum. Vaccines Immunother. 2020, 16, 2809–2815. [Google Scholar] [CrossRef] [PubMed]
- Kirubarajan, A.; Lynch, M.; Nasreen, S.; Gebretekle, G.B.; Fadel, S.A.; Crowcroft, N.S.; Allin, S. Increasing pneumococcal vaccine uptake in older adults: A scoping review of interventions in high-income countries. BMC Geriatr. 2023, 23, 2. [Google Scholar] [CrossRef] [PubMed]

| Characteristics | N | (%) | |
|---|---|---|---|
| Gender | |||
| Male | 179 | (59.7) | |
| Female | 121 | (40.3) | |
| Age | |||
| 40 years or younger | 40 | (13.3) | |
| 41–45 years old | 44 | (14.6) | |
| 46–50 years old | 53 | (17.7) | |
| 51–55 years old | 62 | (20.7) | |
| 56–60 years old | 57 | (19.0) | |
| 60+ years old | 44 | (14.7) | |
| Practice experience | |||
| 2–10 years | 85 | (28.3) | |
| 11–15 years | 62 | (20.7) | |
| 16–20 years | 45 | (15.0) | |
| 21–25 years | 60 | (20.0) | |
| 26+ years | 48 | (16.0) | |
| Number of patients with known risk factors | |||
| 0–20 | 76 | (25.3) | |
| 21–50 | 105 | (35.0) | |
| 51–100 | 73 | (24.3) | |
| More than 100 | 46 | (15.3) | |
| Major region practising in | |||
| Lake Geneva region | 56 | (18.7) | |
| Espace Mittelland | 57 | (19.0) | |
| Northwest Switzerland | 39 | (13.0) | |
| Zurich | 66 | (22.0) | |
| Eastern Switzerland | 40 | (13.3) | |
| Central Switzerland | 42 | (14.0) | |
| Main practising language | |||
| German | 231 | (77.0) | |
| French | 69 | (23.0) | |
| General attitudes towards vaccination | |||
| Confidence in vaccination [0;18] Median and SD | 15 | (2.90) | |
| Calculation [0;18] Median and SD | 15 | (2.69) | |
| Awareness of Recommendation [0;1] | Awareness of All Patient Groups at Risk [0;1] | |||||
|---|---|---|---|---|---|---|
| Variable | (%) | aOR | 95% CI | (%) | aOR | 95% CI |
| Overall | (81.3) | (42.7) | ||||
| Gender | ||||||
| Male | (76.5) | Ref. | (44.1) | Ref. | ||
| Female | (88.4) | 1.792 | 0.858–3.743 | (40.5) | 0.748 | 0.437–1.281 |
| Age | ||||||
| 40 or younger | (92.5) | Ref. | (37.5) | Ref. | ||
| 41–45 | (93.2) | 1.108 | 0.188–6.531 | (36.4) | 0.769 | 0.294–2.006 |
| 46–50 | (81.8) | 0.576 | 0.119–2.778 | (34.0) | 0.554 | 0.205–1.501 |
| 51-55 | (75.8) | 0.358 | 0.069–1.864 | (43.6) | 0.968 | 0.326–2.874 |
| 56–60 | (68.4) | 0.283 | 0.050–1.615 | (40.4) | 0.577 | 0.173–1.925 |
| 61 or older | (84.1) | 0.781 | 0.109–5.583 | (65.9) | 1.424 | 0.377–5.384 |
| Practice experience | ||||||
| 2–10 years | (92.9) | Ref. | (31.8) | Ref. | ||
| 11–15 years | (77.4) | 0.246 | 0.072–0.846 * | (43.6) | 1.711 | 0.763–3.836 |
| 16–20 years | (77.8) | 0.474 | 0.114–1.964 | (40.0) | 1.442 | 0.530–3.921 |
| 21–25 years | (73.3) | 0.341 | 0.081–1.436 | (41.7) | 1.512 | 0.542–4.219 |
| 26+ years | (79.2) | 0.383 | 0.073–2.024 | (64.6) | 2.922 | 0.871–9.803 |
| Number of patients with known risk factors | ||||||
| 0–20 | (73.7) | Ref. | (36.9) | Ref. | ||
| 21–50 | (82.9) | 1.756 | 0.788–3.917 | (36.2) | 1.028 | 0.531–1.989 |
| 51–100 | (89.0) | 3.037 | 1.126–8.190 * | (48.0) | 1.913 | 0.940–3.890 |
| More than 100 | (78.3) | 1.154 | 0.438–3.043 | (58.7) | 3.142 | 1.390–7.105 ** |
| Major region practising in | ||||||
| Lake Geneva region | (83.9) | Ref. | (48.2) | Ref. | ||
| Espace Mittelland | (80.7) | 0.433 | 0.098–1.922 | (43.9) | 0.829 | 0.240–2.866 |
| North-West Switzerland | (79.5) | 0.189 | 0.027–1.330 | (35.9) | 0.555 | 0.118–2.616 |
| Zurich | (84.9) | 0.333 | 0.052–2.139 | (43.9) | 0.746 | 0.173–3.218 |
| Eastern Switzerland | (70.0) | 0.116 | 0.018–0.761 * | (45.0) | 1.110 | 0.238–5.165 |
| Central Switzerland | (85.7) | 0.280 | 0.040–1.942 | (35.7) | 0.536 | 0.117–2.449 |
| Main practising language | ||||||
| German | (81.8) | Ref. | (41.6) | Ref. | ||
| French | (79.7) | 0.308 | 0.061–1.563 | (46.4) | 0.852 | 0.233–3.123 |
| Vaccination attitudes | ||||||
| Confidence | 0.915 | 0.806–1.038 | 0.941 | 0.859–1.029 | ||
| Calculation | 1.109 | 0.977–1.257 | 1.147 | 1.030–1.277 * | ||
| N | 300 | 300 | ||||
| Questionnaire Item | Strongly or Moderately Disagree | Strongly or Moderately Agree | ||
|---|---|---|---|---|
| n | (%) | n | (%) | |
| The treating specialist for the risk factors/chronic conditions should recommend the GP to vaccinate the risk patients. | 4 | (1.3) | 232 | (77.3) |
| I have good arguments to convince adult risk patients of the importance of the pneumococcal vaccination. | 5 | (1.7) | 200 | (66.7) |
| I check the vaccination status of risk patients and propose a pneumococcal vaccination if needed. | 8 | (2.7) | 140 | (46.7) |
| I recognize patients at risk for pneumococcal disease. | 10 | (3.3) | 125 | (41.7) |
| Adult risk group patients are aware that they need a pneumococcal vaccination. | 177 | (59.0) | 16 | (5.3) |
| Pneumococcal vaccination for adult risk groups is not important, since it is not covered by basic health insurance. | 260 | (86.7) | 11 | (3.7) |
| Questionnaire Item | Strongly or Moderately Disagree | Strongly or Moderately Agree | ||
|---|---|---|---|---|
| n | (%) | n | (%) | |
| I think that the pneumococcal disease is serious enough for adults with known risk factors to justify vaccination. | 7 | (2.3) | 256 | (85.3) |
| Pneumococcal disease can cause considerable morbidity and mortality. | 18 | (6.0) | 218 | (72.7) |
| Pneumococcal vaccination of risk groups is even more important during the COVID-19 pandemic. | 11 | (3.7) | 205 | (68.3) |
| Simplification of vaccination guidelines for pneumococcal vaccination in adults would result in more risk patients being vaccinated. | 10 | (3.3) | 179 | (59.7) |
| Pneumococcal disease has a mild disease course for adults with known risk factors. | 237 | (79.0) | 13 | (4.3) |
| The risk of pneumococcal disease is low even for adults with risk factors. | 197 | (65.7) | 7 | (2.3) |
| I am worried about the potential side effects of the pneumococcal vaccine for adults with known risk factors | 215 | (71.7) | 7 | (2.3) |
| Pneumococcal vaccination should mainly target children and not adults because of herd immunity. | 219 | (73.0) | 7 | (2.3) |
| Treating Specialist Should Recommend the GP to Vaccinate the Risk Patients [1;7] | I Have Good Arguments to Convince Patients of the Importance of the Pneumococcal Vaccination [1;7] | I Check the Vaccination Status and Propose a Pneumococcal Vaccination if Needed [1;7] | I Recognize Patients at Risk for Pneumococcal Disease [1;7] | Patients Are Aware that They Need a Pneumococcal Vaccination [1;7] | Vaccination Is Not Important, as It Is Not Covered by Basic Health Insurance [1;7] | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | aOR | 95% CI | aOR | 95% CI | aOR | 95% CI | aOR | 95% CI | aOR | 95% CI | aOR | 95% CI |
| Gender | ||||||||||||
| Male | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | ||||||
| Female | 0.708 | 0.442–1.137 | 0.803 | 0.501–1.287 | 0.992 | 0.632–1.558 | 0.864 | 0.541–1.380 | 0.844 | 0.535–1.331 | 0.732 | 0.433–1.240 |
| Age | ||||||||||||
| 40 or younger | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | ||||||
| 41–45 | 0.818 | 0.350–1.911 | 0.909 | 0.394–2.099 | 1.408 | 0.628–3.157 | 1.065 | 0.476–2.383 | 0.921 | 0.409–2.078 | 0.964 | 0.388–2.396 |
| 46-50 | 1.214 | 0.507–2.905 | 0.730 | 0.313–1.702 | 0.771 | 0.337–1.762 | 0.694 | 0.303–1.588 | 1.534 | 0.655–3.591 | 0.673 | 0.258–1.759 |
| 51–55 | 1.067 | 0.413–2.755 | 0.331 | 0.127–0.863 * | 0.957 | 0.380–2.407 | 0.728 | 0.280–1.893 | 1.581 | 0.628–3.984 | 0.512 | 0.175–1.494 |
| 56–60 | 0.760 | 0.270–2.143 | 0.771 | 0.269–2.211 | 1.774 | 0.650–4.841 | 1.911 | 0.664–5.501 | 1.194 | 0.429–3.324 | 0.450 | 0.138–1.471 |
| 61 or older | 0.694 | 0.210–2.294 | 0.872 | 0.269–2.832 | 2.960 | 0.971–9.019 | 3.806 | 1.171–12.370 * | 1.856 | 0.575–5.991 | 0.346 | 0.086–1.386 |
| Practice experience | ||||||||||||
| 2–10 years | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | ||||||
| 11–15 years | 0.974 | 0.481–1.972 | 0.759 | 0.384–1.499 | 1.371 | 0.700–2.682 | 0.853 | 0.430–1.692 | 1.237 | 0.634–2.413 | 1.153 | 0.531–2.501 |
| 16–20 years | 0.552 | 0.235–1.297 | 1.832 | 0.767–4.377 | 0.820 | 0.352–1.912 | 0.796 | 0.331–1.912 | 0.646 | 0.282–1.479 | 1.727 | 0.653–4.562 |
| 21–25 years | 0.752 | 0.318–1.779 | 1.562 | 0.653–3.736 | 0.637 | 0.274–1.479 | 0.514 | 0.212–1.245 | 1.076 | 0.468–2.473 | 1.762 | 0.654–4.747 |
| 26+ years | 1.003 | 0.355–2.837 | 0.811 | 0.284–2.320 | 0.507 | 0.190–1.351 | 0.245 | 0.084–0.715 * | 1.039 | 0.368–2.932 | 2.167 | 0.620–7.577 |
| Number of patients with known risk factors | ||||||||||||
| 0–20 | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | ||||||
| 21–50 | 1.056 | 0.601–1.856 | 1.374 | 0.784–2.408 | 0.852 | 0.499–1.455 | 1.059 | 0.613–1.828 | 0.781 | 0.455–1.340 | 1.362 | 0.716–2.592 |
| 51–100 | 0.988 | 0.530–1.839 | 1.441 | 0.779–2.667 | 1.121 | 0.614–2.046 | 2.020 | 1.089–3.745 * | 1.285 | 0.710–2.326 | 1.450 | 0.730–2.881 |
| More than 100 | 1.020 | 0.495–2.102 | 1.925 | 0.959–3.864 | 2.180 | 1.093–4.348 * | 2.400 | 1.178–4.888 * | 0.975 | 0.492–1.934 | 1.026 | 0.445–2.364 |
| Major region practising in | ||||||||||||
| Lake Geneva region | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | ||||||
| Espace Mittelland | 0.550 | 0.187–1.613 | 0.674 | 0.232–1.962 | 0.949 | 0.321–2.804 | 0.816 | 0.269–2.478 | 0.235 | 0.078–0.703 ** | 2.278 | 0.652–7.954 |
| North–West Switzerland | 0.427 | 0.109–1.670 | 0.423 | 0.111–1.617 | 0.517 | 0.135–1.989 | 0.377 | 0.097–1.474 | 0.315 | 0.083–1.198 | 1.037 | 0.224–4.800 |
| Zurich | 0.697 | 0.194–2.506 | 0.404 | 0.113–1.448 | 0.557 | 0.156–1.992 | 0.502 | 0.137–1.839 | 0.346 | 0.098–1.226 | 1.099 | 0.258–4.683 |
| Eastern Switzerland | 0.494 | 0.130–1.876 | 0.409 | 0.108–1.555 | 0.464 | 0.122–1.765 | 0.471 | 0.122–1.814 | 0.159 | 0.042–0.607 ** | 1.755 | 0.391–7.881 |
| Central Switzerland | 0.700 | 0.187–2.615 | 0.340 | 0.091–1.267 | 0.705 | 0.190–2.613 | 0.717 | 0.189–2.726 | 0.342 | 0.092–1.270 | 1.517 | 0.343–6.706 |
| Practising language | ||||||||||||
| German | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | ||||||
| French | 1.020 | 0.332–3.131 | 0.446 | 0.144–1.374 | 0.763 | 0.247–2.357 | 1.043 | 0.329–3.302 | 0.353 | 0.111–1.128 | 0.639 | 0.186–2.204 |
| Vaccination attitudes | ||||||||||||
| Confidence | 1.149 | 1.062–1.242 ** | 1.151 | 1.064–1.246 ** | 1.009 | 0.934–1.091 | 0.988 | 0.914–1.068 | 0.967 | 0.897–1.042 | 0.919 | 0.842–1.002 |
| Calculation | 1.124 | 1.028–1.228 * | 1.173 | 1.070–1.285 ** | 1.178 | 1.079–1.287 ** | 1.240 | 1.137–1.352 ** | 0.985 | 0.907–1.070 | 0.852 | 0.774–0.939 ** |
| N | 300 | 300 | 300 | 300 | 300 | 300 | ||||||
| Proportion of Patients Being Vaccinated [1;4] | Proportion of Those Patients Vaccinated by Physician or Clinic [1;4] | |||
|---|---|---|---|---|
| Variable | aOR | 95% CI | aOR | 95% CI |
| Gender | ||||
| Male | Ref. | Ref. | ||
| Female | 0.912 | 0.576–1.444 | 0.996 | 0.630–1.574 |
| Age | ||||
| 40 or younger | Ref. | Ref. | ||
| 41–45 | 0.747 | 0.332–1.678 | 0.604 | 0.268–1.362 |
| 46–50 | 0.825 | 0.360–1.889 | 0.960 | 0.412–2.238 |
| 51–55 | 0.718 | 0.277–1.860 | 0.737 | 0.284–1.910 |
| 56–60 | 1.291 | 0.446–3.736 | 1.680 | 0.565–4.999 |
| 61 or older | 1.928 | 0.567–6.557 | 2.635 | 0.784–8.850 |
| Practice experience | ||||
| 2–10 years | Ref. | Ref. | ||
| 11–15 years | 0.973 | 0.494–1.919 | 1.247 | 0.625–2.488 |
| 16–20 years | 0.443 | 0.187–1.048 | 1.335 | 0.565–3.155 |
| 21–25 years | 0.407 | 0.166–0.998 * | 0.973 | 0.397–2.385 |
| 26+ years | 0.416 | 0.141–1.221 | 0.845 | 0.283–2.522 |
| Number of patients with known risk factors | ||||
| 0–20 | Ref. | Ref. | ||
| 21–50 | 0.619 | 0.354–1.084 | 0.945 | 0.548–1.631 |
| 51–100 | 0.752 | 0.412–1.370 | 2.050 | 1.115–3.769 * |
| More than 100 | 0.628 | 0.306–1.285 | 1.174 | 0.584–2.361 |
| Major region practising in | ||||
| Lake Geneva region | Ref. | Ref. | ||
| Espace Mittelland | 0.267 | 0.089–0.796 * | 0.601 | 0.205–1.760 |
| North–West Switzerland | 0.435 | 0.115–1.644 | 0.190 | 0.051–0.709 * |
| Zurich | 0.463 | 0.130–1.647 | 0.273 | 0.079–0.944 * |
| Eastern Switzerland | 0.133 | 0.035–0.510 ** | 0.183 | 0.049–0.680 * |
| Central Switzerland | 0.345 | 0.092–1.287 | 0.329 | 0.090–1.209 |
| Main practising language | ||||
| German | Ref. | Ref. | ||
| French | 0.389 | 0.126–1.207 | 0.137 | 0.045–0.421 ** |
| Vaccination attitudes | ||||
| Confidence | 1.009 | 0.933–1.091 | 1.074 | 0.989–1.167 |
| Calculation | 1.039 | 0.956–1.129 | 0.993 | 0.911–1.083 |
| N | 300 | 300 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stoffel, S.T.; Schwenkglenks, M.; Mutschler, T. General Practitioners’ Awareness and Perception of Current Pneumococcal Vaccination for Adult Patients with Known Risk Factors in Switzerland: Evidence from a Survey. Vaccines 2023, 11, 1101. https://doi.org/10.3390/vaccines11061101
Stoffel ST, Schwenkglenks M, Mutschler T. General Practitioners’ Awareness and Perception of Current Pneumococcal Vaccination for Adult Patients with Known Risk Factors in Switzerland: Evidence from a Survey. Vaccines. 2023; 11(6):1101. https://doi.org/10.3390/vaccines11061101
Chicago/Turabian StyleStoffel, Sandro Tiziano, Matthias Schwenkglenks, and Thomas Mutschler. 2023. "General Practitioners’ Awareness and Perception of Current Pneumococcal Vaccination for Adult Patients with Known Risk Factors in Switzerland: Evidence from a Survey" Vaccines 11, no. 6: 1101. https://doi.org/10.3390/vaccines11061101
APA StyleStoffel, S. T., Schwenkglenks, M., & Mutschler, T. (2023). General Practitioners’ Awareness and Perception of Current Pneumococcal Vaccination for Adult Patients with Known Risk Factors in Switzerland: Evidence from a Survey. Vaccines, 11(6), 1101. https://doi.org/10.3390/vaccines11061101






