Framing Effects on Willingness and Perceptions towards COVID-19 Vaccination among University Students in Italy: An Exploratory Study
Abstract
1. Introduction
1.1. Frames and Salience
1.2. Experiment Rationale and Research Questions
1.3. Hypotheses Formulation
2. Methods
2.1. Participants and Setting
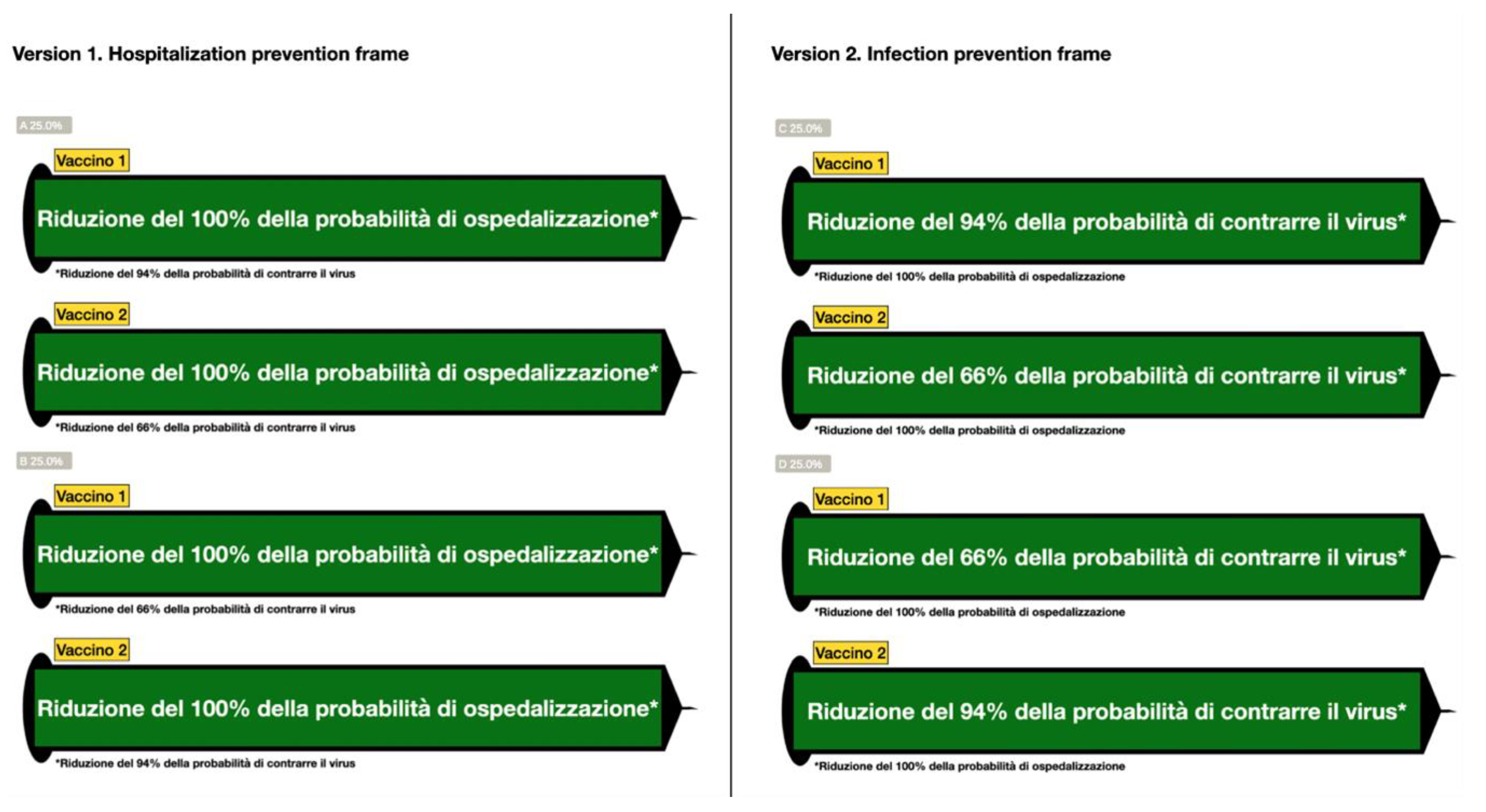
2.2. Experimental Design
2.3. Materials and Methods
2.3.1. Structure of the Questionnaire
2.3.2. Procedure
2.3.3. Ethical Considerations
2.3.4. Analysis
3. Results
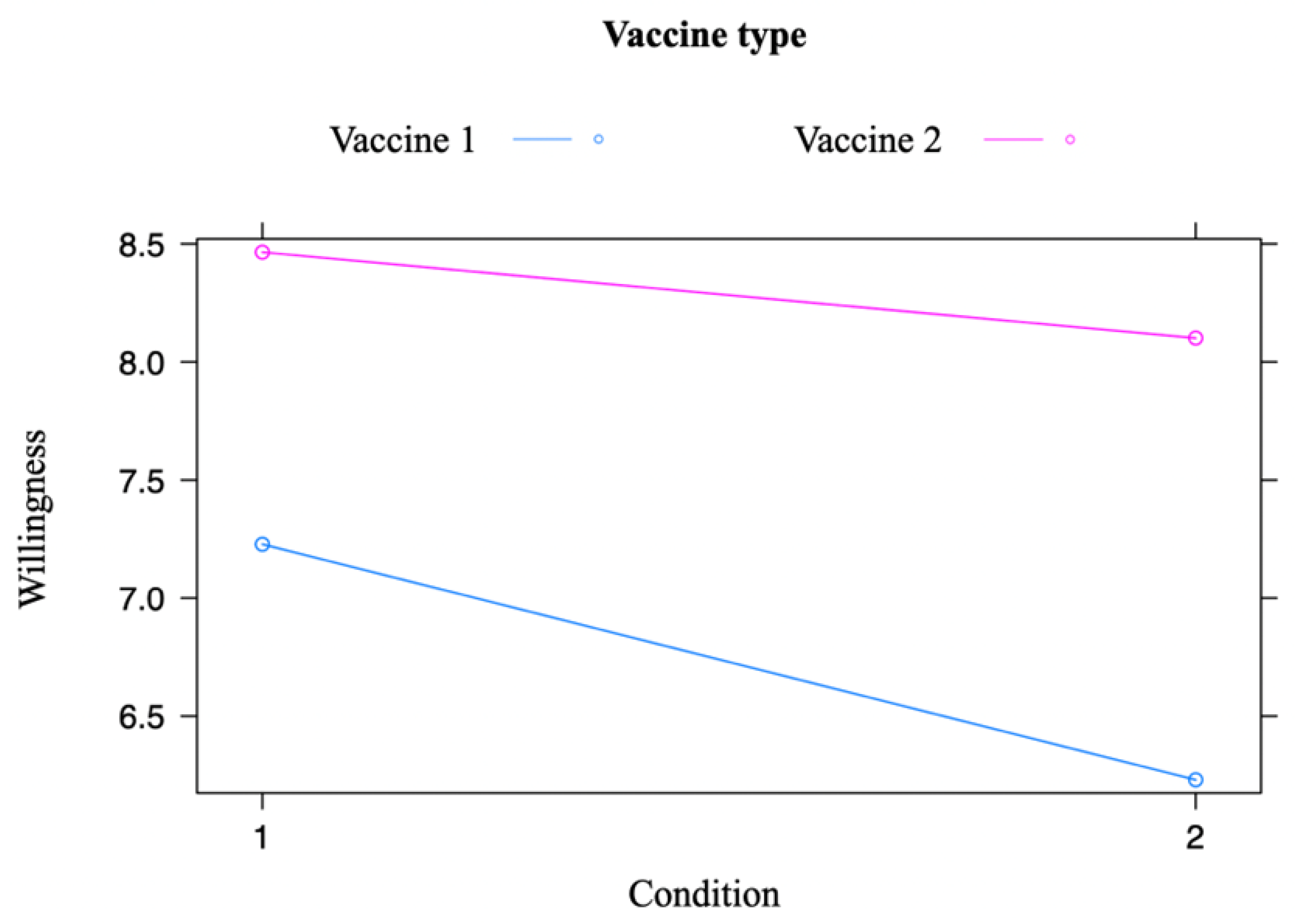
3.1. Main Dimension
3.2. Sub-Dimensions
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dror, A.A.; Eisenbach, N.; Taiber, S.; Morozov, N.G.; Mizrachi, M.; Zigron, A.; Srouji, S.; Sela, E. Vaccine hesitancy: The next challenge in the fight against COVID-19. Eur. J. Epidemiol. 2020, 35, 775–779. [Google Scholar] [CrossRef] [PubMed]
- Sallam, M. COVID-19 Vaccine Hesitancy Worldwide: A Concise Systematic Review of Vaccine Acceptance Rates. Vaccines 2021, 9, 160. [Google Scholar] [CrossRef] [PubMed]
- MacDonald, N.E. Vaccine hesitancy: Definition, scope and determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef] [PubMed]
- WHO. Ten Threats to Global Health in 2019. Available online: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019 (accessed on 27 May 2023).
- Lazarus, J.V.; Wyka, K.; White, T.M.; Picchio, C.A.; Rabin, K.; Ratzan, S.C.; Parsons Leigh, J.; Hu, J.; El-Mohandes, A. Revisiting COVID-19 vaccine hesitancy around the world using data from 23 countries in 2021. Nat. Commun. 2022, 13, 3801. [Google Scholar] [CrossRef] [PubMed]
- Barello, S.; Nania, T.; Dellafiore, F.; Graffigna, G.; Caruso, R. ‘Vaccine hesitancy’ among university students in Italy during the COVID-19 pandemic. Eur. J. Epidemiol. 2020, 35, 781–783. [Google Scholar] [CrossRef] [PubMed]
- Roberts, H.A.; Clark, D.A.; Kalina, C.; Sherman, C.; Brislin, S.; Heitzeg, M.M.; Hicks, B.M. To vax or not to vax: Predictors of anti-vax attitudes and COVID-19 vaccine hesitancy prior to widespread vaccine availability. PLoS ONE 2022, 17, e0264019. [Google Scholar] [CrossRef]
- Jacobson, R.M.; St. Sauver, J.L.; Finney Rutten, L.J. Vaccine Hesitancy. Mayo Clin. Proc. 2015, 90, 1562–1568. [Google Scholar] [CrossRef]
- Smith, K.; Lambe, S.; Freeman, D.; Cipriani, A. COVID-19 vaccines, hesitancy and mental health. Evid. Based Ment. Health 2021, 24, 47. [Google Scholar] [CrossRef]
- De Miguel-Arribas, A.; Aleta, A.; Moreno, Y. Impact of vaccine hesitancy on secondary COVID-19 outbreaks in the US: An age-structured SIR model. BMC Infect. Dis. 2022, 22, 511. [Google Scholar] [CrossRef]
- Gorman, J.M.; Gorman, S.E.; Sandy, W.; Gregorian, N.; Scales, D.A. Implications of COVID-19 Vaccine Hesitancy: Results of Online Bulletin Board Interviews. Front. Public Health 2022, 9, 2269. [Google Scholar] [CrossRef]
- Marcell, L.; Dokania, E.; Navia, I.; Baxter, C.; Crary, I.; Rutz, S.; Soto Monteverde, M.J.; Simlai, S.; Hernandez, C.; Huebner, E.M.; et al. One Vax Two Lives: A social media campaign and research program to address COVID-19 vaccine hesitancy in pregnancy. Am. J. Obs. Gynecol 2022, 227, 685–695.e2. [Google Scholar] [CrossRef] [PubMed]
- Hong, S.-A. COVID-19 vaccine communication and advocacy strategy: A social marketing campaign for increasing COVID-19 vaccine uptake in South Korea. Humanit. Soc. Sci. Commun. 2023, 10, 109. [Google Scholar] [CrossRef] [PubMed]
- Chevallier, C.; Hacquin, A.-S.; Mercier, H. COVID-19 Vaccine Hesitancy: Shortening the Last Mile. Trends Cogn. Sci. 2021, 25, 331–333. [Google Scholar] [CrossRef] [PubMed]
- Shim, E.; Chapman, G.B.; Townsend, J.P.; Galvani, A.P. The influence of altruism on influenza vaccination decisions. J. R. Soc. Interface 2012, 9, 2234–2243. [Google Scholar] [CrossRef]
- Jarrett, C.; Wilson, R.; O’Leary, M.; Eckersberger, E.; Larson, H.J. Strategies for addressing vaccine hesitancy—A systematic review. Vaccine 2015, 33, 4180–4190. [Google Scholar] [CrossRef]
- Dubé, E.; Gagnon, D.; MacDonald, N.E. Strategies intended to address vaccine hesitancy: Review of published reviews. Vaccine 2015, 33, 4191–4203. [Google Scholar] [CrossRef]
- Sadaf, A.; Richards, J.L.; Glanz, J.; Salmon, D.A.; Omer, S.B. A systematic review of interventions for reducing parental vaccine refusal and vaccine hesitancy. Vaccine 2013, 31, 4293–4304. [Google Scholar] [CrossRef]
- Tversky, A.; Kahneman, D. The framing of decisions and the psychology of choice. Science 1981, 211, 453–458. [Google Scholar] [CrossRef]
- Sciurti, A.; Baccolini, V.; Renzi, E.; De Blasiis, M.R.; Siena, L.M.; Isonne, C.; Migliara, G.; Massimi, A.; De Vito, C.; Marzuillo, C.; et al. Attitudes of University Students towards Mandatory COVID-19 Vaccination Policies: A Cross-Sectional Survey in Rome, Italy. Vaccines 2023, 11, 721. [Google Scholar] [CrossRef]
- Baccolini, V.; Renzi, E.; Isonne, C.; Migliara, G.; Massimi, A.; De Vito, C.; Marzuillo, C.; Villari, P. COVID-19 Vaccine Hesitancy among Italian University Students: A Cross-Sectional Survey during the First Months of the Vaccination Campaign. Vaccines 2021, 9, 1292. [Google Scholar] [CrossRef]
- Schäfer, T.; Schwarz, M.A. The meaningfulness of effect sizes in psychological research: Differences between sub-disciplines and the impact of potential biases. Front. Psychol. 2019, 10, 813. [Google Scholar] [CrossRef] [PubMed]
- Geng, H.; Cao, K.; Zhang, J.; Wu, K.; Wang, G.; Liu, C. Attitudes of COVID-19 vaccination among college students: A systematic review and meta-analysis of willingness, associated determinants, and reasons for hesitancy. Hum. Vaccines Immunother. 2022, 18, 2054260. [Google Scholar] [CrossRef]
- Clinic, M. Different Types of COVID-19 Vaccines: How They Work. Available online: https://www.mayoclinic.org/diseases-conditions/coronavirus/in-depth/different-types-of-covid-19-vaccines/art-20506465 (accessed on 29 May 2023).
- WHO. Statement for Healthcare Professionals: How COVID-19 Vaccines are Regulated for Safety and Effectiveness (Revised March 2022). Available online: https://www.who.int/news/item/11-06-2021-statement-for-healthcare-professionals-how-covid-19-vac-cines-are-regulated-for-safety-and-effectiveness#:~:text=The%20most%20commonly%2Dreported,vaccines%20from%20clinical%20trials (accessed on 28 May 2023).
- European Medicines Agency. AstraZeneca’s COVID-19 Vaccine: EMA Finds Possible Link to Very Rare Cases of Unusual Blood Clots with Low Blood Platelets; European Medicines Agency: Amsterdam, The Netherlands, 7 April 2021.
- Simon, H.A. Administrative Behavior: A Study of Decision-Making Processes in Administrative Organization, 2nd ed.; Macmillan: New York, NY, USA, 1957. [Google Scholar]
- Palm, R.; Bolsen, T.; Kingsland, J.T. The Effect of Frames on COVID-19 Vaccine Resistance. Front. Political Sci. 2021, 3, 661257. [Google Scholar] [CrossRef]
- Sudharsanan, N.; Favaretti, C.; Hachaturyan, V.; Bärnighausen, T.; Vandormael, A. The effect of framing and communicating COVID-19 vaccine side-effect risks on vaccine intentions for adults in the UK and the USA: A structured summary of a study protocol for a randomized controlled trial. Trials 2021, 22, 592. [Google Scholar] [CrossRef] [PubMed]
- Gurevich, L. Framing effect method in vaccination status discrimination research. Humanit. Soc. Sci. Commun. 2022, 9, 278. [Google Scholar] [CrossRef]
- Prakash, A.; Jeyakumar Nathan, R.; Kini, S.; Victor, V. Message framing and COVID-19 vaccine acceptance among millennials in South India. PLoS ONE 2022, 17, e0269487. [Google Scholar] [CrossRef]
- Tversky, A.; Kahneman, D. Rational Choice and the Framing of Decisions. J. Bus. 1986, 59, S251–S278. [Google Scholar] [CrossRef]
- Druckman, J.N. The Implications of Framing Effects for Citizen Competence. Polit. Behav. 2001, 23, 225–256. [Google Scholar] [CrossRef]
- Kahneman, D. A perspective on judgment and choice: Mapping bounded rationality. Am. Psychol. 2003, 58, 697–720. [Google Scholar] [CrossRef]
- McNeil, B.J.; Pauker, S.G.; Sox, H.C., Jr.; Tversky, A. On the elicitation of preferences for alternative therapies. N. Engl. J. Med. 1982, 306, 1259–1262. [Google Scholar] [CrossRef]
- Farnsworth, B. Saliency in Human Behavior Research. Available online: https://imotions.com/blog/learning/research-fundamentals/saliency/ (accessed on 30 May 2023).
- Kuznetsova, A.; Brockhoff, P.B.; Christensen, R.H.B. lmerTest Package: Tests in Linear Mixed Effects Models. J. Stat. Softw. 2017, 82, 1–26. [Google Scholar] [CrossRef]
- Zarbo, C.; Candini, V.; Ferrari, C.; d’Addazio, M.; Calamandrei, G.; Starace, F.; Caserotti, M.; Gavaruzzi, T.; Lotto, L.; Tasso, A.; et al. COVID-19 Vaccine Hesitancy in Italy: Predictors of Acceptance, Fence Sitting and Refusal of the COVID-19 Vaccination. Front. Public Health 2022, 10, 873098. [Google Scholar] [CrossRef] [PubMed]
- Pertwee, E.; Simas, C.; Larson, H.J. An epidemic of uncertainty: Rumors, conspiracy theories and vaccine hesitancy. Nat. Med. 2022, 28, 456–459. [Google Scholar] [CrossRef] [PubMed]
- Sapienza, A.; Falcone, R. The Role of Trust in COVID-19 Vaccine Acceptance: Considerations from a Systematic Review. Int. J. Environ. Res. Public Health 2022, 20, 665. [Google Scholar] [CrossRef]
- Chung, R.Y.N.; Chung, G.K.K.; Chan, Y.H.; Lee, T.S.K.; Ho, E.S.C.; Chan, S.M.; Chen, J.K.; Wong, H. Trust in government and compliance to COVID-19 vaccination policy. Ann. Epidemiol. 2022, 73, 48. [Google Scholar] [CrossRef]
- Hong, Y.; Hashimoto, M. I Will Get Myself Vaccinated for Others: The Interplay of Message Frame, Reference Point, and Perceived Risk on Intention for COVID-19 Vaccine. Health Commun. 2023, 38, 813–823. [Google Scholar] [CrossRef]
- Goldstein, S.; MacDonald, N.E.; Guirguis, S. Health communication and vaccine hesitancy. Vaccine 2015, 33, 4212–4214. [Google Scholar] [CrossRef]
- Al-Sanafi, M.; Sallam, M. Psychological Determinants of COVID-19 Vaccine Acceptance among Healthcare Workers in Kuwait: A Cross-Sectional Study Using the 5C and Vaccine Conspiracy Beliefs Scales. Vaccines 2021, 9, 701. [Google Scholar] [CrossRef]
- ISTAT. Nel Mezzogiorno Occupazione più Bassa Anche tra i Laureati, Soprattutto se Hanno Meno di 35 Anni [In the South, Employment is Also Lower among Graduates, Especially If They Are under 35 Years Old.]; ISTAT: Rome, Italy, 22 October 2022.
- Williamson, K.; Bujold, P.M.; Thulin, E. Behavior Change Interventions in Practice: A Synthesis of Criteria, Approaches, Case Studies & Indicators; Rare Center for Behavior & the Environment and the Scientific and Technical Advisory Panel to the Global Environment Facility: Washington, DC, USA, 2020. [Google Scholar]
- Van Hoecke, A.L.; Sanders, J.G. An Online Experiment of NHS Information Framing on Mothers’ Vaccination Intention of Children against COVID-19. Vaccines 2022, 10, 720. [Google Scholar] [CrossRef]
- Van Hoecke, A.-S.; Seghers, J.; Boen, F. Promoting stair climbing in a worksite and public setting: Are footprints enough? Am. J. Health Promot. 2018, 32, 527–535. [Google Scholar] [CrossRef]
- Ebrahimi, O.V.; Johnson, M.S.; Ebling, S.; Amundsen, O.M.; Halsøy, Ø.; Hoffart, A.; Skjerdingstad, N.; Johnson, S.U. Risk, Trust, and Flawed Assumptions: Vaccine Hesitancy During the COVID-19 Pandemic. Front. Public Health 2021, 9, 700213. [Google Scholar] [CrossRef] [PubMed]
- Caserotti, M.; Girardi, P.; Rubaltelli, E.; Tasso, A.; Lotto, L.; Gavaruzzi, T. Associations of COVID-19 risk perception with vaccine hesitancy over time for Italian residents. Soc. Sci. Med. 2021, 272, 113688. [Google Scholar] [CrossRef] [PubMed]
- Couto, K.C.; Lorenzo, F.M.; Tagliabue, M.; Borges Henriques, M.; Freitas Lemos, R. Underlying principles of a COVID-19 behavioral vaccine for a sustainable cultural change. Int. J. Environ. Res. Public Health 2020, 17, 9066. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cesareo, M.; Tagliabue, M.; Lopes, M.E.; Moderato, P. Framing Effects on Willingness and Perceptions towards COVID-19 Vaccination among University Students in Italy: An Exploratory Study. Vaccines 2023, 11, 1079. https://doi.org/10.3390/vaccines11061079
Cesareo M, Tagliabue M, Lopes ME, Moderato P. Framing Effects on Willingness and Perceptions towards COVID-19 Vaccination among University Students in Italy: An Exploratory Study. Vaccines. 2023; 11(6):1079. https://doi.org/10.3390/vaccines11061079
Chicago/Turabian StyleCesareo, Massimo, Marco Tagliabue, Magdalena Edyta Lopes, and Paolo Moderato. 2023. "Framing Effects on Willingness and Perceptions towards COVID-19 Vaccination among University Students in Italy: An Exploratory Study" Vaccines 11, no. 6: 1079. https://doi.org/10.3390/vaccines11061079
APA StyleCesareo, M., Tagliabue, M., Lopes, M. E., & Moderato, P. (2023). Framing Effects on Willingness and Perceptions towards COVID-19 Vaccination among University Students in Italy: An Exploratory Study. Vaccines, 11(6), 1079. https://doi.org/10.3390/vaccines11061079







