A Behavioural-Theory-Based Qualitative Study of the Beliefs and Perceptions of Marginalised Populations towards Community Volunteering to Increase Measles Immunisation Coverage in Sabah, Malaysia
Abstract
1. Introduction
2. Method
2.1. Study Setting
2.2. Sample Selection and Recruitment
2.3. Survey Instrument
2.4. Study Procedures
2.5. Data Analysis
2.6. Ethical Approval
3. Results
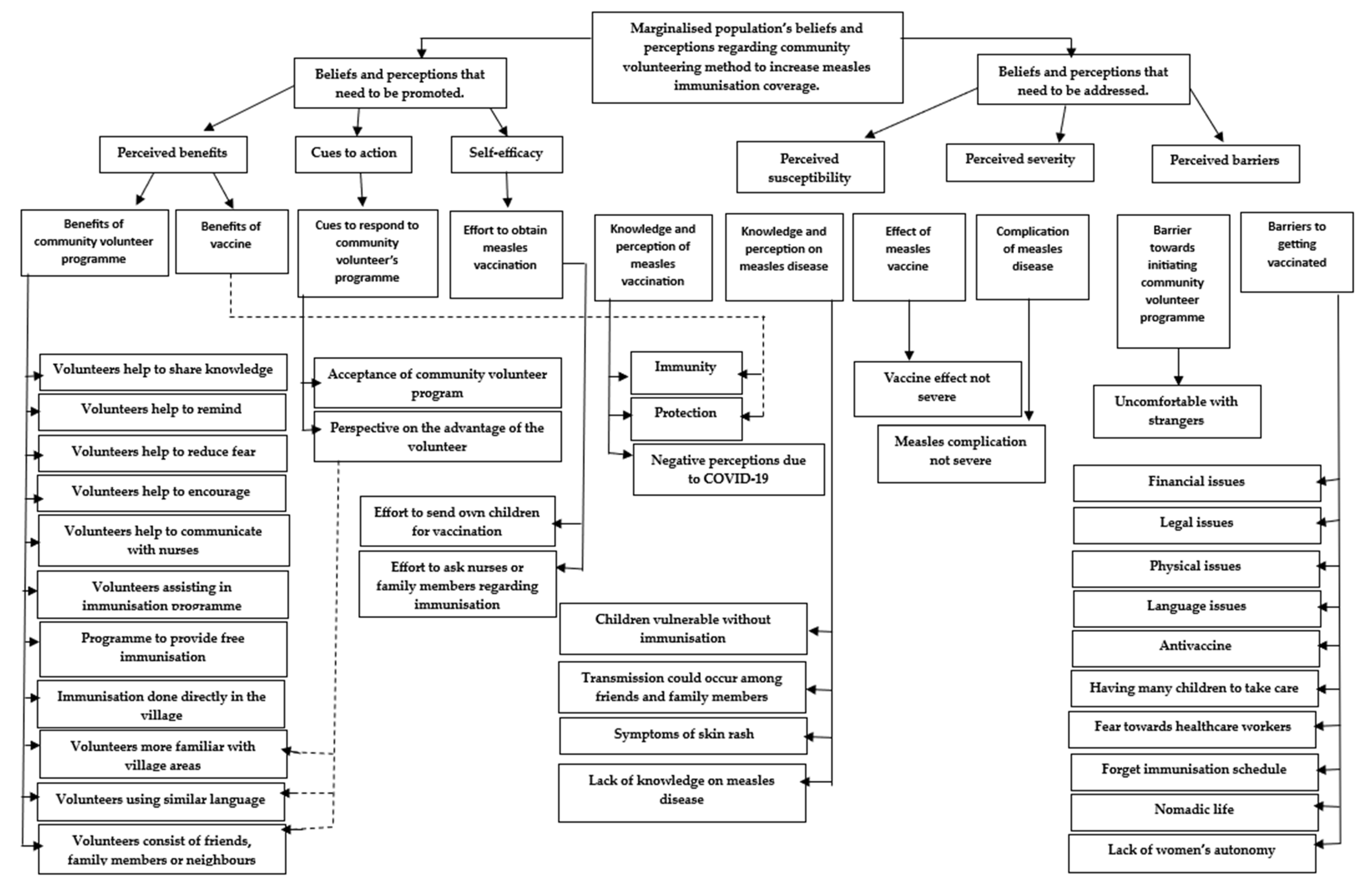
3.1. Components of the Health Belief Model (HBM)
3.1.1. Perceived Susceptibility
“I am not sure. I have never heard of measles.”(ID 2)
“I have heard of measles. Children exhibit skin rashes.”(ID 30).
“We are susceptible to measles as it could be anywhere. Some children in this village have skin rashes which could, possibly, be measles.”(ID 25).
“None of my family members have ever had measles. So, we probably have low susceptibility to measles.”(ID 22).
“At present, as all my family members are completely vaccinated so, we are protected from measles. It is dangerous for children if they are not vaccinated as they have a higher likelihood of contracting the disease.”(ID 1).
“I have heard of measles. The MCV increases the number of antibodies required to fight the disease.”(ID 10).
“Since the beginning of the COVID-19 pandemic, many people have refused to take their children to clinics to get vaccinated. Therefore, someone should come and explain so that people feel confident about vaccinating their children.”(ID 29).
3.1.2. Perceived Severity
“It is normal for children to have a fever and skin rashes. If they are eating and drinking like normal, it means they will recover.”(ID 39).
“My children usually develop a fever post-vaccination but they recover after taking anti-pyretic medication. So, I am not too worried about the side effects of the MCV.”(ID 1).
“This is my third child and his vaccinations are up-to-date. He did not develop any side effects following his measles vaccination.”(ID 5).
3.1.3. Perceived Benefit
“So long as my children are vaccinated, it is okay. It is for their health after all.”(ID 24).
“Having a community volunteer may be beneficial as they can help children get their MCVs.”(ID 9).
“I am not sure how community volunteers could help. Maybe if they promote immunisation, more people would understand and take their children to be vaccinated.”(ID 20).
“As the volunteers can explain immunisation, it would help the people in this village understand better.”(ID 7).
“I agree with this programme as it could help remind me of my children’s appointment. I sometimes I forget.”(ID 9).
“Many people here are afraid of vaccinating their children because of the COVID-19 pandemic. Maybe if the volunteer is from our own village and encourages vaccination, more people will be confident about vaccinating their children.”(ID 28).
“If there are community volunteers in this village, maybe the people of this village will be less afraid of asking questions about vaccination.”(ID 8).
“It will be good if the community volunteers can help inform the nurses when we are unable to attend a vaccination appointment at the clinic as it is difficult to travel when the area is flooded.”(ID 37).
“I agree with the community volunteer programme. If there are people coming to the village to vaccinate the children, they can educate other villagers and neighbouring villages so they can all bring their children with them.”(ID 27).
“The community volunteer programme seems okay to me. It would be even better if people can come and administer the free MCV to the children. After all, it is for their health.”(ID 36).
3.1.4. Perceived Barriers
“What is the point of taking my children to a clinic to be vaccinated if I do not have money?”(ID 11).
“I cannot vaccinate my children at a clinic because I do not have legal documentation. Even if I did have the required documents, I cannot travel there as I cannot afford it.”(ID 36).
“The villagers need to help each other because many do not understand or speak Malay. Most of them only speak Suluk amongst themselves.”(ID 32).
“I have many children, so if there is nobody at home to look after them, I have to bring all of them along with me to the clinic. It is very difficult for me to bring all of them along.”(ID 21).
“The area sometimes floods when it rains heavily. So, it is difficult to travel to the clinic when it is flooded.”(ID 25).
“It is difficult to travel to the clinic when the sea is rough. When it is too windy, I cancel my plans to go to the clinic.”(ID 13).
“I have no problem travelling to the clinic but the walk is quite tiring as I am pregnant. On the island, I have to walk to the boat at the town’s jetty. Then I have to walk further to reach the clinic. It takes about a half an hour of walking from the island to reach the clinic.”(ID 9).
“If I had an illness that I was unfamiliar with, I would ask my family or the nurses at the clinic. But I would prefer to ask my family first because I am scared that the nurses will scold me.”(ID 27).
“I usually ask the nurses but I always get scolded. They always answer me as if they are angry. Even when I ask them politely, I still get scolded.”(ID 16).
“I often forget the children’s vaccination appointments and the nurses never remind me.”(ID 1).
“I do not have any problem taking my children to the clinic to be vaccinated. I used to go to the Maternal and Child Health Clinic (Klinik Kesihatan Ibu dan Anak, KKIA) in Pekan. Now that I have I moved here with my husband, I go to a clinic in Telipok, which is nearer and only five minutes travel by taxi. But some of my children missed their vaccination appointments because I moved around a lot.”(ID 28).
“I always ask my husband before doing anything. If he does not agree, then there is nothing that I can do about it.”(ID 30).
“Some of my nephews and nieces back home are unvaccinated. Some of my family members are anti-vaccine.”(ID 8).
“Even if the community volunteers are from this village, I would not be confident about vaccinations. Maybe because I do not know them well enough.”(ID 19).
3.1.5. Cues to Action
“I would not mind if there was a community volunteer at the village. Most of the villagers are my relatives anyway.”(ID 3).
“Some of the villagers do not understand Malay. So, a volunteer who can actually help would really help the situation.”(ID 30).
“I do not mind having a community volunteer in the village even though I do not understand how it would help. In any case, the villagers often help nurses locate patients in the village.”(ID 17).
3.1.6. Self-Efficacy
“All the children that I look after are fully vaccinated. Now that I am also taking care of my grandchildren, I made sure that they were fully vaccinated as their parents work far away in town.”(ID 34).
“If I do not know something, I will ask the nurses. They always answer all my questions.”(ID 18).
“I asked my family members and my husband. They do not have any qualms about vaccinating the children.”(ID 2)
4. Discussions
4.1. Key Findings
4.2. Programme Framing and Target
4.3. Strengths and Limitations
5. Conclusions
6. Contributions to Literature
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Iqbal, S.; Di Martino, S.; Kagan, C. Volunteering in the community: Understanding personal experiences of South Asians in the United Kingdom. J. Community Psychology 2023, 1–16. [Google Scholar] [CrossRef]
- Crocker-Buque, T.; Mindra, G.; Duncan, R.; Mounier-Jack, S. Immunization, urbanization and slums—A systematic review of factors and interventions. BMC Public Health 2017, 17, 556. [Google Scholar] [CrossRef]
- Bernama. Young Volunteers Join Malaysia’s Fight against COVID-19. 2021. Available online: https://bernama.com/en/features/news.php?id=1993030 (accessed on 12 May 2023).
- Jiee, S.F.; Bondi, M.E.; Emiral, M.E.; Jantim, A. Polio Supplementary Immunization Activities During COVID-19 Pandemic: Experience from Penampang District, Sabah, Malaysia. J. Prim. Care Community Health 2021, 12, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Sveen, S.; Anthun, K.S.; Batt-Rawden, K.B.; Tingvold, L. Volunteering: A Tool for Social Inclusion and Promoting the Well-Being of Refugees? A Qualitative Study. Societies 2023, 13, 12. [Google Scholar] [CrossRef]
- Bowe, M.; Gray, D.; Stevenson, C.; McNamara, N.; Wakefield, J.R.H.; Kellezi, B.; Wilson, I.; Cleveland, M.; Mair, E.; Halder, M.; et al. A social cure in the community: A mixed-method exploration of the role of social identity in the experiences and well-being of community volunteers. Eur. J. Soc. Psychol. 2020, 50, 1523–1539. [Google Scholar] [CrossRef]
- McNamara, N.; Stevenson, C.; Muldoon, O.T. Community identity as resource and context: A mixed method investigation of coping and collective action in a disadvantaged community. Eur. J. Soc. Psychol. 2013, 43, 393–403. [Google Scholar] [CrossRef]
- Bankamp, B.; Hickman, C.; Icenogle, J.P.; Rota, P.A. Successes and challenges for preventing measles, mumps and rubella by vaccination. Curr. Opin. Virol. 2019, 34, 110–116. [Google Scholar] [CrossRef]
- Jikal, M.; Riduan, T.; Aarifin, R.; Jeffree, M.S.; Ahmed, K. Cholera outbreak by Sea Gypsies in Sabah, Malaysia: A challenge in North Borneo. Int. J. Infect. Dis. 2019, 83, 83–85. [Google Scholar] [CrossRef]
- Mohd Rosman, M.H.W.; Yong, C.L.; Azman, M.U.; Mohd Ishar, M.I. The Health Issue in Orang Asli Community. Malays. J. Soc. Sci. Humanit. 2020, 5, 36–41. [Google Scholar] [CrossRef]
- Steven, M.C.; Yusof, M.; Ibrahim, H.; Karim, H.A.; Dhanaraj, P.; Mansin, K.A. Barriers and Drivers towards the Use of Childhood Vaccination Services by Undocumented Migrant Caregivers in Sabah, Malaysia: A Qualitative Analysis. World Acad. Sci. Eng. Technol. Int. J. Nurs. Health Sci. 2021, 15, 247–256. Available online: https://publications.waset.org/10012176/barriers-and-drivers-towards-the-use-of-childhood-vaccination-services-by-undocumented-migrant-caregivers-in-sabah-malaysia-a-qualitative-analysis (accessed on 12 May 2023).
- Mat Daud, M.R.H.; Yaacob, N.A.; Ibrahim, M.I.; Wan Muhammad, W.A.R. Five-Year Trend of Measles and Its Associated Factors in Pahang, Malaysia: A Population-Based Study. Int. J. Environ. Res. Public Health 2022, 19, 8017. [Google Scholar] [CrossRef]
- Masresha, B.; Luce, R.; Katsande, R.; Dosseh, A.; Tanifum, P.; Lebo, E.; Byabamazima, C.; Kfutwah, A. The impact of the covid-19 pandemic on measles surveillance in the world health organisation african region, 2020. Pan Afr. Med. J. 2021, 39, 192. [Google Scholar] [CrossRef]
- Minta, A.A.; Ferrari, M.; Antoni, S.; Portnoy, A.; Sbarra, A.; Lambert, B.; Haurisky, S.; Hatcher, C.; Nedelec, Y.; Datta, D.; et al. Progress Toward Regional Measles Elimination—Worldwide, 2000–2021. MMWR Morb. Mortal. Wkly. Rep. 2021, 2022, 71. [Google Scholar] [CrossRef]
- Kim, S.; Headley, T.Y.; Tozan, Y. Universal healthcare coverage and health service delivery before and during the COVID-19 pandemic: A difference-in-difference study of childhood immunization coverage from 195 countries. PLoS Med. 2022, 19, e1004060. [Google Scholar] [CrossRef]
- Qamruddin, A.A.; Malek, A.; Rozali, A.; Wahid, N. Measles in larut, Matang And Selama: Analysis and evaluation of clinical case definitions for 2015–2019. Malays. J. Public Health Med. 2020, 20, 130–140. [Google Scholar] [CrossRef]
- Ariffin, R. A Measles Prevention and Control in Malaysia, Handbook for Healthcare Personnel. Ministry of Health Malaysia, Malaysia. 2006. Available online: https://docplayer.net/21937846-Measles-prevention-control-in-malaysia-handbook-for-healthcare-personnel.html (accessed on 12 May 2023).
- Hustinx, L.; Grubb, A.; Rameder, P.; Shachar, I.Y. Inequality in Volunteering: Building a New Research Front. Voluntas 2022, 33, 1–17. [Google Scholar] [CrossRef]
- Montesanti, S.R.; Abelson, J.; Lavis, J.N.; Dunn, J.R. Enabling the participation of marginalized populations: Case studies from a health service organization in Ontario, Canada. Health Promot. Int. 2017, 32, 636–649. [Google Scholar] [CrossRef]
- Bernama. Three Measles Cases in Sabah Involved Non-Immunised Children. 2019. Available online: https://borneobulletin.com.bn/three-measles-cases-in-sabah-involved-non-immunised-children/ (accessed on 4 May 2023).
- Oriental, W. Ambil alih 5 Skim Penempatan Sementara Pelarian di Sabah, Pindah Pelarian ke Pulau. 2022. Available online: https://wartaoriental.com/2022/10/05/ambil-alih-5-skim-penempatan-sementara-pelarian-di-sabah-pindah-pelarian-ke-pulau-masiung/ (accessed on 4 May 2023).
- Shah, J.M. Squatters and Socio-Economic Survival Strategies in Kota Kinabalu, Sabah. Borneo Res. J. 2010, 4, pp. 91–104. Available online: https://jati.um.edu.my/index.php/BRJ/article/view/9824 (accessed on 12 May 2023).
- Patton, M.Q. Qualitative Research & Evaluation Methods: Integrating Theory and Practice, 4th ed.; Knight, V., Bierach, K., Felts, D.C., Eds.; Sage Publications: Thousand Oaks, CA, USA, 2014; ISBN 978-1-4129. [Google Scholar]
- Saunders, B.; Sim, J.; Kingstone, T.; Baker, S.; Waterfield, J.; Bartlam, B.; Burroughs, H.; Jinks, C. Saturation in qualitative research: Exploring its conceptualization and operationalization. Qual. Quant. 2018, 52, 1893–1907. [Google Scholar] [CrossRef]
- Hagaman, A.K.; Wutich, A. How Many Interviews Are Enough to Identify Metathemes in Multisited and Cross-cultural Research? Another Perspective on Guest, Bunce, and Johnson’s (2006) Landmark Study. Field Methods 2017, 29, 23–41. [Google Scholar] [CrossRef]
- McMahon, S.A.; Winch, P.J. Systematic debriefing after qualitative encounters: An essential analysis step in applied qualitative research. BMJ Glob. Health 2018, 3, e000837. [Google Scholar] [CrossRef] [PubMed]
- Collins, C.S.; Stockton, C.M. The Central Role of Theory in Qualitative Research. Int. J. Qual. Methods 2018, 17, 1–10. [Google Scholar] [CrossRef]
- Hsieh, H.F.; Shannon, S.E. Three approaches to qualitative content analysis. Qual. Health Res. 2005, 15, 1277–1288. [Google Scholar] [CrossRef] [PubMed]
- Jones, C.L.; Jensen, J.D.; Scherr, C.L.; Brown, N.R.; Christy, K.; Weaver, J. The Health Belief Model as an explanatory framework in communication research: Exploring parallel, serial, and moderated mediation. Health Commun. 2015, 30, 566–576. [Google Scholar] [CrossRef] [PubMed]
- Hu, X.; Xiao, S.; Chen, B.; Sa, Z. Gaps in the 2010 measles SIA coverage among migrant children in Beijing: Evidence from a parental survey. Vaccine 2012, 30, 5721–5725. [Google Scholar] [CrossRef] [PubMed]
- Trivedi, R.; Singh, S.; Adhikari, P.; Jatav, D.P. Coverage evaluation of primary immunization and the associated determinants in an urban slum of Rewa. Indian J. Community Health. 2014, 26, pp. 37–40. Available online: https://iapsmupuk.org/journal/index.php/IJCH/article/view/370 (accessed on 12 May 2023).
- Zolotarova, T.; Dussault, C.; Park, H.; Varsaneux, O.; Basta, N.E.; Watson, L.; Robert, P.; Davis, S.; Mercer, M.; Timmerman, S.; et al. Education increases COVID-19 vaccine uptake among people in Canadian federal prisons in a prospective randomized controlled trial: The EDUCATE study. Vaccine 2023, 41, 1419–1425. [Google Scholar] [CrossRef]
- Ogutu, J.O.; Francis, G.M.; Kamau, D.M.; Omondi, M.; Oyugi, E.O.; Ettyang, G.K. Factors Associated with Low Coverage of the Second Dose of Measles Containing Vaccine among Children Aged 19–59 Months, Alego-Usonga Sub-County, Kenya, 2020. JIEPH. 2023, 6, p. 1. Available online: https://www.afenet-journal.net/content/article/6/1/full/ (accessed on 12 May 2023).
- Tang, S.; Liu, X.; Jia, Y.; Chen, H.; Zheng, P.; Fu, H.; Xiao, Q. Education level modifies parental hesitancy about COVID-19 vaccinations for their children. Vaccine 2023, 41, 496–503. [Google Scholar] [CrossRef]
- Amanna, I.J.; Messaoudi, I.; Slifka, M.K. Protective immunity following vaccination: How is it defined? Hum. Vaccines 2008, 4, 316–319. [Google Scholar] [CrossRef]
- ÇAkirli, M.; AÇIkgÖZ, A.; Arslan, D.T. Evaluation of Mothers’ Perspectives on Childhood Vaccination during the COVID-19 Pandemic. Genel Tıp Dergisi 2022, 32, 781–788. [Google Scholar] [CrossRef]
- Larson, H.J.; Gakidou, E.; Murray, C.J.L. The Vaccine-Hesitant Moment. N. Engl. J. Med. 2022, 387, 58–65. [Google Scholar] [CrossRef]
- Paulys, B. Close to the Street: Nursing Practice with People Marginalized by Homelessness and Substance Use; Guirguis-Yonger, M., McNeil, R., Hwang, S.W., Eds.; University of Ottawa Press: Ottawa, ON, Canada, 2014; p. 211. ISBN 978-0-7766-2148-7. [Google Scholar]
- Mohd Azizi, F.S.; Kew, Y.; Moy, F.M. Vaccine hesitancy among parents in a multi-ethnic country, Malaysia. Vaccine 2017, 35, 2955–2961. [Google Scholar] [CrossRef]
- Rumetta, J.; Abdul-Hadi, H.; Lee, Y.K. A qualitative study on parents’ reasons and recommendations for childhood vaccination refusal in Malaysia. J. Infect. Public Health 2020, 13, 199–203. [Google Scholar] [CrossRef]
- Thompson, S.; Meyer, J.C.; Burnett, R.J.; Campbell, S.M. Mitigating Vaccine Hesitancy and Building Trust to Prevent Future Measles Outbreaks in England. Vaccines 2023, 11, 288. [Google Scholar] [CrossRef]
- Khan, S.; Iqbal, J.; Tayyeb, M.; Fahad, S.; Ullah, A.; Khan, H. Prevalence of pneumonia associated with measles among infants and children hospitalized in Khyber Teaching Hospital Peshawar, KPK, Pakistan. Pure Appl. Biol. 2021, 10, 703–712. [Google Scholar] [CrossRef]
- Lim, W.Y.; Amar-Singh, H.S.S.; Jeganathan, N.; Rahmat, H.; Mustafa, N.A.; Mohd Yusof, F.-S.; Rahman, R.; Itam, S.; Chan, C.H.; N-Julia, M.S. Exploring immunisation refusal by parents in the Malaysian context. Cogent Med. 2016, 3, 1142410. [Google Scholar] [CrossRef]
- Bawa, S.; Afolabi, M.; Abdelrahim, K.; Abba, G.; Ningi, A.; Tafida, S.Y.; Tegegne, S.G.; Warigon, C.; Nomhwange, T.; Umar, S.A.; et al. Transboundary nomadic population movement: A potential for import-export of poliovirus. BMC Public Health 2018, 18, 1316. [Google Scholar] [CrossRef]
- Pertet, A.M.; Kaseje, D.; Otieno-Odawa, C.F.; Kirika, L.; Wanjala, C.; Ochieng, J.; Jaoko, M.; Otieno, W.; Odindo, D. Under vaccination of children among Maasai nomadic pastoralists in Kenya: Is the issue geographic mobility, social demographics or missed opportunities? 11 Medical and Health Sciences 1117 Public Health and Health Services. BMC Public Health 2018, 18, 1389. [Google Scholar] [CrossRef]
- Widayanti, A.W.; Norris, P.; Green, J.A.; Heydon, S. Is expanding service through an outreach programme enough to improve immunisation uptake? A qualitative study in Indonesia. Glob. Public Health 2020, 15, 1168–1181. [Google Scholar] [CrossRef]
- Budu, E.; Seidu, A.A.; Armah-Ansah, E.K.; Sambah, F.; Baatiema, L.; Ahinkorah, B.O. Women’s autonomy in healthcare decisionmaking and healthcare seeking behaviour for childhood illness in Ghana: Analysis of data from the 2014 Ghana Demographic and Health Survey. PLoS ONE 2020, 15, e0241488. [Google Scholar] [CrossRef] [PubMed]
- Harvey, H.; Reissland, N.; Mason, J. Parental reminder, recall and educational interventions to improve early childhood immunisation uptake: A systematic review and meta-analysis. Vaccine 2015, 33, 2862–2880. [Google Scholar] [CrossRef] [PubMed]
- Brewer, N.T. What Works to Increase Vaccination Uptake. Acad. Pediatr. 2021, 21, S9–S16. [Google Scholar] [CrossRef] [PubMed]
- Cataldi, J.R.; Kerns, M.E.; O’Leary, S.T. Evidence-based strategies to increase vaccination uptake: A review. Curr. Opin. Pediatr. 2020, 32, 151–159. [Google Scholar] [CrossRef] [PubMed]
- Wu, S.; Su, J.; Yang, P.; Zhang, H.; Li, H.; Chu, Y.; Hua, W.; Li, C.; Tang, Y.; Wang, Q. Factors associated with the uptake of seasonal influenza vaccination in older and younger adults: A large, population-based survey in Beijing, China. BMJ Open 2017, 7, e017459. [Google Scholar] [CrossRef]
- Goldman, R.D.; McGregor, S.; Marneni, S.R.; Katsuta, T.; Griffiths, M.A.; Hall, J.E.; Seiler, M.; Klein, E.J.; Cotanda, C.P.; Gelernter, R.; et al. Willingness to Vaccinate Children against Influenza after the Coronavirus Disease 2019 Pandemic. J. Pediatr. 2021, 228, 87–93. [Google Scholar] [CrossRef]
- Smith, L.E.; Amlôt, R.; Weinman, J.; Yiend, J.; Rubin, G.J. A systematic review of factors affecting vaccine uptake in young children. Vaccine 2017, 35, 6059–6069. [Google Scholar] [CrossRef]
- Li, J.B.; Lau, E.Y.H.; Chan, D.K.C. Why do Hong Kong parents have low intention to vaccinate their children against COVID-19? testing health belief model and theory of planned behavior in a large-scale survey. Vaccine 2022, 40, 2772–2780. [Google Scholar] [CrossRef]
- Xiao, Q.; Liu, X.; Wang, R.; Mao, Y.; Chen, H.; Li, X.; Liu, X.; Dai, J.; Gao, J.; Fu, H.; et al. Predictors of willingness to receive the COVID-19 vaccine after emergency use authorization: The role of coping appraisal. Vaccines 2021, 9, 967. [Google Scholar] [CrossRef]
- Lin, C.; Tu, P.; Beitsch, L.M. Confidence and receptivity for COVID-19 vaccines: A rapid systematic review. Vaccines 2021, 9, 16. [Google Scholar] [CrossRef]
- Kalra, S.; Kalra, D.; Grafova, I.; Rubin, J.S.; Monheit, A.; Cantor, J.; Duberstein, P.; Bhuyan, S.S. Association of death or illness from COVID-19 among family and friends on vaccine uptake within four months of the Emergency Use Authorization. Findings from a national survey in the United States. Vaccine 2023, 41, 1911–1915. [Google Scholar] [CrossRef]
- Wilson, R.F.; Kota, K.K.; Sheats, K.J.; Luna-pinto, C.; Owens, C.; Harrison, D.D.; Razi, S. Call out racism and inequity in reports on vaccine intentions. Nat. Hum. Behav. 2023, 7, 300–302. [Google Scholar] [CrossRef]
- Moyer-Gusé, E.; Robinson, M.J.; McKnight, J. The Role of Humor in Messaging about the MMR Vaccine. J. Health Commun. 2018, 23, 514–522. [Google Scholar] [CrossRef]
| Behavioural Theory | Construct | Brief Definition |
|---|---|---|
| Health Belief Model | Perceived susceptibility | Beliefs about the likelihood of a child contracting measles. |
| Perceived severity | Beliefs about the severity of the consequences of a child contracting measles. | |
| Perceived benefits | Beliefs about the efficacy of measles vaccination, as well as community volunteers to help reduce the risk and severity of the problem. | |
| Perceived barriers to action | Beliefs on the financial and emotional costs of receiving the measles vaccine, as well as the need for community volunteers to help with the programme. | |
| Cues to action | Strategies to increase a person’s willingness to act to lower the chance of a child contracting measles. | |
| Self-efficacy | The belief that one can take measures and overcome obstacles to prevent the spread of measles among children. |
| Characteristics | n | % | |
|---|---|---|---|
| Gender | Male | 0 | 0 |
| Female | 40 | 100 | |
| Caregiver Status | Parent | 38 | 95 |
| Caregiver | 2 | 5 | |
| Age Range | 17–24 years | 13 | 33 |
| 25–34 years | 18 | 45 | |
| 35–44 years | 8 | 20 | |
| 45–64 years | 1 | 3 | |
| Educational level | High school | 10 | 25 |
| Primary school | 17 | 43 | |
| No schooling | 13 | 33 | |
| Occupation | None | 40 | 100 |
| History of Children Measles Immunisation Status | Complete | 30 | 75 |
| Incomplete | 2 | 5 | |
| Nil | 4 | 10 | |
| Not yet | 4 | 10 | |
| Village | Pulau Gaya | 21 | 52 |
| Skim Penempatan | 19 | 48 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Salleh, H.; Avoi, R.; Abdul Karim, H.; Osman, S.; Dhanaraj, P.; Ab Rahman, M.A.‘I. A Behavioural-Theory-Based Qualitative Study of the Beliefs and Perceptions of Marginalised Populations towards Community Volunteering to Increase Measles Immunisation Coverage in Sabah, Malaysia. Vaccines 2023, 11, 1056. https://doi.org/10.3390/vaccines11061056
Salleh H, Avoi R, Abdul Karim H, Osman S, Dhanaraj P, Ab Rahman MA‘I. A Behavioural-Theory-Based Qualitative Study of the Beliefs and Perceptions of Marginalised Populations towards Community Volunteering to Increase Measles Immunisation Coverage in Sabah, Malaysia. Vaccines. 2023; 11(6):1056. https://doi.org/10.3390/vaccines11061056
Chicago/Turabian StyleSalleh, Hazeqa, Richard Avoi, Haryati Abdul Karim, Suhaila Osman, Prabakaran Dhanaraj, and Mohd Ali ‘Imran Ab Rahman. 2023. "A Behavioural-Theory-Based Qualitative Study of the Beliefs and Perceptions of Marginalised Populations towards Community Volunteering to Increase Measles Immunisation Coverage in Sabah, Malaysia" Vaccines 11, no. 6: 1056. https://doi.org/10.3390/vaccines11061056
APA StyleSalleh, H., Avoi, R., Abdul Karim, H., Osman, S., Dhanaraj, P., & Ab Rahman, M. A. ‘I. (2023). A Behavioural-Theory-Based Qualitative Study of the Beliefs and Perceptions of Marginalised Populations towards Community Volunteering to Increase Measles Immunisation Coverage in Sabah, Malaysia. Vaccines, 11(6), 1056. https://doi.org/10.3390/vaccines11061056







