The Psychology of COVID-19 Booster Hesitancy, Acceptance and Resistance in Australia
Abstract
1. Introduction
1.1. Background and Context of COVID-19 Vaccinations in Australia
1.2. Vaccine Intentions
1.3. Factors Associated with COVID-19 Vaccine and Booster Hesitancy
1.3.1. Sociodemographics
1.3.2. Beliefs and Attitudes about COVID-19
1.3.3. Information Consumption, Perceived Health Literacy and Related Factors
1.3.4. Psychological Characteristics
1.3.5. Political, Cultural and Social Attitudes
1.4. The Present Study
Aims and Hypotheses
2. Materials and Methods
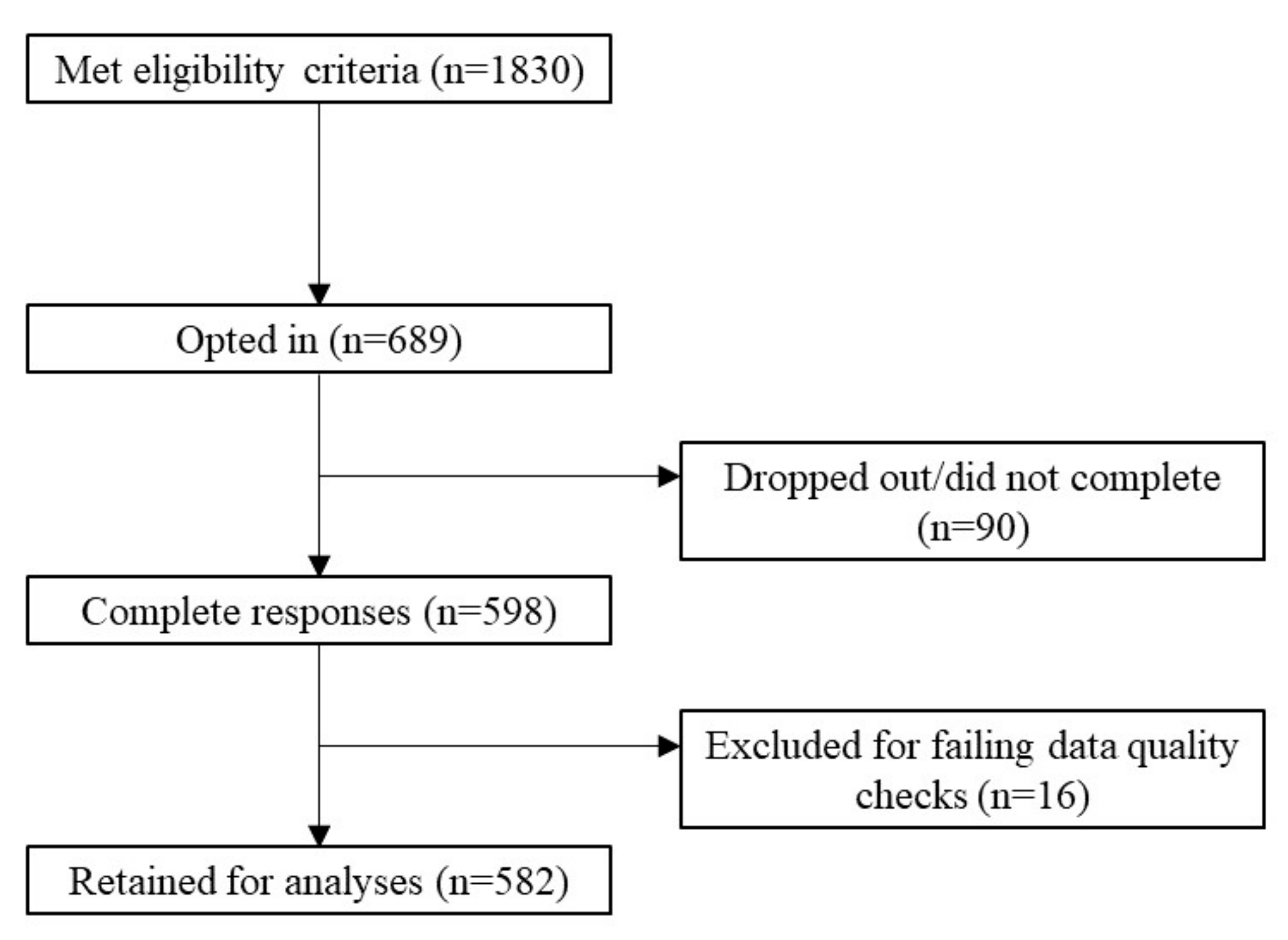
2.1. Participants and Recruitment
2.2. Measures
| Measure (Authors) | Number of Items and Response Scale | Scoring | Dimensions and Example Items | Internal Consistency (Previous Studies) |
|---|---|---|---|---|
| Demographics | ||||
| Financial comfort | 1 item Sliding scale from 0 (not at all comfortable) to 100 (very comfortable) | 0–100 | ‘How would you rate your level of financial comfort currently?’ | - |
| Education level | 1 item 1 = year 11 or below 2 = year 12 3 = trade certificate/apprenticeship 4 = diploma 5 = bachelor’s degree 6 = higher degree | 1–6 | “What is the highest level of education you have completed?’ | - |
| COVID-related variables | ||||
| Vaccination status | 1 item 0 = no doses 1 = one dose only 2 = two doses only [or three doses as primary course if immunocompromised] 3 = primary course and booster | 0–3 | ‘Have you received a COVID-19 vaccination?’ | - |
| Booster willingness | 1 item 1 = definitely not 2 = probably not 3 = unsure 4 = probably 5 = definitely 6 = have already had booster | 1–6 Higher = more willing | ‘When a COVID-19 vaccine booster is available to you to boost your protection against COVID-19, will you get it?’ | - |
| COVID-19 Beliefs (study specific, see Supplementary Materials) | 24 items (1) strongly disagree to (5) strongly agree | Factor scores (Bartlett Method) Higher = greater endorsement |
| - |
| Vaccination Attitudes Examination Scale (modified) [68] | 13 items (1) strongly disagree to (6) strongly agree | Mean scores Higher = less support for vaccinations |
| 0.80 to 0.93 [68] |
| Multidimensional COVID-19 Worry Index (study specific, see Supplementary Materials) | 19 items (1) never to (4) always | Mean scores Higher = more worried |
| - |
| COVID-19 Readiness for Lockdown (study-specific, see Supplementary Materials) | 7 items (1) strongly disagree to (5) strongly agree | Mean score Higher = more ready | ‘Should another lockdown be needed, I will follow the rules’ | - |
| Compliance Attitudes (study specific, see Supplementary Materials) | 5 items, repeated for two time periods: currently and before December 2021 Slider scale from (0) does not apply at all to (100) applies very much | Mean score Higher = more compliant with and understanding of rules/recommendations | ‘I adhere to the current COVID-19 rules or recommendations’ | - |
| Reasons for getting vaccinations (study specific, see Supplementary Materials) | 10 items, repeated for primary vaccination (for those who had received at least two doses), and booster (either relating to reasons one got a booster for those who had received a booster dose, or why one would receive a booster if not yet done so) (1) strongly disagree to (6) strongly agree | Mean scores Higher = greater endorsement of reason |
| - |
| Pandemic Fatigue Scale [32] and Neglect from the Brief Pandemic Fatigue Scale [69] (The Boredom subscale from the Brief Pandemic Fatigue Scale was not included due to its substantial overlap with the Informational Fatigue subscale.) | 9 items (1) strongly disagree to (7) strongly agree | Overall mean score (an exploratory factor analysis was run on the items. All items converged and loaded on a single factor; thus, an overall mean score was calculated based on these results.) Higher = more fatigued | Pandemic Fatigue Scale:
Brief Pandemic Fatigue Scale:
| 0.83 to 0.86 [32] 0.85 [69] |
| Trust (study specific see Supplementary Materials) | 15 items (1) strongly distrust to (5) strongly trust | Mean scores Higher = greater trust |
| - |
| OCEANS Coronavirus Conspiracy Scale [62] | 7 items (1) do not agree to (5) agree completely | Mean score Higher = greater belief in conspiracies | ‘The virus is a hoax’ | 0.94 [62] |
| Information Sources (study-specific, see Supplementary Materials) | 10 items (1) never to (5) all of the time | Mean scores Higher = more frequent use of sources |
| - |
| Check News | 1 item (1) never to (5) all of the time | Higher = more frequent | ‘How often do you check the news regarding COVID-19?’ | - |
| Source Check | 1 item (1) never to (5) all of the time | Higher = more frequent | ‘How often do you check the legitimacy of the source of information about COVID-19?’ | - |
| Share News | 1 item (1) never to (5) all of the time | Higher = more frequent | ‘How often do you share news about COVID-19 with family/friends?’ | - |
| Psychological Variables | ||||
| All Aspects of Health Literacy Scale [70] | 13 items | Overall summed score Higher = better health literacy |
| 0.75 [70] |
| Mini International Personality Item Pool [71] | 20 items (1) very inaccurate to (5) very accurate | Summed scores Higher = higher on trait | Extraversion: ‘I am the life of the party’ Agreeableness: ‘I sympathize with others’ feelings’ Conscientiousness: ‘I get chores done right away’ Neuroticism: ‘I have frequent mood swings’ Intellect/Openness: ‘I have a vivid imagination’ | 0.65 to 0.82 [71] |
| Esoteric Analogies Test [72] | 14 items | 0–100% | ‘FLAME is to HEAT as ROSE is to: (a) LEAVES; (b) SCENT; (c) THORN or (d) PETAL’ | 0.64 and 0.76 [73,74] |
| Cognitive Reflection Test [75] | 4 items | 0–100% | ‘Jerry received both the 15th highest and the 15th lowest mark in the class. How many students are in the class?’ | 0.72 [75] |
| Connor-Davidson Resilience Scale Short [76] | 10 items (0) not true at all to (4) nearly always true | Summed score Higher = more resilient | ‘I can deal with whatever comes’ | 0.85 [76] |
| Intolerance of Uncertainty Scal [56] | 12 items (1) not at all characteristic of me to (4) entirely characteristic of me | Summed score Higher = greater intolerance | ‘Unforeseen events upset me greatly’ | 0.91 [56] |
| Bullshit Receptivity Scale [42] | 10 items (1) not at all profound to (5) very profound | Mean score Higher = more receptive to pseudo-profound statements | ‘Hidden meaning transforms unparalleled abstract beauty’ | 0.82 to 0.96 [42] |
| Hong Psychological Reactance Scale [77] | 14 items (1) strongly disagree to (6) strongly agree | Mean score Higher = more reactance | ‘Regulations trigger a sense of resistance in me’ | 0.75 to 0.80 [78] |
| Political, Cultural, Social Attitudes | ||||
| Social Conservatism Scale [79] | 3 items were selected from the 12-item scale. (1) fully disagree to (5) fully agree | Mean score Higher = more conservative | ‘We have to respect our history and tradition’ | 0.55 [37] |
| Conspiracy Mentality Questionnaire [80] | 13 items (1) strongly disagree to (7) strongly agree | Mean score Higher = greater conspiracy mindset | ‘There are many very important things happening in the world about which the public are not informed’ | 0.84 [81] |
| Persecution from the Persecution and Deservedness Scale [81] | 10 items (10) certainly false to (5) certainly true | Mean score Higher = greater persecutory thinking | ‘There are times when I worry that others may be plotting against me’ | 0.84 [81] |
| Need for Chaos [82] | 7 items (1) strongly disagree to (7) strongly agree | Mean score Higher = greater need for chaos | ‘I get a kick when natural disasters strike in foreign countries’ | 0.90 [82] |
| Cultural Tightness–Looseness [64] | 6 items (1) strongly disagree to (6) strongly agree | Mean score Higher = perceive culture as tighter | ‘There are many social norms that people are supposed to abide by in this country’ | 0.85 [64] |
| Amoral Social Attitudes [83] | 6 items (1) fully disagree to (5) fully agree. | Mean score Higher = greater amorality | ‘I hate obligations and responsibilities of any kind’ | 0.64 [35] |
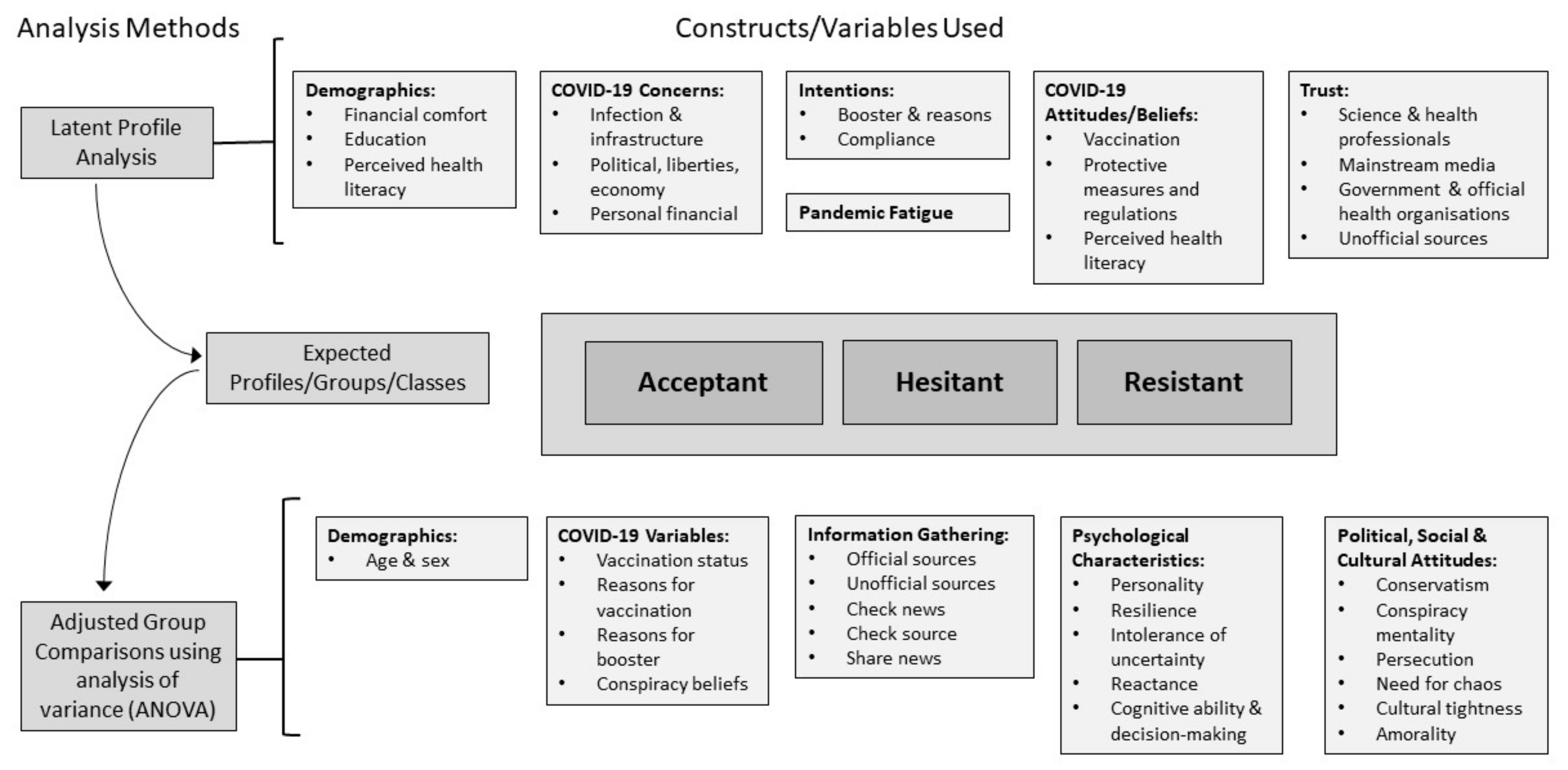
2.3. Statistical Analyses
3. Results
3.1. Sample Characteristics
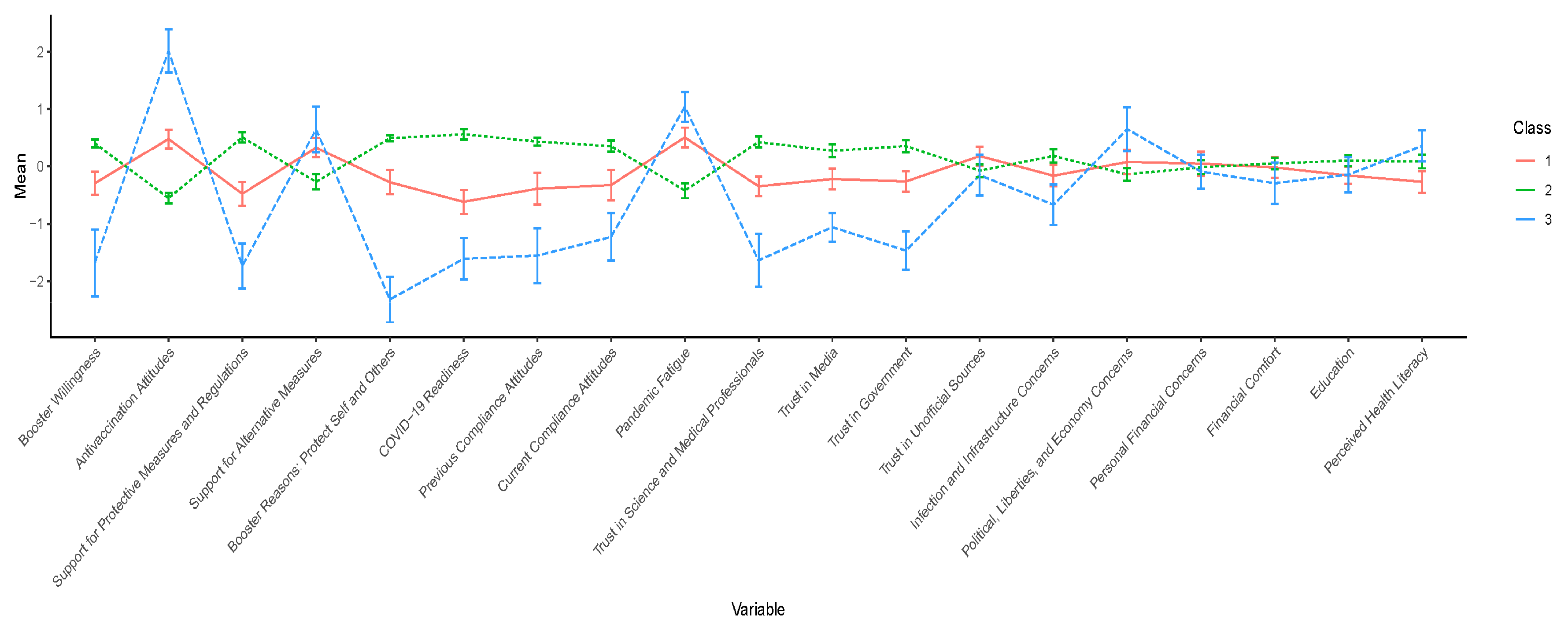
3.2. Profile Selection
3.3. Interpretation of the Three-Class Solution
3.4. Profile Differences in Demographics and COVID-19 Variables
3.4.1. Demographics
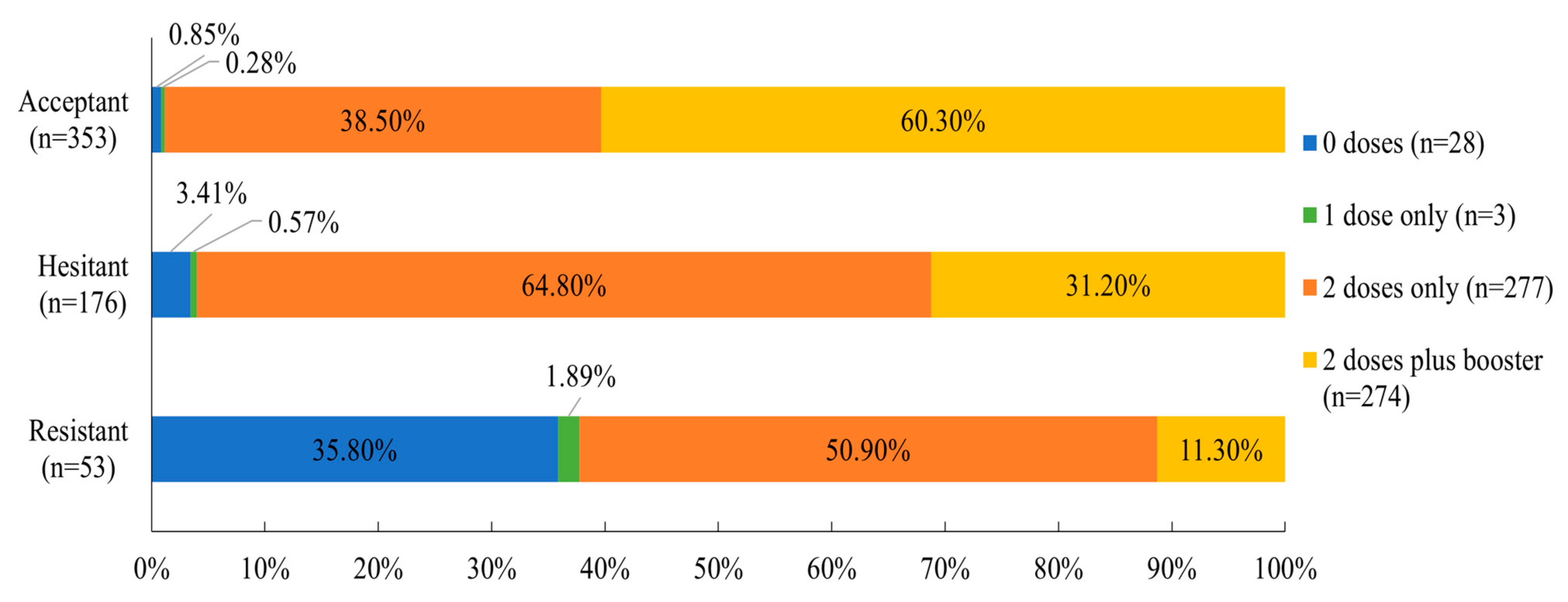
3.4.2. COVID-19 Variables: Vaccination and COVID-19 Conspiracy Beliefs
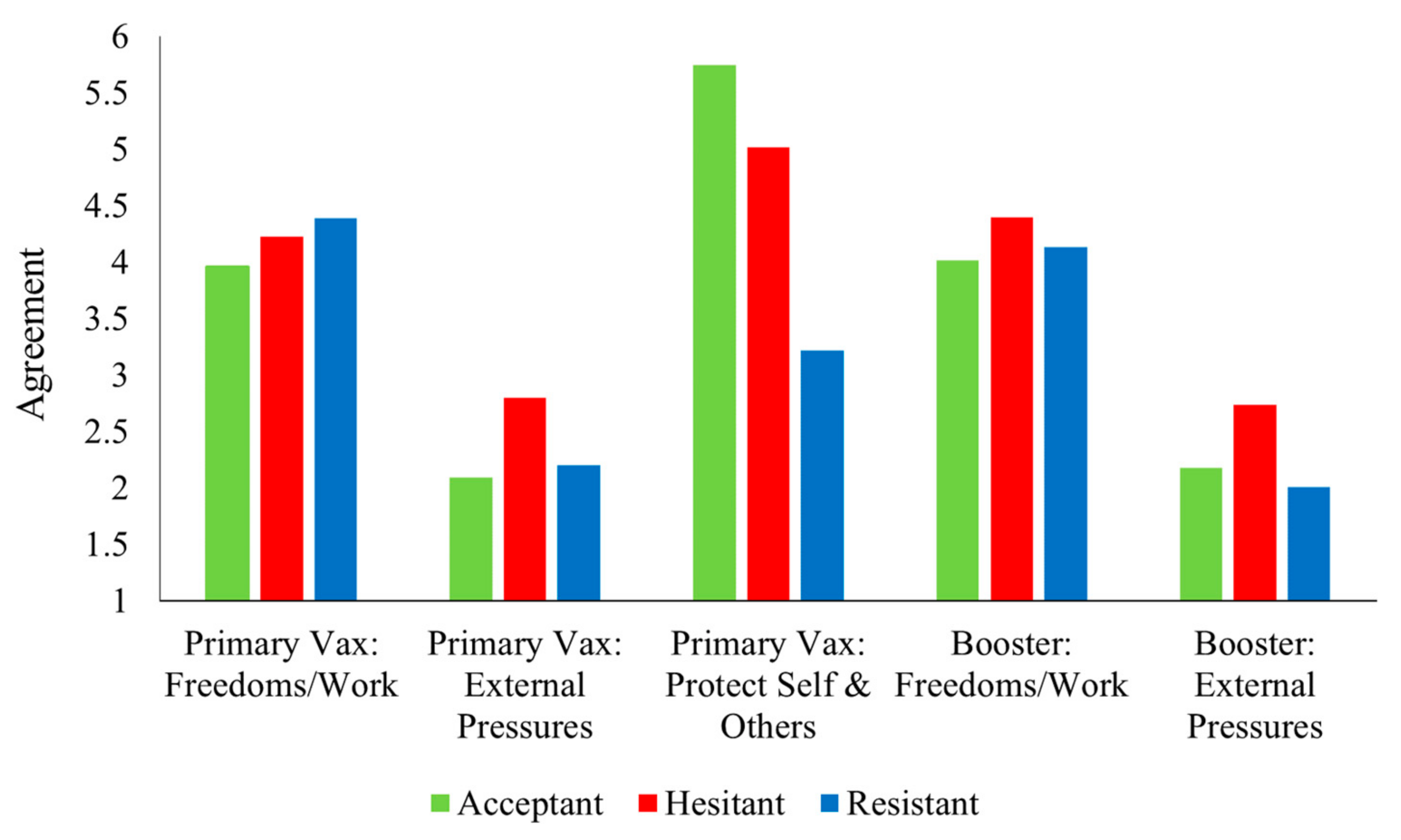
3.4.3. Reasons for Getting Primary and Booster Vaccinations
3.5. Profile Differences in Information Gathering
3.6. Profile Differences in Psychological Measures
3.6.1. Psychological Characteristics and Cognitive Ability
3.6.2. Political, Cultural and Social Attitudes
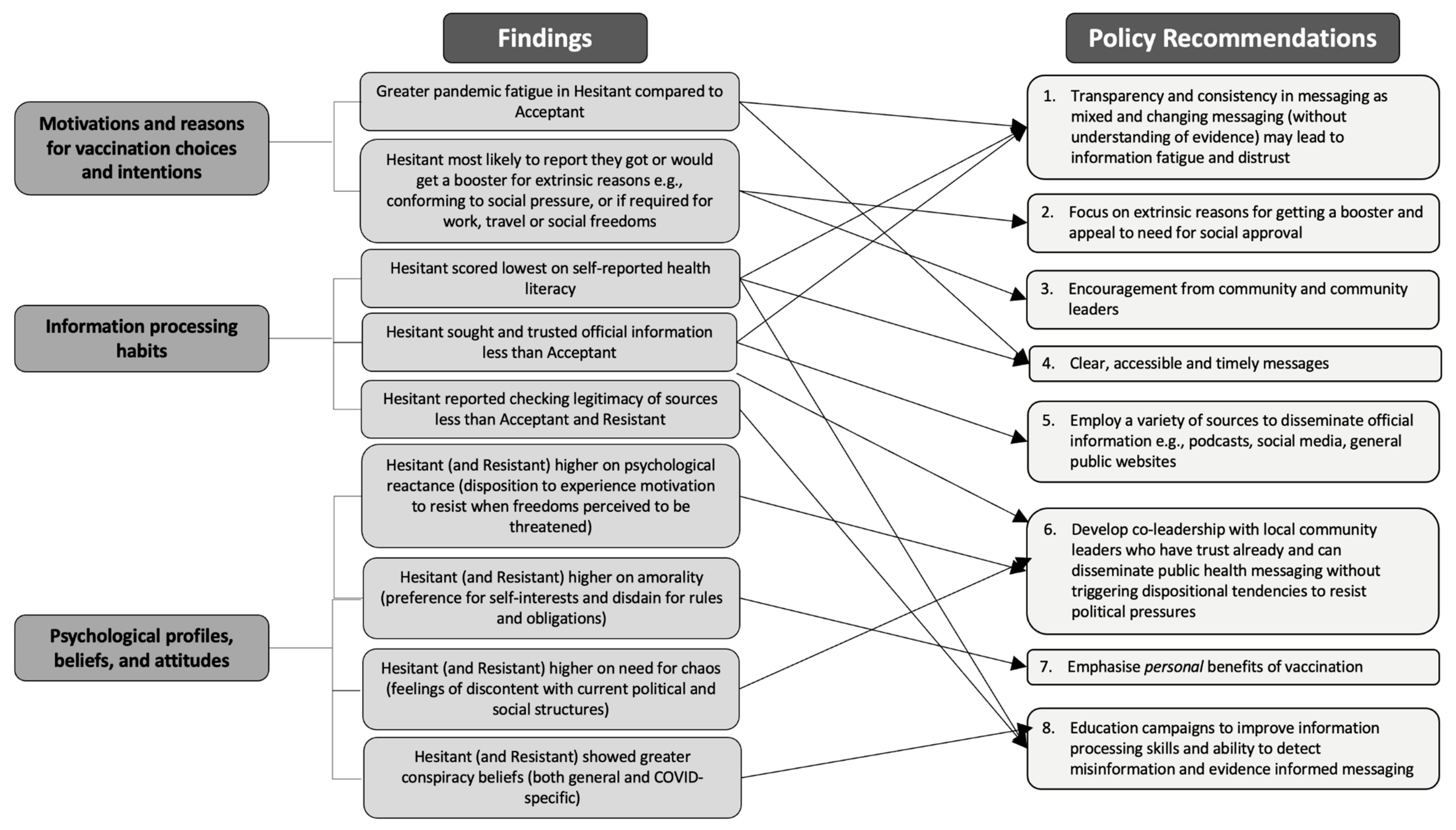
4. Discussion
4.1. Differences in Demographics and COVID-Related Attitudes
4.2. Motivations behind Willingness to Get Vaccinated
4.3. Differences in Perceptions of Health Literacy
4.4. Differences in COVID-19 Information Gathering
4.4.1. Use of Official and Unofficial Information Sources
4.4.2. Trust in Information Sources
4.5. The Psychological Profiles of the Vaccine-Hesitant and -Resistant Groups
4.6. Implications
4.7. Limitations and Future Directions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Global COVID-19 Vaccination Strategy in a Changing World. Available online: https://www.who.int/publications/m/item/global-covid-19-vaccination-strategy-in-a-changing-world--july-2022-update (accessed on 22 July 2022).
- World Health Organization. WHO Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int/ (accessed on 14 April 2023).
- Bennett, N.G.; Bloom, D.E.; Ferranna, M. Factors underlying COVID-19 vaccine and booster hesitancy and refusal, and incentivizing vaccine adoption. PLoS ONE 2022, 17, e0274529. [Google Scholar] [CrossRef] [PubMed]
- Cristea, D.; Ilie, D.-G.; Constantinescu, C.; Fîrțală, V. Acceptance, Hesitancy, and Refusal in Anti-COVID-19 Vaccination: A Cluster Analysis Aiming at the Typology behind These Three Concepts. Vaccines 2022, 10, 1496. [Google Scholar] [CrossRef] [PubMed]
- Murphy, J.; Vallières, F.; Bentall, R.P.; Shevlin, M.; McBride, O.; Hartman, T.K.; McKay, R.; Bennett, K.; Mason, L.; Gibson-Miller, J.; et al. Psychological characteristics associated with COVID-19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nat. Commun. 2021, 12, 29. [Google Scholar] [CrossRef]
- Moffitt, T.E.; Caspi, A.; Ambler, A.; Bourassa, K.; Harrington, H.; Hogan, S.; Houts, R.; Ramrakha, S.; Wood, S.L.; Poulton, R. Deep-seated psychological histories of COVID-19 vaccine hesitance and resistance. PNAS Nexus 2022, 1, 34. [Google Scholar] [CrossRef] [PubMed]
- Singh, P.; Dhalaria, P.; Kashyap, S.; Soni, G.K.; Nandi, P.; Ghosh, S.; Mohapatra, M.K.; Rastogi, A.; Prakash, D. Strategies to overcome vaccine hesitancy: A systematic review. Syst. Rev. 2022, 11, 78. [Google Scholar] [CrossRef]
- Basseal, J.M.; Bennett, C.M.; Collignon, P.; Currie, B.J.; Durrheim, D.N.; Leask, J.; McBryde, E.S.; McIntyre, P.; Russell, F.M.; Smith, D.W.; et al. Key lessons from the COVID-19 public health response in Australia. Lancet Reg. Health—West. Pac. 2022, 30, 100616. [Google Scholar] [CrossRef] [PubMed]
- Mathieu, E.; Ritchie, H.; Rodes-Guirao, L.; Appel, C.; Gavrilov, D.; Giattino, C.; Hasell, J.; Macdonald, B.; Dattani, S.; Beltekian, D.; et al. Coronavirus (COVID-19) Deaths. 2020. Available online: https://ourworldindata.org/covid-deaths (accessed on 13 March 2023).
- Australian Government Department of Health. COVID-19 Vaccine Rollout Update—30 June 2021. Available online: https://www.health.gov.au/resources/publications/covid-19-vaccine-rollout-update-30-june-2021?language=en (accessed on 10 August 2022).
- Nicholas, J. How Australia’s Coronavirus Vaccine Rollout Really Compares with Other Countries. Available online: https://www.theguardian.com/news/datablog/2021/apr/2014/how-australias-coronavirus-vaccine-rollout-really-compares-with-other-countries (accessed on 19 April 2023).
- Australian Government Department of Health. COVID-19 Vaccine Rollout Update—17 December 2021. Available online: https://www.health.gov.au/resources/publications/covid-19-vaccine-rollout-update-17-december-2021 (accessed on 12 October 2022).
- Australian Government Department of Health. Coronavirus (COVID-19) at a Glance. 2022. Available online: https://www.health.gov.au/resources/publications/coronavirus-covid-19-at-a-glance-10-january-2022?language=en (accessed on 15 December 2022).
- Timms, P.; Lloyd, M. COVID-19 Testing under Pressure across Australia, as Rapid Antigen Tests Remain Hard to Find Amid Long Delays for PCRs. Available online: https://www.abc.net.au/news/2022-01-05/covid-testing-pcr-delays-rat-test-supply-issues/100738982 (accessed on 15 December 2022).
- Talbot, J. We Are Not Going Back to Shutting Down Peoples’ Lives’ Says the Prime Minister amid Record COVID-19 Cases across Australia. Available online: https://www.skynews.com.au/australia-news/coronavirus/we-are-not-going-back-to-shutting-down-peoples-lives-says-the-prime-minister-amid-record-covid19-cases-across-australia/news-story/16c17b55522e55582b55512df047283b047289b047283a047286c047286f (accessed on 2 September 2022).
- Australian Medical Association. Australia Must Move Quickly to Speed Up COVID-19 Booster Program. 2021. Available online: https://www.ama.com.au/articles/australia-must-move-quickly-speed-covid-19-booster-program (accessed on 2 September 2022).
- Liu, B.; Gidding, H.; Stepien, S.; Cretikos, M.; Macartney, K. Relative effectiveness of COVID-19 vaccination with 3 compared to 2 doses against SARS-CoV-2 B.1.1.529 (Omicron) among an Australian population with low prior rates of SARS-CoV-2 infection. Lancet 2022, 40, 6288–6294. [Google Scholar]
- Office for National Statistics. Self-Reported Long COVID after Infection with the Omicron Variant in the UK: 6 May 2022. Available online: https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/selfreportedlongcovidafterinfectionwiththeomicronvariant/6may2022 (accessed on 2 September 2022).
- Shen, S.C.; Dubey, V. Addressing vaccine hesitancy: Clinical guidance for primary care physicians working with parents. Can. Fam. Physician 2019, 65, 175–181. [Google Scholar]
- Leask, J. Target the fence-sitters. Nature 2011, 473, 443–445. [Google Scholar] [CrossRef]
- Biddle, N.; Sollis, K. Who Wants to Get Boosted? COVID-19 Vaccine Uptake in Australia in January 2022; ANU Centre for Social Research and Methods: Canberra, Australia, 2022. [Google Scholar]
- Nicholas, J. Australia Won’t Reach 80% Covid Booster Rate until Well into 2022, Analysis Shows. Available online: https://www.theguardian.com/australia-news/2021/dec/2019/australia-wont-reach-2080-covid-booster-rate-until-well-into-2022-analysis-shows (accessed on 10 August 2022).
- Hagger, M.S.; Hamilton, K. Predicting COVID-19 booster vaccine intentions. Appl. Psychol. Health Well-Being 2022, 14, 819–841. [Google Scholar] [CrossRef]
- Klugar, M.; Riad, A.; Mohanan, L.; Pokorná, A. COVID-19 Vaccine Booster Hesitancy (VBH) of Healthcare Workers in Czechia: National Cross-Sectional Study. Vaccines 2021, 9, 1437. [Google Scholar] [CrossRef] [PubMed]
- Paul, E.; Fancourt, D. Predictors of uncertainty and unwillingness to receive the COVID-19 booster vaccine: An observational study of 22,139 fully vaccinated adults in the UK. Lancet Reg. Health Eur. 2022, 14, 100317. [Google Scholar] [CrossRef] [PubMed]
- Tan, K.Y.K.; Soh, A.S.E.; Ong, B.W.L.; Chen, M.I.; Griva, K. Determining the Prevalence and Correlates of COVID-19 Booster Vaccine Hesitancy in the Singapore Population Following the Completion of the Primary Vaccination Series. Vaccines 2022, 10, 1088. [Google Scholar] [CrossRef] [PubMed]
- Yadete, T.; Batra, K.; Netski, D.M.; Antonio, S.; Patros, M.J.; Bester, J.C. Assessing Acceptability of COVID-19 Vaccine Booster Dose among Adult Americans: A Cross-Sectional Study. Vaccines 2021, 9, 1424. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, M.; Kobashi, Y.; Kawamura, T.; Shimazu, Y.; Nishikawa, Y.; Omata, F.; Zhao, T.; Yamamoto, C.; Kaneko, Y.; Nakayama, A.; et al. Factors Associated with COVID-19 Vaccine Booster Hesitancy: A Retrospective Cohort Study, Fukushima Vaccination Community Survey. Vaccines 2022, 10, 515. [Google Scholar] [CrossRef]
- Roberts, H.A.; Clark, D.A.; Kalina, C.; Sherman, C.; Brislin, S.; Heitzeg, M.M.; Hicks, B.M. To vax or not to vax: Predictors of anti-vax attitudes and COVID-19 vaccine hesitancy prior to widespread vaccine availability. PLoS ONE 2022, 17, e0264019. [Google Scholar] [CrossRef] [PubMed]
- Lazarus, J.V.; Ratzan, S.C.; Palayew, A.; Gostin, L.O.; Larson, H.J.; Rabin, K.; Kimball, S.; El-Mohandes, A. A global survey of potential acceptance of a COVID-19 vaccine. Nat. Med. 2021, 27, 225–228. [Google Scholar] [CrossRef]
- World Health Organization. Pandemic Fatigue: Reinvigorating the Public to Prevent COVID-19. Available online: https://apps.who.int/iris/handle/10665/335820 (accessed on 13 October 2022).
- Lilleholt, L.; Zettler, I.; Betsch, C.; Böhm, R. Pandemic fatigue: Measurement, correlates, and consequences. PsyArXiv 2020. [Google Scholar] [CrossRef]
- Bodas, M.; Kaim, A.; Velan, B.; Ziv, A.; Jaffe, E.; Adini, B. Overcoming the effect of pandemic fatigue on vaccine hesitancy-Will belief in science triumph? J. Nurs. Sch. 2022, 55, 262–271. [Google Scholar] [CrossRef]
- Wong, L.P.; Alias, H.; Siaw, Y.-L.; Muslimin, M.; Lai, L.L.; Lin, Y.; Hu, Z. Intention to receive a COVID-19 vaccine booster dose and associated factors in Malaysia. Hum. Vaccines Immunother. 2022, 18, 2078634. [Google Scholar] [CrossRef]
- Kleitman, S.; Fullerton, D.J.; Zhang, L.M.; Blanchard, M.D.; Lee, J.; Stankov, L.; Thompson, V. To comply or not comply? A latent profile analysis of behaviours and attitudes during the COVID-19 pandemic. PLoS ONE 2021, 16, e0255268. [Google Scholar] [CrossRef] [PubMed]
- Loomba, S.; de Figueiredo, A.; Piatek, S.J.; de Graaf, K.; Larson, H.J. Measuring the impact of COVID-19 vaccine misinformation on vaccination intent in the UK and USA. Nat. Hum. Behav. 2021, 5, 337–348. [Google Scholar] [CrossRef] [PubMed]
- Allen, K.; Lambert, S.B.; Yuen, A.; Pourmarzi, D. Factors associated with COVID-19 booster vaccine willingness among migrants from the Eastern Mediterranean living in Australia: A cross-sectional study. Res. Sq. 2022, 22, 2205. [Google Scholar] [CrossRef] [PubMed]
- Ratzan, S.C.; Parker, R.M. Introduction. In National Library of Medicine Current Bibliographies in Medicine: Health Literacy; Seldon, C.R., Zorn, M., Ratzan, S.C., Parker, R.M., Eds.; National Institutes of Health, U.S. Department of Health and Human Services: Bethesda, MD, USA, 2000. [Google Scholar]
- Kricorian, K.; Civen, R.; Equils, O. COVID-19 vaccine hesitancy: Misinformation and perceptions of vaccine safety. Hum. Vaccines Immunother. 2022, 18, 1950504. [Google Scholar] [CrossRef] [PubMed]
- Montagni, I.; Ouazzani-Touhami, K.; Mebarki, A.; Texier, N.; Schück, S.; Tzourio, C. Acceptance of a COVID-19 vaccine is associated with ability to detect fake news and health literacy. J. Public Health 2021, 43, 695–702. [Google Scholar] [CrossRef]
- Zhang, H.; Li, Y.; Peng, S.; Jiang, Y.; Jin, H.; Zhang, F. The effect of health literacy on COVID-19 vaccine hesitancy among community population in China: The moderating role of stress. Vaccine 2022, 40, 4473–4478. [Google Scholar] [CrossRef] [PubMed]
- Pennycook, G.; Cheyne, J.A.; Barr, N.; Koehler, D.J.; Fugelsang, J.A. On the reception and detection of pseudo-profound bullshit. Judgm. Decis.-Mak. 2015, 10, 549–563. [Google Scholar] [CrossRef]
- Roshchina, Y.; Roshchin, S.; Rozhkova, K. Determinants of COVID-19 vaccine hesitancy and resistance in Russia. Vaccine 2022, 40, 5739–5747. [Google Scholar] [CrossRef]
- Salerno, L.; Craxì, L.; Amodio, E.; Lo Coco, G. Factors Affecting Hesitancy to mRNA and Viral Vector COVID-19 Vaccines among College Students in Italy. Vaccines 2021, 9, 927. [Google Scholar] [CrossRef]
- Frederick, S. Cognitive Reflection and Decision Making. J. Econ. Perspect. 2005, 19, 25–42. [Google Scholar] [CrossRef]
- Sinayev, A.; Peters, E. Cognitive reflection vs. calculation in decision making. Front. Psychol. 2015, 6, 532. [Google Scholar] [CrossRef]
- Campitelli, G.; Gerrans, P. Does the cognitive reflection test measure cognitive reflection? A mathematical modeling approach. Mem. Cogn. 2014, 42, 434–447. [Google Scholar] [CrossRef]
- Halstead, I.N.; McKay, R.T.; Lewis, G.J. COVID-19 and seasonal flu vaccination hesitancy: Links to personality and general intelligence in a large, UK cohort. Vaccine 2022, 40, 4488–4495. [Google Scholar] [CrossRef]
- Cattell, R.B. Theory of fluid and crystallized intelligence: A critical experiment. J. Educ. Psychol. 1963, 54, 1–22. [Google Scholar] [CrossRef]
- Steindl, C.; Jonas, E.; Sittenthaler, S.; Traut-Mattausch, E.; Greenberg, J. Understanding Psychological Reactance: New Developments and Findings. Z. Psychol. 2015, 223, 205–214. [Google Scholar] [CrossRef] [PubMed]
- Hornsey, M.J.; Harris, E.A.; Fielding, K.S. The psychological roots of anti-vaccination attitudes: A 24-nation investigation. Health Psychol. 2018, 37, 307–315. [Google Scholar] [CrossRef] [PubMed]
- Sprengholz, P.; Betsch, C.; Böhm, R. Reactance revisited: Consequences of mandatory and scarce vaccination in the case of COVID-19. Appl. Psychol. Health Well-Being 2021, 13, 986–995. [Google Scholar] [CrossRef] [PubMed]
- Sprengholz, P.; Felgendreff, L.; Böhm, R.; Betsch, C. Vaccination policy reactance: Predictors, consequences, and countermeasures. J. Health Psychol. 2022, 27, 1394–1407. [Google Scholar] [CrossRef] [PubMed]
- Albarracin, D.; Jung, H.; Song, W.; Tan, A.; Fishman, J. Rather than inducing psychological reactance, requiring vaccination strengthens intentions to vaccinate in US populations. Sci. Rep. 2021, 11, 20796. [Google Scholar] [CrossRef] [PubMed]
- Christou-Ergos, M.; Wiley, K.E.; Leask, J. Willingness to receive a vaccine is influenced by adverse events following immunisation experienced by others. Vaccine 2023, 41, 246–250. [Google Scholar] [CrossRef]
- Carleton, R.N.; Norton, M.A.; Asmundson, G.J. Fearing the unknown: A short version of the Intolerance of Uncertainty Scale. J. Anxiety Disord. 2007, 21, 105–117. [Google Scholar] [CrossRef]
- McNeil, A.; Purdon, C. Anxiety disorders, COVID-19 fear, and vaccine hesitancy. J. Anxiety Disord. 2022, 90, 102598. [Google Scholar] [CrossRef] [PubMed]
- Zheng, Y.-B.; Sun, J.; Liu, L.; Zhao, Y.-M.; Yan, W.; Yuan, K.; Su, S.-Z.; Lu, Z.-A.; Huang, Y.-T.; Liu, L.; et al. COVID-19 Vaccine-Related Psychological Stress Among General Public in China. Front. Psychiatry 2021, 12, 774504. [Google Scholar] [CrossRef] [PubMed]
- Galanis, P.; Katsiroumpa, A.; Sourtzi, P.; Siskou, O.; Konstantakopoulou, O.; Katsoulas, T.; Kaitelidou, D. COVID-19-Related Burnout and Intention of Fully Vaccinated Individuals to Get a Booster Dose: The Mediating Role of Resilience. Vaccines 2023, 11, 62. [Google Scholar] [CrossRef]
- Peng, Y. Politics of COVID-19 vaccine mandates: Left/right-wing authoritarianism, social dominance orientation, and libertarianism. Personal. Individ. Dif. 2022, 194, 111661. [Google Scholar] [CrossRef]
- Edwards, B.; Biddle, N.; Gray, M.; Sollis, K. COVID-19 vaccine hesitancy and resistance: Correlates in a nationally representative longitudinal survey of the Australian population. PLoS ONE 2021, 16, e0248892. [Google Scholar] [CrossRef]
- Freeman, D.; Loe, B.S.; Chadwick, A.; Vaccari, C.; Waite, F.; Rosebrock, L.; Jenner, L.; Petit, A.; Lewandowsky, S.; Vanderslott, S.; et al. COVID-19 vaccine hesitancy in the UK: The Oxford coronavirus explanations, attitudes, and narratives survey (Oceans) II. Psychol. Med. 2020, 52, 3127–3141. [Google Scholar] [CrossRef] [PubMed]
- Nazlı, Ş.B.; Yığman, F.; Sevindik, M.; Deniz Özturan, D. Psychological factors affecting COVID-19 vaccine hesitancy. Ir. J. Med. Sci. 2022, 191, 71–80. [Google Scholar] [CrossRef]
- Gelfand, M.J.; Raver, J.L.; Nishii, L.; Leslie, L.M.; Lun, J.; Lim, B.C.; Duan, L.; Almaliach, A.; Ang, S.; Arnadottir, J.; et al. Differences Between Tight and Loose Cultures: A 33-Nation Study. Science 2011, 332, 1100–1104. [Google Scholar] [CrossRef]
- Ng, J.H.; Tan, E.K. COVID-19 vaccination and cultural tightness. Psychol. Med. 2021, 53, 1124–1125. [Google Scholar] [CrossRef]
- Mathieu, E.; Ritchie, H.; Rodés-Guirao, L.; Appel, C.; Giattino, C.; Hasell, J.; Macdonald, B.; Dattani, S.; Beltekian, D.; Ortiz-Ospina, E.; et al. Coronavirus Pandemic (COVID-19). 2020. Available online: https://ourworldindata.org/coronavirus (accessed on 10 August 2022).
- Kleitman, S.; Fullerton, D.J.; Zhang, L.M.; Aidman, E. The Role of Cognitive Fitness Constructs in Predicting Mental Well-Being and Its Recovery after the First COVID-19 Lockdown in Australia; The University of Sydney: Sydney, Australia, 2022; submitted. [Google Scholar]
- Martin, L.R.; Petrie, K.J. Understanding the dimensions of anti-vaccination attitudes: The Vaccination Attitudes Examination (VAX) Scale. Ann. Behav. Med. 2017, 51, 652–660. [Google Scholar] [CrossRef] [PubMed]
- Cuadrado, E.; Maldonado, M.A.; Tabernero, C.; Arenas, A.; Castillo-Mayén, R.; Luque, B. Construction and Validation of a Brief Pandemic Fatigue Scale in the Context of the Coronavirus-19 Public Health Crisis. Int. J. Public Health 2021, 66, 1604260. [Google Scholar] [CrossRef] [PubMed]
- Chinn, D.; McCarthy, C. All Aspects of Health Literacy Scale (AAHLS): Developing a tool to measure functional, communicative and critical health literacy in primary healthcare settings. Patient Educ. Couns. 2013, 90, 247–253. [Google Scholar] [CrossRef] [PubMed]
- Donnellan, M.B.; Oswald, F.L.; Baird, B.M.; Lucas, R.E. The Mini-IPIP Scales: Tiny-yet-effective measures of the Big Five factors of personality. Psychol. Assess. 2006, 18, 192–203. [Google Scholar] [CrossRef]
- Stankov, L. Gf-Gc Quickie Test Battery. 1997; unpublished test battery. [Google Scholar]
- Jackson, S.A.; Kleitman, S. Individual differences in decision-making and confidence: Capturing decision tendencies in a fictitious medical test. Metacogn. Learn. 2014, 9, 25–49. [Google Scholar] [CrossRef]
- Jackson, S.A.; Kleitman, S.; Howie, P.; Stankov, L. Cognitive abilities, monitoring confidence, and control thresholds explain individual differences in heuristics and biases. Front. Psychol. 2016, 7, 1559. [Google Scholar] [CrossRef]
- Toplak, M.E.; West, R.F.; Stanovich, K.E. Assessing miserly information processing: An expansion of the Cognitive Reflection Test. Think. Reason. 2014, 20, 147–168. [Google Scholar] [CrossRef]
- Campbell-Sills, L.; Stein, M.B. Psychometric analysis and refinement of the Connor-davidson Resilience Scale (CD-RISC): Validation of a 10-item measure of resilience. J. Trauma. Stress 2007, 20, 1019–1028. [Google Scholar] [CrossRef]
- Hong, S.-M.; Page, S. A psychological reactance scale: Development, factor structure and reliability. Psychol. Rep. 1989, 64, 1323–1326. [Google Scholar] [CrossRef]
- Shen, L.; Dillard, J.P. Psychometric properties of the Hong Psychological Reactance Scale. J. Personal. Assess. 2005, 85, 74–81. [Google Scholar] [CrossRef]
- Everett, J.A.C. The 12 item Social and Economic Conservatism Scale (SECS). PLoS ONE 2013, 8, e82131. [Google Scholar] [CrossRef]
- Bruder, M.; Haffke, P.; Neave, N.; Nouripanah, N.; Imhoff, R. Measuring individual differences in generic beliefs in conspiracy theories across cultures: Conspiracy mentality questionnaire. Front. Psychol. 2013, 4, 225. [Google Scholar] [CrossRef] [PubMed]
- Melo, S.; Corcoran, R.; Shryane, N.; Bentall, R.P. The Persecution and Deservedness Scale. Psychol. Psychother. Theory Res. Pract. 2009, 82, 247–260. [Google Scholar] [CrossRef] [PubMed]
- Petersen, M.; Osmunden, M.; Areceneaux, K. The “need for chaos” and motivations to share hostile political rumors. Am. Political Sci. Rev. 2023, 1–20. [Google Scholar] [CrossRef]
- Stankov, L.; Knezevic, G. Amoral social attitudes and value systems among Serbs and Australians. Aust. J. Psychol. 2005, 57, 115–128. [Google Scholar] [CrossRef]
- Hagenaars, J.A.; McCutcheon, A.L. Applied Latent Class Analysis; Cambridge University Press: Cambridge, UK, 2002. [Google Scholar]
- Marsh, H.W.; Lüdtke, O.; Trautwein, U.; Morin, A.J.S. Classical Latent Profile Analysis of Academic Self-Concept Dimensions: Synergy of Person- and Variable-Centered Approaches to Theoretical Models of Self-Concept. Struct. Equ. Model. Multidiscip. J. 2009, 16, 191–225. [Google Scholar] [CrossRef]
- Spurk, D.; Hirschi, A.; Wang, M.; Valero, D.; Kauffeld, S. Latent profile analysis: A review and “how to” guide of its application within vocational behavior research. J. Vocat. Behav. 2020, 120, 103445. [Google Scholar] [CrossRef]
- Sauder, D.; DeMars, C. An Updated Recommendation for Multiple Comparisons. Adv. Methods Pract. Psychol. Sci. 2019, 2, 251524591880878. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioural Sciences, 2nd ed.; Lawrence Erlbaum Associates, Publishers: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Tabachnick, B.G.; Fidell, L.S. Using Multivariate Statistics, 6th ed.; Pearson: Boston, MA, USA, 2013. [Google Scholar]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2021. [Google Scholar]
- Moore, R.; Purvis, R.S.; Hallgren, E.; Willis, D.E.; Hall, S.; Reece, S.; CarlLee, S.; Judkins, H.; McElfish, P.A. Motivations to Vaccinate Among Hesitant Adopters of the COVID-19 Vaccine. J. Community Health 2022, 47, 237–245. [Google Scholar] [CrossRef]
- Sauch Valmaña, G.; Fuster-Casanovas, A.; Ramírez-Morros, A.; Rodoreda Pallàs, B.; Vidal-Alaball, J.; Ruiz-Comellas, A.; Miró Catalina, Q. Motivation for Vaccination against COVID-19 in Persons Aged between 18 and 60 Years at a Population-Based Vaccination Site in Manresa (Spain). Vaccines 2022, 10, 597. [Google Scholar] [CrossRef]
- Monash University. The Australian Government is Trapped in a Cycle of Distrust—How Can It Break Out? Available online: https://lens.monash.edu/@politics-society/2022/2005/2002/1384632/the-australian-government-is-trapped-in-a-cycle-of-distrust-how-can-it-break-out (accessed on 21 February 2023).
- Edelman. Trust Barometer 2022 Australia. Available online: https://edelman.com.au/trust-barometer-2022-australia (accessed on 21 February 2023).
- Garde, D.; Herper, M. Pfizer and BioNTech to Submit COVID-19 Vaccine Data to FDA as Full Results Show 95% Efficacy. Available online: https://www.statnews.com/2020/2011/2018/pfizer-biontech-covid2019-vaccine-fda-data/ (accessed on 19 April 2023).
- Branswell, H. COVID-19 Vaccines Never Promised Perfection. Experts Say It’s Time to Curb Our Highest Expectations. Available online: https://www.pbs.org/newshour/health/covid-19-vaccines-never-promised-perfection-experts-say-its-time-to-curb-our-highest-expectations (accessed on 19 April 2023).
- Van der Zwet, K.; Barros, A.I.; van Engers, T.M.; Sloot, P.M.A. Emergence of protests during the COVID-19 pandemic: Quantitative models to explore the contributions of societal conditions. Humanit. Soc. Sci. Commun. 2022, 9, 68. [Google Scholar] [CrossRef]
- Kreuter, M.W.; Bull, F.C.; Clark, E.M.; Oswald, D.L. Understanding how people process health information: A comparison of tailored and nontailored weight-loss materials. Health Psychol. 1999, 18, 487–494. [Google Scholar] [CrossRef] [PubMed]
- Fernandez, S.; Wagner, E.; Hospital, M.; Howard, M.; Morris, S. Social media based strategies to reach Hispanic young adults with tailored sexual health information. Soc. Work Soc. Sci. Rev. 2019, 21, 73–93. [Google Scholar] [CrossRef]
- Kreps, G.L.; Sparks, L. Meeting the health literacy needs of immigrant populations. Patient Educ. Couns. 2008, 71, 328–332. [Google Scholar] [CrossRef]
- Desborough, J.; Wright, M.; Parkinson, A.; Hall Dykgraaf, S.; Ball, L.; Dut, G.M.; Sturgiss, E.; de Toca, L.; Kidd, M. What strategies have been effective in optimising COVID-19 vaccine uptake in Australia and internationally? Aust. J. Gen. Pract. 2022, 51, 725–730. [Google Scholar] [CrossRef] [PubMed]
- Australian Bureau of Statistics. National, State and Territory Population. Available online: https://abs.gov.au/statistics/people/population/national-state-and-territory-population/latest-release (accessed on 10 February 2023).
- Australian Bureau of Statistics. Regional Population by Age and Sex. Available online: https://abs.gov.au/statistics/people/population/regional-population-age-and-sex/2021 (accessed on 10 February 2023).
- Australian Bureau of Statistics. Education and Work, Australia. Available online: https://www.abs.gov.au/statistics/people/education/education-and-work-australia/may-2022 (accessed on 21 February 2023).

| Classes | AIC | BIC | SABIC | Entropy | BLRT(p) | LogLik | LogLik(p) * |
|---|---|---|---|---|---|---|---|
| 1 | 31,438 | 31,604 | 31,484 | 1 | - | −15,681 | - |
| 2 | 29,372 | 29,625 | 29,441 | 0.94 | 0.01 | −14,628 | <0.001 |
| 3 | 28,697 | 29,038 | 28,790 | 0.91 | 0.01 | −14,271 | <0.001 |
| 4 | 28,408 | 28,836 | 28,525 | 0.87 | 0.01 | −14,106 | <0.001 |
| 5 | 28,211 | 28,726 | 28,351 | 0.86 | 0.01 | −13,987 | <0.001 |
| 6 | 28,129 | 28,731 | 28,293 | 0.84 | 0.01 | −13,926 | <0.001 |
| 3-class solution | |||||||
| Counts and proportions for latent classes | Average probability of class classification accuracy for each class | ||||||
| Counts | Proportions | Class 1 | Class 2 | Class 3 | |||
| Class 1 | 176 | 0.30 | 0.95 | 0.05 | 0.00 | ||
| Class 2 | 353 | 0.61 | 0.04 | 0.96 | 0.00 | ||
| Class 3 | 53 | 0.09 | 0.03 | 0.00 | 0.97 | ||
| Mean (SD) | ANOVA | Pairwise Comparisons p-Value | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| α | Class 1 Hesitant (n = 176) | Class 2 Acceptant (n = 353) | Class 3 Resistant (n = 53) | F | p-Value | η2 | c1-2 | c1-3 | c2-3 | |
| Hesitant | Acceptant | Resistant | ||||||||
| Demographics | ||||||||||
| Age | - | 32.61 (10.9) | 35.78 (13.82) | 34.15 (10.53) | 4.14 | <0.05 | 0.05 | 0.01 | 0.62 | 0.58 |
| COVID-19 variables: Vaccination and conspiracy beliefs | ||||||||||
| Vaccination Status | - | 2.24 (0.63) | 2.58 (0.55) | 1.38 (1.1) | 45.37 | <0.001 | 0.42 | <0.001 | <0.001 | <0.001 |
| COVID-19 Conspiracy | 0.89 | 1.42 (0.72) | 1.17 (0.45) | 2.32 (1.25) | 28.94 | <0.001 | 0.34 | <0.001 | <0.001 | <0.001 |
| Reasons for getting primary vaccination doses | ||||||||||
| Regaining Freedom/Work Requirements | 0.69 | 4.23 (1.21) | 3.96 (1.44) | 4.39 (1.29) | 3.47 | <0.05 | 0.07 | 0.07 | 0.77 | 0.16 |
| External Pressures | 0.74 | 2.80 (1.21) | 2.09 (1.05) | 2.20 (1.06) | 21.6 | <0.001 | 0.33 | <0.001 | 0.01 | 0.85 |
| Protecting Self and Others | 0.92 | 5.02 (0.70) | 5.75 (0.43) | 3.22 (1.17) | 149.75 | <0.001 | 0.79 | <0.001 | <0.001 | <0.001 |
| Reasons for getting/would get a booster dose | ||||||||||
| Regaining Freedom/Work Requirements | 0.70 | 4.4 (1.19) | 4.03 (1.49) | 4.13 (1.51) | 4.88 | <0.01 | 0.10 | 0.005 | 0.58 | 0.92 |
| External Pressures | 0.75–0.80 | 2.74 (1.25) | 2.18 (1.27) | 2.01 (1.04) | 13.28 | <0.001 | 0.22 | <0.001 | 0.002 | 0.65 |
| Mean (SD) | ANOVA | Pairwise Comparisons (p-Values) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| α | Class 1 (n = 176) | Class 2 (n = 353) | Class 3 (n = 53) | F | p-Value | η2 | c1-2 | c1-3 | c2-3 | |
| Hesitant | Acceptant | Resistant | ||||||||
| Official Sources | 0.80 | 2.42 (0.78) | 2.84 (0.79) | 2.20 (0.74) | 27.64 | <0.001 | 0.28 | <0.001 | 0.14 | <0.001 |
| Unofficial Sources | 0.62 | 2.49 (0.68) | 2.52 (0.66) | 2.41 (0.70) | 0.56 | 0.57 | 0.01 | 0.89 | 0.75 | 0.56 |
| Check News | - | 2.95 (1.01) | 3.51 (0.86) | 2.74 (1.09) | 27.64 | <0.001 | 0.30 | <0.001 | 0.42 | <0.001 |
| Check Source | - | 2.98 (1.07) | 3.54 (1.12) | 3.26 (1.24) | 15.37 | <0.001 | 0.18 | <0.001 | 0.30 | 0.29 |
| Share News | - | 2.42 (1.15) | 2.81 (1.17) | 2.43 (1.29) | 7.50 | <0.001 | 0.10 | <0.001 | 1.00 | 0.12 |
| Mean (SD) | ANOVA | Pairwise Comparisons (p-Values) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| α | Class 1 (n = 176) | Class 2 (n = 353) | Class 3 (n = 53) | F | p-Value | η2 | c1-2 | c1-3 | c2-3 | |
| Hesitant | Acceptant | Resistant | ||||||||
| Psychological Characteristics | ||||||||||
| Agreeableness | 0.81 | 14.55 (3.28) | 15.59 (3.16) | 14.34 (3.03) | 8.25 | <0.001 | 0.10 | 0.002 | 0.90 | 0.02 |
| Conscientiousness | 0.68 | 13.6 (2.81) | 14.11 (3.39) | 14.26 (2.98) | 2.05 | 0.13 | 0.03 | 0.16 | 0.32 | 0.94 |
| Extraversion | 0.80 | 9.96 (3.67) | 10.28 (3.75) | 9.92 (3.59) | 0.55 | 0.58 | 0.01 | 0.62 | 1.00 | 0.78 |
| Neuroticism | 0.77 | 12.12 (3.33) | 12.14 (3.71) | 12.4 (3.45) | 0.14 | 0.87 | 0.00 | 1.00 | 0.86 | 0.87 |
| Openness | 0.74 | 14.51 (3.04) | 15.21 (3.37) | 15.04 (3.19) | 2.96 | 0.05 | 0.04 | 0.04 | 0.53 | 0.93 |
| Resilience | 0.92 | 24.19 (7.27) | 24.81 (7.51) | 24.34 (9.25) | 0.44 | 0.65 | 0.01 | 0.63 | 0.99 | 0.93 |
| Intolerance | 0.91 | 27.64 (7.08) | 27.81 (7.27) | 29.19 (8.10) | 0.80 | 0.45 | 0.01 | 0.96 | 0.42 | 0.48 |
| Reactance | 0.90 | 2.95 (0.60) | 2.45 (0.62) | 3.23 (0.60) | 58.33 | <0.001 | 0.45 | <0.001 | 0.01 | <0.001 |
| Cognitive Ability and Decision Making | ||||||||||
| EAT Accuracy | 0.72 | 62.62 (20.01) | 69.34 (18.6) | 61.45 (22.03) | 8.62 | <0.001 | 0.11 | <0.001 | 0.94 | 0.04 |
| CRT Accuracy | 0.67 | 47.44 (35.26) | 50.42 (34.44) | 46.7 (37.35) | 0.56 | 0.57 | 0.01 | 0.63 | 0.99 | 0.77 |
| Bullshit receptivity | 0.91 | 2.38 (0.90) | 2.22 (0.87) | 2.28 (0.88) | 1.77 | 0.17 | 0.02 | 0.14 | 0.76 | 0.89 |
| Political, Cultural and Social Attitudes | ||||||||||
| Conservatism | 0.62 | 3.31 (0.75) | 2.92 (0.91) | 3.51 (0.86) | 19.12 | <0.001 | 0.21 | <0.001 | 0.28 | <0.001 |
| Conspiracy mentality | 0.83 | 4.36 (0.83) | 3.95 (0.90) | 4.89 (0.96) | 29.91 | <0.001 | 0.30 | <0.001 | 0.001 | <0.001 |
| Persecution | 0.89 | 2.42 (0.94) | 2.03 (0.83) | 2.39 (0.88) | 12.53 | <0.001 | 0.15 | <0.001 | 0.98 | 0.02 |
| Need for Chaos | 0.81 | 2.16 (0.98) | 1.65 (0.71) | 2.32 (1.15) | 25.49 | <0.001 | 0.29 | <0.001 | 0.63 | <0.001 |
| Cultural Tightness | 0.67 | 4.1 (0.53) | 4.16 (0.61) | 4.59 (0.58) | 15.24 | <0.001 | 0.18 | 0.48 | <0.001 | <0.001 |
| Amorality | 0.66 | 2.45 (0.60) | 2.11 (0.55) | 2.75 (0.61) | 38.34 | <0.001 | 0.36 | <0.001 | 0.005 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kleitman, S.; Fullerton, D.J.; Law, M.K.H.; Blanchard, M.D.; Campbell, R.; Tait, M.-A.; Schulz, J.; Lee, J.; Stankov, L.; King, M.T. The Psychology of COVID-19 Booster Hesitancy, Acceptance and Resistance in Australia. Vaccines 2023, 11, 907. https://doi.org/10.3390/vaccines11050907
Kleitman S, Fullerton DJ, Law MKH, Blanchard MD, Campbell R, Tait M-A, Schulz J, Lee J, Stankov L, King MT. The Psychology of COVID-19 Booster Hesitancy, Acceptance and Resistance in Australia. Vaccines. 2023; 11(5):907. https://doi.org/10.3390/vaccines11050907
Chicago/Turabian StyleKleitman, Sabina, Dayna J. Fullerton, Marvin K. H. Law, Matthew D. Blanchard, Rachel Campbell, Margaret-Ann Tait, Jennifer Schulz, Jihyun Lee, Lazar Stankov, and Madeleine T. King. 2023. "The Psychology of COVID-19 Booster Hesitancy, Acceptance and Resistance in Australia" Vaccines 11, no. 5: 907. https://doi.org/10.3390/vaccines11050907
APA StyleKleitman, S., Fullerton, D. J., Law, M. K. H., Blanchard, M. D., Campbell, R., Tait, M.-A., Schulz, J., Lee, J., Stankov, L., & King, M. T. (2023). The Psychology of COVID-19 Booster Hesitancy, Acceptance and Resistance in Australia. Vaccines, 11(5), 907. https://doi.org/10.3390/vaccines11050907









