Abstract
Vaccine hesitancy amongst healthcare workers (HCWs) has been a major challenge throughout the COVID-19 pandemic. While many studies have identified HCW characteristics and specific attitudes associated with COVID-19 vaccine hesitancy, researchers are still working towards developing a holistic understanding of the psychological constructs that influence COVID-19 vaccine decision-making in this population. Between 15 March and 29 March 2021, we distributed an online survey assessing individual characteristics and vaccine-related perceptions to employees of a not-for-profit healthcare system in Southwest Virginia (N = 2459). We then performed exploratory factor analysis (EFA) and confirmatory factor analysis (CFA) to describe patterns of vaccine-related thought amongst HCWs and identify latent psychometric constructs involved in vaccine decision-making. The goodness of model fit was assessed using the Tucker–Lewis Index (TLI), the Comparative Fit Index (CFI), and the Root Mean Square Error of Approximation (RMSEA). Internal consistency and reliability of each factor were assessed using Cronbach’s alpha. EFA identified four latent psychometric constructs: Lack of trust in the COVID-19 vaccine; Anti-science sentiment; Adverse side-effects; and Situational risk assessment. The goodness of EFA model fit was adequate (TLI > 0.90, RMSEA ≤ 0.08) with acceptable internal consistency and reliability for three of four factors (Cronbach’s alpha > 0.70). The CFA model also had adequate goodness of fit (CFI > 0.90, RMSEA ≤ 0.08). We believe the psychometric constructs identified in this study can provide a useful framework for interventions to improve vaccine uptake amongst this critical population.
Keywords:
vaccine; hesitancy; healthcare workers; COVID-19; psychometric constructs; factor analysis 1. Introduction
As of 21 January 2023, SARS-CoV-2 has infected over 101.8 million individuals in the United States, resulting in just under 1.1 million deaths [1]. Four vaccines (Pfizer-BioNTech, Moderna, Johnson & Johnson, and Novavax) have been authorized for use in the US. Despite the widespread availability of these vaccines across the country and their demonstrated safety and efficacy [2,3,4,5], only 69.1% of Americans have completed the primary vaccine series, and just 15.3% have received their bivalent booster [1].
Anti-vaccine sentiment and vaccine hesitancy have been considerable public health challenges since long before the advent of COVID-19. The World Health Organization (WHO) declared vaccine hesitancy to be one of the top ten biggest threats to global health in 2017 [6], and it remains a major international concern that has hampered efforts to control the spread of COVID-19 [7]. Achieving widespread COVID-19 vaccination has become even more complicated by the politically charged nature of the issue, contributing to higher rates of hesitancy for some [8]. In addition, the novelty of mRNA vaccine technology and the speed with which these vaccines were developed may have further intensified hesitancy [9]. This matter is particularly problematic within the United States; a global survey of 17 countries from early in the COVID-19 vaccine rollout found that the US had the second highest proportion of respondents who said they would be unlikely to be vaccinated [10]. Common reasons for COVID-19 vaccine hesitancy included concerns regarding safety, efficacy, and both long- and short-term side-effects. Additionally, both female sex and lower educational attainment have been found to be predictive of hesitancy [11,12].
One group amongst whom COVID-19 vaccine hesitancy has been especially problematic over the course of the pandemic is healthcare workers (HCWs). Studies of HCWs in various contexts found degrees of hesitancy that ranged between 15% and 30% [13,14,15,16,17,18,19]. Demographic factors associated with COVID-19 vaccine hesitancy amongst HCWs included younger age [13,15,16,20,21,22,23], female sex [13,16,17,18,19,21,24,25,26,27], African American race [15,16,17,26,27], and lower educational attainment [17,23,27]. Role in healthcare has also been found to be predictive of vaccine hesitancy, with nurses consistently displaying higher levels of hesitancy compared to physicians [13,15,16,17,18,21,23,24,25,26,27,28]. Common reported reasons for COVID-19 vaccine hesitancy included concerns regarding safety [11,14,19,27,29], efficacy [11,16,17,27,29], fertility [13,15,17], and side-effects [11,13,14,15,16,26], as well as a desire to wait for more data [17,18,19,22,27]. Additionally, data show that more than 25% of HCWs may be hesitant to receive a booster dose [30,31].
While many studies have identified HCW characteristics and specific attitudes that are associated with COVID-19 vaccine hesitancy, to our knowledge, no research performed to present has measured the underlying psychological constructs associated with COVID-19 vaccine decision-making in this population. To fill this gap in the literature, we conducted exploratory and confirmatory factor analyses (EFA/CFA) on data from an internet-based survey of HCWs to characterize these latent constructs.
Factor analysis encompasses a set of analytical techniques that allow researchers to identify latent variables, or “factors,” that lie hidden within a dataset. By examining patterns of interrelationships between a dataset’s observed variables, investigators can characterize factors that cannot be measured directly but which may have broader implications than any individual measured variable has on its own [32].
EFA and CFA have been used to investigate the psychology underlying a wide variety of health behaviors. In their research on oral health practices, Xiang et al. identified six relevant psychometric factors based on the Health Belief Model: perceived susceptibility, perceived benefits, perceived barriers, cues to action, perceived severity, and self-efficacy [33]. Wang et al. determined that benefits, barriers, peer support, and self-efficacy are key factors that contribute to the psychology of medication non-adherence [34]. EFA and CFA have also been employed to deepen researchers’ understanding of food literacy behaviors in university students [35], pre-exposure prophylaxis adherence amongst HIV patients [36], and picky eating in children [37].
This article builds upon previously published research that identified demographic factors and individual beliefs associated with COVID-19 vaccine hesitancy amongst HCWs [16]. The present study employs EFA and CFA to identify and describe latent psychometric constructs that were involved in vaccine decision-making early in the vaccine roll-out. While vaccine mandates have required many HCWs to receive their initial vaccinations, remaining up to date with boosters will continue to be important to prevent COVID-19 infections in this population. Additionally, new, Omicron-adapted bivalent mRNA vaccines were authorized in August 2022 and are now recommended as booster doses [38]. As COVID-19 vaccinations and recommendations continue to evolve, and as we transition into an endemic phase of the pandemic, we believe the constructs characterized herein can provide a framework and efficient targets for interventions designed to improve vaccine and booster uptake amongst this critical population.
2. Materials and Methods
2.1. Sample and Study Design
Detailed study methods, including survey design and participant recruitment, have been described elsewhere [16]. Between 15 March and 29 March 2021, all 13,690 adult employees of a not-for-profit healthcare system in Southwest Virginia received an email with a link to our online questionnaire. Other distribution channels included a posting on the healthcare system intranet and print advertisements located in various clinical sites, which included QR codes for easy access.
Our survey was built in REDCap (Research Electronic Data Capture), a HIPAA-compliant web application and back-end database model developed at Vanderbilt University [39]. Participants could self-administer the questionnaire online using any device of their choosing. The survey instrument was written in English and was composed of 30 items addressing COVID-19 vaccination status, vaccine intentions, personal experiences with COVID-19, thoughts and beliefs regarding COVID-19 vaccines, and sociodemographic variables. The survey contained 15 five-point Likert-type items assessing level of agreement with various vaccine-related perceptions. The responses to four Likert-type items were reverse coded to scale all questions in the same direction, such that all higher scores indicated anti-vaccine sentiment and all lower scores indicated pro-vaccine sentiment. Respondents who had already received either one or two vaccine doses when they completed the questionnaire were categorized as vaccine acceptant. Because the COVID-19 vaccine had been available and accessible to respondents for over three months when we launched our survey, HCWs who had not received at least one vaccine dose at the time of survey completion were considered vaccine hesitant. The complete survey instrument is available in Supplement S1.
We received 2720 total survey responses, out of which 261 (9.6%) had missing information for at least one survey item. Differences between participants with and without missing information were deemed negligible due to small effect sizes (Cramer’s V < 0.40). We thus conducted a complete case analysis and analyzed information only from respondents with complete data on all survey items (N = 2459). The study sample was randomly divided into two groups; Group 1 (n = 1229) was used for exploratory factor analysis (EFA) and Group 2 (n = 1230) was used for confirmatory factor analysis (CFA).
2.2. Statistical Methods
Sociodemographic and work-related characteristics, as well as survey items pertaining to vaccine-related perceptions, were examined using descriptive statistics. The extraction of latent psychometric constructs that influenced COVID-19 vaccine decision-making was performed in Group 1 using EFA, where an oblique rotation (Oblimin) was used to facilitate the interpretation of the factors. Various sources of information were used to determine the number of factors to extract, including scree plots, factor diagrams, and subject matter expertise. The adequacy of the EFA model was assessed using the Tucker–Lewis Index (TLI), the Comparative Fit Index (CFI), and the Root Mean Square Error of Approximation (RMSEA). A CFI or TLI score ≥ 0.90 and a RMSEA < 0.08 indicated good fit [40]. Validation of the factor structure was then examined using CFA in Group 2, where adequate model fit was indicated by correlation residuals < 0.30. Finally, internal consistency and reliability of the factors were evaluated based on Cronbach’s alpha, where values of 0.70 or higher were considered acceptable [41]. All analyses were performed in R using the ‘lavaan’ package [42,43].
3. Results
3.1. Descriptive Statistics
Demographic and other HCW characteristics are presented in Table 1. Respondents were predominantly female (82%), white or Caucasian (89%), and aged 25 years or older (95%). The most represented healthcare role was nursing staff (34%), and the least represented was healthcare providers (8%). The distribution of responses to individual survey items is presented in Table 2.

Table 1.
Demographic and Other Healthcare Worker Characteristics (N = 2459).

Table 2.
Survey Item Responses (N = 2459).
3.2. Exploratory Factor Analysis (EFA)
Combined with scree plots (see Figure A1), factor diagrams, and subject matter expertise, EFA revealed four distinct factors influencing COVID-19 vaccine decision-making amongst HCWs:
- Factor 1: Lack of trust in the COVID-19 vaccine
- Factor 2: Anti-science sentiment
- Factor 3: Adverse side-effects
- Factor 4: Situational risk assessment
Correlations between factors are presented in Table A1 (see Exploratory Factor Analysis) and Figure A2 in Appendix A. Although Factor 4 was weakly correlated with the other three factors, it was retained in our model because excluding the items that loaded onto this factor (Work Risk and Outside Risk) produced a model that did not yield meaningful psychometric constructs. Table 3 contains the survey items that comprised each factor, the spread of the data that was accounted for by each factor (i.e., the proportion of variance explained), and a measure of each factor’s internal consistency and reliability (Cronbach’s alpha). All survey items had strong or moderate correlations with their respective factors. The largest proportion of the variance (40.7%) was accounted for by Factor 1 (Lack of trust in the COVID-19 vaccine). The EFA model demonstrated a good fit to the data distribution (CFI = 0.932; RMSEA = 0.07).

Table 3.
Factor Loadings and Internal Reliability.
3.3. Confirmatory Factor Analysis (CFA)
CFA on the four-factor model showed a good fit to the data as evidenced by weak residual correlations (<0.30). The CFA model is visualized in Figure 1, where the survey items and the extracted factors onto which they loaded most strongly are presented along with the factor loadings (i.e., the correlation of each survey item with its associated factor) and correlations between factors (see Table A1, Confirmatory Factor Analysis). All survey items had strong correlations with their respective factors. Except Factor 4 (Situational risk assessment), which consisted of only two survey items (Cronbach’s alpha = 0.637), all factors demonstrated good internal consistency and reliability with a Cronbach’s alpha > 0.70 (Table 3).
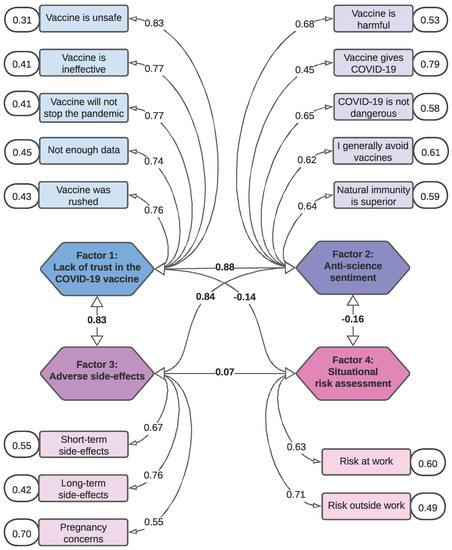
Figure 1.
CFA Factor Diagram. Survey items mapped to the factors onto which they loaded most strongly in CFA. The hexagons in the center represent factors, with each arrow from factor to factor providing the standardized covariance (Pearson’s correlation, r) between those two factors. The rectangles represent survey items, with each arrow from factor to survey item providing the factor loading (correlation between factor and survey item) for the factor onto which that survey item loaded most strongly. The ovals in the outer margins next to the survey items provide the variance of each individual survey item.
4. Discussion
By assessing a broad range of individual beliefs and perceptions, we identified four underlying psychological constructs associated with COVID-19 vaccine decision-making amongst HCWs: Lack of trust in the COVID-19 vaccine; Anti-science sentiment; Adverse side-effects; and Situational risk assessment. Much of the prior research on predictors of COVID-19 vaccine uptake amongst HCWs focused on specific characteristics, attitudes, and opinions associated with vaccine hesitancy. By employing EFA and CFA techniques to extract and validate latent psychometric constructs, we have described broader patterns of thought related to HCW COVID-19 vaccine decision-making.
The psychometric factors we identified share considerable overlap with the 5C psychological antecedents of vaccination, a model that identifies Confidence, Constraints, Complacency, Calculation, and Collective responsibility as contributors to vaccine hesitancy [44]. Elements of the 5C model have been explored as predictors of COVID-19 vaccine hesitancy amongst HCWs in Hong Kong [20], Singapore [30], and Kuwait [45]. The 5C model has also more recently been expanded to a 7C model with the additions of Conspiracy and Compliance [46]. We feel that this manuscript builds on such research by analyzing data from a survey that was expressly developed with COVID-19 vaccines in mind and which may thus hone in more closely on the specific concerns that are relevant to vaccination in the context of a rapidly evolving pandemic. Additionally, both the 5C and 7C models were initially tested on general population convenience samples [44,46], while the present analysis was performed on a convenience sample comprised entirely of HCWs; the factor structure identified herein may thus more closely reflect the psychometric constructs that influence vaccine decision-making in this specific population.
While vaccine mandates have required many healthcare workers to receive their initial COVID-19 vaccines irrespective of individual hesitancy, epidemiologic data demonstrate that staying up to date on booster doses provides the most effective protection over time [47]. Despite such evidence, a survey from 2022 found that 87.3% of HCWs reported finishing their primary vaccine series, but just 67.3% reported receiving a booster dose [48]. More recent data from the CDC show that although 86.4% of nursing home staff in the United States completed their primary vaccination series, only 22.6% remain up to date on their COVID-19 vaccines [49]. Strategies that combat booster hesitancy will thus be essential to protecting the healthcare workforce and supporting robust healthcare systems in the future. Because our data were collected when COVID-19 vaccines were very new, we believe our findings will remain relevant moving forward as HCWs periodically decide whether they will get the latest iteration in an evolving series of new vaccines and booster doses. The psychometric factors identified in our study can provide a theoretical framework and discrete areas of emphasis for nuanced messaging and effective interventions to support vaccine coverage in this high-priority population. Specifically, our results suggest that strategies that build trust in these newer vaccines (e.g., by focusing on safety and efficacy concerns) will address underlying hesitancy and may be the most successful at improving uptake among HCWs. Similarly, interventions that alleviate fears about adverse vaccine-related outcomes (e.g., pregnancy complications, and long-term side-effects) may influence decision-making and reduce hesitancy to adopt new, bivalent mRNA vaccines and boosters.
Prior research has shown the need for nuanced strategies to address the multifactorial causes of vaccine hesitancy amongst a diverse healthcare workforce [50]. Numerous studies have investigated interventional strategies to improve COVID-19 vaccine uptake in the early days of vaccine availability. A brief educational video focused on vaccine characteristics, development, side-effects, conspiracy theories, and public health guidelines enhanced COVID-19 vaccine-related thoughts and perceptions amongst a representative sample of Israeli adults [51]. A physician-led, in-person informational intervention centered around the impact of COVID-19, mRNA vaccines (mechanism of action, clinical trial data, adverse events), and common vaccine myths and concerns decreased hesitancy amongst a sample of US active-duty military members [52]. A multifaceted educational program delivered to HCWs at a large tertiary-care center in Japan that included information pamphlets, hospital-wide announcements encouraging COVID-19 vaccination, and mandatory information sessions was associated with increased vaccine uptake [53]. Our research provides a theoretical basis for the successful results observed in these studies, as each of these interventions focused primarily on the science surrounding the safety, efficacy, and side-effects of the newly available COVID-19 vaccines. While our findings also indicate that general anti-science sentiment plays a role in COVID-19 vaccine decision-making in this context, research suggests that this construct may require more complex persuasive strategies to overcome [54].
This study has several limitations. First, we used a convenience sample of survey respondents, and our results may, therefore, not generalize to other HCWs in this health system; additionally, our narrow geographic focus may limit generalizability to HCWs in other settings. Second, although our survey was self-administered and respondents were frequently reminded that their information would be deidentified throughout the questionnaire, the survey was distributed through work channels, and as a result, our data may include some degree of social desirability bias. Third, all responses were received during a two-week period in March 2021. While our results reflect factors associated with decision-making regarding COVID-19 vaccines when they first became available, our data may not directly mirror the thoughts and perceptions that will emerge related to the novelty of adapted vaccines. However, because the psychometric factors identified herein reflect responses to the initial COVID-19 vaccines when they were still very new, we feel our results will remain relevant as novel vaccines and boosters are released and as vaccine technology continues to develop going forward.
Future plans for these data include logistic regression analyses and multidimensional modeling to determine whether the latent constructs we identified are directly predictive of vaccine hesitancy.
With more than 25% of HCWs hesitant to receive a booster dose and with booster uptake flagging in the United States [1], there is a dire need to reduce hesitancy amongst HCWs with unavoidable occupational exposure risk [30,31]. We believe our findings provide a roadmap for developing interventions that can combat uncertainties around COVID-19 vaccines and booster doses—including new bivalent mRNA vaccines – amongst this critical population.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/vaccines11030556/s1, Supplement S1: Survey Instrument.
Author Contributions
Conceptualization, J.B., M.C.S., M.J., C.J.S. and A.B.-B.; methodology, J.B., A.L., J.W., A.L.H. and I.C.; software, A.L., J.W., and I.C.; formal analysis, A.L., J.W. and I.C.; writing—original draft preparation, J.B.; writing—review and editing, M.C.S., A.L., J.W., I.C. and A.B.-B.; visualization, J.B., A.L. and J.W.; supervision, A.B.-B.; project administration, A.B.-B.; funding acquisition, J.B. and A.B.-B. All authors have read and agreed to the published version of the manuscript.
Funding
Research reported in this publication was supported in part by the National Center For Advancing Translational Sciences of the National Institutes of Health under Award Numbers UL1TR003015 and KL2TR003016. The content is solely the responsibility of the authors and does not represent the views of the National Institutes of Health. The APC was funded by Virginia Tech Libraries and the Carilion Clinic Department of Internal Medicine.
Institutional Review Board Statement
This study received a Not Human Subjects Research designation from the Carilion Clinic Institutional Review Board (IRB-21-1236).
Informed Consent Statement
Informed consent was waived due to Not Human Subjects Research designation and fully deidentified data collection procedures.
Data Availability Statement
The data from this study may be obtained upon email request to the senior author, Anthony Baffoe-Bonnie (awbaffoebonnie@carilionclinic.org).
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
Abbreviations
The following abbreviations are used in this manuscript:
| HCW | Healthcare Worker |
| EFA | Exploratory Factor Analysis |
| CFA | Confirmatory Factor Analysis |
| TLI | Tucker Lewis Index |
| CFI | Comparative Fit Index |
| RMSEA | Root Mean Square Error of Approximation |
Appendix A
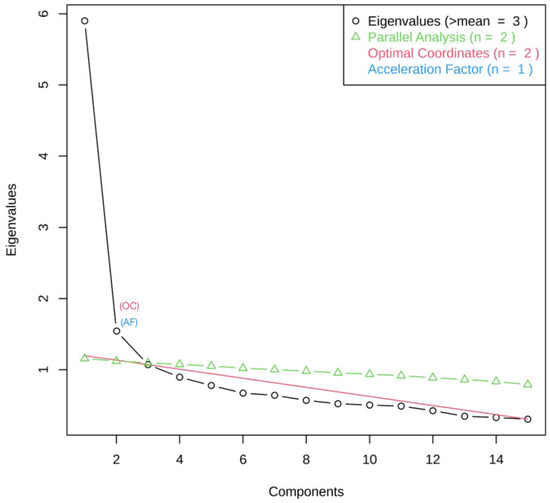
Figure A1.
EFA Scree Plot.
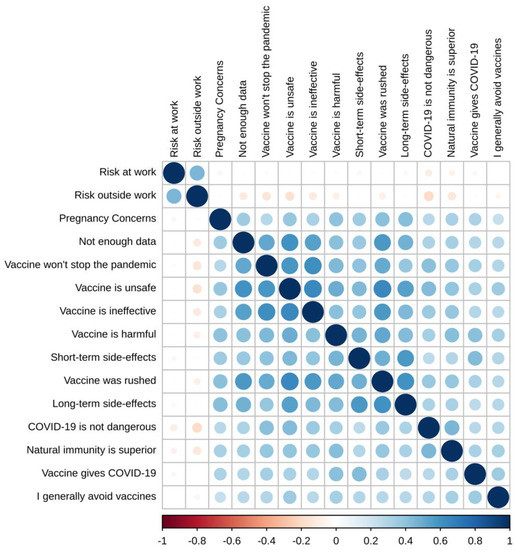
Figure A2.
Graphical Presentation of Correlations Between EFA Factors.

Table A1.
Correlation Matrix of Factors.
Table A1.
Correlation Matrix of Factors.
| Exploratory Factor Analysis | Confirmatory Factor Analysis | |||||||
|---|---|---|---|---|---|---|---|---|
| Factor 1 | Factor 2 | Factor 3 | Factor 4 | Factor 1 | Factor 2 | Factor 3 | Factor 4 | |
| Factor 1: Lack of trust in the COVID-19 vaccine | 1.000 | 0.767 *** | 0.724 *** | −0.211 *** | 1.000 | 0.882 *** | 0.835 *** | −0.142 ** |
| Factor 2: Anti-science sentiment | 0.767 *** | 1.000 | 0.660 *** | −0.143 *** | 0.882 *** | 1.000 | 0.843 *** | −0.163 ** |
| Factor 3: Adverse side-effects | 0.724 *** | 0.660 *** | 1.000 | 0.041 | 0.835 *** | 0.843 *** | 1.000 | 0.066 |
| Factor 4: Situational risk assessment | −0.211 *** | −0.143 *** | 0.041 | 1.000 | −0.142 ** | −0.163 ** | 0.066 | 1.000 |
Note: Pearson’s correlation coefficients (r) are interpreted as small (0.10–0.29), moderate (0.30–0.49), and large (0.50–1.0). * p < 0.05; ** p < 0.01; *** p < 0.001.
References
- CDC. COVID Data Tracker. Available online: https://covid.cdc.gov/covid-data-tracker/#datatracker-home (accessed on 21 January 2023).
- Polack, F.P.; Thomas, S.J.; Kitchin, N.; Absalon, J.; Gurtman, A.; Lockhart, S.; Perez, J.L.; Pérez Marc, G.; Moreira, E.D.; Zerbini, C.; et al. Safety and Efficacy of the BNT162b2 mRNA Covid-19 Vaccine. N. Engl. J. Med. 2020, 383, 2603–2615. [Google Scholar] [CrossRef] [PubMed]
- Baden, L.R.; El Sahly, H.M.; Essink, B.; Kotloff, K.; Frey, S.; Novak, R.; Diemert, D.; Spector, S.A.; Rouphael, N.; Creech, C.B.; et al. Efficacy and Safety of the mRNA-1273 SARS-CoV-2 Vaccine. N. Engl. J. Med. 2021, 384, 403–416. [Google Scholar] [CrossRef] [PubMed]
- Sadoff, J.; Gray, G.; Vandebosch, A.; Cárdenas, V.; Shukarev, G.; Grinsztejn, B.; Goepfert, P.A.; Truyers, C.; Fennema, H.; Spiessens, B.; et al. Safety and Efficacy of Single-Dose Ad26.COV2.S Vaccine against Covid-19. N. Engl. J. Med. 2021, 384, 2187–2201. [Google Scholar] [CrossRef] [PubMed]
- Dunkle, L.M.; Kotloff, K.L.; Gay, C.L.; Áñez, G.; Adelglass, J.M.; Barrat Hernández, A.Q.; Harper, W.L.; Duncanson, D.M.; McArthur, M.A.; Florescu, D.F.; et al. Efficacy and Safety of NVX-CoV2373 in Adults in the United States and Mexico. N. Engl. J. Med. 2022, 386, 531–543. [Google Scholar] [CrossRef]
- Dubé, È.; Ward, J.K.; Verger, P.; MacDonald, N.E. Vaccine Hesitancy, Acceptance, and Anti-Vaccination: Trends and Future Prospects for Public Health. Annu. Rev. Public Health 2021, 42, 175–191. [Google Scholar] [CrossRef]
- Sallam, M.; Al-Sanafi, M.; Sallam, M. A Global Map of COVID-19 Vaccine Acceptance Rates per Country: An Updated Concise Narrative Review. J. Multidiscip. Healthc. 2022, 15, 21–45. [Google Scholar] [CrossRef]
- Albrecht, D. Vaccination, politics and COVID-19 impacts. BMC Public Health 2022, 22, 96. [Google Scholar] [CrossRef]
- Leong, C.; Jin, L.; Kim, D.; Kim, J.; Teo, Y.Y.; Ho, T.H. Assessing the impact of novelty and conformity on hesitancy towards COVID-19 vaccines using mRNA technology. Commun. Med. 2022, 2, 61. [Google Scholar] [CrossRef]
- Wong, L.P.; Alias, H.; Danaee, M.; Ahmed, J.; Lachyan, A.; Cai, C.Z.; Lin, Y.; Hu, Z.; Tan, S.Y.; Lu, Y.; et al. COVID-19 vaccination intention and vaccine characteristics influencing vaccination acceptance: A global survey of 17 countries. Infect. Dis. Poverty 2021, 10, 122. [Google Scholar] [CrossRef]
- de Albuquerque Veloso Machado, M.; Roberts, B.; Wong, B.L.H.; van Kessel, R.; Mossialos, E. The Relationship Between the COVID-19 Pandemic and Vaccine Hesitancy: A Scoping Review of Literature Until August 2021. Front. Public Health 2021, 9, 747787. [Google Scholar] [CrossRef]
- Syan, S.K.; Gohari, M.R.; Levitt, E.E.; Belisario, K.; Gillard, J.; DeJesus, J.; MacKillop, J. COVID-19 Vaccine Perceptions and Differences by Sex, Age, and Education in 1,367 Community Adults in Ontario. Front. Public Health 2021, 9, 719665. [Google Scholar] [CrossRef]
- Gilboa, M.; Tal, I.; Levin, E.G.; Segal, S.; Belkin, A.; Zilberman-Daniels, T.; Biber, A.; Rubin, C.; Rahav, G.; Regev-Yochay, G. Coronavirus disease 2019 (COVID-19) vaccination uptake among healthcare workers. Infect. Control. Hosp. Epidemiol. 2022, 43, 1433–1438. [Google Scholar] [CrossRef]
- King, W.C.; Rubinstein, M.; Reinhart, A.; Mejia, R. Time trends, factors associated with, and reasons for COVID-19 vaccine hesitancy: A massive online survey of US adults from January–May 2021. PLoS ONE 2021, 16, e0260731. [Google Scholar] [CrossRef]
- Toth-Manikowski, S.M.; Swirsky, E.S.; Gandhi, R.; Piscitello, G. COVID-19 vaccination hesitancy among health care workers, communication, and policy-making. Am. J. Infect. Control. 2022, 50, 20–25. [Google Scholar] [CrossRef]
- Swann, M.C.; Bendetson, J.; Johnson, A.; Jatta, M.; Schleupner, C.J.; Baffoe-Bonnie, A. Examining drivers of coronavirus disease 2019 (COVID-19) vaccine hesitancy among healthcare workers. Infect. Control. Hosp. Epidemiol. 2022, 43, 1813–1821. [Google Scholar] [CrossRef]
- Caiazzo, V.; Witkoski Stimpfel, A. Vaccine hesitancy in American healthcare workers during the COVID-19 vaccine roll out: An integrative review. Public Health 2022, 207, 94–104. [Google Scholar] [CrossRef]
- Dzieciolowska, S.; Hamel, D.; Gadio, S.; Dionne, M.; Gagnon, D.; Robitaille, L.; Cook, E.; Caron, I.; Talib, A.; Parkes, L.; et al. Covid-19 vaccine acceptance, hesitancy, and refusal among Canadian healthcare workers: A multicenter survey. Am. J. Infect. Control. 2021, 49, 1152–1157. [Google Scholar] [CrossRef]
- Elliott, T.R.; Perrin, P.B.; Powers, M.B.; Jacobi, K.S.; Warren, A.M. Predictors of Vaccine Hesitancy among Health Care Workers during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2022, 19, 7123. [Google Scholar] [CrossRef]
- Kwok, K.O.; Li, K.K.; Wei, W.I.; Tang, A.; Wong, S.Y.S.; Lee, S.S. Influenza vaccine uptake, COVID-19 vaccination intention and vaccine hesitancy among nurses: A survey. Int. J. Nurs. Stud. 2021, 114, 103854. [Google Scholar] [CrossRef]
- Galanis, P.; Vraka, I.; Fragkou, D.; Bilali, A.; Kaitelidou, D. Intention of health care workers to accept COVID-19 vaccination and related factors: A systematic review and meta-analysis. Asian Pac. J. Trop. Med. 2021, 14, 543–554. [Google Scholar] [CrossRef]
- Huang, D.; Ganti, L.; Graham, E.W.; Shah, D.; Aleksandrovskiy, I.; Al-Bassam, M.; Fraunfelter, F.; Falgiani, M.; Leon, L.; Lopez-Ortiz, C. COVID-19 Vaccine Hesitancy Among Healthcare Providers. Health Psychol. Res. 2022, 10, 3. [Google Scholar] [CrossRef] [PubMed]
- Kandiah, S.; Iheaku, O.; Farrque, M.; Hanna, J.; Johnson, K.B.; Wiley, Z.; Franks, N.M.; Carroll, K.; Shin, S.R.; Sims, K.M.; et al. COVID-19 Vaccine Hesitancy Among Health Care Workers in Four Health Care Systems in Atlanta. Open Forum Infect. Dis. 2022, 9, ofac224. [Google Scholar] [CrossRef] [PubMed]
- Dror, A.A.; Eisenbach, N.; Taiber, S.; Morozov, N.G.; Mizrachi, M.; Zigron, A.; Srouji, S.; Sela, E. Vaccine hesitancy: The next challenge in the fight against COVID-19. Eur. J. Epidemiol. 2020, 35, 775–779. [Google Scholar] [CrossRef] [PubMed]
- Shaw, J.; Hanley, S.; Stewart, T.; Salmon, D.A.; Ortiz, C.; Trief, P.M.; Asiago Reddy, E.; Morley, C.P.; Thomas, S.J.; Anderson, K.B. Healthcare Personnel (HCP) Attitudes About Coronavirus Disease 2019 (COVID-19) Vaccination after Emergency Use Authorization. Clin. Infect. Dis. 2022, 75, e814–e821. [Google Scholar] [CrossRef]
- Browne, S.K.; Feemster, K.A.; Shen, A.K.; Green-McKenzie, J.; Momplaisir, F.M.; Faig, W.; Offit, P.A.; Kuter, B.J. Coronavirus disease 2019 (COVID-19) vaccine hesitancy among physicians, physician assistants, nurse practitioners, and nurses in two academic hospitals in Philadelphia. Infect. Control. Hosp. Epidemiol. 2022, 43, 1424–1432. [Google Scholar] [CrossRef]
- Peterson, C.J.; Lee, B.; Nugent, K. COVID-19 Vaccination Hesitancy among Healthcare Workers—A Review. Vaccines 2022, 10, 948. [Google Scholar] [CrossRef]
- Gadoth, A.; Halbrook, M.; Martin-Blais, R.; Gray, A.; Tobin, N.H.; Ferbas, K.G.; Aldrovandi, G.M.; Rimoin, A.W. Cross-sectional Assessment of COVID-19 Vaccine Acceptance Among Health Care Workers in Los Angeles. Ann. Intern. Med. 2021, 174, 882–885. [Google Scholar] [CrossRef]
- Díaz Luévano, C.; Sicsic, J.; Pellissier, G.; Chyderiotis, S.; Arwidson, P.; Olivier, C.; Gagneux-Brunon, A.; Botelho-Nevers, E.; Bouvet, E.; Mueller, J. Quantifying healthcare and welfare sector workers’ preferences around COVID-19 vaccination: A cross-sectional, single-profile discrete-choice experiment in France. BMJ Open 2021, 11, e055148. [Google Scholar] [CrossRef]
- Koh, S.W.C.; Liow, Y.; Loh, V.W.K.; Liew, S.J.; Chan, Y.H.; Young, D. COVID-19 vaccine acceptance and hesitancy among primary healthcare workers in Singapore. BMC Prim. Care 2022, 23, 81. [Google Scholar] [CrossRef]
- Paris, C.; Bénézit, F.; Geslin, M.; Polard, E.; Baldeyrou, M.; Turmel, V.; Tadié, É.; Garlantezec, R.; Tattevin, P. COVID-19 vaccine hesitancy among healthcare workers. Infect. Dis. Now 2021, 51, 484–487. [Google Scholar] [CrossRef]
- Thompson, B. Exploratory and Confirmatory Factor Analysis: Understanding Concepts and Applications; American Psychological Association: Washington, DC, USA, 2004. [Google Scholar] [CrossRef]
- Xiang, B.; Wong, H.M.; Cao, W.; Perfecto, A.P.; McGrath, C.P.J. Development and validation of the Oral health behavior questionnaire for adolescents based on the health belief model (OHBQAHBM). BMC Public Health 2020, 20, 701. [Google Scholar] [CrossRef]
- Wang, Y.; Wang, X.; Wang, X.; Naqvi, A.A.; Zhang, Q.; Zang, X. Translation and validation of the Chinese version of the general medication adherence scale (GMAS) in patients with chronic illness. Curr. Med. Res. Opin. 2021, 37, 829–837. [Google Scholar] [CrossRef]
- Rhea, K.C.; Cater, M.W.; McCarter, K.; Tuuri, G. Psychometric Analyses of the Eating and Food Literacy Behaviors Questionnaire with University Students. J. Nutr. Educ. Behav. 2020, 52, 1008–1017. [Google Scholar] [CrossRef]
- Yu, X.; Xu, C.; Ni, Y.; Chang, R.; Wang, H.; Gong, R.; Wang, Y.; Wang, S.; Cai, Y. Pre-Exposure Prophylaxis (PrEP) Adherence Questionnaire: Psychometric Validation among Sexually Transmitted Infection Patients in China. Int. J. Environ. Res. Public Health 2021, 18, 10980. [Google Scholar] [CrossRef]
- Brown, C.L.; Perrin, E.M. Defining picky eating and its relationship to feeding behaviors and weight status. J. Behav. Med. 2020, 43, 587–595. [Google Scholar] [CrossRef]
- FDA. Coronavirus (COVID-19) Update: FDA Authorizes Moderna, Pfizer-BioNTech Bivalent COVID-19 Vaccines for Use as a Booster Dose. 2022. Available online: https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-fda-authorizes-moderna-pfizer-biontech-bivalent-covid-19-vaccines-use (accessed on 21 January 2023).
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef]
- Schumacker, R.E.; Lomax, R.G. A Beginner’s Guide to Structural Equation Modeling, 3rd ed.; Routledge: New York, NY, USA, 2010. [Google Scholar]
- Tavakol, M.; Dennick, R. Making sense of Cronbach’s alpha. Int. J. Med. Educ. 2011, 2, 53–55. [Google Scholar] [CrossRef]
- R: A Language and Environment for Statistical Computing. Available online: https://www.r-project.org/ (accessed on 9 March 2022).
- Rosseel, Y. lavaan: An R Package for Structural Equation Modeling. J. Stat. Softw. 2012, 48, 2. [Google Scholar] [CrossRef]
- Betsch, C.; Schmid, P.; Heinemeier, D.; Korn, L.; Holtmann, C.; Böhm, R. Beyond confidence: Development of a measure assessing the 5C psychological antecedents of vaccination. PLoS ONE 2018, 13, e0208601. [Google Scholar] [CrossRef]
- Al-Sanafi, M.; Sallam, M. Psychological Determinants of COVID-19 Vaccine Acceptance among Healthcare Workers in Kuwait: A Cross-Sectional Study Using the 5C and Vaccine Conspiracy Beliefs Scales. Vaccines 2021, 9, 701. [Google Scholar] [CrossRef]
- Geiger, M.; Rees, F.; Lilleholt, L.; Santana, A.P.; Zettler, I.; Wilhelm, O.; Betsch, C.; Böhm, R. Measuring the 7Cs of Vaccination Readiness. Eur. J. Psychol. Assess. 2022, 38, 261–269. [Google Scholar] [CrossRef]
- Link-Gelles, R.; Levy, M.E.; Gaglani, M.; Irving, S.A.; Stockwell, M.; Dascomb, K.; DeSilva, M.B.; Reese, S.E.; Liao, I.C.; Ong, T.C.; et al. Effectiveness of 2, 3, and 4 COVID-19 mRNA Vaccine Doses Among Immunocompetent Adults During Periods when SARS-CoV-2 Omicron BA.1 and BA.2/BA.2.12.1 Sublineages Predominated—VISION Network, 10 States, December 2021–June 2022. MMWR Morb. Mortal. Wkly. Rep. 2022, 71, 931–939. [Google Scholar] [CrossRef] [PubMed]
- Razzaghi, H.; Srivastav, A.; de Perio, M.A.; Laney, A.S.; Black, C.L. Influenza and COVID-19 Vaccination Coverage Among Health Care Personnel—United States, 2021–22. MMWR Morb. Mortal. Wkly. Rep. 2022, 71, 1319–1326. [Google Scholar] [CrossRef] [PubMed]
- Centers for Medicare & Medicaid Services Data. Available online: https://data.cms.gov/covid-19/covid-19-nursing-home-data (accessed on 21 January 2023).
- Chou, W.Y.S.; Budenz, A. Considering Emotion in COVID-19 Vaccine Communication: Addressing Vaccine Hesitancy and Fostering Vaccine Confidence. Health Commun. 2020, 35, 1718–1722. [Google Scholar] [CrossRef]
- Kaim, A.; Siman-Tov, M.; Jaffe, E.; Adini, B. Effect of a Concise Educational Program on COVID-19 Vaccination Attitudes. Front. Public Health 2021, 9, 767447. [Google Scholar] [CrossRef]
- Li, P.C.; Theis, S.R.; Kelly, D.; Ocampo, T.; Berglund, A.; Morgan, D.; Markert, R.; Fisher, E.; Burtson, K. Impact of an Education Intervention on COVID-19 Vaccine Hesitancy in a Military Base Population. Mil. Med. 2022, 187, e1516–e1522. [Google Scholar] [CrossRef]
- Evans, C.T.; DeYoung, B.J.; Gray, E.L.; Wallia, A.; Ho, J.; Carnethon, M.; Zembower, T.R.; Hirschhorn, L.R.; Wilkins, J.T. Coronavirus disease 2019 (COVID-19) vaccine intentions and uptake in a tertiary-care healthcare system: A longitudinal study. Infect. Control. Hosp. Epidemiol. 2021, 43, 1806–1812. [Google Scholar] [CrossRef]
- Hornsey, M.J.; Fielding, K.S. Attitude roots and Jiu Jitsu persuasion: Understanding and overcoming the motivated rejection of science. Am. Psychol. 2017, 72, 459–473. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).