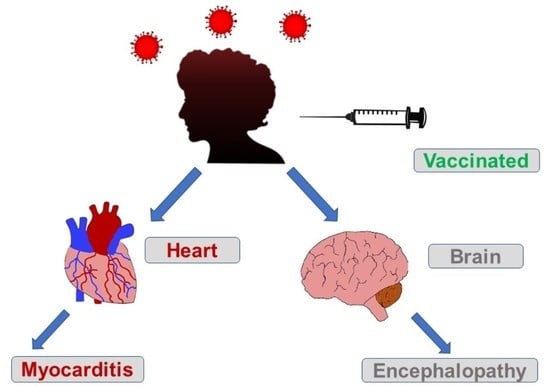
A Rare Single Case of COVID-19-Induced Acute Myocarditis and Encephalopathy Presenting Simultaneously
Abstract
Share and Cite
Saeedullah, U.; Abbas, A.M.; Ward, C.; Bayya, M.; Bhandari, J.; Abbas, A.M.; DeLeon, J.; Reiss, A.B. A Rare Single Case of COVID-19-Induced Acute Myocarditis and Encephalopathy Presenting Simultaneously. Vaccines 2023, 11, 541. https://doi.org/10.3390/vaccines11030541
Saeedullah U, Abbas AM, Ward C, Bayya M, Bhandari J, Abbas AM, DeLeon J, Reiss AB. A Rare Single Case of COVID-19-Induced Acute Myocarditis and Encephalopathy Presenting Simultaneously. Vaccines. 2023; 11(3):541. https://doi.org/10.3390/vaccines11030541
Chicago/Turabian StyleSaeedullah, Usman, Anas M. Abbas, Caitlin Ward, Maha Bayya, Jenish Bhandari, Araf M. Abbas, Joshua DeLeon, and Allison B. Reiss. 2023. "A Rare Single Case of COVID-19-Induced Acute Myocarditis and Encephalopathy Presenting Simultaneously" Vaccines 11, no. 3: 541. https://doi.org/10.3390/vaccines11030541
APA StyleSaeedullah, U., Abbas, A. M., Ward, C., Bayya, M., Bhandari, J., Abbas, A. M., DeLeon, J., & Reiss, A. B. (2023). A Rare Single Case of COVID-19-Induced Acute Myocarditis and Encephalopathy Presenting Simultaneously. Vaccines, 11(3), 541. https://doi.org/10.3390/vaccines11030541