Abstract
Currently, the best method to well control the spread of COVID-19 without severe mental health problems is to reach herd immunity. Therefore, the vaccination rate of the COVID-19 vaccine is critical. Among the populations, children are the vulnerable ones to get vaccinated; therefore, it is important to assess parents’ and guardians’ willingness to have their children vaccinated. The present systematic review and meta-analysis synthesized evidence to estimate the parents’ acceptance rate of COVID-19 vaccination toward their children. Additionally, factors explaining the acceptance rate were investigated. Four academic databases (PubMed, Scopus, Web of Science, and ProQuest) together with Google Scholar were searched, and the references of the included publications were searched as well. Using the PECO-S framework (population, exposure, comparison, outcome, and study design), observational studies of cross-sectional, cohort, or case-control studies were included. The outcome was parents’ or guardians’ willingness to let their children be vaccinated. The studies included in the present review were restricted to English and peer-reviewed papers published between December 2019 and July 2022. A total of 98 papers across 69 different countries with 413,590 participants were included. The mean age of the parents was 39.10 (range: 18–70) years and that of their children was 8.45 (range: 0–18) years. The pooled estimated prevalence of parental acceptance to vaccinate their children with the COVID-19 vaccine was 57% (98 studies, 95% CI: 52–62%, I2: 99.92%, τ2: 0.06). Moreover, data collection time was a significant factor explaining parental willingness in the multivariable meta-regression, with a 13% decrease in parental willingness by each month increase in time, explaining 11.44% of variance. Qualitative synthesis results showed that parents’ COVID-19 vaccine knowledge, trust in theCOVID-19 vaccine, and facilitators in vaccination (e.g., low cost, good vaccine accessibility, and government incentive) were significant factors for higher willingness, while mental health problems (e.g., having worries and psychological distress) were significant factors for lower willingness. Given that the acceptance rate was relatively low (57%) and does not achieve the requirement of herd immunity (i.e., 70%), governments and healthcare authorities should try to elevate parents’ knowledge and trust in the COVID-19 vaccine, facilitate in vaccination, and reduce their mental difficulties to improve the overall vaccination rate among children.
1. Introduction
On 11 March 2020, WHO declared COVID-19 as a global pandemic, which has led to serious disruptions in the economy and society [1,2,3,4,5,6]. Based on the WHO COVID-19 dashboard, as of 31 January 2023, there have been 753,479,439 confirmed cases of COVID-19, including 6,812,798 deaths, globally [7]. Although the control of human movement, including travel restrictions and quarantine, is an effective containment and mitigation strategy for COVID-19, it can lead to psychological problems and a significant social and economic burden [8,9]. Lack of motivation to follow recommendations, resulting from long-term public health measures and restrictions, may contribute to the resurgence of COVID-19 cases [10]. Various physical measures such as wearing masks and social distancing have been implemented to contain the spread of this virus. For children, reducing time in school (e.g., campus closure with online learning at home) has been the primary approach [11]. However, social isolation has negative effects on children’s mental health [12].
In order to overcome the limitations of school time reduction during the pandemic, immunization seems to be the safest and most cost-effective health intervention implemented throughout history, saving millions of lives annually [13,14]. To date, immunization programs against several infectious diseases have been successfully implemented worldwide and have been able to control diseases such as smallpox, polio, diphtheria, pertussis, and rubella [15]. Vaccination is the key to reducing the incidence of COVID-19, which enables children to continue their daily activities [16]. Due to the emergence of some new types of highly transmissible COVID-19 strains, different parties (including the scientists, healthcare providers, and governments) acknowledge the importance of high vaccination uptake for herd immunity [17,18,19], which would reduce the effect of the vaccine on transmission, pathogenicity, and hospitalization rates associated with COVID-19 [20,21]. Therefore, willingness to be vaccinated plays a key role in government vaccination calls to slow down the spread of the virus [22]. However, vaccination hesitancy, which according to the World Health Organization (WHO) poses a threat to global health, has become a significant issue during the COVID-19 pandemic [23,24,25]. In a recent systematic review of 31 peer-reviewed papers, different acceptance rates of COVID-19 vaccination among the general population were reported from 23.6% to 97% across different countries [26,27]. In another narrative review, data regarding COVID-19 vaccine acceptance rate were collected from surveys in 114 countries/territories. Acceptance rates ≥60% were seen in 72/114 countries/territories, with 42 countries/territories having rates between 13% and 59% [28]. Additionally, different acceptance rates at a national level were reported in one recent systematic review in the US: 12 to 91.4% acceptance rate [29]. Factors such as educational qualification, compliance with preventive measures related to COVID-19, age, gender, source of information related to COVID-19, history of influenza vaccination, inefficient government efforts and initiatives, and trust in the government are among the factors affecting the enthusiasm for vaccination against COVID-19 [27,30,31,32,33,34].
Vaccination in children often requires the consent of their parents or guardians [35]. To facilitate the implementation of the COVID-19 vaccine among children, it is thus important to understand parental acceptance of their children’s COVID-19 vaccination and the associated barriers and facilitators. However, current research suggests that parental compliance and influencing factors vary considerably across studies. For example, a systematic review of 44 studies involving 317,055 parents found that the overall proportion of parents planning to vaccinate their children against COVID-19 was 60.1% with heterogeneity ranging from 25.6 to 92.2% [36]. Similar variations were reported in another systematic review including 29 studies from 16 countries and regions with 68,327 participants [37], showing that vaccination willingness could be as high as 91.4% [38] or as low as 21.6% [39].
The purpose of this study is to investigate the prevalence and factors affecting the acceptance of the COVID-19 vaccine for children under legal age among their parents. Specifically, the present study investigated children’s vaccination attitudes, whether their parents have been vaccinated against COVID-19, parents’ age, etc. According to our literature review, prior systematic review and meta-analysis studies did not consider the diverse subgroups when synthesizing data to examine the variables related to the acceptance of the COVID-19 vaccine, especially for children. Moreover, the latest studies recommend new vaccines against COVID-19 for children and adolescents [40,41], which results in difficult decision making for parents and caregivers to vaccinate their children. For this reason, the aim of the current research was to draw a comprehensive and related picture of various factors and attitudes related to this decision. The information obtained will help to provide a better understanding for further research as well as for health authorities and professionals to respond to potential problems in an adequate and targeted manner.
Study Aims
This study aimed primarily to estimate the prevalence of parental acceptance/willingness to vaccinate their children with the COVID-19 vaccine. The secondary aims were:
- Assessment of heterogeneity and its possible sources for estimated pooled prevalence of parental acceptance/willingness to vaccinate their children with the COVID-19 vaccine;
- Moderator analyses to determine influential variables sources for estimated pooled prevalence of parental acceptance/willingness to vaccinate their children with the COVID-19 vaccine;
- Determining influential factors for parents to accept COVID-19 vaccination for their children.
2. Materials and Methods
2.1. Protocol and Registration
The study protocol was registered in the PROSPERO, International prospective register of systematic reviews under decree code of CRD42022333337 [42]. The findings of this systematic review are reported based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) reporting guideline [43].
2.2. Systematic Review Questions
The systematic review question was formulated using PECO-S framework. The PECO-S is a framework to formulate search questions assessing associations between exposures and outcomes in various fields of health [44]. The PECO components are P for Population, E for Exposure, C for Comparison, O for Outcome, and S for Study design. The present study was designed to answer the following main research question:
What is the worldwide estimated prevalence of parental acceptance to vaccinate their children with the COVID-19 vaccine?
2.3. Eligibility Criteria
The eligibility criteria based on PECO components were set as follows: (1) Population: parents or children’s guardian with no limitation regarding their demographic characteristics; (2) Exposure: COVID-19 pandemic; (3) Comparison: other populations other than children; (4) Outcome: Frequency or prevalence of COVID-19 vaccination acceptance (and/or no hesitance) or willingness to receive COVID-19 vaccines for children; and (5) Study design: observational studies including cross sectional, cohort, or case-control design.
Other eligibility criteria include being published between December 2019 and July 2022, using English language, published as a peer-reviewed paper, reporting data on frequency or prevalence of parents or children’s guardian acceptance for their children’s COVID-19 vaccination.
2.4. Information Sources
Academic databases including PubMed, Scopus, Web of Science (WoS), and ProQuest were systematically searched from the beginning of December 2019 to the end of July 2022. To have a more comprehensive search, reference lists of the included publications and medRxiv were independently searched.
2.5. Search Strategy
The main search terms included COVID-19, vaccine, parents, and children. The search strategy was developed using Boolean operators (AND, OR). The advanced search attributes of each database were considered and customizing the search syntax was adapted.
2.6. Study Selection
In the first step, the title and abstract of all retrieved papers during the electronic and manual search processes were evaluated based on the inclusion criteria. This was followed by examination of the full texts of the potentially relevant articles based on the above-mentioned criteria. These processes were performed independently by two reviewers. Initial disagreements about the selection of studies were resolved through discussions.
2.7. Data Collection Process and Data Items
Data were extracted and recorded in pre-designed Excel datasheets by two reviewers independently. The following data were abstracted from each study: first-author name; country in which the study had been conducted as well as its income level and development status based on World Bank data; sample size; data collection date; parents and children ages; country location based on WHO regions; type of study; quality of study; and raw data to calculate prevalence of parents’ willingness of their children to be vaccinated against COVID-19.
2.8. Risk of Bias in Individual Studies
The Newcastle–Ottawa Scale (NOS) was used to assess risk of bias within included studies. This checklist evaluates the methodological quality of observational studies in the following three sections: selection, comparability, and outcome [45,46]. The maximal acquirable score on the NOS checklist is 9 for each study. Studies with less than five points were classified as having a high risk of bias [45]. Methodological quality status was not considered as an eligibility criterion. However, the effect of methodological quality on the pooled effect size was assessed in the subgroup analysis and meta-regression.
2.9. Summary Measures and Data Synthesis
The selected summary measure of the present study for meta-analysis was the frequency or prevalence of the acceptance of the COVID-19 vaccine and their 95% confidence intervals (CIs). Numerical evidence regarding the prevalence of the COVID-19 vaccine acceptance was quantitatively synthesized using STATA software version 14. Meta-analysis using a random-effects model was conducted to consider both within-study and between-study variances [47]. Severity of heterogeneity was estimated using the I2 index [48].
Contributing factors influencing acceptance of COVID-19 vaccines were pooled using a meta-synthesis approach due to methodological heterogeneity of variables and measures.
2.10. Risk of Bias across Studies
Funnel plot and Begg’s test were used to assess publication bias [49]. Meta-trim with the fill and trim method was used to correct probable publication bias [50]. The Jackknife method was used for sensitivity analysis and probable single study effect on pooled effect size [51].
2.11. Additional Analyses
To investigate moderators for COVID-19 vaccine acceptance, subgroup analysis and meta-regression were conducted.
3. Results
3.1. Study Screening and Selection Process
The initial search in four academic databases as well as Google Scholar resulted in retrieval of 8816 records: PubMed (n = 2553); Scopus (n = 1538); WoS (n = 1664); and ProQuest (n = 3061). After removing duplicates (n = 2986), the remaining manuscripts were screened based on their titles and abstracts. Finally, 145 papers appeared to be potentially eligible and their full texts were reviewed. In this process, 98 studies were pooled in the meta-analysis. The search process based on the PRISMA flowchart is illustrated in Figure 1.
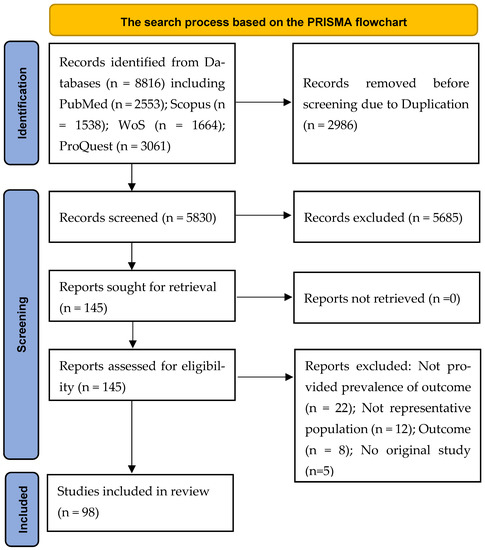
Figure 1.
The search process based on the PRISMA flowchart. A total of 98 studies were finally included in the present systematic review and meta-analysis.
3.2. Description of the Included Studies
Ninety-eight studies comprised 413,590 participants from 69 different countries (Albania, Aruba, Argentina, Antigua and Barbuda, Australia, Bahamas, Bangladesh, Belize, Bolivia, Brazil, Barbados, Canada, China, Chile, Colombia, Costa Rica, Cuba, Cayman Islands, Dominica, Dominican Republic, Ecuador, El Salvador, England, Germany, Greece, Grenada, Guatemala, Guyana, Haiti, Honduras, Hong Kong, India, Iraq, Israel, Italy, Jamaica, Japan, Jordan, Korea, México, New Zealand, Nicaragua, Panama, Paraguay, Peru, Philippines, Poland, Puerto Rico, Qatar, Russia, Saint Maarten, Saudi Arabia, Singapore, South Africa, Spain, St. Kitts and Nevis, St. Lucia, St. Vincent and the Grenadines, Switzerland, Suriname, Taiwan, Trinidad and Tobago, Turkey, Turks and Caicos Isl., UK, USA, Uruguay, Venezuela, Virgin Islands) were included. The highest number of studies were, respectively, conducted in AMR region (Americas; 27 studies), EUR region (Europe; 24 studies), WPR region (Western Pacific; 23 studies), EMR region (Eastern Mediterranean; 17 studies) and SEAR (South-East Asia; 5 studies). Three studies were conducted as multi-country studies. Half of the studies (49 out of 98) were conducted in developed countries with high income (61 out of 98). The smallest sample size was 50 (from the U.S.), and the largest sample size was 227,740 (from Latin America and the Caribbean). Most study respondents (68.1%) were mothers. The mean age of parents was 39.10 (range between 18 and 70 years) and that of their children was 8.45 years (range between 0 and 18 years). Almost all studies used a cross-sectional design, with only two studies adopting a longitudinal design. The first study was conducted during February 2020 in China and the last one was conducted during January 2022 in Saudi Arabia. Table 1 provides the summary characteristics of all included studies.

Table 1.
Summarized characteristics of included studies.
3.3. Methodological Quality Appraisal
Most studies (58 out of 98) were categorized as being low-quality (or high risk of bias) studies. The total score of methodological quality is provided in (Table 1), with details in (Figure 2). The main methodological problems were: (1) description of the response rate or the characteristics of the responders and the non-responders not having been reported (94 out of 98 studies); (2) explanation regarding sample size estimation and justification not having been reported (74 out of 98 studies).
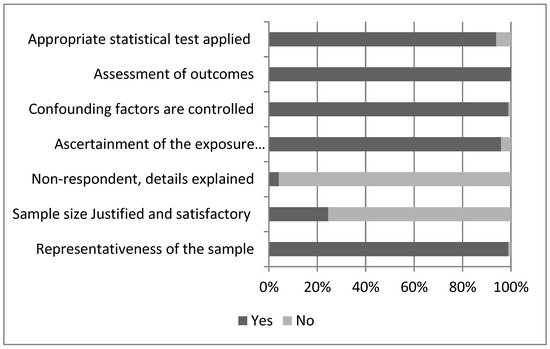
Figure 2.
Details of the methodological quality appraisal of the included studies. In total, 58 of 98 studies were categorized as being low quality.
3.4. Pooled Prevalence of COVID-19 Vaccine Willingness
The pooled estimated prevalence of parental acceptance to vaccinate their children with COVID-19 vaccine was 57% (98 studies, 95% CI: 52–62%, I2: 99.92%, τ2: 0.06). Figure 3 provides the forest plot regarding the pooled prevalence of parental acceptance to vaccinate their children with the COVID-19 vaccine.
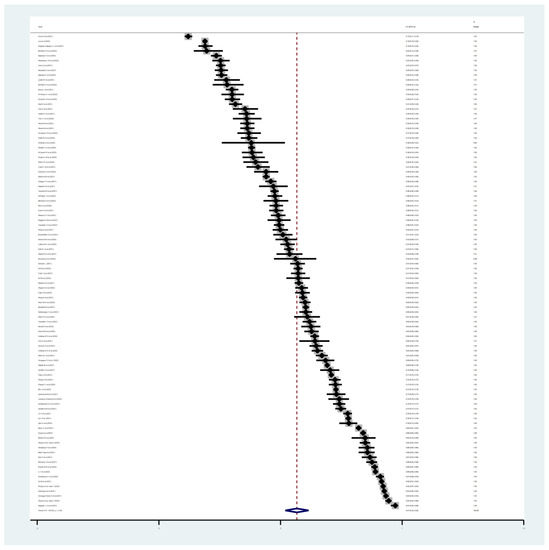
Figure 3.
The forest plot of pooled prevalence of parental acceptance to vaccinate their children with the COVID-19 vaccine. The pooled estimated prevalence of parental acceptance to vaccinate their children with the COVID-19 vaccine was 57%.
The probability of publication bias was assessed using Begg’s test (p < 0.001) and funnel plot. Based on the asymmetric funnel plot (Figure 4), publication bias seems probable. The fill-and-trim method was used to correct probable publication bias, but no study was imputed, and publication bias was ruled out. Sensitivity analysis (based on the one-out or Jack-knife method) showed that the pooled effect size was not affected by a single-study effect.
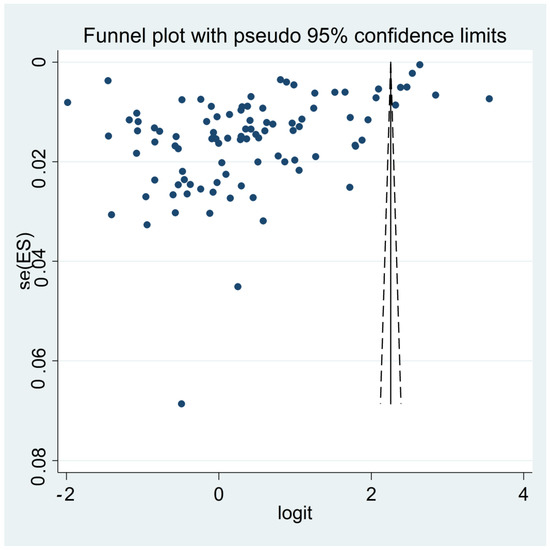
Figure 4.
The funnel plot assessing publication bias among included studies reporting pooled prevalence of parental acceptance to vaccinate their children with COVID-19 vaccine. Publication bias seems probable.
3.5. Predictor Variables of Parental Willingness
Predictors of COVID-19 vaccine willingness were assessed using subgroup analysis (Table 2) and univariable and multivariable meta-regression (Table 3 and Table 4). Country income level, country location in WHO’s regions (i.e., AMR, EUR, WPR, EMR, and SEAR), and data collection method were significant moderators (p = 0.01) of parents’ willingness to vaccinate their children with the COVID-19 vaccine. High-income countries had the lowest prevalence of parental willingness (52%) compared to low- and upper-intermediate-income countries (62 and 65%, respectively). The lowest prevalence of parental willingness was observed in countries located in EMR compared to other regions (45% in EMR vs. 58% in AMR, 62% SEAR, 52% EUR, and 67% WPR). Data collection method was another significant variable influencing the pooled estimated parental willingness (p = 0.02). Studies collected data using phone interview had the lowest prevalence of willingness (35%). In the uni-variable meta-regression, data collection time was the only significant variable (p = 0.001) in predicting parental willingness. Multivariable meta-regression revealed that both data collection time (13% decrease in willingness by each increase in month) and country income level (7% decrease by increasing level of country income) were only significant predictors of parental willingness, which explained 11.44% of variance. None of the examined variables affect the heterogeneity.

Table 2.
Subgroup analyses.

Table 3.
Results of uni-variable meta-regression regarding estimated pooled prevalence.

Table 4.
Results of multivariable meta-regression.
3.6. Contributing Factors of Parental Willingness
Two main categories of contributing factors (i.e., family-related factors and vaccine-related factors) were identified among included studies using a qualitative synthesized approach.
3.6.1. Family Related Contributing Factors
Parent self-vaccination [54,64,90,92,101,113,117,119,120,122,125,127,128,132,134,136] or their willingness for self-vaccination [65,76,77,86,88,92,98,103,125,127,129] showed positive association with parents’ willingness to vaccinate their children in almost all studies. Just one study reported that among participants vaccinated against COVID-19, only 29.0% were willing to vaccinate their children [80].
History of COVID infection in parents, children, or family members did not have consistent results among included studies, showing positive association [113,120,127,135], negative association [100,116], or no significant difference [87,88].
Parents’ age showed associations with their willingness to vaccinate their children. In most studies [38,52,58,62,65,74,86,87,98,110,113,116,119,123,124,125,131,133,135,139], parents with older age showed more willingness, while some inconsistent results were reported regarding higher vaccination hesitation among older parents [75,79,80].
Mothers showed more hesitancy regarding their children’s vaccination compared to fathers in almost all studies [52,57,68,75,79,91,92,93,98,106,116,133]; however, mothers also had higher willingness than fathers to vaccinate their children [83,88,105,115,120], although a few studies found no difference between mothers and fathers [87,130].
Source of information regarding the vaccine influenced parents’ decision for their children’s vaccination. When they received information from healthcare providers, physicians, or pediatrics, they reported more willingness to vaccinate their children [59,80,84,96,99,128,134,136]. Social media played different roles. In most studies, participants reported that social media and exposure to negative information increased parent hesitancy regarding vaccination [75,93,94,105,106], while some others reported a positive influence of social media for increasing parent acceptance [66,70].
Parents reported more willingness to vaccinate children if their children are older [57,75,90,99,100,108,111,118,119,124,125,134,135,138,139].
Parents with a higher number of children reported inconsistent decisions regarding willingness to accept their children’s vaccination. A higher number of children was associated with less willingness in some studies [38,55,87,105,108], higher willingness in other studies [99,102], or no difference in one study [88].
Parents’ higher levels of stress, anxiety, and psychological distress were associated with less intention for children’s vaccination [53,78,89,113]. Only one study reported that higher vaccine acceptability was associated with higher levels of anxiety regarding COVID-19 infection [142].
Parents’ education level showed inconsistent results in association with parental willingness for children’s vaccination. Some studies showed positive association of parents’ higher level of education with vaccination willingness [38,54,58,59,62,75,76,79,87,89,90,91,93,98,110,126,134], while others reported negative [52,74,84,113,116,119,137] or null [88] association.
Parents’ higher economic status showed positively higher association with parents’ willingness to vaccinate their children in almost all included studies [38,54,55,59,77,80,87,88,89,93,95,96,97,98,111,113,125], with only two studies reporting lower vaccination intention among lower income parents [52,137].
Parents having chronic conditions reported higher prevalence of vaccination willingness for their children in three studies [83,113], while lower willingness [57] and no difference [87] each was reported in one study. Additionally, parents whose children have a history of adverse vaccine reactions and allergies were less willing to vaccinate their children [52].
Parents living in rural and sub-urban areas showed less willingness compared to those in urban areas [105,113,125], except for one study reporting higher willingness of rural parents [52].
3.6.2. Vaccine Related Factors
Parents reported more children’s vaccination willingness when they believe that children vaccination is necessary to halt the pandemic and to reach a better national economic situation [65,70,72,77,83,86,97,103,115,120].
Worry about vaccine safety and its potential adverse effect [56,59,64,65,67,70,72,76,77,81,85,86,90,91,92,94,95,98,101,103,105,112,115,116,118,121,126,127,128,131,132,133,140,142], novelty of vaccine and its’ short development time [57,101,116], and hesitancy regarding vaccine’s efficacy and benefits [56,59,66,70,71,72,74,76,92,94,101,105,115,117,118,122,126,128,131,132,133] were among the main predictors of vaccination hesitation of parents. When they perceived more worry about the vaccine’s adverse effect and hesitation regarding its’ efficacy, they preferred not to vaccinate their children.
Cost of vaccine [56,59,73], vaccine accessibility [59,63,101,123,141], and governmental incentive of giving a green pass after vaccination [101,123] were among of contributing factors for parents’ decision-making for their willingness to vaccinate their children.
Trust in the COVID-19 vaccine [59,98,121,126,128,142], trust in governments [104,121], and trust to health system [60,63,72,80,89] were also contributing factors.
Parents who reported more positive attitudes/beliefs toward vaccination [65,83,86,87,107,109] and who had more knowledge on vaccines (vaccine literacy) [58,61,65,79,83,86,88,89,97,108,109,110,121,139,142] had more willingness to vaccinate their children.
Obtaining influenza immunization was a positive contributing factor for parents to accept their children’s COVID-19 vaccination [57,59,65,68,77,86,104,116,121,140].
Parents who perceived the risk of COVID-19 transition from children to adults [60,106,118] and who perceived risk of children’s infection and being hospitalized because of COVID-19 [59,92,99,106,115,118,121,127,128,134] reported more willingness to vaccinate their children.
Comparisons between domestic and foreign vaccine preference have been investigated in very few studies, and domestic vaccines were preferred by parents for themselves and their children [56,142].
4. Discussion
In order to provide thorough estimation regarding parents’ willingness to have their children vaccinated, the present systematic review and meta-analysis synthesized data from studies published between December 2019 and July 2022 (98 papers). Apart from using meta-analysis to quantitatively synthesize parents’ acceptance rate of having children vaccinated, quantitative (i.e., meta-regression and subgroup analysis) and qualitative approaches have been used to synthesize the factors explaining parents’ willingness on their children’s vaccination. The synthesized results showed that the pooled estimated rate of parents’ willingness was 57% (95% CI = 52–62%). The low willingness to let children get vaccinated concurs with prior results reported by meta-analysis: 60.1% [32]. Although the present meta-analysis also revealed high heterogeneity (I2 > 90%) as similar to previous meta-analyses [32,33], the 95% CI in the present meta-analysis was narrower (52–62% vs. 25.6–92.2% and 21.6–91.4%). Nevertheless, the parents generally had low willingness to let their children get vaccinated. Consequently, it is important to know the potential reasons increasing or decreasing parents’ willingness to let their children get vaccinated. Apart from the quantitative finding, qualitative synthesis in the present review showed that the positive factors on parents’ willingness to vaccinate their children were knowledge on the COVID-19 vaccine, trust in the COVID-19 vaccine, and facilitators in vaccination (e.g., low cost, good vaccine accessibility, and government incentive); negative factors were parents’ mental difficulties, including worries, anxiety, and psychological distress.
Although having similar point-estimation in the parents’ willingness to have their children vaccinated, the present systematic review and meta-analysis had a narrower 95% CI than the two previous systematic review and meta-analyses [36,37]. A potential reason is that the papers included in their meta-analyses [36,37] were fewer than the present one, which resulted in an unstable estimation in the 95% CI. Specifically, Galanis et al. reviewed 44 papers [36] and Chen et al. reviewed 29 papers [37], while the present systematic review and meta-analysis reviewed 98 papers. With a double-size reviewed papers, the present systematic review and meta-analysis is likely to have a more precise estimation in the acceptance rate, especially in the interval-estimation.
Data collection time was a significant factor explaining dropped willingness (13% decreased by each month increased). This can be explained by risk compensation [143,144] and diffusion of responsibility with bystander effect [145,146]. It seems that when time progresses and the percent of vaccinated people increases, parents may feel safe not to let their children get COVID-19 vaccinated as other people have already been vaccinated. This point was pointed in regression analysis based on percent of vaccinated people in countries’ national level, which showed that each increased percent in percent of vaccinated people contributes to a 1% decrease in parental willingness. In other words, parents feel that the risk of COVID-19 infection for their children is decreased and they would not like to let their children vaccinated as a type of risk compensation [143,144]. Additionally, when the vaccination rate increases, parents may feel their responsibility of letting their children get vaccinated decreased, which is a phenomenon of diffusion of responsibility and bystander effect [145,146].
Although the parents’ willingness to have their children vaccinated, it is important to maintain the vaccination rate across time to adhere to the herd immunity. That is, a decreased vaccination rate may cause another wave of COVID-19 outbreak as documented in the literature. Therefore, governments and health authorities should have appropriate methods to maintain willingness of having children vaccinated among parents. The present systematic review and meta-analysis used the qualitative synthesis to find the importance of parents’ COVID-19 vaccine knowledge, trust in COVID-19 vaccine, and facilitators in vaccination (e.g., low cost, good vaccine accessibility, and government incentive) to improve their willingness to have children vaccinated. Moreover, mental health problems (e.g., having worries and with high levels of psychological distress) might reduce parents’ willingness to have their children vaccinated. Therefore, government and healthcare authorities should consider building campaigns on COVID-19 vaccine knowledge improvement, COVID-19 vaccine support systems, and psychological distress reduction to elevate the parents’ willingness to have their children vaccinated.
Strengths and Limitations
The strengths of the present systematic review and meta-analysis included (i) a comprehensive search of the literature across WHO-defined regions (i.e., included AMR, EUR, WPR, EMR, and SEAR) to cover different ethnic and country populations; (ii) the use of robust methodology in reviewing papers (i.e., using the NOS checklist to evaluate each paper’s methodological quality; applying subgroup analysis and meta-regression to examine the moderator effects on parents’ willingness of having children vaccinated); (iii) synthesized findings from both quantitative and qualitative approaches to identify all potential factors explaining parents’ willingness of having children vaccinated.
There are some limitations in the present systematic review and meta-analysis. First, the COVID-19 pandemic had different severities and progresses across the studied papers because different countries controlled the COVID-19 pandemic with different situations. Therefore, it is hard to control this important confounder when cumulating the empirical data across countries worldwide. Most of the studies did not report data regarding the time window between vaccines availability at national level or time of vaccine approval for different age groups and collecting the data. Second, almost all papers analyzed in the present systematic review and meta-analysis did not use a standardized instrument assessing willingness to children’s vaccination. Subsequently, there might have been some measurement biases across the analyzed papers. Third, over half of the papers were at high risk of bias and the findings of the present systematic review and meta-analysis could be affected by the high risk of bias. Therefore, additional studies with low risk of bias are needed to further investigate the issue regarding parents’ willingness to have their children vaccinated. Fourth, although the present systematic review and meta-analysis had sought several academic databases (e.g., PubMed) and Google Scholar, the Google’s search engine was not used to search for potential grey literature. Therefore, it is possible that some relevant articles might not be included in the present systematic review and meta-analysis. Lastly, the following important information was not able to retrieve from the analyzed studies in the present systematic review and confounded the present findings: definitions of children (and the actual age ranges used for the analyzed studies); available vaccine (brands or types); and the vaccination procedure (e.g., whether the vaccines have been politicized in other countries as they have been in the US).
5. Conclusions
In conclusion, the present systematic review and meta-analysis updates the current understanding of parents’ willingness and hesitancy of letting their children get vaccinated. The willingness of the parents was generally low (mean acceptance rate: 57%; 95% CI: 52–62%), although it was highly heterogeneous (I2 = 99.92%). Moreover, time appeared to be the primarily significant factor explaining high levels of acceptance. Qualitative synthesized results showed that parents’ knowledge on COVID-19 vaccine, trust in COVID-19 vaccine, and facilitators in vaccination (e.g., low cost, good vaccine accessibility, and government incentive) could improve parents’ acceptance of children vaccination. In contrast, parents’ mental difficulties (e.g., having worries and psychological distress) were barriers to improve their willingness.
Author Contributions
Conceptualization, Z.A. and A.H.P.; methodology, Z.A. and A.H.P.; software, Z.A.; validation, A.H.P.; formal analysis, Z.A.; investigation, Z.A.; data curation, A.H.P.; writing—original draft preparation, Z.A.; writing—review and editing, A.H.P. and C.-Y.L.; supervision, Z.A.; project administration, Z.A.; funding acquisition, Z.A. and A.H.P. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Qazvin University of Medical Sciences, grant number 1401.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable as the study is a systematic review.
Data Availability Statement
Data will be available via email to corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Liu, E.; Arledge, S. Individual characteristics and demographics associated with mask wearing during the COVID-19 pandemic in the United States. Asian J. Soc. Health Behav. 2022, 5, 3–9. [Google Scholar] [CrossRef]
- Prasiska, D.; Muhlis, A.; Megatsari, H. Effectiveness of the emergency public activity restrictions on COVID-19 epidemiological parameter in East Java Province, Indonesia: An ecological study. Asian J. Soc. Health Behav. 2022, 5, 33–39. [Google Scholar] [CrossRef]
- Sandya, P.; Shetty, K.; Jaise, J.; Manikappa, S.; Pai, N. Stress and burden among caregivers of persons with bipolar affective disorder during the COVID-19 pandemic in India. Asian J. Soc. Health Behav. 2022, 5, 51–56. [Google Scholar] [CrossRef]
- Sangma, R.; Kumar, P.; Nerli, L.; Khanna, A.; Vasavada, D.; Tiwari, D. Social stigma and discrimination in Coronavirus Disease-2019 survivors and its changing trend: A longitudinal study at tertiary care center Gujarat, India. Asian J. Soc. Health Behav. 2022, 5, 68–74. [Google Scholar] [CrossRef]
- Soltani, R.; Shamsi, M.; Moradi, A. Do perceived barriers, benefits, and severity have effect on mask-wearing habits during the coronavirus disease-2019 pandemic? Asian J. Soc. Health Behav. 2022, 5, 186–192. [Google Scholar] [CrossRef]
- Vicerra, P.; Pano, J.; Estanislao, J. Nutrition status of lower-income older adults in Thailand during COVID-19 pandemic. Asian J. Soc. Health Behav. 2022, 5, 147–153. [Google Scholar] [CrossRef]
- WHO. WHO COVID-19 Dashboard. Available online: https://covid19.who.int/ (accessed on 31 January 2023).
- Bonaccorsi, G.; Pierri, F.; Cinelli, M.; Flori, A.; Galeazzi, A.; Porcelli, F.; Schmidt, A.L.; Valensise, C.M.; Scala, A.; Quattrociocchi, W. Economic and social consequences of human mobility restrictions under COVID-19. Proc. Natl. Acad. Sci. USA 2020, 117, 15530–15535. [Google Scholar] [CrossRef]
- Yee, A.; Hodori, N.A.M.; Tung, Y.-Z.; Ooi, P.-L.; Latif, S.A.B.A.; Isa, H.M.; Ng, D.-L.-C.; Chai, C.-S.; Tan, S.-B. Depression level and coping responses toward the movement control order and its impact on quality of life in the Malaysian community during the COVID-19 pandemic: A web-based cross-sectional study. Ann. Gen. Psychiatry 2021, 20, 31. [Google Scholar] [CrossRef]
- WHO. Pandemic Fatigue: Reinvigorating the Public to Prevent COVID-19: Policy Considerations for Member States in the WHO European Region. Available online: https://apps.who.int/iris/handle/10665/335820. (accessed on 24 January 2023).
- Auger, K.A.; Shah, S.S.; Richardson, T.; Hartley, D.; Hall, M.; Warniment, A.; Timmons, K.; Bosse, D.; Ferris, S.A.; Brady, P.W. Association between statewide school closure and COVID-19 incidence and mortality in the US. JAMA 2020, 324, 859–870. [Google Scholar] [CrossRef]
- Liu, J.J.; Bao, Y.; Huang, X.; Shi, J.; Lu, L. Mental health considerations for children quarantined because of COVID-19. Lancet Child Adolesc. Health 2020, 4, 347–349. [Google Scholar] [CrossRef]
- Hajj Hussein, I.; Chams, N.; Chams, S.; El Sayegh, S.; Badran, R.; Raad, M.; Gerges-Geagea, A.; Leone, A.; Jurjus, A. Vaccines through centuries: Major cornerstones of global health. Front. Public Health 2015, 3, 269. [Google Scholar] [CrossRef]
- Rodrigues, C.M.; Plotkin, S.A. Impact of vaccines; health, economic and social perspectives. Front. Microbiol. 2020, 11, 1526. [Google Scholar] [CrossRef]
- Andre, F.E.; Booy, R.; Bock, H.L.; Clemens, J.; Datta, S.K.; John, T.J.; Lee, B.W.; Lolekha, S.; Peltola, H.; Ruff, T. Vaccination greatly reduces disease, disability, death and inequity worldwide. Bull. World Health Organ. 2008, 86, 140–146. [Google Scholar] [CrossRef]
- Opel, D.J.; Diekema, D.S.; Ross, L.F. Should we mandate a COVID-19 vaccine for children? JAMA Pediatr. 2021, 175, 125–126. [Google Scholar] [CrossRef]
- Kotecha, I.; Vasavada, D.; Kumar, P.; Nerli, L.; Tiwari, D.; Parmar, D. Knowledge, attitude, and belief of health-care workers toward COVID-19 Vaccine at a tertiary care center in India. Asian J. Soc. Health Behav. 2022, 5, 63–67. [Google Scholar] [CrossRef]
- Nascimento, M.; Nunes, A.; Juchem, L. “I believe in science and in all vaccines:” Older adult and the intention for a vaccine against COVID-19. Asian J. Soc. Health Behav. 2022, 5, 108–114. [Google Scholar] [CrossRef]
- Rieger, M. Willingness to vaccinate against COVID-19 might be systematically underestimated. Asian J. Soc. Health Behav. 2021, 4, 81–83. [Google Scholar] [CrossRef]
- Araf, Y.; Akter, F.; Tang, Y.d.; Fatemi, R.; Parvez, M.S.A.; Zheng, C.; Hossain, M.G. Omicron variant of SARS-CoV-2: Genomics, transmissibility, and responses to current COVID-19 vaccines. J. Med. Virol. 2022, 94, 1825–1832. [Google Scholar] [CrossRef] [PubMed]
- Tregoning, J.S.; Flight, K.E.; Higham, S.L.; Wang, Z.; Pierce, B.F. Progress of the COVID-19 vaccine effort: Viruses, vaccines and variants versus efficacy, effectiveness and escape. Nat. Rev. Immunol. 2021, 21, 626–636. [Google Scholar] [CrossRef]
- Schoch-Spana, M.; Brunson, E.K.; Long, R.; Ruth, A.; Ravi, S.J.; Trotochaud, M.; Borio, L.; Brewer, J.; Buccina, J.; Connell, N. The public’s role in COVID-19 vaccination: Human-centered recommendations to enhance pandemic vaccine awareness, access, and acceptance in the United States. Vaccine 2021, 39, 6004–6012. [Google Scholar] [CrossRef]
- Bronstein, M.V.; Kummerfeld, E.; MacDonald III, A.; Vinogradov, S. Willingness to vaccinate against SARS-CoV-2: The role of reasoning biases and conspiracist ideation. Vaccine 2022, 40, 213–222. [Google Scholar] [CrossRef] [PubMed]
- Geoghegan, S.; O’Callaghan, K.P.; Offit, P.A. Vaccine safety: Myths and misinformation. Front. Microbiol. 2020, 11, 372. [Google Scholar] [CrossRef] [PubMed]
- Luo, C.; Chen, A.; Cui, B.; Liao, W. Exploring public perceptions of the COVID-19 vaccine online from a cultural perspective: Semantic network analysis of two social media platforms in the United States and China. Telemat. Inform. 2021, 65, 101712. [Google Scholar] [CrossRef] [PubMed]
- Sallam, M. COVID-19 Vaccine Hesitancy Worldwide: A Concise Systematic Review of Vaccine Acceptance Rates. Vaccines 2021, 9, 160. [Google Scholar] [CrossRef]
- Shakeel, C.S.; Mujeeb, A.A.; Mirza, M.S.; Chaudhry, B.; Khan, S.J. Global COVID-19 Vaccine Acceptance: A Systematic Review of Associated Social and Behavioral Factors. Vaccines 2022, 10, 110. [Google Scholar] [CrossRef]
- Sallam, M.; Al-Sanafi, M.; Sallam, M. A Global Map of COVID-19 Vaccine Acceptance Rates per Country: An Updated Concise Narrative Review. J. Multidiscip. Healthc. 2022, 15, 21–45. [Google Scholar] [CrossRef] [PubMed]
- Yasmin, F.; Najeeb, H.; Moeed, A.; Naeem, U.; Asghar, M.S.; Chughtai, N.U.; Yousaf, Z.; Seboka, B.T.; Ullah, I.; Lin, C.-Y. COVID-19 vaccine hesitancy in the United States: A systematic review. Front. Public Health 2021, 9, 770985. [Google Scholar] [CrossRef]
- Altenbuchner, A.; Haug, S.; Schnell, R.; Scharf, A.; Weber, K. Impfbereitschaft von Eltern mit einem COVID-19-Vakzin. Pädiatrie Pädologie 2021, 56, 230–234. [Google Scholar] [CrossRef]
- Bendau, A.; Plag, J.; Petzold, M.B.; Ströhle, A. COVID-19 vaccine hesitancy and related fears and anxiety. Int. Immunopharmacol. 2021, 97, 107724. [Google Scholar] [CrossRef]
- Lazarus, J.V.; Wyka, K.; Rauh, L.; Rabin, K.; Ratzan, S.; Gostin, L.O.; Larson, H.J.; El-Mohandes, A. Hesitant or not? The association of age, gender, and education with potential acceptance of a COVID-19 vaccine: A country-level analysis. J. Health Commun. 2020, 25, 799–807. [Google Scholar] [CrossRef]
- Schernhammer, E.; Weitzer, J.; Laubichler, M.D.; Birmann, B.M.; Bertau, M.; Zenk, L.; Caniglia, G.; Jäger, C.C.; Steiner, G. Correlates of COVID-19 vaccine hesitancy in Austria: Trust and the government. J. Public Health 2022, 44, e106–e116. [Google Scholar] [CrossRef] [PubMed]
- Umakanthan, S.; Lawrence, S. Predictors of COVID-19 vaccine hesitancy in Germany: A cross-sectional, population-based study. Postgrad. Med. J. 2022, 98, 756–764. [Google Scholar] [CrossRef] [PubMed]
- Morgan, L.; Schwartz, J.L.; Sisti, D.A. COVID-19 vaccination of minors without parental consent: Respecting emerging autonomy and advancing public health. JAMA Pediatr. 2021, 175, 995–996. [Google Scholar] [CrossRef] [PubMed]
- Galanis, P.; Vraka, I.; Siskou, O.; Konstantakopoulou, O.; Katsiroumpa, A.; Kaitelidou, D. Willingness, refusal and influential factors of parents to vaccinate their children against the COVID-19: A systematic review and meta-analysis. Prev. Med. 2022, 157, 106994. [Google Scholar] [CrossRef] [PubMed]
- Chen, F.; He, Y.; Shi, Y. Parents’ and guardians’ willingness to vaccinate their children against COVID-19: A systematic review and meta-analysis. Vaccines 2022, 10, 179. [Google Scholar] [CrossRef]
- Bagateli, L.E.; Saeki, E.Y.; Fadda, M.; Agostoni, C.; Marchisio, P.; Milani, G.P. COVID-19 vaccine hesitancy among parents of children and adolescents living in Brazil. Vaccines 2021, 9, 1115. [Google Scholar] [CrossRef]
- Marquez, R.R.; Gosnell, E.S.; Thikkurissy, S.; Schwartz, S.B.; Cully, J.L. Caregiver acceptance of an anticipated COVID-19 vaccination. J. Am. Dent. Assoc. 2021, 152, 730–739. [Google Scholar] [CrossRef]
- Ali, K.; Berman, G.; Zhou, H.; Deng, W.; Faughnan, V.; Coronado-Voges, M.; Ding, B.; Dooley, J.; Girard, B.; Hillebrand, W. Evaluation of mRNA-1273 SARS-CoV-2 vaccine in adolescents. N. Engl. J. Med. 2021, 385, 2241–2251. [Google Scholar] [CrossRef]
- Walter, E.B.; Talaat, K.R.; Sabharwal, C.; Gurtman, A.; Lockhart, S.; Paulsen, G.C.; Barnett, E.D.; Muñoz, F.M.; Maldonado, Y.; Pahud, B.A. Evaluation of the BNT162b2 COVID-19 vaccine in children 5 to 11 years of age. N. Engl. J. Med. 2022, 386, 35–46. [Google Scholar] [CrossRef]
- Alimoradi, Z.; Pakpour, A. Challenges to Parents in COVID-19 Vaccination for Children. PROSPERO 2022 CRD42022333342. Available online: https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=333342 (accessed on 5 January 2023).
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann. Intern. Med. 2009, 151, 264–269. [Google Scholar] [CrossRef]
- Morgan, R.L.; Whaley, P.; Thayer, K.A.; Schünemann, H.J. Identifying the PECO: A framework for formulating good questions to explore the association of environmental and other exposures with health outcomes. Environ. Int. 2018, 121, 1027–1031. [Google Scholar] [CrossRef] [PubMed]
- Luchini, C.; Stubbs, B.; Solmi, M.; Veronese, N. Assessing the quality of studies in meta-analyses: Advantages and limitations of the Newcastle Ottawa Scale. World J. Meta-Anal. 2017, 5, 80–84. [Google Scholar] [CrossRef]
- Wells, G.A.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses. Available online: https://www.ohri.ca//programs/clinical_epidemiology/oxford.asp (accessed on 22 August 2022).
- Hox, J.J.; Leeuw, E.D.d. Multilevel models for meta-analysis. In Multilevel Modeling: Methodological Advances, Issues, and Applications; Lawrence Erlbaum Associates Publishers: Mahwah, NJ, USA, 2003; pp. 90–111. [Google Scholar]
- Huedo-Medina, T.B.; Sánchez-Meca, J.; Marín-Martínez, F.; Botella, J. Assessing heterogeneity in meta-analysis: Q statistic or I2 index? Psychol. Methods 2006, 11, 193–206. [Google Scholar] [CrossRef] [PubMed]
- Rothstein, H.R.; Sutton, A.J.; Borenstein, M. Publication Bias in Meta-Analysis: Prevention, Assessment and Adjustments; John Wiley & Sons, Ltd.: Hoboken, NJ, USA, 2005; pp. 1–7. [Google Scholar]
- Duval, S.; Tweedie, R. Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 2000, 56, 455–463. [Google Scholar] [CrossRef] [PubMed]
- Hedges, L.V.; Olkin, I. Statistical Methods for Meta-Analysis; Academic Press: Cambridge, MA, USA; Elsevier Inc.: Amsterdam, The Netherlands, 1985. [Google Scholar] [CrossRef]
- Yang, J.; Zhang, T.; Qi, W.; Zhang, X.; Jia, M.; Leng, Z.; Wang, Q.; Yang, Y.; Yang, W.; Ma, L. COVID-19 vaccination in Chinese children: A cross-sectional study on the cognition, psychological anxiety state and the willingness toward vaccination. Hum. Vaccines Immunother. 2022, 18, 1–7. [Google Scholar] [CrossRef]
- Yılmazbas, P.; Terzi, O.; Ozceker, D. Did COVID-19 Pandemic Changed Parents’ Approach to Vaccination? Soc. Behav. 2021, 43, 130–134. [Google Scholar] [CrossRef]
- Kelly, B.J.; Southwell, B.G.; McCormack, L.A.; Bann, C.M.; MacDonald, P.D.; Frasier, A.M.; Bevc, C.A.; Brewer, N.T.; Squiers, L.B. Predictors of willingness to get a COVID-19 vaccine in the US. BMC Infect. Dis. 2021, 21, 338. [Google Scholar]
- Bell, S.; Clarke, R.; Mounier-Jack, S.; Walker, J.L.; Paterson, P. Parents’ and guardians’ views on the acceptability of a future COVID-19 vaccine: A multi-methods study in England. Vaccine 2020, 38, 7789–7798. [Google Scholar] [CrossRef]
- Lin, Y.; Hu, Z.; Zhao, Q.; Alias, H.; Danaee, M.; Wong, L.P. Chinese parents’ intentions to vaccinate their children against SARS-CoV-2 infection and vaccine preferences. Hum. Vaccines Immunother. 2021, 17, 4806–4815. [Google Scholar] [CrossRef]
- Goldman, R.D.; Yan, T.D.; Seiler, M.; Cotanda, C.P.; Brown, J.C.; Klein, E.J.; Hoeffe, J.; Gelernter, R.; Hall, J.E.; Davis, A.L. Caregiver willingness to vaccinate their children against COVID-19: Cross sectional survey. Vaccine 2020, 38, 7668–7673. [Google Scholar] [CrossRef]
- Goldman, R.D.; Ceballo, R.; Group, I.C.P.A.S. Parental gender differences in attitudes and willingness to vaccinate against COVID-19. J. Paediatr. Child Health 2022, 58, 1016–1021. [Google Scholar] [CrossRef]
- Hetherington, E.; Edwards, S.A.; MacDonald, S.E.; Racine, N.; Madigan, S.; McDonald, S.; Tough, S. SARS-CoV-2 vaccination intentions among mothers of children aged 9 to 12 years: A survey of the All Our Families cohort. Can. Med. Assoc. Open Access J. 2021, 9, E548–E555. [Google Scholar] [CrossRef] [PubMed]
- Ennaceur, S.; Al-Mohaithef, M. Parents’ Willingness to Vaccinate Children against COVID-19 in Saudi Arabia: A Cross-Sectional Study. Vaccines 2022, 10, 156. [Google Scholar] [CrossRef] [PubMed]
- Brandstetter, S.; Böhmer, M.M.; Pawellek, M.; Seelbach-Göbel, B.; Melter, M.; Kabesch, M.; Apfelbacher, C. Parents’ intention to get vaccinated and to have their child vaccinated against COVID-19: Cross-sectional analyses using data from the KUNO-Kids health study. Eur. J. Pediatr. 2021, 180, 3405–3410. [Google Scholar] [CrossRef]
- Davis, M.M.; Zickafoose, J.S.; Halvorson, A.E.; Patrick, S.W. Parents’ likelihood to vaccinate their children and themselves against COVID-19. MedRxiv 2020. [Google Scholar] [CrossRef]
- Gjini, E.; Moramarco, S.; Carestia, M.; Cenko, F.; Ylli, A.; Mehmeti, I.; Palombi, L.; Buonomo, E. Parents’ and caregivers’ role toward childhood vaccination in Albania: Assessment of predictors of vaccine hesitancy. Ann. Di Ig. Med. Prev. E Di Comunita 2022, 35, 75–83. [Google Scholar]
- Kezhong, A.; Lu, X.; Wang, J.; Hu, L.; Li, B.; Lu, Y. Association between adult vaccine hesitancy and parental acceptance of childhood COVID-19 vaccines: A web-based survey in a northwestern region in China. Vaccines 2021, 9, 1088. [Google Scholar]
- Çelik, M.Y. The thoughts of parents to vaccinate their children against COVID-19: An assessment of situations that may affect them. J. Child Adolesc. Psychiatr. Nurs. 2022, 35, 189–195. [Google Scholar] [CrossRef]
- Zhang, K.C.; Fang, Y.; Cao, H.; Chen, H.; Hu, T.; Chen, Y.Q.; Zhou, X.; Wang, Z. Parental acceptability of COVID-19 vaccination for children under the age of 18 years: Cross-sectional online survey. JMIR Pediatr. Parent. 2020, 3, e24827. [Google Scholar] [CrossRef]
- Wang, Q.; Xiu, S.; Yang, L.; Han, Y.; Cui, T.; Shi, N.; Liu, M.; Yi, Y.; Liu, C.; Wang, X. Changes in Parental Attitudes Toward COVID-19 Vaccination and Routine Childhood Vaccination During the COVID-19 Pandemic: Repeated Cross-sectional Survey Study. JMIR Public Health Surveill. 2022, 8, e33235. [Google Scholar] [CrossRef]
- Letterie, M.C.; Patrick, S.W.; Halvorson, A.E.; Dupont, W.D.; Carroll, K.N.; Zickafoose, J.S.; Williams, S.E. Factors Associated With Parental COVID-19 Vaccination Acceptance. Clin. Pediatr. 2022, 61, 393–401. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Xiu, S.; Zhao, S.; Wang, J.; Han, Y.; Dong, S.; Huang, J.; Cui, T.; Yang, L.; Shi, N. Vaccine hesitancy: COVID-19 and influenza vaccine willingness among parents in Wuxi, China—A cross-sectional study. Vaccines 2021, 9, 342. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; She, R.; Chen, X.; Li, L.; Li, L.; Huang, Z.; Lau, J.T. Parental acceptability of COVID-19 vaccination for children under the age of 18 years among Chinese doctors and nurses: A cross-sectional online survey. Hum. Vaccines Immunother. 2021, 17, 3322–3332. [Google Scholar] [CrossRef] [PubMed]
- Altulahi, N.; AlNujaim, S.; Alabdulqader, A.; Alkharashi, A.; AlMalki, A.; AlSiari, F.; Bashawri, Y.; Alsubaie, S.; AlShahrani, D.; AlGoraini, Y. Willingness, beliefs, and barriers regarding the COVID-19 vaccine in Saudi Arabia: A multiregional cross-sectional study. BMC Fam. Pract. 2021, 22, 247. [Google Scholar] [CrossRef] [PubMed]
- Skjefte, M.; Ngirbabul, M.; Akeju, O.; Escudero, D.; Hernandez-Diaz, S.; Wyszynski, D.F.; Wu, J.W. COVID-19 vaccine acceptance among pregnant women and mothers of young children: Results of a survey in 16 countries. Eur. J. Epidemiol. 2021, 36, 197–211. [Google Scholar] [CrossRef]
- Reindl, D.; Catma, S. A pre-vaccine analysis using the Health Belief Model to explain parents’ willingness to vaccinate (WTV) their children in the United States: Implications for vaccination programs. Expert Rev. Pharm. Outcomes Res. 2022, 22, 753–761. [Google Scholar] [CrossRef]
- Feng, H.; Zhu, H.; Zhang, H.; Cao, L.; Li, L.; Wang, J.; Huang, Y.; Lai, X.; Lyu, Y.; Jing, R. Caregivers’ intentions to COVID-19 vaccination for their children in China: A cross-sectional survey. Hum. Vaccines Immunother. 2021, 17, 4799–4805. [Google Scholar] [CrossRef]
- Montalti, M.; Rallo, F.; Guaraldi, F.; Bartoli, L.; Po, G.; Stillo, M.; Perrone, P.; Squillace, L.; Dallolio, L.; Pandolfi, P. Would parents get their children vaccinated against SARS-CoV-2? Rate and predictors of vaccine hesitancy according to a survey over 5000 families from Bologna, Italy. Vaccines 2021, 9, 366. [Google Scholar] [CrossRef]
- Padhi, B.K.; Satapathy, P.; Rajagopal, V.; Rustagi, N.; Vij, J.; Jain, L.; Chakrapani, V.; Patro, B.K.; Kar, S.S.; Singh, R. Parents’ Perceptions and Intention to Vaccinate Their Children Against COVID-19: Results From a Cross-Sectional National Survey in India. Front. Med. 2022, 9, 806702. [Google Scholar] [CrossRef]
- Humble, R.M.; Sell, H.; Dubé, E.; MacDonald, N.E.; Robinson, J.; Driedger, S.M.; Sadarangani, M.; Meyer, S.B.; Wilson, S.; Benzies, K.M. Canadian parents’ perceptions of COVID-19 vaccination and intention to vaccinate their children: Results from a cross-sectional national survey. Vaccine 2021, 39, 7669–7676. [Google Scholar] [CrossRef]
- Xu, Y.; Zhang, R.; Zhou, Z.; Fan, J.; Liang, J.; Cai, L.; Peng, L.; Ren, F.; Lin, W. Parental psychological distress and attitudes towards COVID-19 vaccination: A cross-sectional survey in Shenzhen, China. J. Affect. Disord. 2021, 292, 552–558. [Google Scholar] [CrossRef] [PubMed]
- Du, M.; Tao, L.; Liu, J. The association between risk perception and COVID-19 vaccine hesitancy for children among reproductive women in China: An online survey. Front. Med. 2021, 8, 1494. [Google Scholar] [CrossRef] [PubMed]
- Alsulaiman, J.W.; Mazin, M.; Al-Shatanawi, T.N.; Kheirallah, K.A.; Allouh, M.Z. Parental Willingness to Vaccinate Their Children Against SARS-CoV-2 in Jordan: An Explanatory Cross-Sectional Study. Risk Manag. Healthc. Policy 2022, 15, 955. [Google Scholar] [CrossRef] [PubMed]
- Aldakhil, H.; Albedah, N.; Alturaiki, N.; Alajlan, R.; Abusalih, H. Vaccine hesitancy towards childhood immunizations as a predictor of mothers’ intention to vaccinate their children against COVID-19 in Saudi Arabia. J. Infect. Public Health 2021, 14, 1497–1504. [Google Scholar] [CrossRef]
- Kreuter, M.W.; Garg, R.; Marsh, A.; Thompson, T.; Caburnay, C.; Teshome, E.; Kulkarni, S.; Tanpattana, T.; Wolff, J.; McQueen, A. Intention to vaccinate children for COVID-19: A segmentation analysis among Medicaid parents in Florida. Prev. Med. 2022, 156, 106959. [Google Scholar] [CrossRef]
- Wan, X.; Huang, H.; Shang, J.; Xie, Z.; Jia, R.; Lu, G.; Chen, C. Willingness and influential factors of parents of 3-6-year-old children to vaccinate their children with the COVID-19 vaccine in China. Hum. Vaccines Immunother. 2021, 17, 3969–3974. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Yan, W.; Lu, L.; Cao, L.; Tian, Y.; Zhou, K. Chinese parent intention to vaccinate children with special diseases against COVID-19. Front. Public Health 2021, 9, 725980. [Google Scholar] [CrossRef]
- Evans, S.; Klas, A.; Mikocka-Walus, A.; German, B.; Rogers, G.; Ling, M.; Fernando, J.; Kothe, E.; Westrupp, E. “Poison” or “protection”? A mixed methods exploration of Australian parents’ COVID-19 vaccination intentions. J. Psychosom. Res. 2021, 150, 110626. [Google Scholar] [CrossRef]
- Delgado-Gallegos, J.L.; Padilla-Rivas, G.R.; Gastelum-Arias, L.J.; Zuñiga-Violante, E.; Avilés-Rodríguez, G.; Arellanos-Soto, D.; Franco-Villareal, H.; Garza-Treviño, E.N.; Cosío-León, M.d.l.Á.; Romo-Cardenas, G.S. Parent’s perspective towards child COVID-19 vaccination: An online cross-sectional study in Mexico. Int. J. Environ. Res. Public Health 2021, 19, 290. [Google Scholar] [CrossRef]
- Yılmaz, M.; Sahin, M.K. Parents’ willingness and attitudes concerning the COVID-19 vaccine: A cross-sectional study. Int. J. Clin. Pract. 2021, 75, e14364. [Google Scholar] [CrossRef]
- Al-Khlaiwi, T.; Meo, S.A.; Almousa, H.A.; Almebki, A.A.; Albawardy, M.K.; Alshurafa, H.H.; Althunayan, M.A.; Alsayyari, M.S. National COVID-19 vaccine program and parent’s perception to vaccinate their children: A cross-sectional study. Vaccines 2022, 10, 168. [Google Scholar] [CrossRef] [PubMed]
- Derdemezis, C.; Markozannes, G.; Rontogianni, M.O.; Trigki, M.; Kanellopoulou, A.; Papamichail, D.; Aretouli, E.; Ntzani, E.; Tsilidis, K.K. Parental Hesitancy towards the Established Childhood Vaccination Programmes in the COVID-19 Era: Assessing the Drivers of a Challenging Public Health Concern. Vaccines 2022, 10, 814. [Google Scholar] [CrossRef] [PubMed]
- Szilagyi, P.G.; Shah, M.D.; Delgado, J.R.; Thomas, K.; Vizueta, N.; Cui, Y.; Vangala, S.; Shetgiri, R.; Kapteyn, A. Parents’ intentions and perceptions about COVID-19 vaccination for their children: Results from a national survey. Pediatrics 2021, 14, e2021052335. [Google Scholar] [CrossRef] [PubMed]
- Çağ, Y.; Bektemür, G.; Karabela, Ş.; Öztürk-Engin, D.; Çağ, Y.; Aktaş, S.; Kart-Yaşar, K. Parents’ Attitudes Toward COVID-19 Vaccination and Childhood Vaccines During the COVID-19 Pandemic. Asia Pac. J. Public Health 2022, 34, 270–272. [Google Scholar] [CrossRef] [PubMed]
- Teasdale, C.A.; Borrell, L.N.; Shen, Y.; Kimball, S.; Rinke, M.L.; Fleary, S.A.; Nash, D. Parental plans to vaccinate children for COVID-19 in New York city. Vaccine 2021, 39, 5082–5086. [Google Scholar] [CrossRef]
- Teasdale, C.A.; Borrell, L.N.; Kimball, S.; Rinke, M.L.; Rane, M.; Fleary, S.A.; Nash, D. Plans to vaccinate children for coronavirus disease 2019: A survey of United States parents. J. Pediatr. 2021, 237, 292–297. [Google Scholar] [CrossRef]
- Schilling, S.; Orr, C.J.; Delamater, A.M.; Flower, K.B.; Heerman, W.J.; Perrin, E.M.; Rothman, R.L.; Yin, H.S.; Sanders, L. COVID-19 vaccine hesitancy among low-income, racially and ethnically diverse US parents. Patient Educ. Couns. 2022, 105, 2771–2777. [Google Scholar] [CrossRef]
- Skeens, M.A.; Hill, K.; Olsavsky, A.; Buff, K.; Stevens, J.; Akard, T.F.; Shah, N.; Gerhardt, C.A. Factors affecting COVID-19 vaccine hesitancy in parents of children with cancer. Pediatr. Blood Cancer 2022, 69, e29707. [Google Scholar] [CrossRef]
- Alfieri, N.L.; Kusma, J.D.; Heard-Garris, N.; Davis, M.M.; Golbeck, E.; Barrera, L.; Macy, M.L. Parental COVID-19 vaccine hesitancy for children: Vulnerability in an urban hotspot. BMC Public Health 2021, 21, 1662. [Google Scholar] [CrossRef]
- Lachance-Grzela, M.; Charbonneau, A.; Dubé, A.; Jbilou, J.; Richard, J. Parents and caregivers’ willingness to vaccinate their children against COVID-19. Can. J. Behav. Sci./Rev. Can. Des Sci. Du Comport. 2022, 1–6. [Google Scholar] [CrossRef]
- Yoda, T.; Katsuyama, H. Parents’ hesitation about getting their children vaccinated against COVID-19 in Japan. Hum. Vaccines Immunother. 2021, 17, 4993–4998. [Google Scholar] [CrossRef] [PubMed]
- Di Giuseppe, G.; Pelullo, C.P.; Volgare, A.S.; Napolitano, F.; Pavia, M. Parents’ Willingness to Vaccinate Their Children With COVID-19 Vaccine: Results of a Survey in Italy. J. Adolesc. Health 2022, 70, 550–558. [Google Scholar] [CrossRef] [PubMed]
- Musa, S.; Dergaa, I.; Abdulmalik, M.A.; Ammar, A.; Chamari, K.; Saad, H.B. BNT162b2 COVID-19 vaccine hesitancy among parents of 4023 young adolescents (12–15 years) in Qatar. Vaccines 2021, 9, 981. [Google Scholar] [CrossRef]
- Atad, E.; Netzer, I.; Peleg, O.; Landsman, K.; Dalyot, K.; Reuven, S.E.; Baram-Tsabari, A. Vaccine-hesitant parents’ considerations regarding COVID-19 vaccination of adolescents. medRxiv 2021. [Google Scholar] [CrossRef]
- Al-Nafeesah, A.S.; Aldamigh, A.S.; Almansoor, B.A.; Al-Wutayd, O. The impact of the COVID-19 pandemic on parents’ behavior toward scheduled pediatric vaccinations in Saudi Arabia. J. Infect. Dev. Ctries. 2021, 15, 1054–1058. [Google Scholar] [CrossRef]
- Choi, S.-H.; Jo, Y.H.; Jo, K.J.; Park, S.E. Pediatric and parents’ attitudes towards COVID-19 vaccines and intention to vaccinate for children. J. Korean Med. Sci. 2021, 36, e227. [Google Scholar] [CrossRef]
- Wagner, A.; Liberatore, F.; Schmelzer, S.; Dratva, J. Confident and altruistic–parents’ motives to vaccinate their children against COVID-19: A cross-sectional online survey in a Swiss vaccination centre. Swiss Med. Wkly. 2022, 152, w30156. [Google Scholar] [CrossRef]
- Babicki, M.; Pokorna-Kałwak, D.; Doniec, Z.; Mastalerz-Migas, A. Attitudes of parents with regard to vaccination of children against COVID-19 in Poland. a nationwide online survey. Vaccines 2021, 9, 1192. [Google Scholar] [CrossRef]
- Horiuchi, S.; Sakamoto, H.; Abe, S.K.; Shinohara, R.; Kushima, M.; Otawa, S.; Yui, H.; Akiyama, Y.; Ooka, T.; Kojima, R. Factors of parental COVID-19 vaccine hesitancy: A cross sectional study in Japan. PLoS ONE 2021, 16, e0261121. [Google Scholar] [CrossRef]
- Choi, K.; Becerra-Culqui, T.; Bhakta, B.; Bruxvoort, K.; Coleman, K.J. Parent intentions to vaccinate children with autism spectrum disorder against COVID-19. J. Pediatr. Nurs. 2022, 63, 108–110. [Google Scholar] [CrossRef]
- Samannodi, M.; Alwafi, H.; Naser, A.Y.; Alabbasi, R.; Alsahaf, N.; Alosaimy, R.; Minshawi, F.; Almatrafi, M.; Khalifa, R.; Ekram, R. Assessment of caregiver willingness to vaccinate their children against COVID-19 in Saudi Arabia: A cross-sectional study. Hum. Vaccines Immunother. 2021, 17, 4857–4864. [Google Scholar] [CrossRef]
- Gendler, Y.; Ofri, L. Investigating the influence of vaccine literacy, vaccine perception and vaccine hesitancy on Israeli parents’ acceptance of the COVID-19 vaccine for their children: A cross-sectional study. Vaccines 2021, 9, 1391. [Google Scholar] [CrossRef] [PubMed]
- Zona, S.; Partesotti, S.; Bergomi, A.; Rosafio, C.; Antodaro, F.; Esposito, S. Anti-COVID vaccination for adolescents: A survey on determinants of vaccine parental hesitancy. Vaccines 2021, 9, 1309. [Google Scholar] [CrossRef] [PubMed]
- McKinnon, B.; Quach, C.; Dubé, È.; Nguyen, C.T.; Zinszer, K. Social inequalities in COVID-19 vaccine acceptance and uptake for children and adolescents in Montreal, Canada. Vaccine 2021, 39, 7140–7145. [Google Scholar] [CrossRef] [PubMed]
- Almusbah, Z.; Alhajji, Z.; Alshayeb, Z.; Alhabdan, R.; Alghafli, S.; Almusabah, M.; Almuqarrab, F.; Aljazeeri, I.; Almuhawas, F. Caregivers’ willingness to vaccinate their children against COVID-19 in Saudi Arabia: A cross-sectional survey. Cureus 2021, 13, e17243. [Google Scholar] [CrossRef]
- Urrunaga-Pastor, D.; Herrera-Añazco, P.; Uyen-Cateriano, A.; Toro-Huamanchumo, C.J.; Rodriguez-Morales, A.J.; Hernandez, A.V.; Benites-Zapata, V.A.; Bendezu-Quispe, G. Prevalence and factors associated with parents’ non-intention to vaccinate their children and adolescents against COVID-19 in Latin America and the Caribbean. Vaccines 2021, 9, 1303. [Google Scholar] [CrossRef]
- Kocamaz, E.B.; Kocamaz, H. Awareness of COVID-19 and attitudes toward vaccination in parents of children between 0 and 18 years: A cross-sectional study. J. Pediatr. Nurs. 2022, 65, 75–81. [Google Scholar] [CrossRef]
- Griva, K.; Tan, K.Y.; Chan, F.H.; Periakaruppan, R.; Ong, B.W.; Soh, A.S.; Chen, M.I. Evaluating Rates and Determinants of COVID-19 Vaccine Hesitancy for Adults and Children in the Singapore Population: Strengthening Our Community’s Resilience against Threats from Emerging Infections (SOCRATEs) Cohort. Vaccines 2021, 9, 1415. [Google Scholar] [CrossRef]
- Alhazza, S.F.; Altalhi, A.M.; Alamri, K.M.; Alenazi, S.S.; Alqarni, B.A.; Almohaya, A.M. Parents’ Hesitancy to Vaccinate Their Children Against COVID-19, a Country-Wide Survey. Front. Public Health 2022, 10, 755073. [Google Scholar] [CrossRef]
- McElfish, P.A.; Willis, D.E.; Shah, S.K.; Reece, S.; Andersen, J.A.; Schootman, M.; Richard-Davis, G.; Selig, J.P.; Warmack, T.S. Parents’ and Guardians’ Intentions to Vaccinate Children against COVID-19. Vaccines 2022, 10, 361. [Google Scholar] [CrossRef]
- Russo, L.; Croci, I.; Campagna, I.; Pandolfi, E.; Villani, A.; Reale, A.; Barbieri, M.A.; Raponi, M.; Gesualdo, F.; Tozzi, A.E. Intention of Parents to Immunize Children against SARS-CoV-2 in Italy. Vaccines 2021, 9, 1469. [Google Scholar] [CrossRef] [PubMed]
- Temsah, M.-H.; Alhuzaimi, A.N.; Aljamaan, F.; Bahkali, F.; Al-Eyadhy, A.; Alrabiaah, A.; Alhaboob, A.; Bashiri, F.A.; Alshaer, A.; Temsah, O. Parental attitudes and hesitancy about COVID-19 vs. routine childhood vaccinations: A national survey. Front. Public Health 2021, 9, 752323. [Google Scholar] [CrossRef] [PubMed]
- Mohan, R.; Pandey, V.; Kumar, A.; Gangadevi, P.; Goel, A.D.; Joseph, J.; Kurien, N. Acceptance and Attitude of Parents Regarding COVID-19 Vaccine for Children: A Cross-Sectional Study. Cureus 2022, 14, 24518. [Google Scholar] [CrossRef]
- Galanis, P.; Vraka, I.; Siskou, O.; Konstantakopoulou, O.; Katsiroumpa, A.; Moisoglou, I.; Kaitelidou, D. Predictors of parents’ intention to vaccinate their children against the COVID-19 in Greece: A cross-sectional study. medRxiv 2021. [Google Scholar] [CrossRef]
- Willis, D.E.; Schootman, M.; Shah, S.K.; Reece, S.; Selig, J.P.; Andersen, J.A.; McElfish, P.A. Parent/guardian intentions to vaccinate children against COVID-19 in the United States. Hum. Vaccines Immunother. 2022, 18, 2071078. [Google Scholar] [CrossRef] [PubMed]
- Shmueli, L. Parents’ intention to vaccinate their 5-11 years old children with the COVID-19 vaccine: Rates, predictors and the role of incentives. MedRxiv 2021. [Google Scholar] [CrossRef] [PubMed]
- Ma, L.; Yang, J.; Zhang, T.; Han, X.; Huang, Q.; Yang, Y.; Feng, L.; Yang, W.; Wang, C. Willingness toward COVID-19 vaccination, coadministration with other vaccines and receive a COVID-19 vaccine booster: A cross-sectional study on the guardians of children in China. Hum. Vaccines Immunother. 2022, 18, 2049169. [Google Scholar] [CrossRef]
- Ali, M.; Ahmed, S.; Bonna, A.S.; Sarkar, A.-s.; Islam, M.A.; Urmi, T.A.; Proma, T.S. Parental coronavirus disease vaccine hesitancy for children in Bangladesh: A cross-sectional study. F1000Research 2022, 11, 90. [Google Scholar] [CrossRef]
- Li, T.; Qiu, X.; Gong, X.; Zhan, R.; Zheng, X. The cross-sectional survey on COVID-19 vaccine hesitancy and it predictors among Chinese parents of 3–17 years aged children in Shenzhen City. Ann. Agric. Environ. Med. 2022, 29, 120–125. [Google Scholar] [CrossRef]
- Ali, M.; Proma, T.S.; Tasnim, Z.; Islam, M.; Urmi, T.A.; Ahmed, S.; Sarkar, A.-S.; Bonna, A.S.; Khan, U.S. Parental COVID-19 vaccine hesitancy for children with neurodevelopmental disorders: A cross-sectional survey. Trop. Med. Health 2022, 50, 24. [Google Scholar] [CrossRef]
- Fisher, C.B.; Gray, A.; Sheck, I. COVID-19 pediatric vaccine hesitancy among racially diverse parents in the United States. Vaccines 2021, 10, 31. [Google Scholar] [CrossRef]
- Al-Qerem, W.; Al Bawab, A.Q.; Hammad, A.; Jaber, T.; Khdair, S.I.; Kalloush, H.; Ling, J.; Mosleh, R. Parents’ attitudes, knowledge and practice towards vaccinating their children against COVID-19: A cross-sectional study. Hum. Vaccines Immunother. 2022, 18, 2044257. [Google Scholar] [CrossRef]
- Tsai, C.-S.; Wang, L.-J.; Hsiao, R.C.; Yen, C.-F. Second Wave of the Study of Taiwanese Caregivers of Children with ADHD in the COVID-19 Pandemic: Intentions to Vaccinate Their Children for COVID-19, and Related Factors. Vaccines 2022, 10, 753. [Google Scholar] [CrossRef]
- Kheil, M.H.; Jain, D.; Jomaa, J.; Askar, B.; Alcodray, Y.; Wahbi, S.; Brikho, S.; Kadouh, A.; Harajli, D.; Jawad, Z.N. COVID-19 Vaccine Hesitancy among Arab Americans. Vaccines 2022, 10, 610. [Google Scholar] [CrossRef]
- Al-Qerem, W.; Jarab, A.; Hammad, A.; Alasmari, F.; Ling, J.; Alsajri, A.H.; Al-Hishma, S.W.; Abu Heshmeh, S.R. Iraqi Parents’ Knowledge, Attitudes, and Practices towards Vaccinating Their Children: A Cross-Sectional Study. Vaccines 2022, 10, 820. [Google Scholar] [CrossRef] [PubMed]
- Almalki, O.S.; Alfayez, O.M.; Al Yami, M.S.; Asiri, Y.A.; Almohammed, O.A. Parents’ Hesitancy to Vaccinate Their 5–11-Year-Old Children Against COVID-19 in Saudi Arabia: Predictors From the Health Belief Model. Front. Public Health 2022, 10, 842862. [Google Scholar] [CrossRef] [PubMed]
- Miraglia del Giudice, G.; Napoli, A.; Corea, F.; Folcarelli, L.; Angelillo, I.F. Evaluating COVID-19 Vaccine Willingness and Hesitancy among Parents of Children Aged 5–11 Years with Chronic Conditions in Italy. Vaccines 2022, 10, 396. [Google Scholar] [CrossRef] [PubMed]
- Buonsenso, D.; Valentini, P.; Macchi, M.; Folino, F.; Pensabene, C.; Patria, M.F.; Agostoni, C.; Castaldi, S.; Lecce, M.; Giannì, M.L. Caregivers’ Attitudes Toward COVID-19 Vaccination in Children and Adolescents With a History of SARS-CoV-2 Infection. Front. Pediatr. 2022, 10, 867968. [Google Scholar] [CrossRef]
- Miliordos, K.; Giannouchos, T.; Steletou, E.; Sanidas, G.; Karkania, A.; Vervenioti, A.; Dimitriou, G.; Gkentzi, D. Parental attitudes towards vaccination against COVID-19 of children 5–11 years old in Greece. J. Eval. Clin. Pract. 2022, 28, 943–947. [Google Scholar] [CrossRef]
- Lau, E.Y.H.; Li, J.-B.; Chan, D.K.C. Intention to vaccinate young children against COVID-19: A large-scale survey of Hong Kong parents. Hum. Vaccines Immunother. 2022, 18, 2065838. [Google Scholar] [CrossRef]
- Aljamaan, F.; Alhaboob, A.; Saddik, B.; Bassrawi, R.; Assiri, R.; Saeed, E.; Alhasan, K.; Alenezi, S.; Alarabi, M.; Alrabiaah, A. In-Person Schooling Amidst Children’s COVID-19 Vaccination: Exploring Parental Perceptions Just after Omicron Variant Announcement. Vaccines 2022, 10, 768. [Google Scholar] [CrossRef] [PubMed]
- Altulaihi, B.A.; Alaboodi, T.; Alharbi, K.G.; Alajmi, M.S.; Alkanhal, H.; Alshehri, A. Perception of parents towards COVID-19 vaccine for children in Saudi population. Cureus 2021, 13, e18342. [Google Scholar] [CrossRef] [PubMed]
- Ruggiero, K.M.; Wong, J.; Sweeney, C.F.; Avola, A.; Auger, A.; Macaluso, M.; Reidy, P. Parents’ intentions to vaccinate their children against COVID-19. J. Pediatr. Health Care 2021, 35, 509–517. [Google Scholar] [CrossRef] [PubMed]
- Al Yamani, Z.J.; AlJohani, M.M. Vaccine Hesitancy among Parents and its Determinants in PHC in Al Madinah City 2020. Egypt. J. Hosp. Med. 2022, 87, 1619–1625. [Google Scholar] [CrossRef]
- Yigit, M.; Ozkaya-Parlakay, A.; Senel, E. Evaluation of COVID-19 vaccine refusal in parents. Pediatr. Infect. Dis. J. 2021, 40, e134–e136. [Google Scholar] [CrossRef]
- Wilde, G.J. The theory of risk homeostasis: Implications for safety and health. Risk Anal. 1982, 2, 209–225. [Google Scholar] [CrossRef]
- DiLillo, D.; Tremblay, G. Maternal and child reports of behavioral compensation in response to safety equipment usage. J. Pediatr. Psychol. 2001, 26, 175–184. [Google Scholar] [CrossRef]
- Wallach, M.A.; Kogan, N.; Bem, D.J. Diffusion of responsibility and level of risk taking in groups. J. Abnorm. Soc. Psychol. 1964, 68, 263. [Google Scholar] [CrossRef]
- Hudson, J.M.; Bruckman, A.S. The bystander effect: A lens for understanding patterns of participation. J. Learn. Sci. 2004, 13, 165–195. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).