Using Social Marketing to Promote COVID-19 Vaccination Uptake: A Case Study from the “AUBe Vaccinated” Campaign
Abstract
1. Introduction
2. Materials and Methods
2.1. The Context
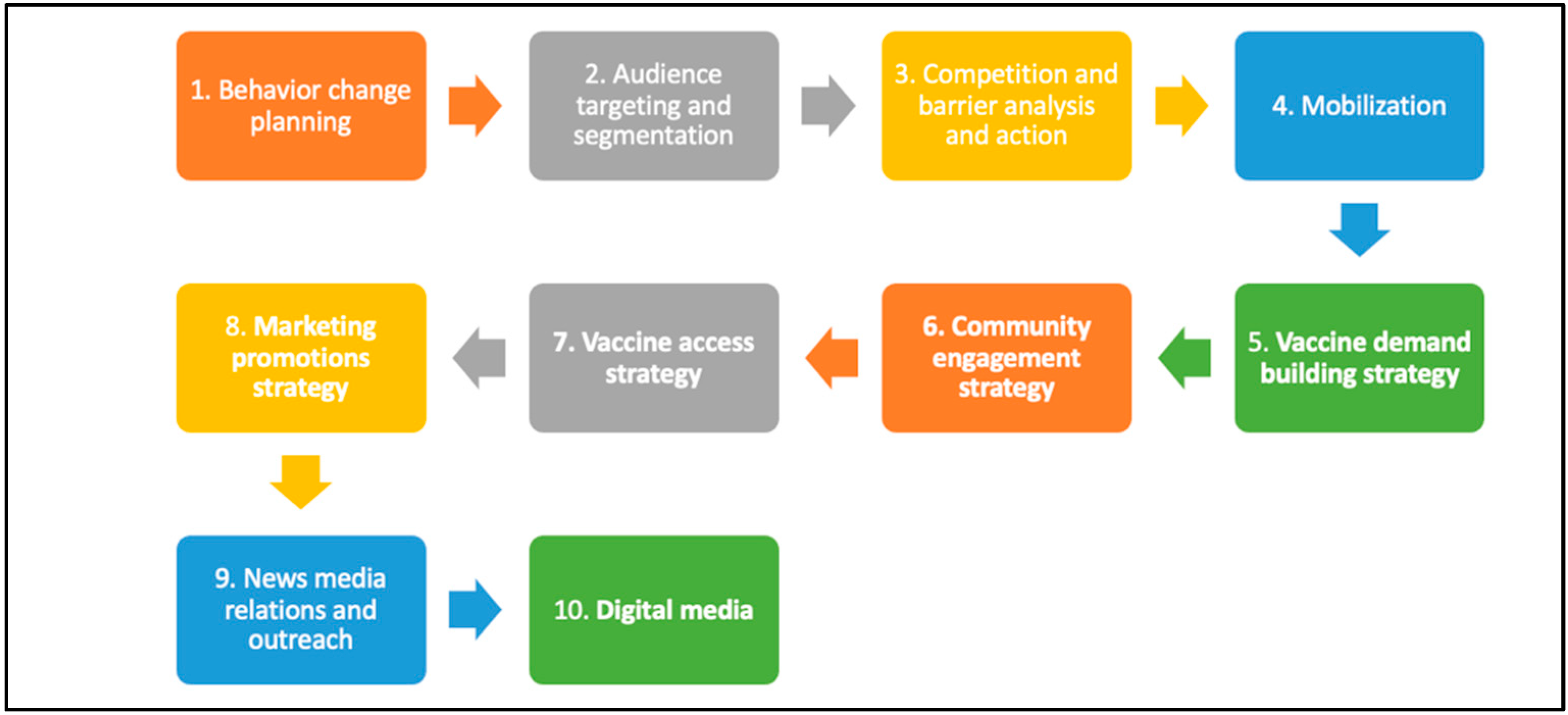
2.2. Planning Framework
2.2.1. Behavior Change Planning
2.2.2. Audience Targeting and Segmentation
2.2.3. Competition Analysis
2.2.4. Mobilization and Community Engagement
2.2.5. Vaccine Demand-Building and Access Strategy
2.3. Monitoring and Evaluation
3. Results
3.1. Audience Insights, Competition Analysis, Segmentation
3.2. Mobilization and Community Engagement
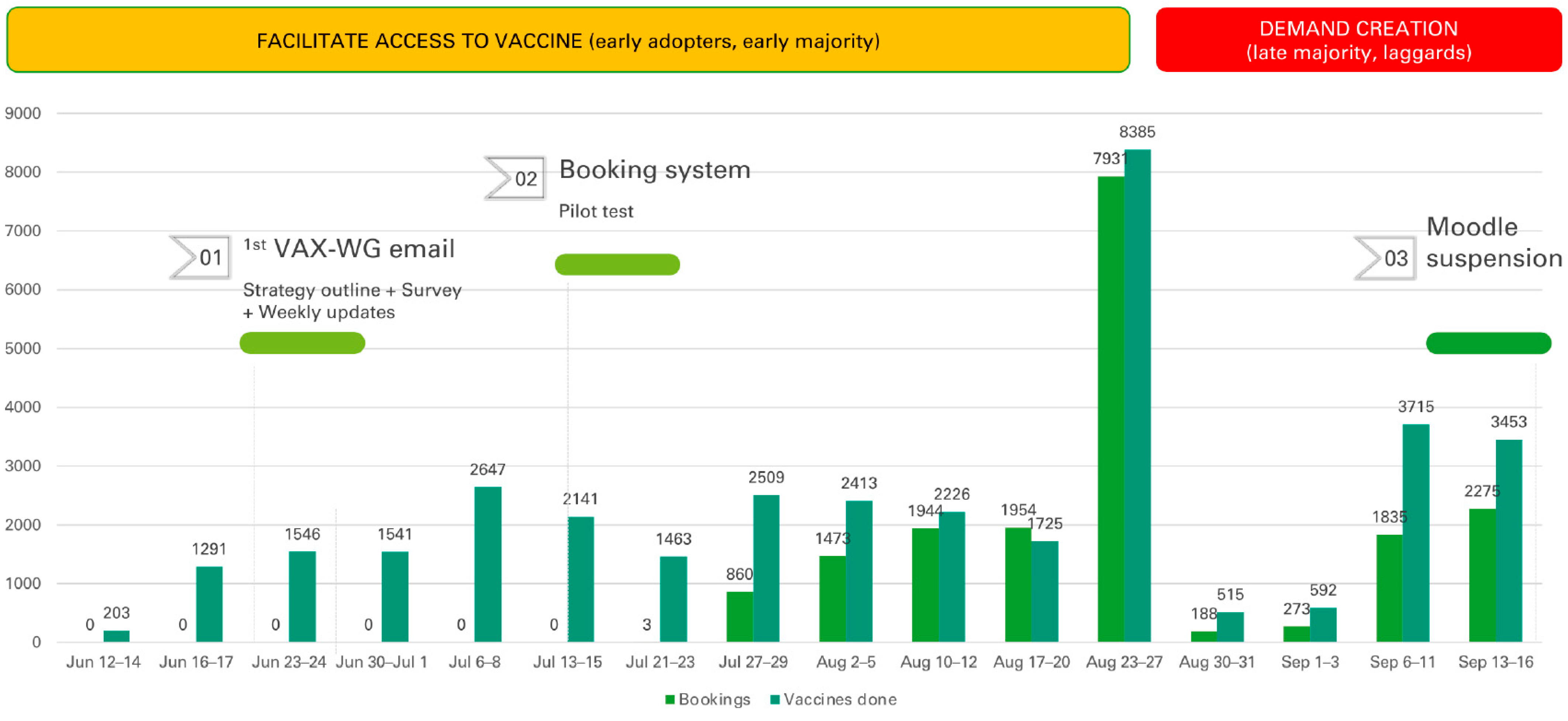
3.3. Vaccine Demand-Building and Access Strategy
4. Discussion
4.1. Behavior Change Planning
4.2. Formative Research Insights, Competition Analysis, Audience Segmentation
4.3. Mobilization and Community Engagement
4.4. Vaccine Demand-Building and Access Strategy
4.5. Strengths and Limitations
5. Conclusions and Recommendations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mahmood, S.; Hasan, K.; Carras, M.C.; Labrique, A. Global Preparedness Against COVID-19: We Must Leverage the Power of Digital Health. JMIR Public Health Surveill. 2020, 6, e18980. [Google Scholar] [CrossRef] [PubMed]
- UN. United Nations UN/DESA Policy Brief #66: COVID-19 and the Least Developed Countries | Department of Economic and Social Affairs. Available online: https://www.un.org/development/desa/dpad/publication/un-desa-policy-brief-66-covid-19-and-the-least-developed-countries/ (accessed on 24 January 2023).
- OECD. Organisation for Economic Co-Operation and Development Developing Countries and Development Co-Operation: What is at Stake? Available online: https://www.oecd.org/coronavirus/policy-responses/developing-countries-and-development-co-operation-what-is-at-stake-50e97915/#snotes-d4e116 (accessed on 24 January 2023).
- Oxfam International. Pandemic of Greed: A Wake-Up Call for Vaccine Equity at a Grim Milestone. Available online: https://www.oxfam.org/en/research/pandemic-greed (accessed on 24 January 2023).
- Grochowska, M.; Ratajczak, A.; Zdunek, G.; Adamiec, A.; Waszkiewicz, P.; Feleszko, W. A Comparison of the Level of Acceptance and Hesitancy towards the Influenza Vaccine and the Forthcoming COVID-19 Vaccine in the Medical Community. Vaccines 2021, 9, 475. [Google Scholar] [CrossRef] [PubMed]
- Patwary, M.M.; Alam, M.A.; Bardhan, M.; Disha, A.S.; Haque, M.Z.; Billah, S.M.; Kabir, M.P.; Browning, M.H.E.M.; Rahman, M.M.; Parsa, A.D.; et al. COVID-19 Vaccine Acceptance among Low- and Lower-Middle-Income Countries: A Rapid Systematic Review and Meta-Analysis. Vaccines 2022, 10, 427. [Google Scholar] [CrossRef] [PubMed]
- Mathieu, E.; Ritchie, H.; Ortiz-Ospina, E.; Roser, M.; Hasell, J.; Appel, C.; Giattino, C.; Rodés-Guirao, L. A global database of COVID-19 vaccinations. Nat. Hum. Behav. 2021, 5, 947–953. [Google Scholar] [CrossRef] [PubMed]
- Mathieu, E.; Ritchie, H.; Rodés-Guirao, L.; Appel, C.; Giattino, C.; Hasell, J.; Macdonald, B.; Dattani, S.; Beltekian, D.; Ortiz-Ospina, E.; et al. Coronavirus Pandemic (COVID-19). Available online: https://ourworldindata.org/covid-vaccinations (accessed on 24 January 2023).
- Dubé, E.; Gagnon, D.; MacDonald, N.E. Strategies intended to address vaccine hesitancy: Review of published reviews. Vaccine 2015, 33, 4191–4203. [Google Scholar] [CrossRef] [PubMed]
- Kaufman, J.; Ryan, R.; Walsh, L.; Horey, D.; Leask, J.; Robinson, P.; Hill, S. Face-to-face interventions for informing or educating parents about early childhood vaccination. Cochrane Database Syst. Rev. 2018, 5, CD010038. [Google Scholar] [CrossRef] [PubMed]
- Saeterdal, I.; Lewin, S.; Austvoll-Dahlgren, A.; Glenton, C.; Munabi-Babigumira, S. Interventions aimed at communities to inform and/or educate about early childhood vaccination. Cochrane Database Syst. Rev. 2014, 11, CD010232. [Google Scholar] [CrossRef]
- De Vere Hunt, I.; Dunn, T.; Mahoney, M.; Chen, M.; Zhang, L.; Bousheri, S.; Bernard, D.; Linos, E. A social media-based campaign to promote COVID-19 vaccine uptake in underrepresented groups in the US. Eur. J. Public Health 2021, 31, ckab165.170. [Google Scholar] [CrossRef]
- Meng, Z.; Shan, S.; Zhang, R. China’s COVID-19 Vaccination Strategy and Its Impact on the Global Pandemic. Risk Manag. Healthc. Policy 2021, 14, 4649–4655. [Google Scholar] [CrossRef]
- Jarrett, C.; Wilson, R.; O’Leary, M.; Eckersberger, E.; Larson, H.J. Strategies for addressing vaccine hesitancy—A systematic review. Vaccine 2015, 33, 4180–4190. [Google Scholar] [CrossRef]
- iSMA, International Social Marketing Association; ESMA, European Social Marketing Association; AASM, Australian Association of Social Marketing; SMANA, S.M.A. of N.A.; ALAMS. Asociación Latinoamericana De Mercadeo Social Global Consensus on Social Marketing Principles, Concepts, and Techniques. Available online: http://smana.org/wp-content/uploads/2017/04/ESMA-AASM-SMANA-endorsed-Consensus-Principles-and-concepts-paper.pdf (accessed on 24 January 2023).
- Nowak, G.J.; Gellin, B.G.; MacDonald, N.E.; Butler, R. Addressing vaccine hesitancy: The potential value of commercial and social marketing principles and practices. Vaccine 2015, 33, 4204–4211. [Google Scholar] [CrossRef]
- Opel, D.J.; Diekema, D.S.; Lee, N.R.; Marcuse, E.K. Social Marketing as a Strategy to Increase Immunization Rates. Arch. Pediatr. Adolesc. Med. 2009, 163, 432–437. [Google Scholar] [CrossRef] [PubMed]
- Ling, J.C.; Franklin, B.A.K.; Lindsteadt, J.F.; Gearon, S.A.N. Social Marketing: Its Place in Public Health. Annu. Rev. Public Health 1992, 13, 341–362. [Google Scholar] [CrossRef] [PubMed]
- Cates, J.R.; Shafer, A.; Diehl, S.J.; Deal, A.M. Evaluating a County-Sponsored Social Marketing Campaign to Increase Mothers’ Initiation of HPV Vaccine for Their Preteen Daughters in a Primarily Rural Area. Soc. Mark. Q. 2011, 17, 4–26. [Google Scholar] [CrossRef] [PubMed]
- Cates, J.R.; Diehl, S.J.; Crandell, J.L.; Coyne-Beasley, T. Intervention effects from a social marketing campaign to promote HPV vaccination in preteen boys. Vaccine 2014, 32, 4171–4178. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.; Rundle-Thiele, S.; Fong, B.Y.F.; Li, G. The Application and Outcome Evaluation of a Social Marketing Intervention to Increase Seasonal Influenza Vaccination among University Students. Vaccines 2022, 10, 1671. [Google Scholar] [CrossRef]
- Shekhar, S.K. Social Marketing Plan to Decrease the COVID-19 Vaccine Hesitancy among Senior Citizens in Rural India. Sustainability 2022, 14, 7561. [Google Scholar] [CrossRef]
- Evans, W.D.; French, J. Demand Creation for COVID-19 Vaccination: Overcoming Vaccine Hesitancy through Social Marketing. Vaccines 2021, 9, 319. [Google Scholar] [CrossRef]
- French, J.; Deshpande, S.; Evans, W.; Obregon, R. Key Guidelines in Developing a Pre-Emptive COVID-19 Vaccination Uptake Promotion Strategy. Int. J. Environ. Res. Public. Health 2020, 17, 5893. [Google Scholar] [CrossRef]
- Dul, J.; Hak, T. Case Study Methodology in Business Research; Routledge: London, UK, 2007; ISBN 978-1-138-17416-0. [Google Scholar]
- MOPH. Ministry of Public Health Minister Hasan Announces First Coronavirus Case in Lebanon. Available online: http://www.moph.gov.lb (accessed on 24 January 2023).
- Middle East Eye. Coronavirus: Lebanon Records First Death from the Disease. Available online: http://www.middleeasteye.net/news/coronavirus-first-death-recorded-lebanon-egyptian-middle-east (accessed on 24 January 2023).
- Project HOPE. W. On-The-Record Updates: The COVID-19 Situation in Lebanon. Available online: https://www.projecthope.org/on-the-record-updates-the-covid-19-situation-in-lebanon/01/2021/ (accessed on 24 January 2023).
- Asfahani, F.; Varkey, S.; Nguyen, S.N. Lebanon: Fair and Transparent Distribution of COVID1-9 Vaccine Key to Real Success. Available online: https://blogs.worldbank.org/arabvoices/lebanon-fair-and-transparent-distribution-covid19-vaccine-key-real-success (accessed on 24 January 2023).
- MOPH. Ministry of Public Health Lebanon National Deployment and Vaccination Plan for COVID-19 Vaccines. Available online: https://www.moph.gov.lb/userfiles/files/Prevention/COVID-19%20Vaccine/Lebanon%20NDVP-%20Feb%2016%202021.pdf (accessed on 24 January 2023).
- Internews. Vaccine Inequality: Why Vaccine Inequality Is Our Biggest COVID-19 Communication Challenge Yet. Available online: https://internews.org/resource/vaccine-inequality-why-vaccine-inequality-our-biggest-covid-19-communication-challenge-yet (accessed on 24 January 2023).
- Hamdan, M.B.; Singh, S.; Polavarapu, M.; Jordan, T.R.; Melhem, N.M. COVID-19 vaccine hesitancy among university students in Lebanon. Epidemiol. Infect. 2021, 149, e242. [Google Scholar] [CrossRef]
- AUB. For the People of Lebanon: AUB and the University Hospitals Consortium Vaccination Drive. Available online: https://www.aub.edu.lb/advancement/Development/Documents/For%20the%20People%20of%20Lebanon%20-%20The%20University%20Hospitals%20Consortium%20Vaccination%20Drive.pdf (accessed on 24 January 2023).
- AUB. Facts and Figures. Available online: https://www.aub.edu.lb/AboutUs/Pages/facts.aspx (accessed on 24 January 2023).
- Zhang, K.; Fang, Y.; Chan, P.S.; Cao, H.; Chen, H.; Hu, T.; Chen, Y.; Zhou, X.; Wang, Z. Behavioral Intention to Get a Booster Dose of COVID-19 Vaccine among Chinese Factory Workers. Int. J. Environ. Res. Public. Health 2022, 19, 5245. [Google Scholar] [CrossRef] [PubMed]
- Zhang, K.C.; Fang, Y.; Cao, H.; Chen, H.; Hu, T.; Chen, Y.; Zhou, X.; Wang, Z. Behavioral Intention to Receive a COVID-19 Vaccination Among Chinese Factory Workers: Cross-sectional Online Survey. J. Med. Internet Res. 2021, 23, e24673. [Google Scholar] [CrossRef] [PubMed]
- Evans, W.D.; Blitstein, J.; Hersey, J.C.; Renaud, J.; Yaroch, A.L. Systematic review of public health branding. J. Health Commun. 2008, 13, 721. [Google Scholar] [CrossRef] [PubMed]
- Evans, W.D.; Blitstein, J.; Vallone, D.; Post, S.; Nielsen, W. Systematic review of health branding: Growth of a promising practice. Transl. Behav. Med. 2015, 5, 24–36. [Google Scholar] [CrossRef] [PubMed]
- Evans, W.D.; Hastings, G. Public Health Branding: Applying Marketing for Social Change; Evans, W.D., Hastings, G., Eds.; Oxford University Press: New York, NY, USA, 2008; ISBN 978-0-19-923713-5. [Google Scholar]
- AUB. AUBe Vaccinated Campaign. Available online: https://www.aub.edu.lb/emergency/AVC/Pages/default.aspx (accessed on 24 January 2023).
- Burchell, K.; Rettie, R.; Patel, K. Marketing social norms: Social marketing and the ‘social norm approach. J. Consum. Behav. 2013, 12, 1–9. [Google Scholar] [CrossRef]
- French, J. Social Marketing’s Contribution to Macro-Social Policy and Economics, Beyond Upstream, Midstream, and Downstream Analysis. In Macro-Social Marketing Insights; Routledge: London, UK, 2019; ISBN 978-0-429-45230-7. [Google Scholar]
- Kubacki, K.; Rundle-Thiele, S.; Pang, B.; Carins, J.; Parkinson, J.; Fujihira, H.; Ronto, R. An Umbrella Review of the Use of Segmentation in Social Marketing Interventions. In Segmentation in Social Marketing: Process, Methods and Application; Dietrich, T., Rundle-Thiele, S., Kubacki, K., Eds.; Springer: Singapore, 2017; pp. 9–23. ISBN 978-981-10-1835-0. [Google Scholar]
- Thaker, J.; Richardson, L.M.; Holmes, D.C. Audience segmentation analysis of public intentions to get a COVID-19 vaccine in Australia. Public Underst. Sci. 2022, 09636625221138494. [Google Scholar] [CrossRef] [PubMed]
- Humanitarian Aid. Fuel Crisis in Lebanon Potential Catastrophe for Thousands: Senior UN official | UN News. Available online: https://news.un.org/en/story/2021/08/1097962 (accessed on 24 January 2023).
- World Health Organization. Behavioural Considerations for Acceptance and Uptake of COVID-19 Vaccines: WHO Technical Advisory Group on Behavioural Insights and Sciences for Health, Meeting Report, 15 October 2020; World Health Organization: Geneva, Switzerland, 2020; ISBN 978-92-4-001692-7.
- Abdullah, M.; Ahmad, T.; Kazmi, T.; Sultan, F.; Afzal, S.; Safdar, R.M.; Khan, A.A. Community engagement to increase vaccine uptake: Quasi-experimental evidence from Islamabad and Rawalpindi, Pakistan. PLoS ONE 2022, 17, e0274718. [Google Scholar] [CrossRef]
- Parchment, A.; Lawrence, W.; Perry, R.; Rahman, E.; Townsend, N.; Wainwright, E.; Wainwright, D. Making Every Contact Count and Healthy Conversation Skills as very brief or brief behaviour change interventions: A scoping review. J. Public Health 2021, 1–8. [Google Scholar] [CrossRef]
- Bardus, M.; Keriabian, A.; Elbejjani, M.; Al-Hajj, S. Assessing eHealth literacy among internet users in Lebanon: A cross-sectional study. Digit. Health 2022, 8, 20552076221119336. [Google Scholar] [CrossRef]
- Kabakian-Khasholian, T.; Makhoul, J.; Bardus, M. To wear or not to wear a mask in the COVID-19 era? The broken bridge between recommendations and implementation in Lebanon. J. Glob. Health 2020, 10, 020322. [Google Scholar] [CrossRef]
- French, J. The case for social marketing in public health. In Social Marketing and Public Health; French, J., Ed.; Oxford University Press: London, UK, 2017; ISBN 978-0-19-178811-6. [Google Scholar]
- Savulescu, J.; Pugh, J.; Wilkinson, D. Balancing incentives and disincentives for vaccination in a pandemic. Nat. Med. 2021, 27, 1500–1503. [Google Scholar] [CrossRef] [PubMed]
- Antonini, M.; Eid, M.A.; Falkenbach, M.; Rosenbluth, S.T.; Prieto, P.A.; Brammli-Greenberg, S.; McMeekin, P.; Paolucci, F. An analysis of the COVID-19 vaccination campaigns in France, Israel, Italy and Spain and their impact on health and economic outcomes. Health Policy Technol. 2022, 11, 100594. [Google Scholar] [CrossRef] [PubMed]
- Sommariva, S.; Mote, J.; Ballester Bon, H.; Razafindraibe, H.; Ratovozanany, D.; Rasoamanana, V.; Abeyesekera, S.; Muhamedkhojaeva, P.; Bashar, T.; James, J.; et al. Social Listening in Eastern and Southern Africa, a UNICEF Risk Communication and Community Engagement Strategy to Address the COVID-19 Infodemic. Health Secur. 2021, 19, 57–64. [Google Scholar] [CrossRef] [PubMed]
- Bardus, M.; Domegan, C.T.; Suggs, L.S.; Mikkelsen, B.E. Engaging Students and Communities through Service Learning and Community-Academia Partnerships: Lessons from Social Marketing Education. In Research Anthology on Business and Technical Education in the Information Era; Information Resources Management Association, Ed.; IGI Global: Hershey, PA, USA, 2021; pp. 832–856. ISBN 978-1-79985-345-9. [Google Scholar]
- Bardus, M.; Nasser AlDeen, K.; Kabakian-Khasholian, T.; Kanj, M.; Germani, A. Teaching Social Marketing using E-Service Learning Amidst Health and Humanitarian Crises: A Case Study from Lebanon. Int. J. Environ. Res. Public. Health 2022, 19, 12696. [Google Scholar] [CrossRef]
- Oldenburg, B.; Glanz, K. Diffusion of Innovations. In Health Behavior and Health Education; Glanz, K., Rimer, B.K., Viswanath, K.V., Eds.; Jossey-Bass: San Francisco, CA, USA, 2008; pp. 313–330. [Google Scholar]
- Rogers, E.M. Diffusion of Innovations, 5th ed.; Free Press: New York, NY, USA, 2003. [Google Scholar]
- Mo, P.K.; Luo, S.; Wang, S.; Zhao, J.; Zhang, G.; Li, L.; Li, L.; Xie, L.; Lau, J.T.F. Intention to Receive the COVID-19 Vaccination in China: Application of the Diffusion of Innovations Theory and the Moderating Role of Openness to Experience. Vaccines 2021, 9, 129. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bardus, M.; Assaf, S.A.; Sakr, C.J. Using Social Marketing to Promote COVID-19 Vaccination Uptake: A Case Study from the “AUBe Vaccinated” Campaign. Vaccines 2023, 11, 459. https://doi.org/10.3390/vaccines11020459
Bardus M, Assaf SA, Sakr CJ. Using Social Marketing to Promote COVID-19 Vaccination Uptake: A Case Study from the “AUBe Vaccinated” Campaign. Vaccines. 2023; 11(2):459. https://doi.org/10.3390/vaccines11020459
Chicago/Turabian StyleBardus, Marco, Sara A. Assaf, and Carine J. Sakr. 2023. "Using Social Marketing to Promote COVID-19 Vaccination Uptake: A Case Study from the “AUBe Vaccinated” Campaign" Vaccines 11, no. 2: 459. https://doi.org/10.3390/vaccines11020459
APA StyleBardus, M., Assaf, S. A., & Sakr, C. J. (2023). Using Social Marketing to Promote COVID-19 Vaccination Uptake: A Case Study from the “AUBe Vaccinated” Campaign. Vaccines, 11(2), 459. https://doi.org/10.3390/vaccines11020459






