Factors Influencing COVID-19 Vaccine Hesitancy among Patients with Serious Chronic Illnesses during the Initial Australian Vaccine Rollout: A Multi-Centre Qualitative Analysis Using the Health Belief Model
Abstract
1. Introduction
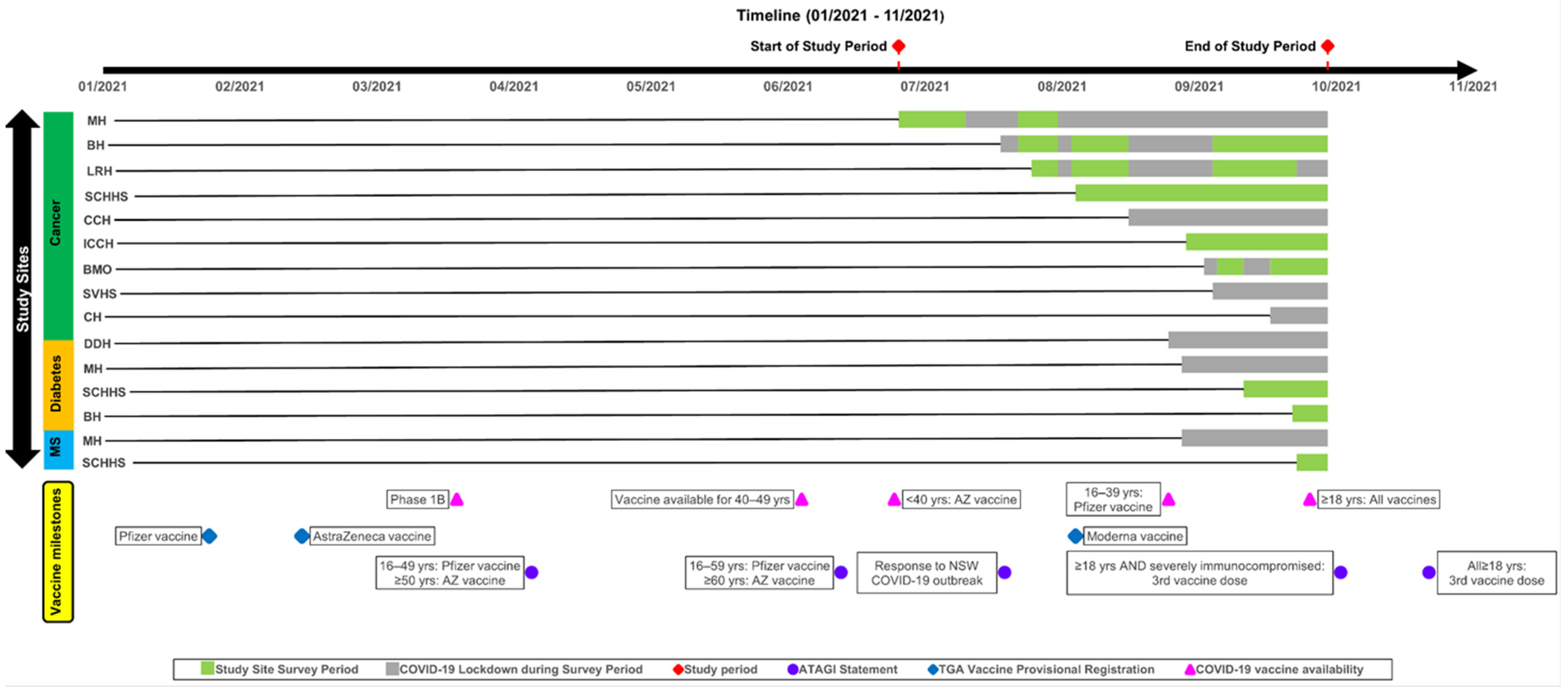
2. Materials and Methods
2.1. Participants and Procedures
2.2. Measures
2.2.1. Quantitative Measures
2.2.2. Qualitative Responses
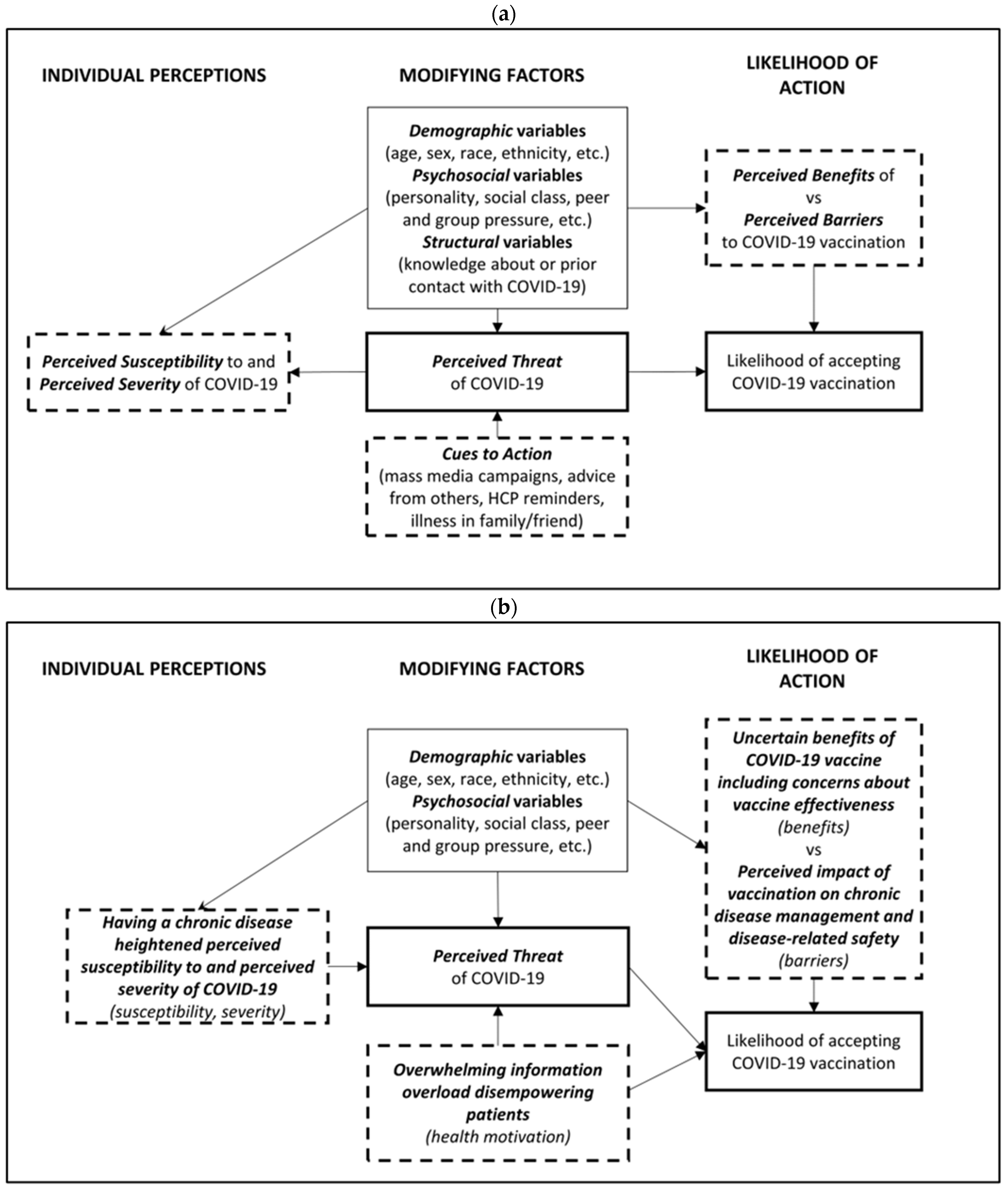
2.3. Data Analysis and Interpretative Framework
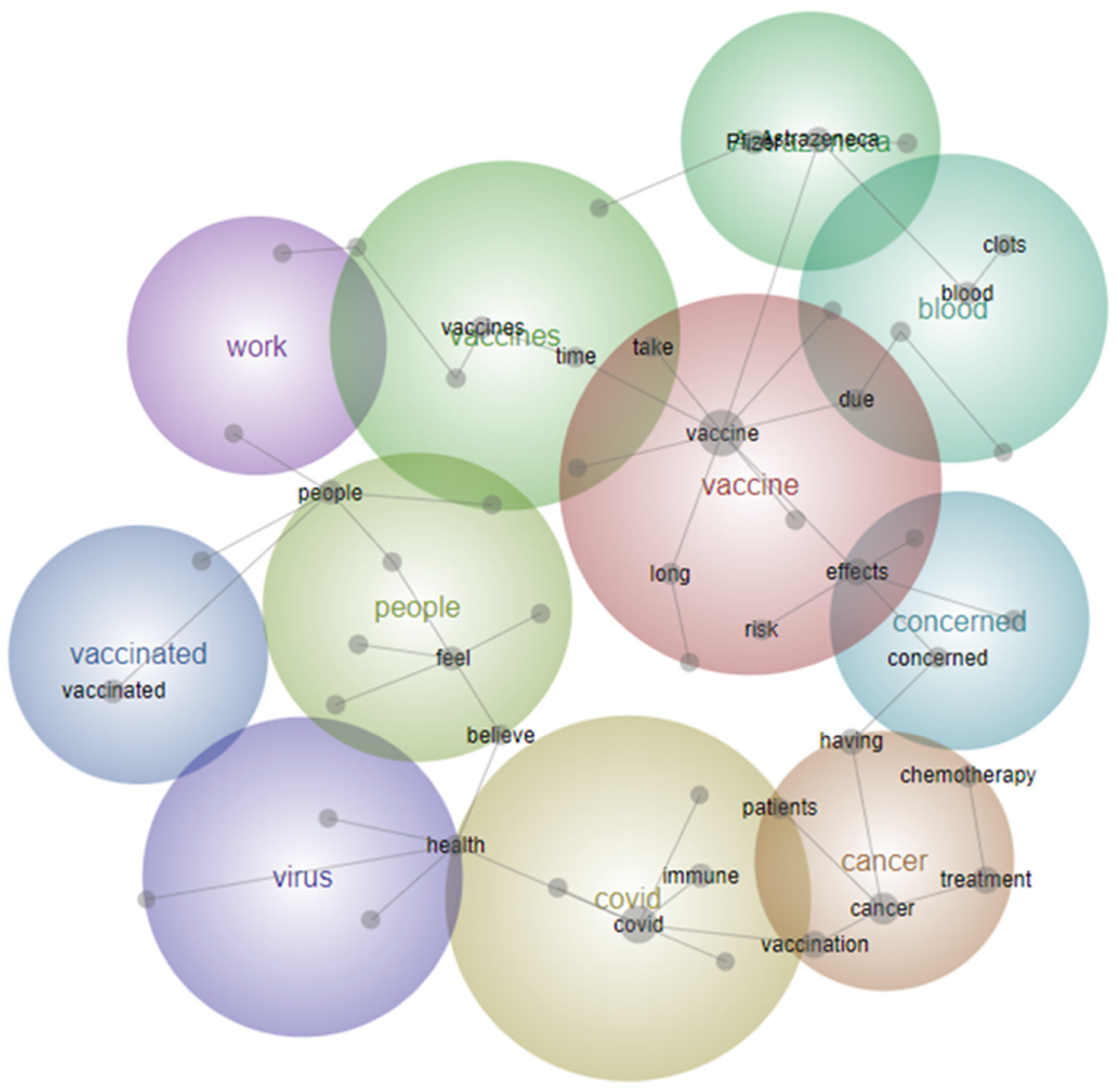
2.3.1. Qualitative Analysis
2.3.2. Trustworthiness and Rigour
2.3.3. Theoretical Framework
2.4. Consent and Ethics Statement
3. Results
3.1. Participant Characteristics
3.1.1. Commenters vs. Non-Commenters
3.1.2. Characteristics of Commenters
3.2. Key Themes
3.2.1. THEME 1. Having a Chronic Disease Heightened Perceived Susceptibility to, and Perceived Severity of COVID-19
Cancer patients like myself should be given an opportunity as soon as possible whilst doing chemotherapy, as we are more vulnerable due to our weakened immune [system] and health.(Breast cancer, localised, female, age 47, unvaccinated).
Got the COVID-19 shot as my immune system is weak due to type 2 diabetes.(Type 2 diabetes, female, age 64, vaccinated).
3.2.2. THEME 2. Perceived Impact of Vaccination on Chronic Disease Management and Disease-Related Safety
Having diabetes that isn’t well controlled at the moment, and knowledge of some of the side-effects being those that I am already [at] high risk for concerns me, so as much as I want the vaccine, I am scared to do it.(Type 1 diabetes, female, age 36, unvaccinated).
Already having a weak immune system prone to infection, I obviously am scared of what COVID-19 could do, but also scared of the minimal research on short term and long-term effects of the vaccine and what that could mean for my body.(MS, relapsing-remitting, female, age 32, unvaccinated).
I had concerns about getting COVID-19 and how it would affect my MS, how sick I would get if I got it. But I also had reservations at first about having vaccination as to how my body would react and how it would affect my MS.(MS, relapsing-remitting, female, age 53, vaccinated).
My MS is well controlled at this stage. So I would like to know whether [the] COVID-19 vaccine will push any of the symptoms of my MS and will make my life miserable.(MS, relapsing-remitting, female, age 32, unvaccinated).
I do believe that vaccines are necessary but I’m between a rock and a hard place. I don’t know how my body will react, both with heart disease, blood clotting in my legs and diabetes.(Type 2 diabetes, male, age 72, unvaccinated).
My only reservation was whether COVID-19 vaccine side effects may delay treatment. Thus [I] waited for a break in treatment before going ahead.(Gastrointestinal cancer, metastatic, male, age 58, vaccinated).
So hesitancy about the vaccine is not only about its effectiveness but also about longer term impacts on MS progression. There [are] simply no studies with data available to assist with the decision.(MS, primary progressive, female, age 42, vaccinated).
There [have] been no studies regarding targeted immune therapies and the COVID-19 vaccine. [As] cancer patients, our immune system is precious and this is a big unknown.(Lung cancer, metastatic, female, age 57, unvaccinated).
I am concerned about recent overseas studies which have shown decreased immune response after mRNA vaccination in patients on certain cancer drugs, and in particular Imatinib.(Blood cancer, female, age 50, vaccinated).
I am reluctant to take the vaccine until I have more data of the longer-term effects it has on someone with diabetes. Until then, I do not wish to risk any further inconvenience to being a diabetic.(Type 1 diabetes, male, age 25, unvaccinated).
I personally have had enough with the cancer treatment and am not willing to also be a guinea pig for this vaccine.(Head and neck cancer, localised, male, age 60, unvaccinated).
I honestly do not know what to do regarding vaccination. I am concerned about long term side-effects with COVID-19 vaccine.(Type 1 diabetes, female, age 46, unvaccinated).
I have [stage] 4 metastatic cancer. My immune system is shattered and I am terrified that the actual vaccine will either kill me or have a detrimental effect on my cancer treatment.(Breast cancer, metastatic, female, age 70, unvaccinated).
I am normally pro-vaccination but given my current diagnosis (terminal), I believe getting the vaccination could shorten my lifespan.(Gastrointestinal cancer, metastatic, female, age 61, unvaccinated).
3.2.3. THEME 3. Uncertain Benefits of COVID-19 Vaccine Including Concerns about Vaccine Effectiveness
I am currently on Gilenya [Fingolimod]. Research says effectiveness is only 3.7%. This is why I am not getting vaccinated.(MS, relapsing-remitting, female, age 39, unvaccinated).
I am worried that the efficacy [of the COVID-19 vaccine] will be lowered while undergoing treatment, especially chemotherapy.(Gastrointestinal cancer, localised, male, age 37, unvaccinated).
3.2.4. THEME 4. Overwhelming Information Overload Disempowering Patients
I am very confused with which vaccine would be best for me. I am concerned about both the Pfizer AND the AstraZeneca [vaccines] and I am wondering whether I should wait for the Moderna vaccination. It is all SO confusing!!!!!(Lung cancer, localised, female, age 63, unvaccinated).
Feeling unsure with all the negative commentary from some experts, [I] find it hard to trust and who to believe.(Type 2 diabetes, male, age 59, unvaccinated).
I am concerned by the levels of misinformation that are circulating, perpetuated in large part by a media more interested in ratings and ‘clickbait’ than science.(Type 2 diabetes, male, age 66, vaccinated).
I’m very confused, there are too many options and conspiracies that are tainting the facts, I just don’t know who to believe. I might even die before I know what’s real. It doesn’t matter if it’s COVID-19 or cancer. Dead is dead.(Genitourinary cancer, metastatic, male, age 59, unvaccinated).
Because of all the medications I take, I’m worried that taking the vaccine will endanger my life. An American friend of mine has had the Moderna vaccines...since the 2nd dose she has been in and out of hospital and has had constant fever.(Type 2 diabetes, female, age 56, unvaccinated).
4. Discussion
4.1. Heightened Susceptibility and Severity to COVID-19
4.2. Disruption to Chronic Disease Management
4.3. Vaccine Safety and Efficacy
4.4. Information Overload and Inconsistency
4.5. Implications for Future Research and Practice
4.6. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bendau, A.; Plag, J.; Petzold, M.B.; Strohle, A. COVID-19 vaccine hesitancy and related fears and anxiety. Int. Immunopharmacol. 2021, 97, 107724. [Google Scholar] [CrossRef] [PubMed]
- Polack, F.P.; Thomas, S.J.; Kitchin, N.; Absalon, J.; Gurtman, A.; Lockhart, S.; Perez, J.L.; Perez Marc, G.; Moreira, E.D.; Zerbini, C.; et al. Safety and Efficacy of the BNT162b2 mRNA Covid-19 Vaccine. N. Engl. J. Med. 2020, 383, 2603–2615. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Maruggi, G.; Shan, H.; Li, J. Advances in mRNA Vaccines for Infectious Diseases. Front. Immunol. 2019, 10, 594. [Google Scholar] [CrossRef] [PubMed]
- Day, D.; Grech, L.; Nguyen, M.; Bain, N.; Kwok, A.; Harris, S.; Chau, H.; Chan, B.; Blennerhassett, R.; Nott, L.; et al. Serious Underlying Medical Conditions and COVID-19 Vaccine Hesitancy: A Large Cross-Sectional Analysis from Australia. Vaccines 2022, 10, 851. [Google Scholar] [CrossRef]
- Epstein, S.; Xia, Z.; Lee, A.J.; Dahl, M.; Edwards, K.; Levit, E.; Longbrake, E.E.; Perrone, C.; Kavak, K.; Weinstock-Guttman, B.; et al. Vaccination Against SARS-CoV-2 in Neuroinflammatory Disease: Early Safety/Tolerability Data. Mult. Scler. Relat. Disord. 2022, 57, 103433. [Google Scholar] [CrossRef]
- Erdem, D.; Karaman, I. Impact of corona-phobia on attitudes and acceptance towards COVID-19 vaccine among cancer patients: A single-center study. Future Oncol. 2022, 18, 457–469. [Google Scholar] [CrossRef]
- Booth, A.; Reed, A.B.; Ponzo, S.; Yassaee, A.; Aral, M.; Plans, D.; Labrique, A.; Mohan, D. Population risk factors for severe disease and mortality in COVID-19: A global systematic review and meta-analysis. PLoS ONE 2021, 16, e0247461. [Google Scholar] [CrossRef]
- Australian Bureau of Statistics. Health Conditions Prevalence 2020–2021. Available online: https://www.abs.gov.au/statistics/health/health-conditions-and-risks/health-conditions-prevalence/latest-release (accessed on 21 December 2022).
- MacDonald, N.E. Vaccine hesitancy: Definition, scope and determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef]
- Solis Arce, J.S.; Warren, S.S.; Meriggi, N.F.; Scacco, A.; McMurry, N.; Voors, M.; Syunyaev, G.; Malik, A.A.; Aboutajdine, S.; Adeojo, O.; et al. COVID-19 vaccine acceptance and hesitancy in low- and middle-income countries. Nat. Med. 2021, 27, 1385–1394. [Google Scholar] [CrossRef]
- Ziello, A.; Scavone, C.; Di Battista, M.E.; Salvatore, S.; Di Giulio Cesare, D.; Moreggia, O.; Allegorico, L.; Sagnelli, A.; Barbato, S.; Manzo, V.; et al. Influenza Vaccine Hesitancy in Patients with Multiple Sclerosis: A Monocentric Observational Study. Brain Sci. 2021, 11, 890. [Google Scholar] [CrossRef]
- Cordina, M.; Lauri, M.A.; Lauri, J. Attitudes towards COVID-19 vaccination, vaccine hesitancy and intention to take the vaccine. Pharm. Pract. (Granada) 2021, 19, 2317. [Google Scholar] [CrossRef]
- Aldossari, K.K.; Alharbi, M.B.; Alkahtani, S.M.; Alrowaily, T.Z.; Alshaikhi, A.M.; Twair, A.A. COVID-19 vaccine hesitancy among patients with diabetes in Saudi Arabia. Diabetes Metab. Syndr. 2021, 15, 102271. [Google Scholar] [CrossRef]
- Osterholm, M.T.; Kelley, N.S.; Sommer, A.; Belongia, E.A. Efficacy and effectiveness of influenza vaccines: A systematic review and meta-analysis. Lancet Infect. Dis. 2012, 12, 36–44. [Google Scholar] [CrossRef]
- Barchielli, B.; Cricenti, C.; Gallè, F.; Sabella, E.A.; Liguori, F.; Da Molin, G.; Liguori, G.; Orsi, G.B.; Giannini, A.M.; Ferracuti, S.; et al. Climate Changes, Natural Resources Depletion, COVID-19 Pandemic, and Russian-Ukrainian War: What Is the Impact on Habits Change and Mental Health? Int. J. Environ. Res. Public Health 2022, 19, 11929. [Google Scholar] [CrossRef]
- Fisher, A.; Roberts, A.; McKinlay, A.R.; Fancourt, D.; Burton, A. The impact of the COVID-19 pandemic on mental health and well-being of people living with a long-term physical health condition: A qualitative study. BMC Public Health 2021, 21, 1801. [Google Scholar] [CrossRef]
- Tsai, R.; Hervey, J.; Hoffman, K.; Wood, J.; Johnson, J.; Deighton, D.; Clermont, D.; Loew, B.; Goldberg, S.L. COVID-19 Vaccine Hesitancy and Acceptance Among Individuals With Cancer, Autoimmune Diseases, or Other Serious Comorbid Conditions: Cross-sectional, Internet-Based Survey. JMIR Public Health Surveill. 2022, 8, e29872. [Google Scholar] [CrossRef]
- Al-Hanawi, M.K.; Ahmad, K.; Haque, R.; Keramat, S.A. Willingness to receive COVID-19 vaccination among adults with chronic diseases in the Kingdom of Saudi Arabia. J. Infect. Public Health 2021, 14, 1489–1496. [Google Scholar] [CrossRef]
- Liamputtong, P. Qualitative Research Methods, 5th ed.; Oxford University Press Australia and New Zealand: Melbourne, Australia, 2020. [Google Scholar]
- Steffens, M.S.; Bullivant, B.; King, C.; Bolsewicz, K. “I’m scared that if I have the vaccine, it’s going to make my lung condition worse, not better.” COVID-19 vaccine acceptance in adults with underlying health conditions—A qualitative investigation. Vaccine X 2022, 12, 100243. [Google Scholar] [CrossRef]
- Rosenstock, I.M. Historical Origins of the Health Belief Model. Health Educ. Monogr. 1974, 2, 328–335. [Google Scholar] [CrossRef]
- Santos, A.J.; Kislaya, I.; Machado, A.; Nunes, B. Beliefs and attitudes towards the influenza vaccine in high-risk individuals. Epidemiol. Infect. 2017, 145, 1786–1796. [Google Scholar] [CrossRef]
- Wong, M.C.S.; Wong, E.L.Y.; Huang, J.; Cheung, A.W.L.; Law, K.; Chong, M.K.C.; Ng, R.W.Y.; Lai, C.K.C.; Boon, S.S.; Lau, J.T.F.; et al. Acceptance of the COVID-19 vaccine based on the health belief model: A population-based survey in Hong Kong. Vaccine 2021, 39, 1148–1156. [Google Scholar] [CrossRef] [PubMed]
- Servidio, R.; Malvaso, A.; Vizza, D.; Valente, M.; Campagna, M.R.; Iacono, M.L.; Martin, L.R.; Bruno, F. The intention to get COVID-19 vaccine and vaccine uptake among cancer patients: An extension of the theory of planned behaviour (TPB). Support. Care Cancer 2022, 30, 7973–7982. [Google Scholar] [CrossRef] [PubMed]
- Freeman, D.; Loe, B.S.; Chadwick, A.; Vaccari, C.; Waite, F.; Rosebrock, L.; Jenner, L.; Petit, A.; Lewandowsky, S.; Vanderslott, S.; et al. COVID-19 vaccine hesitancy in the UK: The Oxford coronavirus explanations, attitudes, and narratives survey (Oceans) II. Psychol. Med. 2020, 52, 3127–3141. [Google Scholar] [CrossRef] [PubMed]
- Grech, L.; Loe, B.S.; Day, D.; Freeman, D.; Kwok, A.; Nguyen, M.; Bain, N.; Segelov, E. The Disease Influenced Vaccine Acceptance Scale-Six (DIVAS-6): Validation of a Measure to Assess Disease-Related COVID-19 Vaccine Attitudes and Concerns. Behav. Med. 2022, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Leximancer. Available online: https://info.leximancer.com/ (accessed on 10 January 2023).
- Smith, A.E.; Humphreys, M.S. Evaluation of unsupervised semantic mapping of natural language with Leximancer concept mapping. Behav. Res. Methods 2006, 38, 262–279. [Google Scholar] [CrossRef]
- Angus, D.; Rintel, S.; Wiles, J. Making sense of big text: A visual-first approach for analysing text data using Leximancer and Discursis. Int. J. Soc. Res. Methodol. 2013, 16, 261–267. [Google Scholar] [CrossRef]
- Wang, Y.; Duan, L.; Li, M.; Wang, J.; Yang, J.; Song, C.; Li, J.; Wang, J.; Jia, J.; Xu, J. COVID-19 Vaccine Hesitancy and Associated Factors among Diabetes Patients: A Cross-Sectional Survey in Changzhi, Shanxi, China. Vaccines 2022, 10, 129. [Google Scholar] [CrossRef]
- Rodriguez, M.; López-Cepero, A.; Ortiz-Martínez, A.P.; Fernández-Repollet, E.; Pérez, C.M. Influence of Health Beliefs on COVID-19 Vaccination among Individuals with Cancer and Other Comorbidities in Puerto Rico. Vaccines 2021, 9, 994. [Google Scholar] [CrossRef]
- Kaufman, J.; Bagot, K.L.; Tuckerman, J.; Biezen, R.; Oliver, J.; Jos, C.; Ong, D.S.; Manski-Nankervis, J.A.; Seale, H.; Sanci, L.; et al. Qualitative exploration of intentions, concerns and information needs of vaccine-hesitant adults initially prioritised to receive COVID-19 vaccines in Australia. Aust. N. Z. J. Public Health 2022, 46, 16–24. [Google Scholar] [CrossRef]
- Sattui, S.E.; Liew, J.W.; Kennedy, K.; Sirotich, E.; Putman, M.; Moni, T.T.; Akpabio, A.; Alpízar-Rodríguez, D.; Berenbaum, F.; Bulina, I.; et al. Early experience of COVID-19 vaccination in adults with systemic rheumatic diseases: Results from the COVID-19 Global Rheumatology Alliance Vaccine Survey. RMD Open 2021, 7, e001814. [Google Scholar] [CrossRef]
- Ehde, D.M.; Roberts, M.K.; Herring, T.E.; Alschuler, K.N. Willingness to obtain COVID-19 vaccination in adults with multiple sclerosis in the United States. Mult. Scler. Relat. Disord. 2021, 49, 102788. [Google Scholar] [CrossRef]
- Wargo, J.A.; Reuben, A.; Cooper, Z.A.; Oh, K.S.; Sullivan, R.J. Immune effects of chemotherapy, radiation, and targeted therapy and opportunities for combination with immunotherapy. Semin. Oncol. 2015, 42, 601–616. [Google Scholar] [CrossRef]
- Al-Khamis, F.A. The use of immune modulating drugs for the treatment of multiple sclerosis. Neurosciences (Riyadh) 2016, 21, 4–9. [Google Scholar] [CrossRef]
- Gonzalez, H.; Hagerling, C.; Werb, Z. Roles of the immune system in cancer: From tumor initiation to metastatic progression. Genes Dev. 2018, 32, 1267–1284. [Google Scholar] [CrossRef]
- Wu, X.; Wang, L.; Shen, L.; Tang, K. Response of COVID-19 vaccination in multiple sclerosis patients following disease-modifying therapies: A meta-analysis. eBioMedicine 2022, 81, 104102. [Google Scholar] [CrossRef]
- Liu, H.; Chen, S.; Liu, M.; Nie, H.; Lu, H. Comorbid chronic ciseases are strongly correlated with disease severity among COVID-19 patients: A systematic review and meta-analysis. Aging Dis. 2020, 11, 668–678. [Google Scholar] [CrossRef]
- Australian Government Department of Health and Aged Care. Priority Groups for COVID-19 Vaccination Program: Phase 1B. Available online: https://www.health.gov.au/sites/default/files/documents/2021/03/priority-groups-for-covid-19-vaccination-program-phase-1b_1.pdf (accessed on 22 December 2022).
- Mekkawi, R.; Elkattan, B.A.; Shablak, A.; Bakr, M.; Yassin, M.A.; Omar, N.E. COVID-19 vaccination in cancer patients: A review article. Cancer Control 2022, 29, 10732748221106266. [Google Scholar] [CrossRef]
- Nabavi, S.M.; Mehrabani, M.; Ghalichi, L.; Nahayati, M.A.; Ghaffari, M.; Ashtari, F.; Mohammadianinejad, S.E.; Karimi, S.; Faghani, L.; Yazdanbakhsh, S.; et al. COVID-19 Vaccination Willingness and Acceptability in Multiple Sclerosis Patients: A Cross Sectional Study in Iran. Vaccines 2022, 10, 135. [Google Scholar] [CrossRef]
- Mailand, M.T.; Frederiksen, J.L. Vaccines and multiple sclerosis: A systematic review. J. Neurol. 2017, 264, 1035–1050. [Google Scholar] [CrossRef]
- Nistri, R.; Barbuti, E.; Rinaldi, V.; Tufano, L.; Pozzilli, V.; Ianniello, A.; Marinelli, F.; De Luca, G.; Prosperini, L.; Tomassini, V.; et al. Case report: Multiple sclerosis relapses after vaccination against SARS-CoV2: A series of clinical cases. Front. Neurol. 2021, 12, 765954. [Google Scholar] [CrossRef]
- Berbudi, A.; Rahmadika, N.; Tjahjadi, A.I.; Ruslami, R. Type 2 Diabetes and its Impact on the Immune System. Curr. Diabetes Rev. 2020, 16, 442–449. [Google Scholar] [CrossRef] [PubMed]
- Scoccimarro, D.; Panichi, L.; Ragghianti, B.; Silverii, A.; Mannucci, E.; Monami, M. Sars-CoV2 vaccine hesitancy in Italy: A survey on subjects with diabetes. Nutr. Metab. Cardiovasc. Dis. 2021, 31, 3243–3246. [Google Scholar] [CrossRef]
- Yazdani, A.; Mirmosayyeb, O.; Ghaffary, E.M.; Hashemi, M.S.; Ghajarzadeh, M. COVID-19 vaccines and patients with multiple sclerosis: Willingness, unwillingness and hesitancy: A systematic review and meta-analysis. Neurol. Sci. 2022, 43, 4085–4094. [Google Scholar] [CrossRef] [PubMed]
- Chebel, R.; Labaki, C.; Farhat, M.; Kattan, J. Safety, efficacy and acceptability of SARS-CoV-2 vaccines in patients with cancer. Future Virol. 2021, 16, 443–446. [Google Scholar] [CrossRef] [PubMed]
- Fendler, A.; de Vries, E.G.E.; GeurtsvanKessel, C.H.; Haanen, J.B.; Wörmann, B.; Turajlic, S.; von Lilienfeld-Toal, M. COVID-19 vaccines in patients with cancer: Immunogenicity, efficacy and safety. Nat. Rev. Clin. Oncol. 2022, 19, 385–401. [Google Scholar] [CrossRef]
- Alduraywish, S.A.; Altamimi, L.A.; Aldhuwayhi, R.A.; AlZamil, L.R.; Alzeghayer, L.Y.; Alsaleh, F.S.; Aldakheel, F.M.; Tharkar, S. Sources of health information and their impacts on medical knowledge perception among the Saudi Arabian population: Cross-sectional study. J. Med. Internet Res. 2020, 22, e14414. [Google Scholar] [CrossRef]
- Hesse, B.W.; Nelson, D.E.; Kreps, G.L.; Croyle, R.T.; Arora, N.K.; Rimer, B.K.; Viswanath, K. Trust and Sources of health Information: The impact of the internet and its implications for health care providers: Findings from the first Health Information National Trends survey. Arch. Internal Med. 2005, 165, 2618–2624. [Google Scholar] [CrossRef]
- Australian Government COVID-19 Vaccine Roll-Out Update—5 October 2021. Available online: https://www.health.gov.au/sites/default/files/documents/2021/10/covid-19-vaccine-rollout-update-5-october-2021_0.pdf (accessed on 21 December 2022).
- Cook, E.J.; Elliott, E.; Gaitan, A.; Nduka, I.; Cartwright, S.; Egbutah, C.; Randhawa, G.; Waqar, M.; Ali, N. Vaccination against COVID-19: Factors That Influence Vaccine Hesitancy among an Ethnically Diverse Community in the UK. Vaccines 2022, 10, 106. [Google Scholar] [CrossRef]
- Vanderpool, R.C.; Gaysynsky, A.; Chou, W.-Y.S.; Tonorezos, E.S. Using Behavioral Science to Address COVID-19 Vaccine Hesitancy Among Cancer Survivors: Communication Strategies and Research Opportunities. J. Behav. Med. 2022. [Google Scholar] [CrossRef]
| Characteristic | All n = 1604 n, (%) | Cancer n = 1248 n, (%) | Diabetes n = 244 n, (%) | MS n = 112 n, (%) |
|---|---|---|---|---|
| Gender a | ||||
| Male | 658 (41.0) | 511 (40.9) | 120 (49.2) | 27 (24.1) |
| Female | 937 (58.4) | 730 (58.5) | 124 (50.8) | 83 (74.1) |
| Age (years) | ||||
| Median (Range) | 62.0 (19.0–88.0) | 64.0 (20.0–88.0) | 58.0 (19.0–87.0) | 47.0 (19.0–77.0) |
| 18–29 | 34 (2.1) | 9 (0.7) | 14 (5.7) | 11 (9.8) |
| 30–49 | 272 (17.0) | 166 (13.3) | 54 (22.1) | 52 (46.4) |
| 50–69 | 876 (54.6) | 687 (55.0) | 145 (59.4) | 44 (39.3) |
| ≥70 | 422 (26.3) | 386 (30.9) | 31 (12.7) | 5 (4.5) |
| Highest level of education b | ||||
| No formal/primary school | 40 (2.5) | 27 (2.2) | 10 (4.1) | 3 (2.7) |
| Secondary school | 450 (28.1) | 340 (27.2) | 79 (32.4) | 31 (27.7) |
| Vocational/Trade | 416 (25.9) | 320 (25.6) | 69 (28.3) | 27 (24.1) |
| University | 693 (43.2) | 559 (44.8) | 84 (34.4) | 50 (44.6) |
| Annual household income (AUD) | ||||
| <50 K | 530 (33.0) | 405 (32.5) | 99 (40.6) | 26 (23.2) |
| 50–100 K | 411 (25.6) | 310 (24.8) | 68 (27.9) | 33 (29.5) |
| 100 K–150 K | 213 (13.3) | 174 (13.9) | 23 (9.4) | 16 (14.3) |
| >150 K | 188 (11.7) | 153 (12.3) | 20 (8.2) | 15 (13.4) |
| Prefer not to say | 262 (16.3) | 206 (16.5) | 34 (13.9) | 22 (19.6) |
| Aboriginal/Torres Strait Islander c | ||||
| Yes | 23 (1.4) | 18 (1.4) | 5 (2.0) | 0 (0.0) |
| No | 1558 (97.1) | 1212 (97.1) | 234 (95.9) | 112 (100.0) |
| English as dominant language | ||||
| Yes | 1453 (90.6) | 1150 (92.1) | 203 (83.2) | 100 (89.3) |
| No | 151 (9.4) | 98 (7.9) | 41 (16.8) | 12 (10.7) |
| Location | ||||
| Metropolitan | 1072 (66.8) | 808 (64.7) | 171 (70.1) | 93 (83.0) |
| Regional | 532 (33.2) | 440 (35.3) | 73 (29.9) | 19 (17.0) |
| Location (state) | ||||
| Victoria | 669 (41.7) | 433 (34.7) | 143 (58.6) | 93 (83.0) |
| New South Wales | 592 (36.9) | 553 (44.3) | 39 (16.0) | 0 (0.0) |
| Border (Victoria/New South Wales) | 12 (0.7) | 12 (1.0) | 0 (0.0) | 0 (0.0) |
| Queensland | 247 (15.4) | 166 (13.3) | 62 (25.4) | 19 (17.0) |
| Tasmania | 84 (5.2) | 84 (6.7) | 0 (0.0) | 0 (0.0) |
| Vaccination status | ||||
| 1 dose | 321 (20.0) | 270 (21.6) | 39 (16.0) | 12 (10.7) |
| 2 doses | 841 (52.4) | 636 (51.0) | 132 (54.1) | 73 (65.2) |
| No doses | 442 (27.6) | 342 (27.4) | 73 (29.9) | 27 (24.1) |
| Vaccination intent d | ||||
| Likely | 1330 (82.9) | 1056 (84.6) | 183 (75.0) | 91 (81.3) |
| Unsure | 141 (8.8) | 102 (8.2) | 28 (11.5) | 11 (9.8) |
| Unlikely | 133 (8.3) | 90 (7.2) | 33 (13.5) | 10 (8.9) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Choi, T.; Chan, B.; Grech, L.; Kwok, A.; Webber, K.; Wong, J.; Nguyen, M.; Bain, N.; Day, D.; McCartney, A.; et al. Factors Influencing COVID-19 Vaccine Hesitancy among Patients with Serious Chronic Illnesses during the Initial Australian Vaccine Rollout: A Multi-Centre Qualitative Analysis Using the Health Belief Model. Vaccines 2023, 11, 239. https://doi.org/10.3390/vaccines11020239
Choi T, Chan B, Grech L, Kwok A, Webber K, Wong J, Nguyen M, Bain N, Day D, McCartney A, et al. Factors Influencing COVID-19 Vaccine Hesitancy among Patients with Serious Chronic Illnesses during the Initial Australian Vaccine Rollout: A Multi-Centre Qualitative Analysis Using the Health Belief Model. Vaccines. 2023; 11(2):239. https://doi.org/10.3390/vaccines11020239
Chicago/Turabian StyleChoi, Tammie, Bryan Chan, Lisa Grech, Alastair Kwok, Kate Webber, Jennifer Wong, Mike Nguyen, Nathan Bain, Daphne Day, Amelia McCartney, and et al. 2023. "Factors Influencing COVID-19 Vaccine Hesitancy among Patients with Serious Chronic Illnesses during the Initial Australian Vaccine Rollout: A Multi-Centre Qualitative Analysis Using the Health Belief Model" Vaccines 11, no. 2: 239. https://doi.org/10.3390/vaccines11020239
APA StyleChoi, T., Chan, B., Grech, L., Kwok, A., Webber, K., Wong, J., Nguyen, M., Bain, N., Day, D., McCartney, A., Hamer, R., Segelov, E., & on behalf of the CANVACCS DIABVACCS and MSVACCS Investigators. (2023). Factors Influencing COVID-19 Vaccine Hesitancy among Patients with Serious Chronic Illnesses during the Initial Australian Vaccine Rollout: A Multi-Centre Qualitative Analysis Using the Health Belief Model. Vaccines, 11(2), 239. https://doi.org/10.3390/vaccines11020239







