Challenges and Opportunities in the Process Development of Chimeric Vaccines
Abstract
1. Introduction
2. Chimeric Vaccines: Future of Vaccinology with State-of-the-Art Technologies
- Robust immune response against multiple infectious agents;
- Elevated humoral response generated by B-cell lymphocyte epitopes;
- Elevated cytotoxic immunity elicited by T-cell lymphocyte epitopes;
- Good safety profile with no risk of exposure to infectious agents;
- Provides cross-neutralization activity in a single formulation;
- Effective against multi-drug resistant pathogens;
- Selected adjuvants provide an elevated immune response;
- Higher stability;
- Ease of storage and transportation;
- Rapid and reproducible large-scale production.
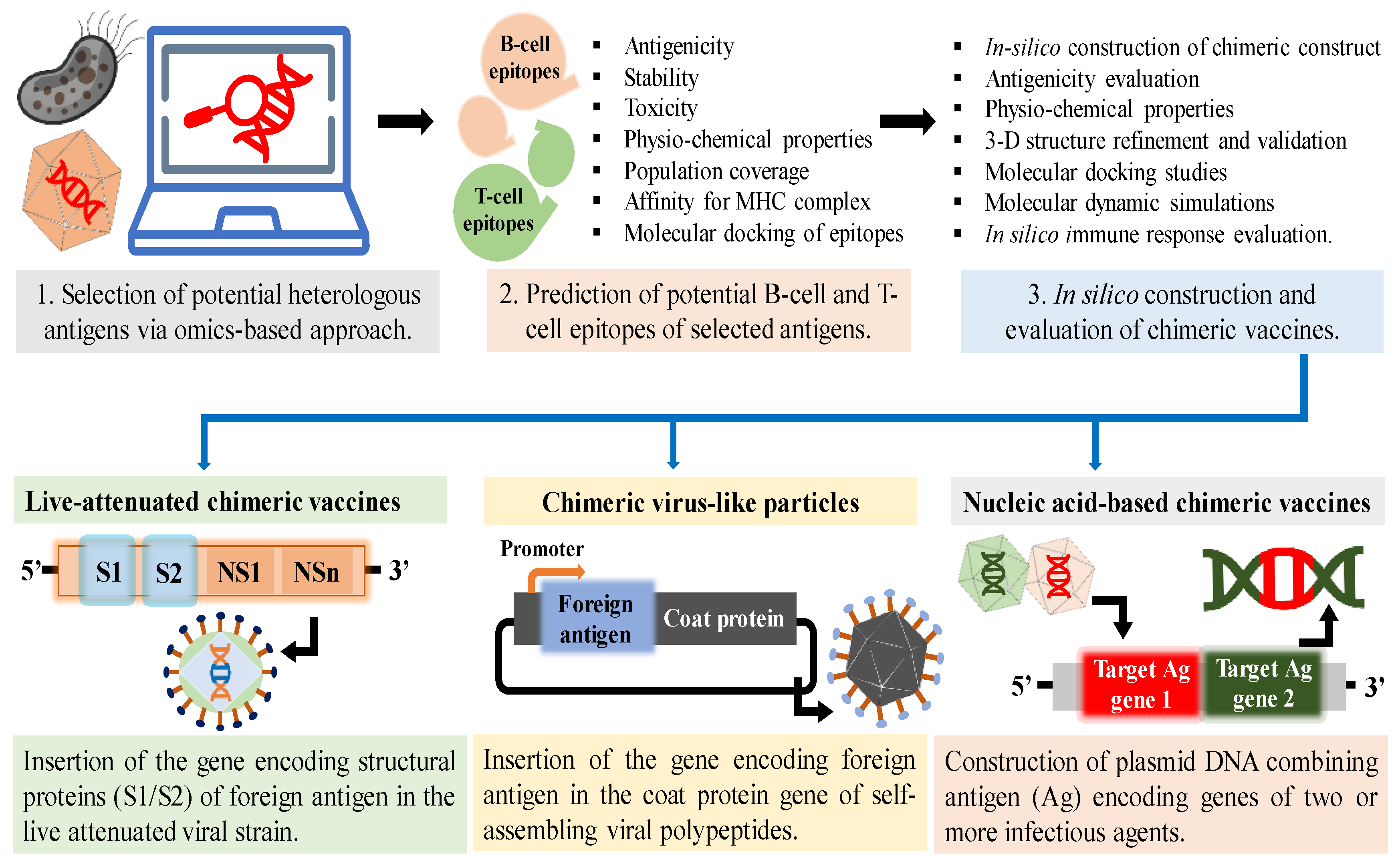
2.1. Strategies to Design Chimeric Vaccines
2.2. Types of Chimeric Vaccines
3. Bioprocess Development of Chimeric Vaccines: Challenges and Opportunities
4. Expression Platforms and Upstream Process Development of Chimeric Vaccines
4.1. Bacterial Expression System
4.2. Yeast Expression System
4.3. Insect Cell Expression System
4.4. Mammalian Cell Expression System
4.5. Other Expression Platforms
5. Emergent Technologies in Upstream Process Development
6. Downstream Process Development: Current Approaches and Future Trends
6.1. Chromatography Techniques: Conventional and Modern Approaches
6.2. Emergent Technologies in Product Recovery
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Arnon, R.; Ben-Yedidia, T. Old and new vaccine approaches. Int. Immunopharmacol. 2003, 3, 1195–1204. [Google Scholar] [CrossRef]
- Minor, P.D. Live attenuated vaccines: Historical successes and current challenges. Virology 2015, 479–480, 379–392. [Google Scholar] [CrossRef]
- Plotkin, S. History of vaccination. Proc. Natl. Acad. Sci. USA 2014, 111, 12283–12287. [Google Scholar] [CrossRef]
- Schneerson, R.; Robbins, J.B.; Taranger, J.; Lagergard, T.; Trollfors, B. A toxoid vaccine for pertussis as well as diphtheria? Lessons to be relearned. Lancet 1996, 348, 1289–1292. [Google Scholar] [CrossRef]
- Girard, M.P.; Preziosi, M.P.; Aguado, M.T.; Kieny, M.P. A review of vaccine research and development: Meningococcal disease. Vaccine 2006, 24, 4692–4700. [Google Scholar] [CrossRef]
- Paton, J.C.; Trappetti, C. Streptococcus pneumoniae capsular polysaccharide. Microbiol. Spectr. 2019, 7, 33. [Google Scholar] [CrossRef]
- Kong, Q.; Richter, L.; Yang, Y.F.; Arntzen, C.J.; Mason, H.S.; Thanavala, Y. Oral immunization with hepatitis B surface antigen expressed in transgenic plants. Proc. Natl. Acad. Sci. USA 2001, 98, 11539–11544. [Google Scholar] [CrossRef]
- Josefsberg, J.O.; Buckland, B. Vaccine process technology. Biotechnol. Bioeng. 2012, 109, 1443–1460. [Google Scholar] [CrossRef]
- Gomez, P.L.; Robinson, J.M.; Rogalewicz, J.A. Vaccine manufacturing. In Vaccines; Elsevier Inc.: Amsterdam, The Netherlands, 2013; p. 44. [Google Scholar] [CrossRef]
- Nooraei, S.; Bahrulolum, H.; Hoseini, Z.S.; Katalani, C.; Hajizade, A.; Easton, A.J.; Ahmadian, G. Virus-like particles: Preparation, immunogenicity and their roles as nanovaccines and drug nanocarriers. J. Nanobiotechnol. 2021, 19, 59. [Google Scholar] [CrossRef]
- Finn, A.; Heath, P. Conjugate vaccines. Arch. Dis. Child. 2005, 90, 667–669. [Google Scholar] [CrossRef][Green Version]
- Sucher, A.J.; Chahine, E.B.; Nelson, M.; Sucher, B.J. Prevnar 13, the new 13-valent pneumococcal conjugate vaccine. Ann. Pharmacother. 2011, 45, 1516–1524. [Google Scholar] [CrossRef]
- Recombivax HB®. Available online: https://www.merckvaccines.com/recombivax-hb/ (accessed on 5 July 2023).
- Engerix®. Available online: https://www.fda.gov/vaccines-blood-biologics/vaccines/engerix-b (accessed on 5 July 2023).
- GeneVac-B. Available online: https://www.seruminstitute.com/product_ind_genevacb.php (accessed on 5 July 2023).
- Zuckerman, J.N.; Zuckerman, A.J. Recombinant hepatitis B triple antigen vaccine: Hepacare. Expert Rev. Vaccines 2002, 1, 141–144. [Google Scholar] [CrossRef]
- Twinrix. Available online: https://www.fda.gov/vaccines-blood-biologics/vaccines/twinrix (accessed on 5 July 2023).
- HBVaxPRO®. Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/hbvaxpro (accessed on 5 July 2023).
- LYMErix®. Available online: https://www.rxlist.com/lymerix-drug.htm (accessed on 5 July 2023).
- Trumenba®. Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/trumenba (accessed on 5 July 2023).
- Bexsero®. Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/bexsero (accessed on 5 July 2023).
- Gardasil®. Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/gardasil (accessed on 5 July 2023).
- Gardasil 9. Available online: https://www.fda.gov/vaccines-blood-biologics/vaccines/gardasil-9 (accessed on 5 July 2023).
- Cecolin®. Available online: https://extranet.who.int/pqweb/content/cecolin%C2%AE (accessed on 5 July 2023).
- MosquirixTM. Available online: https://www.ema.europa.eu/en/opinion-medicine-use-outside-EU/human/mosquirix (accessed on 5 July 2023).
- SHINGRIX. Available online: https://www.fda.gov/vaccines-blood-biologics/vaccines/shingrix (accessed on 5 July 2023).
- Ghaffarifar, F. Plasmid DNA vaccines: Where are we now? Drugs Today 2018, 54, 315–333. [Google Scholar] [CrossRef]
- Isaguliants, M.; Burt, F.J. Perspective Technologies of Vaccination: Do We Still Need Old Vaccines? Vaccines 2022, 10, 891. [Google Scholar] [CrossRef]
- Ulmer, J.B.; Mason, P.W.; Geall, A.; Mandl, C.W. RNA-based vaccines. Vaccine 2012, 30, 4414–4418. [Google Scholar] [CrossRef]
- Soria-Guerra, R.E.; Moreno-Fierros, L.; Rosales-Mendoza, S. Two decades of plant-based candidate vaccines: A review of the chimeric protein approaches. Plant Cell Rep. 2011, 30, 1367–1382. [Google Scholar] [CrossRef]
- Bárcena, J.; Blanco, E. Design of novel vaccines based on virus-like particles or chimeric virions. In Structure and Physics of Viruses. Subcellular Biochemistry; Mateu, M., Ed.; Springer: Dordrecht, The Netherlands, 2013; pp. 631–665. [Google Scholar] [CrossRef]
- Monterrubio-Lopez, G.P.; Delgadillo-Gutierrez, K. Reverse vaccinology: Strategy against emerging pathogens. Rev. Med. Inst. Mex. Seguro Soc. 2021, 59, 233–241. [Google Scholar]
- Ysrafil, Y.; Sapiun, Z.; Astuti, I.; Anasiru, M.A.; Slamet, N.S.; Hartati, H.; Husain, F.; Damiti, S.A. Designing multi-epitope based peptide vaccine candidates against SARS-CoV-2 using immunoinformatics approach. Bioimpacts 2022, 12, 359. [Google Scholar] [CrossRef]
- Dorosti, H.; Eskandari, S.; Zarei, M.; Nezafat, N.; Ghasemi, Y. Design of a multi-epitope protein vaccine against herpes simplex virus, human papillomavirus and Chlamydia trachomatis as the main causes of sexually transmitted diseases. Infect. Genet. Evol. 2021, 96, 105136. [Google Scholar] [CrossRef]
- Berzofsky, J.A.; Ahlers, J.D.; Belyakov, I.M. Strategies for designing and optimizing new generation vaccines. Nat. Rev. Immunol. 2001, 1, 209–219. [Google Scholar] [CrossRef]
- Abadi, M.H.J.N.; Abyaneh, F.A.; Zare, N.; Zamani, J.; Abdoli, A.; Aslanbeigi, F.; Hamblin, M.R.; Tarrahimofrad, H.; Rahimi, M.; Hashemian, S.M. In silico design and immunoinformatics analysis of a chimeric vaccine construct based on Salmonella pathogenesis factors. Microb. Pathog. 2023, 180, 106130. [Google Scholar] [CrossRef]
- Khan, M.A.; Amin, A.; Farid, A.; Ullah, A.; Waris, A.; Shinwari, K.; Hussain, Y.; Alsharif, K.F.; Alzahrani, K.J.; Khan, H. Recent Advances in Genomics-Based Approaches for the Development of Intracellular Bacterial Pathogen Vaccines. Pharmaceutics 2022, 15, 152. [Google Scholar] [CrossRef]
- Satyam, R.; Bhardwaj, T.; Jha, N.K.; Jha, S.K.; Nand, P. Toward a chimeric vaccine against multiple isolates of Mycobacteroides—An integrative approach. Life Sci. 2020, 250, 117541. [Google Scholar] [CrossRef]
- Donnarumma, D.; Faleri, A.; Costantino, P.; Rappuoli, R.; Norais, N. The role of structural proteomics in vaccine development: Recent advances and future prospects. Expert Rev. Proteomics 2016, 13, 55–68. [Google Scholar] [CrossRef] [PubMed]
- Hossan, M.I.; Chowdhury, A.S.; Hossain, M.U.; Khan, M.A.; Mahmood, T.B.; Mizan, S. Immunoinformatics aided-design of novel multi-epitope based peptide vaccine against Hendra henipavirus through proteome exploration. Inform. Med. Unlocked 2021, 25, 100678. [Google Scholar] [CrossRef]
- Shah, S.Z.; Jabbar, B.; Mirza, M.U.; Waqas, M.; Aziz, S.; Halim, S.A.; Ali, A.; Rafique, S.; Idrees, M.; Khalid, A. An Immunoinformatics Approach to Design a Potent Multi-Epitope Vaccine against Asia-1 Genotype of Crimean–Congo Haemorrhagic Fever Virus Using the Structural Glycoproteins as a Target. Vaccines 2022, 11, 61. [Google Scholar] [CrossRef]
- Kaliamurthi, S.; Selvaraj, G.; Chinnasamy, S.; Wang, Q.; Nangraj, A.S.; Cho, W.C.; Gu, K.; Wei, D.Q. Exploring the Papillomaviral Proteome to Identify Potential Candidates for a Chimeric Vaccine against Cervix Papilloma Using Immunomics and Computational Structural Vaccinology. Viruses 2019, 11, 63. [Google Scholar] [CrossRef]
- Waheed, Y.; Sah, R.; Muhammad, K. Recent developments in vaccines for viral diseases. Vaccines 2023, 11, 198. [Google Scholar] [CrossRef]
- Choo, J.J.; Vet, L.J.; McMillan, C.L.; Harrison, J.J.; Scott, C.A.; Depelsenaire, A.C.; Fernando, G.J.; Watterson, D.; Hall, R.A.; Young, P.R. A chimeric dengue virus vaccine candidate delivered by high density microarray patches protects against infection in mice. npj Vaccines 2021, 6, 66. [Google Scholar] [CrossRef] [PubMed]
- Vet, L.J.; Setoh, Y.X.; Amarilla, A.A.; Habarugira, G.; Suen, W.W.; Newton, N.D.; Harrison, J.J.; Hobson-Peters, J.; Hall, R.A.; Bielefeldt-Ohmann, H. Protective efficacy of a chimeric insect-specific flavivirus vaccine against West Nile virus. Vaccines 2020, 8, 258. [Google Scholar] [CrossRef]
- Adam, A.; Lee, C.; Wang, T. Rational Development of Live-Attenuated Zika Virus Vaccines. Pathogens 2023, 12, 194. [Google Scholar] [CrossRef]
- Mhaske, A.; Singh, S.; Abourehab, M.A.; Kumar, A.; Kesharwani, P.; Shukla, R. Recent pharmaceutical engineered trends as theranostics for Japanese Encephalitis. Process Biochem. 2022, 122, 115–127. [Google Scholar] [CrossRef]
- Chokephaibulkit, K.; Houillon, G.; Feroldi, E.; Bouckenooghe, A. Safety and immunogenicity of a live attenuated Japanese encephalitis chimeric virus vaccine (IMOJEV®) in children. Expert Rev. Vaccines 2016, 15, 153–166. [Google Scholar] [CrossRef] [PubMed]
- Lei, X.; Cai, X.; Yang, Y. Genetic engineering strategies for construction of multivalent chimeric VLPs vaccines. Expert Rev. Vaccines 2020, 19, 235–246. [Google Scholar] [CrossRef]
- Tang, S.; Xuan, B.; Ye, X.; Huang, Z.; Qian, Z. A modular vaccine development platform based on sortase-mediated site-specific tagging of antigens onto virus-like particles. Sci. Rep. 2016, 6, 25741. [Google Scholar] [CrossRef]
- Kheirvari, M.; Liu, H.; Tumban, E. Virus-like Particle Vaccines and Platforms for Vaccine Development. Viruses 2023, 15, 1109. [Google Scholar] [CrossRef] [PubMed]
- Laurens, M.B. RTS,S/AS01 vaccine (Mosquirix): An overview. Hum. Vaccines Immunother. 2020, 16, 480–489. [Google Scholar] [CrossRef]
- Ojha, R.; Singh, S.; Gupta, N.; Kumar, K.; Padhi, A.K.; Prajapati, V.K. Multi-pathogen based chimeric vaccine to fight against COVID-19 and concomitant coinfections. Biotechnol. Lett. 2023, 45, 779–797. [Google Scholar] [CrossRef]
- Lage, D.P.; Vale, D.L.; Linhares, F.P.; Freitas, C.S.; Machado, A.S.; Cardoso, J.M.; de Oliveira, D.; Galvani, N.C.; de Oliveira, M.P.; Oliveira-da-Silva, J.A. A recombinant chimeric protein-based vaccine containing T-cell epitopes from amastigote proteins and combined with distinct adjuvants, induces immunogenicity and protection against leishmania infantum infection. Vaccines 2022, 10, 1146. [Google Scholar] [CrossRef]
- Riccardo, F.; Bolli, E.; Macagno, M.; Arigoni, M.; Cavallo, F.; Quaglino, E. Chimeric DNA vaccines: An effective way to overcome immune tolerance. Curr. Top. Microbiol. Immunol. 2017, 405, 99–122. [Google Scholar] [CrossRef]
- Zareitaher, T.; Ahmadi, T.S.; Gargari, S.L.M. Immunogenic efficacy of DNA and protein-based vaccine from a chimeric gene consisting OmpW, TcpA and CtxB, of Vibrio cholerae. Immunobiology 2022, 227, 152190. [Google Scholar] [CrossRef]
- Jeong, H.; Choi, Y.-M.; Seo, H.; Kim, B.-J. A novel DNA vaccine against SARS-CoV-2 encoding a chimeric protein of its receptor-binding domain (RBD) fused to the amino-terminal region of hepatitis B virus preS1 with a W4P mutation. Front. Immunol. 2021, 12, 637654. [Google Scholar] [CrossRef]
- Hu, Q.; Zhao, Y.; Shaabani, N.; Lyu, X.; Powers, C.; Sun, H.; Cruz, V.; Stegman, K.; Xu, J.; Fossier, A. Chimeric mRNA-based COVID-19 vaccine induces protective immunity against Omicron and Delta variants. Mol. Ther.-Nucleic Acids 2022, 30, 465–476. [Google Scholar] [CrossRef]
- Weekly Epidemiological Update on COVID-19. Available online: https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19 (accessed on 25 May 2023).
- Tripathi, N.K.; Shrivastava, A. Recent Developments in Bioprocessing of Recombinant Proteins: Expression Hosts and Process Development. Front. Bioeng. Biotechnol. 2019, 7, 420. [Google Scholar] [CrossRef]
- Gupta, R.; Arora, K.; Roy, S.S.; Joseph, A.; Rastogi, R.; Arora, N.M.; Kundu, P.K. Platforms, advances, and technical challenges in virus-like particles-based vaccines. Front. Immunol. 2023, 14, 1123805. [Google Scholar] [CrossRef]
- Gronemeyer, P.; Ditz, R.; Strube, J. Trends in upstream and downstream process development for antibody manufacturing. Bioengineering 2014, 1, 188–212. [Google Scholar] [CrossRef]
- Chen, R. Bacterial expression systems for recombinant protein production: E. coli and beyond. Biotechnol. Adv. 2012, 30, 1102–1107. [Google Scholar] [CrossRef]
- Qian, C.; Yang, Y.; Xu, Q.; Wang, Z.; Chen, J.; Chi, X.; Yu, M.; Gao, F.; Xu, Y.; Lu, Y.; et al. Characterization of an Escherichia coli-derived triple-type chimeric vaccine against human papillomavirus types 39, 68 and 70. npj Vaccines 2022, 7, 134. [Google Scholar] [CrossRef]
- Yu, M.; Chi, X.; Huang, S.; Wang, Z.; Chen, J.; Qian, C.; Han, F.; Cao, L.; Li, J.; Sun, H.; et al. A bacterially expressed triple-type chimeric vaccine against human papillomavirus types 51, 69, and 26. Vaccine 2022, 40, 6141–6152. [Google Scholar] [CrossRef]
- Middelberg, A.P.; Rivera-Hernandez, T.; Wibowo, N.; Lua, L.H.; Fan, Y.; Magor, G.; Chang, C.; Chuan, Y.P.; Good, M.F.; Batzloff, M.R. A microbial platform for rapid and low-cost virus-like particle and capsomere vaccines. Vaccine 2011, 29, 7154–7162. [Google Scholar] [CrossRef]
- Piubelli, L.; Campa, M.; Temporini, C.; Binda, E.; Mangione, F.; Amicosante, M.; Terreni, M.; Marinelli, F.; Pollegioni, L. Optimizing Escherichia coli as a protein expression platform to produce Mycobacterium tuberculosis immunogenic proteins. Microb. Cell Fact. 2013, 12, 115. [Google Scholar] [CrossRef]
- Bell, B.A.; Wood, J.F.; Bansal, R.; Ragab, H.; Cargo, J., 3rd; Washington, M.A.; Wood, C.L.; Ware, L.A.; Ockenhouse, C.F.; Yadava, A. Process development for the production of an E. coli produced clinical grade recombinant malaria vaccine for Plasmodium vivax. Vaccine 2009, 27, 1448–1453. [Google Scholar] [CrossRef]
- Kim, H.; Kim, H.J. Yeast as an expression system for producing virus-like particles: What factors do we need to consider? Lett. Appl. Microbiol. 2017, 64, 111–123. [Google Scholar] [CrossRef]
- Tan, Y.; Chen, L.; Li, K.; Lou, B.; Liu, Y.; Liu, Z. Yeast as carrier for drug delivery and vaccine construction. J. Control. Release 2022, 346, 358–379. [Google Scholar] [CrossRef]
- Baghban, R.; Farajnia, S.; Rajabibazl, M.; Ghasemi, Y.; Mafi, A.; Hoseinpoor, R.; Rahbarnia, L.; Aria, M. Yeast expression systems: Overview and recent advances. Mol. Biotechnol. 2019, 61, 365–384. [Google Scholar] [CrossRef]
- Bill, R.M. Recombinant protein subunit vaccine synthesis in microbes: A role for yeast? J. Pharm. Pharmacol. 2015, 67, 319–328. [Google Scholar] [CrossRef]
- Powilleit, F.; Breinig, T.; Schmitt, M.J. Exploiting the yeast LA viral capsid for the in vivo assembly of chimeric VLPs as platform in vaccine development and foreign protein expression. PLoS ONE 2007, 2, e415. [Google Scholar] [CrossRef]
- Zhao, H.; Li, H.-Y.; Han, J.-F.; Deng, Y.-Q.; Zhu, S.-Y.; Li, X.-F.; Yang, H.-Q.; Li, Y.-X.; Zhang, Y.; Qin, E.-D. Novel recombinant chimeric virus-like particle is immunogenic and protective against both enterovirus 71 and coxsackievirus A16 in mice. Sci. Rep. 2015, 5, 7878. [Google Scholar] [CrossRef]
- Balamurugan, V.; Reddy, G.; Suryanarayana, V. Pichia pastoris: A notable heterologous expression system for the production of foreign proteins—Vaccines. Indian J. Biotechnol. 2007, 6, 175–186. [Google Scholar]
- Arora, U.; Tyagi, P.; Swaminathan, S.; Khanna, N. Virus-like particles displaying envelope domain III of dengue virus type 2 induce virus-specific antibody response in mice. Vaccine 2013, 31, 873–878. [Google Scholar] [CrossRef]
- Etemad, B.; Batra, G.; Raut, R.; Dahiya, S.; Khanam, S.; Swaminathan, S.; Khanna, N. An envelope domain III-based chimeric antigen produced in Pichia pastoris elicits neutralizing antibodies against all four dengue virus serotypes. Am. J. Trop. Med. Hyg. 2008, 79, 353–363. [Google Scholar] [CrossRef]
- Shukla, R.; Rajpoot, R.K.; Arora, U.; Poddar, A.; Swaminathan, S.; Khanna, N. Pichia pastoris-Expressed Bivalent Virus-Like Particulate Vaccine Induces Domain III-Focused Bivalent Neutralizing Antibodies without Antibody-Dependent Enhancement in Vivo. Front. Microbiol. 2017, 8, 2644. [Google Scholar] [CrossRef]
- Shanmugam, R.K.; Ramasamy, V.; Shukla, R.; Arora, U.; Swaminathan, S.; Khanna, N. Pichia pastoris-expressed Zika virus envelope domain III on a virus-like particle platform: Design, production and immunological evaluation. Pathog. Dis. 2019, 77, ftz026. [Google Scholar] [CrossRef]
- Lau, Y.L.; Thiruvengadam, G.; Lee, W.W.; Fong, M.Y. Immunogenic characterization of the chimeric surface antigen 1 and 2 (SAG1/2) of Toxoplasma gondii expressed in the yeast Pichia pastoris. Parasitol. Res. 2011, 109, 871–878. [Google Scholar] [CrossRef]
- Eraghi, V.; Derakhshandeh, A.; Hosseini, A.; Motamedi-Boroojeni, A. In silico design and expression of a novel fusion protein of HBHA and high antigenic region of FAP-P of Mycobacterium avium subsp. paratuberculosis in Pichia pastoris. Mol. Biol. Res. Commun. 2017, 6, 161–168. [Google Scholar] [CrossRef]
- Bredell, H.; Smith, J.J.; Gorgens, J.F.; van Zyl, W.H. Expression of unique chimeric human papilloma virus type 16 (HPV-16) L1-L2 proteins in Pichia pastoris and Hansenula polymorpha. Yeast 2018, 35, 519–529. [Google Scholar] [CrossRef]
- Rocha, M.V.; Francoso, K.S.; Lima, L.C.; Camargo, T.M.; Machado, R.L.D.; Costa, F.T.M.; Renia, L.; Nosten, F.; Russell, B.; Rodrigues, M.M.; et al. Generation, characterization and immunogenicity of a novel chimeric recombinant protein based on Plasmodium vivax AMA-1 and MSP1(19). Vaccine 2017, 35, 2463–2472. [Google Scholar] [CrossRef]
- Ojha, R.; Chand, K.; Vellingiri, B.; Prajapati, V.K. Cloning, expression and in vitro validation of chimeric multi epitope vaccine candidate against visceral leishmaniasis infection. Life Sci. 2023, 323, 121689. [Google Scholar] [CrossRef]
- Saraswat, S.; Athmaram, T.N.; Parida, M.; Agarwal, A.; Saha, A.; Dash, P.K. Expression and Characterization of Yeast Derived Chikungunya Virus Like Particles (CHIK-VLPs) and Its Evaluation as a Potential Vaccine Candidate. PLoS Negl. Trop. Dis. 2016, 10, e0004782. [Google Scholar] [CrossRef]
- Yang, L.; Xiao, A.; Wang, H.; Zhang, X.; Zhang, Y.; Li, Y.; Wei, Y.; Liu, W.; Chen, C. A VLP-Based Vaccine Candidate Protects Mice against Japanese Encephalitis Virus Infection. Vaccines 2022, 10, 197. [Google Scholar] [CrossRef]
- Silva, A.J.D.; Jesus, A.L.S.; Leal, L.R.S.; Silva, G.A.S.; Melo, C.M.L.; Freitas, A.C. Pichia pastoris displaying ZIKV protein epitopes from the Envelope and NS1 induce in vitro immune activation. Vaccine 2021, 39, 2545–2554. [Google Scholar] [CrossRef]
- Batra, G.; Raut, R.; Dahiya, S.; Kamran, N.; Swaminathan, S.; Khanna, N. Pichia pastoris-expressed dengue virus type 2 envelope domain III elicits virus-neutralizing antibodies. J. Virol. Methods 2010, 167, 10–16. [Google Scholar] [CrossRef]
- Gupta, J.; Kaul, S.; Srivastava, A.; Kaushik, N.; Ghosh, S.; Sharma, C.; Batra, G.; Banerjee, M.; Shalimar; Nayak, B.; et al. Expression, Purification and Characterization of the Hepatitis E Virus Like-Particles in the Pichia pastoris. Front. Microbiol. 2020, 11, 141. [Google Scholar] [CrossRef]
- Sherry, L.; Grehan, K.; Swanson, J.J.; Bahar, M.W.; Porta, C.; Fry, E.E.; Stuart, D.I.; Rowlands, D.J.; Stonehouse, N.J. Production and Characterisation of Stabilised PV-3 Virus-like Particles Using Pichia pastoris. Viruses 2022, 14, 2159. [Google Scholar] [CrossRef]
- Poddar, A.; Ramasamy, V.; Shukla, R.; Rajpoot, R.K.; Arora, U.; Jain, S.K.; Swaminathan, S.; Khanna, N. Virus-like particles derived from Pichia pastoris-expressed dengue virus type 1 glycoprotein elicit homotypic virus-neutralizing envelope domain III-directed antibodies. BMC Biotechnol. 2016, 16, 50. [Google Scholar] [CrossRef]
- Khetarpal, N.; Shukla, R.; Rajpoot, R.K.; Poddar, A.; Pal, M.; Swaminathan, S.; Arora, U.; Khanna, N. Recombinant Dengue Virus 4 Envelope Glycoprotein Virus-Like Particles Derived from Pichia pastoris are Capable of Eliciting Homotypic Domain III-Directed Neutralizing Antibodies. Am. J. Trop. Med. Hyg. 2017, 96, 126–134. [Google Scholar] [CrossRef]
- Lee, J.; Liu, Z.; Chen, W.-H.; Wei, J.; Kundu, R.; Adhikari, R.; Rivera, J.A.; Gillespie, P.M.; Strych, U.; Zhan, B. Process development and scale-up optimization of the SARS-CoV-2 receptor binding domain–based vaccine candidate, RBD219-N1C1. Appl. Microbiol. Biotechnol. 2021, 105, 4153–4165. [Google Scholar] [CrossRef]
- Errico Provenzano, A.; Posteri, R.; Giansanti, F.; Angelucci, F.; Flavell, S.U.; Flavell, D.J.; Fabbrini, M.S.; Porro, D.; Ippoliti, R.; Ceriotti, A. Optimization of construct design and fermentation strategy for the production of bioactive ATF-SAP, a saporin based anti-tumoral uPAR-targeted chimera. Microb. Cell Fact. 2016, 15, 194. [Google Scholar] [CrossRef]
- Eto, Y.; Saubi, N.; Ferrer, P.; Joseph-Munné, J. Expression of chimeric HPV-HIV protein L1P18 in Pichia pastoris; purification and characterization of the virus-like particles. Pharmaceutics 2021, 13, 1967. [Google Scholar] [CrossRef]
- Pan, W.; Huang, D.; Zhang, Q.; Qu, L.; Zhang, D.; Zhang, X.; Xue, X.; Qian, F. Fusion of two malaria vaccine candidate antigens enhances product yield, immunogenicity, and antibody-mediated inhibition of parasite growth in vitro. J. Immunol. 2004, 172, 6167–6174. [Google Scholar] [CrossRef]
- Zhang, D.; Pan, W. Evaluation of three Pichia pastoris-expressed Plasmodium falciparum merozoite proteins as a combination vaccine against infection with blood-stage parasites. Infect. Immun. 2005, 73, 6530–6536. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kazaks, A.; Lu, I.-N.; Farinelle, S.; Ramirez, A.; Crescente, V.; Blaha, B.; Ogonah, O.; Mukhopadhyay, T.; De Obanos, M.P.; Krimer, A. Production and purification of chimeric HBc virus-like particles carrying influenza virus LAH domain as vaccine candidates. BMC Biotechnol. 2017, 17, 79. [Google Scholar] [CrossRef] [PubMed]
- Limonta-Fernández, M.; Chinea-Santiago, G.; Martín-Dunn, A.M.; Gonzalez-Roche, D.; Bequet-Romero, M.; Marquez-Perera, G.; González-Moya, I.; Canaan-Haden-Ayala, C.; Cabrales-Rico, A.; Espinosa-Rodríguez, L.A. An engineered SARS-CoV-2 receptor-binding domain produced in Pichia pastoris as a candidate vaccine antigen. New Biotechnol. 2022, 72, 11–21. [Google Scholar] [CrossRef] [PubMed]
- Manfrão-Netto, J.H.C.; Gomes, A.M.V.; Parachin, N.S. Advances in using Hansenula polymorpha as chassis for recombinant protein production. Front. Bioeng. Biotechnol. 2019, 7, 94. [Google Scholar] [CrossRef] [PubMed]
- Janowicz, Z.A.; Melber, K.; Merckelbach, A.; Jacobs, E.; Harford, N.; Comberbach, M.; Hollenberg, C.P. Simultaneous expression of the S and L surface antigens of hepatitis B, and formation of mixed particles in the methylotrophic yeast, Hansenula polymorpha. Yeast 1991, 7, 431–443. [Google Scholar] [CrossRef]
- Xu, X.; Ren, S.; Chen, X.; Ge, J.; Xu, Z.; Huang, H.; Sun, H.; Gu, Y.; Zhou, T.; Li, J. Generation of hepatitis B virus PreS2-S antigen in Hansenula polymorpha. Virol. Sin. 2014, 29, 403–409. [Google Scholar] [CrossRef]
- Smith, J.; Burke, A.; Bredell, H.; Van Zyl, W.; Görgens, J. Comparing cytosolic expression to peroxisomal targeting of the chimeric L1/L2 (ChiΔH-L2) gene from human papillomavirus type 16 in the methylotrophic yeasts Pichia pastoris and Hansenula polymorpha. Yeast 2012, 29, 385–393. [Google Scholar] [CrossRef]
- Yu, Y.; Guo, J.; Li, D.; Liu, Y.; Yu, Y.; Wang, L. Development of a human papillomavirus type 6/11 vaccine candidate for the prevention of condyloma acuminatum. Vaccine 2018, 36, 4927–4934. [Google Scholar] [CrossRef]
- Cox, M.M. Recombinant protein vaccines produced in insect cells. Vaccine 2012, 30, 1759–1766. [Google Scholar] [CrossRef]
- Tani, H.; Abe, T.; Matsunaga, T.M.; Moriishi, K.; Matsuura, Y. Baculovirus vector for gene delivery and vaccine development. Future Virol. 2008, 3, 35–43. [Google Scholar] [CrossRef]
- Liu, F.; Wu, X.; Li, L.; Liu, Z.; Wang, Z. Use of baculovirus expression system for generation of virus-like particles: Successes and challenges. Protein Expr. Purif. 2013, 90, 104–116. [Google Scholar] [CrossRef] [PubMed]
- Hong, M.; Li, T.; Xue, W.; Zhang, S.; Cui, L.; Wang, H.; Zhang, Y.; Zhou, L.; Gu, Y.; Xia, N. Genetic engineering of baculovirus-insect cell system to improve protein production. Front. Bioeng. Biotechnol. 2022, 10, 994743. [Google Scholar] [CrossRef] [PubMed]
- Felberbaum, R.S. The baculovirus expression vector system: A commercial manufacturing platform for viral vaccines and gene therapy vectors. Biotechnol. J. 2015, 10, 702–714. [Google Scholar] [CrossRef] [PubMed]
- Cervarix®. Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/cervarix (accessed on 5 July 2023).
- Provenge®. Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/provenge (accessed on 5 July 2023).
- Flublok®. Available online: https://www.fda.gov/vaccines-blood-biologics/vaccines/flublok (accessed on 5 July 2023).
- FlublokQuadrivalent®. Available online: https://www.drugs.com/history/flublok-quadrivalent.html (accessed on 5 July 2023).
- Nuvaxovid. Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/nuvaxovid (accessed on 5 July 2023).
- CovovaxTM. Available online: https://www.fda.gov.ph/sars-cov-2-rs-protein-nanoparticle-vaccine-covovax/ (accessed on 5 July 2023).
- Porcilis Pesti®. Available online: https://www.ema.europa.eu/en/medicines/veterinary/EPAR/porcilis-pesti (accessed on 5 July 2023).
- Porcilis® PCV. Available online: https://www.ema.europa.eu/en/medicines/veterinary/EPAR/porcilis-pcv (accessed on 5 July 2023).
- CircoFLEX®. Available online: https://www.ema.europa.eu/en/medicines/veterinary/EPAR/ingelvac-circoflex (accessed on 5 July 2023).
- Circumvent®. Available online: https://www.merck-animal-health-usa.com/species/swine/circumvent-g2 (accessed on 5 July 2023).
- CircoGard®. Available online: https://www.pharmgate.com/usa/circogard/ (accessed on 5 July 2023).
- ReproCyc®. Available online: https://www.ema.europa.eu/en/medicines/veterinary/EPAR/reprocyc-parvoflex (accessed on 5 July 2023).
- Chen, J.; Xu, W.; Li, L.; Yi, L.; Jiang, Y.; Hao, P.; Xu, Z.; Zou, W.; Li, P.; Gao, Z. Immunogenicity and protective potential of chimeric virus-like particles containing SARS-CoV-2 spike and H5N1 matrix 1 proteins. Front. Cell. Infect. Microbiol. 2022, 12, 967493. [Google Scholar] [CrossRef]
- Pillay, S.; Meyers, A.; Williamson, A.L.; Rybicki, E.P. Optimization of chimeric HIV-1 virus-like particle production in a baculovirus-insect cell expression system. Biotechnol. Prog. 2009, 25, 1153–1160. [Google Scholar] [CrossRef]
- Wu, F.; Zhang, S.; Zhang, Y.; Mo, R.; Yan, F.; Wang, H.; Wong, G.; Chi, H.; Wang, T.; Feng, N. A chimeric Sudan virus-like particle vaccine candidate produced by a recombinant baculovirus system induces specific immune responses in mice and horses. Viruses 2020, 12, 64. [Google Scholar] [CrossRef]
- Wang, Z.; Zhang, T.; Xu, X. Combined truncations at both N-and C-terminus of human papillomavirus type 58 L1 enhanced the yield of virus-like particles produced in a baculovirus system. J. Virol. Methods 2022, 301, 114403. [Google Scholar] [CrossRef]
- Ma, M.; Xia, B.; Wang, Z.; Hao, Y.; Zhang, T.; Xu, X. A novel C-terminal modification method enhanced the yield of human papillomavirus L1 or chimeric L1-L2 virus-like particles in the baculovirus system. Front. Bioeng. Biotechnol. 2022, 10, 1073892. [Google Scholar] [CrossRef]
- Liu, C.-C.; Liu, D.-J.; Yue, X.-Y.; Zhong, X.-Q.; Wu, X.; Chang, H.-Y.; Wang, B.-Z.; Wan, M.-Y.; Deng, L. Chimeric Virus-like Particles Co-Displaying Hemagglutinin Stem and the C-Terminal Fragment of DnaK Confer Heterologous Influenza Protection in Mice. Viruses 2022, 14, 2109. [Google Scholar] [CrossRef]
- Kang, H.; Qi, Y.; Wang, H.; Zheng, X.; Gao, Y.; Li, N.; Yang, S.; Xia, X. Chimeric rabies virus-like particles containing membrane-anchored GM-CSF enhances the immune response against rabies virus. Viruses 2015, 7, 1134–1152. [Google Scholar] [CrossRef]
- O’Flaherty, R.; Bergin, A.; Flampouri, E.; Mota, L.M.; Obaidi, I.; Quigley, A.; Xie, Y.; Butler, M. Mammalian cell culture for production of recombinant proteins: A review of the critical steps in their biomanufacturing. Biotechnol. Adv. 2020, 43, 107552. [Google Scholar] [CrossRef] [PubMed]
- Khan, K.H. Gene expression in mammalian cells and its applications. Adv. Pharm. Bull. 2013, 3, 257. [Google Scholar] [CrossRef]
- Yuk, I.H.; Lin, G.B.; Ju, H.; Sifi, I.; Lam, Y.; Cortez, A.; Liebertz, D.; Berry, J.M.; Schwartz, R.M. A serum-free Vero production platform for a chimeric virus vaccine candidate. Cytotechnology 2006, 51, 183–192. [Google Scholar] [CrossRef] [PubMed]
- Lorenzo, E.; Méndez, L.; Rodríguez, E.; Gonzalez, N.; Cabrera, G.; Pérez, C.; Pimentel, R.; Sordo, Y.; Molto, M.P.; Sardina, T.; et al. Plasticity of the HEK-293 cells, related to the culture media, as platform to produce a subunit vaccine against classical swine fever virus. AMB Express 2019, 9, 139. [Google Scholar] [CrossRef]
- Fontana, D.; Garay, E.; Cervera, L.; Kratje, R.; Prieto, C.; Gòdia, F. Chimeric vlps based on hiv-1 gag and a fusion rabies glycoprotein induce specific antibodies against rabies and foot-and-mouth disease virus. Vaccines 2021, 9, 251. [Google Scholar] [CrossRef] [PubMed]
- Kaewborisuth, C.; Wanitchang, A.; Koonpaew, S.; Srisutthisamphan, K.; Saenboonrueng, J.; Im-Erbsin, R.; Inthawong, M.; Sunyakumthorn, P.; Thaweerattanasinp, T.; Tanwattana, N. Chimeric virus-like particle-based COVID-19 vaccine confers strong protection against SARS-CoV-2 viremia in K18-hACE2 mice. Vaccines 2022, 10, 786. [Google Scholar] [CrossRef]
- Guan, Z.-j.; Guo, B.; Huo, Y.-l.; Guan, Z.-p.; Dai, J.-k.; Wei, Y.-h. Recent advances and safety issues of transgenic plant-derived vaccines. Appl. Microbiol. Biotechnol. 2013, 97, 2817–2840. [Google Scholar] [CrossRef]
- Gaobotse, G.; Venkataraman, S.; Mmereke, K.M.; Moustafa, K.; Hefferon, K.; Makhzoum, A. Recent Progress on Vaccines Produced in Transgenic Plants. Vaccines 2022, 10, 1861. [Google Scholar] [CrossRef]
- Su, H.; Van Eerde, A.; Rimstad, E.; Bock, R.; Branza-Nichita, N.; Yakovlev, I.A.; Clarke, J.L. Plant-made vaccines against viral diseases in humans and farm animals. Front. Plant Sci. 2023, 14, 1170815. [Google Scholar] [CrossRef]
- Dobrica, M.-O.; Lazar, C.; Paruch, L.; Skomedal, H.; Steen, H.; Haugslien, S.; Tucureanu, C.; Caras, I.; Onu, A.; Ciulean, S. A novel chimeric Hepatitis B virus S/preS1 antigen produced in mammalian and plant cells elicits stronger humoral and cellular immune response than the standard vaccine-constituent, S protein. Antivir. Res. 2017, 144, 256–265. [Google Scholar] [CrossRef]
- Yanez, R.J.; Lamprecht, R.; Granadillo, M.; Weber, B.; Torrens, I.; Rybicki, E.P.; Hitzeroth, I.I. Expression optimization of a cell membrane-penetrating human papillomavirus type 16 therapeutic vaccine candidate in Nicotiana benthamiana. PLoS ONE 2017, 12, e0183177. [Google Scholar] [CrossRef] [PubMed]
- Yiemchavee, S.; Wong-Arce, A.; Romero-Maldonado, A.; Shanmugaraj, B.; Monsivais-Urenda, A.E.; Phoolcharoen, W.; Rosales-Mendoza, S. Expression and immunogenicity assessment of a plant-made immunogen targeting the cytotoxic T-lymphocyte associated antigen-4: A possible approach for cancer immunotherapy. J. Biotechnol. 2021, 329, 29–37. [Google Scholar] [CrossRef] [PubMed]
- Mardanova, E.S.; Kotlyarov, R.Y.; Stuchinskaya, M.D.; Nikolaeva, L.I.; Zahmanova, G.; Ravin, N.V. High-Yield Production of Chimeric Hepatitis E Virus-Like Particles Bearing the M2e Influenza Epitope and Receptor Binding Domain of SARS-CoV-2 in Plants Using Viral Vectors. Int. J. Mol. Sci. 2022, 23, 15684. [Google Scholar] [CrossRef]
- Rosales-Mendoza, S.; Solís-Andrade, K.I.; Márquez-Escobar, V.A.; González-Ortega, O.; Bañuelos-Hernandez, B. Current advances in the algae-made biopharmaceuticals field. Expert Opin. Biol. Ther. 2020, 20, 751–766. [Google Scholar] [CrossRef]
- Arias, C.A.D.; Oliveira, C.F.M.d.; Molino, J.V.D.; Ferreira-Camargo, L.S.; Matsudo, M.C.; Carvalho, J.C.M.d. Production of Recombinant Biopharmaceuticals in Chlamydomonas reinhardtii. Int. J. Plant Biol. 2022, 14, 39–52. [Google Scholar] [CrossRef]
- Hernández-Ramírez, J.; Wong-Arce, A.; González-Ortega, O.; Rosales-Mendoza, S. Expression in algae of a chimeric protein carrying several epitopes from tumor associated antigens. Int. J. Biol. Macromol. 2020, 147, 46–52. [Google Scholar] [CrossRef]
- Gregory, J.A.; Topol, A.B.; Doerner, D.Z.; Mayfield, S. Alga-produced cholera toxin-Pfs25 fusion proteins as oral vaccines. Appl. Environ. Microbiol. 2013, 79, 3917–3925. [Google Scholar] [CrossRef]
- Beltrán-López, J.I.; Romero-Maldonado, A.; Monreal-Escalante, E.; Bañuelos-Hernández, B.; Paz-Maldonado, L.M.; Rosales-Mendoza, S. Chlamydomonas reinhardtii chloroplasts express an orally immunogenic protein targeting the p210 epitope implicated in atherosclerosis immunotherapies. Plant Cell Rep. 2016, 35, 1133–1141. [Google Scholar] [CrossRef]
- Márquez-Escobar, V.A.; Bañuelos-Hernández, B.; Rosales-Mendoza, S. Expression of a Zika virus antigen in microalgae: Towards mucosal vaccine development. J. Biotechnol. 2018, 282, 86–91. [Google Scholar] [CrossRef]
- Matanguihan, C.; Wu, P. Upstream continuous processing: Recent advances in production of biopharmaceuticals and challenges in manufacturing. Curr. Opin. Biotechnol. 2022, 78, 102828. [Google Scholar] [CrossRef]
- Göbel, S.; Jaén, K.E.; Dorn, M.; Neumeyer, V.; Jordan, I.; Sandig, V.; Reichl, U.; Altomonte, J.; Genzel, Y. Process intensification strategies toward cell culture-based high-yield production of a fusogenic oncolytic virus. Biotechnol. Bioeng. 2023. [Google Scholar] [CrossRef]
- Alvim, R.G.F.; Itabaiana, I.; Castilho, L.R. Zika virus-like particles (VLPs): Stable cell lines and continuous perfusion processes as a new potential vaccine manufacturing platform. Vaccine 2019, 37, 6970–6977. [Google Scholar] [CrossRef]
- Duetz, W.A. Microtiter plates as mini-bioreactors: Miniaturization of fermentation methods. Trends Microbiol. 2007, 15, 469–475. [Google Scholar] [CrossRef]
- Rosen, O.; Jayson, A.; Goldvaser, M.; Dor, E.; Monash, A.; Levin, L.; Cherry, L.; Lupu, E.; Natan, N.; Girshengorn, M. Optimization of VSV-ΔG-spike production process with the Ambr15 system for a SARS-COV-2 vaccine. Biotechnol. Bioeng. 2022, 119, 1839–1848. [Google Scholar] [CrossRef]
- Junne, S.; Neubauer, P. How scalable and suitable are single-use bioreactors? Curr. Opin. Biotechnol. 2018, 53, 240–247. [Google Scholar] [CrossRef]
- Ton, C.; Stabile, V.; Carey, E.; Maraikar, A.; Whitmer, T.; Marrone, S.; Afanador, N.L.; Zabrodin, I.; Manomohan, G.; Whiteman, M. Development and Scale-up of rVSV-SARS-CoV-2 Vaccine Process Using Single Use Bioreactor. Biotechnol. Rep. 2023, 37, e00782. [Google Scholar] [CrossRef]
- Mercier, S.M.; Diepenbroek, B.; Dalm, M.C.; Wijffels, R.H.; Streefland, M. Multivariate data analysis as a PAT tool for early bioprocess development data. J. Biotechnol. 2013, 167, 262–270. [Google Scholar] [CrossRef]
- Guardalini, L.G.O.; da Silva Cavalcante, P.E.; Leme, J.; de Mello, R.G.; Bernardino, T.C.; Astray, R.M.; Barbosa, E.; da Silveira, S.R.; Ho, P.L.; Tonso, A. Biochemical monitoring throughout all stages of rabies virus-like particles production by Raman spectroscopy using global models. J. Biotechnol. 2022, 363, 19–31. [Google Scholar] [CrossRef]
- Baumann, P.; Hubbuch, J. Downstream process development strategies for effective bioprocesses: Trends, progress, and combinatorial approaches. Eng. Life Sci. 2017, 17, 1142–1158. [Google Scholar] [CrossRef]
- Yamaguchi, H.; Miyazaki, M. Refolding techniques for recovering biologically active recombinant proteins from inclusion bodies. Biomolecules 2014, 4, 235–251. [Google Scholar] [CrossRef]
- Maltoni, G.; Scutteri, L.; Mensitieri, F.; Piaz, F.D.; Hochkoeppler, A. High-yield production in Escherichia coli and convenient purification of a candidate vaccine against SARS-CoV-2. Biotechnol. Lett. 2022, 44, 1313–1322. [Google Scholar] [CrossRef] [PubMed]
- Combe, M.; Lacoux, X.; Martinez, J.; Méjan, O.; Luciani, F.; Daniel, S. Expression, refolding and bio-structural analysis of a tetravalent recombinant dengue envelope domain III protein for serological diagnosis. Protein Expr. Purif. 2017, 133, 57–65. [Google Scholar] [CrossRef]
- Zhang, Y.; Yin, S.; Zhang, B.; Bi, J.; Liu, Y.; Su, Z. HBc-based virus-like particle assembly from inclusion bodies using 2-methyl-2, 4-pentanediol. Process Biochem. 2020, 89, 233–237. [Google Scholar] [CrossRef]
- Zhao, M.; Vandersluis, M.; Stout, J.; Haupts, U.; Sanders, M.; Jacquemart, R. Affinity chromatography for vaccines manufacturing: Finally ready for prime time? Vaccine 2019, 37, 5491–5503. [Google Scholar] [CrossRef] [PubMed]
- Jafari, E.; Mahmoodi, S. Design, expression, and purification of a multi-epitope vaccine against Helicobacter Pylori based on Melittin as an adjuvant. Microb. Pathog. 2021, 157, 104970. [Google Scholar] [CrossRef] [PubMed]
- Rostami, A.; Goshadrou, F.; Langroudi, R.P.; Bathaie, S.Z.; Riazi, A.; Amani, J.; Ahmadian, G. Design and expression of a chimeric vaccine candidate for avian necrotic enteritis. Protein Eng. Des. Sel. 2016, 30, 39–45. [Google Scholar] [CrossRef]
- Jin, J.; Hjerrild, K.A.; Silk, S.E.; Brown, R.E.; Labbé, G.M.; Marshall, J.M.; Wright, K.E.; Bezemer, S.; Clemmensen, S.B.; Biswas, S.; et al. Accelerating the clinical development of protein-based vaccines for malaria by efficient purification using a four amino acid C-terminal ‘C-tag’. Int. J. Parasitol. 2017, 47, 435–446. [Google Scholar] [CrossRef]
- Chevrel, A.; Candela, L.; Innocenti, E.; Golibrzuch, C.; Skudas, R.; Schwämmle, A.; Carrondo, M.J.T.; Kitten, O.; Nissum, M.; Silva, R.J.S. Development of versatile affinity-based system for one step purification process: Case of Group A Streptococcus vaccine. Biotechnol. Bioeng. 2022, 119, 3210–3220. [Google Scholar] [CrossRef]
- Santos, T.; Brito, A.; Boto, R.; Sousa, P.; Almeida, P.; Cruz, C.; Tomaz, C. Influenza DNA vaccine purification using pHEMA cryogel support. Sep. Purif. Technol. 2018, 206, 192–198. [Google Scholar] [CrossRef]
- Solis-Andrade, K.I.; Gonzalez-Ortega, O.; Govea-Alonso, D.O.; Comas-Garcia, M.; Rosales-Mendoza, S. Production and Purification of LTB-RBD: A Potential Antigen for Mucosal Vaccine Development against SARS-CoV-2. Vaccines 2022, 10, 1759. [Google Scholar] [CrossRef]
- Li, Z.; Wei, J.; Yang, Y.; Ma, X.; Hou, B.; An, W.; Hua, Z.; Zhang, J.; Li, Y.; Ma, G.; et al. Strong hydrophobicity enables efficient purification of HBc VLPs displaying various antigen epitopes through hydrophobic interaction chromatography. Biochem. Eng. J. 2018, 140, 157–167. [Google Scholar] [CrossRef]
- Chen, C.-W.; Saubi, N.; Joseph-Munné, J. Chimeric Human Papillomavirus-16 Virus-like Particles Presenting HIV-1 P18I10 Peptide: Expression, Purification, Bio-Physical Properties and Immunogenicity in BALB/c Mice. Int. J. Mol. Sci. 2023, 24, 8060. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.-w.; Kilpeläinen, A.; Joseph-munn, J. Chimeric Human Papillomavirus-16 Virus-like Particles Presenting P18I10 and T20 Peptides from HIV-1 Envelope Induce HPV16 and HIV-1-Specific Humoral and T Cell-Mediated Immunity in BALB/c Mice. Vaccines 2022, 11, 15. [Google Scholar] [CrossRef]
- Singh, S.K.; Plieskatt, J.; Chourasia, B.K.; Singh, V.; Bengtsson, K.L.; Reimer, J.M.; van Daalen, R.C.; Teelen, K.; van de Vegte-Bolmer, M.; van Gemert, G.J.; et al. Preclinical development of a Pfs230-Pfs48/45 chimeric malaria transmission-blocking vaccine. npj Vaccines 2021, 6, 120. [Google Scholar] [CrossRef]
- Anand, G.; Biswas, S.; Yadav, N.; Mukherjee, P.; Chauhan, V.S. Production and immunogenicity of a tag-free recombinant chimera based on PfMSP-1 and PfMSP-3 using alhydrogel and dipeptide-based hydrogels. Vaccines 2021, 9, 782. [Google Scholar] [CrossRef]
- Dishlers, A.; Petrovskis, I.; Skrastina, D.; Zarina, I.; Lieknina, I.; Jansons, J.; Akopjana, I.; Zakova, J.; Ose, V.; Sominskaya, I. PreS1 Containing HBc VLPs for the Development of a Combined Therapeutic/Prophylactic Hepatitis B Vaccine. Microorganisms 2023, 11, 972. [Google Scholar] [CrossRef]
- González-Domínguez, I.; Lorenzo, E.; Bernier, A.; Cervera, L.; Gòdia, F.; Kamen, A. A Four-Step Purification Process for Gag VLPs: From Culture Supernatant to High-Purity Lyophilized Particles. Vaccines 2021, 9, 1154. [Google Scholar] [CrossRef]
- Boix-besora, A.; Lorenzo, E. Optimization, Production, Purification and Characterization of HIV-1 GAG-Based Virus-like Particles Functionalized with SARS-CoV-2. Vaccines 2022, 10, 250. [Google Scholar] [CrossRef]
- Saylor, K.; Waldman, A.; Gillam, F.; Zhang, C. Multi-epitope insert modulates solubility-based and chromatographic purification of human papilloma virus 16 L1-based vaccine without inhibiting virus-like particle assembly. J. Chromatogr. A 2020, 1631, 461567. [Google Scholar] [CrossRef] [PubMed]
- Gustavo, D.; Jan, S.; Adrien, S.; Werle, L.B. Scalable chromatography-based purification of virus-like particle carrier for epitope based Influenza A vaccine produced in Escherichia coli. J. Virol. Methods 2016, 232, 8–11. [Google Scholar] [CrossRef]
- Lerer, E.; Oren, Z.; Kafri, Y.; Adar, Y.; Toister, E.; Cherry, L.; Lupu, E.; Monash, A.; Levy, R.; Dor, E. Highly efficient purification of recombinant VSV-∆ G-spike vaccine against SARS-CoV-2 by flow-through chromatography. BioTech 2021, 10, 22. [Google Scholar] [CrossRef] [PubMed]
- Reiter, K.; Steppert, P.; Jungbauer, A.; Grammelhofer, D.; Joseph, J. SEPARATION by polymer-grafted anion exchanger. J. Sep. Sci. 2020, 43, 2270–2278. [Google Scholar] [CrossRef]
- Leong, H.Y.; Fu, X.Q.; Show, P.L.; Yao, S.J.; Lin, D.Q. Downstream processing of virus-like particles with aqueous two-phase systems: Applications and challenges. J. Sep. Sci. 2022, 45, 2064–2076. [Google Scholar] [CrossRef]
- Jacinto, M.; Soares, R.; Azevedo, A.; Chu, V.; Tover, A.; Conde, J.; Aires-Barros, M. Optimization and miniaturization of aqueous two phase systems for the purification of recombinant human immunodeficiency virus-like particles from a CHO cell supernatant. Sep. Purif. Technol. 2015, 154, 27–35. [Google Scholar] [CrossRef]
- Joshi, P.U.; Turpeinen, D.G.; Schroeder, M.; Jones, B.; Lyons, A.; Kriz, S.; Khaksari, M.; O’Hagan, D.; Nikam, S.; Heldt, C.L. Osmolyte enhanced aqueous two-phase system for virus purification. Biotechnol. Bioeng. 2021, 118, 3251–3262. [Google Scholar] [CrossRef]
- Marchel, M.; Niewisiewicz, J.; Coroadinha, A.S.; Marrucho, I.M. Purification of virus-like particles using aqueous biphasic systems composed of natural deep eutectic solvents. Sep. Purif. Technol. 2020, 252, 117480. [Google Scholar] [CrossRef]
- Menzel, S.; Holland, T.; Boes, A.; Spiegel, H.; Fischer, R.; Felix, J. Protein Expression and Purification Downstream processing of a plant-derived malaria transmission-blocking vaccine candidate. Protein Expr. Purif. 2018, 152, 122–130. [Google Scholar] [CrossRef]
- Gillespie, P.F.; Wang, Y.; Hofmann, C.; Kuczynski, L.E.; Winters, M.A.; Teyral, J.L.; Tubbs, C.M.; Shiflett, K.; Patel, N.; Rustandi, R.R. Understanding the Spike Protein in COVID-19 Vaccine in Recombinant Vesicular Stomatitis Virus (rVSV) Using Automated Capillary Western Blots. ACS Omega 2023, 8, 3319–3328. [Google Scholar] [CrossRef]
- Charretier, C.; Saulnier, A.; Benair, L.; Armanet, C.; Bassard, I.; Daulon, S.; Bernigaud, B.; Rodrigues de Sousa, E.; Gonthier, C.; Zorn, E.; et al. Robust real-time cell analysis method for determining viral infectious titers during development of a viral vaccine production process. J. Virol. Methods 2018, 252, 57–64. [Google Scholar] [CrossRef] [PubMed]
- Mittal, M.; Banerjee, M.; Lua, L.H.; Rathore, A.S. Current status and future challenges in transitioning to continuous bioprocessing of virus-like particles. J. Chem. Technol. Biotechnol. 2022, 97, 2376–2385. [Google Scholar] [CrossRef]
- Gerstweiler, L.; Billakanti, J.; Bi, J.; Middelberg, A.P. An integrated and continuous downstream process for microbial virus-like particle vaccine biomanufacture. Biotechnol. Bioeng. 2022, 119, 2122–2133. [Google Scholar] [CrossRef] [PubMed]
- Hillebrandt, N.; Vormittag, P.; Bluthardt, N.; Dietrich, A.; Hubbuch, J. Integrated process for capture and purification of virus-like particles: Enhancing process performance by cross-flow filtration. Front. Bioeng. Biotechnol. 2020, 8, 489. [Google Scholar] [CrossRef] [PubMed]

| Commercial Vaccines | Target | Protective Antigen/Formulation | Expression Host | Manufacturer | Reference |
|---|---|---|---|---|---|
| Recombivax HB® | Hepatitis B virus | Hepatitis B surface antigen (HBsAg)/Subunit | S. cerevisiae | Merck & Co., Inc.,NJ, USA | [13] |
| Engerix®-B | Hepatitis B virus | Hepatitis B surface antigen (HBsAg)/Subunit | S. cerevisiae | GlaxoSmithKline, Brentford, UK | [14] |
| GeneVac-B | Hepatitis B virus | Hepatitis B surface antigen (HBsAg)/Subunit | H. polymorpha | Serum Institute of India Pvt. Ltd., Pune, India | [15] |
| Hepacare® | Hepatitis B virus | Triple antigen (S, pre-S1, and pre-S2)/Subunit | Mammalian cell line | Medeva Pharma Plc, Speke, UK. | [16] |
| Twinrix | Hepatitis A and Hepatitis B virus | Inactivated hepatitis A virus (strain HM175) and non-infectious HBsAg/Bivalent subunit | S. cerevisiae | GlaxoSmithKline, Brentford, UK | [17] |
| HBVaxPRO® | Hepatitis B virus | Hepatitis B surface antigen (HBsAg)/Subunit | S. cerevisiae | Sanofi Pasteur MSD, Lyon, France | [18] |
| LYMErix® | Borrelia burgdorferi | Lipoprotein OspA/Subunit | E. coli | GlaxoSmithKline, Brentford, UK | [19] |
| Trumenba® | Neisseria meningitidis serogroup B | Recombinant factor H binding protein (fHbp), from subfamily A (A05) and subfamily B (B01)/Subunit | E. coli | Pfizer Inc., New York, USA | [20] |
| Bexsero® | Neisseria meningitidis serogroup B | Outer membrane vesicle protein, fHbp fusion protein, NadA protein, and NHBA fusion protein/Multicomponent recombinant | E. coli | GlaxoSmithKline, Brentford, UK | [21] |
| Gardasil® | Human papillomavirus (HPV) | HPV (Types 6, 11, 16, and 18) L1 protein/VLPs | S. cerevisiae | Merck & Co., Inc.,NJ, USA | [22] |
| Gardasil® 9 | Human papillomavirus (HPV) | Nine-valent HPV (Types 6,11,16,18,31,33,45,52,58) L1 protein/VLPs | S. cerevisiae | Merck & Co., Inc.,NJ, USA | [23] |
| Cecolin® | Human papillomavirus (HPV) | HPV (Types 16,18) L1 protein/VLPs | E. coli | Xiamen Innovax Biotech Co., Ltd., Xiamen, China | [24] |
| MosquirixTM (RTS,S/AS01) | Plasmodium falciparum (Malaria) | Chimeric protein: RTS in fusion with HBsAg/VLPs | S. cerevisiae | GlaxoSmithKline, Brentford, UK | [25] |
| Shingrix | Varicella zoster virus (Shingles) | Glycoprotein E antigen (gE)/Subunit | CHO cell line | GlaxoSmithKline, Brentford, UK | [26] |
| Pathogens | Target Antigen/Vector/Host Strain | Strategy and Outcome | References |
|---|---|---|---|
| Chimeric vaccines: | |||
| Dengue virus (DENV) | HBcAg-EDIII-2/pPICZ A/P. pastoris KM71H strain. | Chimeric vaccine developed displaying the envelope domain III of dengue virus type-2 (DENV-2) on hepatitis B core antigen (HBcAg)-based VLPs. Insertion of EDIII-2 in the c/e1 loop of HBcAg yielded structurally and functionally stable chimeric VLPs. A modest titer of DENV-2-specific virus-neutralizing antibodies was found in the mice immunized with chimeric VLPs. | [76] |
| Dengue virus (DENV) | rEDIII-T/pPIC9K vector/P. pastoris GS115 (his4) strain. | Tetravalent chimeric vaccine developed via fusion of receptor-binding envelope domain III of four serotypes DENV-1, DENV-2, DENV-3, and DENV-4 via pentaglycyl peptide linkers. Neutralizing activity against infectivity of all four serotypes of the dengue virus was obtained in the BALB/c mice model. The in vitro studies revealed Th2 (T helper 2) immune response activation. | [77] |
| Dengue virus (DENV) | Bivalent antigen/pAO815 vector/P. pastoris GS115 (his4) strain. | Co-expression and co-assembly of envelope (E) proteins from DENV-1 and DENV-2 into bivalent mosaic chimeric VLPs known as mE1E2bv VLPs. Serotype-specific virus-neutralizing antibodies obtained in BALB/c mice model and lack of antibody-mediated antibody-dependent enhancement (ADE) activity in vivo model. | [78] |
| Zika virus (ZIKV) | ZIKV EDIII/pAO815 vector/P. pastoris GS115 (his4) strain. | Chimeric VLPs developed by co-expression and co-purification of ZS (envelope domain III of Zika virus fused with hepatitis B surface antigen) and S (hepatitis B surface antigen) in a 1:4 ratio. Chimeric VLPs were found to be immunogenic in BALB/c mice model, capable of neutralizing ZIKV particles. | [79] |
| Toxoplasma gondii | SAG1/2/pPICZα A vector/P. pichia X-33 strain. | Recombinant chimeric surface antigens 1 and 2 (SAG1/2) of T. gondii in fusion with C-terminal-his tag was expressed and purified via Ni-NTA affinity chromatography. Vaccination via immunogenic chimeric protein exhibited SAG1- and SAG2-specific immune response in BALB/c mice model and the secretion of IFN-γ, the Th1 (T helper 1)-specific cytokines. | [80] |
| Mycobacterium avium subsp. paratuberculosis (MAP) | HBHA-FAP-P/pPICK9K vector/P. pastoris strain GS115 strain. | Expression of the chimeric fusion protein consisting of heparin-binding hemagglutinin (HBHA) adhesin protein and the antigenic region of the fibronectin attachment protein-P (FAP-P) of Mycobacterium avium subsp. paratuberculosis. Post-translationally methylated HBHA protein in fusion with FAP-P developed similarly to the native HBHA in 3D structure. | [81] |
| Human papillomavirus (HPV) | Chimeric HPV-16 LI-L2 protein/pBLHIS–IX/P. pastoris KM71 strain. | Chimeric protein known as ChiΔF-L2, developed via replacing the h4 helix of HPV-16 L1 major capsid protein by the 108–120 amino acids corresponding to L2 minor capsid protein. Successfully produced ~23.61 mg/L chimeric HPV L1/L2 protein during fed-batch fermentation. | [82] |
| Plasmodium vivax | PvAMA166-MSP119/pPIC9K vector/Pichia pastoris GS115 strain. | Chimeric antigen developed, consisting of the immunogenic apical membrane antigen 1 (AMA-1) ectodomain and the C-terminal region of the merozoite surface protein 1 (MSP-1) of P. vivax. High anti-AMA-1, anti-MSP-1 antibody titers and the induction of IFN-gamma secreting immune cells in immunized mice model. | [83] |
| Leishmania donovani (Visceral leishmaniasis) | Synthetic gene (LeiSp)/pPICZA vector/P. pastoris X-33 strain. | Reverse vaccinology was implemented to develop a chimeric LeiSp multi-epitope vaccine candidate consisting immunogenic membrane and secretory proteins of L. donovali infantum and salivary proteins of P. argentipes sand fly vector. Significant upregulation of proinflammatory cytokines and decreased anti-inflammatory cytokines in THP1 cell line. | [84] |
| Recombinant vaccines: | |||
| Chikungunya virus (CHIKV) | Structural capsid and envelope (E3, E2, 6K, E1) protein/pPIC9K vector/Pichia pastoris GS115 strain. | Structural and capsid protein of CHIKV expressed and purified via ultrafiltration using discontinuous sucrose gradient. CHIKV-VLPs induced both cellular and humoral immune responses in mice models. Positive in vitro and in vivo neutralization activity of anti-CHIKV-VLPs antibodies. | [85] |
| Japanese encephalitis virus (JEV) | Modified JEV prM/Env gene/pPICZA vector/Pichia pastoris X-33 strain. | Expression and purification of JEV prM/ENV proteins via Ni-NTA chromatography followed by an in vitro assembly of JEV-VLPs. Robust cellular and humoral immune response in mice models. After immunization, a high titer of neutralizing antibodies against JEV was obtained in the pig model. | [86] |
| Zika virus (ZIKV) | ZIKV Env and NS1 proteins/pPGKΔ3α vector /P. pastoris GS115 strain. | Immunogenic epitopes ZIKV envelope (E) and NS1 proteins displayed on the surface of P. pastoris via GPI anchored AG-α1 protein. The in vitro immunogenic activity of recombinant yeast indicated by the activation of the lymphocytes and monocytes of mouse spleen. | [87] |
| Dengue virus (DENV) | ENVIII-2 gene/pPICZA vector/P. pastoris KM71H strain. | Intracellular expression of dengue Virus type-2 envelope domain III. Elevation of virus-neutralizing antibodies in BALB/c mice model estimated by plaque-reduction neutralization test. | [88] |
| Hepatitis E virus | ORF-2/pPICZα vector/P. pastoris KM71H strain. | Gene-encoding 112–608 aa of capsid forming ORF-2 of the hepatitis E virus expressed and purified as potential virus-like particles. Generation of ORF-2-specific IgG antibody and splenocyte proliferation in BALB/c mice model. | [89] |
| Polio virus | PV-3 SC8/pPink HC vector/PichiaPinkTM strain. | Thermally stable PV-3 SC8 VPLs developed under dual AOX1 regulation, consisting structural precursor protein (P1) and viral protease (3CD). Wild-type PV-3 VLPs elicited high C and D antigenicity whereas, thermally stable PV-3 SC8 VLPs exhibited more D antigens. | [90] |
| Dengue virus (DENV) | DENV-1 EDIII/pPICZA vector/P. pastoris KM71H strain. | Codon-optimized gene E glycoprotein (ectodomain III) of DENV-1 expressed and purified as self-assembled VLPs. DENV-1 E VLPs elicited virus-serotype-specific neutralizing antibodies in mice model. | [91] |
| Dengue virus (DENV) | DENV-4 EDIII/pPICZ-A vector/P. pastoris KM71H strain. | Codon optimized gene DENV-4 EDIII expressed and purified as VLPs via Ni-NTA affinity chromatography under denaturing conditions. DENV-4 E VLPs generated immunogenic response and EDIII-derived virus serotype-specific neutralizing antibodies in mice models. | [92] |
| Disease/Pathogen | Commercial Vaccine | Protective Agent/Vaccine Type | Insect Cells Lines | Manufacturer | References |
|---|---|---|---|---|---|
| Vaccines for human-use | |||||
| Cervical Cancer (HPV) | Cervarix® | L1 protein/VLP | High Five Cells | GlaxoSmithKline, Brentford, UK | [110] |
| Prostate Cancer | Provenge® | PAP-GM-CSF Fusion protein/Cellular vaccine | Sf-21 cells | Dendreon Corporation, California, USA | [111] |
| Influenza Virus | Flublok® | HA glycoprotein/Subunit | expresSF+ cells | Sanofi Pasteur, Paris, France | [112] |
| Influenza Virus | FlublokQuadrivalent® | HA quadrivalent/Subunit | expresSF+ cells | Sanofi Pasteur, Paris, France | [113] |
| COVID-19 | Nuvaxovid/ CovovaxTM | Spike S protein/Spike protein nanoparticle | Sf9 cells | Novavax, Malvern, PA, USA/ Serum Institute of India, Pune, India | [114,115] |
| Vaccines for veterinary use | |||||
| Classical Swine Flu Fever Virus | Porcilis Pesti® | E2 protein/Subunit | Sf-21 cells | Merck & Co., Inc., NJ, USA | [116] |
| Classical Swine Flu Fever Virus | Bayovac® CSF E2 | E2 protein/Subunit | Sf-21 cells | BAYER AG/Pfizer Animal Health (Nordrhein-Westfalen, Germany/Groton, CT, USA (Discontinued) | [109] |
| Porcine Circovirus Type 2 (PCV-2) | Porcilis® PCV | PCV2a ORF2 protein/VLP | Tn5 cells | Merck & Co., Inc., NJ, USA | [117] |
| Porcine Circovirus Type 2 (PCV-2) | IngelVac CircoFLEX® | PCV2a ORF2 protein/VLP | Tn5 cells | B. Ingelheim, Berlin, Germany | [118] |
| Porcine Circovirus Type 2 (PCV-2) | Circumvent® PCV2 | PCV2a ORF2 protein/VLP | Tn5 cells | Merck & Co., Inc., NJ, USA | [119] |
| Porcine Circovirus Type 2 (PCV-2) | CircoGard® | PCV2b ORF2 protein/VLP | (Not specified) | Pharmgate Animal Health, Wilmington, North Carolina, USA | [120] |
| Porcine Parvovirus (PPV) | ReproCyc® ParvoFLEX | PPV 27a VP2/VLP | (Not specified) | B. Ingelheim, Berlin, Germany | [121] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chauhan, S.; Khasa, Y.P. Challenges and Opportunities in the Process Development of Chimeric Vaccines. Vaccines 2023, 11, 1828. https://doi.org/10.3390/vaccines11121828
Chauhan S, Khasa YP. Challenges and Opportunities in the Process Development of Chimeric Vaccines. Vaccines. 2023; 11(12):1828. https://doi.org/10.3390/vaccines11121828
Chicago/Turabian StyleChauhan, Shivani, and Yogender Pal Khasa. 2023. "Challenges and Opportunities in the Process Development of Chimeric Vaccines" Vaccines 11, no. 12: 1828. https://doi.org/10.3390/vaccines11121828
APA StyleChauhan, S., & Khasa, Y. P. (2023). Challenges and Opportunities in the Process Development of Chimeric Vaccines. Vaccines, 11(12), 1828. https://doi.org/10.3390/vaccines11121828







