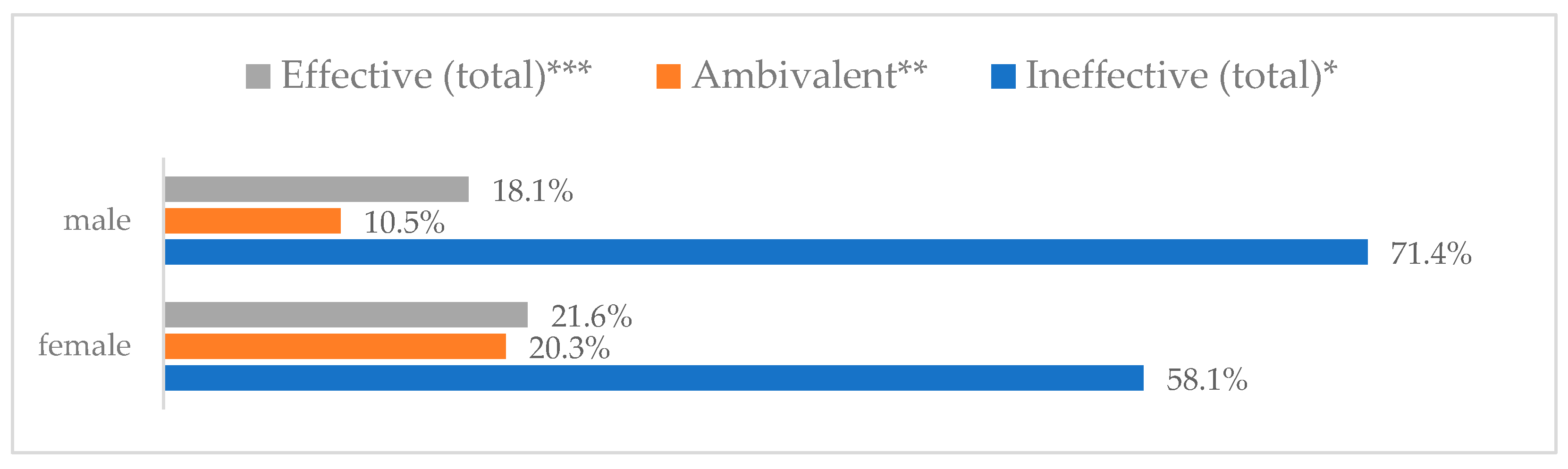
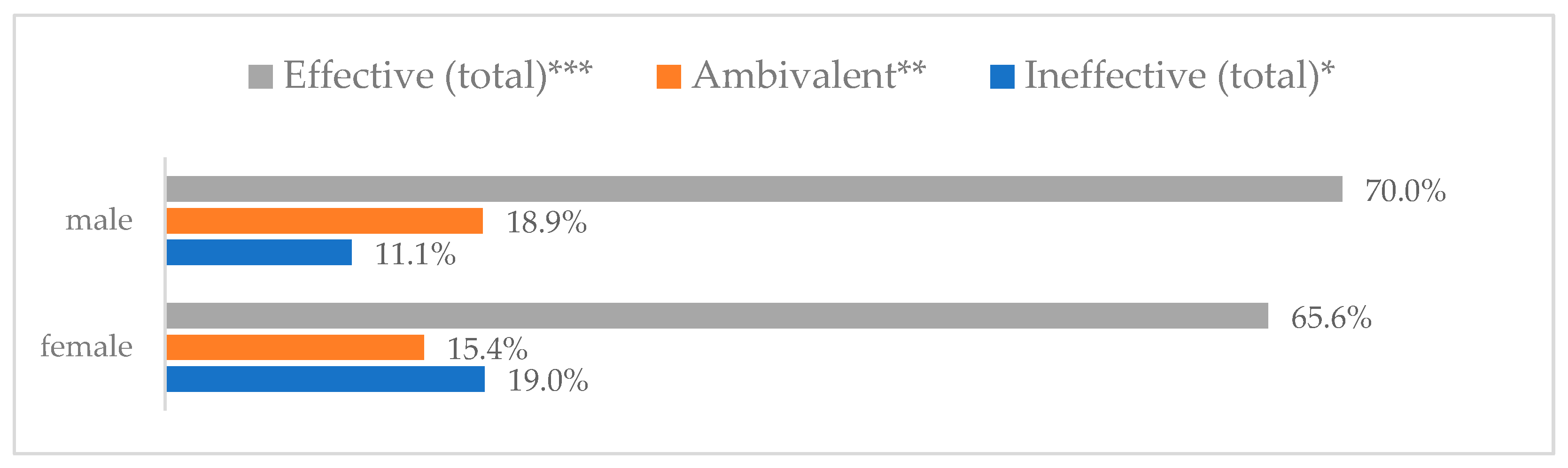
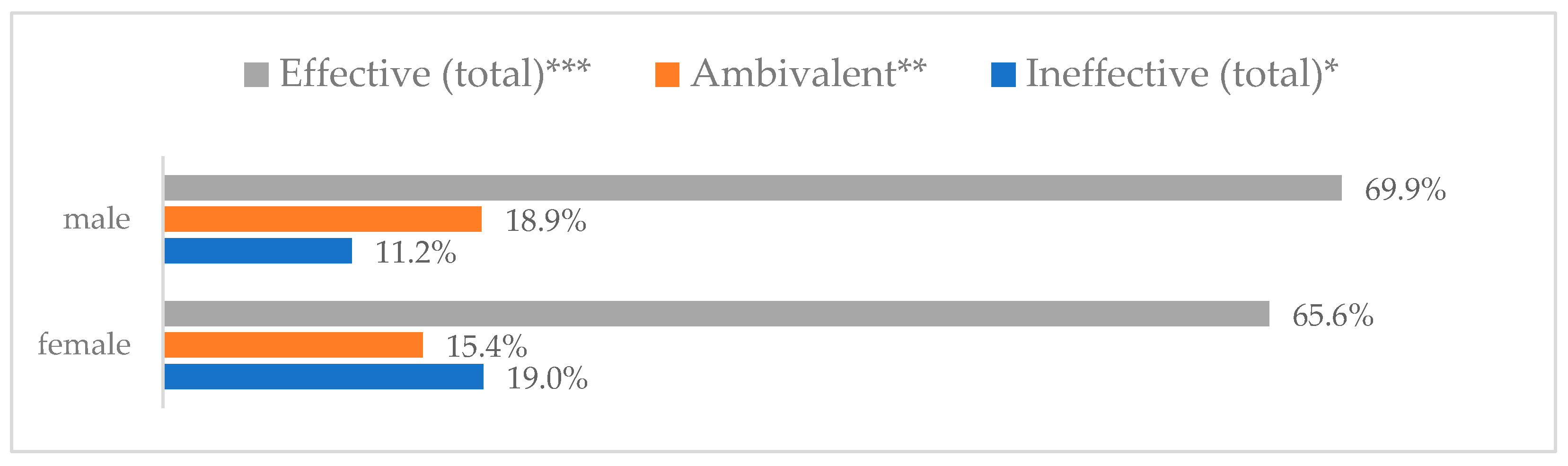
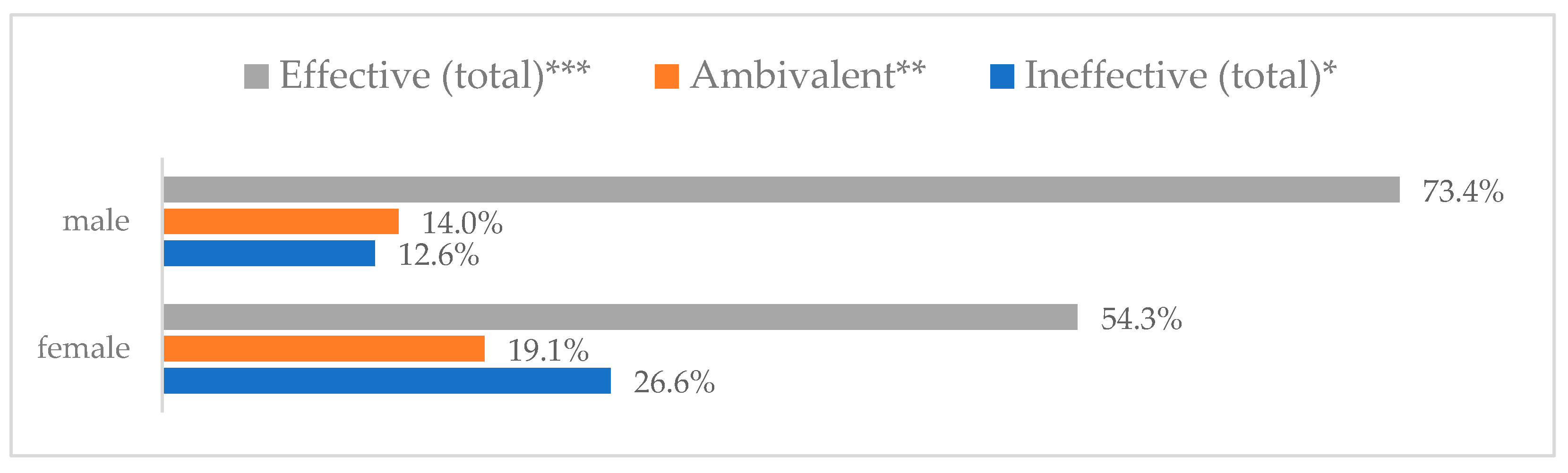
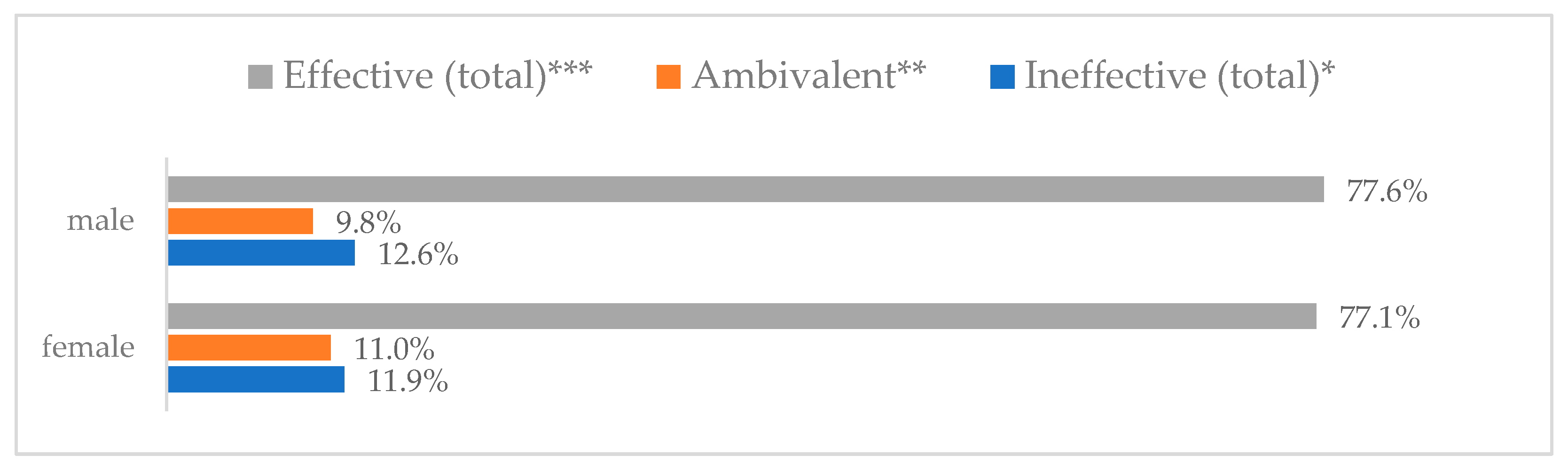
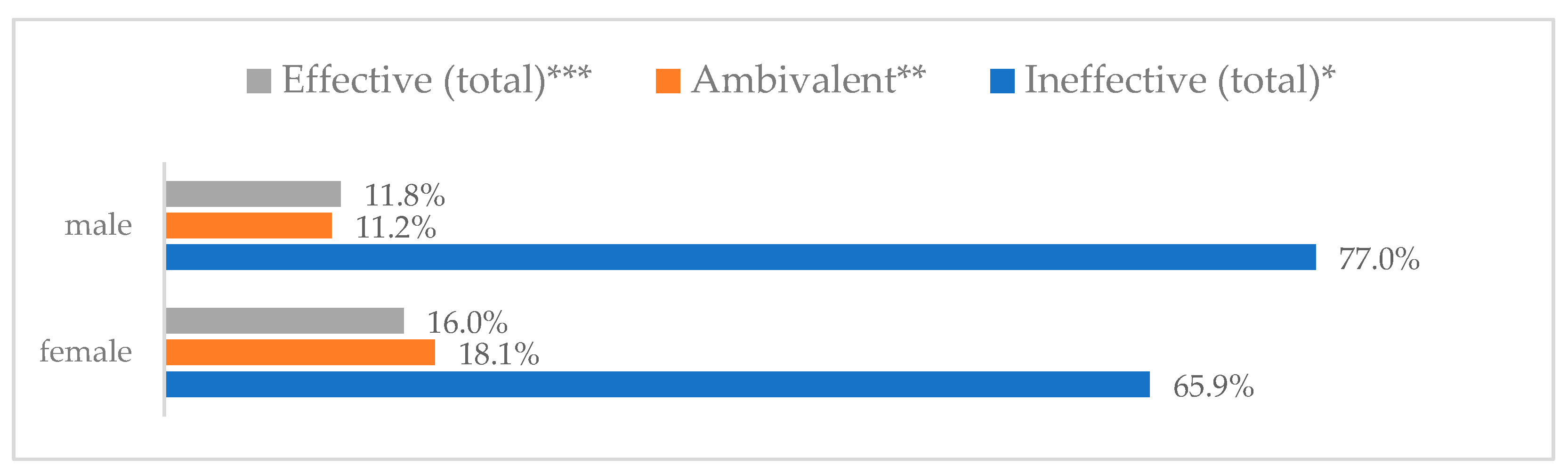
Figure 1.
Wearing a protective mask that covers the mouth and nose to prevent influenza virus infection by gender (N = 905). * Sum of responses: completely ineffective, ineffective, rather ineffective; ** Response: neither ineffective nor effective; *** Sum of responses: rather effective, effective, completely effective.
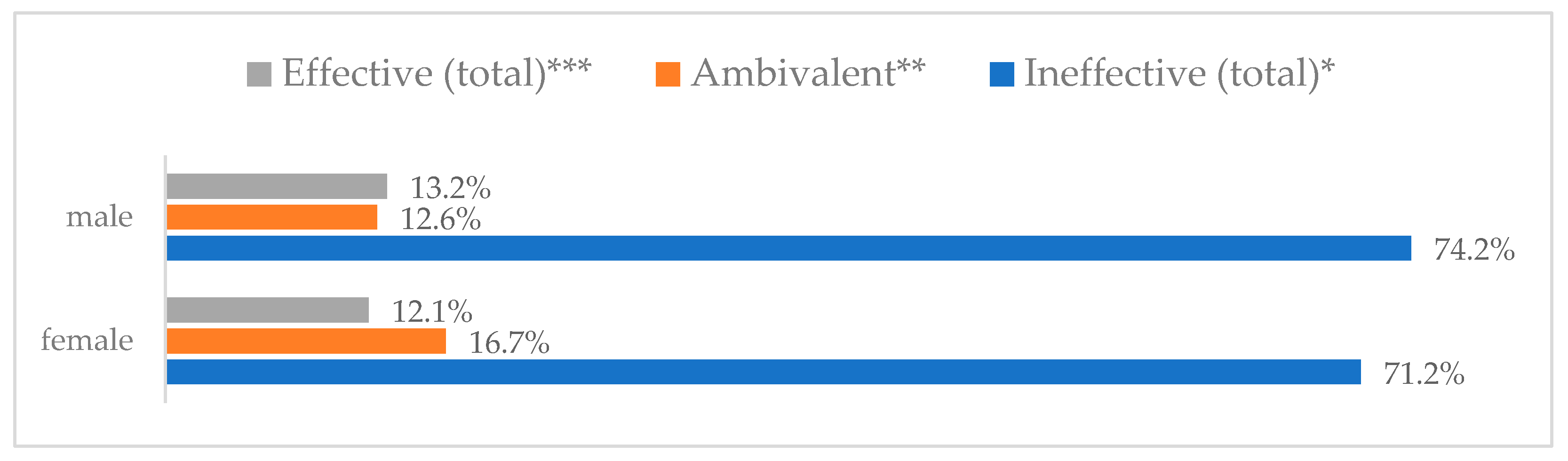
Figure 1.
Wearing a protective mask that covers the mouth and nose to prevent influenza virus infection by gender (N = 905). * Sum of responses: completely ineffective, ineffective, rather ineffective; ** Response: neither ineffective nor effective; *** Sum of responses: rather effective, effective, completely effective.
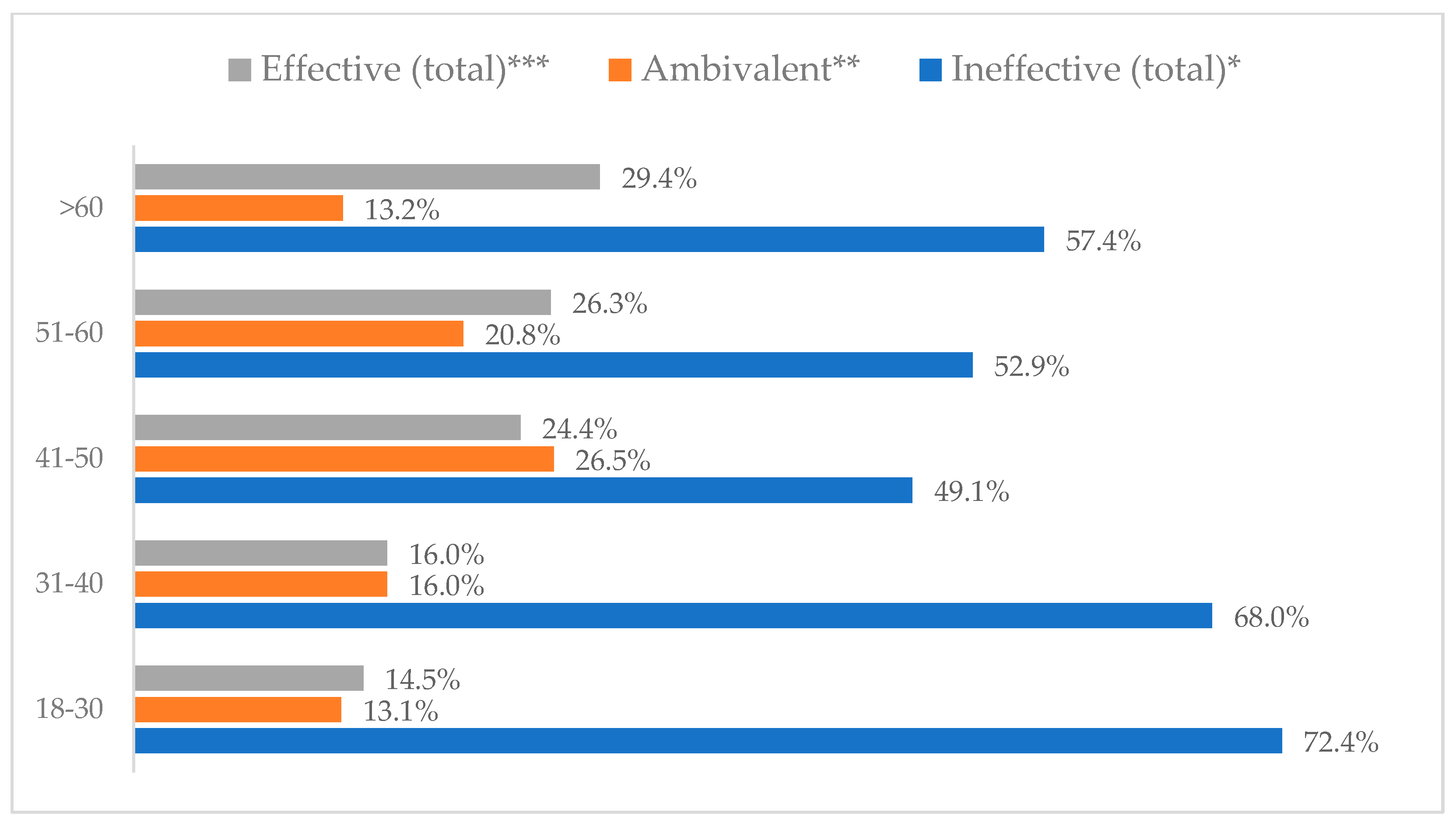
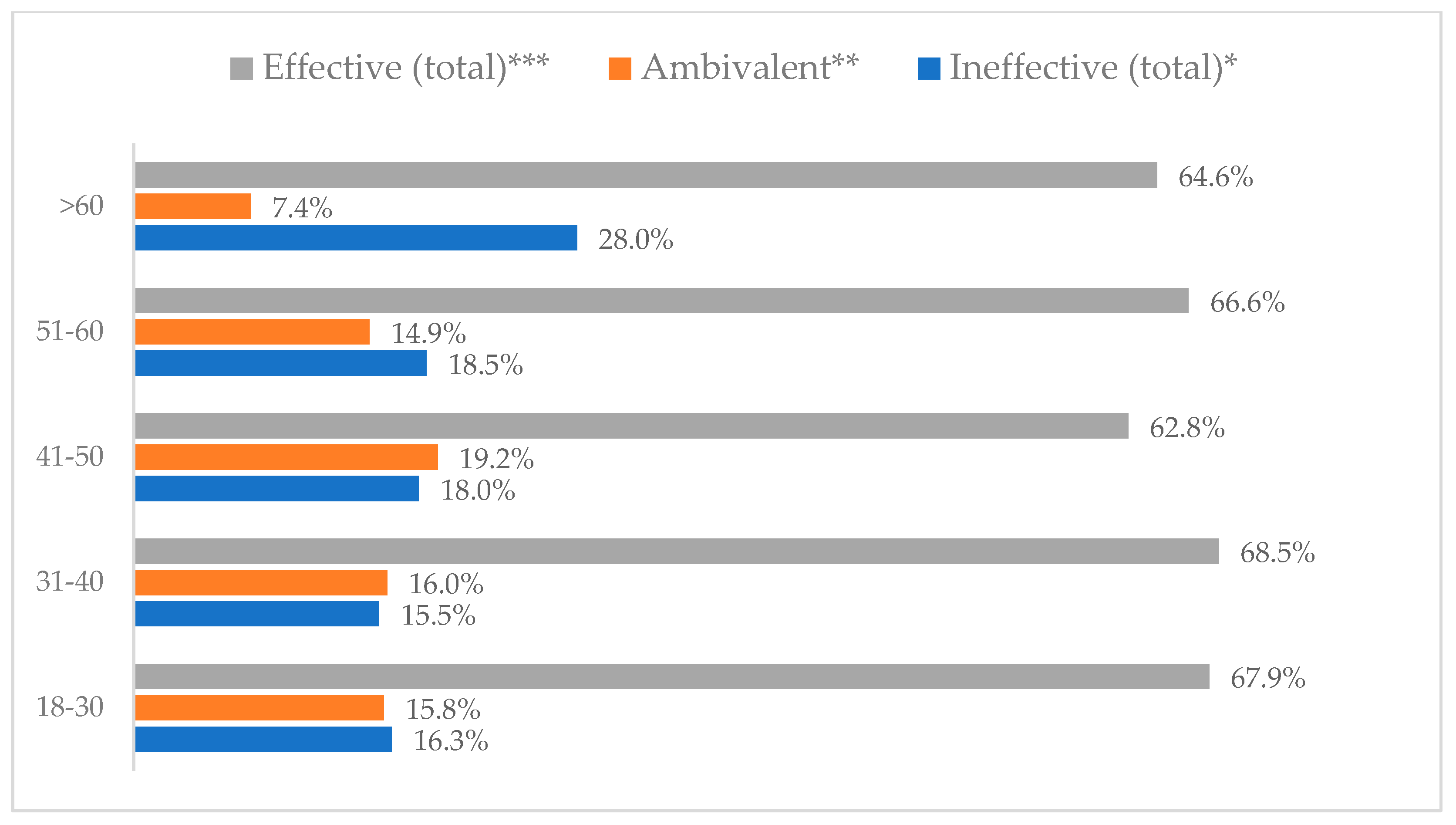
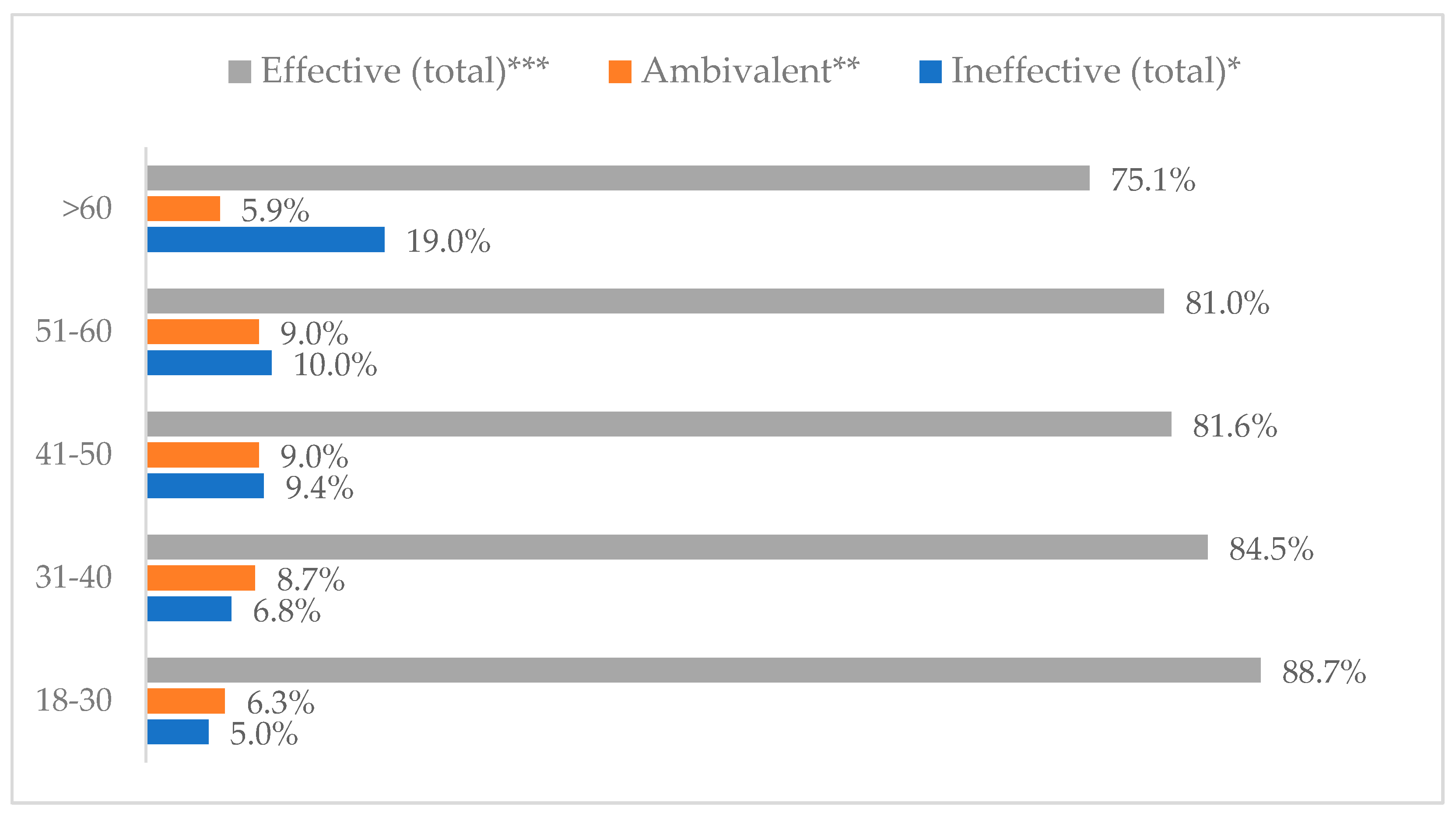
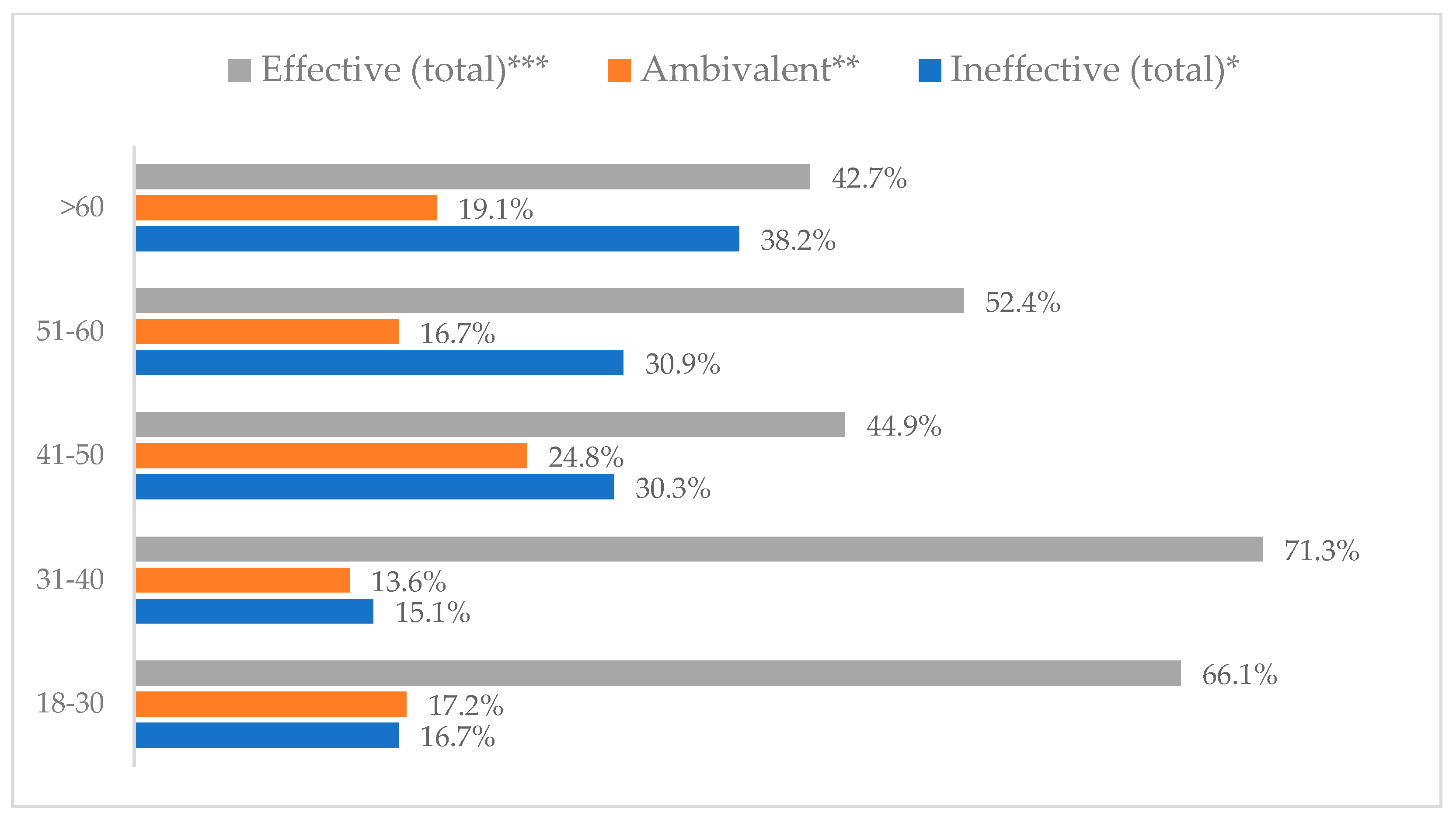
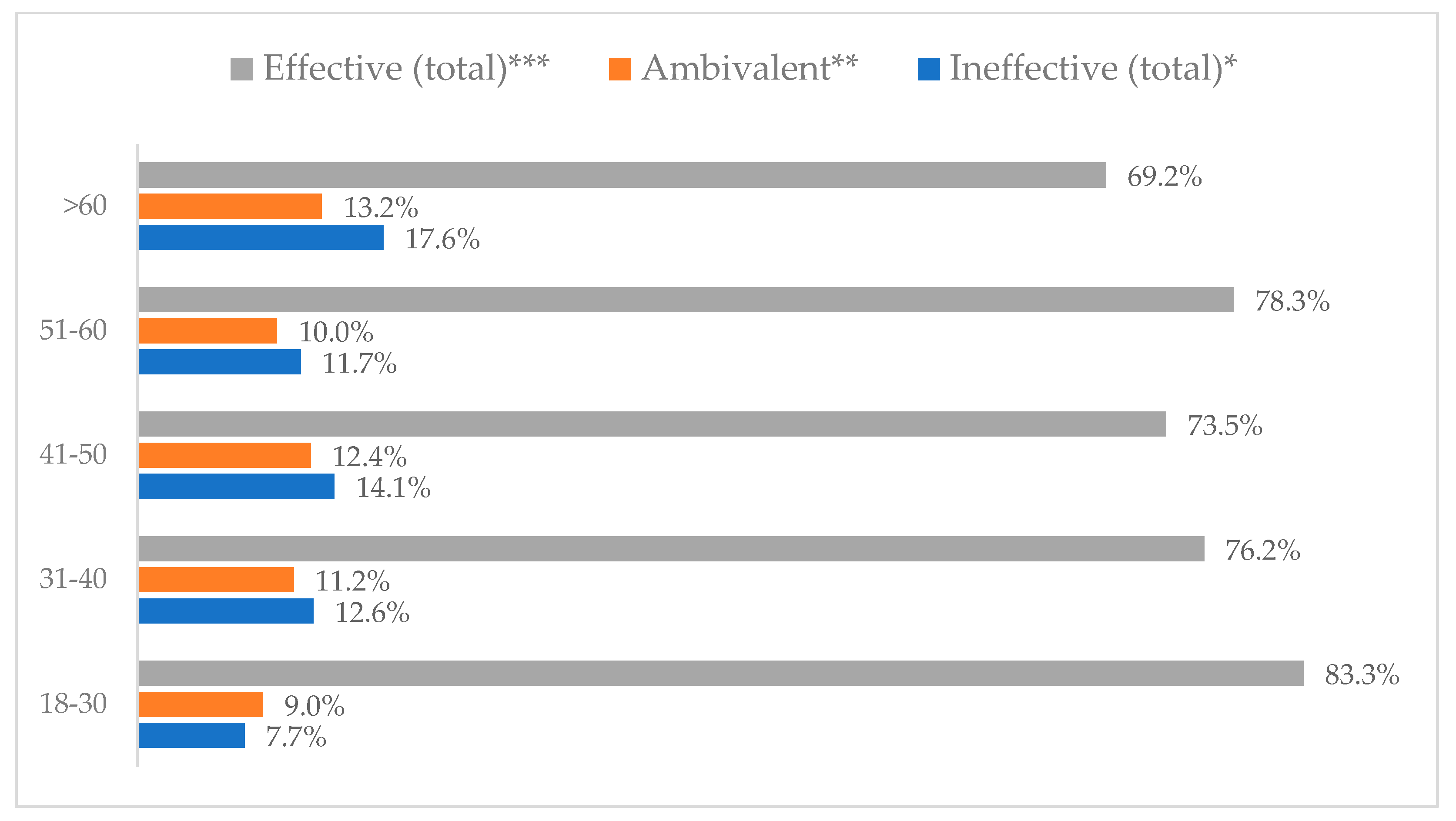
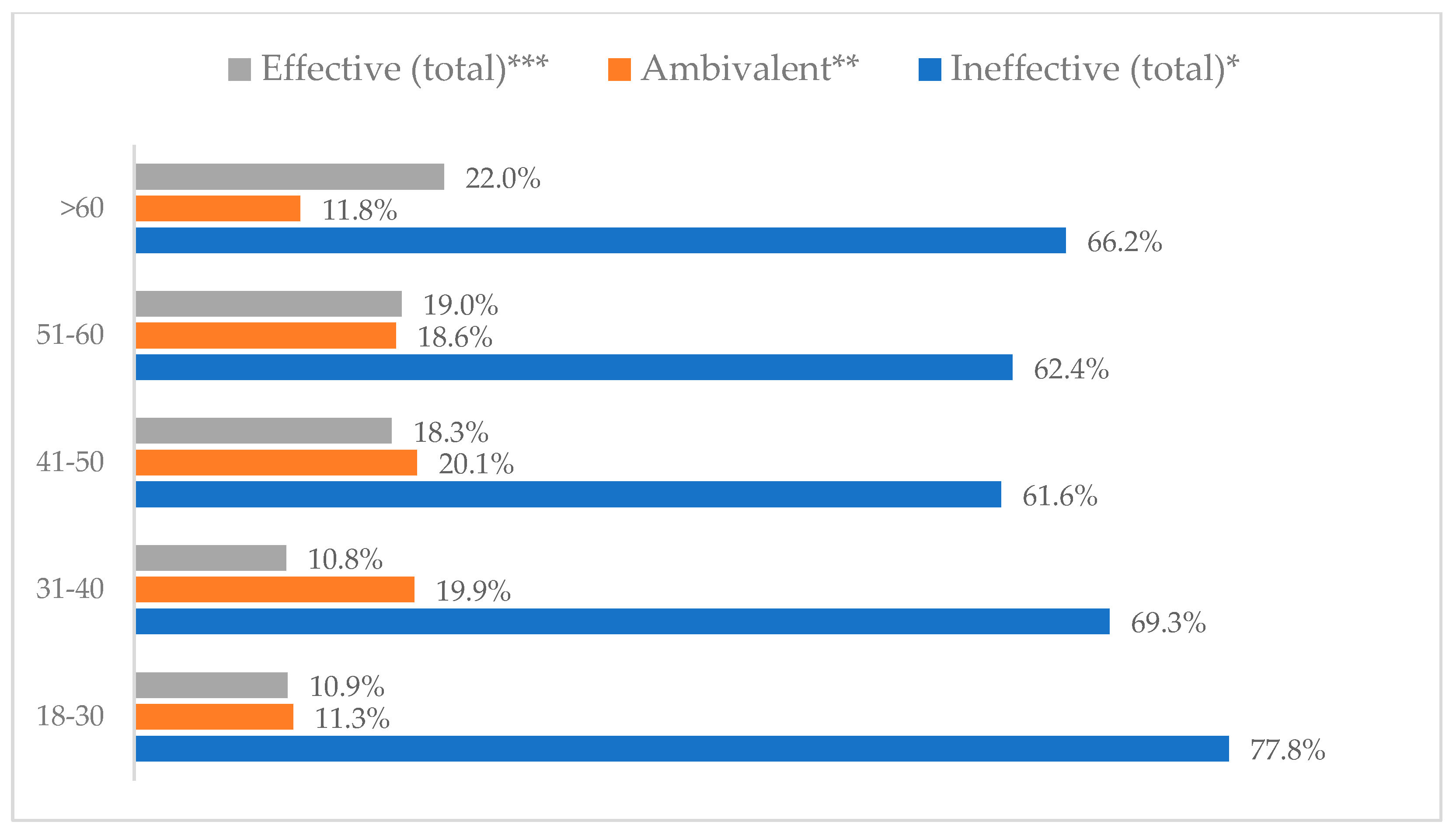
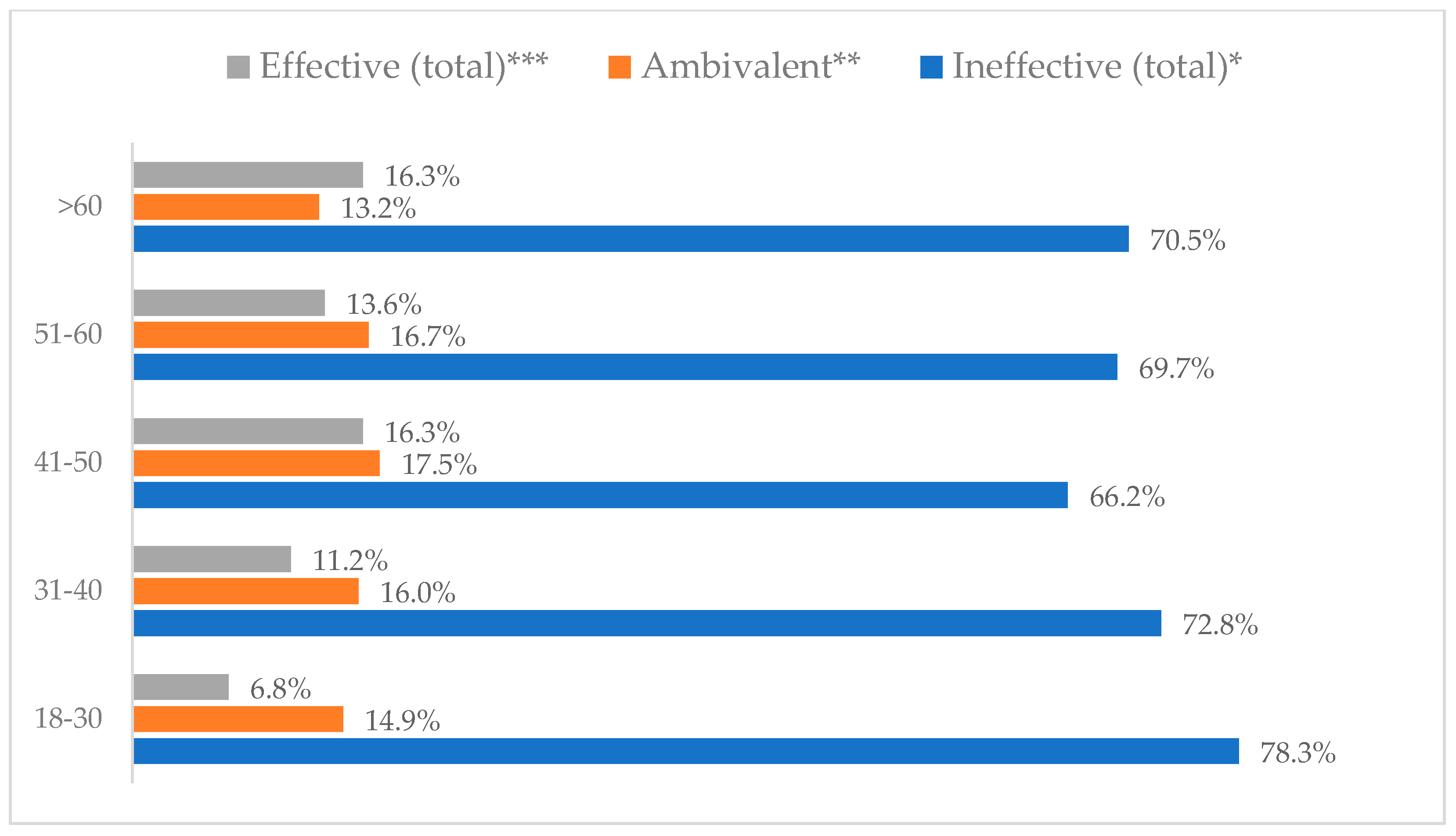
Figure 2.
Wearing a protective mask that covers the mouth and nose to prevent influenza virus infection by age (N = 905). * Sum of responses: completely ineffective, ineffective, rather ineffective; ** Response: neither ineffective nor effective; *** Sum of responses: rather effective, effective, completely effective.
Figure 2.
Wearing a protective mask that covers the mouth and nose to prevent influenza virus infection by age (N = 905). * Sum of responses: completely ineffective, ineffective, rather ineffective; ** Response: neither ineffective nor effective; *** Sum of responses: rather effective, effective, completely effective.
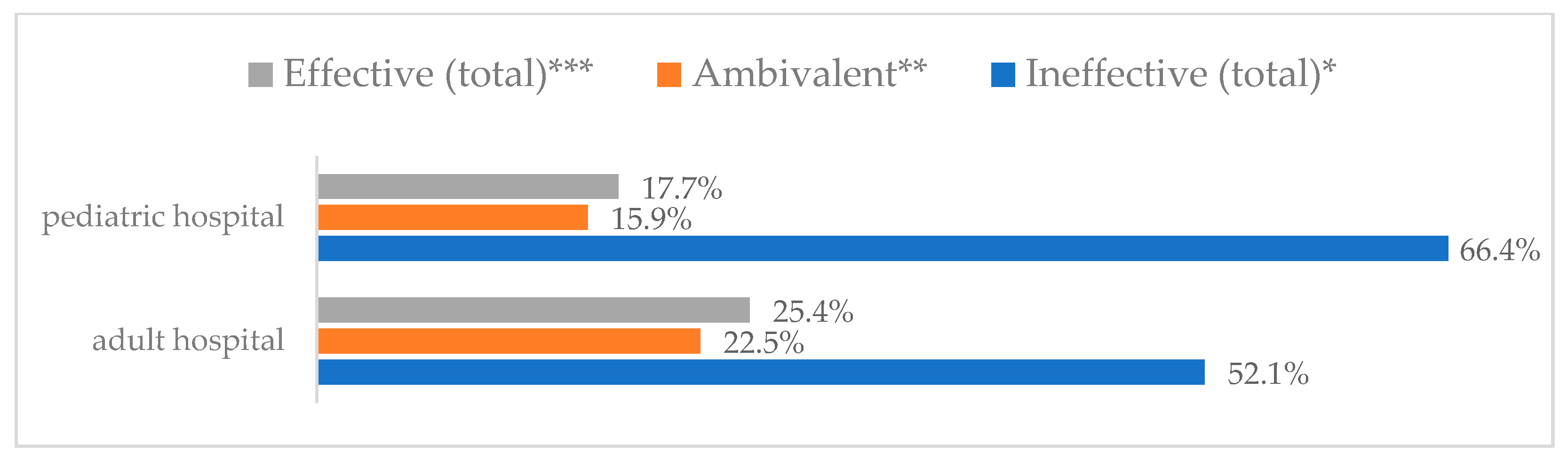
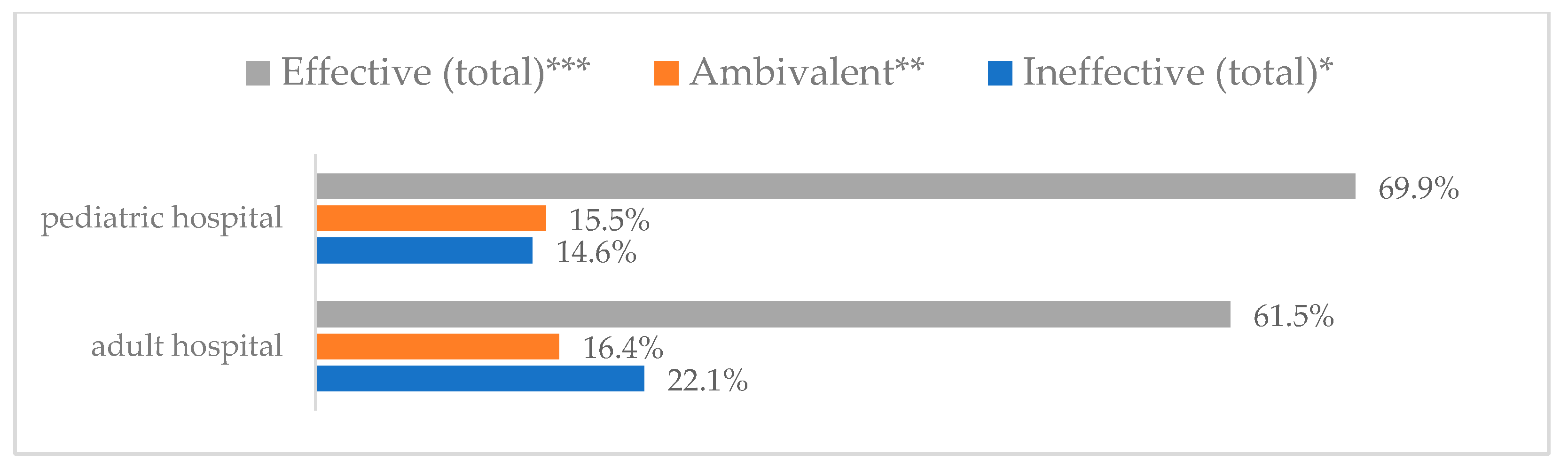
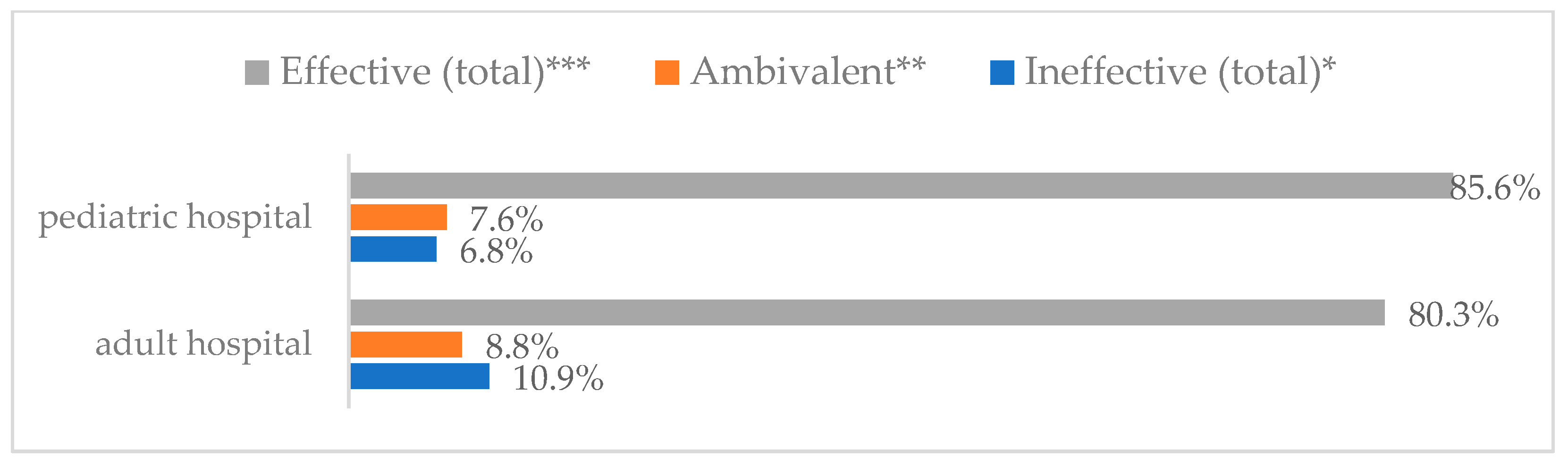
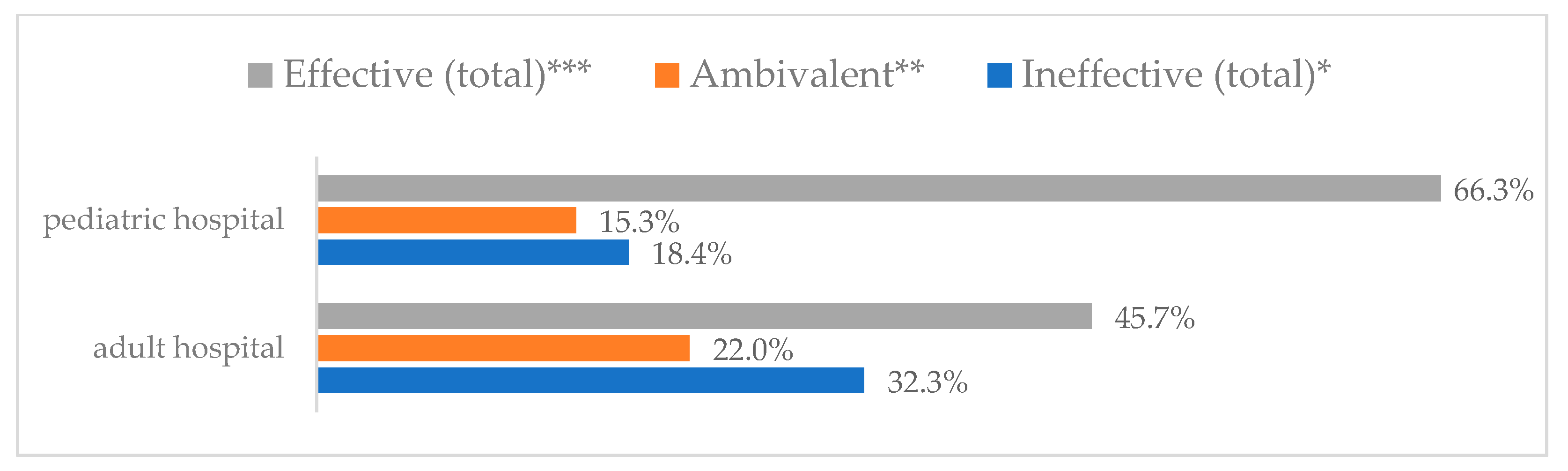
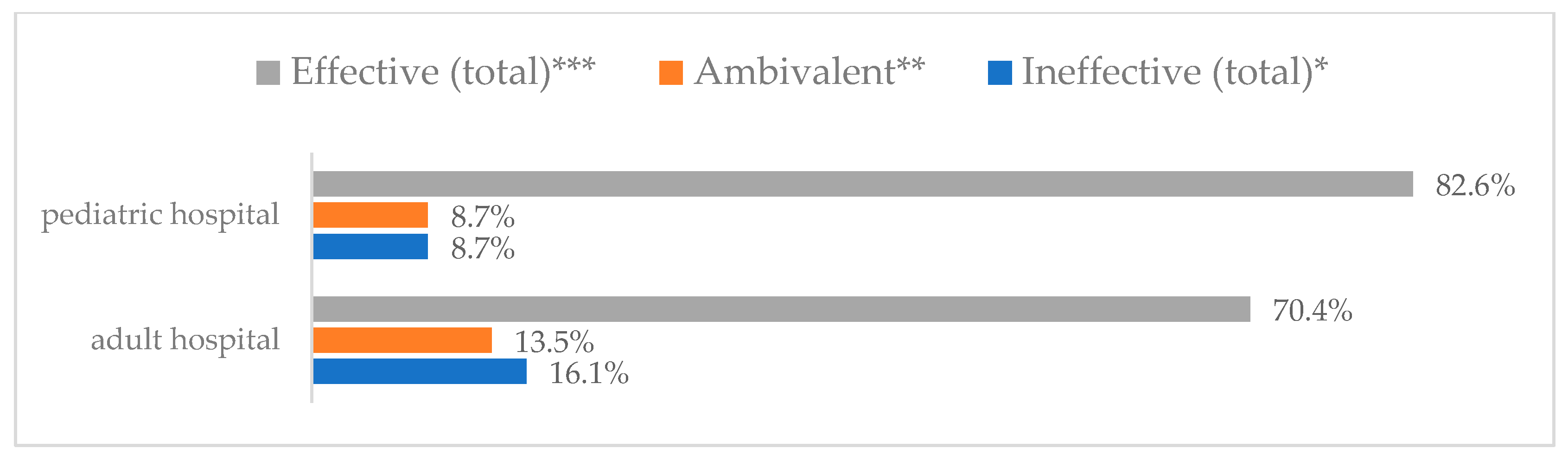
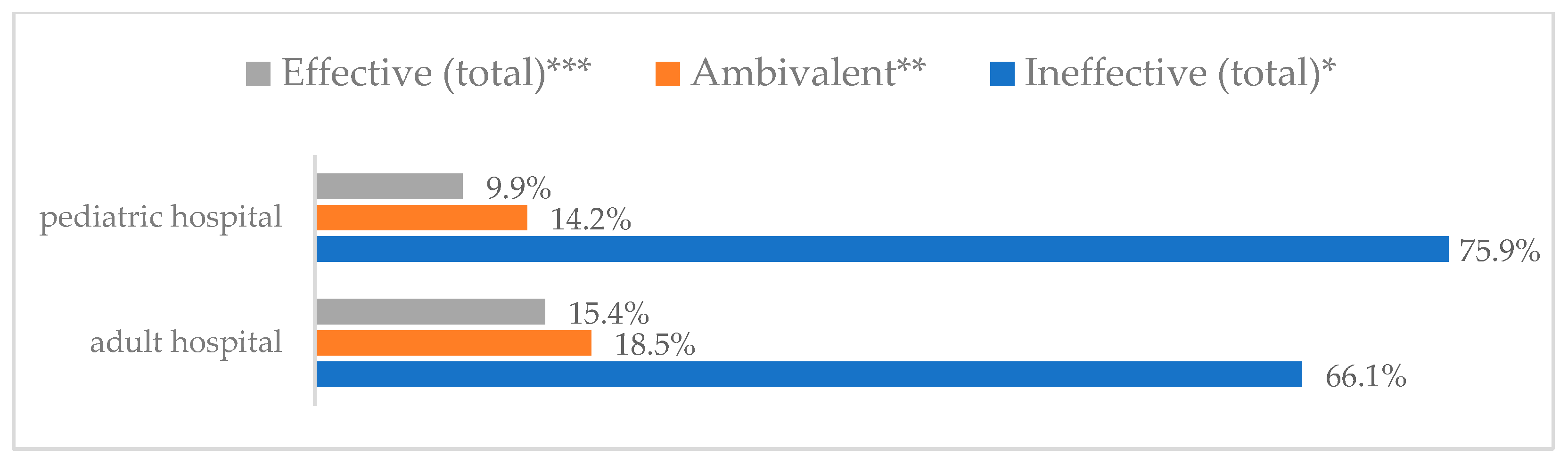
Figure 3.
Wearing a protective mask that covers the mouth and nose to prevent influenza virus infection by type of hospital (N = 905). * Sum of responses: completely ineffective, ineffective, rather ineffective; ** Response: neither ineffective nor effective; *** Sum of responses: rather effective, effective, completely effective.
Figure 3.
Wearing a protective mask that covers the mouth and nose to prevent influenza virus infection by type of hospital (N = 905). * Sum of responses: completely ineffective, ineffective, rather ineffective; ** Response: neither ineffective nor effective; *** Sum of responses: rather effective, effective, completely effective.
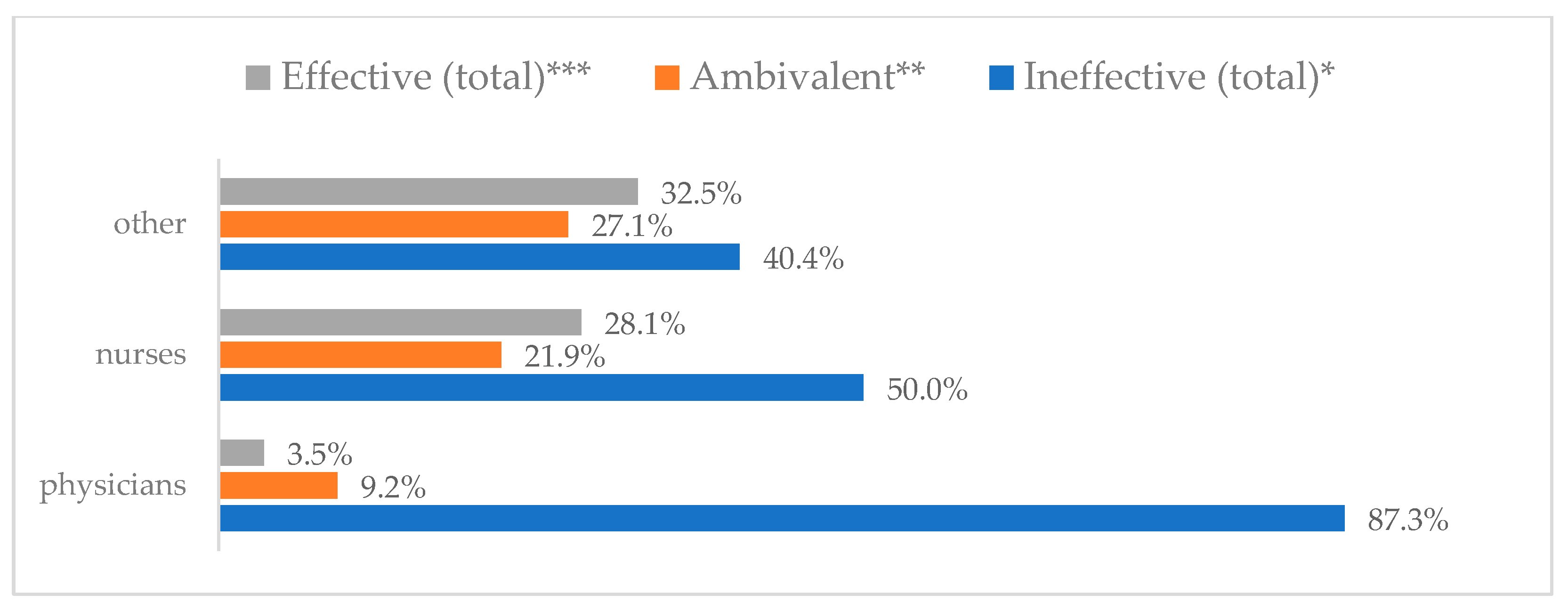
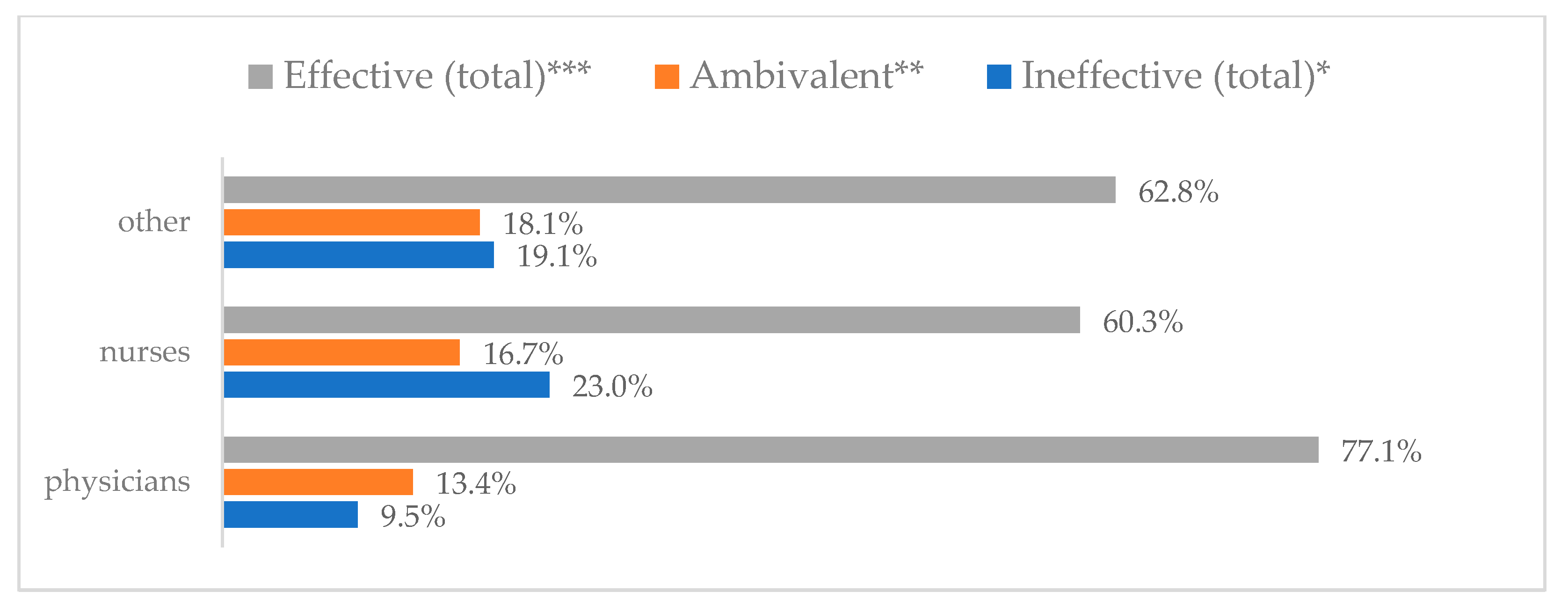
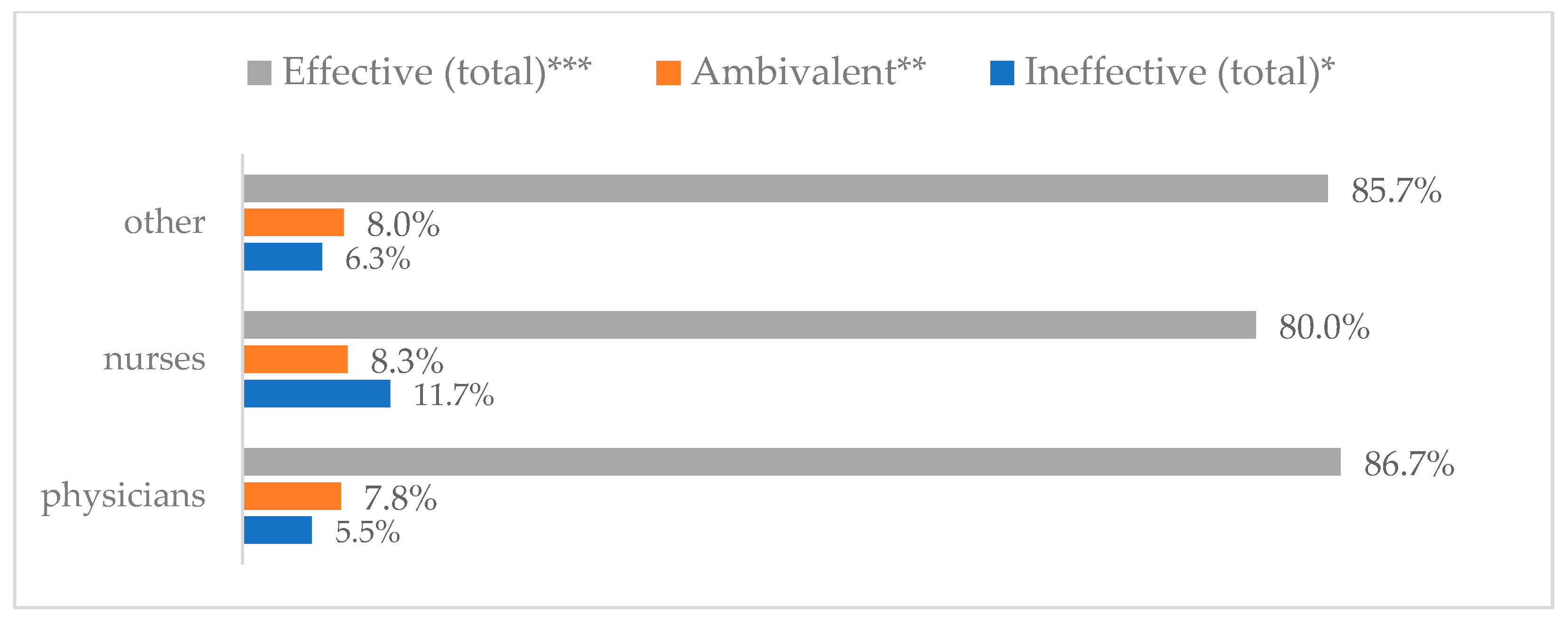
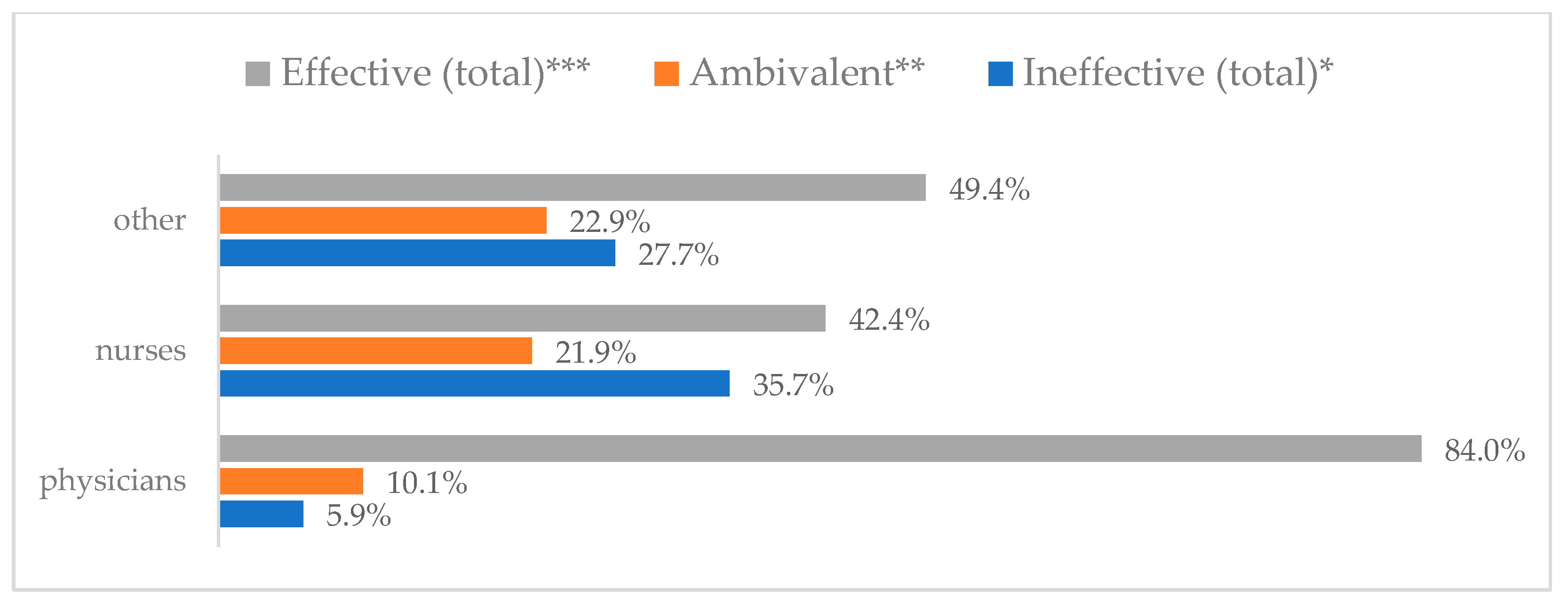
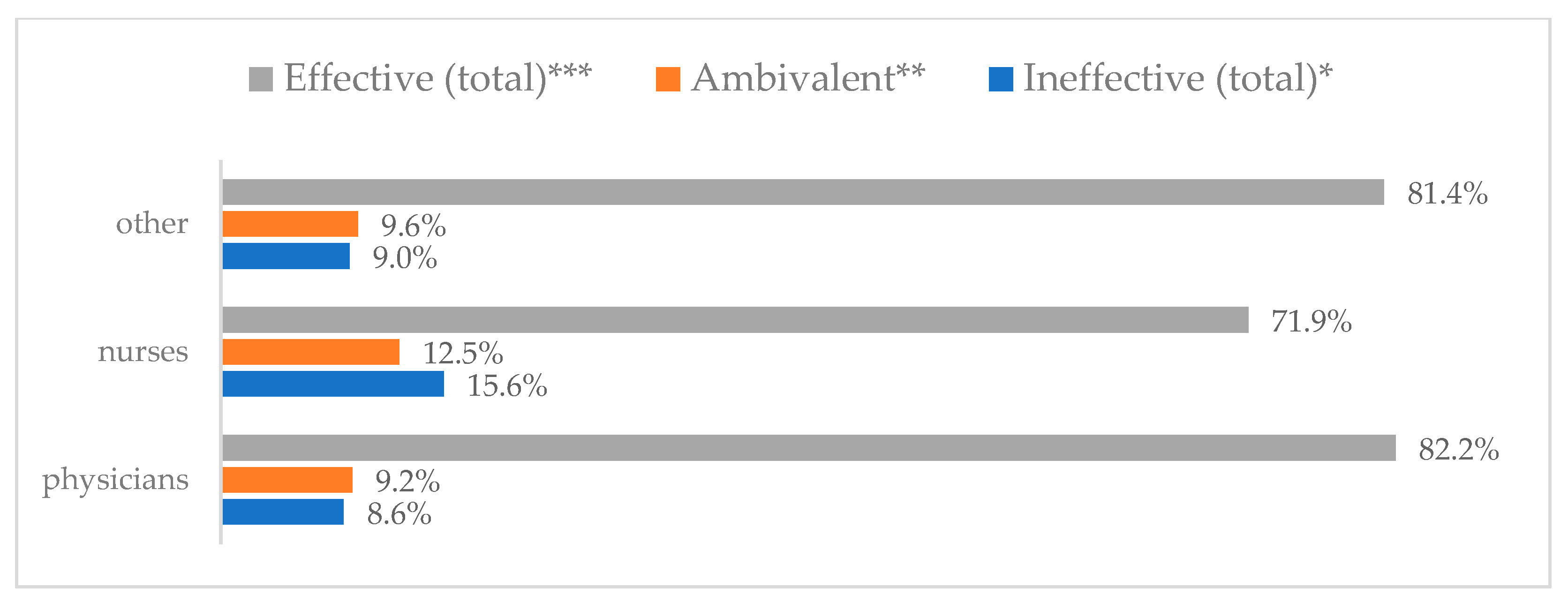
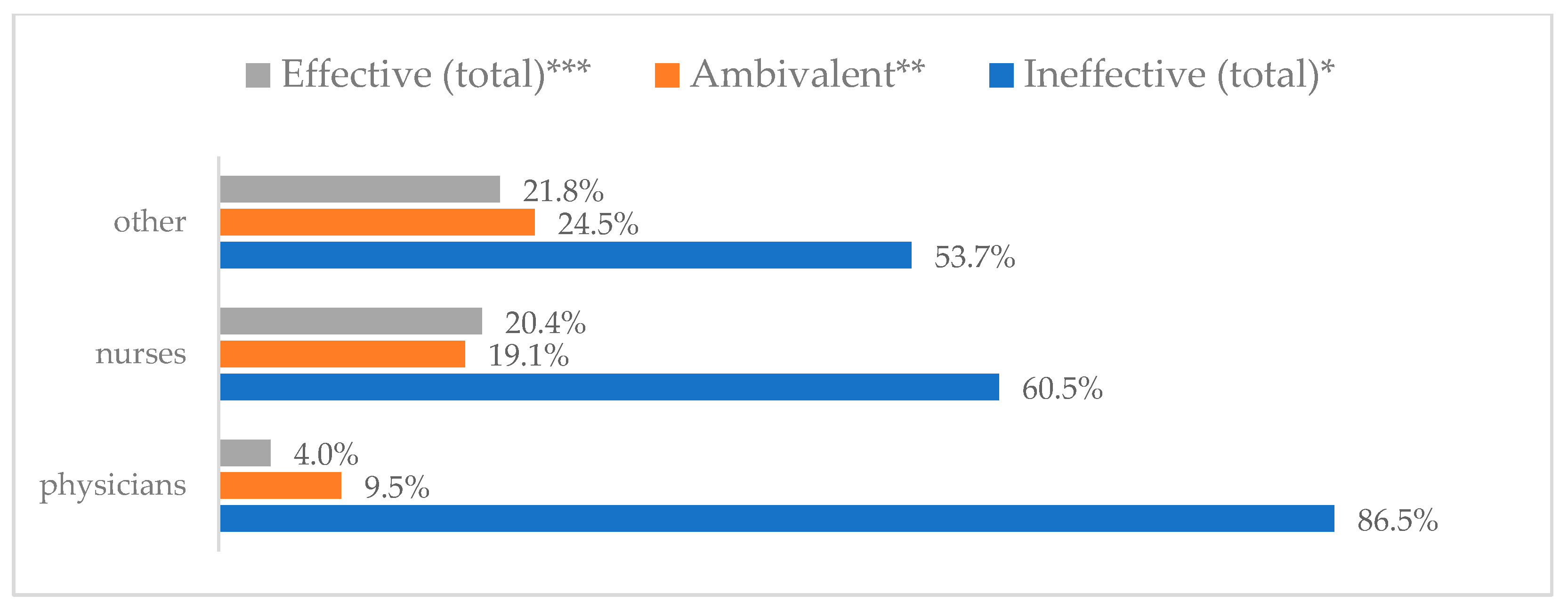
Figure 4.
Wearing a protective mask that covers the mouth and nose to prevent influenza virus infection by profession (N = 905). * Sum of responses: completely ineffective, ineffective, rather ineffective; ** Response: neither ineffective nor effective; *** Sum of responses: rather effective, effective, completely effective.
Figure 4.
Wearing a protective mask that covers the mouth and nose to prevent influenza virus infection by profession (N = 905). * Sum of responses: completely ineffective, ineffective, rather ineffective; ** Response: neither ineffective nor effective; *** Sum of responses: rather effective, effective, completely effective.
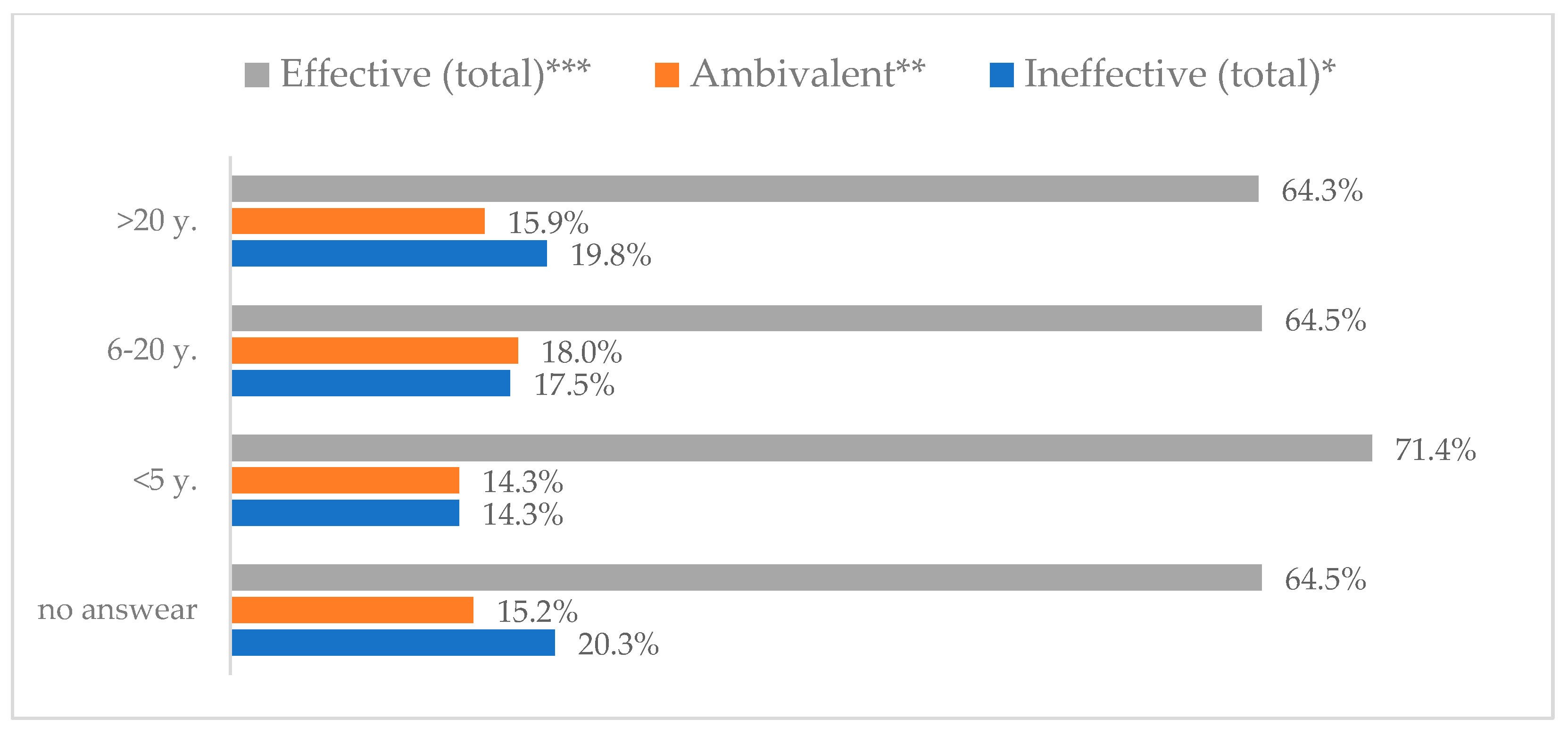
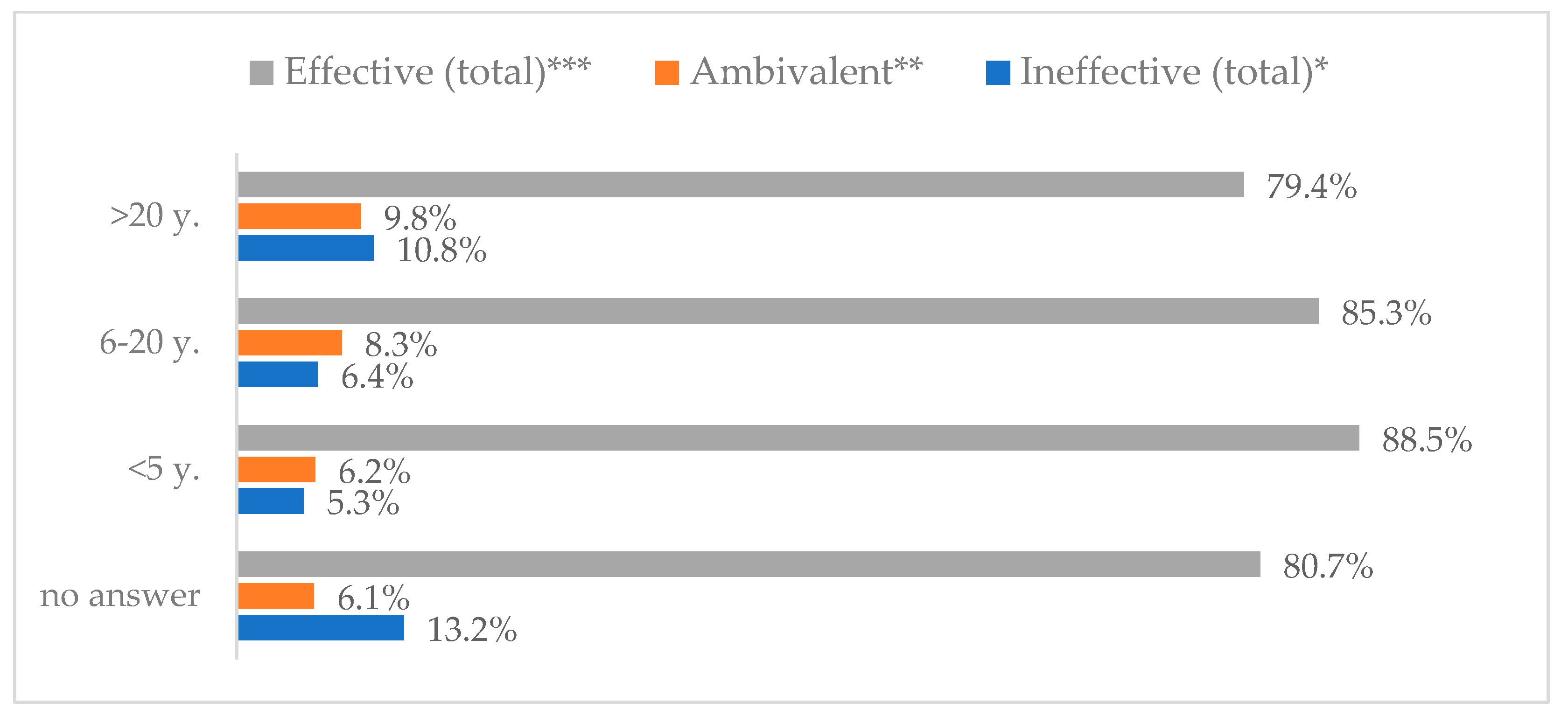
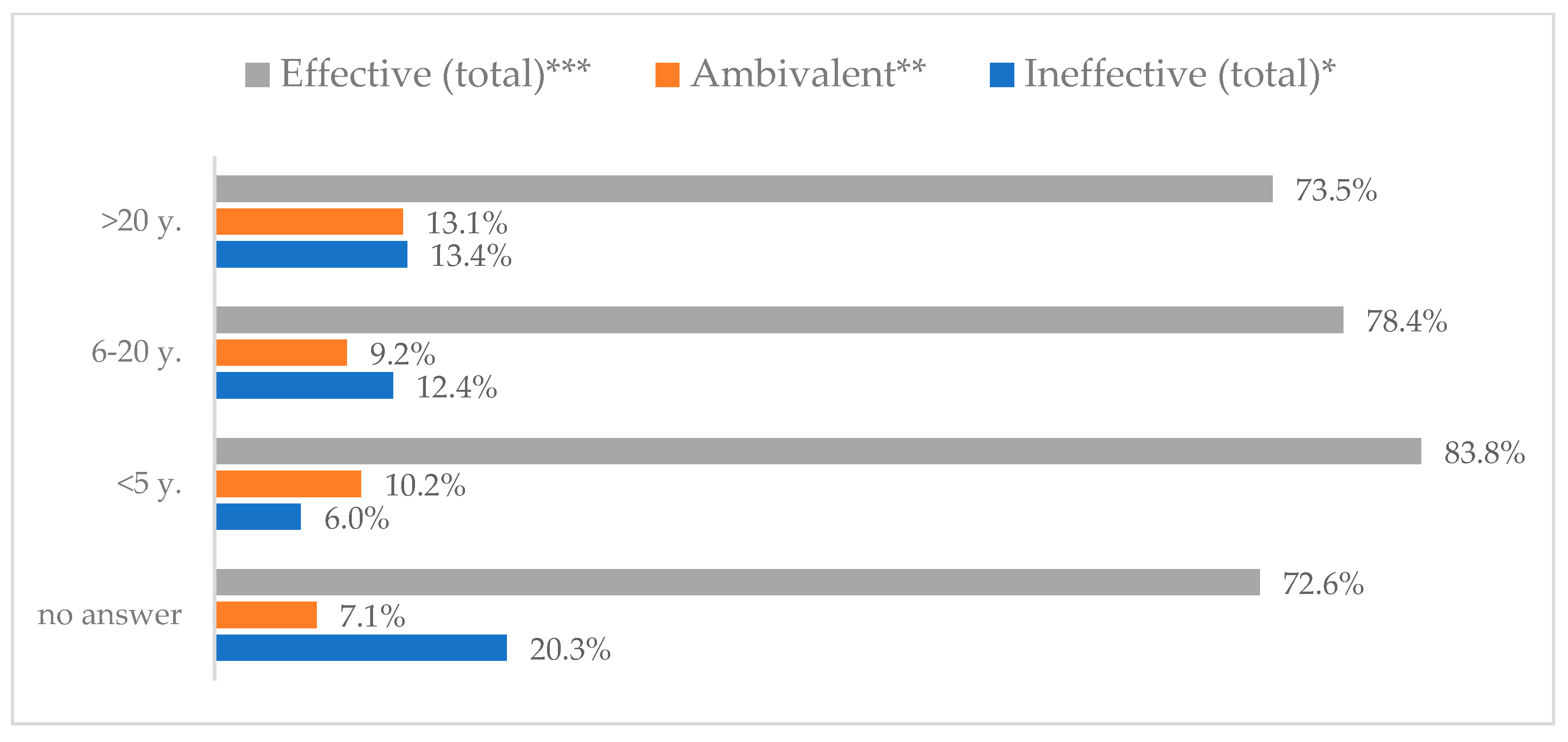
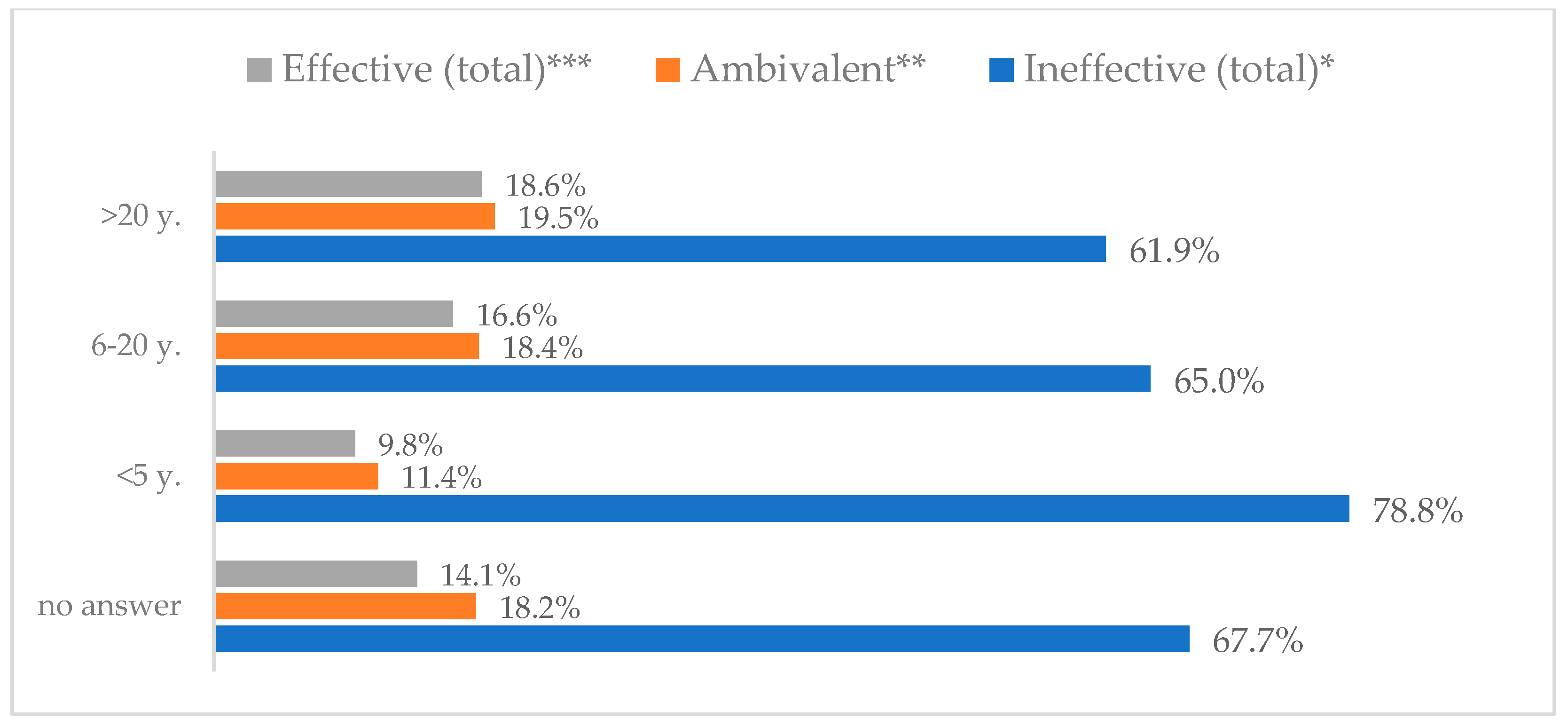
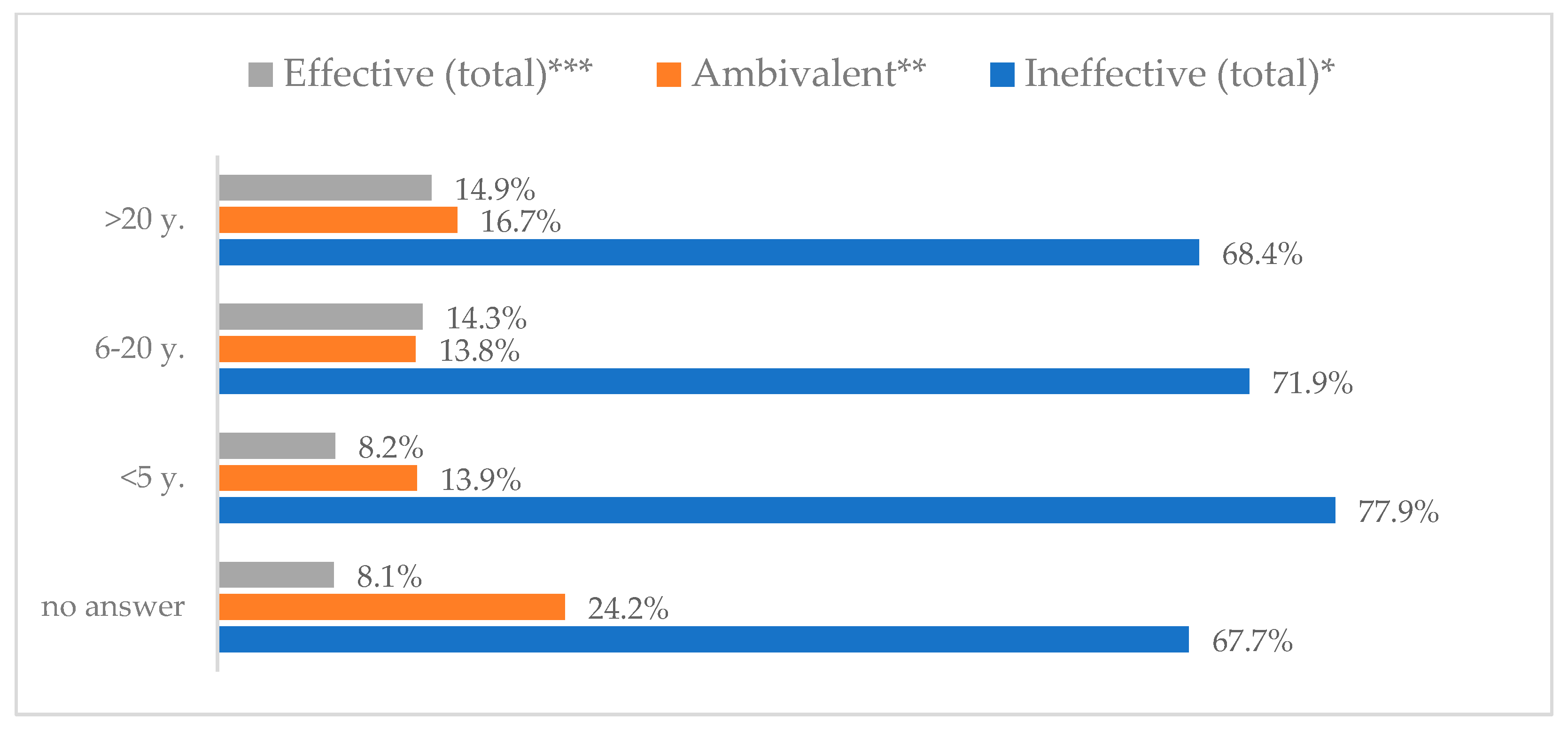
Figure 5.
Wearing a protective mask that covers the mouth and nose to prevent influenza virus infection by seniority (N = 905). * Sum of responses: completely ineffective, ineffective, rather ineffective; ** Response: neither ineffective nor effective; *** Sum of responses: rather effective, effective, completely effective.
Figure 5.
Wearing a protective mask that covers the mouth and nose to prevent influenza virus infection by seniority (N = 905). * Sum of responses: completely ineffective, ineffective, rather ineffective; ** Response: neither ineffective nor effective; *** Sum of responses: rather effective, effective, completely effective.
Figure 6.
Hand washing to prevent influenza virus infection by gender (N = 905). * Sum of responses: completely ineffective, ineffective, rather ineffective; ** Response: neither ineffective nor effective; *** Sum of responses: rather effective, effective, completely effective.
Figure 6.
Hand washing to prevent influenza virus infection by gender (N = 905). * Sum of responses: completely ineffective, ineffective, rather ineffective; ** Response: neither ineffective nor effective; *** Sum of responses: rather effective, effective, completely effective.
Figure 7.
Hand washing to prevent influenza virus infection by age (N = 905). * Sum of responses: completely ineffective, ineffective, rather ineffective; ** Response: neither ineffective nor effective; *** Sum of responses: rather effective, effective, completely effective.
Figure 7.
Hand washing to prevent influenza virus infection by age (N = 905). * Sum of responses: completely ineffective, ineffective, rather ineffective; ** Response: neither ineffective nor effective; *** Sum of responses: rather effective, effective, completely effective.
Figure 8.
Hand washing as a means of preventing influenza virus infection by type of hospital (N = 905). * Sum of responses: completely ineffective, ineffective, rather ineffective; ** Response: neither ineffective nor effective; *** Sum of responses: rather effective, effective, completely effective.
Figure 8.
Hand washing as a means of preventing influenza virus infection by type of hospital (N = 905). * Sum of responses: completely ineffective, ineffective, rather ineffective; ** Response: neither ineffective nor effective; *** Sum of responses: rather effective, effective, completely effective.
Figure 9.
Hand washing to prevent influenza virus infection by profession (N = 905). * Sum of responses: completely ineffective, ineffective, rather ineffective; ** Response: neither ineffective nor effective; *** Sum of responses: rather effective, effective, completely effective.
Figure 9.
Hand washing to prevent influenza virus infection by profession (N = 905). * Sum of responses: completely ineffective, ineffective, rather ineffective; ** Response: neither ineffective nor effective; *** Sum of responses: rather effective, effective, completely effective.
Figure 10.
Hand washing to prevent influenza virus infection by seniority (N = 905). * Sum of responses: completely ineffective, ineffective, rather ineffective; ** Response: neither ineffective nor effective; *** Sum of responses: rather effective, effective, completely effective.
Figure 10.
Hand washing to prevent influenza virus infection by seniority (N = 905). * Sum of responses: completely ineffective, ineffective, rather ineffective; ** Response: neither ineffective nor effective; *** Sum of responses: rather effective, effective, completely effective.
Figure 11.
Influenza vaccination to prevent influenza virus infection by gender (N = 905). * Sum of responses: completely ineffective, ineffective, rather ineffective; ** Response: neither ineffective nor effective; *** Sum of responses: rather effective, effective, completely effective.
Figure 11.
Influenza vaccination to prevent influenza virus infection by gender (N = 905). * Sum of responses: completely ineffective, ineffective, rather ineffective; ** Response: neither ineffective nor effective; *** Sum of responses: rather effective, effective, completely effective.
Figure 12.
Influenza vaccination to prevent influenza virus infection by age (N = 905). * Sum of responses: completely ineffective, ineffective, rather ineffective; ** Response: neither ineffective nor effective; *** Sum of responses: rather effective, effective, completely effective.
Figure 12.
Influenza vaccination to prevent influenza virus infection by age (N = 905). * Sum of responses: completely ineffective, ineffective, rather ineffective; ** Response: neither ineffective nor effective; *** Sum of responses: rather effective, effective, completely effective.
Figure 13.
Influenza vaccination to prevent influenza virus infection by type of hospital (N = 905). * Sum of responses: completely ineffective, ineffective, rather ineffective; ** Response: neither ineffective nor effective; *** Sum of responses: rather effective, effective, completely effective.
Figure 13.
Influenza vaccination to prevent influenza virus infection by type of hospital (N = 905). * Sum of responses: completely ineffective, ineffective, rather ineffective; ** Response: neither ineffective nor effective; *** Sum of responses: rather effective, effective, completely effective.
Figure 14.
Influenza vaccination to prevent influenza virus infection by profession (N = 905). * Sum of responses: completely ineffective, ineffective, rather ineffective; ** Response: neither ineffective nor effective; *** Sum of responses: rather effective, effective, completely effective.
Figure 14.
Influenza vaccination to prevent influenza virus infection by profession (N = 905). * Sum of responses: completely ineffective, ineffective, rather ineffective; ** Response: neither ineffective nor effective; *** Sum of responses: rather effective, effective, completely effective.
Figure 15.
Influenza vaccination to prevent influenza virus infection by seniority (N = 905). * Sum of responses: completely ineffective, ineffective, rather ineffective; ** Response: neither ineffective nor effective; *** Sum of responses: rather effective, effective, completely effective.
Figure 15.
Influenza vaccination to prevent influenza virus infection by seniority (N = 905). * Sum of responses: completely ineffective, ineffective, rather ineffective; ** Response: neither ineffective nor effective; *** Sum of responses: rather effective, effective, completely effective.
Figure 16.
Avoiding contact with sick people to prevent influenza virus infection by gender (N = 905). * Sum of responses: completely ineffective, ineffective, rather ineffective; ** Response: neither ineffective nor effective; *** Sum of responses: rather effective, effective, completely effective.
Figure 16.
Avoiding contact with sick people to prevent influenza virus infection by gender (N = 905). * Sum of responses: completely ineffective, ineffective, rather ineffective; ** Response: neither ineffective nor effective; *** Sum of responses: rather effective, effective, completely effective.
Figure 17.
Avoiding contact with sick people to prevent influenza virus infection by age (N = 905). * Sum of responses: completely ineffective, ineffective, rather ineffective; ** Response: neither ineffective nor effective; *** Sum of responses: rather effective, effective, completely effective.
Figure 17.
Avoiding contact with sick people to prevent influenza virus infection by age (N = 905). * Sum of responses: completely ineffective, ineffective, rather ineffective; ** Response: neither ineffective nor effective; *** Sum of responses: rather effective, effective, completely effective.
Figure 18.
Avoiding contact with sick people to prevent influenza virus infection by type of hospital (N = 905). * Sum of responses: completely ineffective, ineffective, rather ineffective; ** Response: neither ineffective nor effective; *** Sum of responses: rather effective, effective, completely effective.
Figure 18.
Avoiding contact with sick people to prevent influenza virus infection by type of hospital (N = 905). * Sum of responses: completely ineffective, ineffective, rather ineffective; ** Response: neither ineffective nor effective; *** Sum of responses: rather effective, effective, completely effective.
Figure 19.
Avoiding contact with sick people to prevent influenza virus infection by profession (N = 905). * Sum of responses: completely ineffective, ineffective, rather ineffective; ** Response: neither ineffective nor effective; *** Sum of responses: rather effective, effective, completely effective.
Figure 19.
Avoiding contact with sick people to prevent influenza virus infection by profession (N = 905). * Sum of responses: completely ineffective, ineffective, rather ineffective; ** Response: neither ineffective nor effective; *** Sum of responses: rather effective, effective, completely effective.
Figure 20.
Avoiding contact with sick people to prevent influenza virus infection by seniority (N = 905). * Sum of responses: completely ineffective, ineffective, rather ineffective; ** Response: neither ineffective nor effective; *** Sum of responses: rather effective, effective, completely effective.
Figure 20.
Avoiding contact with sick people to prevent influenza virus infection by seniority (N = 905). * Sum of responses: completely ineffective, ineffective, rather ineffective; ** Response: neither ineffective nor effective; *** Sum of responses: rather effective, effective, completely effective.
Figure 21.
Eating garlic to prevent influenza virus infection by gender (N = 905). * Sum of responses: completely ineffective, ineffective, rather ineffective; ** Response: neither ineffective nor effective; *** Sum of responses: rather effective, effective, completely effective.
Figure 21.
Eating garlic to prevent influenza virus infection by gender (N = 905). * Sum of responses: completely ineffective, ineffective, rather ineffective; ** Response: neither ineffective nor effective; *** Sum of responses: rather effective, effective, completely effective.
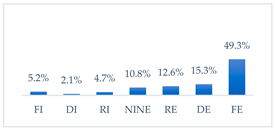
Figure 22.
Eating garlic to prevent influenza virus infection by age (N = 905). * Sum of responses: completely ineffective, ineffective, rather ineffective; ** Response: neither ineffective nor effective; *** Sum of responses: rather effective, effective, completely effective.
Figure 22.
Eating garlic to prevent influenza virus infection by age (N = 905). * Sum of responses: completely ineffective, ineffective, rather ineffective; ** Response: neither ineffective nor effective; *** Sum of responses: rather effective, effective, completely effective.
Figure 23.
Eating garlic to prevent influenza virus infection by type of hospital (N = 905). * Sum of responses: completely ineffective, ineffective, rather ineffective; ** Response: neither ineffective nor effective; *** Sum of responses: rather effective, effective, completely effective.
Figure 23.
Eating garlic to prevent influenza virus infection by type of hospital (N = 905). * Sum of responses: completely ineffective, ineffective, rather ineffective; ** Response: neither ineffective nor effective; *** Sum of responses: rather effective, effective, completely effective.
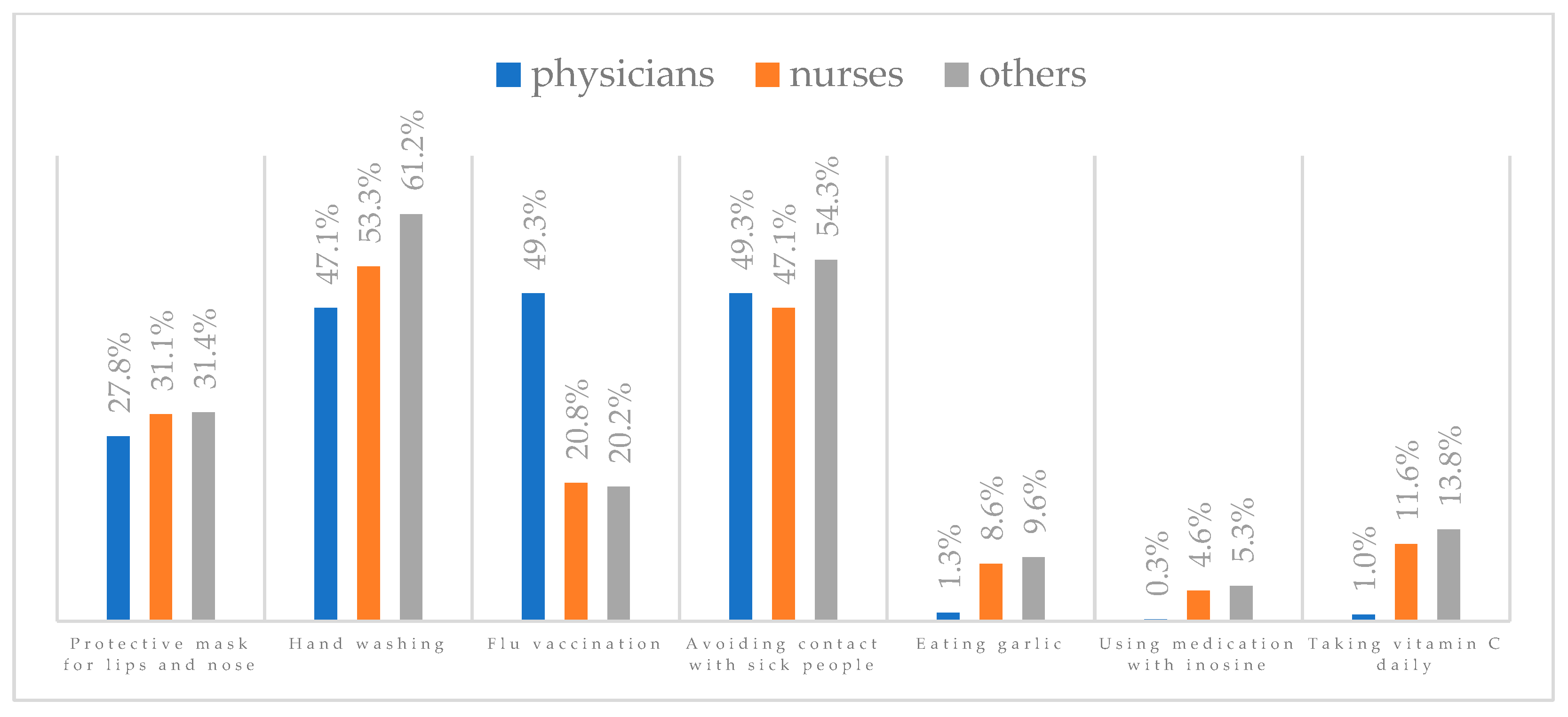
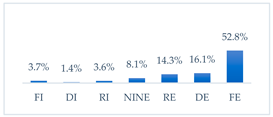
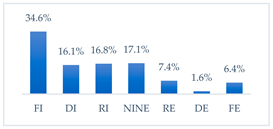
Figure 24.
Eating garlic to prevent influenza virus infection by profession (N = 905). * Sum of responses: completely ineffective, ineffective, rather ineffective; ** Response: neither ineffective nor effective; *** Sum of responses: rather effective, effective, completely effective.
Figure 24.
Eating garlic to prevent influenza virus infection by profession (N = 905). * Sum of responses: completely ineffective, ineffective, rather ineffective; ** Response: neither ineffective nor effective; *** Sum of responses: rather effective, effective, completely effective.
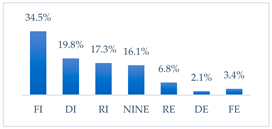
Figure 25.
Eating garlic to prevent influenza virus infection by seniority (N = 905). * Sum of responses: completely ineffective, ineffective, rather ineffective; ** Response: neither ineffective nor effective; *** Sum of responses: rather effective, effective, completely effective.
Figure 25.
Eating garlic to prevent influenza virus infection by seniority (N = 905). * Sum of responses: completely ineffective, ineffective, rather ineffective; ** Response: neither ineffective nor effective; *** Sum of responses: rather effective, effective, completely effective.
Figure 26.
Taking preparations with inosine to prevent influenza virus infection by gender (N = 905). * Sum of responses: completely ineffective, ineffective, rather ineffective; ** Response: neither ineffective nor effective; *** Sum of responses: rather effective, effective, completely effective.
Figure 26.
Taking preparations with inosine to prevent influenza virus infection by gender (N = 905). * Sum of responses: completely ineffective, ineffective, rather ineffective; ** Response: neither ineffective nor effective; *** Sum of responses: rather effective, effective, completely effective.
Figure 27.
Taking preparations with inosine to prevent influenza virus infection by age (N = 905). * Sum of responses: completely ineffective, ineffective, rather ineffective; ** Response: neither ineffective nor effective; *** Sum of responses: rather effective, effective, completely effective.
Figure 27.
Taking preparations with inosine to prevent influenza virus infection by age (N = 905). * Sum of responses: completely ineffective, ineffective, rather ineffective; ** Response: neither ineffective nor effective; *** Sum of responses: rather effective, effective, completely effective.
Figure 28.
Taking preparations with inosine to prevent influenza virus infection by type of hospital (N = 905). * Sum of responses: completely ineffective, ineffective, rather ineffective; ** Response: neither ineffective nor effective; *** Sum of responses: rather effective, effective, completely effective.
Figure 28.
Taking preparations with inosine to prevent influenza virus infection by type of hospital (N = 905). * Sum of responses: completely ineffective, ineffective, rather ineffective; ** Response: neither ineffective nor effective; *** Sum of responses: rather effective, effective, completely effective.
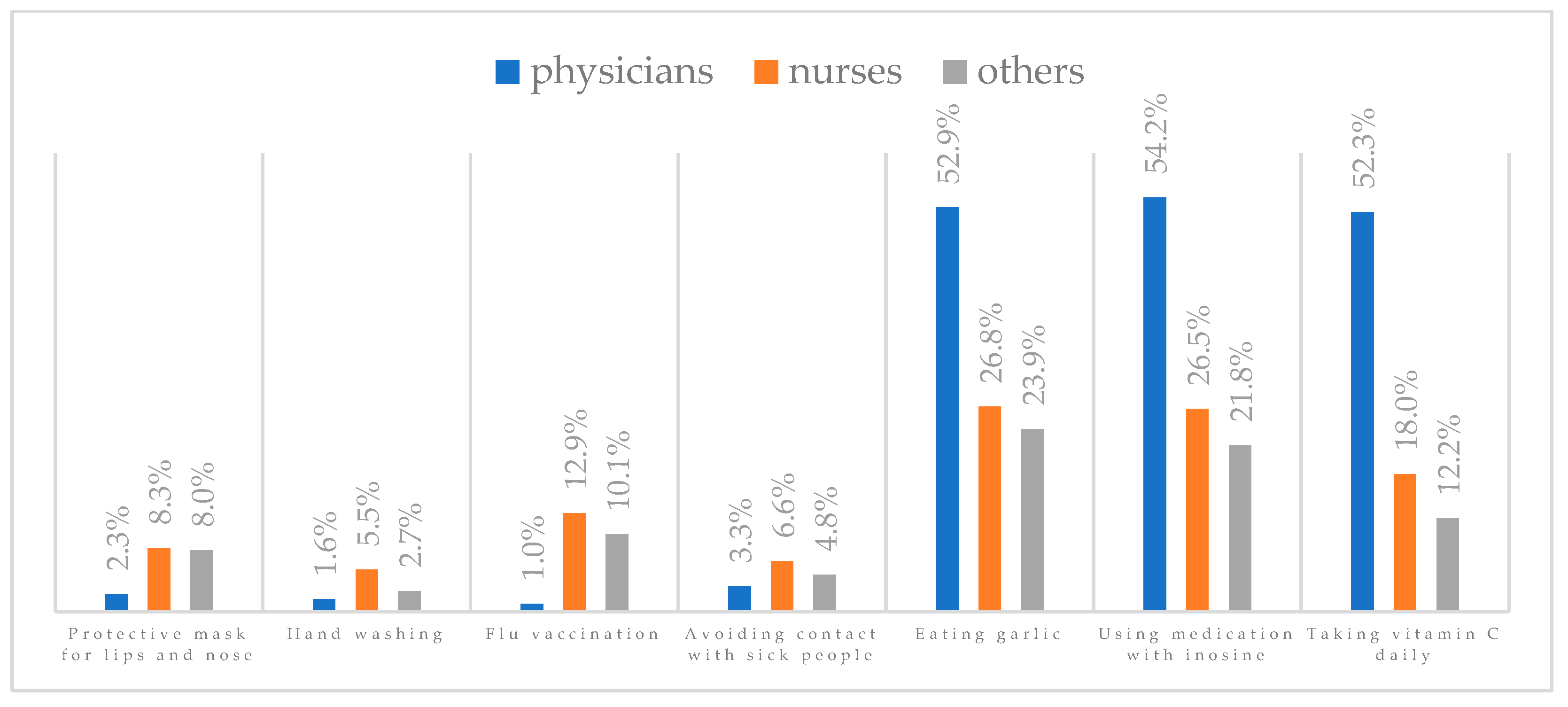
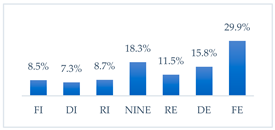
Figure 29.
Taking preparations with inosine to prevent influenza virus infection by profession (N = 905). * Sum of responses: completely ineffective, ineffective, rather ineffective; ** Response: neither ineffective nor effective; *** Sum of responses: rather effective, effective, completely effective.
Figure 29.
Taking preparations with inosine to prevent influenza virus infection by profession (N = 905). * Sum of responses: completely ineffective, ineffective, rather ineffective; ** Response: neither ineffective nor effective; *** Sum of responses: rather effective, effective, completely effective.
Figure 30.
Taking preparations with inosine to prevent influenza virus infection by seniority (N = 905). * Sum of responses: completely ineffective, ineffective, rather ineffective; ** Response: neither ineffective nor effective; *** Sum of responses: rather effective, effective, completely effective.
Figure 30.
Taking preparations with inosine to prevent influenza virus infection by seniority (N = 905). * Sum of responses: completely ineffective, ineffective, rather ineffective; ** Response: neither ineffective nor effective; *** Sum of responses: rather effective, effective, completely effective.
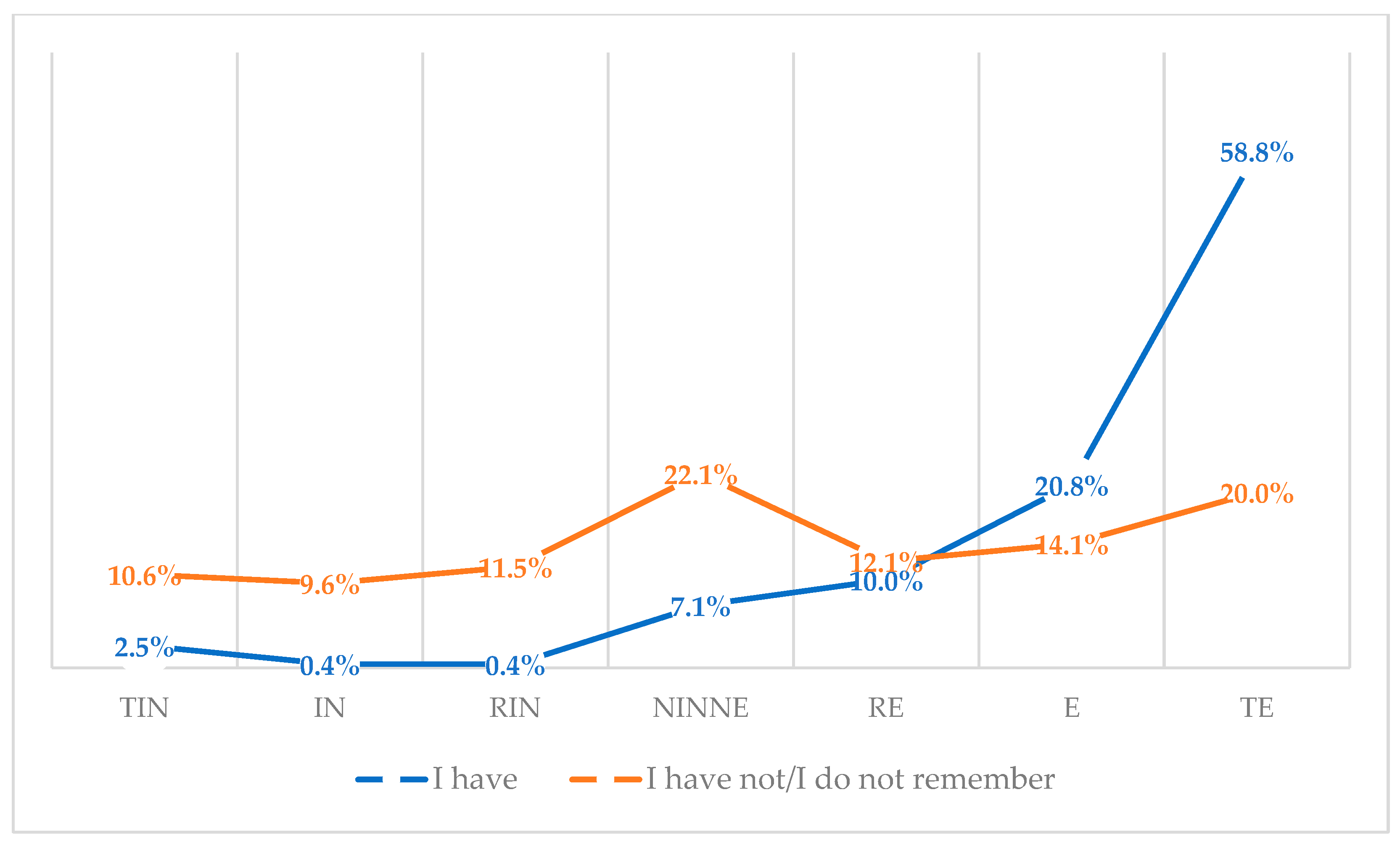
Figure 38.
Attitudes toward influenza vaccination to prevent influenza virus infection among vaccinated and unvaccinated against influenza (N = 950). Note. TIN-totally ineffective, IN-ineffective, RIN-rather ineffective, NINE-neither ineffective nor effective, RE-rather effective, E-effective, TE-totally effective.
Figure 38.
Attitudes toward influenza vaccination to prevent influenza virus infection among vaccinated and unvaccinated against influenza (N = 950). Note. TIN-totally ineffective, IN-ineffective, RIN-rather ineffective, NINE-neither ineffective nor effective, RE-rather effective, E-effective, TE-totally effective.
Table 1.
Sociodemographic characteristics (N = 950).
Table 1.
Sociodemographic characteristics (N = 950).
| Variables | N (%) |
|---|
| Gender |
| Female | 807 (84.9) |
| Male | 143 (15.1) |
| Age |
| 18–30 | 221 (23.3) |
| 31–40 | 206 (21.7) |
| 41–50 | 234 (24.6) |
| 51–60 | 221 (23.3) |
| >60 | 68 (7.1) |
| Type of hospital |
| Adult hospital | 422 (44.4) |
| Pediatric hospital | 528 (55.6) |
| Profession |
| Physician | 306 (32.2) |
| Nurse | 456 (48.0) |
| Other | 188 (19.8) |
| Seniority |
| <5 y. | 245 (25.8) |
| 6–20 y. | 217 (22.8) |
| >20 y. | 389 (40.9) |
| Refuse to answer | 99 (10.5) |
Table 2.
Evaluation of the effectiveness of methods to prevent influenza infections (N = 950).
Table 3.
Evaluation of mouth and nose covering mask to prevent influenza virus infection by sociodemographic category (N = 950).
Table 3.
Evaluation of mouth and nose covering mask to prevent influenza virus infection by sociodemographic category (N = 950).
| Variables | Mean | 95% CI | SE | MD | OR | χ2 | df | p-Value |
|---|
| Gender |
| Female | 5.05 | 4.92–5.18 | 0.065 | 5.00 | 1.836 | 8.251 | 6 | 0.220 |
| Male | 5.23 | 4.98–5.49 | 0.129 | 5.00 | 1.546 |
| Age |
| 18–30 | 5.05 | 4.83–5.26 | 0.111 | 5.00 | 1.645 | 41.541 | 24 | 0.015 |
| 31–40 | 5.11 | 4.87–5.35 | 0.112 | 5.00 | 1.748 |
| 41–50 | 5.06 | 4.83–5.29 | 0.118 | 5.00 | 1.803 |
| 51–60 | 5.16 | 4.91–5.42 | 0.125 | 5.00 | 1.863 |
| >60 | 4.88 | 4.36–5.41 | 0.262 | 5.00 | 2.162 |
| Type of hospital |
| Adult hospital | 4.93 | 4.75–5.12 | 0.093 | 5.00 | 1.908 | 13.162 | 6 | 0.041 |
| Pediatric hospital | 5.19 | 5.05–5.34 | 0.074 | 5.00 | 1.694 |
| Profession |
| Physicians | 5.43 | 5.27–5.59 | 0.082 | 6.00 | 1.443 | 53.776 | 12 | <0.001 |
| Nurses | 4.88 | 4.70–5.06 | 0.091 | 5.00 | 1.939 |
| Others | 4.99 | 4.72–5.26 | 0.137 | 5.00 | 1.876 |
| Seniority |
| <5 y. | 5.19 | 4.98–5.40 | 0.481 | 6.00 | 1.649 | 38.867 | 18 | 0.003 |
| 6–20 y. | 5.01 | 4.77–5.24 | 0.120 | 5.00 | 1.761 |
| >20 y. | 5.10 | 4.91–5.29 | 0.096 | 5.00 | 1.903 |
| Refuse to answer | 4.87 | 4.51–5.23 | 0.180 | 5.00 | 1.788 |
Table 4.
Evaluation of handwashing as a means of preventing influenza virus infection by sociodemographic category (N = 950).
Table 4.
Evaluation of handwashing as a means of preventing influenza virus infection by sociodemographic category (N = 950).
| Variables | Mean | 95% CI | SE | MD | OR | χ2 | df | p-Value |
|---|
| Gender |
| Female | 5.89 | 5.78–6.00 | 0.055 | 7.00 | 1.562 | 6.759 | 6 | 0.334 |
| Male | 5.80 | 5.54–6.06 | 0.132 | 6.00 | 1.577 |
| Age |
| 18–30 | 5.99 | 5.82–6.15 | 0.084 | 6.00 | 1.249 | 76.026 | 24 | <0.001 |
| 31–40 | 5.87 | 5.67–6.07 | 0.101 | 6.00 | 1.456 |
| 41–50 | 5.89 | 5.68–6.10 | 0.337 | 7.00 | 1.645 |
| 51–60 | 5.86 | 5.64–6.08 | 0.112 | 7.00 | 1.660 |
| >60 | 5.51 | 4.99–6.03 | 0.260 | 7.00 | 2.147 |
| Type of hospital |
| Adult hospital | 5.78 | 5.61–5.95 | 0.083 | 7.00 | 1.748 | 22.752 | 6 | <0.001 |
| Pediatric hospital | 5.95 | 5.84–6.07 | 0.061 | 7.00 | 1.396 |
| Profession |
| Physicians | 5.94 | 5.79–6.10 | 0.077 | 6.00 | 1.340 | 33.346 | 12 | <0.001 |
| Nurses | 5.75 | 5.59–5.91 | 0.081 | 7.00 | 1.731 |
| Others | 6.07 | 5.87–6.28 | 0.106 | 7.00 | 1.450 |
| Seniority |
| <5 y. | 6.00 | 5.84–6.16 | 0.083 | 6.00 | 1.293 | 66.493 | 18 | <0.001 |
| 6–20 y. | 5.89 | 5.70–6.09 | 0.097 | 7.00 | 1.428 |
| >20 y. | 5.84 | 5.67–6.01 | 0.088 | 7.00 | 1.740 |
| Refuse to answer | 5.68 | 5.33–6.02 | 0.173 | 6.00 | 1.719 |
Table 5.
Evaluation of influenza vaccination as a means of preventing influenza virus infection by sociodemographic category (N = 950).
Table 5.
Evaluation of influenza vaccination as a means of preventing influenza virus infection by sociodemographic category (N = 950).
| Variables | Mean | 95% CI | SE | MD | OR | χ2 | df | p-Value |
|---|
| Gender |
| Female | 4.72 | 4.58–4.86 | 0.070 | 5.00 | 1.991 | 20.859 | 6 | 0.002 |
| Male | 5.51 | 5.23–5.79 | 0.143 | 6.00 | 1.707 |
| Age |
| 18–30 | 5.23 | 5.00–5.47 | 0.119 | 6.00 | 1.775 | 82.197 | 24 | <0.001 |
| 31–40 | 5.32 | 5.07–5.57 | 0.125 | 6.00 | 1.787 |
| 41–50 | 4.36 | 4.11–4.61 | 0.128 | 4.00 | 1.952 |
| 51–60 | 4.66 | 4.38–4.93 | 0.141 | 5.00 | 2.093 |
| >60 | 4.35 | 3.82–4.89 | 0.267 | 4.00 | 2.204 |
| Type of hospital |
| Adult hospital | 4.39 | 4.20–4.58 | 0.098 | 4.00 | 2.007 | 58.481 | 6 | <0.001 |
| Pediatric hospital | 5.20 | 5.04–5.36 | 0.081 | 6.00 | 1.866 |
| Profession |
| Physicians | 5.97 | 5.82–6.12 | 0.077 | 6.00 | 1.353 | 165.902 | 12 | <0.001 |
| Nurses | 4.23 | 4.04–4.41 | 0.095 | 4.00 | 2.020 |
| Others | 4.48 | 4.21–4.54 | 0.139 | 4.00 | 1.911 |
| Seniority |
| <5 y. | 5.37 | 5.15–5.59 | 0.111 | 6.00 | 1.740 | 62.899 | 12 | <0.001 |
| 6–20 y. | 4.96 | 4.70–5.21 | 0.130 | 5.00 | 1.908 |
| >20 y. | 4.56 | 4.36–4.77 | 0.104 | 4.00 | 2.058 |
Table 6.
Rating of avoiding contact with sick people to prevent influenza virus infection by sociodemographic category (N = 950).
Table 6.
Rating of avoiding contact with sick people to prevent influenza virus infection by sociodemographic category (N = 950).
| Variables | Mean | 95% CI | SE | MD | OR | χ2 | df | p-Value |
|---|
| Gender |
| Female | 5.68 | 5.56–5.80 | 0.061 | 7.00 | 1.719 | 6.750 | 6 | 0.345 |
| Male | 5.57 | 5.27–5.86 | 0.151 | 6.00 | 1.802 |
| Age |
| 18–30 | 5.89 | 5.70–6.08 | 0.097 | 6.00 | 1.446 | 41.724 | 24 | 0.014 |
| 31–40 | 5.61 | 5.37–5.84 | 0.120 | 6.00 | 1.729 |
| 41–50 | 5.52 | 5.28–5.75 | 0.120 | 6.00 | 1.837 |
| 51–60 | 5.75 | 5.52–5.98 | 0.116 | 7.00 | 1.731 |
| >60 | 5.35 | 4.84–5.86 | 0.256 | 6.50 | 2.114 |
| Type of hospital |
| Adult hospital | 5.39 | 5.21–5.57 | 0.092 | 6.00 | 1.889 | 24.783 | 6 | <0.001 |
| Pediatric hospital | 5.88 | 5.75–6.02 | 0.068 | 7.00 | 1.561 |
| Profession |
| Physicians | 5.84 | 5.66–6.01 | 0.089 | 6.00 | 1.549 | 22.939 | 12 | 0.028 |
| Nurses | 5.46 | 5.29–5.64 | 0.087 | 6.00 | 1.864 |
| Others | 5.87 | 5.64–6.11 | 0.119 | 7.00 | 1.627 |
| Seniority |
| <5 y. | 5.92 | 5.74–6.10 | 0.091 | 6.00 | 1.428 | 42.802 | 18 | <0.001 |
| 6–20 y. | 5.72 | 5.50–5.95 | 0.116 | 7.00 | 1.702 |
| >20 y. | 5.54 | 5.36–5.71 | 0.094 | 6.00 | 1.853 |
| Refuse to answer | 5.39 | 5.01–5.77 | 0.192 | 6.00 | 1.910 |
Table 7.
Evaluation of eating garlic to prevent influenza virus infection by sociodemographic category (N = 950).
Table 7.
Evaluation of eating garlic to prevent influenza virus infection by sociodemographic category (N = 950).
| Variables | Mean | 95% CI | SE | MD | OR | χ2 | df | p-Value |
|---|
| Gender |
| Female | 2.85 | 2.73–2.97 | 0.062 | 3.00 | 1.770 | 19.857 | 6 | 0.003 |
| Male | 2.30 | 2.02–2.58 | 0.142 | 2.00 | 1.695 |
| Age |
| 18–30 | 2.37 | 2.15–2.58 | 0.110 | 2.00 | 1.631 | 41.606 | 24 | 0.014 |
| 31–40 | 2.56 | 2.34–2.78 | 0.111 | 2.00 | 1.591 |
| 41–50 | 3.08 | 2.84–3.32 | 0.121 | 3.00 | 1.851 |
| 51–60 | 3.01 | 2.77–3.25 | 0.123 | 3.00 | 1.829 |
| >60 | 2.87 | 2.40–3.34 | 0.235 | 2.00 | 1.939 |
| Type of hospital |
| Adult hospital | 2.95 | 2.77–3.13 | 0.091 | 3.00 | 1.869 | 12.990 | 6 | 0.043 |
| Pediatric hospital | 2.62 | 2.48–2.76 | 0.073 | 2.00 | 1.673 |
| Profession |
| Physicians | 1.98 | 1.84–2.13 | 0.074 | 1.00 | 1.294 | 102.456 | 12 | <0.001 |
| Nurses | 3.10 | 2.93–3.27 | 0.086 | 3.00 | 1.840 |
| Others | 3.25 | 2.98–3.52 | 0.135 | 3.00 | 1.849 |
| Seniority |
| <5 y. | 2.31 | 2.11–2.50 | 0.099 | 2.00 | 1.542 | 33.377 | 18 | 0.015 |
| 6–20 y. | 2.84 | 2.59–3.09 | 0.126 | 3.00 | 1.855 |
| >20 y. | 3.00 | 2.82–3.19 | 0.093 | 3.00 | 1.842 |
| Refuse to answer | 2.84 | 2.52–3.16 | 0.162 | 3.00 | 1.614 |
Table 8.
Taking preparations with inosine to prevent influenza virus infection by sociodemographic category (N = 950).
Table 8.
Taking preparations with inosine to prevent influenza virus infection by sociodemographic category (N = 950).
| Variables | Mean | 95% CI | SE | MD | OR | χ2 | df | p-Value |
|---|
| Gender |
| Female | 2.64 | 2.53–2.75 | 0.056 | 2.00 | 1.592 | 7.795 | 6 | 0.254 |
| Male | 2.45 | 2.17–2.73 | 0.142 | 2.00 | 1.702 |
| Age |
| 18–30 | 2.30 | 2.11–2.49 | 0.097 | 2.00 | 1.444 | 57.539 | 24 | <0.001 |
| 31–40 | 2.43 | 2.21–2.64 | 0.110 | 2.00 | 1.578 |
| 41–50 | 2.86 | 2.66–3.07 | 0.105 | 3.00 | 1.599 |
| 51–60 | 2.80 | 2.58–3.02 | 0.112 | 2.00 | 1.659 |
| >60 | 2.65 | 2.19–3.10 | 0.228 | 2.00 | 1.883 |
| Type of hospital |
| Adult hospital | 2.80 | 2.64–2.96 | 0.082 | 3.00 | 1.675 | 13.356 | 6 | 0.038 |
| Pediatric hospital | 2.46 | 2.32–2.59 | 0.067 | 2.00 | 1.541 |
| Profession |
| Physicians | 1.88 | 1.74–2.01 | 0.067 | 1.00 | 1.175 | 112.718 | 12 | <0.001 |
| Nurses | 2.87 | 2.72–3.03 | 0.078 | 3.00 | 1.665 |
| Others | 3.15 | 2.91–3.40 | 0.122 | 3.00 | 1.675 |
| Seniority |
| <5 y. | 2.30 | 2.12–2.48 | 0.092 | 2.00 | 1.433 | 26.390 | 18 | 0.091 |
| 6–20 y. | 2.59 | 2.37–2.82 | 0.114 | 2.00 | 1.681 |
| >20 y. | 2.80 | 2.63–2.97 | 0.085 | 3.00 | 1.673 |
| Refuse to answer | 2.65 | 2.35–2.95 | 0.151 | 2.00 | 1.507 |
Table 9.
Taking vitamin C daily to prevent influenza virus infection by sociodemographic category (N = 950).
Table 9.
Taking vitamin C daily to prevent influenza virus infection by sociodemographic category (N = 950).
| Variables | Mean | 95% CI | SE | MD | OR | χ2 | df | p-Value |
|---|
| Gender |
| Female | 3.19 | 3.06–3.32 | 0.066 | 3.00 | 1.874 | 20.548 | 6 | 0.002 |
| Male | 2.69 | 2.38–3.01 | 0.160 | 2.00 | 1.918 |
| Age |
| 18–30 | 2.60 | 2.38–2.82 | 0.113 | 2.00 | 1.683 | 74.040 | 24 | <0.001 |
| 31–40 | 2.73 | 2.49–2.98 | 0.125 | 2.00 | 1.800 |
| 41–50 | 3.56 | 3.32–3.79 | 0.110 | 4.00 | 1.825 |
| 51–60 | 3.49 | 3.24–3.75 | 0.131 | 3.00 | 1.914 |
| >60 | 3.22 | 2.69–3.75 | 0.267 | 2.50 | 2.198 |
| Type of hospital |
| Adult hospital | 3.41 | 3.22–3.59 | 0.093 | 3.00 | 1.920 | 22.345 | 6 | 0.001 |
| Pediatric hospital | 2.89 | 2.73–3.04 | 0.080 | 3.00 | 1.831 |
| Profession |
| Physicians | 1.93 | 1.79–2.07 | 0.072 | 1.00 | 1.254 | 205.275 | 12 | <0.001 |
| Nurses | 3.59 | 3.42–3.77 | 0.089 | 3.50 | 1.892 |
| Others | 3.89 | 3.62–4.15 | 0.134 | 4.00 | 1.834 |
| Seniority |
| <5 y. | 2.55 | 2.35–2.76 | 0.104 | 2.00 | 1.628 | 62.446 | 18 | <0.001 |
| 6–20 y. | 3.00 | 2.74–3.26 | 0.134 | 3.00 | 1.967 |
| >20 y. | 3.43 | 3.24–3.63 | 0.098 | 3.00 | 1.926 |
| Refuse to answer | 3.53 | 3.16–3.89 | 0.182 | 3.00 | 1.815 |