Knowledge and Attitudes of Healthcare Professionals Regarding Perinatal Influenza Vaccination during the COVID-19 Pandemic
Abstract
1. Introduction
2. Materials and Methods
3. Results
Association between Responders’ Characteristics and Knowledge about the Flu Vaccine
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Petersen, E.; Koopmans, M.; Go, U.; Hamer, D.H.; Petrosillo, N.; Castelli, F.; Storgaard, M.; Al Khalili, S.; Simonsen, L. Comparing SARS-CoV-2 with SARS-CoV and influenza pandemics. Lancet Infect. Dis. 2020, 20, e238–e244. [Google Scholar] [CrossRef] [PubMed]
- Girard, M.P.; Tam, J.S.; Assossou, O.M.; Kieny, M.P. The 2009A (H1N1) influenza virus pandemic: A review. Vaccine 2010, 28, 4895–4902. [Google Scholar] [CrossRef] [PubMed]
- Neumann, G.; Noda, T.; Kawaoka, Y. Emergence and pandemic potential of swine-origin H1N1 influenza virus. Nature 2009, 459, 931–939. [Google Scholar] [CrossRef] [PubMed]
- Loeb, M.; Singh, P.K.; Fox, J.; Russell, M.L.; Pabbaraju, K.; Zarra, D.; Wong, S.; Neupane, B.; Webby, R.; Fonseca, K. Longitudinal study of influenza molecular viral shedding in Hutterite communities. J. Infect. Dis. 2012, 206, 1078–1084. [Google Scholar] [CrossRef] [PubMed]
- Nunes, M.C.; Cutland, C.; Jones, S.; Hugo, A.; Madimabe, R.; Simões, E.A.F.; Weinberg, A.; Madhi, S.A. Duration of infant protection against influenza illness conferred by maternal immunization: Secondary Analysis of a Randomized Clinical Trial. JAMA Pediatr. 2016, 170, 840–847. [Google Scholar] [CrossRef] [PubMed]
- Gaunt, G.; Ramin, K. Immunological tolerance of the human fetus. Am. J. Perinatol. 2001, 18, 299–312. [Google Scholar] [CrossRef] [PubMed]
- Mertz, D.; Geraci, J.; Winkup, J.; Gessner, B.D.; Ortiz, J.R.; Loeb, M. Pregnancy as a risk factor for severe outcomes from influenza virus infection: A systematic review and meta-analysis of observational studies. Vaccine 2017, 35, 521–528. [Google Scholar] [CrossRef] [PubMed]
- Jamieson, D.J.; Honein, M.A.; Rasmussen, S.A.; Williams, J.L.; Swerdlow, D.L.; Biggerstaff, M.S.; Lindstrom, S.; Louie, J.K.; Christ, C.M.; Bohm, S.R.; et al. H1N1 2009 influenza virus infection during pregnancy in the USA. Lancet 2009, 374, 451–458. [Google Scholar] [CrossRef]
- Knight, M.; Bunch, K.; Vousden, N.; Morris, E.; Simpson, N.; Gale, C.; O’Brien, P.; Quigley, M.; Brocklehurst, P.; Kurinczuk, J.J. Characteristics and outcomes of pregnant women admitted to hospital with confirmed SARS-CoV-2 infection in UK: National population-based cohort study. BMJ 2020, 369, m2107. [Google Scholar] [CrossRef]
- Mertz, D.; Kim, T.H.; Johnstone, J.; Lam, P.P.; Science, M.; Kuster, S.P.; Fadel, S.A.; Tran, D.; Fernandez, E.; Bhatnagar, N.; et al. Populations at risk for severe or complicated influenza illness: Systematic review and meta-analysis. BMJ 2013, 347, f5061. [Google Scholar] [CrossRef]
- Fell, D.; Savitz, D.; Kramer, M.; Gessner, B.; Katz, M.; Knight, M.; Luteijn, J.; Marshall, H.; Bhat, N.; Gravett, M.; et al. Maternal influenza and birth outcomes: Systematic review of comparative studies. BJOG Int. J. Obstet. Gynaecol. 2017, 124, 48–59. [Google Scholar] [CrossRef]
- Song, J.Y.; Park, K.V.; Han, S.W.; Choi, M.J.; Noh, J.Y.; Cheong, H.J.; Kim, W.J.; Oh, M.-J.; Cho, G.J. Paradoxical long-term impact of maternal influenza infection on neonates and infants. BMC Infect. Dis. 2020, 20, 502. [Google Scholar] [CrossRef]
- Moretti, M.E.; Bar-Oz, B.; Fried, S.K.G. Maternal hyperthermia and the risk for neural tube defects in offspring: Systematic review and meta-analysis. Epidemiology 2005, 16, 216–219. [Google Scholar] [CrossRef]
- Center of Disease Control and Prevention (CDC). Key Facts about Seasonal Flu Vaccine. 2020. Available online: https://www.cdc.gov/flu/prevent/keyfacts.htm (accessed on 16 December 2020).
- Fell, D.B.; Platt, R.; Lanes, A.; Wilson, K.; Kaufman, J.; Basso, O.; Buckeridge, D. Fetal death and preterm birth associated with maternal influenza vaccination: Systematic review. BJOG Int. J. Obstet. Gynaecol. 2015, 122, 17–26. [Google Scholar] [CrossRef]
- Fell, D.B.; Sprague, A.E.; Liu, N.; Yasseen, A.S.; Wen, S.-W.; Smith, G.; Walker, M.C. H1N1 influenza vaccination during pregnancy and fetal and neonatal outcomes. Am. J. Public Health 2012, 102, e33–e40. [Google Scholar] [CrossRef]
- McMillan, M.; Porritt, K.; Kralik, D.; Costi, L.; Marshall, H. Influenza vaccination during pregnancy: A systematic review of fetal death, spontaneous abortion, and congenital malformation safety outcomes. Vaccine 2015, 33, 2108–2117. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. National Center for Immunization and Respiratory Diseases (NCIRD). Available online: https://www.cdc.gov/ncird/index.html (accessed on 30 October 2022).
- Yuen, C.Y.; Tarrant, M. A comprehensive review of influenza and influenza vaccination during pregnancy. J. Perinat. Neonatal Nurs. 2014, 28, 261–270. [Google Scholar] [CrossRef]
- Adeyanju, G.C.; Engel, E.; Koch, L.; Ranzinger, T.; Shahid, I.B.M.; Head, M.G.; Eitze, S.; Betsch, C. Determinants of influenza vaccine hesitancy among pregnant women in Europe: A systematic review. Eur. J. Med. Res. 2021, 26, 116. [Google Scholar] [CrossRef]
- Loubet, P.; Nguyen, C.; Burnet, E.; Launay, O. Influenza vaccination of pregnant women in Paris, France: Knowledge, attitudes and practices among midwives. PLoS ONE 2019, 14, e0215251. [Google Scholar] [CrossRef]
- Ugezu, C.; Essajee, M. Exploring patients’ awareness and healthcare professionals’ knowledge and attitude to pertussis and influenza vaccination during the antenatal periods in Cavan Monaghan general hospital. Hum. Vaccines Immunother. 2018, 14, 978–983. [Google Scholar] [CrossRef]
- Lu, A.B.; Halim, A.A.; Dendle, C.; Kotsanas, D.; Giles, M.L.; Wallace, E.M.; Buttery, J.P.; Stuart, R.L. Influenza vaccination uptake among pregnant women and maternal care providers is suboptimal. Vaccine 2012, 30, 4055–4059. [Google Scholar] [CrossRef] [PubMed]
- Influenza and Seasonal Influenza. Available online: https://eody.gov.gr/wp-content/uploads/2020/10/antigripikos-emvoliasmos-prosopikou-2020-2021-1.pdf (accessed on 20 March 2020).
- Vishram, B.; Letley, L.; Van Hoek, A.J.; Silverton, L.; Donovan, H.; Adams, C.; Green, D.; Edwards, A.; Yarwood, J.; Bedford, H.; et al. Vaccination in pregnancy: Attitudes of nurses, midwives and health visitors in England. Hum. Vaccines Immunother. 2018, 14, 179–188. [Google Scholar] [CrossRef] [PubMed]
- Ahluwalia, I.B.; Jamieson, D.J.; Rasmussen, S.A.; D’Angelo, D.; Goodman, D.; Kim, H. Correlates of seasonal influenza vaccine coverage among pregnant women in Georgia and Rhode Island. Obstet. Gynecol. 2010, 116, 949–955. [Google Scholar] [CrossRef] [PubMed]
- Shavell, V.I.; Moniz, M.H.; Gonik, B.; Beigi, R.H. Influenza immunization in pregnancy: Overcoming patient and health care provider barriers. Am. J. Obstet. Gynecol. 2012, 207, S67–S74. [Google Scholar] [CrossRef]
- Sarantaki, A.; Kalogeropoulou, V.E.; Taskou, C.; Nanou, C.; Lykeridou, A. COVID-19 Vaccination and Related Determinants of Hesitancy among Pregnant Women: A Systematic Review and Meta-Analysis. Vaccines 2022, 10, 2055. [Google Scholar] [CrossRef]


| Variable | Mean | Standard Deviation |
|---|---|---|
| Age (years) | 38.96 | 9.56 |
| Years of service | 8.48 | 11.45 |
| Number of conferences/seminars/workshops attended per year | 3.96 | 4.59 |
| Gender | N | % |
| Female | 212 | 88.3 |
| Male | 28 | 11.7 |
| Marital status | ||
| Single | 99 | 41.2 |
| Married | 132 | 55 |
| Other | 9 | 3.8 |
| Number of children | ||
| 0 | 109 | 45.4 |
| 1 | 45 | 18.8 |
| 2 | 71 | 29.6 |
| 3 | 12 | 5 |
| 4 | 3 | 1.3 |
| Age of older child | ||
| 0–6 months | 8 | 3.3 |
| 6 months–2 years | 15 | 6.3 |
| 2 years–10 years | 47 | 19.6 |
| >10 years | 54 | 22.5 |
| Profession/specialty | ||
| Midwife | 191 | 79.6 |
| Gynecologist–Obstetrician | 27 | 11.3 |
| Pediatrician | 22 | 9.2 |
| Section of work | ||
| Public hospital | 130 | 54.2 |
| Private clinic | 80 | 33.3 |
| Private practice | 30 | 12.5 |
| Educational level | ||
| Bachelor | 138 | 57.5 |
| Master | 91 | 37.9 |
| Doctorate | 11 | 4.6 |
| Use of the Internet as a means of information and additional medical knowledge | ||
| No | 29 | 12.1 |
| Yes | 211 | 87.9 |
| Attendance of conferences/seminars/workshops per year | ||
| No | 23 | 9.6 |
| Yes | 217 | 90.4 |
| Question | ||
|---|---|---|
| What is influenza, and how is it caused? (Multiple responses are allowed) | N | % |
| Viral contagious infection affecting the respiratory system | 228 | 95 |
| Caused by RNA viruses | 88 | 36.7 |
| The types of the virus are A, B, C, D | 17 | 7.1 |
| The types that cause the disease are A, B and C | 62 | 25.8 |
| I don’t know | 4 | 1.7 |
| Is the flu more serious than a “common cold”? | ||
| Yes | 221 | 92.1 |
| No | 15 | 6.3 |
| I don’t know | 4 | 1.7 |
| Have you received any information from competent bodies on issues related to the flu? | ||
| No | 170 | 70.8 |
| Yes | 70 | 29.2 |
| Which of the following is the official crisis response plan for influenza? | ||
| PERSEUS | 17 | 7.1 |
| SOSTRATOS | 2 | 0.8 |
| ARTEMIS | 33 | 13.8 |
| ATHENA | 2 | 0.8 |
| I don’t know | 186 | 77.5 |
| What are the ways of transmission of the flu?(Multiple responses are allowed) | ||
| Cough | 235 | 97.9 |
| Sneezing | 232 | 96.7 |
| Through the hands | 202 | 84.2 |
| Blood | 16 | 6.7 |
| Body fluids | 41 | 17.1 |
| Do you think the chance of flu transmission is higher in the hospital? | ||
| Yes | 156 | 65 |
| No | 75 | 31.3 |
| I don’t know | 9 | 3.8 |
| Do you think the flu is more likely to be spread in crowded places? | ||
| Yes | 239 | 99.6 |
| No | 1 | 0.4 |
| Are healthcare professionals less vulnerable to influenza infections than other people? | ||
| Yes | 29 | 12.1 |
| No | 207 | 86.3 |
| I don’t know | 4 | 1.7 |
| Can healthcare professionals spread the flu even when they feel well but are sick? | ||
| Yes | 230 | 95.8 |
| No | 5 | 2.1 |
| I don’t know | 5 | 2.1 |
| Can people who are sick with the flu virus spread it only after they develop symptoms? | ||
| Yes | 37 | 15.4 |
| No | 199 | 82.9 |
| I don’t know | 4 | 1.7 |
| For how many days can a person who has the flu transmit it?(Multiple responses are allowed) | ||
| One day before the onset up to 5–7 days after the onset of symptoms? | 170 | 70.8 |
| From the moment symptoms appear up to 5–7 days | 61 | 25.4 |
| Children and severely immunosuppressed patients may transmit for more than a week | 66 | 27.5 |
| I don’t know | 13 | 5.4 |
| Do you know what are the necessary measures to take in order not to transmit the flu virus?(Multiple responses are allowed) | ||
| Use a tissue when coughing/sneezing | 207 | 86.3 |
| Regular hand washing using antiseptic | 220 | 91.7 |
| Washing hands after contact with patients | 233 | 97.1 |
| Washing with soap and hot water at the highest possible temperature, objects (utensils, sheets, towels, etc.) used by a patient with the flu in order to reuse them | 155 | 64.6 |
| Washing objects (dishes, sheets, towels, etc.) with antiseptic substances | 113 | 47.1 |
| Use of mask | 220 | 91.7 |
| Use of gloves | 173 | 72.1 |
| Use of protective glasses | 0 | 0 |
| Use of disposable blouse/apron | 127 | 52.9 |
| Disinfection of multi-use materials (sphygmomanometer, etc.) | 171 | 71.3 |
| Isolation of patients with influenza who require hospitalization, co-hospitalization of these patients (cohorting) | 172 | 71.7 |
| Avoiding unnecessary movement of patients in public places | 195 | 81.3 |
| In case of necessary transport of a patient, use of a mask also by him | 189 | 78.8 |
| Avoiding patient visits | 0 | 0 |
| I don’t know | 0 | 0 |
| Question | ||
|---|---|---|
| Do you know there is a vaccine for the flu? | N | % |
| Yes | 240 | 100 |
| No | 0 | 0 |
| Have you been informed about the flu vaccine? | ||
| Yes | 220 | 91.7 |
| No | 20 | 7.6 |
| If so, how did you learn about the flu vaccine? (Multiple responses are allowed) | ||
| Hellenic National Public Health Organization instructions | 61 | 25.4 |
| Hospital training program | 74 | 30.8 |
| Leaflet or posters | 35 | 14.6 |
| Seminars—Speeches | 49 | 20.4 |
| Media | 44 | 18.3 |
| Does the flu vaccine contain live viruses that can cause people to get the flu? | ||
| Yes | 58 | 24.2 |
| No | 160 | 66.7 |
| I don’t know | 22 | 9.2 |
| Are you aware of the guidelines of the Hellenic National Public Health Organization regarding flu vaccination? | ||
| Yes | 177 | 73.8 |
| No | 63 | 25.9 |
| Are you up to date on the developments surrounding the flu vaccine? | ||
| Yes | 150 | 62.5 |
| No | 89 | 37.1 |
| Does the Hellenic National Public Health Organization recommend influenza vaccination for healthcare professionals? | ||
| Yes | 233 | 97.1 |
| No | 7 | 2.9 |
| In which population groups is vaccination necessary? (Multiple responses are allowed) | ||
| In people older than 50 years | 154 | 64.2 |
| In adults with a Body Mass Index (BMI) > 40 kg/m2 | 144 | 60 |
| In children, who are over 6 months old and suffer from diabetes, chronic heart and lung diseases | 169 | 70.4 |
| In children taking long-term aspirin (e.g., Kawasaki disease, rheumatoid arthritis, etc.) to reduce the risk of developing Reye’s syndrome after the flu | 134 | 55.8 |
| In pregnant women | 187 | 77.9 |
| In lactating women | 136 | 56.7 |
| To those suffering from chronic diseases | 214 | 89.2 |
| In people who are immunosuppressed | 192 | 80 |
| To people who are in contact with high-risk people | 207 | 86.3 |
| I don’t know | 9 | 3.8 |
| From what age is vaccination allowed for children? | ||
| After the 1st year of life | 94 | 39.2 |
| After 6 months of life | 146 | 60.8 |
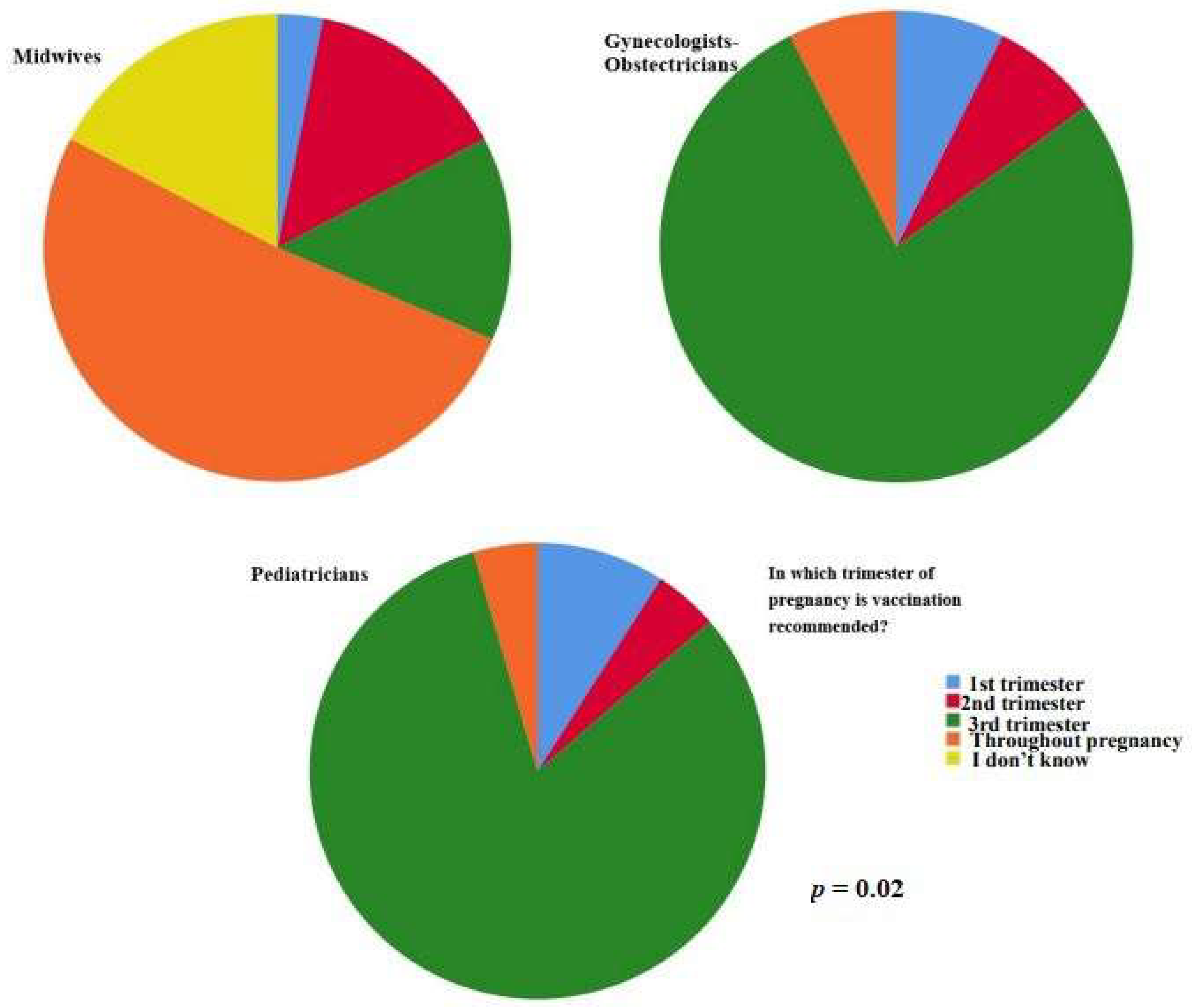
| In which trimester of pregnancy is vaccination recommended? | ||
| 1st trimester | 10 | 4.2 |
| 2nd trimester | 29 | 12.1 |
| 3rd trimester | 28 | 11.7 |
| Throughout pregnancy | 137 | 57.1 |
| I don’t know | 36 | 15 |
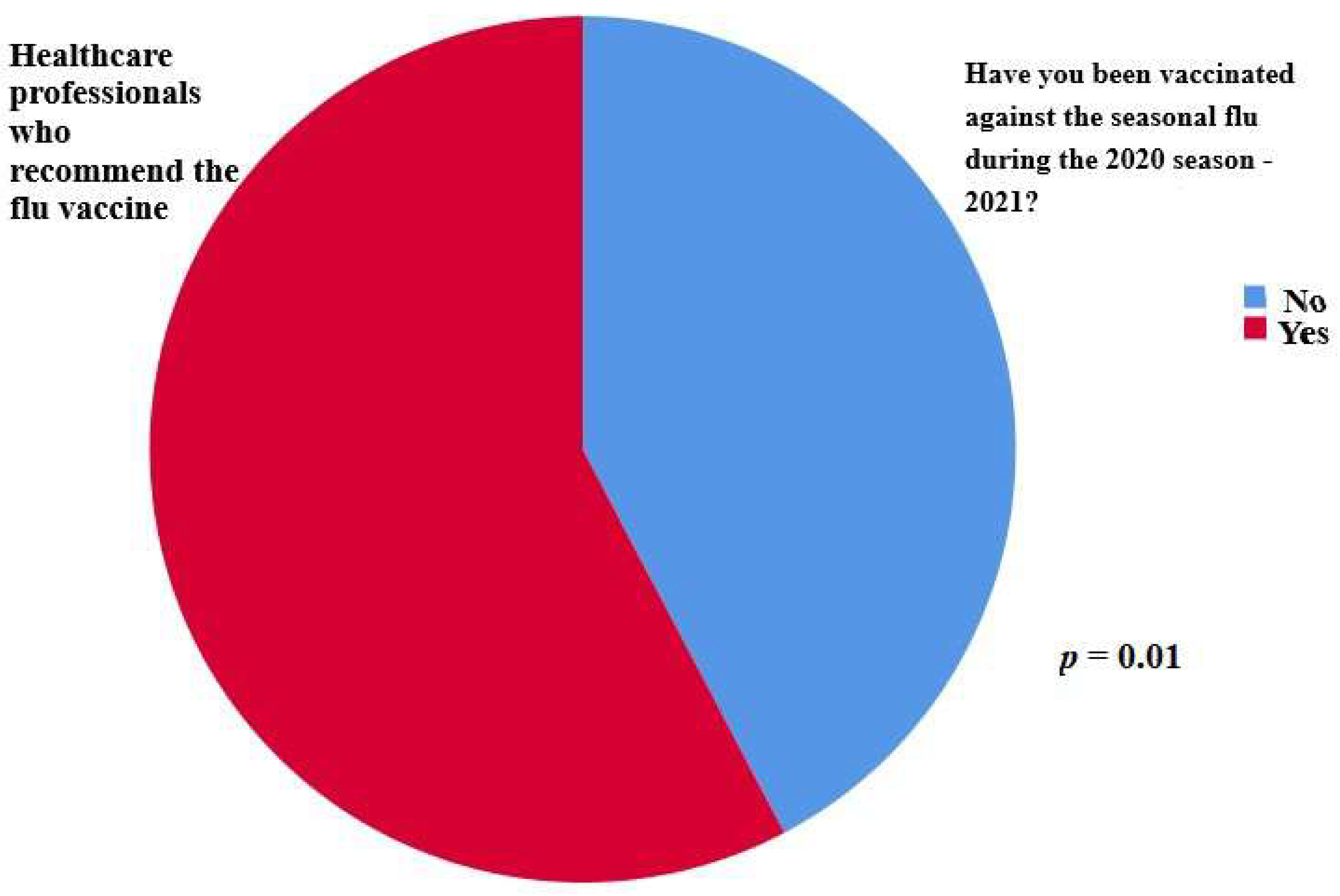
| Have you been vaccinated against the seasonal flu during the 2020–2021 season? | ||
| Yes | 131 | 54.6 |
| No | 107 | 45.4 |
| Reasons for vaccination against the influenza virus (Multiple responses are allowed) | ||
| The flu vaccine is effective | 148 | 61.7 |
| The flu shot is safe | 159 | 66.3 |
| The flu shot is free | 102 | 42.5 |
| Influenza is a serious illness | 102 | 42.5 |
| To protect myself | 172 | 71.7 |
| I suffer from a chronic illness | 81 | 33.8 |
| To protect my family | 189 | 78.8 |
| Encouragement from the workplace | 96 | 40 |
| Desire for immunization due to work | 157 | 65.4 |
| To protect my patients | 173 | 72.1 |
| Reasons for not vaccinating against the influenza virus(Multiple responses are allowed) | ||
| It is not efficient | 46 | 19.2 |
| It is not safe | 49 | 20.4 |
| Worry about side effects | 118 | 49.2 |
| The vaccine causes influenza | 23 | 9.6 |
| The vaccine costs | 24 | 10 |
| Not readily available | 106 | 44.2 |
| Insufficient information about the vaccine | 50 | 20.8 |
| Prevention by others | 52 | 21.7 |
| I forget/don’t have time | 66 | 27.5 |
| It is not necessary for me | 45 | 18.8 |
| Flu is not a serious illness | 23 | 9.6 |
| I have a phobia of needles | 11 | 4.6 |
| I’m worried I’m going to hurt | 39 | 16.3 |
| I am against vaccines in general | 52 | 21.7 |
| I belong to a population group that is not allowed to be vaccinated | 86 | 35.8 |
| Allergy to previous vaccination | 18 | 7.5 |
| Pregnancy | 18 | 7.5 |
| Breastfeeding | 1 | 0.4 |
| Do you think there is sufficient information for health professionals about the use of the flu vaccine? | ||
| Yes | 91 | 37.9 |
| No | 141 | 58.8 |
| I don’t know | 8 | 3.3 |
| Do you think the SARS-CoV-2 pandemic will increase influenza virus recommendation and vaccination rates? | ||
| Yes | 204 | 84 |
| No | 27 | 11.3 |
| I don’t know | 9 | 0.8 |
| Which of the following recommendations do you think would help promote flu vaccination? (Multiple responses are allowed) | ||
| Better inform healthcare professionals about the vaccine and its recommendations | 212 | 88.3 |
| Less workload for healthcare professionals | 54 | 22.5 |
| Greater and easier availability of vaccines | 101 | 42.1 |
| Automatic vaccination reminder system | 151 | 62.9 |
| To be imposed by the state | 37 | 15.4 |
| Vaccine information campaigns in the general population | 120 | 50 |
| I do not agree with the promotion of vaccination | 5 | 2.1 |
| Do you recommend the flu vaccine? | ||
| Yes | 227 | 94.6 |
| No | 13 | 5.4 |
| Occupation/Specialty | Are You Aware of the Guidelines of the Hellenic National Public Health Organization Regarding Flu Vaccination? | Total | p | |
|---|---|---|---|---|
| No | Yes | |||
| Midwife | 54 | 136 | 190 | 0.211 |
| Obstetrician–Gynecologist | 5 | 22 | 27 | |
| Pediatrician | 3 | 19 | 22 | |
| Are you up to date on the developments surrounding the flu vaccine? | Total | p | ||
| No | Yes | |||
| Midwife | 79 | 111 | 190 | 0.016 |
| Obstetrician–Gynecologist | 7 | 20 | 27 | |
| Pediatrician | 3 | 19 | 22 | |
| Does the Hellenic National Public Health Organization recommend influenza vaccination for healthcare professionals? | Total | p | ||
| Yes | No | |||
| Midwife | 184 | 7 | 191 | 0.397 |
| Obstetrician–Gynecologist | 27 | 0 | 27 | |
| Pediatrician | 22 | 0 | 22 | |
| From what age is vaccination allowed for children? | Total | p | ||
| After the first year of life | After the first six months of life | |||
| Midwife | 80 | 111 | 191 | 0.010 |
| Obstetrician–Gynecologist | 12 | 15 | 27 | |
| Pediatrician | 2 | 20 | 22 | |
| In which trimester of pregnancy is vaccination recommended? | Total | p | ||
| Throughout entire pregnancy | Other | |||
| Midwife | 98 | 93 | 191 | 0.020 |
| Obstetrician–Gynecologist | 21 | 6 | 27 | |
| Pediatrician | 18 | 4 | 22 | |
| Have you been vaccinated against the seasonal flu during the 2020–2021 season? | Total | p | ||
| No | Yes | |||
| Midwife | 94 | 97 | 191 | 0.065 |
| Obstetrician–Gynecologist | 8 | 19 | 27 | |
| Pediatrician | 7 | 15 | 22 | |
| Do you recommend the flu vaccine? | Total | p | ||
| No | Yes | |||
| Midwife | 13 | 178 | 191 | 0.172 |
| Obstetrician–Gynecologist | 0 | 27 | 27 | |
| Pediatrician | 0 | 22 | 22 | |
| Is the flu vaccine recommended for the general population? | ||||
| No | Yes | I don’t know | p | |
| Midwife | 46 | 140 | 5 | 0.021 |
| Obstetrician–Gynecologist | 11 | 15 | 1 | |
| Pediatrician | 12 | 10 | 0 | |
| May the flu shot not be effective if the vaccine contains other types of the virus than the ones that are in an outbreak? | ||||
| No | Yes | I don’t know | p | |
| Midwife | 24 | 120 | 47 | 0.126 |
| Obstetrician–Gynecologist | 2 | 21 | 4 | |
| Pediatrician | 2 | 19 | 1 | |
| Section of Work | Are You Aware of the Guidelines of the Hellenic National Public Health Organization Regarding Flu Vaccination? | Total | p | |
|---|---|---|---|---|
| No | Yes | |||
| Public hospital | 40 | 90 | 130 | 0.030 |
| Private clinic | 21 | 59 | 80 | |
| Private practice | 2 | 28 | 30 | |
| Are you up to date on the developments surrounding the flu vaccine? | Total | p | ||
| No | Yes | |||
| Public hospital | 54 | 76 | 130 | 0.298 |
| Private clinic | 28 | 52 | 80 | |
| Private practice | 8 | 22 | 30 | |
| Does the Hellenic National Public Health Organization recommend influenza vaccination for healthcare professionals? | Total | p | ||
| Yes | No | |||
| Public hospital | 126 | 4 | 130 | 0.961 |
| Private clinic | 78 | 2 | 80 | |
| Private practice | 29 | 1 | 30 | |
| From what age is vaccination allowed for children? | Total | p | ||
| After the first year of life | After the first six months of life | |||
| Public hospital | 52 | 78 | 130 | 0.941 |
| Private clinic | 31 | 49 | 80 | |
| Private practice | 11 | 19 | 30 | |
| In which trimester of pregnancy is vaccination recommended? | Total | p | ||
| Throughout entire pregnancy | Other | |||
| Public hospital | 75 | 55 | 130 | 0.030 |
| Private clinic | 39 | 41 | 80 | |
| Private practice | 23 | 7 | 30 | |
| Have you been vaccinated against the seasonal flu during the 2020–2021 season? | Total | p | ||
| No | Yes | |||
| Public hospital | 67 | 63 | 130 | 0.039 |
| Private clinic | 34 | 46 | 80 | |
| Private practice | 8 | 22 | 30 | |
| Do you recommend the flu vaccine? | Total | p | ||
| No | Yes | |||
| Public hospital | 7 | 123 | 130 | 0.834 |
| Private clinic | 5 | 75 | 80 | |
| Private practice | 1 | 29 | 30 | |
| Is the flu vaccine recommended for the general population? | ||||
| No | Yes | I don’t know | p | |
| Public hospital | 34 | 93 | 3 | 0.224 |
| Private clinic | 21 | 57 | 2 | |
| Private practice | 14 | 15 | 1 | |
| May the flu shot not be effective if the vaccine contains other types of the virus than the ones that are in an outbreak? | ||||
| No | Yes | I don’t know | p | |
| Public hospital | 16 | 85 | 29 | 0.484 |
| Private clinic | 11 | 51 | 18 | |
| Private practice | 1 | 24 | 5 | |
| Time of service (years) ± Standard Deviation | Are you aware of the guidelines of the Hellenic National Public Health Organization regarding flu vaccination? | p | ||
| No 10.39 ± 8.5 | Yes 11.70 ± 8.39 | 0.186 | ||
| Are you up to date on the developments surrounding the flu vaccine? | p | |||
| No | Yes | 0.077 | ||
| 10.23 ± 8.12 | 12.05 ± 8.54 | |||
| Does the Hellenic National Public Health Organization recommend influenza vaccination for healthcare professionals? | p | |||
| Yes | No | 0.864 | ||
| 11.42 ± 8.47 | 12.28 ± 9.42 | |||
| From what age is vaccination allowed for children? | p | |||
| After the first year of life | After the first six months of life | 0.089 | ||
| 12.56 ± 8.67 | 10.71 ± 8.31 | |||
| In which trimester of pregnancy is vaccination recommended? | p | |||
| Throughout entire pregnancy | Other | 0.906 | ||
| 11.23 ± 7.92 | 11.73 ± 9.22 | |||
| Have you been vaccinated against the seasonal flu during the 2020–2021 season? | p | |||
| No | Yes | 0.125 | ||
| 10.81 ± 8.96 | 11.97 ± 8.06 | |||
| Do you recommend the flu vaccine? | p | |||
| No | Yes | 0.026 | ||
| 6.71 ± 5.79 | 11.73 ± 8.54 | |||
| Is the flu vaccine recommended for the general population? | p | |||
| No | Yes | I don’t know | 0.112 | |
| 10.82 ± 7.68 | 11.92 ± 8.8 | 6.16 ± 7.57 | ||
| May the flu shot not be effective if the vaccine contains other types of the virus than the ones that are in an outbreak? | p | |||
| No | Yes | I don’t know | 0.150 | |
| 8.48 ± 6.62 | 12.04 ± 8.75 | 11.22 ± 8.48 | ||
| Are You Aware of the Guidelines of the Hellenic National Public Health Organization Regarding Flu Vaccination? | p | |||
|---|---|---|---|---|
| Number of attended conferences/seminars/ workshops per year ± Standard Deviation | No 3.84 ± 6.97 | Yes 4.02 ± 3.43 | 0.013 | |
| Are you up to date on the developments surrounding the flu vaccine? | p | |||
| No | Yes | 0.001 | ||
| 3.06 ± 3.39 | 4.5 ± 5.12 | |||
| Does the Hellenic National Public Health Organization recommend influenza vaccination for healthcare professionals? | p | |||
| Yes | No | 0.002 | ||
| 4.05 ± 4.63 | 1 ± 0.81 | |||
| From what age is vaccination allowed for children? | p | |||
| After the first year of life | After the first six months of life | 0.108 | ||
| 3.73 ± 5.55 | 4.1 ± 3.87 | |||
| In which trimester of pregnancy is vaccination recommended? | p | |||
| Throughout entire pregnancy | Other | 0.121 | ||
| 3.96 ± 3.41 | 3.95 ± 5.82 | |||
| Have you been vaccinated against the seasonal flu during the 2020–2021 season? | p | |||
| No | Yes | 0.547 | ||
| 4.1 ± 5.72 | 3.84 ± 3.4 | |||
| Do you recommend the flu vaccine? | p | |||
| No | Yes | 0.013 | ||
| 1.77 ± 1.30 | 4.08 ± 4.68 | |||
| Is the flu vaccine recommended for the general population? | p | |||
| No | Yes | I don’t know | 0.555 | |
| 3.87 ± 3.06 | 4.02 ± 5.15 | 3.17 ± 2.85 | ||
| May the flu shot not be effective if the vaccine contains other types of the virus than the ones that are in an outbreak? | No | Yes | I don’t know | p |
| Number of attended conferences/seminars/ workshops per year ± Standard Deviation | 5.07 ± 4.30 | 4.10 ± 4.99 | 2.92 ± 3.09 | 0.150 |
| Have You Been Informed about the Flu Vaccine? | ||||
|---|---|---|---|---|
| Do you recommend the flu vaccine? | No | Yes | Total | p |
| No | 5 | 8 | 13 | 0.01 |
| Yes | 15 | 212 | 227 | |
| Are you aware of the guidelines of the Hellenic National Public Health Organization regarding flu vaccination? | ||||
| Do you recommend the flu vaccine? | No | Yes | Total | p |
| No | 7 | 6 | 13 | 0.044 |
| Yes | 56 | 171 | 227 | |
| Are you up to date on the developments surrounding the flu vaccine? | ||||
| Do you recommend the flu vaccine? | No | Yes | Total | p |
| No | 8 | 5 | 13 | 0.079 |
| Yes | 82 | 145 | 227 | |
| Have you been vaccinated against the seasonal flu during the 2020–2021 season? | ||||
| Do you recommend the flu vaccine? | No | Yes | Total | p |
| No | 13 | 0 | 13 | 0.01 |
| Yes | 96 | 131 | 227 | |
| Have you been informed about the flu vaccine? | ||||
| Have you been vaccinated against the seasonal flu during the 2020–2021 season? | No | Yes | Total | p |
| No | 15 | 94 | 109 | 0.001 |
| Yes | 5 | 126 | 131 | |
| Are you aware of the guidelines of the Hellenic National Public Health Organization regarding flu vaccination? | ||||
| Have you been vaccinated against the seasonal flu during the 2020–2021 season? | No | Yes | Total | p |
| No | 40 | 69 | 109 | 0.002 |
| Yes | 23 | 108 | 131 | |
| Are you up to date on the developments surrounding the flu vaccine? | ||||
| Have you been vaccinated against the seasonal flu during the 2020–2021 season? | No | Yes | Total | p |
| No | 51 | 58 | 109 | 0.011 |
| Yes | 39 | 92 | 131 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Taskou, C.; Sarantaki, A.; Beloukas, A.; Georgakopoulou, V.Ε.; Daskalakis, G.; Papalexis, P.; Lykeridou, A. Knowledge and Attitudes of Healthcare Professionals Regarding Perinatal Influenza Vaccination during the COVID-19 Pandemic. Vaccines 2023, 11, 168. https://doi.org/10.3390/vaccines11010168
Taskou C, Sarantaki A, Beloukas A, Georgakopoulou VΕ, Daskalakis G, Papalexis P, Lykeridou A. Knowledge and Attitudes of Healthcare Professionals Regarding Perinatal Influenza Vaccination during the COVID-19 Pandemic. Vaccines. 2023; 11(1):168. https://doi.org/10.3390/vaccines11010168
Chicago/Turabian StyleTaskou, Chrysoula, Antigoni Sarantaki, Apostolos Beloukas, Vasiliki Ε. Georgakopoulou, Georgios Daskalakis, Petros Papalexis, and Aikaterini Lykeridou. 2023. "Knowledge and Attitudes of Healthcare Professionals Regarding Perinatal Influenza Vaccination during the COVID-19 Pandemic" Vaccines 11, no. 1: 168. https://doi.org/10.3390/vaccines11010168
APA StyleTaskou, C., Sarantaki, A., Beloukas, A., Georgakopoulou, V. Ε., Daskalakis, G., Papalexis, P., & Lykeridou, A. (2023). Knowledge and Attitudes of Healthcare Professionals Regarding Perinatal Influenza Vaccination during the COVID-19 Pandemic. Vaccines, 11(1), 168. https://doi.org/10.3390/vaccines11010168











