Intranasal Treatment of Ferrets with Inert Bacterial Spores Reduces Disease Caused by a Challenging H7N9 Avian Influenza Virus
Abstract
1. Introduction
2. Materials and Methods
2.1. Spore Inoculum
2.2. Virus
2.3. Ferret Study
2.4. Assessment of Clinical Scores
2.5. Sampling and Analysis
2.6. Serology
2.7. RT-qPCR Analysis
3. Results
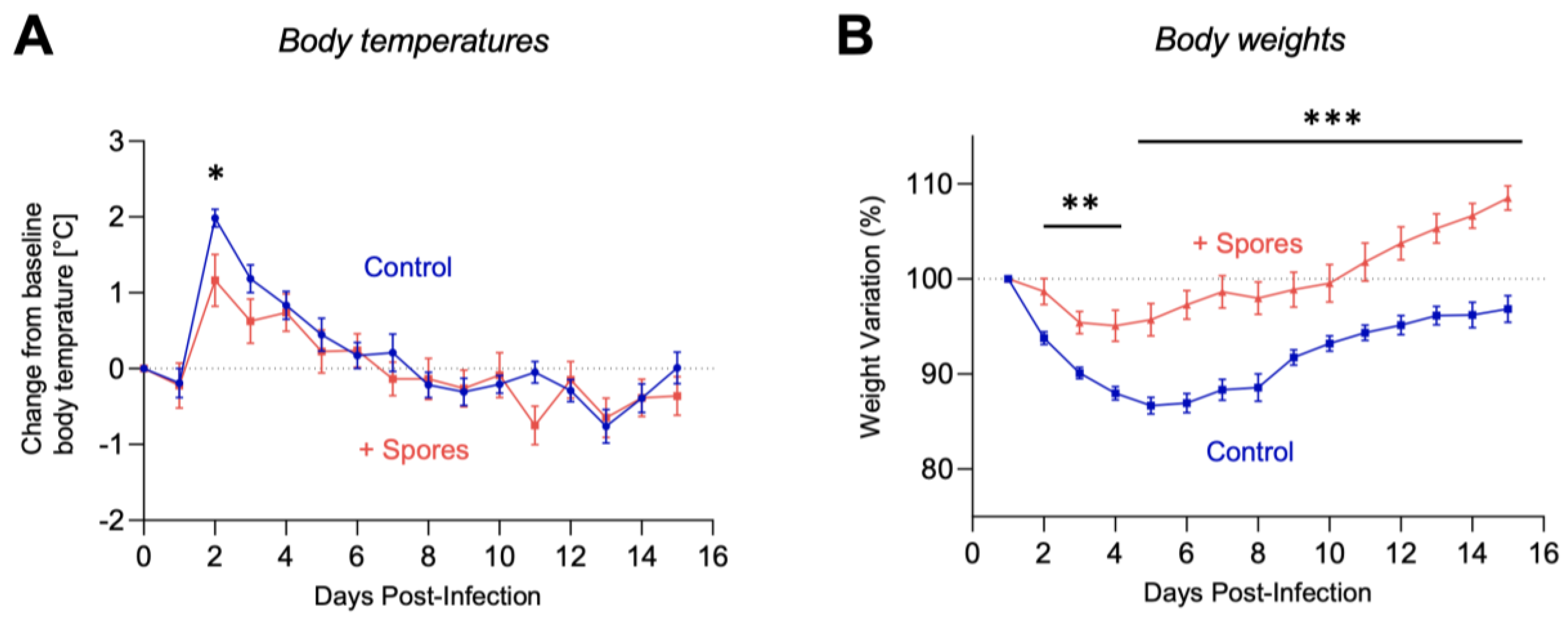
3.1. Symptomatic Protection to H7N9 AIV Infection
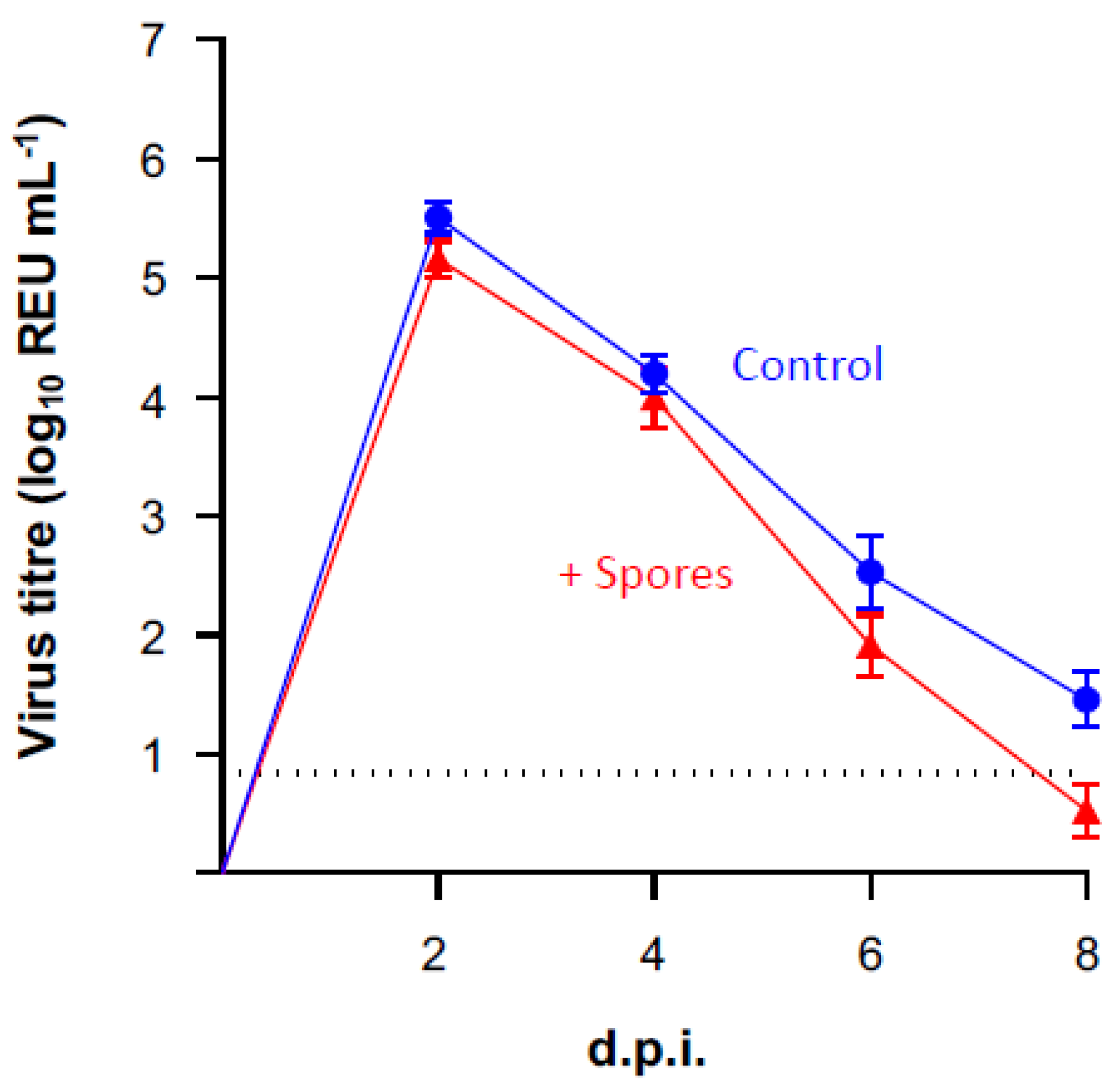
3.2. Protection against Viral Shedding
3.3. Effect of DSM 32444K on Seroconversion to Influenza A Virus
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Permpoonpattana, P.; Hong, H.A.; Phetcharaburanin, J.; Huang, J.M.; Cook, J.; Fairweather, N.F.; Cutting, S.M. Immunization with Bacillus spores expressing toxin A peptide repeats protects against infection with Clostridium difficile strains producing toxins A and B. Infect. Immun. 2011, 79, 2295–2302. [Google Scholar] [CrossRef] [PubMed]
- Reljic, R.; Sibley, L.; Huang, J.M.; Pepponi, I.; Hoppe, A.; Hong, H.A.; Cutting, S.M. Mucosal vaccination against tuberculosis using inert bioparticles. Infect. Immun. 2013, 81, 4071–4080. [Google Scholar] [CrossRef]
- Song, M.; Hong, H.A.; Huang, J.M.; Colenutt, C.; Khang, D.D.; Nguyen, T.V.; Park, S.M.; Shim, B.S.; Song, H.H.; Cheon, I.S.; et al. Killed Bacillus subtilis spores as a mucosal adjuvant for an H5N1 vaccine. Vaccine 2012, 30, 3266–3277. [Google Scholar] [CrossRef] [PubMed]
- de Souza, R.D.; Batista, M.T.; Luiz, W.B.; Cavalcante, R.C.; Amorim, J.H.; Bizerra, R.S.; Martins, E.G.; Ferreira, L.C. Bacillus subtilis spores as vaccine adjuvants: Further insights into the mechanisms of action. PLoS ONE 2014, 9, e87454. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.M.; La Ragione, R.M.; Nunez, A.; Cutting, S.M. Immunostimulatory activity of Bacillus spores. FEMS Immunol. Med. Microbiol. 2008, 53, 195–203. [Google Scholar] [CrossRef]
- Wang, X.; Hu, W.; Zhu, L.; Yang, Q. Bacillus subtilis and surfactin inhibit the transmissible gastroenteritis virus from entering the intestinal epithelial cells. Biosci. Rep. 2017, 37, BSR20170082. [Google Scholar] [CrossRef] [PubMed]
- Barnes, A.G.; Cerovic, V.; Hobson, P.S.; Klavinskis, L.S. Bacillus subtilis spores: A novel microparticle adjuvant which can instruct a balanced Th1 and Th2 immune response to specific antigen. Eur. J. Immunol. 2007, 37, 1538–1547. [Google Scholar] [CrossRef]
- Iuliano, A.D.; Roguski, K.M.; Chang, H.H.; Muscatello, D.J.; Palekar, R.; Tempia, S.; Cohen, C.; Gran, J.M.; Schanzer, D.; Cowling, B.J.; et al. Estimates of global seasonal influenza-associated respiratory mortality: A modelling study. Lancet 2018, 391, 1285–1300. [Google Scholar] [CrossRef]
- WHO. Influenza (Seasonal) Fact Sheet; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Mostafa, A.; Abdelwhab, E.M.; Mettenleiter, T.C.; Pleschka, S. Zoonotic Potential of Influenza A Viruses: A Comprehensive Overview. Viruses 2018, 10, 497. [Google Scholar] [CrossRef]
- Belser, J.A.; Katz, J.M.; Tumpey, T.M. The ferret as a model organism to study influenza A virus infection. Dis. Model. Mech. 2011, 4, 575–579. [Google Scholar] [CrossRef]
- Maassab, H.F.; Kendal, A.P.; Abrams, G.D.; Monto, A.S. Evaluation of a cold-recombinant influenza virus vaccine in ferrets. J. Infect. Dis. 1982, 146, 780–790. [Google Scholar] [CrossRef]
- Fan, S.; Gu, C.; Kong, H.; Guan, L.; Neumann, G.; Kawaoka, Y. Influenza Viruses Suitable for Studies in Syrian Hamsters. Viruses 2022, 14, 1629. [Google Scholar] [CrossRef] [PubMed]
- Lowen, A.C.; Mubareka, S.; Tumpey, T.M.; Garcia-Sastre, A.; Palese, P. The guinea pig as a transmission model for human influenza viruses. Proc. Natl. Acad. Sci. USA 2006, 103, 9988–9992. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Zhou, L.; Zhou, M.; Chen, Z.; Li, F.; Wu, H.; Xiang, N.; Chen, E.; Tang, F.; Wang, D.; et al. Epidemiology of human infections with avian influenza A(H7N9) virus in China. N. Engl. J. Med. 2014, 370, 520–532. [Google Scholar] [CrossRef]
- Huesca-Espitia, L.C.; Suvira, M.; Rosenbeck, K.; Korza, G.; Setlow, B.; Li, W.; Wang, S.; Li, Y.Q.; Setlow, P. Effects of steam autoclave treatment on Geobacillus stearothermophilus spores. J. Appl. Microbiol. 2016, 121, 1300–1311. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, V.A.; Huynh, H.A.; Hoang, T.V.; Ninh, N.T.; Pham, A.T.; Nguyen, H.A.; Phan, T.N.; Cutting, S.M. Killed Bacillus subtilis spores expressing streptavidin: A novel carrier of drugs to target cancer cells. J. Drug Target. 2013, 21, 528–541. [Google Scholar] [CrossRef] [PubMed]
- Bhat, S.; James, J.; Sadeyen, J.R.; Mahmood, S.; Everest, H.J.; Chang, P.; Walsh, S.K.; Byrne, A.M.P.; Mollett, B.; Lean, F.; et al. Coinfection of Chickens with H9N2 and H7N9 Avian Influenza Viruses Leads to Emergence of Reassortant H9N9 Virus with Increased Fitness for Poultry and a Zoonotic Potential. J. Virol. 2022, 96, e0185621. [Google Scholar] [CrossRef] [PubMed]
- de Jonge, J.; Isakova-Sivak, I.; van Dijken, H.; Spijkers, S.; Mouthaan, J.; de Jong, R.; Smolonogina, T.; Roholl, P.; Rudenko, L. H7N9 Live Attenuated Influenza Vaccine Is Highly Immunogenic, Prevents Virus Replication, and Protects Against Severe Bronchopneumonia in Ferrets. Mol. Ther. 2016, 24, 991–1002. [Google Scholar] [CrossRef]
- Jonges, M.; Liu, W.M.; van der Vries, E.; Jacobi, R.; Pronk, I.; Boog, C.; Koopmans, M.; Meijer, A.; Soethout, E. Influenza virus inactivation for studies of antigenicity and phenotypic neuraminidase inhibitor resistance profiling. J. Clin. Microbiol. 2010, 48, 928–940. [Google Scholar] [CrossRef]
- Nagy, A.; Cernikova, L.; Kunteova, K.; Dirbakova, Z.; Thomas, S.S.; Slomka, M.J.; Dan, A.; Varga, T.; Mate, M.; Jirincova, H.; et al. A universal RT-qPCR assay for "One Health" detection of influenza A viruses. PLoS ONE 2021, 16, e0244669. [Google Scholar] [CrossRef]
- Iwasaki, A.; Pillai, P.S. Innate immunity to influenza virus infection. Nat. Rev. Immunol. 2014, 14, 315–328. [Google Scholar] [CrossRef] [PubMed]
- Schmitz, N.; Beerli, R.R.; Bauer, M.; Jegerlehner, A.; Dietmeier, K.; Maudrich, M.; Pumpens, P.; Saudan, P.; Bachmann, M.F. Universal vaccine against influenza virus: Linking TLR signaling to anti-viral protection. Eur. J. Immunol. 2012, 42, 863–869. [Google Scholar] [CrossRef]
- Jiang, T.; Zhao, H.; Li, X.F.; Deng, Y.Q.; Liu, J.; Xu, L.J.; Han, J.F.; Cao, R.Y.; Qin, E.D.; Qin, C.F. CpG oligodeoxynucleotides protect against the 2009 H1N1 pandemic influenza virus infection in a murine model. Antivir. Res. 2011, 89, 124–126. [Google Scholar] [CrossRef] [PubMed]
- Abdul-Careem, M.F.; Firoz Mian, M.; Gillgrass, A.E.; Chenoweth, M.J.; Barra, N.G.; Chan, T.; Al-Garawi, A.A.; Chew, M.V.; Yue, G.; van Roojen, N.; et al. FimH, a TLR4 ligand, induces innate antiviral responses in the lung leading to protection against lethal influenza infection in mice. Antivir. Res. 2011, 92, 346–355. [Google Scholar] [CrossRef] [PubMed]
- Mifsud, E.J.; Tan, A.C.; Jackson, D.C. TLR Agonists as Modulators of the Innate Immune Response and Their Potential as Agents Against Infectious Disease. Front. Immunol. 2014, 5, 79. [Google Scholar] [CrossRef]
- Huang, J.M.; La Ragione, R.M.; Cooley, W.A.; Todryk, S.; Cutting, S.M. Cytoplasmic delivery of antigens, by Bacillus subtilis enhances Th1 responses. Vaccine 2008, 26, 6043–6052. [Google Scholar] [CrossRef] [PubMed]
- Chadwick, S.; Kriegel, C.; Amiji, M. Nanotechnology solutions for mucosal immunization. Adv. Drug Deliv. Rev. 2010, 62, 394–407. [Google Scholar] [CrossRef]
- Maines, T.R.; Belser, J.A.; Gustin, K.M.; van Hoeven, N.; Zeng, H.; Svitek, N.; von Messling, V.; Katz, J.M.; Tumpey, T.M. Local innate immune responses and influenza virus transmission and virulence in ferrets. J. Infect. Dis. 2012, 205, 474–485. [Google Scholar] [CrossRef]
- Skarlupka, A.L.; Ross, T.M. Immune Imprinting in the Influenza Ferret Model. Vaccines 2020, 8, 173. [Google Scholar] [CrossRef]
- Oh, J.E.; Song, E.; Moriyama, M.; Wong, P.; Zhang, S.; Jiang, R.; Strohmeier, S.; Kleinstein, S.H.; Krammer, F.; Iwasaki, A. Intranasal priming induces local lung-resident B cell populations that secrete protective mucosal antiviral IgA. Sci. Immunol. 2021, 6, eabj5129. [Google Scholar] [CrossRef]
- Fiorini, G.; Cimminiello, C.; Chianese, R.; Visconti, G.P.; Cova, D.; Uberti, T.; Gibelli, A. Bacillus subtilis selectively stimulates the synthesis of membrane bound and secreted IgA. Chemioterapia 1985, 4, 310–312. [Google Scholar] [PubMed]
- Ciprandi, G.; Tosca, M.A.; Milanese, M.; Caligo, G.; Ricca, V. Cytokines evaluation in nasal lavage of allergic children after Bacillus clausii administration: A pilot study. Pediatr. Allergy Immunol. 2004, 15, 148–151. [Google Scholar] [CrossRef] [PubMed]
- Elshaghabee, F.M.F.; Rokana, N.; Gulhane, R.D.; Sharma, C.; Panwar, H. Bacillus As Potential Probiotics: Status, Concerns, and Future Perspectives. Front. Microbiol. 2017, 8, 1490. [Google Scholar] [CrossRef] [PubMed]
- Ricci, A.; Allende, A.; Bolton, D.; Chemaly, M.; Davies, R.; Girones, R.; Herman, L.; Koutsoumanis, K.; Lindqvist, R.; Norrung, B.; et al. Scientific Opinion on the update of the list of QPS-recommended biological agents intentionally added to food or feed as notified to EFSA. EFSA J. 2017, 15, e04664. [Google Scholar] [CrossRef]
- Burrows, S.M.; Elbert, W.; Lawrence, M.G.; Poschl, U. Bacteria in the global atmosphere—Part 1: Review and synthesis of literature data for different ecosystems. Atmos. Chem. Phys. 2009, 9, 9263–9280. [Google Scholar] [CrossRef]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
James, J.; Meyer, S.M.; Hong, H.A.; Dang, C.; Linh, H.T.Y.; Ferreira, W.; Katsande, P.M.; Vo, L.; Hynes, D.; Love, W.; et al. Intranasal Treatment of Ferrets with Inert Bacterial Spores Reduces Disease Caused by a Challenging H7N9 Avian Influenza Virus. Vaccines 2022, 10, 1559. https://doi.org/10.3390/vaccines10091559
James J, Meyer SM, Hong HA, Dang C, Linh HTY, Ferreira W, Katsande PM, Vo L, Hynes D, Love W, et al. Intranasal Treatment of Ferrets with Inert Bacterial Spores Reduces Disease Caused by a Challenging H7N9 Avian Influenza Virus. Vaccines. 2022; 10(9):1559. https://doi.org/10.3390/vaccines10091559
Chicago/Turabian StyleJames, Joe, Stephanie M. Meyer, Huynh A. Hong, Chau Dang, Ho T. Y. Linh, William Ferreira, Paidamoyo M. Katsande, Linh Vo, Daniel Hynes, William Love, and et al. 2022. "Intranasal Treatment of Ferrets with Inert Bacterial Spores Reduces Disease Caused by a Challenging H7N9 Avian Influenza Virus" Vaccines 10, no. 9: 1559. https://doi.org/10.3390/vaccines10091559
APA StyleJames, J., Meyer, S. M., Hong, H. A., Dang, C., Linh, H. T. Y., Ferreira, W., Katsande, P. M., Vo, L., Hynes, D., Love, W., Banyard, A. C., & Cutting, S. M. (2022). Intranasal Treatment of Ferrets with Inert Bacterial Spores Reduces Disease Caused by a Challenging H7N9 Avian Influenza Virus. Vaccines, 10(9), 1559. https://doi.org/10.3390/vaccines10091559








