Individual- and Neighborhood-Level Factors of Measles Vaccination Coverage in Niamey, Niger: A Multilevel Analysis
Abstract
:1. Introduction
2. Methods
2.1. Study Area
2.2. Study Design and Data Collection
2.3. Data Analysis
3. Results
3.1. Study Population Characteristics
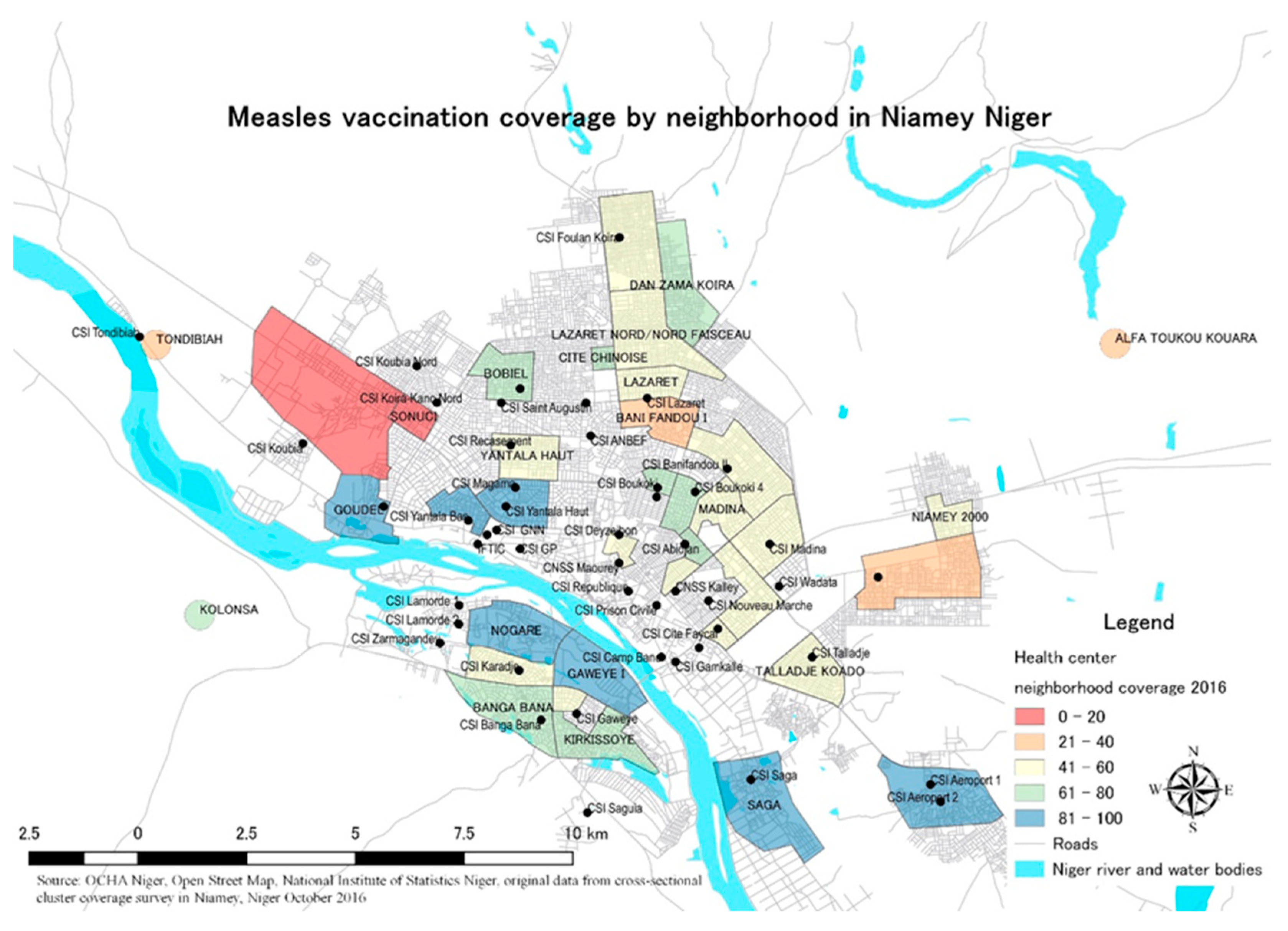
3.2. Map of Measles 1 Vaccination Coverage by Neighborhood
3.3. Multilevel Logistic Regression
4. Discussion
4.1. Individual-Level Factors Associated with Measles 1 Vaccination
4.2. Neighborhood-Level Factors Associated with Measles 1 Vaccination
4.3. Actionable Factors for Measles Vaccination Coverage
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Black, R.E.; Laxminarayan, R.; Temmerman, M.; Walker, N. (Eds.) Reproductive, Maternal, Newborn, and Child Health Disease Control Priorities; The International Bank for Reconstruction and Development/The World Bank: Washington, DC, USA, 2016; Volume 2. [Google Scholar]
- WHO. Explorations of Inequality: Childhood Immunization; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Kazungu, J.S.; Adetifa, I.M.O. Crude childhood vaccination coverage in West Africa: Trends and predictors of completeness. Wellcome Open Res. 2017, 2, 12. [Google Scholar] [CrossRef] [PubMed]
- Russo, G.; Miglietta, A.; Pezzotti, P.; Biguioh, R.M.; Bouting Mayaka, G.; Sobze, M.S.; Stefanelli, P.; Vullo, V.; Rezza, G. Vaccine coverage and determinants of incomplete vaccination in children aged 12–23 months in Dschang, West Region, Cameroon: A cross-sectional survey during a polio outbreak. BMC Public Health 2015, 15, 630. [Google Scholar] [CrossRef] [PubMed]
- Schoeps, A.; Ouédraogo, N.; Kagoné, M.; Sié, A.; Müller, O.; Becher, H. Socio-demographic determinants of timely adherence to BCG, Penta3, measles, and complete vaccination schedule in Burkina Faso. Vaccine 2013, 32, 96–102. [Google Scholar] [CrossRef] [PubMed]
- Kunieda, M.K.; Manzo, M.L.; Shibanuma, A.; Jimba, M. Rapidly modifiable factors associated with full vaccination status among children in Niamey, Niger: A cross-sectional, random cluster household survey. PLoS ONE 2021, 16, e0249026. [Google Scholar] [CrossRef] [PubMed]
- Gage, A.J.; Sommerfelt, A.E.; Piani, A.L. Household structure and childhood immunization in Niger and Nigeria. Demography 1997, 34, 295–309. [Google Scholar] [CrossRef] [PubMed]
- Bangura, J.B.; Xiao, S.; Qiu, D.; Ouyang, F.; Chen, L. Barriers to childhood immunization in sub-Saharan Africa: A systematic review. BMC Public Health 2020, 20, 1108. [Google Scholar] [CrossRef]
- Douba, A.; Aka, L.B.N.; Yao, G.H.A.; Zengbé-Acray, P.; Akani, B.C. Sociodemographic factors associated with incomplete immunization of children aged 12 to 59 months in six West African countries. Sante Publique 2015, 27, 575–584. [Google Scholar] [CrossRef]
- Uthman, O.A.; Sambala, E.Z.; Adamu, A.A.; Ndwandwe, D.; Wiyeh, A.B.; Olukade, T.; Bishwajit, G.; Yaya, S.; Okwo-Bele, J.-M.; Wiysonge, C.S. Does it really matter where you live? A multilevel analysis of factors associated with missed opportunities for vaccination in sub-Saharan Africa. Hum. Vaccines Immunother. 2018, 14, 2397–2404. [Google Scholar] [CrossRef]
- Tesema, G.A.; Tessema, Z.T.; Tamirat, K.S.; Teshale, A.B. Complete basic childhood vaccination and associated factors among children aged 12–23 months in East Africa: A multilevel analysis of recent demographic and health surveys. BMC Public Health 2020, 20, 1837. [Google Scholar] [CrossRef]
- Oyo-Ita, A.; Wiysonge, C.; Oringanje, C.; E Nwachukwu, C.; Oduwole, O.; Meremikwu, M.M. Interventions for improving coverage of childhood immunisation in low- and middle-income countries. Cochrane Database Syst. Rev. 2016, 7, CD008145. [Google Scholar] [CrossRef] [Green Version]
- Banerjee, A.; Chandrasekhar, A.; Dalpath, S.; Duflo, E.; Floretta, J.; Jackson, M.; Kannan, H.; Loza, F.; Sankar, A.; Schrimpf, A.; et al. Selecting the Most Effective Nudge: Evidence from a Large-Scale Experiment on Immunization; In NBER Working Paper Series; National Bureau of Economic Research: Cambridge, MA, USA, 2021. [Google Scholar]
- Shetty, P. Nutrition, Immunity and Infection; CABI: Wallingford, UK, 2010. [Google Scholar]
- Bartlett, S. Water, sanitation and urban children: The need to go beyond “improved” provision. Environ. Urban. 2016, 15, 57–70. [Google Scholar] [CrossRef]
- Alirol, E.; Getaz, L.; Stoll, B.; Chappuis, F.; Loutan, L. Urbanisation and infectious diseases in a globalised world. Lancet Infect. Dis. 2011, 11, 131–141. [Google Scholar] [CrossRef]
- Grais, R.; Ferrari, M.; DuBray, C.; Bjørnstad, O.; Grenfell, B.; Djibo, A.; Fermon, F.; Guerin, P. Estimating transmission intensity for a measles epidemic in Niamey, Niger: Lessons for intervention. Trans. R. Soc. Trop. Med. Hyg. 2006, 100, 867–873. [Google Scholar] [CrossRef] [PubMed]
- Besada, D.; Kerber, K.; Leon, N.; Sanders, D.; Daviaud, E.; Rohde, S.; Rohde, J.; Van Damme, W.; Kinney, M.; Manda, S.; et al. Niger’s Child Survival Success, Contributing Factors and Challenges to Sustainability: A Retrospective Analysis. PLoS ONE 2016, 11, e0146945. [Google Scholar] [CrossRef] [PubMed]
- Cockcroft, A.; Andersson, N.; Omer, K.; Ansari, N.M.; Khan, A.; Chaudhry, U.U.; Ansari, U. One size does not fit all: Local determinants of measles vaccination in four districts of Pakistan. BMC Int. Health Hum. Rights 2009, 9 (Suppl. 1), S4. [Google Scholar] [CrossRef] [PubMed]
- Sissoko, D.; Trottier, H.; Malvy, D.; Johri, M. The Influence of Compositional and Contextual Factors on Non-Receipt of Basic Vaccines among Children of 12–23 Month Old in India: A Multilevel Analysis. PLoS ONE 2014, 9, e106528. [Google Scholar] [CrossRef]
- Halonen, J.I.; Kivimäki, M.; Pentti, J.; Kawachi, I.; Virtanen, M.; Martikainen, P.; Subramanian, S.V.; Vahtera, J. Quantifying Neighbourhood Socioeconomic Effects in Clustering of Behaviour-Related Risk Factors: A Multilevel Analysis. PLoS ONE 2012, 7, e32937. [Google Scholar] [CrossRef] [PubMed]
- Kinfe, Y.; Gebre, H.; Bekele, A. Factors associated with full immunization of children 12–23 months of age in Ethiopia: A multilevel analysis using 2016 Ethiopia Demographic and Health Survey. PLoS ONE 2019, 14, e0225639. [Google Scholar] [CrossRef]
- Antai, D. Migration and child immunization in Nigeria: Individual- and community-level contexts. BMC Public Health 2010, 10, 116. [Google Scholar] [CrossRef]
- Antai, D. Inequitable childhood immunization uptake in Nigeria: A multilevel analysis of individual and contextual determinants. BMC Infect. Dis. 2009, 9, 181. [Google Scholar] [CrossRef] [Green Version]
- Wiysonge, C.S.; Uthman, O.A.; Ndumbe, P.M.; Hussey, G.D. Individual and Contextual Factors Associated with Low Childhood Immunisation Coverage in Sub-Saharan Africa: A Multilevel Analysis. PLoS ONE 2012, 7, e37905. [Google Scholar] [CrossRef] [PubMed]
- World Bank. Niger Education Statistics. 2020. Available online: https://data.worldbank.org/country/niger (accessed on 6 September 2022).
- WHO; UNICEF. Measles vaccination coverage (for Niger by year). Available online: https://immunizationdata.who.int/pages/coverage/mcv.html?CODE=NER&ANTIGEN=&YEAR= (accessed on 6 September 2022).
- INS. Présentation des résultats préliminaires du quatrième (4ème) Recensement Général de la Population et de l’Habitat (RGP/H) 2012; Institut National de la Statistique: Niamey, Niger, 2013. [Google Scholar]
- UN Department of Economic and Social Affairs, Statistics Division (Ed.) World Statistics Pocketbook 2016 edition World Statistics Pocketbook Series V; UN: New York, NY, USA, 2016; Volume 40. [Google Scholar]
- Rossi, J.-P.; Dobigny, G. Urban Landscape Structure of a Fast-Growing African City: The Case of Niamey (Niger). Urban Sci. 2019, 3, 63. [Google Scholar] [CrossRef]
- ICF; INS. Enquête Démographique et de Santé et à Indicateurs Multiples du Niger 2012; ICF: Rockville, MD, USA, 2012. [Google Scholar]
- Blanford, J.I.; Kumar, S.; Luo, W.; MacEachren, A.M. It’s a long, long walk: Accessibility to hospitals, maternity and integrated health centers in Niger. Int. J. Health Geogr. 2012, 11, 24. [Google Scholar] [CrossRef] [PubMed]
- Sommet, N.; Morselli, D. Keep Calm and Learn Multilevel Logistic Modeling: A Simplified Three-Step Procedure Using Stata, R, Mplus, and SPSS. Int. Rev. Soc. Psychol. 2017, 30, 203–218. [Google Scholar] [CrossRef]
- Subramanian, S.; Jones, K. Multilevel Statistical Models: Concepts and Applications, 2017–2018 ed.; Harvard School of Public Health and Centre for Multilevel Modelling, University of Bristol: Bristol, UK, 2017; Volume 359. [Google Scholar]
- Austin, P.C.; Merlo, J. Intermediate and advanced topics in multilevel logistic regression analysis. Stat. Med. 2017, 36, 3257–3277. [Google Scholar] [CrossRef]
- Merlo, J.; Chaix, B.; Ohlsson, H.; Beckman, A.; Johnell, K.; Hjerpe, P.; Råstam, L.; Larsen, K. A brief conceptual tutorial of multilevel analysis in social epidemiology: Using measures of clustering in multilevel logistic regression to investigate contextual phenomena. J. Epidemiol. Community Health 2006, 60, 290–297. [Google Scholar] [CrossRef]
- UNESCO. Niger: Participation in Education. 2021. Available online: http://uis.unesco.org/en/country/ne (accessed on 20 February 2021).
- Smith, S.K.; Dixon, A.; Trevena, L.; Nutbeam, D.; McCaffery, K.J. Exploring patient involvement in healthcare decision making across different education and functional health literacy groups. Soc. Sci. Med. 2009, 69, 1805–1812. [Google Scholar] [CrossRef]
- Geremew, T.T.; Gezie, L.D.; Abejie, A.N. Geographical variation and associated factors of childhood measles vaccination in Ethiopia: A spatial and multilevel analysis. BMC Public Health 2019, 19, 1194. [Google Scholar] [CrossRef]
- Byberg, S.; Fisker, A.B.; Rodrigues, A.; Balde, I.; Enemark, U.; Aaby, P.; Benn, C.S.; Griffiths, U.K. Household experience and costs of seeking measles vaccination in rural Guinea-Bissau. Trop. Med. Int. Health 2016, 22, 12–20. [Google Scholar] [CrossRef]
- Assi, T.M.; Brown, S.T.; Djibo, A.; Norman, B.A.; Rajgopal, J.; Welling, J.S.; Chen, S.I.; Bailey, R.R.; Kone, S.; Kenea, H.; et al. Impact of changing the measles vaccine vial size on Niger’s vaccine supply chain: A computational model. BMC Public Health 2011, 11, 425. [Google Scholar] [CrossRef] [Green Version]
- HABITAT. Profil Urbain National du Niger; HABITAT: Brighton, UK, 2007. [Google Scholar]
- Abdourazack, N.A. Urbanisation et Précarité de L’énergie Électrique dans les Grandes Villes d’Afrique de l’Ouest: L’exemple de Niamey au Niger (Analyse Bibliographique), in Faculté des Lettres et Sciences Humaines Département de Géographie; Université Abdou Moumouni de Niamey: Niamey, Niger, 2017. [Google Scholar]
- Chen, Y.J.; Chindarkar, N.; Xiao, Y. Effect of reliable electricity on health facilities, health information, and child and maternal health services utilization: Evidence from rural Gujarat, India. J. Health Popul. Nutr. 2019, 38, 7. [Google Scholar] [CrossRef] [PubMed]
- Rose, T. The End of Average: How We Succeed in a World That Values Sameness; Penguin Random House: London, UK, 2016. [Google Scholar]
- Agha, S.; Tollefson, D.; Paul, S.; Green, D.; Babigumira, J.B. Use of the Fogg Behavior Model to Assess the Impact of a Social Marketing Campaign on Condom Use in Pakistan. J. Health Commun. 2019, 24, 284–292. [Google Scholar] [CrossRef] [PubMed]
- Fogg, B. Tiny Habits: The Small Changes That Change Everything; Houghton Mifflin Harcourt: Boston, MA, USA, 2019. [Google Scholar]
- Seidu, A.-A.; Ahinkorah, B.O.; Ameyaw, E.K.; Budu, E.; Yaya, S. Women empowerment indicators and uptake of child health services in sub-Saharan Africa: A multilevel analysis using cross-sectional data from 26 countries. J. Public Health 2021. [Google Scholar] [CrossRef] [PubMed]
- Moumouni, A.; Doingalé, H.; Mahamadou, D.; Attoh, T.; Tiembré, I. Séroprévalence de la Rubéole au Niger de 2005 à 2019: Estimations Issues du Système de Surveillance Épidémiologique de la Rougeole. St. Publique 2021, 33, 591–596. [Google Scholar] [CrossRef] [PubMed]
- Aheto, J.M.K.; Pannell, O.; Dotse-Gborgbortsi, W.; Trimner, M.K.; Tatem, A.J.; Rhoda, D.A.; Cutts, F.T.; Utazi, C.E. Multilevel analysis of predictors of multiple indicators of childhood vaccination in Nigeria. PLoS ONE 2022, 17, e0269066. [Google Scholar] [CrossRef]
| Variable | Total | Child Vaccinated Against Measles 1 | Child Not Vaccinated Against Measles 1 | ||||
|---|---|---|---|---|---|---|---|
| n | (%) | n | (%) | n | (%) | p-Value | |
| Maternal Education Level | 0.037 | ||||||
| No education | 150 | (33.7) | 84 | (56.0) | 66 | (44.0) | |
| Basic literacy | 87 | (19.6) | 50 | (57.5) | 37 | (42.5) | |
| Primary-secondary education | 182 | (40.9) | 128 | (70.3) | 54 | (29.7) | |
| Secondary plus education | 26 | (5.8) | 17 | (65.4) | 9 | (34.6) | |
| Mother’s Age | 0.433 | ||||||
| 15 to 19 years old | 32 | (7.2) | 17 | (53.1) | 15 | (46.9) | |
| 20 to 24 years old | 103 | (23.3) | 69 | (66.0) | 35 | (34.0) | |
| 25 to 29 years old | 132 | (29.8) | 86 | (65.2) | 46 | (34.9) | |
| 30 to 34 years old | 80 | (18.1) | 44 | (55.0) | 36 | (45.0) | |
| 35 to 39 years old | 73 | (16.5) | 48 | (65.8) | 25 | (34.3) | |
| 40 years old or more | 23 | (5.2) | 16 | (30.4) | 7 | (69.6) | |
| Mother Tongue | 0.912 | ||||||
| Hausa | 143 | (32.1) | 87 | (60.8) | 56 | (39.2) | |
| Zarma | 240 | (53.9) | 154 | (64.2) | 86 | (35.8) | |
| Fulani | 35 | (7.9) | 22 | (62.9) | 13 | (37.1) | |
| Tamachek | 8 | (1.8) | 4 | (50.0) | 4 | (50.0) | |
| Others | 19 | (4.3) | 12 | (63.2) | 7 | (36.8) | |
| Husband’s Job | 0.464 | ||||||
| Unemployed | 19 | (4.3) | 13 | (68.4) | 6 | (31.6) | |
| Informal work | 194 | (43.6) | 119 | (61.3) | 75 | (38.7) | |
| Formal employment | 147 | (33.0) | 88 | (59.9) | 59 | (40.1) | |
| Public servant | 85 | (19.1) | 59 | (69.4) | 26 | (30.6) | |
| Gave Birth | 0.017 | ||||||
| At home | 47 | (10.6) | 22 | (46.8) | 25 | (53.2) | |
| At health center | 398 | (89.4) | 257 | (64.6) | 141 | (35.4) | |
| Mother Discussed Vaccination with Friends | 0.311 | ||||||
| No discussion | 163 | (37.7) | 100 | (61.4) | 63 | (38.7) | |
| Had discussed | 269 | (62.3) | 178 | (66.2) | 91 | (33.8) | |
| Time to (Access) Health Center | 0.033 | ||||||
| 1 to 30 min | 302 | (73.8) | 204 | (67.6) | 98 | (32.5) | |
| 31 to 60 min | 84 | (20.5) | 49 | (58.3) | 35 | (41.7) | |
| 61 to 90 min | 10 | (2.4) | 3 | (30.0) | 7 | (70.0) | |
| 91 to 150 min | 13 | (3.2) | 10 | (76.9) | 3 | (23.1) | |
| Access to Electricity | 0.076 | ||||||
| No | 101 | (23.1) | 56 | (55.5) | 45 | (44.6) | |
| Yes | 336 | (76.9) | 219 | (65.2) | 117 | (34.8) | |
| Mean Centered Wealth Scores | 0.092 | ||||||
| Total | 436 | 275 | (63.1) | 161 | (36.9) | ||
| Variables | Model 0 (Empty Model) | Model 1 (Only Individual Level Variables) | Model 2 (Only Neighborhood-Level Variables) | Model 3 (Multilevel) | ||||
|---|---|---|---|---|---|---|---|---|
| n = 445 | n = 431 | n = 401 | n = 400 | |||||
| OR | (95% CI) | OR | (95% CI) | OR | (95% CI) | OR | (95% CI) | |
| Maternal Education | ||||||||
| No education (ref) | ||||||||
| Basic literacy | 1.05 | (0.57–1.95) | 0.94 | (0.49–1.82) | ||||
| Primary-secondary education | 1.92 * | (1.14–3.22) | 1.97 * | (1.11–3.51) | ||||
| Secondary plus education | 1.75 | (0.60–5.13) | 1.53 | (0.48–4.83) | ||||
| Mother’s Age | ||||||||
| 15 to 19 years old (ref) | ||||||||
| 20 to 24 years old | 1.72 | (0.73–4.05) | 1.40 | (0.56–3.53) | ||||
| 25 to 29 years old | 1.81 | (0.78–4.20) | 1.62 | (0.65–4.04) | ||||
| 30 to 34 years old | 1.27 | (0.53–3.06) | 1.01 | (0.39–2.60) | ||||
| 35 to 39 years old | 2.01 | (0.80–5.06) | 1.87 | (0.70–5.00) | ||||
| 40 years old or more | 3.01 | (0.82–10.98) | 3.91 | (0.90–16.92) | ||||
| Mother Tongue | ||||||||
| Hausa (ref) | ||||||||
| Zarma | 1.05 | (0.64–1.72) | 1.17 | (0.69–1.98) | ||||
| Fulani | 0.98 | (0.38–2.52) | 1.35 | (0.47–3.85) | ||||
| Tamachek | 0.84 | (0.15–4.62) | 1.27 | (0.21–7.50) | ||||
| Others | 0.93 | (0.31–2.73) | 0.93 | (0.29–3.02) | ||||
| Husband’s Job | ||||||||
| Unemployed (ref) | ||||||||
| Informal work | 0.51 | (0.16–1.66) | 0.47 | (0.13–1.64) | ||||
| Formal employment | 0.51 | (0.15–1.68) | 0.54 | (0.15–1.95) | ||||
| Public servant | 0.63 | (0.18–2.24) | 0.51 | (0.13–1.99) | ||||
| Gave Birth | ||||||||
| At home (ref) | 1.83 | (0.85–3.94) | ||||||
| At health center | 2.04 | (0.84–4.94) | ||||||
| Mother Discussed Vaccination with Friends | ||||||||
| No discussion (ref) | ||||||||
| Had discussed | 1.25 | (0.75–2.07) | 1.09 | (0.63–1.87) | ||||
| Time to (Access) Health Center | ||||||||
| 1 to 30 min (ref) | ||||||||
| 31 to 60 min | 0.68 | (0.39–1.18) | 0.71 | (0.39–1.28) | ||||
| 61 to 90 min | 0.23 | (0.05–1.02) | 0.23 | (0.04–1.26) | ||||
| 91 to 150 min | 2.35 | (0.51–10.76) | 4.12 | (0.77–22.03) | ||||
| Access to Electricity | ||||||||
| No (ref) | ||||||||
| Yes | 1.06 | (0.50–2.26) | 0.85 | (0.38–1.92) | ||||
| Mean Centered Wealth Scores | 1.11 | (0.92–1.34) | 1.11 | (0.90–1.36) | ||||
| Intercept (SE) | 1.71 | (0.23) | 0.77 | (0.63) | 2.02 | (0.69) | 1.06 | (1.00) |
| Random Effects | ||||||||
| Neighborhood variance (SE) | 0.29 | (0.19) | 0.25 | (0.20) | 0.25 | (0.20) | 0.30 | (0.23) |
| VPC | 0.08 | 0.07 | 0.07 | 0.08 | ||||
| PCV (%) | - | 13.8% | 13.8% | −3.5% | ||||
| Interclass Correlation (ICC, %) | 8.1% | 7.1% | 7.1% | 8.3% | ||||
| Median Odds Ratio (MOR) | 1.67 | 1.61 | 1.61 | 1.68 | ||||
| Log Pseudolikelihood | −291.61 | −268.48 | −251.60 | −241.47 | ||||
| AIC | 587.23 | 574.96 | 517.21 | 530.93 | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kunieda, M.K.; Manzo, M.L.; Subramanian, S.V.; Jimba, M. Individual- and Neighborhood-Level Factors of Measles Vaccination Coverage in Niamey, Niger: A Multilevel Analysis. Vaccines 2022, 10, 1513. https://doi.org/10.3390/vaccines10091513
Kunieda MK, Manzo ML, Subramanian SV, Jimba M. Individual- and Neighborhood-Level Factors of Measles Vaccination Coverage in Niamey, Niger: A Multilevel Analysis. Vaccines. 2022; 10(9):1513. https://doi.org/10.3390/vaccines10091513
Chicago/Turabian StyleKunieda, Mika Kondo, Mahamane Laouali Manzo, S. V. Subramanian, and Masamine Jimba. 2022. "Individual- and Neighborhood-Level Factors of Measles Vaccination Coverage in Niamey, Niger: A Multilevel Analysis" Vaccines 10, no. 9: 1513. https://doi.org/10.3390/vaccines10091513
APA StyleKunieda, M. K., Manzo, M. L., Subramanian, S. V., & Jimba, M. (2022). Individual- and Neighborhood-Level Factors of Measles Vaccination Coverage in Niamey, Niger: A Multilevel Analysis. Vaccines, 10(9), 1513. https://doi.org/10.3390/vaccines10091513









