Ensuring Equitable COVID-19 Vaccine Allocation in New Hampshire: The First Eight Months toward a New Era
Abstract
:1. Introduction
2. Methods & Approaches towards Developing the State Vaccine Allocation Strategy
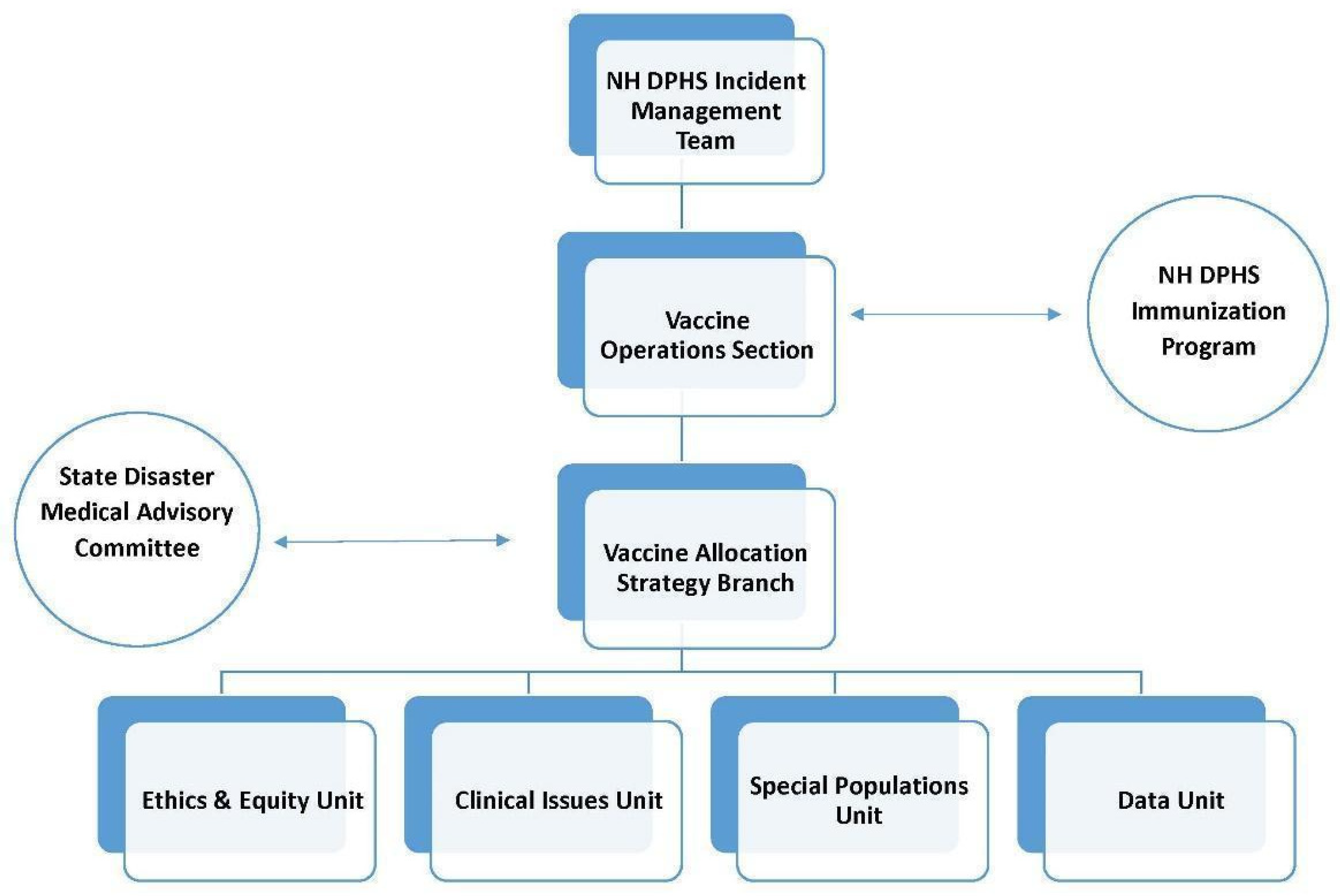
2.1. Organization to Create the NH Vaccine Allocation Strategy
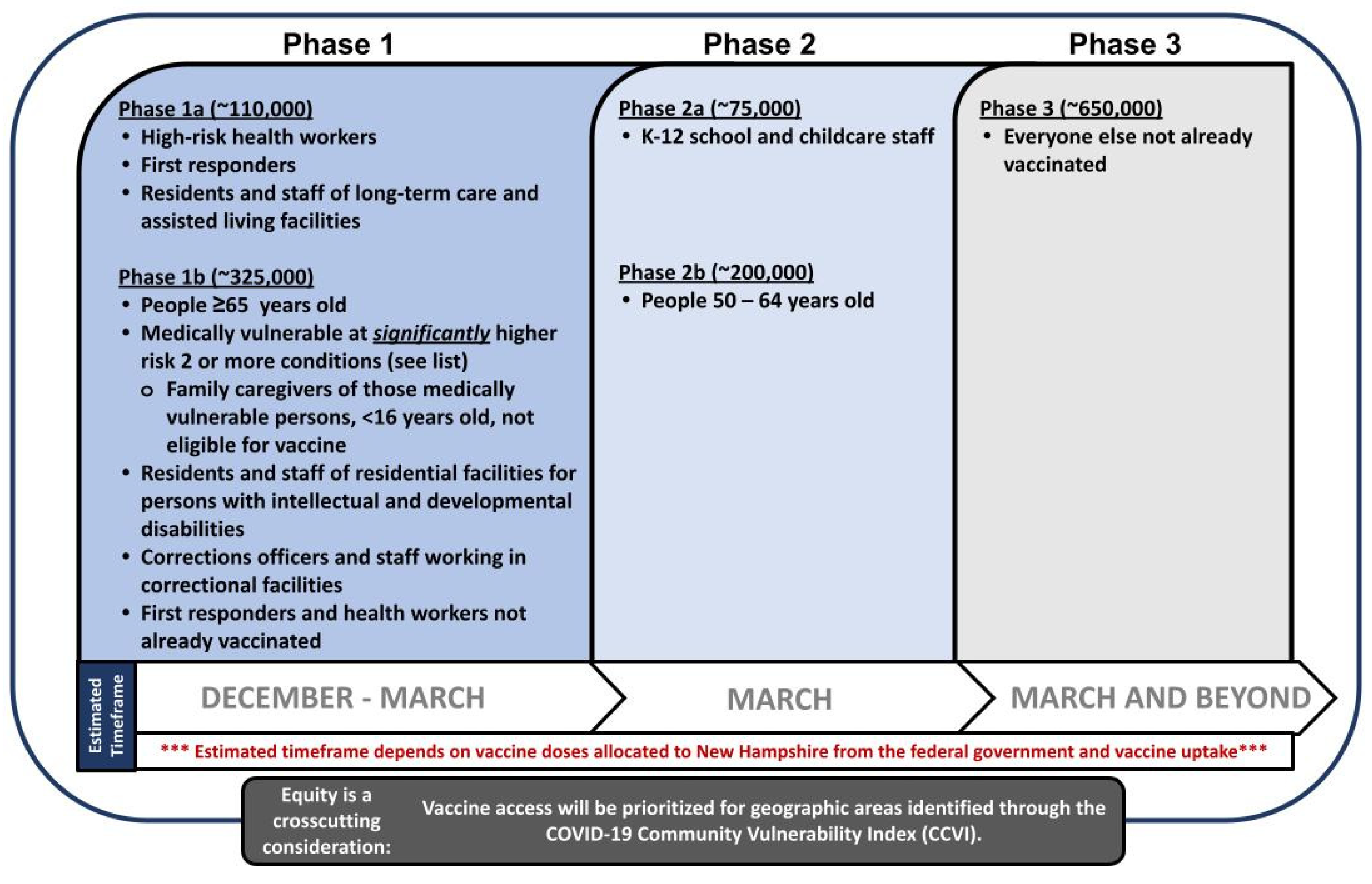
2.2. The VASB Approach to Establish an Equitable Vaccine Allocation Strategy
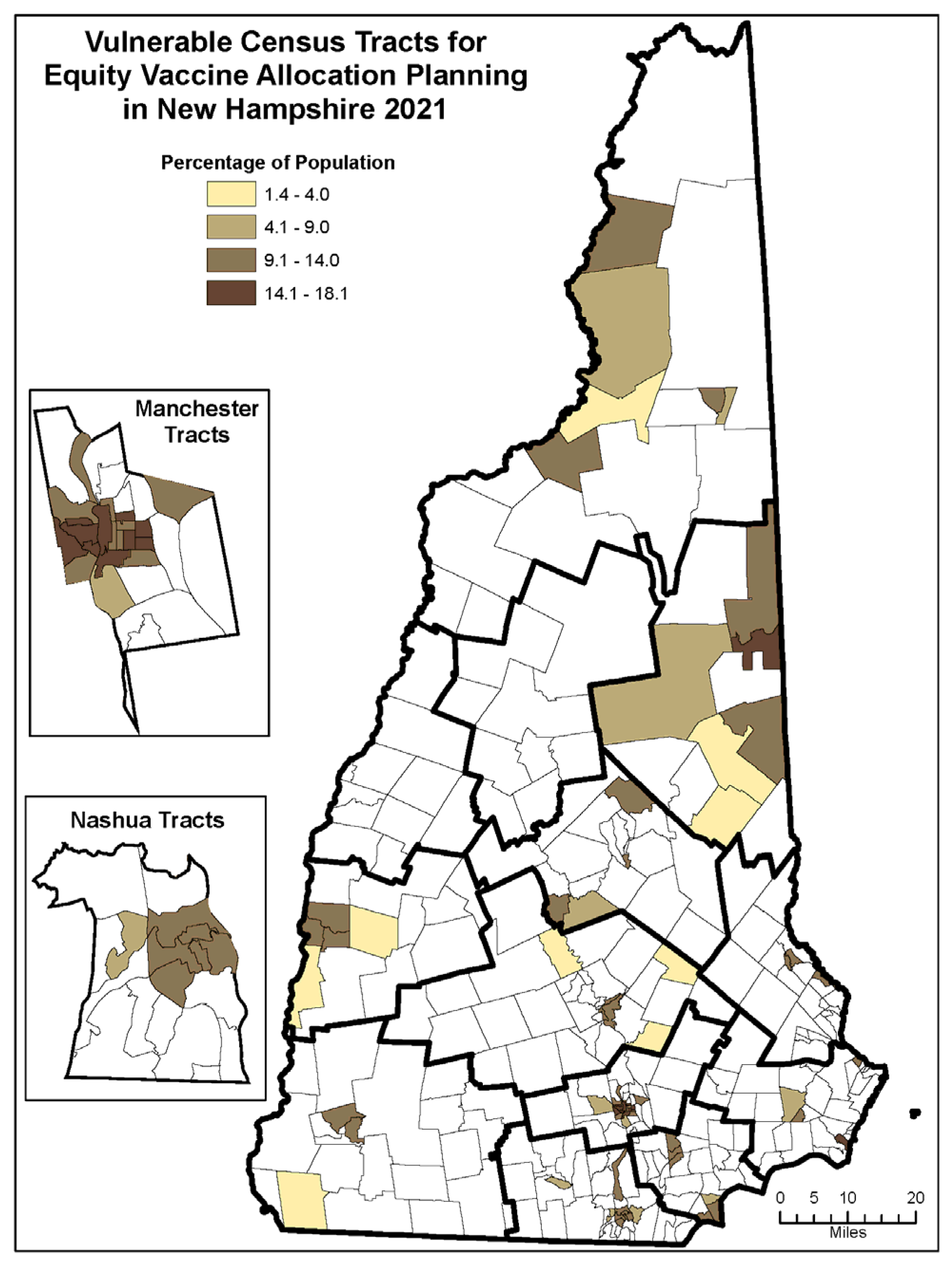
- Resided in highly vulnerable census tracts (see Figure 3) using the CCVI and US Census data for population estimates; and/or
- Met one or more eligibility criteria regardless of residence:
- ○
- Identified as a racial and ethnic minority (all persons identified as other than White, non-Hispanic)
- ○
- Were experiencing homelessness (sheltered and unsheltered)
- ○
- Qualified as low income (household income at or below 185% of the poverty level)
- ○
- Reported being geographically isolated or encountering physical or other barriers to travel (i.e., limited access to transportation) to points of vaccine distribution
- ○
- Were homebound including:
- The person’s doctor believed that their health or illness could get worse if they left the home;
- The person required the help of another person and/or medical equipment to leave the home, or found it difficult to leave the home and typically could not do so except for medical appointments or treatment or for short periods of time or for special non-medical events
- ○
- Reported lacking a medical home through which to verify their medical vulnerability
- ○
- Experienced language/communication access barriers that prevented them from understanding vaccine registration instructions and assent during the documentation process
- ○
- Reported other significant barriers that prevented them from being vaccinated through other mechanisms
2.3. Resources Needed for Developing an Equitable Vaccine Allocation Strategy
2.4. Partner and Community Consensus on Allocation
3. Results: COVID-19 Vaccine Allocation Challenges
3.1. Unanticipated Consequences of the Equitable Allocation Strategy
3.2. Allowing for a Dynamic Allocation Strategy
3.3. Anticipating Uncertainties during Planning for Equitable Vaccine Allocation
3.4. Operational Challenges during Development of the Equitable Vaccine Allocation Strategy
4. Discussion: Preparing for the Next Pandemic
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Disclaimer
Appendix A. Programs Represented in Vaccine Allocation Strategy Branch (VASB)
- Office of the Governor
- NH DHHS/Office of the Commissioner
- NH DHHS/Bureau of Housing Supports
- NH DHHS/Division of Medicaid Services
- NH DHHS/DPHS/Bureau of Emergency Preparedness, Response, and Recovery
- NH DHHS/DPHS/Bureau of Infectious Disease Control
- NH DHHS/DPHS/Bureau of Public Health Statistics and Informatics
- NH DHHS/DPHS/Community Health Development
- NH DHHS/Public Information Office
- NH Department of Safety/Fire Standards and Training/Emergency Medical Services
- NH National Guard
References
- COVID-19 Dashboard. Available online: https://coronavirus.jhu.edu/map.html (accessed on 13 August 2022).
- Hospitalization and Death by Race/Ethnicity. Available online: https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/hospitalization-death-by-race-ethnicity.html (accessed on 24 June 2022).
- U.S. Census Bureau. Available online: https://data.census.gov/cedsci/table?g=0400000US33&tid=DECENNIALPL2020.P2&tp=false (accessed on 15 July 2022).
- Governor’s COVID-19 Equity Response Team Initial Report and Recommendations 2020. Available online: https://www.governor.nh.gov/sites/g/files/ehbemt336/files/documents/equity-response-team.pdf (accessed on 15 July 2022).
- COVID-19 Vaccination Program Interim Operational Guidance Jurisdiction Operations. Available online: https://www.cdc.gov/vaccines/imz-managers/downloads/Covid-19-Vaccination-Program-Interim_Playbook.pdf (accessed on 15 July 2022).
- Crisis Standards of Care State Disaster Medical Advisory Committee. Available online: https://www.dhhs.nh.gov/about-dhhs/advisory-organizations/crisis-standards-care-state-disaster-medical-advisory-committee (accessed on 15 July 2022).
- National Academies of Sciences Engineering and Medicine; Health and Medicine Division; Board on Global Health; Forum on Microbial Threats; Committee on Equitable Allocation of Vaccine for the Novel Coronavirus. The National Academies Collection: Reports funded by National Institutes of Health. In Framework for Equitable Allocation of COVID-19 Vaccine; Kahn, B., Brown, L., Foege, W., Gayle, H., Eds.; National Academies Press (US): Washington, DC, USA, 2020. [Google Scholar]
- New Hampshire Coronavirus Disease 2019 Vaccination Plan. Available online: https://www.covid19.nh.gov/sites/g/files/ehbemt481/files/inline-documents/sonh/covid19-vac-plan.pdf (accessed on 15 July 2022).
- New Hampshire COVID-19 Vaccination Allocation Plan Summary. Available online: https://www.covid19.nh.gov/sites/g/files/ehbemt481/files/inline-documents/sonh/covid19-vaccine-allocation-plan-summary.pdf (accessed on 15 July 2022).
- The, U.S. COVID Community Vulnerability Index (CCVI). Available online: https://precisionforcovid.org/ccvi (accessed on 15 July 2022).
- Guidelines for Vaccine Equity Allocation (VEA). Available online: https://www.covid19.nh.gov/sites/g/files/ehbemt481/files/inline-documents/sonh/equity-technical-assistance.pdf (accessed on 15 July 2022).
- Brownson, R.C.; Burke, T.A.; Colditz, G.A.; Samet, J.M. Reimagining Public Health in the Aftermath of a Pandemic. Am. J. Public Health 2020, 110, 1605–1610. [Google Scholar] [CrossRef] [PubMed]
- National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Population Health and Public Health Practice; Board on Health Sciences Policy; Committee on Equitable Allocation of Vaccine for the Novel Coronavirus; Framework for Equitable Allocation of COVID-19 Vaccine. Available online: https://nap.nationalacademies.org/resource/25917/Framework%20for%20Equitable%20Allocation%20of%20COVID-19%20Vaccine_Public%20Briefing_Slides.pdf (accessed on 15 July 2022).
- Dooling, K.; Marin, M.; Wallace, M.; McClung, N.; Chamberland, M.; Lee, G.M.; Talbot, H.K.; Romero, J.R.; Bell, B.P.; Oliver, S.E. The Advisory Committee on Immunization Practices’ Updated Interim Recommendation for Allocation of COVID-19 Vaccine—United States, December 2020. MMWR Morb. Mortal. Wkly. Rep. 2021, 69, 1657–1660. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, H.; Weintraub, R.; Williams, M.A.; Miller, K.; Buttenheim, A.; Sadecki, E.; Wu, H.; Doiphode, A.; Nagpal, N.; Gostin, L.O.; et al. Equitable allocation of COVID-19 vaccines in the United States. Nat. Med. 2021, 27, 1298–1307. [Google Scholar] [CrossRef] [PubMed]
- The Robert Wood Johnson Foundation, National Commission to Transform Public Health Data Systems. Charting a Course for an Equity-Centered Data System: Recommendations from the National Commission to Transform Public Health Data Systems; 2021. Available online: https://www.rwjf.org/en/library/research/2021/10/charting-a-course-for-an-equity-centered-data-system.html (accessed on 13 August 2022).
- Wyche Etheridge, K.; Justice, A.D.; Lewis, M.; Plescia, M. Strategies to Operationalize Health Equity in State and Territorial Health Departments. J. Public Health Manag. Pract. 2022, 28, 433–434. [Google Scholar] [CrossRef] [PubMed]
- Community Engagement: A Health Promotion Guide for Universal Health Coverage in the Hands of the People; World Health Organization: Geneva, Switzerland, 2020.
- Hernandez, I.; Dickson, S.; Tang, S.; Gabriel, N.; Berenbrok, L.A.; Guo, J. Disparities in distribution of COVID-19 vaccines across US counties: A geographic information system-based cross-sectional study. PLoS Med. 2022, 19, e1004069. [Google Scholar] [CrossRef] [PubMed]
| Foundational Principles | Definition |
|---|---|
| Ethical Principles: | |
| Maximum benefit | Encompasses the obligation to protect and promote the public’s health and its socioeconomic well-being in the short and long term |
| Equal concern | Requires that every person be considered and treated as having equal dignity, worth, and value |
| Mitigation of health inequities | Includes the obligation to explicitly address the higher burden of COVID-19 experienced by the populations affected most heavily, given their exposure and compounding health inequities. |
| Procedural Principles: | |
| Fairness | Requires engagement with the public, particularly those most affected by the pandemic, and impartial decision making about and evenhanded application of allocation criteria and priority categories. |
| Transparency | Includes the obligation to communicate with the public openly, clearly, accurately, and straightforwardly about the allocation framework as it is being developed, deployed, and modified. |
| Evidence-based | Expresses the requirement to base the allocation framework, including its goal, criteria, and phases, on the best available and constantly updated scientific information and data. |
| Phase | Predicted Supply & Demand | Target/Focus |
|---|---|---|
| 1 | Severely limited doses available | Those at highest risk of morbidity and mortality and frontline healthcare workers |
| 2 | Large number of doses available, supply likely to meet demand | Additional high-risk populations not vaccinated during phase one |
| 3 | Likely sufficient supply, slowing demand | Equitable vaccination access |
| Features of Early Pandemic Vaccine Allocation | Implications for Equity |
|---|---|
| Uncertain number and timing of available vaccine doses | ● The inability to commit to vaccine allocation in advance likely disproportionately negatively impacted persons who qualified for equity doses, because they often require more time to plan and access vaccine than those who do not (e.g., finding childcare, arranging transportation, planning day off work) ● Messaging that described tentative vaccination availability could undermine already fragile trust in government public health systems among populations requiring equitable distribution, particularly among historically marginalized populations |
| Uncertain vaccine efficacy, especially for vulnerable populations | ● Community partners sometimes expressed preference for the more operationally feasible but less efficacious single-dose Johnson and Johnson / Janssen vaccine, which may have resulted in disproportionate allocation for transient and high-need populations (e.g., migrant, incarcerated, homeless and homebound) ● Differences in feasibility/efficacy required careful balance between public demand and public benefit, including the decision to not direct only one vaccine product based on logistical considerations (e.g., challenges with reaching transient populations for second doses) |
| Vaccine safety, overall and in different populations | ● Communicating incomplete vaccine safety data may have increased vaccine hesitancy, which was initially higher among populations requiring equitable distribution, particularly among historically marginalized populations ● Development of clear messaging regarding safety was delayed for certain populations, particularly those requiring non-English and plain language messaging |
| Extreme cold chain requirements for the mRNA vaccines | ● Some groups requested specific vaccine based on ease of handling and storage capacities. Sites serving lower resource communities were less likely to have the logistical capability to handle all storage and handling requirements, resulting in less vaccine access to the highest need populations ● Unanticipated resources were required to maintain cold chain, including appropriate refrigerators/freezers and dedicated mobile providers |
| Social, economic, and legal contexts | ● Considerable resources were required to balance and communicate differential risk that resulted in the prioritizing of some populations over others ● Equitable allocation practices should incorporate a public input process, including a mechanism for requests for prioritization, and transparency of final decisions and the decision-making process |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Selembo, T.D.; Talbot, E.A.; Courtine, C.T.; Daly, E.R.; Hull, T.W.; Durzy, K.J. Ensuring Equitable COVID-19 Vaccine Allocation in New Hampshire: The First Eight Months toward a New Era. Vaccines 2022, 10, 1421. https://doi.org/10.3390/vaccines10091421
Selembo TD, Talbot EA, Courtine CT, Daly ER, Hull TW, Durzy KJ. Ensuring Equitable COVID-19 Vaccine Allocation in New Hampshire: The First Eight Months toward a New Era. Vaccines. 2022; 10(9):1421. https://doi.org/10.3390/vaccines10091421
Chicago/Turabian StyleSelembo, Taylor D., Elizabeth A. Talbot, Christophe T. Courtine, Elizabeth R. Daly, Torane W. Hull, and Kirsten J. Durzy. 2022. "Ensuring Equitable COVID-19 Vaccine Allocation in New Hampshire: The First Eight Months toward a New Era" Vaccines 10, no. 9: 1421. https://doi.org/10.3390/vaccines10091421
APA StyleSelembo, T. D., Talbot, E. A., Courtine, C. T., Daly, E. R., Hull, T. W., & Durzy, K. J. (2022). Ensuring Equitable COVID-19 Vaccine Allocation in New Hampshire: The First Eight Months toward a New Era. Vaccines, 10(9), 1421. https://doi.org/10.3390/vaccines10091421






