Cautious Sexual Attitudes Diminish Intent to Vaccinate Children against HPV in Utah
Abstract
:1. Introduction
2. Materials and Methods
2.1. Survey of Utah Residents
2.2. Survey Description
2.3. Confirmatory Factor Analysis and Structural Equation Modeling
2.4. Univariate Analysis
3. Results
3.1. Demographic Characteristics of Survey Respondents
3.2. Confirmatory Factor Analysis
3.3. Structural Equation Modeling
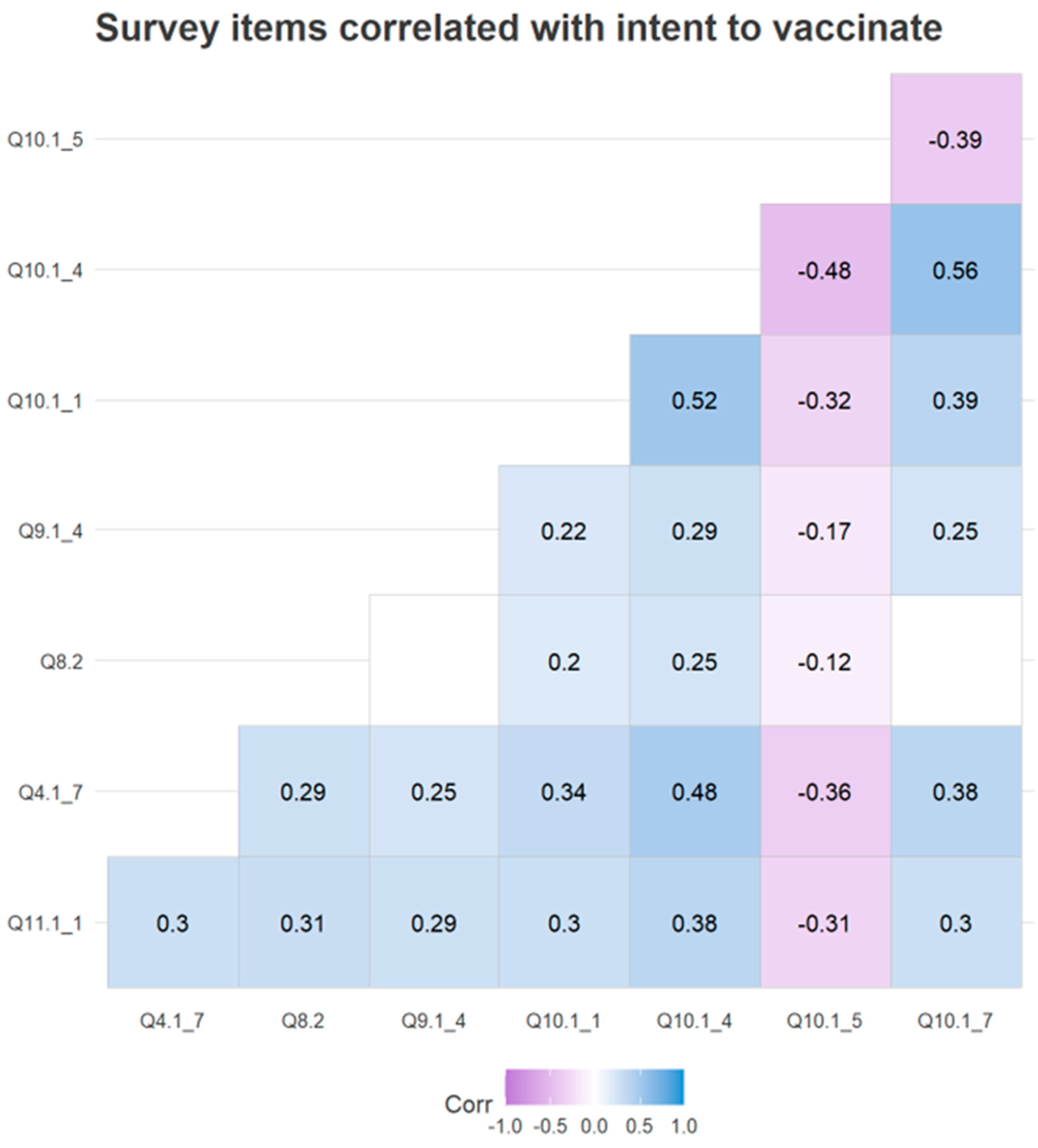
3.4. Univariate Analysis
4. Discussion
4.1. General Attitudes toward Vaccines Are Predictive of Intent to Vaccinate
4.2. High Religious Practice Negatively Impacts Intent to Vaccinate by Influencing Sexual Attitudes
4.3. Knowledge about HPV Increases Intent to Vaccinate, and Sex Education Can Increase HPV Knowledge
4.4. HPV Vaccination Is Viewed Positively in Our Sample Population
4.5. Trust in Health Guidelines Increases Intent to Vaccinate
4.6. Belief That Vaccination Protects against HPV-Induced Cancer Increases Intent to Vaccinate
4.7. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Doorbar, J.; Egawa, N.; Griffin, H.; Kranjec, C.; Murakami, I. Human papillomavirus molecular biology and disease association. Rev. Med. Virol. 2015, 25 (Suppl. 1), 2–23. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McMurray, H.R.; Nguyen, D.; Westbrook, T.F.; Mcance, D.J. Biology of human papillomaviruses. Int. J. Exp. Pathol. 2001, 82, 15–33. [Google Scholar] [CrossRef]
- Braaten, K.P.; Laufer, M.R. Human Papillomavirus (HPV), HPV-Related Disease, and the HPV Vaccine. Rev. Obstet. Gynecol. 2008, 1, 2–10. [Google Scholar] [PubMed]
- Bansal, A.; Singh, M.P.; Rai, B. Human papillomavirus-associated cancers: A growing global problem. Int. J. Appl. Basic Med. Res. 2016, 6, 84–89. [Google Scholar] [PubMed] [Green Version]
- Petca, A.; Borislavschi, A.; Zvanca, M.E.; Petca, R.-C.; Sandru, F.; Dumitrascu, M.C. Non-sexual HPV transmission and role of vaccination for a better future (Review). Exp. Ther. Med. 2020, 20, 186. [Google Scholar] [CrossRef] [PubMed]
- Phillips, A.; Patel, C.; Pillsbury, A.; Brotherton, J.; Macartney, K. Safety of Human Papillomavirus Vaccines: An Updated Review. Drug Saf. 2018, 41, 329–346. [Google Scholar] [CrossRef]
- Brianti, P.; de Flammineis, E.; Mercuri, S.R. Review of HPV-related diseases and cancers. New Microbiol. 2017, 40, 80–85. [Google Scholar]
- Meyers, J.; Ryndock, E.; Conway, M.J.; Meyers, C.; Robison, R. Susceptibility of high-risk human papillomavirus type 16 to clinical disinfectants. J. Antimicrob. Chemother. 2014, 69, 1546–1550. [Google Scholar] [CrossRef] [Green Version]
- Berenson, A.B.; Hirth, J.M.; Chang, M. Change in Human Papillomavirus Prevalence among U.S. Women Aged 18–59 Years, 2009–2014. Obstet. Gynecol. 2017, 130, 693–701. [Google Scholar] [CrossRef]
- Cheng, L.; Wang, Y.; Du, J. Human Papillomavirus Vaccines: An Updated Review. Vaccines 2020, 8, 391. [Google Scholar] [CrossRef]
- Teitelman, A.M.; Stringer, M.; Nguyen, G.T.; Hanlon, A.L.; Averbuch, T.; Stimpfel, A.W. Social cognitive and clinical factors associated with HPV vaccine initiation among urban, economically disadvantaged women. J. Obstet. Gynecol. Neonatal Nurs. 2011, 40, 691–701. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.; Lin, Z.; He, F.; Chen, H.; Lin, X.; Zimet, G.D.; Alias, H.; He, S.; Hu, Z.; Wong, L.P. HPV vaccination intent and willingness to pay for 2-,4-, and 9-valent HPV vaccines: A study of adult women aged 27–45 years in China. Vaccine 2020, 38, 3021–3030. [Google Scholar] [CrossRef] [PubMed]
- Rositch, A.F.; Liu, T.; Chao, C.; Moran, M.; Beavis, A.L. Levels of Parental Human Papillomavirus Vaccine Hesitancy and Their Reasons for Not Intending to Vaccinate: Insights from the 2019 National Immunization Survey-Teen. J. Adolesc. Health 2022, 71, 39–46. [Google Scholar] [CrossRef] [PubMed]
- Patel, D.A.; Zochowski, M.; Peterman, S.; Dempsey, A.F.; Ernst, S.; Dalton, V.K. Human Papillomavirus Vaccine Intent and Uptake among Female College Students. J. Am. Coll. Health 2012, 60, 151–161. [Google Scholar] [CrossRef] [Green Version]
- Horn, S.; Chapman, G.B.; Chouhan, K. Doctor recommendations and parents’ HPV vaccination intentions in Kenya: A randomized survey. Prev. Med. Rep. 2022, 25, 101659. [Google Scholar] [CrossRef]
- Brawner, B.M.; Baker, J.L.; Voytek, C.D.; Leader, A.; Cashman, R.R.; Silverman, R.; Peter, N.; Buchner, B.J.; Barnes, C.A.; Jemmott, L.S.; et al. The development of a culturally relevant, theoretically driven HPV prevention intervention for urban adolescent females and their parents/guardians. Health Promot. Pract. 2013, 14, 624–636. [Google Scholar] [CrossRef] [PubMed]
- Spayne, J.; Hesketh, T. Estimate of global human papillomavirus vaccination coverage: Analysis of country-level indicators. BMJ Open 2021, 11, e052016. [Google Scholar] [CrossRef] [PubMed]
- Walker, T.Y.; Elam-Evans, L.D.; Singleton, J.A.; Yankey, D.; Markowitz, L.E.; Fredua, B.; Williams, C.L.; Meyer, S.A.; Stokley, S. National, Regional, State, and Selected Local Area Vaccination Coverage among Adolescents Aged 13–17 Years—United States, 2016. MMWR Morb. Mortal. Wkly. Rep. 2017, 66, 874–882. [Google Scholar] [CrossRef] [Green Version]
- Reagan-Steiner, S.; Yankey, D.; Jeyarajah, J.; Elam-Evans, L.D.; Singleton, J.A.; Curtis, C.R.; MacNeil, J.; Markowitz, L.E.; Stokley, S. National, Regional, State, and Selected Local Area Vaccination Coverage among Adolescents Aged 13–17 Years—United States, 2014. MMWR Morb. Mortal. Wkly. Rep. 2015, 64, 784–792. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- American Health Rankings. Explore HPV Vaccination in the United States: 2021 Annual Report. 2021. Available online: https://www.americashealthrankings.org/explore/annual/measure/Immunize_HPV/state/ALL (accessed on 2 August 2022).
- Harris, K.L.; Tay, D.; Kaiser, D.; Praag, A.; Rutkoski, H.; Dixon, B.L.; Pinzon, L.M.; Winkler, J.R.; Kepka, D. The perspectives, barriers, and willingness of Utah dentists to engage in human papillomavirus (HPV) vaccine practices. Hum. Vaccines Immunother. 2020, 16, 436–444. [Google Scholar] [CrossRef]
- Warner, E.L.; Ding, Q.; Pappas, L.; Bodson, J.; Fowler, B.; Mooney, R.; Kirchhoff, A.C.; Kepka, D. Health Care Providers’ Knowledge of HPV Vaccination, Barriers, and Strategies in a State with Low HPV Vaccine Receipt: Mixed-Methods Study. JMIR Cancer 2017, 3, e12. [Google Scholar] [CrossRef] [PubMed]
- Bodson, J.; Wilson, A.; Warner, E.L.; Kepka, D. Religion and HPV vaccine-related awareness, knowledge, and receipt among insured women aged 18–26 in Utah. PLoS ONE 2017, 12, e0183725. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Redd, D.S.; Jensen, J.L.; Hughes, S.J.; Pogue, K.; Sloan-Aagard, C.D.; Miner, D.S.; Altman, J.D.; Crook, T.B.; Zentz, L.; Bodily, R.J.; et al. Effects of Religious Practice and Teachings about Sexual Behavior on Intent to Vaccinate against Human Papillomavirus. Vaccines 2022, 10, 397. [Google Scholar] [CrossRef] [PubMed]
- Shams, A.B.; Apu, E.H.; Rahman, A.; Raihan, S.; Siddika, N.; Preo, R.; Hussein, M.; Mostari, S.; Kabir, R. Web Search Engine Misinformation Notifier Extension (SEMiNExt): A Machine Learning Based Approach during COVID-19 Pandemic. Healthcare 2021, 9, 156. [Google Scholar] [CrossRef]
- LDS_Church. What Is the Law of Chastity. Teaching Pamphlets 2022. Available online: https://www.churchofjesuschrist.org/study/manual/chastity/what-is-the-law-of-chastity?lang=eng (accessed on 27 July 2022).
- CDC. HPV Vaccination Recommendations. 2022. Available online: https://www.cdc.gov/vaccines/vpd/hpv/hcp/recommendations.html (accessed on 2 August 2022).






| Range | Number | Percent of Total Responses |
|---|---|---|
| Number of Children | n = 365 | |
| 1 | 134 | 36.7% |
| 2 | 116 | 31.8% |
| 3 | 64 | 17.5% |
| 4 | 33 | 9.0% |
| More than 4 | 18 | 4.9% |
| Age | n = 365 | |
| 18–25 | 23 | 6.3% |
| 26–35 | 144 | 39.5% |
| 36–45 | 155 | 42.5% |
| 46–55 | 33 | 9.0% |
| Over 55 | 10 | 2.7% |
| Gender | n = 363 | |
| Male | 113 | 31.1% |
| Female | 250 | 68.9% |
| Ethnicity | n = 365 | |
| American Indian or Alaskan native | 2 | 0.55% |
| Asian | 10 | 2.74% |
| Black or African American | 3 | 0.82% |
| Latino or Hispanic | 30 | 8.22% |
| Pacific Islander or Native Hawaiian | 8 | 2.19% |
| White | 303 | 83.01% |
| Two or More | 5 | 1.37% |
| Other/Unknown | 2 | 0.55% |
| I prefer not to answer | 2 | 0.55% |
| Marital Status | n = 364 | |
| Single | 46 | 12.64% |
| Married | 249 | 68.41% |
| Partnered (non-married) | 27 | 7.42% |
| Divorced | 33 | 9.07% |
| Widow/Widower | 6 | 1.65% |
| Other | 3 | 0.82% |
| Education | n = 365 | |
| Have not completed High School | 9 | 2.47% |
| Finished High School | 92 | 25.48% |
| Some College | 100 | 27.40% |
| Associates degree | 41 | 11.23% |
| Bachelors degree | 84 | 23.01% |
| Post-baccalaureate/professional degree | 38 | 10.41% |
| Yearly Household Income | n = 364 | |
| Less than $25,000 | 46 | 12.64% |
| $25,000–$50,000 | 97 | 26.65% |
| $50,000–$100,000 | 157 | 43.13% |
| $100,000–$150,000 | 48 | 13.19% |
| $150,000–$200,000 | 15 | 4.12% |
| More than $200,000 | 1 | 0.27% |
| Political affiliation | n = 364 | |
| Democrat | 69 | 19.0% |
| Republican | 137 | 37.6% |
| No political affiliation | 122 | 33.5% |
| I prefer not to answer | 27 | 7.4% |
| Other | 9 | 2.5% |
| Political leanings on social issues | n = 365 | |
| Very Liberal | 25 | 6.8% |
| Liberal | 29 | 7.9% |
| Somewhat Liberal | 37 | 10.1% |
| Neither Liberal nor Conservative | 134 | 36.7% |
| Somewhat Conservative | 61 | 16.7% |
| Conservative | 54 | 14.8% |
| Strongly Conservative | 25 | 6.8% |
| Religious Affiliation | n = 364 | |
| Buddhism | 2 | 0.82% |
| Christianity | 211 | 57.81% |
| Hinduism | 3 | 0.82% |
| Islam | 1 | 0.27% |
| Judaism | 3 | 0.82% |
| Other | 43 | 11.78% |
| No Religious Affiliation | 101 | 27.67% |
| Model (Latent Variables) | TLI | CFI | RMSEA | SRMR | χ2 | Chi-Square Test df | p-Value |
|---|---|---|---|---|---|---|---|
| Combined model | 0.886 | 0.900 | 0.057 | 0.076 | 887.029 | 408 | <0.001 |
| Model (Latent Variables) | TLI | CFI | RMSEA | SRMR | χ2 | Chi-Square Test df | p-Value |
|---|---|---|---|---|---|---|---|
| Combined model | 0.885 | 0.902 | 0.050 | 0.067 | 1013.133 | 528 | <0.001 |
| Model A | 0.916 | 0.929 | 0.070 | 0.062 | 398.635 | 143 | <0.001 |
| Model B | 0.928 | 0.943 | 0.071 | 0.055 | 268.436 | 95 | <0.001 |
| # | Text | PCC | p-Value |
|---|---|---|---|
| 4.1.7 | I trust in public health guidelines provided by the CDC (Centers for Disease Control and Prevention) | 0.31 | <0.0001 |
| 8.2 | Sexual education is a necessary part of school curriculum | 0.31 | <0.0001 |
| 9.1.4 | The HPV vaccine is effective at preventing almost all cancers caused by HPV | 0.29 | <0.0001 |
| 10.1.1 | Vaccines are more helpful than harmful | 0.30 | <0.0001 |
| 10.1.4 | Vaccines are extensively tested to ensure their safety | 0.38 | <0.0001 |
| 10.1.5 | Vaccines contain dangerous toxins | −0.31 | <0.0001 |
| 10.1.7 | Vaccination efforts have considerably reduced the transmission of infectious diseases in the United States | 0.30 | <0.0001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Redd, D.S.; Jensen, J.L.; Bodily, R.J.; Lee, A.A.; Skyles, T.J.; Poole, B.D. Cautious Sexual Attitudes Diminish Intent to Vaccinate Children against HPV in Utah. Vaccines 2022, 10, 1382. https://doi.org/10.3390/vaccines10091382
Redd DS, Jensen JL, Bodily RJ, Lee AA, Skyles TJ, Poole BD. Cautious Sexual Attitudes Diminish Intent to Vaccinate Children against HPV in Utah. Vaccines. 2022; 10(9):1382. https://doi.org/10.3390/vaccines10091382
Chicago/Turabian StyleRedd, David S., Jamie L. Jensen, Ruth J. Bodily, Abigail A. Lee, Ty J. Skyles, and Brian D. Poole. 2022. "Cautious Sexual Attitudes Diminish Intent to Vaccinate Children against HPV in Utah" Vaccines 10, no. 9: 1382. https://doi.org/10.3390/vaccines10091382
APA StyleRedd, D. S., Jensen, J. L., Bodily, R. J., Lee, A. A., Skyles, T. J., & Poole, B. D. (2022). Cautious Sexual Attitudes Diminish Intent to Vaccinate Children against HPV in Utah. Vaccines, 10(9), 1382. https://doi.org/10.3390/vaccines10091382






