Risk Factors and Incidence Rates of Self-Reported Short-Term Adverse Events of COVID-19 Vaccine Booster Dose
Abstract
:1. Introduction
2. Materials and Methods
2.1. Overview
2.1.1. Booster Vaccination Program in Taiwan
2.1.2. VAERS in Taipei Veterans General Hospital (TVGH)
2.2. Setting, Data Source, and Ethical Concerns
2.3. Data Processing
2.3.1. Classification of AE, Short-Term Serious Adverse Events (SAE) and Short-Term Non-Serious Adverse Events (NSAE)
2.3.2. Definition of Mix-and-Match Method
2.4. Statistical Analysis
3. Results
3.1. Characteristics and Adverse Events (AE) Reported to Vaccine Adverse Event Reporting System (VAERS)
3.2. Reports of Adverse Events (AE) to Vaccine Adverse Event Reporting System(VAERS) by COVID-19 Booster Vaccine Recipients
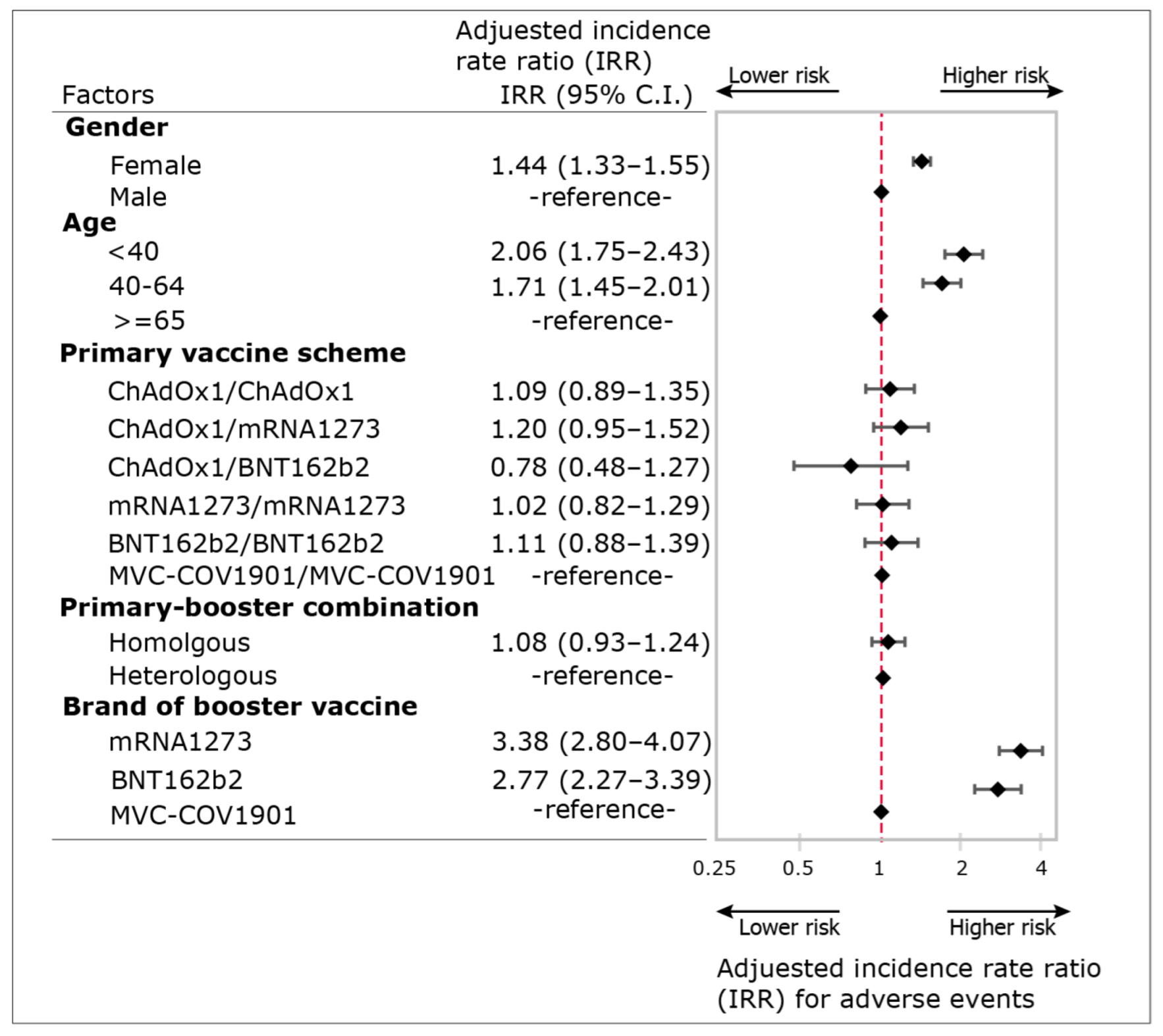
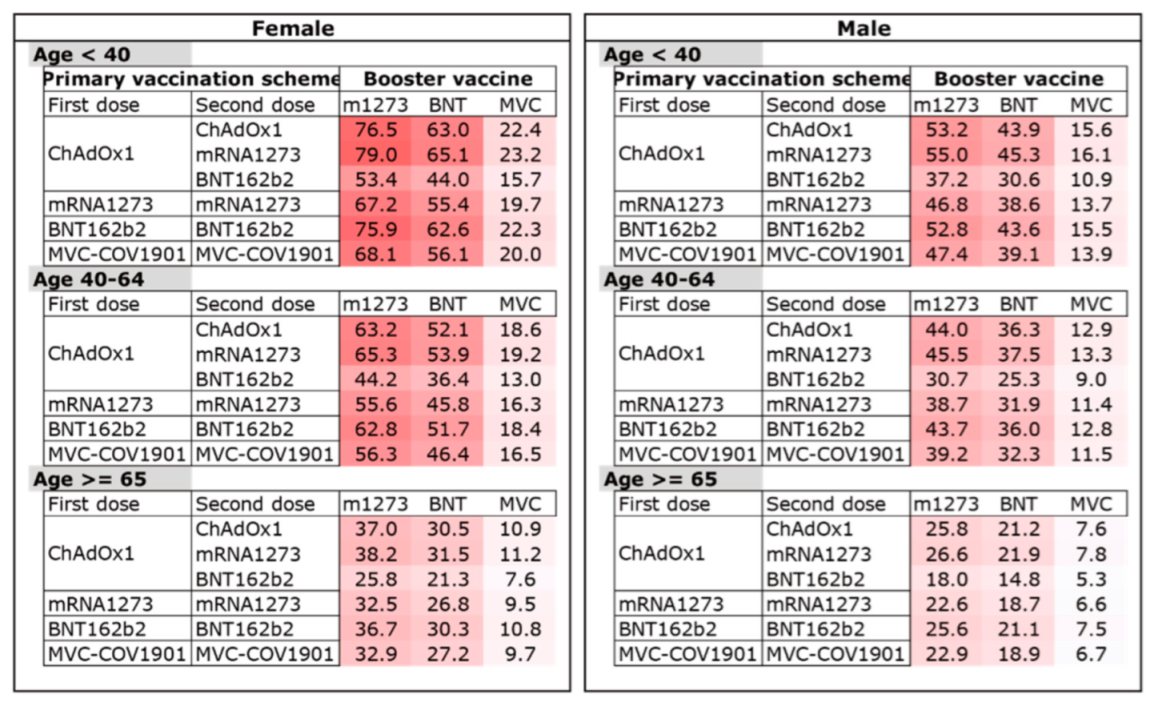
3.3. Estimated Incidence Rates (eIR) of Self-Reported Adverse Events (AE) after Booster Dose among Respondents
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Vaccine | Available Formulation | Component | Recommend Age |
|---|---|---|---|
| ChAdOx1 | 5 mL multidose vial 1 | Each dose (0.5 mL): Chimpanzee Adenovirus encoding the SARS-CoV-2 Spike glycoprotein (ChAdOx1-S), not less than 2.5 × 108 infectious units (Inf.U). List of excipients:
| ≥18 years |
| mRNA1273 | 5 mL multidose vial 1 | Each dose (0.25 mL): 50 μg of elasomeran, a COVID-19 mRNA Vaccine (embedded in SM-102 lipid nanoparticles). List of excipients:
| ≥18 years |
| BNT162b2 | 0.45 mL multidose vial 2 diluted in its original vial with 1.8 mL sodium chloride 9 mg/mL (0.9%) solution for injection | Each dose (0.3 mL): 30 μg of tozinameran, a BNT162b2 RNA (embedded in lipid nanoparticles). List of excipients:
| ≥12 years |
| MVC-COV1901 | 0.5 mL syringe. 5 mL multidose vial 1 | Each dose (0.5 mL): 15 μg of SARS-CoV 2 recombinant spike protein. List of excipients:
| ≥20 years |
References
- Saddik, B.; Al-Bluwi, N.; Shukla, A.; Barqawi, H.; Alsayed, H.A.H.; Sharif-Askari, N.S.; Temsah, M.H.; Bendardaf, R.; Hamid, Q.; Halwani, R. Determinants of healthcare workers perceptions, acceptance and choice of COVID-19 vaccines: A cross-sectional study from the United Arab Emirates. Hum. Vaccin. Immunother. 2022, 18, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Palanica, A.; Jeon, J. Initial Mix-and-Match COVID-19 Vaccination Perceptions, Concerns, and Side Effects across Canadians. Vaccines 2022, 10, 93. [Google Scholar] [CrossRef] [PubMed]
- Klein, N.P.; Lewis, N.; Goddard, K.; Fireman, B.; Zerbo, O.; Hanson, K.E.; Donahue, J.G.; Kharbanda, E.O.; Naleway, A.; Nelson, J.C.; et al. Surveillance for Adverse Events After COVID-19 mRNA Vaccination. JAMA 2021, 326, 1390–1399. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Vaccine Safety Monitoring. Available online: https://www.cdc.gov/vaccinesafety/ensuringsafety/monitoring/index.html (accessed on 5 May 2022).
- Medicines and Healthcare Products Regulatory Agency. The Yellow Card Scheme. Available online: https://yellowcard.mhra.gov.uk/ (accessed on 10 May 2022).
- Menni, C.; May, A.; Polidori, L.; Louca, P.; Wolf, J.; Capdevila, J.; Hu, C.; Ourselin, S.; Steves, C.J.; Valdes, A.M.; et al. COVID-19 vaccine waning and effectiveness and side-effects of boosters: A prospective community study from the ZOE COVID Study. Lancet Infect. Dis. 2022, 22, 1002–1010. [Google Scholar] [CrossRef]
- Paran, Y.; Saiag, E.; Spitzer, A.; Angel, Y.; Yakubovsky, M.; Padova, H.; Ben-Ami, R.; Goldinger, I.; Gamzu, R.; Sprecher, E.; et al. Short-Term Safety of Booster Immunization With BNT162b2 mRNA COVID-19 Vaccine in Healthcare Workers. Open Forum. Infect Dis. 2022, 9, ofab656. [Google Scholar] [CrossRef] [PubMed]
- Taiwan Centers for Disease Control. COVID-19 Vaccine. Available online: https://www.cdc.gov.tw/Category/Page/9jFXNbCe-sFK9EImRRi2Og (accessed on 24 May 2022).
- World Health Organization. WHO Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int/ (accessed on 20 May 2022).
- Medigen Vaccine Biologics Corporation. Clinical Development Updates on Medigen’s MVC-COV1901 in COVID-19 Solidarity Trial Vaccines. Available online: https://www.medigenvac.com/en/news_view.php?id=134 (accessed on 24 May 2022).
- Taiwan Centers for Disease Control. Vaccine Adverse Event Reporting System (VAERS). Available online: https://www.cdc.gov.tw/Category/Page/3-aXlTBq4ggn5Hg2dveHBg (accessed on 21 May 2022).
- Cascini, F.; Pantovic, A.; Al-Ajlouni, Y.; Failla, G.; Ricciardi, W. Attitudes, acceptance and hesitancy among the general population worldwide to receive the COVID-19 vaccines and their contributing factors: A systematic review. EClinicalMedicine 2021, 40, 101113. [Google Scholar] [CrossRef] [PubMed]
- Paris, C.; Benezit, F.; Geslin, M.; Polard, E.; Baldeyrou, M.; Turmel, V.; Tadie, E.; Garlantezec, R.; Tattevin, P. COVID-19 vaccine hesitancy among healthcare workers. Infect Dis. Now 2021, 51, 484–487. [Google Scholar] [CrossRef] [PubMed]
- Omeish, H.; Najadat, A.; Al-Azzam, S.; Tarabin, N.; Abu Hameed, A.; Al-Gallab, N.; Abbas, H.; Rababah, L.; Rabadi, M.; Karasneh, R.; et al. Reported COVID-19 vaccines side effects among Jordanian population: A cross sectional study. Hum. Vaccin. Immunother. 2022, 18, 1981086. [Google Scholar] [CrossRef] [PubMed]
- Atmar, R.L.; Lyke, K.E.; Deming, M.E.; Jackson, L.A.; Branche, A.R.; El Sahly, H.M.; Rostad, C.A.; Martin, J.M.; Johnston, C.; Rupp, R.E.; et al. Homologous and Heterologous Covid-19 Booster Vaccinations. N. Engl. J. Med. 2022, 386, 1046–1057. [Google Scholar] [CrossRef] [PubMed]
- Costa Clemens, S.A.; Weckx, L.; Clemens, R.; Almeida Mendes, A.V.; Ramos Souza, A.; Silveira, M.B.V.; da Guarda, S.N.F.; de Nobrega, M.M.; de Moraes Pinto, M.I.; Gonzalez, I.G.S.; et al. Heterologous versus homologous COVID-19 booster vaccination in previous recipients of two doses of CoronaVac COVID-19 vaccine in Brazil (RHH-001): A phase 4, non-inferiority, single blind, randomised study. Lancet 2022, 399, 521–529. [Google Scholar] [CrossRef]
- Menni, C.; Klaser, K.; May, A.; Polidori, L.; Capdevila, J.; Louca, P.; Sudre, C.H.; Nguyen, L.H.; Drew, D.A.; Merino, J.; et al. Vaccine side-effects and SARS-CoV-2 infection after vaccination in users of the COVID Symptom Study app in the UK: A prospective observational study. Lancet Infect. Dis. 2021, 21, 939–949. [Google Scholar] [CrossRef]
- Munro, A.P.S.; Janani, L.; Cornelius, V.; Aley, P.K.; Babbage, G.; Baxter, D.; Bula, M.; Cathie, K.; Chatterjee, K.; Dodd, K.; et al. Safety and immunogenicity of seven COVID-19 vaccines as a third dose (booster) following two doses of ChAdOx1 nCov-19 or BNT162b2 in the UK (COV-BOOST): A blinded, multicentre, randomised, controlled, phase 2 trial. Lancet 2021, 398, 2258–2276. [Google Scholar] [CrossRef]
- Meo, S.A.; Bukhari, I.A.; Akram, J.; Meo, A.S.; Klonoff, D.C. COVID-19 vaccines: Comparison of biological, pharmacological characteristics and adverse effects of Pfizer/BioNTech and Moderna Vaccines. Eur. Rev. Med. Pharmacol. Sci. 2021, 25, 1663–1669. [Google Scholar] [CrossRef] [PubMed]
- Valera-Rubio, M.M.; Sierra-Torres, M.I.M.; Castillejo Garcia, R.R.; Cordero-Ramos, J.J.; Lopez-Marquez, M.R.M.; Cruz-Salgado, O.O.; Calleja-Hernandez, M.A.M. Adverse events reported after administration of BNT162b2 and mRNA-1273 COVID-19 vaccines among hospital workers: A cross-sectional survey-based study in a Spanish hospital. Expert Rev. Vaccines 2022, 21, 533–540. [Google Scholar] [CrossRef]
- Watad, A.; De Marco, G.; Mahajna, H.; Druyan, A.; Eltity, M.; Hijazi, N.; Haddad, A.; Elias, M.; Zisman, D.; Naffaa, M.E.; et al. Immune-Mediated Disease Flares or New-Onset Disease in 27 Subjects Following mRNA/DNA SARS-CoV-2 Vaccination. Vaccines 2021, 9, 435. [Google Scholar] [CrossRef]
- Lupica, A.; Di Stefano, V.; Iacono, S.; Pignolo, A.; Quartana, M.; Gagliardo, A.; Fierro, B.; Brighina, F. Impact of COVID-19 in AChR Myasthenia Gravis and the Safety of Vaccines: Data from an Italian Cohort. Neurol. Int. 2022, 14, 406–416. [Google Scholar] [CrossRef]
- Li, Y.K.; Lui, M.P.K.; Yam, L.L.; Cheng, C.S.; Tsang, T.H.T.; Kwok, W.S.; Chung, H.Y. COVID-19 vaccination in patients with rheumatic diseases: Vaccination rates, patient perspectives, and side effects. Immun. Inflamm. Dis. 2022, 10, e589. [Google Scholar] [CrossRef]
- Du, Y.; Chen, L.; Shi, Y. Safety, Immunogenicity, and Efficacy of COVID-19 Vaccines in Adolescents, Children, and Infants: A Systematic Review and Meta-Analysis. Front. Public Health 2022, 10, 829176. [Google Scholar] [CrossRef] [PubMed]
- Lv, M.; Luo, X.; Shen, Q.; Lei, R.; Liu, X.; Liu, E.; Li, Q.; Chen, Y. Safety, Immunogenicity, and Efficacy of COVID-19 Vaccines in Children and Adolescents: A Systematic Review. Vaccines 2021, 9, 1102. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.W.; Sa, S.; Hong, M.; Kim, J.; Shim, S.R.; Han, H.W. Adverse Events and Safety Profile of the COVID-19 Vaccines in Adolescents: Safety Monitoring for Adverse Events Using Real-World Data. Vaccines 2022, 10, 744. [Google Scholar] [CrossRef] [PubMed]
- Taiwan Food and Drug Administration. Information on COVID-19 Vaccines for Approval of Specific Medical Products’ Manufacturing or Importing. Available online: https://www.fda.gov.tw/TC/siteList.aspx?sid=11845 (accessed on 26 May 2022).

| Primary Vaccine | Booster Dose | Type of Primary-Booster Combination | |
|---|---|---|---|
| 1st Dose | 2nd Dose | 3rd Dose | |
| mRNA1273 | mRNA1273 | mRNA1273 | Homologous booster |
| mRNA1273 | ChAdOx1 | ChAdOx1 | Homologous booster |
| mRNA1273 | ChAdOx1 | mRNA1273 | Heterologous booster |
| ChAdOx1 | ChAdOx1 | mRNA1273 | Heterologous booster |
| ChAdOx1 | mRNA1273 | MVC-COV1901 | Heterologous booster |
| No. of Respondents | Occurrence of Any Adverse Event | ||||
|---|---|---|---|---|---|
| Factors | Count | (%) | Count | Incidence Rate per 100 Respondents (95% C.I.) | p-Value 2 |
| Overall | 7382 | (100.0) | 3852 | 52.2 (51.0–53.3) | |
| Gender | <0.001 | ||||
| Female | 4921 | (66.7) | 2908 | 59.0 (57.6–60.3) | |
| Male | 2461 | (33.3) | 944 | 38.2 (36.3–40.2) | |
| Age group | <0.001 | ||||
| <40 | 3011 | (40.8) | 1863 | 61.9 (60.1–63.6) | |
| <65 | 3751 | (50.8) | 1826 | 48.7 (47.1–50.3) | |
| ≥65 | 620 | (8.4) | 163 | 26.3 (23.0–29.9) | |
| Primary vaccination scheme | <0.001 | ||||
| ChAdOx1/ChAdOx1 | 4407 | (59.7) | 2403 | 54.5 (53.1–56.0) | |
| ChAdOx1/mRNA1273 | 515 | (7.0) | 332 | 64.5 (60.2–68.5) | |
| ChAdOx1/BNT162b2 | 48 | (0.7) | 19 | 39.6 (26.9–53.9) | |
| mRNA1273/mRNA1273 | 1438 | (19.5) | 671 | 46.7 (44.1–49.2) | |
| BNT162b2/BNT162b2 | 550 | (7.5) | 313 | 56.9 (52.7–61.0) | |
| MVC-COV1901/MVC-COV1901 | 424 | (5.7) | 114 | 26.9 (22.9–31.3) | |
| Type of primary-booster combination 1 | <0.001 | ||||
| Homologous booster vaccination | 2138 | (29.0) | 1016 | 47.5 (45.4–49.6) | |
| Heterologous booster vaccination | 5244 | (71.0) | 2836 | 54.1 (52.7–55.4) | |
| Type and brand of booster vaccine | <0.001 | ||||
| RNA-based | 6556 | (88.8) | 3718 | 56.7 (55.5–57.9) | |
| mRNA1273 | 5374 | (72.8) | 3156 | 58.7 (57.4–60.0) | |
| BNT162b2 | 1182 | (16.0) | 562 | 47.5 (44.7–50.4) | |
| Protein subunit | |||||
| MVC-COV1901 | 826 | (11.2) | 134 | 16.2 (13.9–18.9) | |
| Overall (n = 7382) | mRNA1273 (n = 5374) | BNT162b2 (n = 1182) | MVC-COV1901 (n = 826) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Count 1 | IR 2 (%) | Count 1 | IR 2 (%) | Count 1 | IR 2 (%) | Count 1 | IR 2 (%) | p-Value 3 | |
| Total no. of any adverse events | 3852 | 52.2 | 3156 | 58.7 | 562 | 47.5 | 134 | 16.2 | <0.001 |
| Serious adverse events (SAE) | 174 | 2.4 | 121 | 2.3 | 40 | 3.4 | 13 | 1.6 | 0.019 |
| Cardiac symptoms | 116 | 1.6 | 79 | 1.5 | 30 | 2.5 | 7 | 0.8 | 0.006 |
| Chest pain | 81 | 1.1 | 52 | 1.0 | 26 | 2.2 | 3 | 0.4 | <0.001 |
| Short of breath | 49 | 0.7 | 38 | 0.7 | 7 | 0.6 | 4 | 0.5 | 0.72 |
| Systematic allergic reactions | 64 | 0.9 | 45 | 0.8 | 12 | 1.0 | 7 | 0.8 | 0.83 |
| Non-serious adverse events (NSAE) | 3831 | 51.9 | 3147 | 58.6 | 557 | 47.1 | 127 | 15.4 | <0.001 |
| Local reactions | 3483 | 47.2 | 2916 | 54.3 | 486 | 41.1 | 81 | 9.8 | <0.001 |
| Flu like symptoms | |||||||||
| Tiredness | 2393 | 32.4 | 2018 | 37.6 | 323 | 27.3 | 52 | 6.3 | <0.001 |
| Headache | 1482 | 20.1 | 1245 | 23.2 | 208 | 17.6 | 29 | 3.5 | <0.001 |
| Fever | 1319 | 17.9 | 1163 | 21.6 | 147 | 12.4 | 9 | 1.1 | <0.001 |
| Chillness | 139 | 1.9 | 117 | 2.2 | 21 | 1.8 | 1 | 0.1 | <0.001 |
| Cardiac symptoms | |||||||||
| Palpitation | 78 | 1.1 | 46 | 0.9 | 24 | 2.0 | 8 | 1.0 | 0.002 |
| Gastrointestinal symptoms | |||||||||
| Nausea | 66 | 0.9 | 56 | 1.0 | 8 | 0.7 | 2 | 0.2 | 0.052 |
| Muscle/joint pain | 374 | 5.1 | 307 | 5.7 | 56 | 4.7 | 11 | 1.3 | <0.001 |
| Menstrual problems | 12 | 0.2 | 9 | 0.2 | 1 | 0.1 | 2 | 0.2 | 0.68 |
| Others | 288 | 3.9 | 193 | 3.6 | 63 | 5.3 | 32 | 3.9 | 0.02 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, P.-Y.; Wu, B.-J.; Su, M.-C.; Lin, Y.-H.; Chiang, S.-C.; Wu, J.-C.; Chen, T.-J.; Chen, Y.-C. Risk Factors and Incidence Rates of Self-Reported Short-Term Adverse Events of COVID-19 Vaccine Booster Dose. Vaccines 2022, 10, 1115. https://doi.org/10.3390/vaccines10071115
Chen P-Y, Wu B-J, Su M-C, Lin Y-H, Chiang S-C, Wu J-C, Chen T-J, Chen Y-C. Risk Factors and Incidence Rates of Self-Reported Short-Term Adverse Events of COVID-19 Vaccine Booster Dose. Vaccines. 2022; 10(7):1115. https://doi.org/10.3390/vaccines10071115
Chicago/Turabian StyleChen, Po-Yu, Bih-Ju Wu, Mei-Chin Su, Yen-Hsi Lin, Shu-Chiung Chiang, Jau-Ching Wu, Tzeng-Ji Chen, and Yu-Chun Chen. 2022. "Risk Factors and Incidence Rates of Self-Reported Short-Term Adverse Events of COVID-19 Vaccine Booster Dose" Vaccines 10, no. 7: 1115. https://doi.org/10.3390/vaccines10071115
APA StyleChen, P.-Y., Wu, B.-J., Su, M.-C., Lin, Y.-H., Chiang, S.-C., Wu, J.-C., Chen, T.-J., & Chen, Y.-C. (2022). Risk Factors and Incidence Rates of Self-Reported Short-Term Adverse Events of COVID-19 Vaccine Booster Dose. Vaccines, 10(7), 1115. https://doi.org/10.3390/vaccines10071115









