Transmission of H9N2 Low Pathogenicity Avian Influenza Virus (LPAIV) in a Challenge-Transmission Model
Abstract
:1. Introduction
2. Materials and Methods
2.1. Chickens
2.2. Virus Propagation and Infectious Dose
2.3. Experimental Design
2.4. Virus Isolation and Processing of Swab Samples
2.5. Hemagglutination Inhibition (HI) Assay
2.6. Statistical Analysis
3. Results
3.1. H9N2 AIV Infection within the Inoculated Seeder Groups
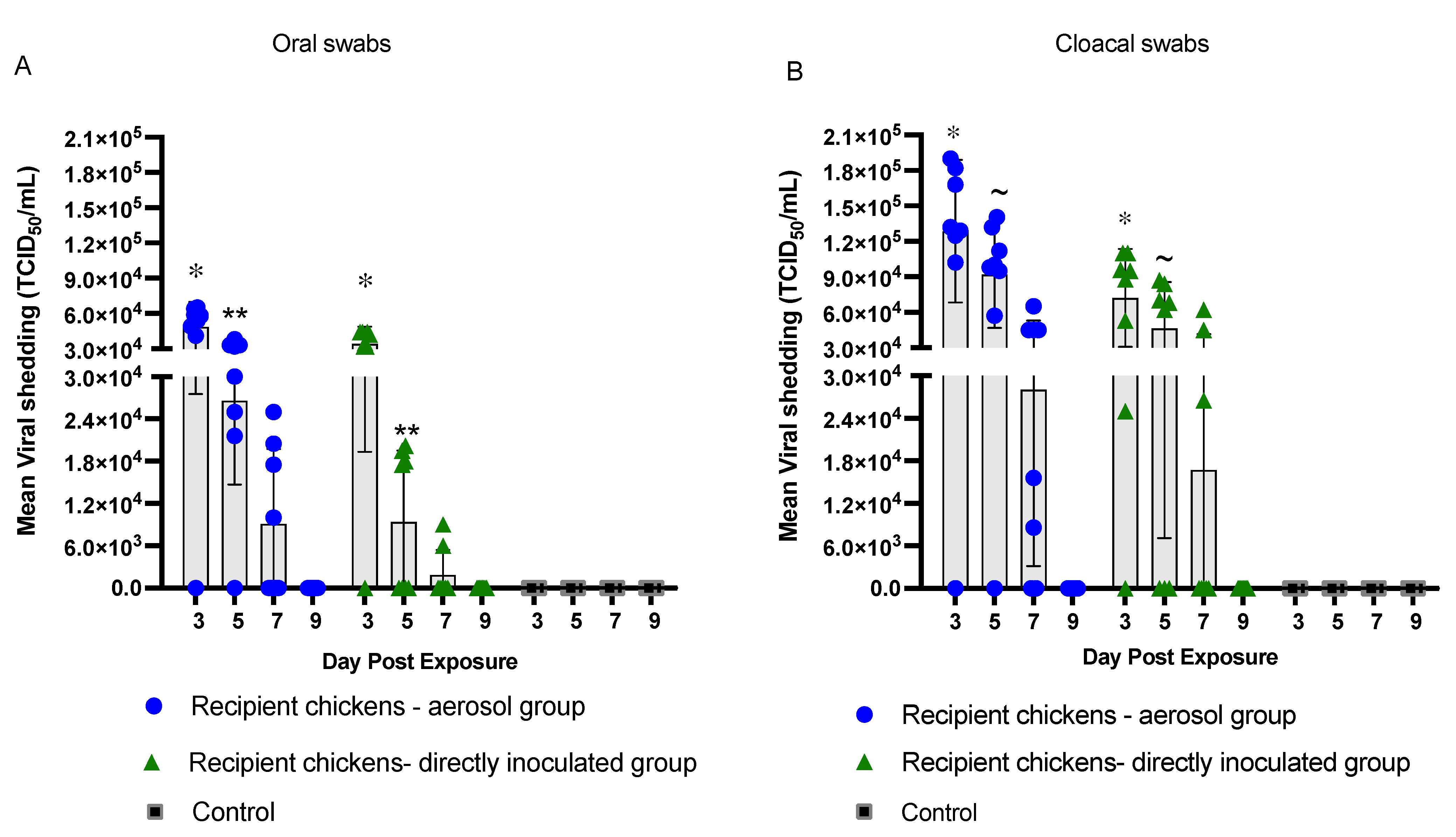
3.2. Transmission of H9N2 AIV in Recipient Chickens
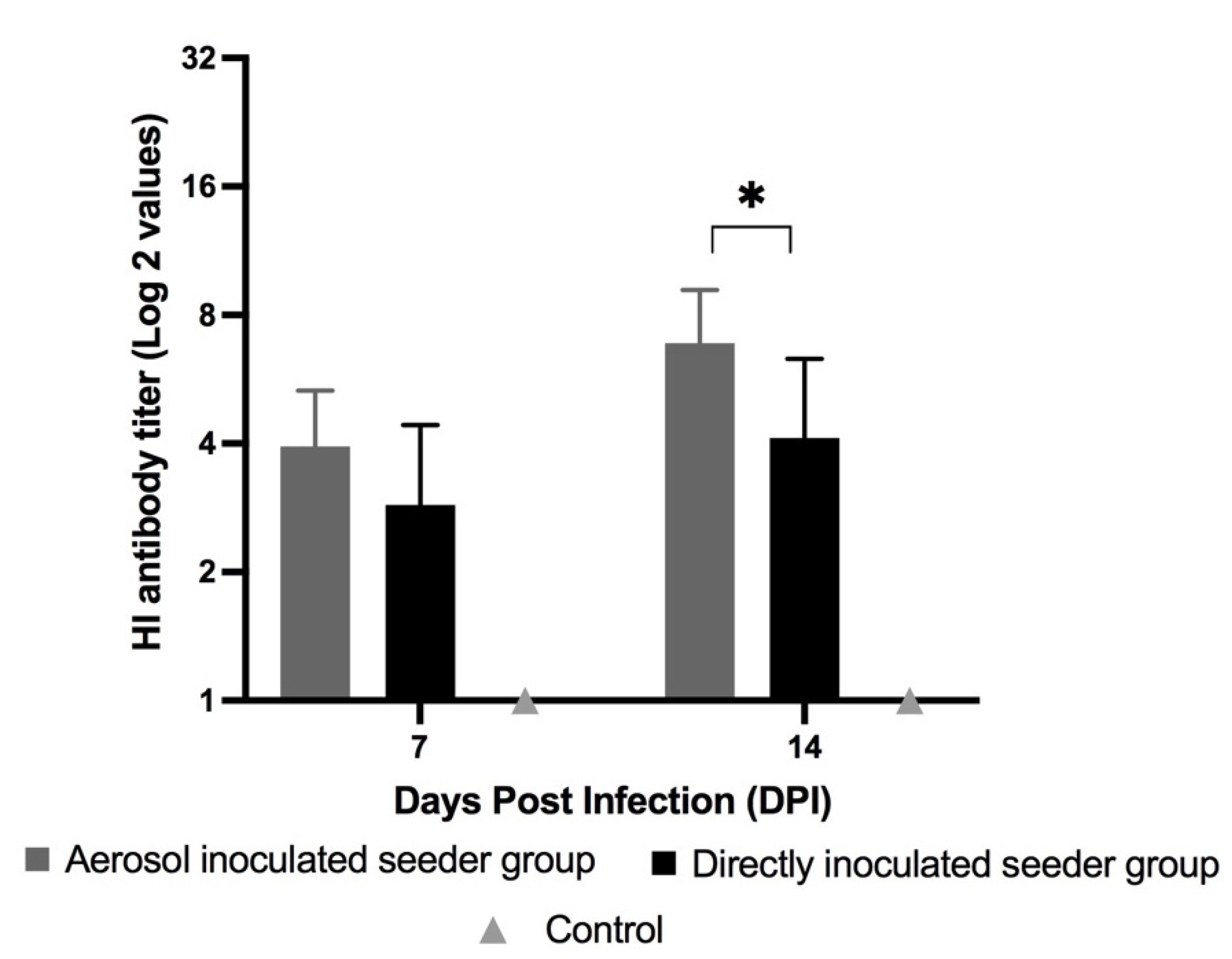
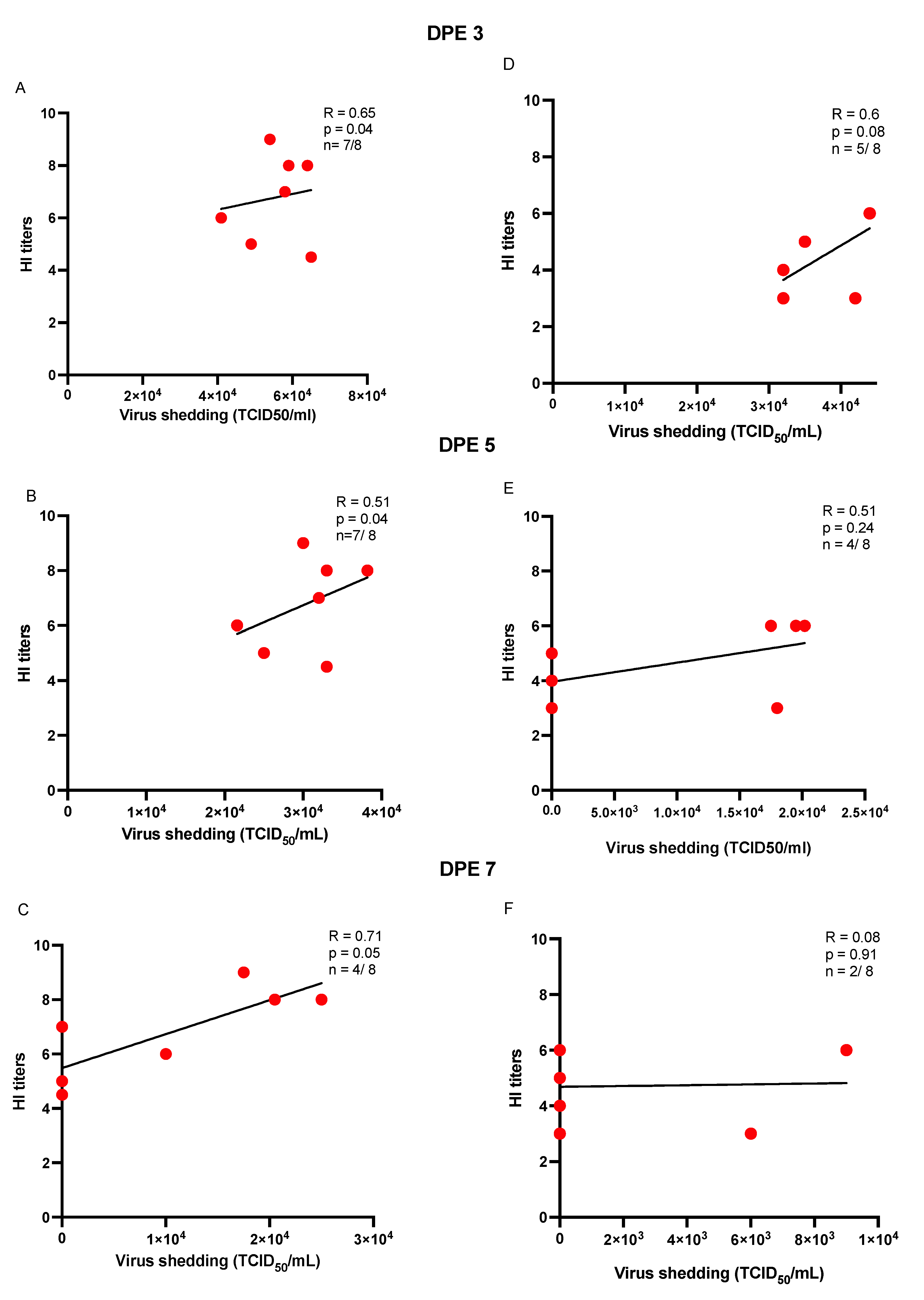
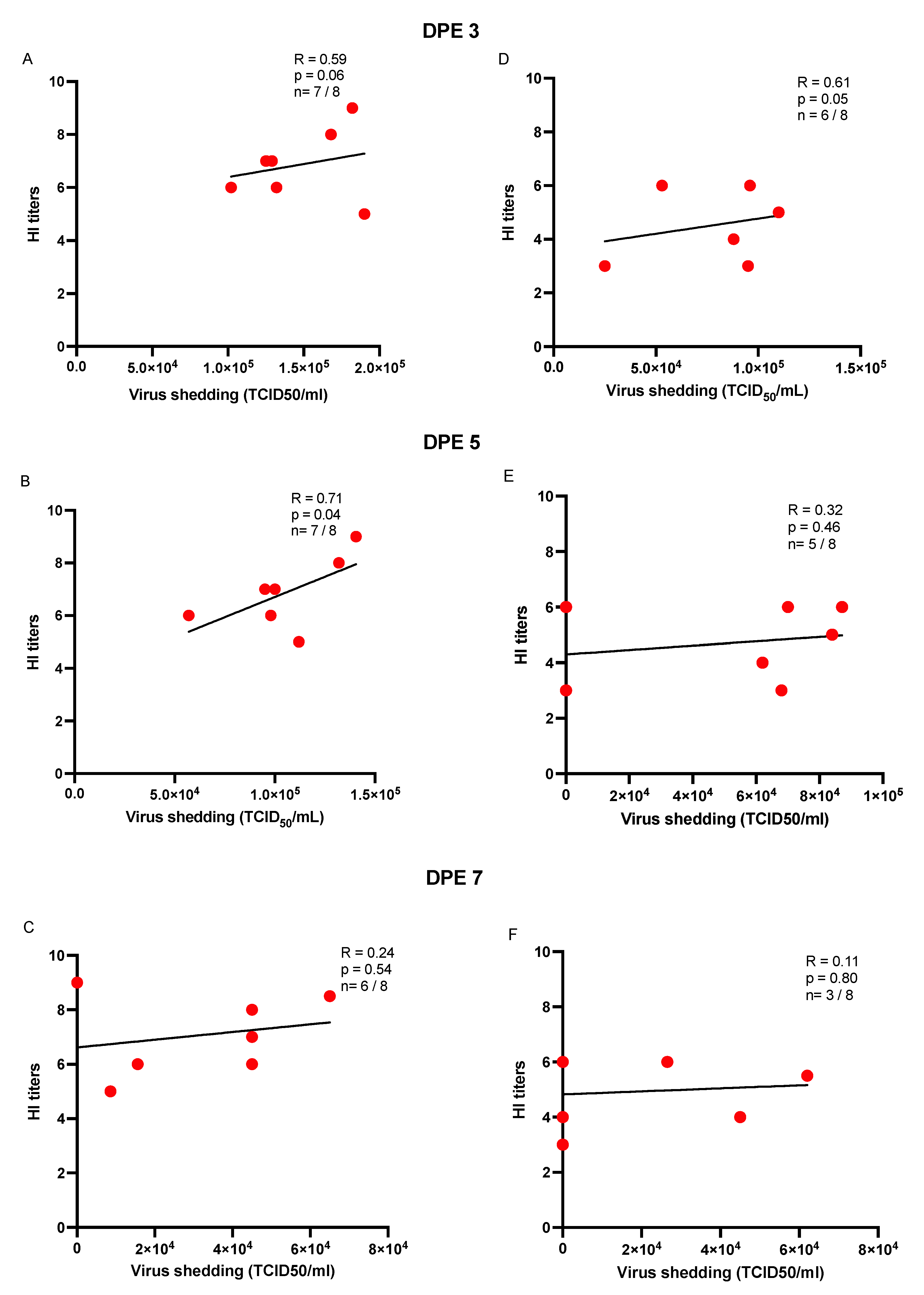
3.3. HI Antibody Titers, Seroconversion and Seroprotection
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- St Paul, M.; Mallick, A.I.; Read, L.R.; Villanueva, A.I.; Parvizi, P.; Abdul-Careem, M.F.; Nagy, É.; Sharif, S. Prophylactic treatment with Toll-like receptor ligands enhances host immunity to avian influenza virus in chickens. Vaccine 2012, 30, 4524–4531. [Google Scholar] [CrossRef] [PubMed]
- Dhama, K.; Chauhan, R.S.; Kataria, J.M.; Mahendran, M.; Tomar, S. Avian Influenza: The Current Perspectives. J. Immunol. Immunopathol. 2005, 7, 1–33. [Google Scholar]
- Nagy, A.; Mettenleiter, T.C.; Abdelwhab, E.M. A brief summary of the epidemiology and genetic relatedness of avian influenza H9N2 virus in birds and mammals in the Middle East and North Africa. Epidemiol. Infect. 2017, 145, 3320–3333. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alexander, D.J. An overview of the epidemiology of avian influenza. Vaccine 2007, 25, 5637–5644. [Google Scholar] [CrossRef]
- Nili, H.; Asasi, K. Natural cases and an experimental study of H9N2 avian influenza in commercial broiler chickens of Iran. Avian Pathol. 2002, 31, 247–252. [Google Scholar] [CrossRef]
- Perdue, M.L.; Swayne, D.E. Public Health Risk from Avian Influenza Viruses. Avian Dis. 2005, 49, 317–327. [Google Scholar] [CrossRef]
- Heidari, A.; Righetto, I.; Filippini, F. Electrostatic Variation of Haemagglutinin as a Hallmark of the Evolution of Avian Influenza Viruses. Sci. Rep. 2018, 8, 1929. [Google Scholar] [CrossRef] [Green Version]
- Zanaty, A.M.; Erfan, A.M.; Mady, W.H.; Amer, F.; Nour, A.A.; Rabie, N.; Samy, M.; Selim, A.A.; Hassan, W.M.M.; Naguib, M.M. Avian influenza virus surveillance in migratory birds in Egypt revealed a novel reassortant H6N2 subtype. Avian Res. 2019, 10, 41. [Google Scholar] [CrossRef] [Green Version]
- Ma, M.-J.; Zhao, T.; Chen, S.-H.; Xia, X.; Yang, X.-X.; Wang, G.-L.; Fang, L.-Q.; Ma, G.-Y.; Wu, M.-N.; Qian, Y.-H.; et al. Avian Influenza A Virus Infection among Workers at Live Poultry Markets, China, 2013–2016. Emerg. Infect. Dis. J. 2018, 24, 1246–1256. [Google Scholar] [CrossRef]
- WHO. WHO|Weekly Epidemiological Record, 24 March 2017; WHO: Geneva, Switzerland, 2017; Volume 92, pp. 129–144. Available online: http://www.who.int/wer/2017/wer9212/en/ (accessed on 28 April 2017).
- Cáceres, C.J.; Rajao, D.S.; Perez, D.R. Airborne Transmission of Avian Origin H9N2 Influenza A Viruses in Mammals. Viruses 2021, 13, 1919. [Google Scholar] [CrossRef]
- WHO. WHO|Avian Influenza Weekly Update Number 817; WHO: Geneva, Switzerland, 2021; pp. 1–4. Available online: https://www.who.int/docs/default-source/wpro--- (accessed on 16 April 2021).
- Wang, J.; Wu, M.; Hong, W.; Fan, X.; Chen, R.; Zheng, Z.; Zeng, Y.; Huang, R.; Zhang, Y.; Lam, T.T.-Y.; et al. Infectivity and Transmissibility of Avian H9N2 Influenza Viruses in Pigs. J. Virol. 2016, 90, 3506–3514. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Righetto, I.; Filippini, F. Normal modes analysis and surface electrostatics of haemagglutinin proteins as fingerprints for high pathogenic type A influenza viruses. BMC Bioinform. 2020, 21, 354. [Google Scholar] [CrossRef]
- Sun, X.; Belser, J.A.; Maines, T.R. Adaptation of H9N2 Influenza Viruses to Mammalian Hosts: A Review of Molecular Markers. Viruses 2020, 12, 541. [Google Scholar] [CrossRef] [PubMed]
- Guan, J.; Fu, Q.; Chan, M.; Spencer, J.L. Aerosol transmission of an avian influenza H9N2 virus with a tropism for the respiratory tract of chickens. Avian Dis. 2013, 57, 645–649. [Google Scholar] [CrossRef] [PubMed]
- Sang, X.; Wang, A.; Ding, J.; Kong, H.; Gao, X.; Li, L.; Chai, T.; Li, Y.; Zhang, K.; Wang, C.; et al. Adaptation of H9N2 AIV in guinea pigs enables efficient transmission by direct contact and inefficient transmission by respiratory droplets. Sci. Rep. 2015, 5, 15928. [Google Scholar] [CrossRef] [Green Version]
- Sergeev, A.A.; Demina, O.K.; Pyankov, O.V.; Pyankova, O.G.; Agafonov, A.P.; Kiselev, S.A.; Agranovski, I.E.; Sergeev, A.A.; Shikov, A.N.; Shishkina, L.N.; et al. Infection of Chickens Caused by Avian Influenza Virus A/H5N1 Delivered by Aerosol and Other Routes. Transbound. Emerg. Dis. 2013, 60, 159–165. [Google Scholar] [CrossRef]
- Sun, Y.; Bi, Y.; Pu, J.; Hu, Y.; Wang, J.; Gao, H.; Liu, L.; Xu, Q.; Tan, Y.; Liu, M.; et al. Guinea Pig Model for Evaluating the Potential Public Health Risk of Swine and Avian Influenza Viruses. PLoS ONE 2010, 5, e15537. [Google Scholar] [CrossRef] [Green Version]
- Reed, L.J.; Muench, H. A Simple method of estimating fifty per cent endpoints. Am. J. Epidemiol. 1938, 27, 493–497. [Google Scholar] [CrossRef]
- Swayne, D.E.; Slemons, R.D. Using Mean Infectious Dose of High- and Low-Pathogenicity Avian Influenza Viruses Originating from Wild Duck and Poultry as One Measure of Infectivity and Adaptation to Poultry. Avian Dis. 2008, 52, 455–460. [Google Scholar] [CrossRef]
- Ku, K.B.; Park, E.H.; Yum, J.; Kim, H.M.; Kang, Y.M.; Kim, J.C.; Kim, J.A.; Kim, H.S.; Seo, S.H. Transmissibility of novel H7N9 and H9N2 avian influenza viruses between chickens and ferrets. Virology 2014, 450–451, 316–323. [Google Scholar] [CrossRef] [Green Version]
- Tumpey, T.M.; Kapczynski, D.R.; Swayne, D.E. Comparative Susceptibility of Chickens and Turkeys to Avian Influenza A H7N2 Virus Infection and Protective Efficacy of a Commercial Avian Influenza H7N2 Virus Vaccine. Avian Dis. 2004, 48, 167–176. [Google Scholar] [CrossRef] [PubMed]
- Abdul-Careem, M.F.; Javaheri-Vayeghan, A.; Shanmuganathan, S.; Haghighi, H.R.; Read, L.R.; Haq, K.; Hunter, D.B.; Schat, K.A.; Heidari, M.; Sharif, S. Establishment of an Aerosol-Based Marek’s Disease Virus Infection Model. Avian Dis. 2009, 53, 387–391. [Google Scholar] [CrossRef] [PubMed]
- Hauck, R.; Crossley, B.; Rejmanek, D.; Zhou, H.; Gallardo, R.A. Persistence of Highly Pathogenic and Low Pathogenic Avian Influenza Viruses in Footbaths and Poultry Manure. Avian Dis. 2017, 61, 64–69. [Google Scholar] [CrossRef] [PubMed]
- WHO. Manual for the Laboratory Diagnosis and Virological Surveillance of Influenza; World Health Organization: Geneva, Switzerland, 2011. [Google Scholar]
- Singh, S.M.; Alkie, T.N.; Hodgins, D.C.; Nagy, É.; Shojadoost, B.; Sharif, S. Systemic immune responses to an inactivated, whole H9N2 avian influenza virus vaccine using class B CpG oligonucleotides in chickens. Vaccine 2015, 33, 3947–3952. [Google Scholar] [CrossRef]
- Peacock, T.P.; James, J.; Sealy, J.E.; Iqbal, M. A Global Perspective on H9N2 Avian Influenza Virus. Viruses 2019, 11, 620. [Google Scholar] [CrossRef] [Green Version]
- Chen, J.; Fang, F.; Yang, Z.; Liu, X.; Zhang, H.; Zhang, Z.; Zhang, X.; Chen, Z. Characterization of highly pathogenic H5N1 avian influenza viruses isolated from poultry markets in central China. Virus Res. 2009, 146, 19–28. [Google Scholar] [CrossRef]
- Swayne, D.E.; Pantin-Jackwood, M. Pathogenicity of avian influenza viruses in poultry. Dev. Biol. 2006, 124, 61–67. [Google Scholar]
- Iqbal, M.; Yaqub, T.; Mukhtar, N.; Shabbir, M.Z.; McCauley, J.W. Infectivity and transmissibility of H9N2 avian influenza virus in chickens and wild terrestrial birds. Vet. Res. 2013, 44, 100. [Google Scholar] [CrossRef] [Green Version]
- Ruiz-Hernandez, R.; Mwangi, W.; Peroval, M.; Sadeyen, J.-R.; Ascough, S.; Balkissoon, D.; Staines, K.; Boyd, A.; McCauley, J.; Smith, A.; et al. Host genetics determine susceptibility to avian influenza infection and transmission dynamics. Sci. Rep. 2016, 6, 26787. [Google Scholar] [CrossRef] [Green Version]
- Yao, M.; Lv, J.; Huang, R.; Yang, Y.; Chai, T. Determination of Infective Dose of H9N2 Avian Influenza Virus in Different Routes: Aerosol, Intranasal, and Gastrointestinal. Intervirology 2014, 57, 369–374. [Google Scholar] [CrossRef]
- Costa, T.; Chaves, A.J.; Valle, R.; Darji, A.; van Riel, D.; Kuiken, T.; Majó, N.; Ramis, A. Distribution patterns of influenza virus receptors and viral attachment patterns in the respiratory and intestinal tracts of seven avian species. Vet. Res. 2012, 43, 28. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- França, M.; Poulson, R.; Brown, J.; Howerth, E.W.; Berghaus, R.D.; Carter, D.; Stallknecht, D.E. Effect of Different Routes of Inoculation on Infectivity and Viral Shedding of LPAI Viruses in Mallards. Avian Dis. 2012, 56, 981–985. [Google Scholar] [CrossRef] [PubMed]
- Smith, J.H.; Brooks, P.; Johnson, S.; Tompkins, S.M.; Custer, K.M.; Haas, D.L.; Mair, R.; Papania, M.; Tripp, R.A. Aerosol vaccination induces robust protective immunity to homologous and heterologous influenza infection in mice. Vaccine 2011, 29, 2568–2575. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Leung, N.H.L. Transmissibility and transmission of respiratory viruses. Nat. Rev. Microbiol. 2021, 19, 528–545. [Google Scholar] [CrossRef]
- Yee, K.S.; Carpenter, T.E.; Farver, T.B.; Cardona, C.J. An evaluation of transmission routes for low pathogenicity avian influenza virus among chickens sold in live bird markets. Virology 2009, 394, 19–27. [Google Scholar] [CrossRef] [Green Version]
- Meijer, A.; van der Goot, J.A.; Koch, G.; van Boven, M.; Kimman, T.G. Oseltamivir reduces transmission, morbidity, and mortality of highly pathogenic avian influenza in chickens. Int. Congr. Ser. 2004, 1263, 495–498. [Google Scholar] [CrossRef]
- Zhou, J.; Wu, J.; Zeng, X.; Huang, G.; Zou, L.; Song, Y.; Gopinath, D.; Zhang, X.; Kang, M.; Lin, J.; et al. Isolation of H5N6, H7N9 and H9N2 avian influenza A viruses from air sampled at live poultry markets in China, 2014 and 2015. Eurosurveillance 2016, 21, 30331. [Google Scholar] [CrossRef] [Green Version]
- Barjesteh, N.; Alkie, T.N.; Hodgins, D.C.; Nagy, É.; Sharif, S. Local Innate Responses to TLR Ligands in the Chicken Trachea. Viruses 2016, 8, 207. [Google Scholar] [CrossRef] [Green Version]
- Lam, J.H.; Baumgarth, N. The Multifaceted B Cell Response to Influenza Virus. J. Immunol. 2019, 202, 351–359. [Google Scholar] [CrossRef] [Green Version]
- Guan, J.; Fu, Q.; Sharif, S. Replication of an H9N2 Avian Influenza Virus and Cytokine Gene Expression in Chickens Exposed by Aerosol or Intranasal Routes. Avian Dis. 2015, 59, 263–268. [Google Scholar] [CrossRef]
- Smialek, M.; Tykalowski, B.; Stenzel, T.; Koncicki, A. Local immunity of the respiratory mucosal system in chickens and turkeys. Pol. J. Vet. Sci. Wars. 2011, 14, 291–297. [Google Scholar]
- Takaoka, A.; Taniguchi, T. New aspects of IFN-α/β signalling in immunity, oncogenesis and bone metabolism. Cancer Sci. 2003, 94, 405–411. [Google Scholar] [CrossRef] [PubMed] [Green Version]


| No. of Swabs Positive/No. of Swabs Tested | ||||
|---|---|---|---|---|
| Swabs (DPI) | Aerosol | Direct Inoculation | ||
| Oral | Birds positive | Mean 1 | Birds positive | Mean 1 |
| 3 | 15/16 | 1.20 × 105 | 14/16 | 7.10 × 104 |
| 5 | 13/16 | 3.60 × 104 | 12/16 | 1.50 × 104 |
| 7 | 10/16 | 1.10 × 104 | 9/16 | 2.00 × 103 |
| 9 | 6/16 | 3.50 × 102 | 0/16 | - |
| Cloacal | Birds positive | Mean 1 | Birds positive | Mean 1 |
| 3 | 15/16 | 4.40 × 105 | 11/16 | 2.40 × 105 |
| 5 | 12/16 | 1.80 × 105 | 10/16 | 9.80 × 104 |
| 7 | 10/16 | 2.80 × 104 | 5/16 | 1.20 × 104 |
| 9 | 8/16 | 1.50 × 103 | 0/16 | - |
| No. of Swabs Positive/No. of Swabs Tested | ||||
|---|---|---|---|---|
| Swabs (PE) | Aerosol | Direct Contact | ||
| Oral | Birds positive | Mean 1 | Birds positive | Mean 1 |
| 3 | 7/8 | 4.80 × 104 | 5/8 | 3.4 × 104 |
| 5 | 7/8 | 2.60 × 104 | 4/8 | 9.4 × 103 |
| 7 | 4/8 | 9.10 × 103 | 2/8 | 1.8 × 103 |
| 9 | 0/8 | - | 0/8 | - |
| Cloacal | Birds positive | Mean 1 | Birds positive | Mean 1 |
| 3 | 7/8 | 1.30 × 105 | 6/8 | 7.30 × 104 |
| 5 | 7/8 | 9.20 × 104 | 4/8 | 4.60 × 104 |
| 7 | 6/8 | 2.80 × 104 | 3/8 | 1.60 × 104 |
| 9 | 0/8 | - | 0/8 | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Raj, S.; Astill, J.; Alqazlan, N.; Boodhoo, N.; Hodgins, D.C.; Nagy, É.; Mubareka, S.; Karimi, K.; Sharif, S. Transmission of H9N2 Low Pathogenicity Avian Influenza Virus (LPAIV) in a Challenge-Transmission Model. Vaccines 2022, 10, 1040. https://doi.org/10.3390/vaccines10071040
Raj S, Astill J, Alqazlan N, Boodhoo N, Hodgins DC, Nagy É, Mubareka S, Karimi K, Sharif S. Transmission of H9N2 Low Pathogenicity Avian Influenza Virus (LPAIV) in a Challenge-Transmission Model. Vaccines. 2022; 10(7):1040. https://doi.org/10.3390/vaccines10071040
Chicago/Turabian StyleRaj, Sugandha, Jake Astill, Nadiyah Alqazlan, Nitish Boodhoo, Douglas C. Hodgins, Éva Nagy, Samira Mubareka, Khalil Karimi, and Shayan Sharif. 2022. "Transmission of H9N2 Low Pathogenicity Avian Influenza Virus (LPAIV) in a Challenge-Transmission Model" Vaccines 10, no. 7: 1040. https://doi.org/10.3390/vaccines10071040
APA StyleRaj, S., Astill, J., Alqazlan, N., Boodhoo, N., Hodgins, D. C., Nagy, É., Mubareka, S., Karimi, K., & Sharif, S. (2022). Transmission of H9N2 Low Pathogenicity Avian Influenza Virus (LPAIV) in a Challenge-Transmission Model. Vaccines, 10(7), 1040. https://doi.org/10.3390/vaccines10071040







