Supporting Immunization Uptake during a Pandemic, Using Remote Phone Call Intervention among Babies Discharged from a Special Neonatal Care Unit (SNCU) in South India
Abstract
1. Introduction
2. Methods
2.1. Study Sites
2.2. Study Participants
2.3. Study Procedures
3. Findings
3.1. Sociodemographic Characteristics
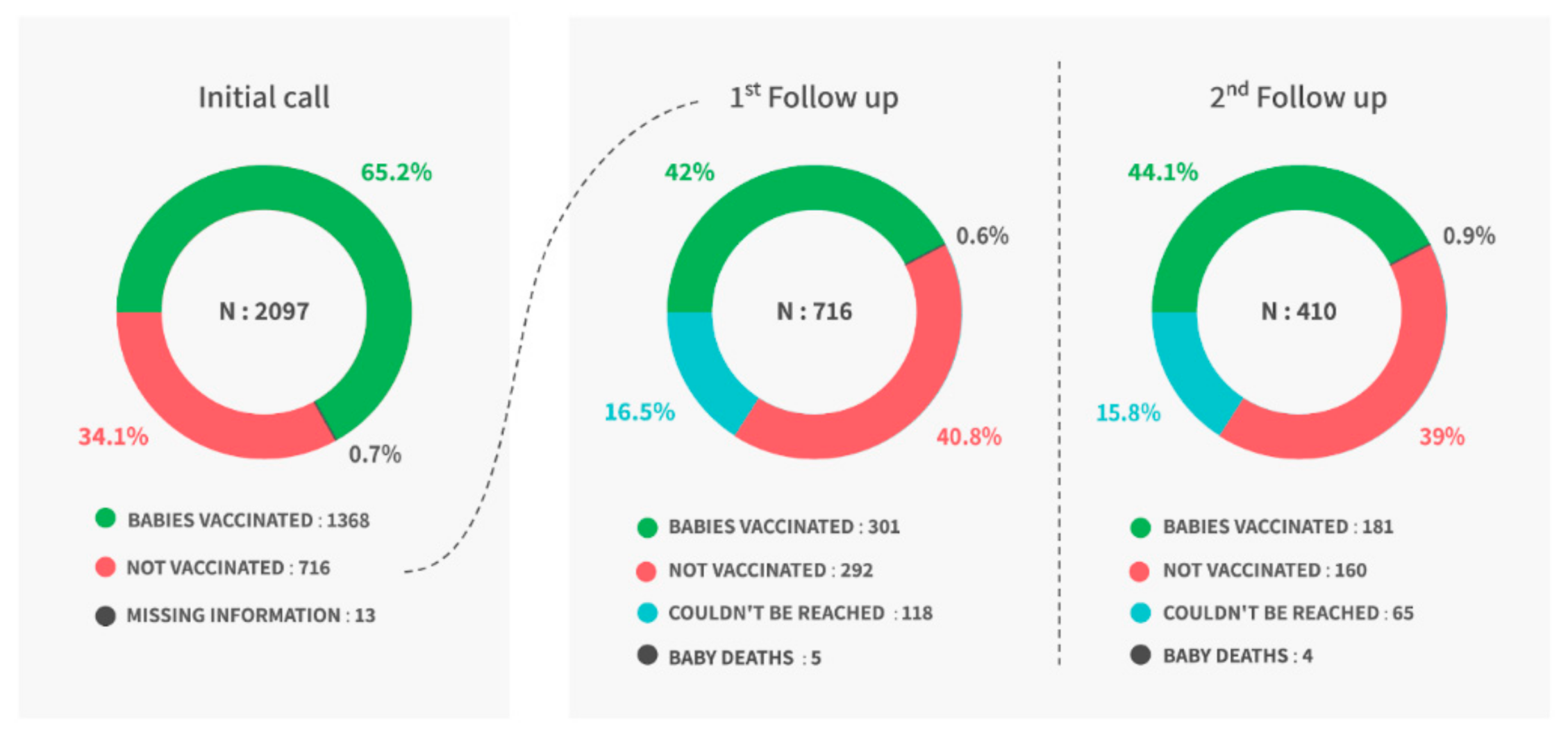
3.2. Immunization Coverage
3.3. Post Call Change in Immunization Uptake
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization Immunization Coverage. Available online: https://www.who.int/en/news-room/fact-sheets/detail/immunization-coverage (accessed on 5 October 2020).
- United Nations Children Funds (UNICEF) Child Mortality and COVID-19. Available online: https://data.unicef.org/topic/child-survival/covid-19/ (accessed on 10 March 2021).
- World Health Organization WHO. MDG 4: Reduce Child Mortality. Available online: https://www.who.int/topics/millennium_development_goals/child_mortality/en/ (accessed on 8 February 2021).
- United Nations Children Funds (UNICEF). Newborn and Child Health: Let’s Ensure Newborns Survive and Thrive. Available online: https://www.unicef.org/india/what-we-do/newborn-and-child-health (accessed on 11 October 2021).
- Vakili, R.; Hashemi, A.G.; Khademi, G.; Abbasi, M.A.; Saeidi, M. Immunization Coverage in WHO Regions: A Review Article. Int. J. Pediatrics 2015, 3, 111–118. [Google Scholar]
- Laxminarayan, R.; Ganguly, N.K. India’s Vaccine Deficit: Why More than Half of Indian Children Are Not Fully Immunized, and What Can—And Should—Be Done. Health Aff. Proj. Hope 2011, 30, 1096–1103. [Google Scholar] [CrossRef] [PubMed]
- Vashishtha, V.M.; Kumar, P. 50 Years of Immunization in India: Progress and Future. Indian Pedia 2013, 50, 111–118. [Google Scholar] [CrossRef] [PubMed]
- Newtonraj, A. India’s Fight against Vaccine-Preventable Diseases; Newer Changes and Challenges. J. Med. Soc. 2019, 33, 64–65. [Google Scholar] [CrossRef]
- Palanisamy, B.; Gopichandran, V.; Kosalram, K. Social Capital, Trust in Health Information, and Acceptance of Measles-Rubella Vaccination Campaign in Tamil Nadu: A Case-Control Study. J. Postgrad. Med. 2018, 64, 212–219. [Google Scholar] [CrossRef] [PubMed]
- Kasi, S.G.; Dhir, S.K.; Verma, S.; Pemde, H.K.; Balasubramanian, S.; Shah, A.K.; Shivananda, S.; Marathe, S.; Chatarjee, K.; Kalyani, S.; et al. Immunization During the COVID-19 Pandemic: Recommendations From Indian Academy of Pediatrics Advisory Committee on Vaccines and Immunization Practices. Indian Pediatrics 2020, 57, 1147–1152. [Google Scholar] [CrossRef] [PubMed]
- Adamu, A.A.; Jalo, R.I.; Habonimana, D.; Wiysonge, C.S. COVID-19 and Routine Childhood Immunization in Africa: Leveraging Systems Thinking and Implementation Science to Improve Immunization System Performance. Int. J. Infect. Dis. 2020, 98, 161–165. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization WHO. UNICEF. Warn of a Decline in Vaccinations during COVID-19. Available online: https://www.who.int/news/item/15-07-2020-who-and-unicef-warn-of-a-decline-in-vaccinations-during-covid-19 (accessed on 9 February 2021).
- Hossain, M.M.; Abdulla, F.; Karimuzzaman, M.; Rahman, A. Routine Vaccination Disruption in Low-Income Countries: An Impact of COVID-19 Pandemic. Asia. Pac. J. Public Health 2020, 32, 509–510. [Google Scholar] [CrossRef] [PubMed]
- Dobility Inc. SurveyCTO; Dobility, Inc.: Cambridge, MA, USA, 2020. [Google Scholar]
- National Health Portal Immunization in India. Available online: https://www.nhp.gov.in/Immunization_ms (accessed on 3 October 2019).
- Dhirar, N.; Dudeja, S.; Khandekar, J.; Bachani, D. Childhood Morbidity and Mortality in India—Analysis of National Family Health Survey 4 (NFHS-4) Findings. Indian Pediatrics 2018, 55, 335–338. [Google Scholar] [CrossRef] [PubMed]
- International Institute for Population Sciences (IIPS). National Family Health Survey (NFHS-5), 2019–2021: India; International Institute for Population Sciences (IIPS): Mumbai, India, 2021. [Google Scholar]
- Takahashi, S.; Metcalf, C.J.E.; Ferrari, M.J.; Moss, W.J.; Truelove, S.A.; Tatem, A.J.; Grenfell, B.T.; Lessler, J. Reduced Vaccination and the Risk of Measles and Other Childhood Infections Post-Ebola. Science 2015, 347, 1240–1242. [Google Scholar] [CrossRef] [PubMed]
- Sun, X.; Samba, T.T.; Yao, J.; Yin, W.; Xiao, L.; Liu, F.; Liu, X.; Zhou, J.; Kou, Z.; Fan, H.; et al. Impact of the Ebola Outbreak on Routine Immunization in Western Area, Sierra Leone—A Field Survey from an Ebola Epidemic Area. BMC Public Health 2017, 17, 363. [Google Scholar] [CrossRef] [PubMed]
- Cowling, B.J.; Chan, K.-H.; Fang, V.J.; Cheng, C.K.Y.; Fung, R.O.P.; Wai, W.; Sin, J.; Seto, W.H.; Yung, R.; Chu, D.W.S.; et al. Facemasks and Hand Hygiene to Prevent Influenza Transmission in Households: A Cluster Randomized Trial. Ann. Intern. Med. 2009, 151, 437–446. [Google Scholar] [CrossRef] [PubMed]
- Cowling, B.J.; Fang, V.J.; Riley, S.; Malik Peiris, J.S.; Leung, G.M. Estimation of the Serial Interval of Influenza. Epidemiol. Camb. Mass 2009, 20, 344–347. [Google Scholar] [CrossRef] [PubMed]
- Stebbins, S.; Downs, J.S.; Vukotich, C. Using Nonpharmaceutical Interventions to Prevent Influenza Transmission in Elementary School Children: Parent and Teacher Perspectives. J. Public Health Manag. Pract. JPHMP 2009, 15, 112–117. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Vukotich, C.J.; Coulborn, R.M.; Aragon, T.J.; Baker, M.G.; Burrus, B.B.; Aiello, A.E.; Cowling, B.J.; Duncan, A.; Enanoria, W.; Fabian, M.P.; et al. Findings, Gaps, and Future Direction for Research in Nonpharmaceutical Interventions for Pandemic Influenza. Emerg. Infect. Dis. J. 2010, 16. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Oyo-Ita, A.; Wiysonge, C.S.; Oringanje, C.; Nwachukwu, C.E.; Oduwole, O.; Meremikwu, M.M. Interventions for Improving Coverage of Childhood Immunisation in Low- and Middle-income Countries. Cochrane Database Syst. Rev. 2016. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. First Large Scale Maternal and Child Health Campaign Underway after End of Ebola Outbreak in Sierra Leone. Available online: https://www.afro.who.int/news/first-large-scale-maternal-and-child-health-campaign-underway-after-end-ebola-outbreak-sierra (accessed on 24 November 2021).
- Usman, H.R.; Akhtar, S.; Habib, F.; Jehan, I. Redesigned Immunization Card and Center-Based Education to Reduce Childhood Immunization Dropouts in Urban Pakistan: A Randomized Controlled Trial. Vaccine 2009, 27, 467–472. [Google Scholar] [CrossRef] [PubMed]

| Reason | Population Size (N) | Sample Size (n) | % |
|---|---|---|---|
| List of Families Obtained from the Hospital | 3115 | ||
| Excluded from the study | 3115 | 802 | 25.7% |
| Baby/mother died before discharge | 802 | 173 | 21.5% |
| Baby/mother died after discharge | 802 | 91 | 11.3% |
| Invalid/wrong number | 802 | 197 | 24.5% |
| Switched off phones | 802 | 332 | 41.4% |
| Data enumerator spoke a different language | 802 | 9 | 1.1% |
| Included in the Study | 3115 | 2313 | 74.3% |
| Included in the study and survey complete | 2313 | 2097 | 90.6% |
| Included in the study but survey not complete | 2313 | 216 | 9.3% |
| • Not available | 216 | 71 | 32.8% |
| • Not picked up or answered the call | 216 | 61 | 28.2% |
| • The family refused to participate | 216 | 51 | 23.6% |
| • Baby not yet discharged | 216 | 18 | 8.3% |
| • Other reasons * | 216 | 15 | 6.9% |
| Variables | n | % |
|---|---|---|
| State-wise Respondents | ||
| Andhra Pradesh | 948 | 45.2% |
| Karnataka | 732 | 34.9% |
| Telangana | 417 | 19.9% |
| Respondents | ||
| Mother | 1849 | 88.2% |
| Father | 128 | 6.1% |
| Other | 120 | 5.7% |
| Education Level | ||
| No education | 399 | 19.0% |
| No formal education but can read and write | 23 | 1.1% |
| Up to 5th standard | 126 | 6.0% |
| 6th to 10th standard | 785 | 37.4% |
| 11th standard to degree/diploma | 575 | 27.4% |
| Graduate | 137 | 6.5% |
| Post-graduate | 52 | 2.5% |
| Owns BPL * Card | 1415 | 67.5% |
| Received Vaccination Card | 1996 | 95.2% |
| Received and accessible at home | 1922 | 96.3% |
| Received but not accessible | 74 | 3.7% |
| Did not receive | 101 | 4.8% |
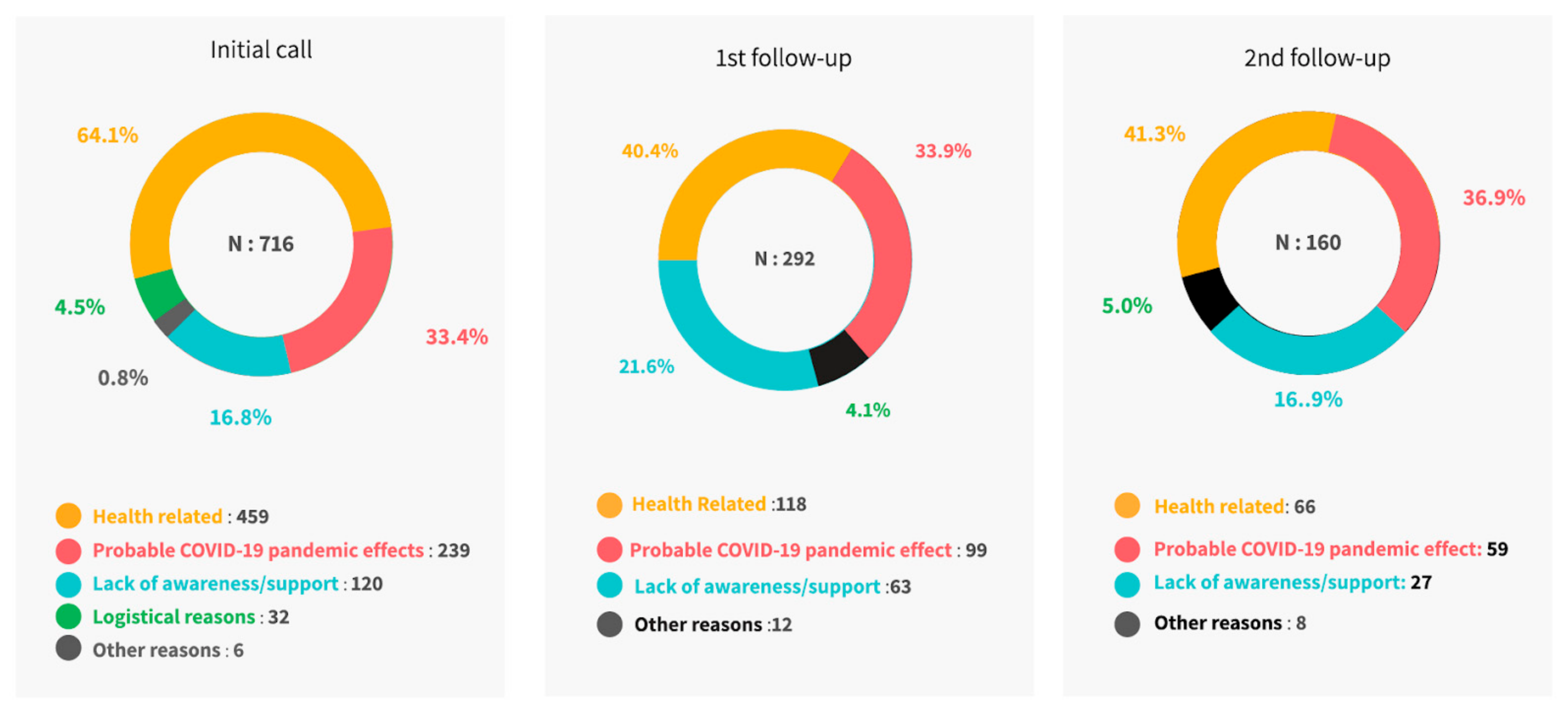
| Reasons | Initial Call (N = 716) | 1st Follow-Up Call (N = 292) | 2nd Follow-Up Call (N = 160) |
|---|---|---|---|
| n (%) | n (%) | n (%) | |
| Health-related | 459 (64.1) | 118 (40.4) | 66 (41.3) |
| Underweight | 211 (29.5) | 81 (27.7) | 45 (28.1) |
| Child ill and not brought to the facility | 106 (14.8) | 36 (12.3) | 18 (11.3) |
| Doctors not recommended | 62 (8.7) | 1 (0.3) | 3 (1.9) |
| Baby born prematurely | 39 (5.4) | none | None |
| Child ill, brought but not given vaccines | 34 (4.7) | none | None |
| Delay in previous vaccination | 7 (1) | none | None |
| Probable COVID-19 pandemic effects | 239 (33.4) | 99 (33.9) | 59 (36.9) |
| Lockdown | 86 (12.0) | 57 (19.5) | 29 (18.1) |
| Transportation problem | 60 (8.4) | none | None |
| Insufficient staff (ASHA/ANMs) | 29 (4.1) | 40 (13.7) | 30 (18.8) |
| Fear of coronavirus affecting the child | 24 (3.4) | none | None |
| Not knowing time/place for vaccination | 20 (2.8) | none | None |
| Insufficient vaccines | 11 (1.5) | 2 (0.7) | 2 (1.3) |
| ASHA/ANM having COVID-19 | 4 (0.6) | none | None |
| Long wait | 3 (0.4) | none | None |
| Insufficient number of babies | 2 (0.3) | none | None |
| Lack of awareness/support | 120 (16.8) | 63 (21.6) | 27 (16.9) |
| Lack of awareness about vaccine | 43 (6) | 27 (9.2) | 11 (6.9) |
| Community worker/ANM did not inform | 42 (5.9) | 36 (12.3) | None |
| Lack of awareness about schedule | 25 (5.7) | none | 15 (9.4) |
| Fear/rumours about side effects/no faith | 10 (1.4) | none | None |
| Logistical Reasons* | 32 (4.5) | none | None |
| Other Reasons† | 6 (0.8) | 12 | 8 (5.0) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Murthy, S.; Sawant, M.; Doreswamy, S.S.; Chandra Pothula, S.; Yan, S.D.; Singh Pathani, T.; Thakur, D.; Rajarama Sastry Vemuri, S.; Upadhyaya, S.; Alam, S.; et al. Supporting Immunization Uptake during a Pandemic, Using Remote Phone Call Intervention among Babies Discharged from a Special Neonatal Care Unit (SNCU) in South India. Vaccines 2022, 10, 507. https://doi.org/10.3390/vaccines10040507
Murthy S, Sawant M, Doreswamy SS, Chandra Pothula S, Yan SD, Singh Pathani T, Thakur D, Rajarama Sastry Vemuri S, Upadhyaya S, Alam S, et al. Supporting Immunization Uptake during a Pandemic, Using Remote Phone Call Intervention among Babies Discharged from a Special Neonatal Care Unit (SNCU) in South India. Vaccines. 2022; 10(4):507. https://doi.org/10.3390/vaccines10040507
Chicago/Turabian StyleMurthy, Seema, Meenal Sawant, Sahana Sadholalu Doreswamy, Sateesh Chandra Pothula, Shirley Du Yan, Tanmay Singh Pathani, Deepali Thakur, Srikrishna Rajarama Sastry Vemuri, Sanjeev Upadhyaya, Shahed Alam, and et al. 2022. "Supporting Immunization Uptake during a Pandemic, Using Remote Phone Call Intervention among Babies Discharged from a Special Neonatal Care Unit (SNCU) in South India" Vaccines 10, no. 4: 507. https://doi.org/10.3390/vaccines10040507
APA StyleMurthy, S., Sawant, M., Doreswamy, S. S., Chandra Pothula, S., Yan, S. D., Singh Pathani, T., Thakur, D., Rajarama Sastry Vemuri, S., Upadhyaya, S., Alam, S., Alimelu, M., & Singh, H. (2022). Supporting Immunization Uptake during a Pandemic, Using Remote Phone Call Intervention among Babies Discharged from a Special Neonatal Care Unit (SNCU) in South India. Vaccines, 10(4), 507. https://doi.org/10.3390/vaccines10040507






