Willingness to Receive COVID-19 Booster Vaccine: Associations between Green-Pass, Social Media Information, Anti-Vax Beliefs, and Emotional Balance
Abstract
:1. Introduction
Information, Trust, and Willingness to Vaccine
2. Materials and Methods
2.1. Study Design and Participants
2.2. Instruments
- (1)
- Sociodemographic/SARS-CoV-2 and related COVID-19 diseases questions;
- (2)
- Attitudes towards COVID-19 passes and vaccination;
- (3)
- Optimism assessment;
- (4)
- Depression, anxiety, and stress assessment.
2.3. Sample Size Calculation
2.4. Data Collection
2.5. Statistical Analysis
3. Results
4. Discussion
4.1. Theoretical Implications
4.2. Practical Implications
4.3. Limitations and Further Research
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Qu, Y.M.; Kang, E.M.; Cong, H.Y. Positive Result of Sars-Cov-2 in Sputum from a Cured Patient with COVID-19. Travel Med. Infect. Dis. 2020, 34, 101619. [Google Scholar] [CrossRef] [PubMed]
- WHO Coronavirus Disease (COVID-19) Pandemic. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019 (accessed on 14 February 2022).
- Sohrabi, C.; Alsafi, Z.; O’Neill, N.; Khan, M.; Kerwan, A.; Al-Jabir, A.; Iosifidis, C.; Agha, R. World Health Organization Declares Global Emergency: A Review of the 2019 Novel Coronavirus (COVID-19). Int. J. Surg. 2020, 76, 71–76. [Google Scholar] [CrossRef] [PubMed]
- Porcheddu, R.; Serra, C.; Kelvin, D.; Kelvin, N.; Rubino, S. Similarity in Case Fatality Rates (CFR) of COVID-19/SARS-COV-2 in Italy and China. J. Infect. Dev. Ctries. 2020, 14, 125–128. [Google Scholar] [CrossRef] [PubMed]
- Mahase, E. Covid-19: What Do We Know about “Long Covid”? BMJ 2020, 370, m2815. [Google Scholar] [CrossRef]
- De Giorgio, A. COVID-19 Is Not Just a Flu. Learn from Italy and Act Now. Travel Med. Infect. Dis. 2020, 35, 101655. [Google Scholar] [CrossRef]
- De Giorgio, A. Global Psychological Implications of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) and Coronavirus Disease-2019 (COVID-19). What Can Be Learned from Italy. Reflections, Perspectives, Opportunities. Front. Psychol. 2020, 11, 1836. [Google Scholar] [CrossRef]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The Psychological Impact of Quarantine and How to Reduce It: Rapid Review of the Evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef] [Green Version]
- Tee, M.L.; Tee, C.A.; Anlacan, J.P.; Aligam, K.J.G.; Reyes, P.W.C.; Kuruchittham, V.; Ho, R.C. Psychological Impact of COVID-19 Pandemic in the Philippines. J. Affect. Disord. 2020, 277, 379–391. [Google Scholar] [CrossRef]
- Killgore, W.D.S.; Taylor, E.C.; Cloonan, S.A.; Dailey, N.S. Psychological Resilience during the COVID-19 Lockdown. Psychiatry Res. 2020, 291, 113216. [Google Scholar] [CrossRef]
- Wilf-Miron, R.; Myers, V.; Saban, M. Incentivizing Vaccination Uptake: The “Green Pass” Proposal in Israel. JAMA 2021, 325, 1503–1504. [Google Scholar] [CrossRef]
- Razai, M.S.; Oakeshott, P.; Esmail, A.; Wiysonge, C.S.; Viswanath, K.; Mills, M.C. COVID-19 Vaccine Hesitancy: The Five Cs to Tackle Behavioural and Sociodemographic Factors. J. R. Soc. Med. 2021, 114, 295–298. [Google Scholar] [CrossRef] [PubMed]
- Karafillakis, E.; Dinca, I.; Apfel, F.; Cecconi, S.; Wűrz, A.; Takacs, J.; Suk, J.; Celentano, L.P.; Kramarz, P.; Larson, H.J. Vaccine Hesitancy among Healthcare Workers in Europe: A Qualitative Study. Vaccine 2016, 34, 5013–5020. [Google Scholar] [CrossRef] [PubMed]
- Barattucci, M.; Chirico, A.; Kuvačić, G.; De Giorgio, A. Rethinking the Role of Affect in Risk Judgment: What We Have Learned From COVID-19 During the First Week of Quarantine in Italy. Front. Psychol. 2020, 11, 554561. [Google Scholar] [CrossRef] [PubMed]
- Hou, J.; Shim, M. The Role of Provider-Patient Communication and Trust in Online Sources in Internet Use for Health-Related Activities. J. Health Commun. 2010, 15, 186–199. [Google Scholar] [CrossRef]
- Yun, E.K.; Park, H.A. Consumers’ Disease Information-Seeking Behaviour on the Internet in Korea. J. Clin. Nurs. 2010, 19, 2860–2868. [Google Scholar] [CrossRef]
- Ba, S.; Wang, L. Digital Health Communities: The Effect of Their Motivation Mechanisms. Decis. Support Syst. 2013, 55, 941–947. [Google Scholar] [CrossRef]
- Yan, Z.; Wang, T.; Chen, Y.; Zhang, H. Knowledge Sharing in Online Health Communities: A Social Exchange Theory Perspective. Inf. Manag. 2016, 53, 643–653. [Google Scholar] [CrossRef]
- Bi, D.; Kong, J.; Zhang, X.; Yang, J. Analysis on Health Information Acquisition of Social Network Users by Opinion Mining: Case Analysis Based on the Discussion on COVID-19 Vaccinations. J. Healthc. Eng. 2021, 2021, 1–11. [Google Scholar] [CrossRef]
- Guidry, J.P.D.; Laestadius, L.I.; Vraga, E.K.; Miller, C.A.; Perrin, P.B.; Burton, C.W.; Ryan, M.; Fuemmeler, B.F.; Carlyle, K.E. Willingness to Get the COVID-19 Vaccine with and without Emergency Use Authorization. Am. J. Infect. Control 2021, 49, 137. [Google Scholar] [CrossRef]
- WHO Ten Threats to Global Health in 2019. Available online: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019 (accessed on 21 February 2022).
- Lazarus, J.V.; Ratzan, S.C.; Palayew, A.; Gostin, L.O.; Larson, H.J.; Rabin, K.; Kimball, S.; El-Mohandes, A. A Global Survey of Potential Acceptance of a COVID-19 Vaccine. Nat. Med. 2020, 27, 225–228. [Google Scholar] [CrossRef]
- Shmueli, L. Predicting Intention to Receive COVID-19 Vaccine among the General Population Using the Health Belief Model and the Theory of Planned Behavior Model. BMC Public Health 2021, 21, 804. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Han, B.; Zhao, T.; Liu, H.; Liu, B.; Chen, L.; Xie, M.; Liu, J.; Zheng, H.; Zhang, S.; et al. Vaccination Willingness, Vaccine Hesitancy, and Estimated Coverage at the First Round of COVID-19 Vaccination in China: A National Cross-Sectional Study. Vaccine 2021, 39, 2833–2842. [Google Scholar] [CrossRef] [PubMed]
- Dodd, R.H.; Cvejic, E.; Bonner, C.; Pickles, K.; McCaffery, K.J.; Ayre, J.; Batcup, C.; Copp, T.; Cornell, S.; Dakin, T.; et al. Willingness to Vaccinate against COVID-19 in Australia. Lancet Infect. Dis. 2021, 21, 318–319. [Google Scholar] [CrossRef]
- Malik, A.A.; McFadden, S.A.M.; Elharake, J.; Omer, S.B. Determinants of COVID-19 Vaccine Acceptance in the US. EClinicalMedicine 2020, 26, 100495. [Google Scholar] [CrossRef]
- Brailovskaia, J.; Schneider, S.; Margraf, J. To Vaccinate or Not to Vaccinate!? Predictors of Willingness to Receive COVID-19 Vaccination in Europe, the U.S., and China. PLoS ONE 2021, 16, e0260230. [Google Scholar] [CrossRef]
- Dror, A.A.; Eisenbach, N.; Taiber, S.; Morozov, N.G.; Mizrachi, M.; Zigron, A.; Srouji, S.; Sela, E. Vaccine Hesitancy: The next Challenge in the Fight against COVID-19. Eur. J. Epidemiol. 2020, 35, 775–779. [Google Scholar] [CrossRef]
- Wang, K.; Wong, E.L.Y.; Ho, K.F.; Cheung, A.W.L.; Yau, P.S.Y.; Dong, D.; Wong, S.Y.S.; Yeoh, E.K. Change of Willingness to Accept COVID-19 Vaccine and Reasons of Vaccine Hesitancy of Working People at Different Waves of Local Epidemic in Hong Kong, China: Repeated Cross-Sectional Surveys. Vaccines 2021, 9, 62. [Google Scholar] [CrossRef]
- EuroNews Omicron Variant Likely to Resist COVID Vaccines as Updated Jabs Months Away. Available online: https://www.euronews.com/next/2021/11/30/omicron-variant-likely-to-resist-covid-vaccines-warns-moderna-ceo (accessed on 16 February 2022).
- Etikan, I.; Alkassim, R.; Abubakar, S. Comparision of Snowball Sampling and Sequential Sampling Technique. Biom. Biostat. Int. J. 2016, 3, 55. [Google Scholar] [CrossRef] [Green Version]
- Van, D.; McLaws, M.L.; Crimmins, J.; MacIntyre, C.R.; Seale, H. University Life and Pandemic Influenza: Attitudes and Intended Behaviour of Staff and Students towards Pandemic (H1N1) 2009. BMC Public Health 2010, 10, 130. [Google Scholar] [CrossRef] [Green Version]
- Arafa, A.; Mohammed, Z.; Mahmoud, O.; Elshazley, M.; Ewis, A. Depressed, Anxious, and Stressed: What Have Healthcare Workers on the Frontlines in Egypt and Saudi Arabia Experienced during the COVID-19 Pandemic? J. Affect. Disord. 2021, 278, 365–371. [Google Scholar] [CrossRef]
- Scheier, M.F.; Carver, C.S.; Bridges, M.W. Distinguishing Optimism from Neuroticism (and Trait Anxiety, Self-Mastery, and Self-Esteem): A Reevaluation of the Life Orientation Test. J. Personal. Soc. Psychol. 1994, 67, 1063–1078. [Google Scholar] [CrossRef]
- Lovibond, P.F.; Lovibond, S.H. The Structure of Negative Emotional States: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav. Res. Ther. 1995, 33, 335–343. [Google Scholar] [CrossRef]
- Raosoft Sample Size Calculator. Available online: http://www.raosoft.com/samplesize.html (accessed on 14 February 2022).
- Tabachnick, B.G.; Fidell, L.S. Using Multivariate Statistics, 6th ed.; Pearson: Boston, MA, USA, 2013. [Google Scholar]
- Bailey, K. Typologies and Taxonomies—An Introduction to Classification Techniques. J. Am. Soc. Inf. Sci. 1994, 47, 328–329. [Google Scholar]
- Gallagher, M.W.; Lopez, S.J.; Pressman, S.D. Optimism Is Universal: Exploring the Presence and Benefits of Optimism in a Representative Sample of the World. J. Personal. 2013, 81, 429–440. [Google Scholar] [CrossRef] [PubMed]
- Genç, E.; Arslan, G. Optimism and Dispositional Hope to Promote College Students’ Subjective Well-Being in the Context of the COVID-19 Pandemic. J. Posit. Psychol. Wellbeing 2021, 5, 87–96. [Google Scholar] [CrossRef]
- Diener, E. Subjective Well-Being. Psychol. Bull. 1984, 95, 542–575. [Google Scholar] [CrossRef] [PubMed]
- Hart, S.L.; Vella, L.; Mohr, D.C. Relationships among Depressive Symptoms, Benefit-Finding, Optimism, and Positive Affect in Multiple Sclerosis Patients after Psychotherapy for Depression. Health Psychol. 2008, 27, 230–238. [Google Scholar] [CrossRef] [Green Version]
- Gassen, J.; Nowak, T.J.; Henderson, A.D.; Weaver, S.P.; Baker, E.J.; Muehlenbein, M.P. Unrealistic Optimism and Risk for COVID-19 Disease. Front. Psychol. 2021, 12, 647461. [Google Scholar] [CrossRef]
- Sharot, T.; Korn, C.W.; Dolan, R.J. How Unrealistic Optimism Is Maintained in the Face of Reality. Nat. Neurosci. 2011, 14, 1475–1479. [Google Scholar] [CrossRef]
- Jefferson, A.; Bortolotti, L.; Kuzmanovic, B. What Is Unrealistic Optimism? Conscious. Cogn. 2017, 50, 3–11. [Google Scholar] [CrossRef] [Green Version]
- Wang, X.; Chao, F.; Yu, G.; Zhang, K. Factors Influencing Fake News Rebuttal Acceptance during the COVID-19 Pandemic and the Moderating Effect of Cognitive Ability. Comput. Hum. Behav. 2022, 130, 107174. [Google Scholar] [CrossRef] [PubMed]
- Time What You Think You Know about the Web Is Wrong. Available online: https://time.com/12933/what-you-think-you-know-about-the-web-is-wrong/ (accessed on 16 February 2022).
- WHO Munich Security Conference. Available online: https://www.who.int/director-general/speeches/detail/munich-security-conference (accessed on 16 February 2022).
- Meta Keeping People Safe and Informed about the Coronavirus. Available online: https://about.fb.com/news/2020/12/coronavirus/#joint-statement (accessed on 16 February 2022).
- Dolinski, D.; Kulesza, W.; Muniak, P.; Dolinska, B.; Węgrzyn, R.; Izydorczak, K. Media Intervention Program for Reducing Unrealistic Optimism Bias: The Link between Unrealistic Optimism, Well-Being, and Health. Appl. Psychol. Health Well-Being 2021, 1–20. [Google Scholar] [CrossRef] [PubMed]
- Geoghegan, S.; O’Callaghan, K.P.; Offit, P.A. Vaccine Safety: Myths and Misinformation. Front. Microbiol. 2020, 11, 372. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rubin, G.J.; Potts, H.W.W.; Michie, S. Likely Uptake of Swine and Seasonal Flu Vaccines among Healthcare Workers. A Cross-Sectional Analysis of UK Telephone Survey Data. Vaccine 2011, 29, 2421–2428. [Google Scholar] [CrossRef]
- Verger, P.; Fressard, L.; Collange, F.; Gautier, A.; Jestin, C.; Launay, O.; Raude, J.; Pulcini, C.; Peretti-Watel, P. Vaccine Hesitancy Among General Practitioners and Its Determinants During Controversies: A National Cross-Sectional Survey in France. EBioMedicine 2015, 2, 891–897. [Google Scholar] [CrossRef] [Green Version]
- Schmelz, K.; Bowles, S. Overcoming COVID-19 Vaccination Resistance When Alternative Policies Affect the Dynamics of Conformism, Social Norms, and Crowding Out. Proc. Natl. Acad. Sci. USA 2021, 118, e2104912118. [Google Scholar] [CrossRef]
- Cialdini, R.B.; Trost, M.R. Social Influence: Social Norms, Conformity and Compliance. In The Handbook of Social Psychology; Gilbert, D.T., Fiske, S.T., Lindzey, G., Eds.; McGraw-Hill: New York, NY, USA, 1998. [Google Scholar]
- Aronson, E.; Wilson, T.D.; Akert, R.M. Social Psychology, 7th ed.; Pearson Higher Education: London, UK, 2010. [Google Scholar]
- Packer, D.J.; Ungson, N.D.; Marsh, J.K. Conformity and Reactions to Deviance in the Time of COVID-19. Group Processes Intergroup Relat. 2021, 24, 311–317. [Google Scholar] [CrossRef]
| Item/Response | Overall (n = 1003) | Vaccinated (n = 435) | Not Vaccinated (n = 568) | p-Value | ||||
|---|---|---|---|---|---|---|---|---|
| Age | 40 | (30; 49) | 40 | (33; 50) | 39 | (27; 48) | <0.001 a | |
| Gender | Male | 414 | (41.3) | 182 | (41.8) | 232 | (40.8) | 0.905 b |
| Female | 581 | (57.9) | 250 | (57.5) | 331 | (58.3) | ||
| Other/prefer not to say | 8 | (0.8) | 3 | (0.7) | 5 | (0.9) | ||
| Education | High school | 253 | (25.2) | 98 | (22.3) | 155 | (27.3) | <0.001 b |
| Bachelor degree | 228 | (22.7) | 83 | (19.8) | 145 | (25.5) | ||
| Master degree | 385 | (38.4) | 168 | (38.6) | 217 | (38.2) | ||
| Postgraduate degree | 51 | (5.1) | 29 | (6.7) | 22 | (3.9) | ||
| PhD | 86 | (8.6) | 57 | (13.1) | 29 | (5.1) | ||
| Employment | Unemployed | 64 | (6.4) | 14 | (3.2) | 50 | (8.8) | <0.001 b |
| Full | 749 | (74.7) | 348 | (80) | 401 | (70.6) | ||
| Retired | 56 | (5.6) | 26 | (6) | 30 | (5.3) | ||
| Part-time | 22 | (2.2) | 10 | (2.3) | 12 | (2.1) | ||
| Student | 112 | (11.1) | 37 | (8.5) | 75 | (13.2) | ||
| Q6 | Yes | 114 | (11.4) | 64 | (14.7) | 50 | (8.8) | 0.003 b |
| No | 889 | (88.6) | 371 | (85.3) | 518 | (91.2) | ||
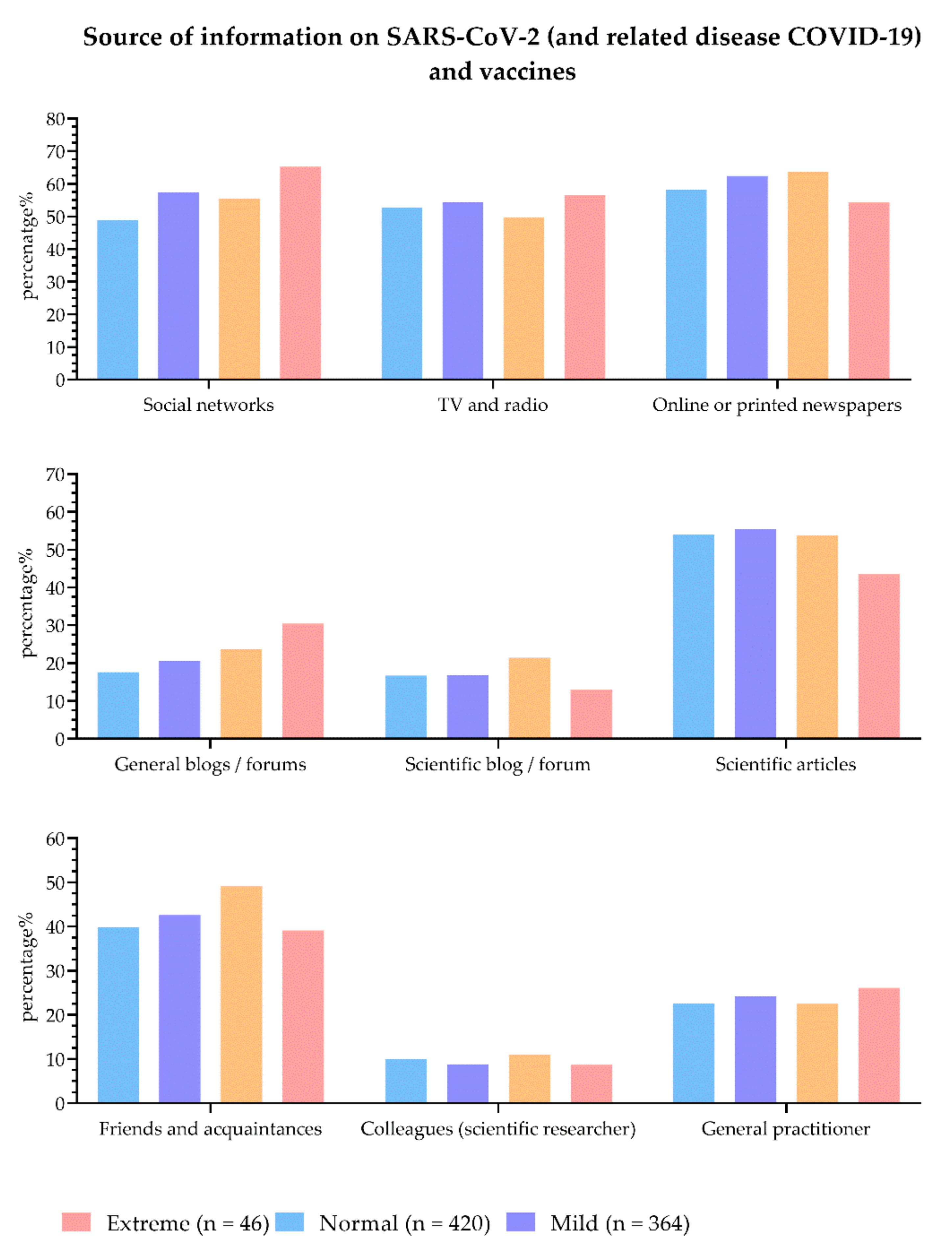
| Q5 | Social networks | 540 | (53.8) | 164 | (37.7) | 376 | (66.2) | <0.001 b |
| TV and radio | 531 | (52.9) | 269 | (61.8) | 262 | (46.1) | <0.001 b | |
| Online or printed newspapers | 606 | (60.4) | 263 | (60.5) | 343 | (60.4) | 0.981 b | |
| General internet blogs/forums | 204 | (20.3) | 47 | (10.8) | 157 | (27.6) | <0.001 b | |
| Blog/forum (recognized as scientific) | 174 | (17.3) | 55 | (12.6) | 119 | (21) | 0.001 b | |
| Scientific articles | 542 | (54) | 212 | (48.7) | 330 | (58.1) | 0.003 b | |
| Friends and acquaintances | 425 | (42.4) | 149 | (34.3) | 276 | (48.6) | <0.001 b | |
| Colleagues (I am a scientific researcher) | 97 | (9.7) | 46 | (10.6) | 51 | (9) | 0.397 b | |
| General practitioner | 234 | (23.3) | 137 | (31.5) | 97 | (17.1) | <0.001 b | |
| Q16 | Fully beneficial | 81 | (8.1) | 80 | (18.4) | 1 | (0.2) | <0.001 b |
| Potentially beneficial | 336 | (33.5) | 267 | (61.4) | 69 | (12.1) | ||
| Non-beneficial | 214 | (21.3) | 43 | (9.9) | 171 | (30.1) | ||
| Harmful | 372 | (37.1) | 45 | (10.3) | 327 | (57.6) | ||
| Q17 | Do not deserve additional hospital costs | 777 | (77.5) | 234 | (53.8) | 543 | (95.6) | <0.001 b |
| Deserve additional hospital costs | 221 | (22) | 196 | (45.1) | 25 | (4.4) | ||
| Do not deserve hospital treatment | 5 | (0.5) | 5 | (1.1) | 0 | (0) | ||
| Q18 | Yes | 73 | (7.3) | 73 | (16.8) | 0 | (0) | <0.001 b |
| I do not know | 182 | (18.1) | 161 | (37) | 21 | (3.7) | ||
| No | 748 | (74.6) | 201 | (46.2) | 547 | (96.3) | ||
| Q19 | Yes | 201 | (20) | 197 | (45.3) | 4 | (0.7) | <0.001 b |
| I do not know | 119 | (12.0) | 101 | (31.5) | 18 | (3.2) | ||
| No | 683 | (68.1) | 137 | (23.2) | 546 | (96.1) | ||
| LOT-R | Optimism | 17 | (14; 19) | 16 | (14; 19) | 17 | (14; 19) | <0.001 a |
| DASS21 | Depression | 4 | (0; 10) | 4 | (0; 8) | 4 | (0; 10) | 0.398 a |
| Anxiety | 2 | (0; 6) | 2 | (0; 6) | 2 | (0; 6) | 0.511 a | |
| Stress | 8 | (2; 14) | 8 | (2; 14) | 8 | (3; 14) | 0.447 a | |
| Item/Response | Univariate | Multivariate | |||||
|---|---|---|---|---|---|---|---|
| OR | 95% CI | p-Value | OR | 95% CI | p-Value | ||
| Age | 1.02 | 1.01–1.03 | <0.001 | 1.01 | 0.99–1.02 | 0.249 | |
| Gender | Male | 1.31 | 0.31–5.54 | 0.716 | |||
| Female | 1.26 | 0.30–5.32 | 0.754 | ||||
| Other/prefer not to say | ref | ||||||
| Education | High school | ref | |||||
| Bacchelor degree | 0.91 | 0.63–1.31 | 0.598 | 0.85 | 0.55–1.32 | 0.473 | |
| Master degree | 1.22 | 0.89–1.69 | 0.220 | 1.14 | 0.78–1.65 | 0.494 | |
| Postgraduate degree | 2.09 | 1.13–3.83 | 0.018 | 2.25 | 1.14–4.46 | 0.020 | |
| PhD | 3.11 | 1.86–5.20 | <0.001 | 1.97 | 1.11–3.52 | 0.021 | |
| Employment | Unemployed | ref | |||||
| Full | 3.10 | 1.68–5.70 | <0.001 | 2.92 | 1.47–5.80 | 0.002 | |
| Retired | 3.10 | 1.40–6.83 | 0.005 | 2.35 | 0.92–6.05 | 0.075 | |
| Part-time | 2.98 | 1.07–8.31 | 0.037 | 3.92 | 1.20–12.82 | 0.024 | |
| Student | 1.76 | 0.86–3.59 | 0.119 | 2.80 | 1.20–6.51 | 0.017 | |
| Q6 | Yes | 1.79 | 1.21–2.65 | 0.004 | 1.34 | 0.85–2.12 | 0.207 |
| No | ref | ||||||
| Q5 | Social networks | 0.31 | 0.24–0.40 | <0.001 | 0.36 | 0.27–0.49 | <0.001 |
| TV and radio | 1.89 | 1.47–2.44 | <0.001 | 2.35 | 1.71–3.23 | <0.001 | |
| Online or printed newspapers | 0.98 | 0.78–1.29 | 0.981 | ||||
| General internet blogs/forums | 0.32 | 0.22–0.45 | <0.001 | 0.34 | 0.22–0.52 | <0.001 | |
| Blog/forum (recognized as scientific) | 0.55 | 0.37–0.77 | 0.001 | 0.85 | 0.55–1.32 | 0.474 | |
| Scientific articles | 0.69 | 0.53–0.88 | 0.003 | 0.73 | 0.54–1.01 | 0.057 | |
| Friends and acquaintances | 0.55 | 0.43–0.71 | <0.001 | 0.66 | 0.48–0.91 | 0.011 | |
| Colleagues (I am a scientific researcher) | 1.20 | 0.79–1.82 | 0.397 | ||||
| General practitioner | 2.23 | 1.66–3.01 | <0.001 | 2.53 | 1.78–3.61 | <0.001 | |
| LOT-R | Optimism | 0.94 | 0.91–0.97 | <0.001 | 0.93 | 0.89–0.96 | <0.001 |
| DASS21 | Depression | 0.99 | 0.97–1.01 | 0.491 | |||
| Anxiety | 1.01 | 0.99–1.03 | 0.220 | ||||
| Stress | 0.99 | 0.98–1.01 | 0.521 | ||||
| n | (%) | ||
|---|---|---|---|
| Vaccine received | Pfizer/BioNTech | 319 | (73.3) |
| AstraZeneca | 53 | (12.2) | |
| Johnson & Johnson | 34 | (7.8) | |
| Moderna | 18 | (4.1) | |
| Combination | 8 | (1.8) | |
| Other | 3 | (0.7) | |
| Doses received (including Johnson & Johnson) | One | 69 | (15.9) |
| Two | 326 | (74.9) | |
| Three | 40 | (9.2) | |
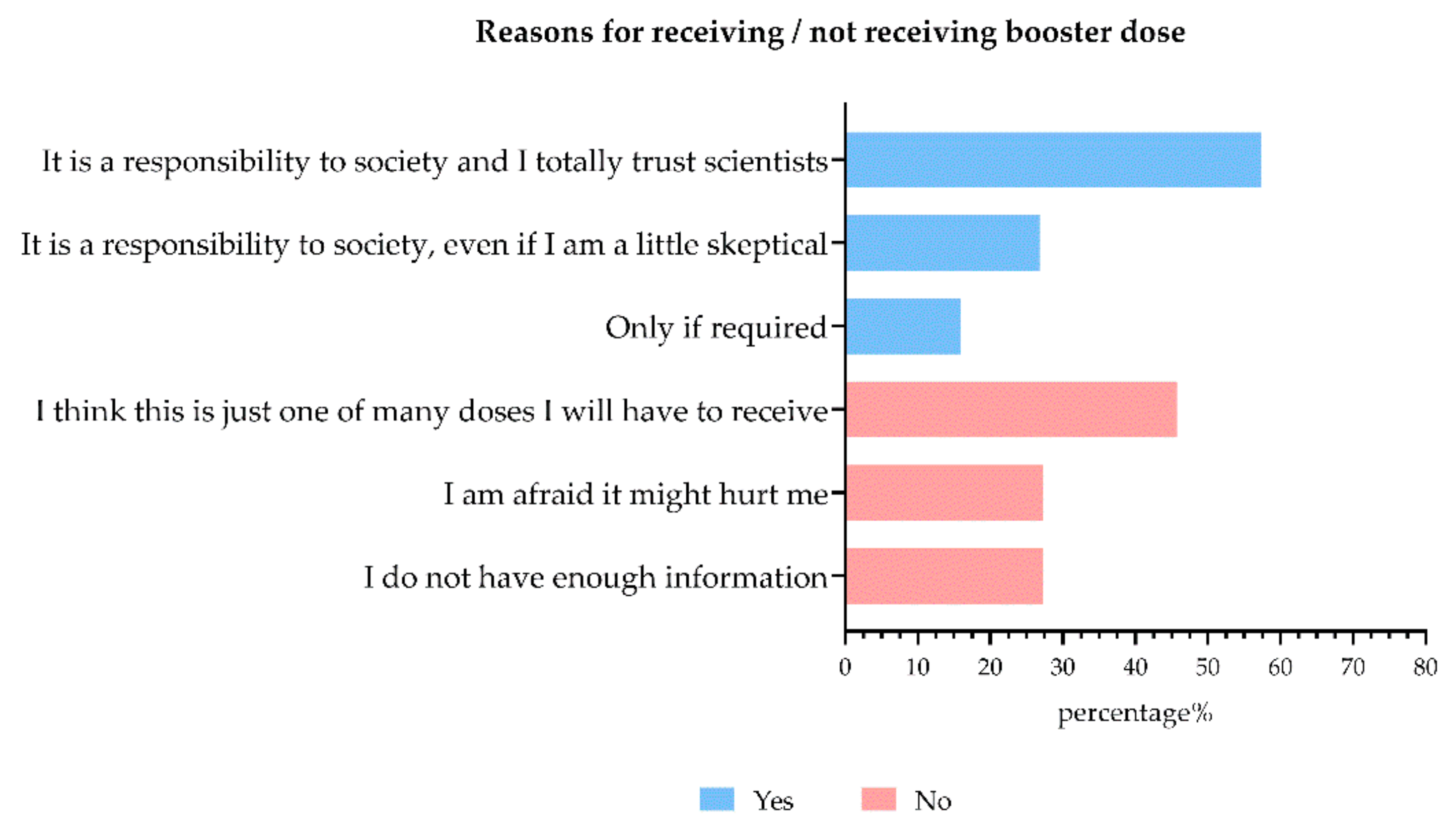
| Willingness to receive second and third (booster) dose | Yes | 31 | (88.6) |
| No | 4 | (11.4) | |
| Willingness to receive second (booster) dose for Johnson & Johnson vaccine | Yes | 14 | (41.2) |
| No | 20 | (58.8) | |
| Willingness to receive third (booster) dose | Yes | 269 | (82.5) |
| No | 57 | (17.5) |
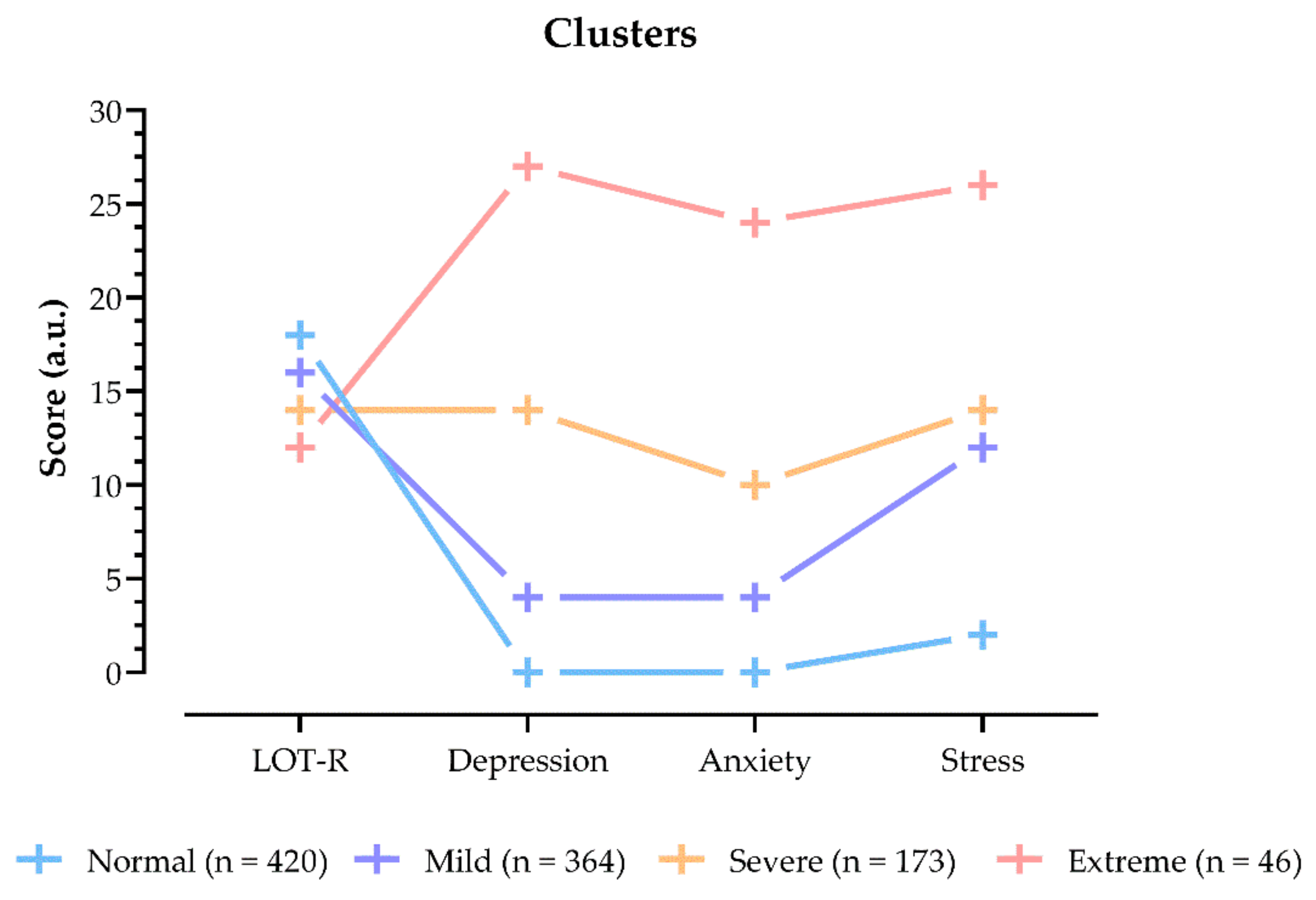
| Item/Response | Normal (n = 420) | Mild (n = 364) | Severe (n = 173) | Extreme (n = 46) | p-Value | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Age | 40 | (30; 49) | 40 | (32; 49) | 39 | (29; 49) | 38.5 | (27; 50) | 0.94 a | |
| Gender | Male | 205 | (48.8) | 132 | (36.3) | 60 | (34.7) | 17 | (58.7) | <0.001 b |
| Female | 211 | (50.2) | 231 | (63.5) | 112 | (64.7) | 27 | (37) | ||
| Other/prefer not to say | 4 | (1) | 1 | (0.3) | 1 | (0.6) | 2 | (4.3) | ||
| Education | High school | 111 | (26.4) | 74 | (20.3) | 45 | (26) | 23 | (50) | 0.042 c |
| Bachelor degree | 101 | (24) | 81 | (22.3) | 37 | (21.4) | 9 | (19.6) | ||
| Master degree | 149 | (35.5) | 158 | (43.4) | 67 | (38.7) | 11 | (23.9) | ||
| Postgraduate degree | 22 | (5.2) | 18 | (4.9) | 10 | (5.8) | 1 | (2.2) | ||
| PhD | 37 | (8.8) | 33 | (9.1) | 14 | (8.1) | 2 | (4.3) | ||
| Employment | Unemployed | 20 | (4.8) | 24 | (6.6) | 18 | (10.4) | 2 | (4.3) | 0.448 c |
| Full | 319 | (76) | 273 | (75) | 125 | (72.3) | 32 | (69.6) | ||
| Retired | 25 | (6) | 19 | (5.2) | 10 | (5.8) | 2 | (4.3) | ||
| Part-time | 9 | (2.1) | 8 | (2.2) | 2 | (1.2) | 3 | (6.5) | ||
| Student | 47 | (11.2) | 40 | (11) | 18 | (10.4) | 7 | (15.2) | ||
| Vaccinated | Yes | 185 | (44) | 158 | (43.4) | 68 | (39.3) | 24 | (52.2) | 0.442 d |
| No | 235 | (56) | 206 | (56.6) | 105 | (60.7) | 22 | (47.8) | ||
| Q6 | Yes | 47 | (11.2) | 39 | (10.7) | 14 | (8.1) | 14 | (30.4) | <0.001 d |
| No | 373 | (88.8) | 325 | (89.3) | 159 | (91.9) | 32 | (69.6) | ||
| Item/Response | Fully Beneficial (n = 81) | Potentially Beneficial (n = 336) | Non-Beneficial (n = 214) | Harmful (n = 372) | p-Value | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Age | 44 | (35; 54) | 40 | (33; 49) | 37.5 | (26; 45) | 40 | (30; 49) | <0.001 a | |
| Gender | Male | 37 | (45.7) | 132 | (39.3) | 98 | (45.8) | 147 | (39.5) | 0.538 b |
| Female | 43 | (53.1) | 202 | (60.1) | 115 | (53.7) | 221 | (59.4) | ||
| Other/prefer not to say | 1 | (1.2) | 2 | (0.6) | 1 | (0.5) | 4 | (1.1) | ||
| Education | High school | 17 | (21) | 84 | (25) | 68 | (31.8) | 84 | (22.6) | <0.001 b |
| Bachelor degree | 12 | (14.8) | 59 | (17.6) | 52 | (24.3) | 105 | (28.2) | ||
| Master degree | 36 | (44.4) | 130 | (38.7) | 70 | (32.7) | 149 | (40.1) | ||
| Postgraduate degree | 7 | (8.6) | 19 | (5.7) | 10 | (4.7) | 15 | (4.0) | ||
| PhD | 9 | (11.1) | 44 | (13.1) | 14 | (6.5) | 19 | (5.1) | ||
| Employment | Unemployed | 6 | (7.4) | 11 | (3.3) | 17 | (7.9) | 30 | (8.1) | <0.001 b |
| Full | 55 | (67.9) | 281 | (83.6) | 147 | (68.7) | 266 | (71.5) | ||
| Retired | 11 | (13.6) | 16 | (4.8) | 9 | (4.2) | 20 | (5.4) | ||
| Part-time | 1 | (1.2) | 7 | (2.1) | 6 | (2.8) | 8 | (2.2) | ||
| Student | 8 | (9.9) | 21 | (6.3) | 35 | (16.4) | 48 | (12.9) | ||
| Cluster | Normal | 38 | (46.9) | 133 | (39.6) | 100 | (46.7) | 149 | (40.1) | 0.246 b |
| Mild | 28 | (34.6) | 130 | (38.7) | 74 | (34.6) | 132 | (35.5) | ||
| Severe | 8 | (9.9) | 58 | (17.3) | 33 | (15.4) | 74 | (19.9) | ||
| Extreme | 7 | (8.6) | 15 | (4.5) | 7 | (3.3) | 17 | (4.6) | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
De Giorgio, A.; Kuvačić, G.; Maleš, D.; Vecchio, I.; Tornali, C.; Ishac, W.; Ramaci, T.; Barattucci, M.; Milavić, B. Willingness to Receive COVID-19 Booster Vaccine: Associations between Green-Pass, Social Media Information, Anti-Vax Beliefs, and Emotional Balance. Vaccines 2022, 10, 481. https://doi.org/10.3390/vaccines10030481
De Giorgio A, Kuvačić G, Maleš D, Vecchio I, Tornali C, Ishac W, Ramaci T, Barattucci M, Milavić B. Willingness to Receive COVID-19 Booster Vaccine: Associations between Green-Pass, Social Media Information, Anti-Vax Beliefs, and Emotional Balance. Vaccines. 2022; 10(3):481. https://doi.org/10.3390/vaccines10030481
Chicago/Turabian StyleDe Giorgio, Andrea, Goran Kuvačić, Dražen Maleš, Ignazio Vecchio, Cristina Tornali, Wadih Ishac, Tiziana Ramaci, Massimiliano Barattucci, and Boris Milavić. 2022. "Willingness to Receive COVID-19 Booster Vaccine: Associations between Green-Pass, Social Media Information, Anti-Vax Beliefs, and Emotional Balance" Vaccines 10, no. 3: 481. https://doi.org/10.3390/vaccines10030481
APA StyleDe Giorgio, A., Kuvačić, G., Maleš, D., Vecchio, I., Tornali, C., Ishac, W., Ramaci, T., Barattucci, M., & Milavić, B. (2022). Willingness to Receive COVID-19 Booster Vaccine: Associations between Green-Pass, Social Media Information, Anti-Vax Beliefs, and Emotional Balance. Vaccines, 10(3), 481. https://doi.org/10.3390/vaccines10030481









