Modified Hemagglutination Tests for COVID-19 Serology in Resource-Poor Settings: Ready for Prime-Time?
Abstract
:Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| RBD | receptor-binding domain |
| POCT | point-of-care testing |
| CAT | column agglutination technology |
| HAT | hemagglutination tests |
References
- Focosi, D.; Franchini, M. COVID-19 convalescent plasma therapy: Hit fast, hit hard! Vox Sang. 2021, 116, 935–942. [Google Scholar] [CrossRef]
- Violi, F.; Ceccarelli, G.; Loffredo, L.; Alessandri, F.; Cipollone, F.; D’Ardes, D.; D’Ettorre, G.; Pignatelli, P.; Venditti, M.; Mastroianni, C.M.; et al. Albumin Supplementation Dampens Hypercoagulability in COVID-19: A Preliminary Report. Thromb. Haemost. 2021, 121, 102–105. [Google Scholar] [CrossRef] [PubMed]
- Hernandez Cordero, A.I.; Li, X.; Milne, S.; Yang, C.X.; Bosse, Y.; Joubert, P.; Timens, W.; Berge, M.V.D.; Nickle, D.; Hao, K.; et al. Multi-omics highlights ABO plasma protein as a causal risk factor for COVID-19. Hum. Genet. 2020, 140, 969–979. [Google Scholar] [CrossRef] [PubMed]
- Villafañe, L.; Vaulet, L.G.; Viere, F.M.; Klepp, L.I.; Forrellad, M.A.; Bigi, M.M.; Romano, M.I.; Magistrelli, G.; Fermepin, M.R.; Bigi, F. Development and evaluation of a low cost IgG ELISA test based in RBD protein for COVID-19. J. Immunol. Methods 2022, 500, 113182. [Google Scholar] [CrossRef] [PubMed]
- Hirst, G.K. The Agglutination of Red Cells by Allantoic Fluid of Chick Embryos Infected with Influenza Virus. Science 1941, 94, 22–23. [Google Scholar] [CrossRef] [PubMed]
- Hirst, G.K. Adsorption of Influenza Hemagglutinins and Virus by Red Blood Cells. J. Exp. Med. 1942, 76, 195–209. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Salk, J.E. A Plastic Plate for Use in Tests Involving Virus Hemagglutination and Other Similar Reactions. Science 1948, 108, 749. [Google Scholar] [CrossRef] [PubMed]
- Jia, N.; Wang, S.X.; Liu, Y.X.; Zhang, P.H.; Zuo, S.Q.; Lin, Z.; Dang, R.L.; Ma, Y.H.; Zhang, C.; Zhang, L.; et al. Increased sensitivity for detecting avian influenza-specific antibodies by a modified hemagglutination inhibition assay using horse erythrocytes. J. Virol. Methods 2008, 153, 43–48. [Google Scholar] [CrossRef]
- WHO. Serological Detection of Avian Influenza A(H7N9) Virus Infections by Modified Horse Red Blood Cells Haemagglutination-Inhibition Assay. 20 December 2013. Available online: https://www.who.int/influenza/gisrs_laboratory/cnic_serological_diagnosis_hai_a_h7n9_20131220.pdf (accessed on 25 January 2022).
- Rosen, L. Hemagglutination by adenoviruses. Virology 1958, 5, 574–577. [Google Scholar] [CrossRef]
- Demeio, J.L.; Gower, T.A. Hemagglutination by measles virus. Virology 1961, 13, 367–368. [Google Scholar] [CrossRef]
- Marsh, W.L. Scoring of hemagglutination reactions. Transfusion 1972, 12, 352–353. [Google Scholar] [CrossRef]
- Killian, M.L. Hemagglutination Assay for Influenza Virus. Methods Mol. Biol. 2020, 2123, 3–10. [Google Scholar] [CrossRef]
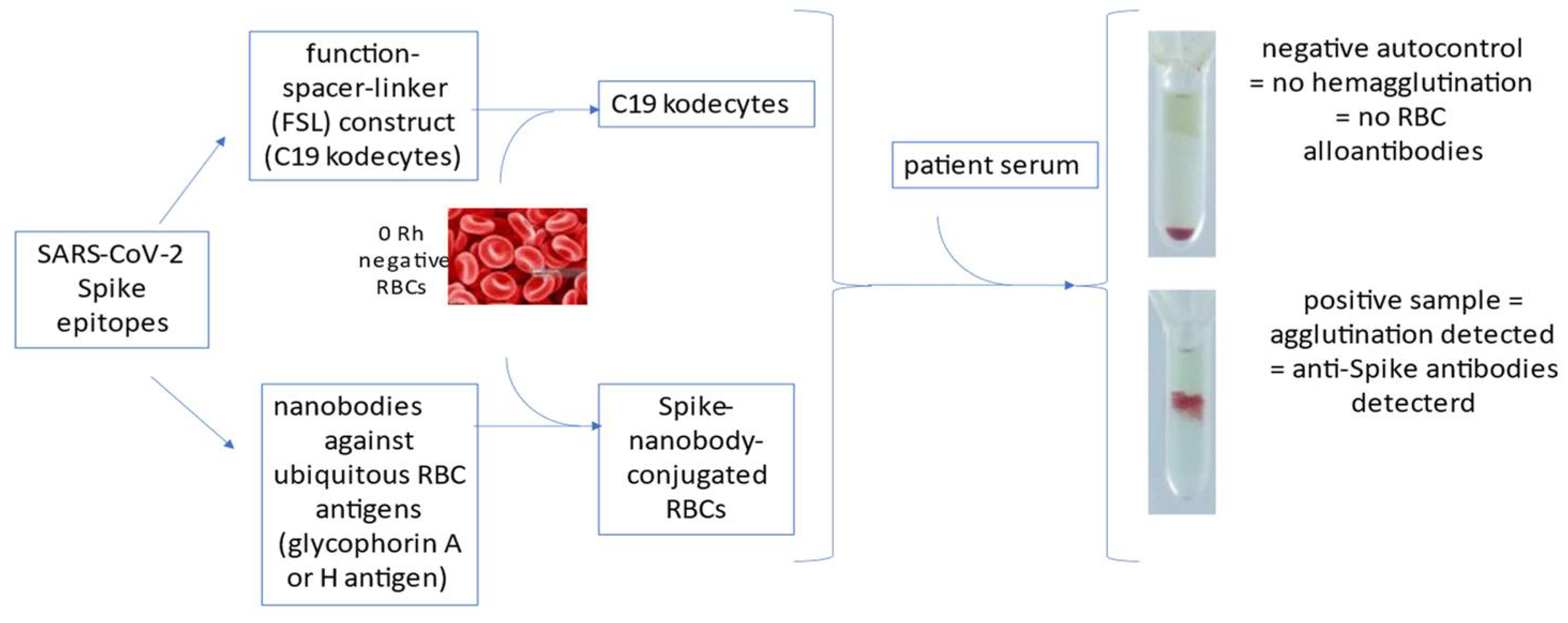
- Nagappan, R.; Flegel, W.A.; Srivastava, K.; Williams, E.C.; Ryzhov, I.; Tuzikov, A.; Galanina, O.; Shilova, N.; Sukhikh, G.; Perry, H.; et al. COVID-19 antibody screening with SARS-CoV-2 red cell kodecytes using routine serologic diagnostic platforms. Transfusion 2021, 61, 1171–1180. [Google Scholar] [CrossRef]
- Weinstock, C.; Flegel, W.A.; Srivastava, K.; Kaiser, S.; Schrezenmeier, H.; Tsamadou, C.; Ludwig, C.; Jahrsdoerfer, B.; Bovin, N.V.; Henry, S.M. Erytra Blood Group Analyser and Kode Technology testing of SARS-CoV-2 antibodies among convalescent patients and vaccinated individuals. Eur. J. Haematol. 2021, 3, 72–79. [Google Scholar] [CrossRef]
- Srivastava, K.; West, K.A.; De Giorgi, V.; Holbrook, M.R.; Bovin, N.V.; Henry, S.M.; Flegel, W.A. COVID-19 antibody detection and assay performance using red cell agglutination. Microbiol. Spectr. 2021, 9, e0083021. [Google Scholar] [CrossRef]
- Catimel, B.; Wilson, K.M.; Kemp, B.E. Kinetics of the autologous red cell agglutination test. J. Immunol. Methods 1993, 165, 183–192. [Google Scholar] [CrossRef]
- Kemp, B.E.; Rylatt, D.B.; Bundesen, P.G.; Doherty, R.R.; McPhee, D.A.; Stapleton, D.; Cottis, L.E.; Wilson, K.; John, M.A.; Khan, J.M.; et al. Autologous red cell agglutination assay for HIV-1 antibodies: Simplified test with whole blood. Science 1988, 241, 1352–1354. [Google Scholar] [CrossRef]
- Wilson, K.M.; Gerometta, M.; Rylatt, D.B.; Bundesen, P.G.; McPhee, D.A.; Hillyard, C.J.; Kemp, B.E. Rapid whole blood assay for HIV-1 seropositivity using an Fab-peptide conjugate. J. Immunol. Methods 1991, 138, 111–119. [Google Scholar] [CrossRef]
- Habib, I.; Smolarek, D.; Hattab, C.; Grodecka, M.; Hassanzadeh-Ghassabeh, G.; Muyldermans, S.; Sagan, S.; Gutiérrez, C.; Laperche, S.; Le-Van-Kim, C.; et al. V(H)H (nanobody) directed against human glycophorin A: A tool for autologous red cell agglutination assays. Anal. Biochem. 2013, 438, 82–89. [Google Scholar] [CrossRef]
- Townsend, A.; Rijal, P.; Xiao, J.; Tan, T.K.; Huang, K.-Y.A.; Schimanski, L.; Huo, J.; Gupta, N.; Rahikainen, R.; Matthews, P.C.; et al. A haemagglutination test for rapid detection of antibodies to SARS-CoV-2. Nat. Commun. 2021, 12, 1951. [Google Scholar] [CrossRef]
- Nguyen, D.; Xiao, J.; Simmonds, P.; Lamikanra, A.; Odon, V.; Ratcliff, J.; Townsend, A.; Roberts, D.; Harvala, H. Effects of SARS-CoV-2 strain variation on virus neutralisation titres: Therapeutic use of convalescent plasma. J. Infect. Dis. 2021, 204, S817–S824. [Google Scholar] [CrossRef]
- Kruse, R.; Huang, Y.; Lee, A.; Zhu, X.; Shrestha, R.; Laeyendecker, O.; Littlefield, K.; Pekosz, A.; Bloch, E.M.; Tobian, A.A.R.; et al. A hemagglutination-based, semi-quantitative test for point-of-care determination of SARS-CoV-2 antibody levels. J. Clin. Microbiol. 2021, 59, e01186-21. [Google Scholar] [CrossRef]
- Alves, D.; Curvello, R.; Henderson, E.; Kesarwani, V.; Walker, J.A.; Leguizamon, S.C.; McLiesh, H.; Raghuwanshi, V.S.; Samadian, H.; Wood, E.M.; et al. Rapid Gel Card Agglutination Assays for Serological Analysis Following SARS-CoV-2 Infection in Humans. ACS Sens. 2020, 5, 2596–2603. [Google Scholar] [CrossRef]
- Redecke, V.; Tawaratsumida, K.; Larragoite, E.T.; Williams, E.S.C.P.; Planelles, V.; Spivak, A.M.; Hirayama, L.; Elgort, M.; Swenson, S.; Smith, R.; et al. A rapid and affordable point of care test for antibodies against SARS-CoV-2 based on hemagglutination and artificial intelligence interpretation. Sci. Rep. 2021, 11, 24507. [Google Scholar] [CrossRef]
- Khawaja, E.A.; Shasoddin, E.; Ferro Desideri, L.; Tovani-Palone, M.R. Infection of red blood cells by SARS-CoV-2: New evidence. Einstein 2021, 19, eCE6285. [Google Scholar] [CrossRef]
- Thomas, T.; Stefanoni, D.; Dzieciatkowska, M. Evidence of structural protein damage and membrane lipid remodeling in red blood cells from COVID-19 patients. J. Proteome Res. 2020, 19, 4455–4469. [Google Scholar] [CrossRef]
- Esmail, S.; Knauer, M.J.; Abdoh, H.; Voss, C.; Chin-Yee, B.; Stogios, P.; Seitova, A.; Hutchinson, A.; Yusifov, F.; Skarina, T.; et al. Rapid and accurate agglutination-based testing for SARS-CoV-2 antibodies. Cell Rep. Methods 2021, 1, 100011. [Google Scholar] [CrossRef]
- Scheim, D. From Cold to Killer: How SARS-CoV-2 Evolved without Hemagglutinin Esterase to Agglutinate, Then Clot Blood Cells in Pulmonary and Systemic Microvasculature. SSRN 2020. [Google Scholar] [CrossRef]
- Mabey, D.; Peeling, R.W.; Ustianowski, A.; Perkins, M.D. Diagnostics for the developing world. Nat. Rev. Microbiol. 2004, 2, 231–240. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Focosi, D.; Franchini, M.; Maggi, F. Modified Hemagglutination Tests for COVID-19 Serology in Resource-Poor Settings: Ready for Prime-Time? Vaccines 2022, 10, 406. https://doi.org/10.3390/vaccines10030406
Focosi D, Franchini M, Maggi F. Modified Hemagglutination Tests for COVID-19 Serology in Resource-Poor Settings: Ready for Prime-Time? Vaccines. 2022; 10(3):406. https://doi.org/10.3390/vaccines10030406
Chicago/Turabian StyleFocosi, Daniele, Massimo Franchini, and Fabrizio Maggi. 2022. "Modified Hemagglutination Tests for COVID-19 Serology in Resource-Poor Settings: Ready for Prime-Time?" Vaccines 10, no. 3: 406. https://doi.org/10.3390/vaccines10030406
APA StyleFocosi, D., Franchini, M., & Maggi, F. (2022). Modified Hemagglutination Tests for COVID-19 Serology in Resource-Poor Settings: Ready for Prime-Time? Vaccines, 10(3), 406. https://doi.org/10.3390/vaccines10030406






