Intentions Regarding COVID-19 Vaccination in Females Aged 15–49 Years
Abstract
:1. Introduction
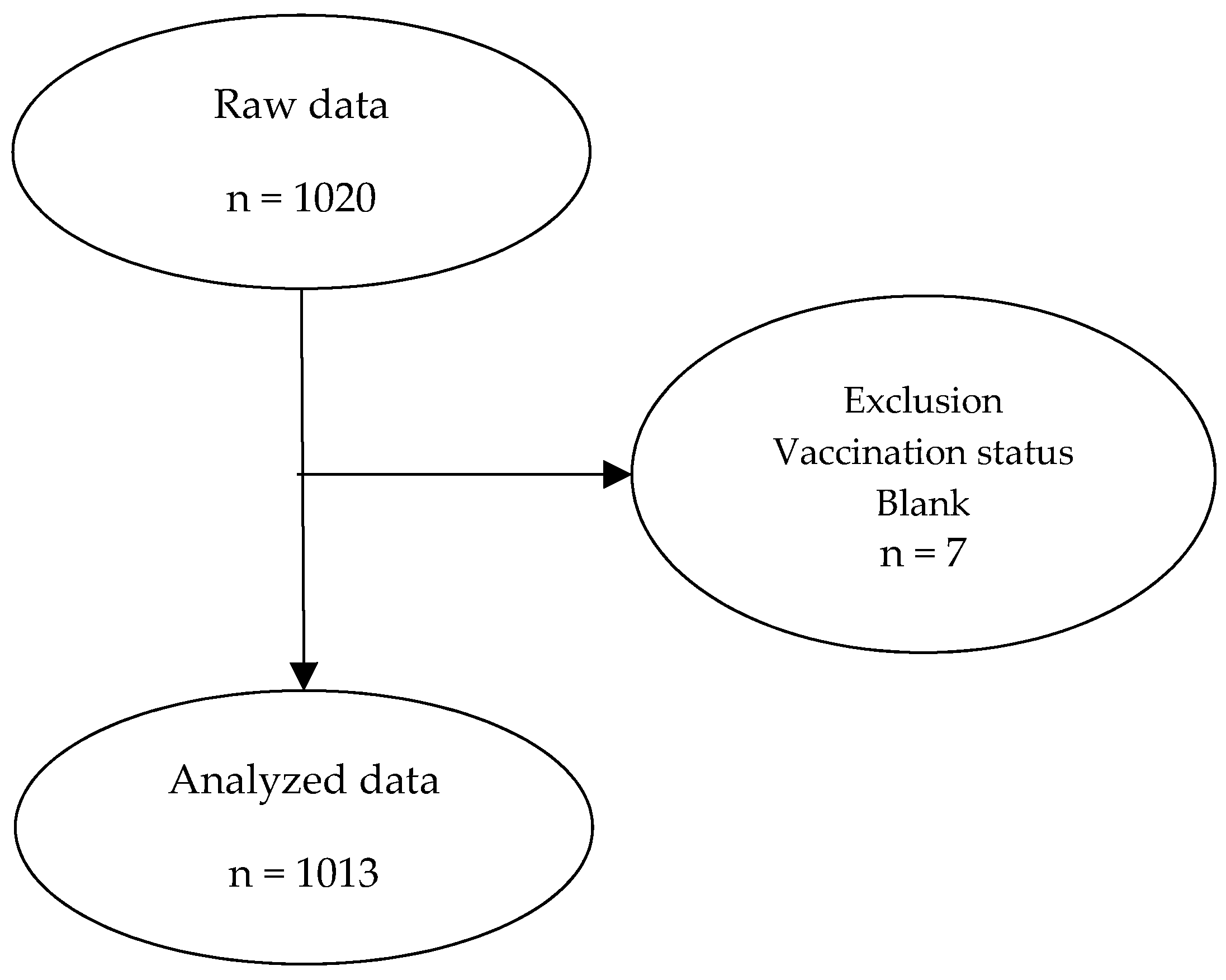
2. Materials and Methods
2.1. Measures
2.2. Analyses
3. Results
3.1. Vaccination Status and Proportion of Those Who Answered “I Will Not Get Vaccinated in the First Place”
3.2. Reasons for Giving the Answer “I Will Not Get Vaccinated in the First Place”
3.3. Intention Regarding the Third Vaccination among Those Who Answered, “My Second Vaccination Is Complete”
3.4. Reasons for Giving the Answer, “I Will Not Get Vaccinated” or, “I Am Not Sure”, Regarding the Third Vaccination
4. Major Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ministry of Health, Labor and Welfare. Suicide Situation in 2020. Available online: https://www.mhlw.go.jp/content/R2kakutei-01.pdf (accessed on 23 December 2021). (In Japanese)
- Ministry of Health, Labor and Welfare. About Vaccine Development Status. Available online: https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/0000121431_00223.html (accessed on 23 December 2021). (In Japanese)
- Yoda, T.; Katsuyama, H. Willingness to receive COVID-19 vaccination in Japan. Vaccines 2021, 9, 48. [Google Scholar] [CrossRef] [PubMed]
- Machida, M.; Nakamura, I.; Kojima, T.; Saito, R.; Nakaya, T.; Hanibuchi, T.; Takamiya, T.; Odagiri, Y.; Fukushima, N.; Kikuchi, H.; et al. Acceptance of a COVID-19 vaccine in Japan during the COVID-19 pandemic. Vaccines 2021, 9, 210. [Google Scholar] [CrossRef] [PubMed]
- Ishimaru, T.; Okawara, M.; Ando, H.; Hino, A.; Nagata, T.; Tateishi, S.; Tsuji, M.; Matsuda, S.; Fujino, Y.; CORoNaWork Project. Gender differences in the determinants of willingness to get the COVID-19 vaccine among the working-age population in Japan. Hum. Vaccin. Immunother. 2021, 17, 3975–3981. [Google Scholar] [CrossRef] [PubMed]
- Neumann-Böhme, S.; Varghese, N.E.; Sabat, I.; Barros, P.P.; Brouwer, W.; van Exel, J.; Schreyögg, J.; Stargardt, T. Once we have it, will we use it? A European survey on willingness to be vaccinated against COVID-19. Eur. J. Health Econ. 2020, 21, 977–982. [Google Scholar] [CrossRef] [PubMed]
- Kadoya, Y.; Watanapongvanich, S.; Yuktadatta, P.; Putthinun, P.; Lartey, S.T.; Khan, M. Willing or hesitant? A socioeconomic study on the potential acceptance of COVID-19 vaccine in Japan. Int. J. Environ. Res. Public Health 2021, 18, 4864. [Google Scholar] [CrossRef] [PubMed]
- Latkin, C.A.; Dayton, L.; Yi, G.; Colon, B.; Kong, X. Mask usage, social distancing, racial, and gender correlates of COVID-19 vaccine intentions among adults in the US. PLoS ONE 2021, 16, e0246970. [Google Scholar] [CrossRef] [PubMed]
- Freeman, D.; Loe, B.S.; Yu, L.M.; Freeman, J.; Chadwick, A.; Vaccari, C.; Shanyinde, M.; Harris, V.; Waite, F.; Rosebrock, L.; et al. Effects of different types of written vaccination information on COVID-19 vaccine hesitancy in the UK (OCEANS-III): A single-blind, parallel-group, randomized controlled trial. Lancet Public Health 2021, 6, e416–e427. [Google Scholar] [CrossRef]
- Ehde, D.M.; Roberts, M.K.; Humbert, A.T.; Herring, T.E.; Alschuler, K.N. COVID-19 vaccine hesitancy in adults with multiple sclerosis in the United States: A follow up survey during the initial vaccine rollout in 2021. Mult. Scler. Relat. Disord. 2021, 54, 103163. [Google Scholar] [CrossRef] [PubMed]
- Yahia, A.; Alshahrani, A.M.; Alsulmi, W.; Alqarni, M.; Abdulrahim, T.; Heba, W.; Alqarni, T.; Alharthi, K.; Buhran, A. Determinants of COVID-19 vaccine acceptance and hesitancy: A cross-sectional study in Saudi Arabia. Hum. Vaccin. Immunother. 2021, in press. [Google Scholar] [CrossRef] [PubMed]
- Reiter, P.L.; Pennell, M.L.; Katz, M.L. Acceptability of a COVID-19 vaccine among adults in the United States: How many people would get vaccinated? Vaccine 2020, 38, 6500–6507. [Google Scholar] [CrossRef] [PubMed]
- Wake, A.D. The willingness to receive COVID-19 vaccine and its associated factors: “Vaccination refusal could prolong the war of this pandemic”—A systematic review. Risk Manag. Healthc. Policy 2021, 14, 2609–2623. [Google Scholar] [CrossRef] [PubMed]
- Sallam, M. COVID-19 vaccine hesitancy worldwide: A concise systematic review of vaccine acceptance rates. Vaccines 2021, 9, 160. [Google Scholar] [CrossRef] [PubMed]
- De Figueiredo, A.; Simas, C.; Karafillakis, E.; Paterson, P.; Larson, H.J. Mapping global trends in vaccine confidence and investigating barriers to vaccine uptake: A large-scale retrospective temporal modelling study. Lancet 2020, 396, 898–908. [Google Scholar] [CrossRef]
- Hara, M.; Ishibashi, M.; Nakane, A.; Nakano, T.; Hirota, Y. Differences in COVID-19 vaccine acceptance, hesitancy, and confidence between healthcare workers and the general population in Japan. Vaccines 2021, 9, 1389. [Google Scholar] [CrossRef] [PubMed]
- Ragusa, R.; Bertino, G.; Bruno, A.; Frazzetto, E.; Cicciu, F.; Giorgianni, G.; Lupo, L. Evaluation of health status in patients with hepatitis c treated with and without interferon. Health Qual. Life Outcomes 2018, 16, 17. [Google Scholar] [CrossRef]
- Male, V. Menstrual changes after COVID-19 vaccination. BMJ 2021, 374, n2211. [Google Scholar] [CrossRef]
- Speed, B. Young Women Are the Unlikely New Face of COVID-19 Vaccine Resistance. i News 6 January 2021. Available online: https://inews.co.uk/news/health/coronavirus-latest-experts-debunk-vaccine-fertility-myths-women-819783 (accessed on 30 January 2022).
- Yagi, A.; Ueda, Y.; Tanaka, Y.; Nakae, R.; Kakubari, R.; Morimoto, A.; Terai, Y.; Ohmichi, M.; Ichimura, T.; Sumi, T.; et al. Time-dependent changes of the intention of mothers in Japan to inoculate their daughters with the HPV vaccine after suspension of governmental recommendation. Hum. Vaccines Immunother. 2018, 14, 2497–2502. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pharmaceuticals and Medical Devices Agency. Comirnaty Intramuscular Injection Pfizer Japan Inc. Report on Special Approval for Emergency 2021. Available online: https://www.pmda.go.jp/drugs/2021/P20210212001/672212000_30300AMX00231_A100_5.pdf (accessed on 23 December 2021). (In Japanese)
- Hamed, T. Determining sample size; how to calculate survey sample size. Int. J. Econ. Manag. Syst. 2017, 2, 237–239. [Google Scholar]
- Bartlett, J.E.; Kotrlik, J.; Higgins, C. Organizational research: Determining appropriate sample size in survey research. Inf. Technol. Learn Perform. J. 2001, 19, 43–50. [Google Scholar]
| Total | 15–19 Years | 20–29 Years | 30–39 Years | 40–49 Years | p-Value | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n = 1013 (%) | n = 250 (%) | n = 257 (%) | n = 252 (%) | n = 254 (%) | |||||||
| First vaccination is complete | 234 | (23.0) | 59 | (23.6) | 53 | (20.6) | 61 | (24.2) | 61 | (24.0) | 0.003 |
| Second vaccination is complete | 350 | (34.6) | 65 | (26.0) | 87 | (33.9) | 88 | (34.9) | 110 | (43.3) | |
| No reservation | 257 | (25.4) | 82 | (32.8) | 71 | (27.6) | 57 | (22.6) | 47 | (18.5) | |
| I will not get vaccinated | 172 | (17.0) | 44 | (17.6) | 46 | (17.9) | 46 | (18.3) | 36 | (14.2) | |
| I will not get vaccinated | 172 | (17.0) | 44 | (17.6) | 46 | (17.9) | 46 | (18.3) | 36 | (14.2) | 0.574 |
| Other | 841 | (83.0) | 206 | (82.4) | 211 | (82.1) | 206 | (81.7) | 218 | (85.8) | |
| Total | 15–19 Years | 20–29 Years | 30–39 Years | 40–49 Years | p-Value | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n = 172 (%) | n = 44 (%) | n = 46 (%) | n = 46 (%) | n = 36 (%) | |||||||
| I am allergic to vaccines/I have other physical reasons. | |||||||||||
| Agree | 24 | (14.0) | 5 | (11.4) | 5 | (10.9) | 6 | (13.0) | 8 | (22.2) | 0.481 |
| Disagree | 148 | (86.0) | 39 | (88.6) | 41 | (89.1) | 40 | (87.0) | 28 | (77.8) | |
| I do not like needles/injections. | |||||||||||
| Agree | 12 | (7.0) | 9 | (20.5) | 2 | (4.3) | 0 | (0.0) | 1 | (2.8) | <0.001 |
| Disagree | 160 | (93.0) | 35 | (79.5) | 44 | (95.7) | 46 | (100.0) | 35 | (97.2) | |
| I am not concerned about getting seriously ill from the coronavirus/I do not need it. | |||||||||||
| Agree | 16 | (9.3) | 3 | (6.8) | 4 | (8.7) | 3 | (6.5) | 6 | (16.7) | 0.431 |
| Disagree | 156 | (90.7) | 41 | (93.2) | 42 | (91.3) | 43 | (93.5) | 30 | (83.3) | |
| I will not have time to get vaccinated | |||||||||||
| Agree | 1 | (0.6) | 1 | (2.3) | 0 | (0.0) | 0 | (0.0) | 0 | (0.0) | 0.433 |
| Disagree | 171 | (99.4) | 43 | (97.7) | 46 | (100.0) | 46 | (100.0) | 36 | (100.0) | |
| I would be concerned about getting infected with the coronavirus/other disease from the vaccine/I am worried about its safety. | |||||||||||
| Agree | 44 | (25.6) | 7 | (15.9) | 15 | (32.6) | 12 | (26.1) | 10 | (27.8) | 0.306 |
| Disagree | 128 | (74.4) | 37 | (84.1) | 31 | (67.4) | 34 | (73.9) | 26 | (72.2) | |
| I am afraid/anxious. | |||||||||||
| Agree | 20 | (11.6) | 11 | (25.0) | 4 | (8.7) | 5 | (10.9) | 0 | (0.0) | 0.002 |
| Disagree | 152 | (88.4) | 33 | (75.0) | 42 | (91.3) | 41 | (89.1) | 36 | (100.0) | |
| I would be concerned about side effects from the vaccine. | |||||||||||
| Agree | 38 | (22.1) | 13 | (29.5) | 9 | (19.6) | 11 | (23.9) | 5 | (13.9) | 0.359 |
| Disagree | 134 | (77.9) | 31 | (70.5) | 37 | (80.4) | 35 | (76.1) | 31 | (86.1) | |
| I do not think vaccines work very well. | |||||||||||
| Agree | 11 | (6.4) | 1 | (2.3) | 4 | (8.7) | 4 | (8.7) | 2 | (5.6) | 0.490 |
| Disagree | 161 | (93.6) | 43 | (97.7) | 42 | (91.3) | 42 | (91.3) | 34 | (94.4) | |
| The coronavirus outbreak is not as serious as some people say it is/There is no need for society. | |||||||||||
| Agree | 0 | (0.0) | 0 | (0.0) | 0 | (0.0) | 0 | (0.0) | 0 | (0.0) | NA |
| Disagree | 172 | (100.0) | 44 | (100.0) | 46 | (100.0) | 46 | (100.0) | 36 | (100.0) | |
| Blank/No reasons/Bad answer | |||||||||||
| Agree | 20 | (11.6) | 3 | (6.8) | 6 | (13.0) | 7 | (15.2) | 4 | (11.1) | 0.621 |
| Disagree | 152 | (88.4) | 41 | (93.2) | 40 | (87.0) | 39 | (84.8) | 32 | (88.9) | |
| Others | |||||||||||
| Agree | 9 | (5.2) | 4 | (9.1) | 1 | (2.2) | 3 | (6.5) | 1 | (2.8) | 0.413 |
| Disagree | 163 | (94.8) | 40 | (90.9) | 45 | (97.8) | 43 | (93.5) | 35 | (97.2) | |
| Total | 15–19 Years | 20–29 Years | 30–39 Years | 40–49 Years | p-Value | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n = 348 (%) | n = 65 (%) | n = 87 (%) | n = 88 (%) | n = 108 (%) | |||||||
| I will get vaccinated. | 234 | (67.2) | 38 | (58.5) | 55 | (63.2) | 65 | (73.9) | 76 | (70.4) | 0.212 |
| I will not get vaccinated. | 12 | (3.5) | 4 | (6.1) | 4 | (4.6) | 3 | (3.4) | 1 | (0.9) | |
| I am not sure. | 102 | (29.3) | 23 | (35.4) | 28 | (32.2) | 20 | (22.7) | 31 | (28.7) | |
| Total | 15–19 Years | 20–29 Years | 30–39 Years | 40–49 Years | p-Value | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n = 114 (%) | n = 27 (%) | n = 32 (%) | n = 23 (%) | n = 32 (%) | |||||||
| I am allergic to vaccines/I have other physical reasons. | |||||||||||
| Agree | 1 | (0.9) | 0 | (0.0) | 0 | (0.0) | 0 | (0.0) | 1 | (3.1) | 0.464 |
| Disagree | 113 | (99.1) | 27 | (100.0) | 32 | (100.0) | 23 | (100.0) | 31 | (96.9) | |
| I do not like needles/injections. | |||||||||||
| Agree | 1 | (0.9) | 0 | 0.0) | 0 | 0.0) | 1 | (0.0) | 0 | (0.0) | 0.357 |
| Disagree | 113 | (99.1) | 27 | (100.0) | 32 | 100.0) | 22 | (100.0) | 32 | (100.0) | |
| I am not concerned about getting seriously ill from the coronavirus/I do not need it. | |||||||||||
| Agree | 10 | (8.8) | 2 | (7.4) | 3 | (9.4) | 4 | (17.4) | 1 | (3.1) | 0.328 |
| Disagree | 104 | (91.2) | 25 | (92.6) | 29 | (90.6) | 19 | (82.6) | 31 | (96.9) | |
| I will not have time to get vaccinated. | |||||||||||
| Disagree | 114 | (100.0) | 27 | (100.0) | 32 | (100.0) | 23 | (100.0) | 32 | (100.0) | NA |
| I would be concerned about getting infected with the coronavirus/other disease from the vaccine/I am worried about its safety. | |||||||||||
| Agree | 8 | (7.0) | 3 | (11.1) | 1 | (3.1) | 2 | (8.7) | 2 | (6.3) | 0.650 |
| Disagree | 106 | (93.0) | 24 | (88.9) | 31 | (96.9) | 21 | (91.3) | 30 | (93.8) | |
| I am afraid/anxious. | |||||||||||
| Agree | 1 | (0.9) | 0 | (0.0) | 0 | (0.0) | 1 | (4.3) | 0 | (0.0) | 0.357 |
| Disagree | 113 | (99.1) | 27 | (100.0) | 32 | (100.0) | 22 | (95.7) | 32 | (100.0) | |
| I would be concerned about side effects from the vaccine. | |||||||||||
| Agree | 37 | (32.5) | 9 | (33.3) | 9 | (28.1) | 9 | (39.1) | 10 | (31.2) | 0.858 |
| Disagree | 77 | (67.5) | 18 | (66.7) | 23 | (71.9) | 14 | (60.9) | 22 | (68.8) | |
| I do not think vaccines work very well. | |||||||||||
| Agree | 7 | (6.1) | 0 | (0.0) | 3 | (9.4) | 1 | (4.3) | 3 | (9.4) | 0.206 |
| Disagree | 107 | (93.9) | 27 | (100.0) | 29 | (90.6) | 22 | (95.7) | 29 | (90.6) | |
| The coronavirus outbreak is not as serious as some people say it is/There is no need for society. | |||||||||||
| Disagree | 114 | (100.0) | 27 | (100.0) | 32 | (100.0) | 23 | (100.0) | 32 | (100.0) | NA |
| Blank/No reasons/Bad answer | |||||||||||
| Agree | 16 | (14.0) | 2 | (7.4) | 9 | (28.1) | 1 | (4.3) | 4 | (12.5) | 0.049 |
| Disagree | 98 | (86.0) | 25 | (92.6) | 23 | (71.9) | 22 | (95.7) | 28 | (87.5) | |
| Others | |||||||||||
| Agree | 15 | (13.2) | 3 | (11.1) | 3 | (9.4) | 1 | (4.3) | 8 | (25.0) | 0.121 |
| Disagree | 99 | (86.8) | 24 | (88.9) | 29 | (90.6) | 22 | (95.7) | 24 | (75.0) | |
| It depends on what people around me do/There is not enough information to make a decision. | |||||||||||
| 26 | (22.8) | 9 | (33.3) | 4 | (12.5) | 5 | (21.7) | 8 | (25.0) | 0.277 | |
| 88 | (77.2) | 18 | (66.7) | 28 | (87.5) | 18 | (78.3) | 24 | (75.0) | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kajiwara, S.; Akiyama, N.; Ohta, M. Intentions Regarding COVID-19 Vaccination in Females Aged 15–49 Years. Vaccines 2022, 10, 336. https://doi.org/10.3390/vaccines10020336
Kajiwara S, Akiyama N, Ohta M. Intentions Regarding COVID-19 Vaccination in Females Aged 15–49 Years. Vaccines. 2022; 10(2):336. https://doi.org/10.3390/vaccines10020336
Chicago/Turabian StyleKajiwara, Shihoko, Naomi Akiyama, and Michio Ohta. 2022. "Intentions Regarding COVID-19 Vaccination in Females Aged 15–49 Years" Vaccines 10, no. 2: 336. https://doi.org/10.3390/vaccines10020336
APA StyleKajiwara, S., Akiyama, N., & Ohta, M. (2022). Intentions Regarding COVID-19 Vaccination in Females Aged 15–49 Years. Vaccines, 10(2), 336. https://doi.org/10.3390/vaccines10020336





