Modulation of Inflammatory Signaling Molecules in Bordetella pertussis Antigen-Challenged Human Monocytes in Presence of Adrenergic Agonists
Abstract
1. Introduction
2. Materials and Methods
2.1. Chemicals
2.2. Cell Culture and Treatments
2.3. Fluorescence Multiplex Bead-Based Immune Assay (FMIA)
2.4. Prostanoids Extraction and Quantification by UPLC–MS/MS
2.5. Statistical Analysis
3. Results
3.1. THP-1 Cell Expression of Chemokine CCL20 (MIP-3α) in Response to LPS or B. pertussis Antigens, BscF and Tdap Are Modulated by Adrenergic Agonists
3.2. THP-1 Cell Expression of Chemokine CXCL10 (IP-10) in Response to LPS or B. pertussis Antigens, BscF and Tdap Are Modulated by Adrenergic Agonists
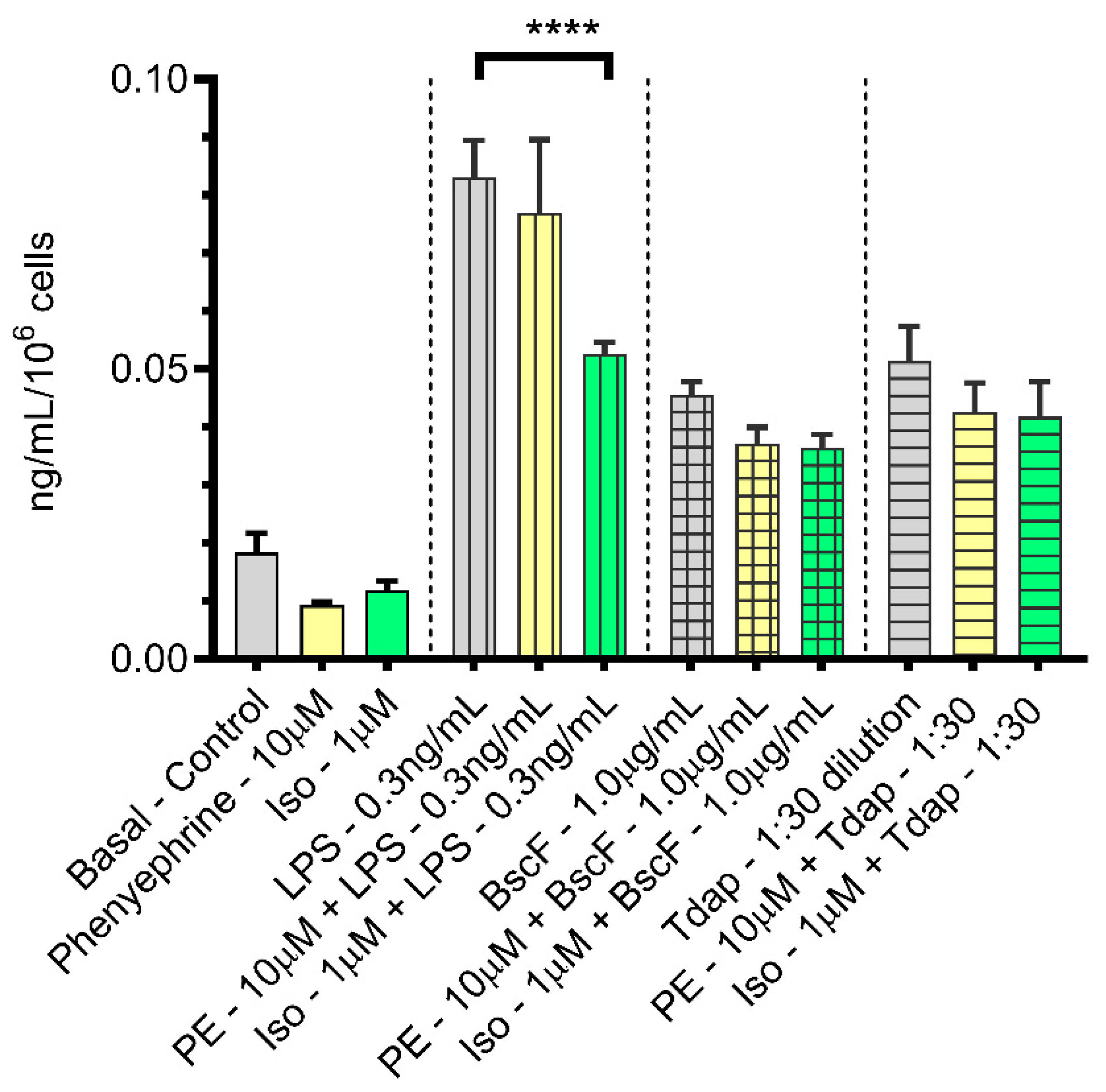
3.3. Immunomodulation of PGE2 Expression in THP-1 Cells in the Presence of Adrenergic Agonists
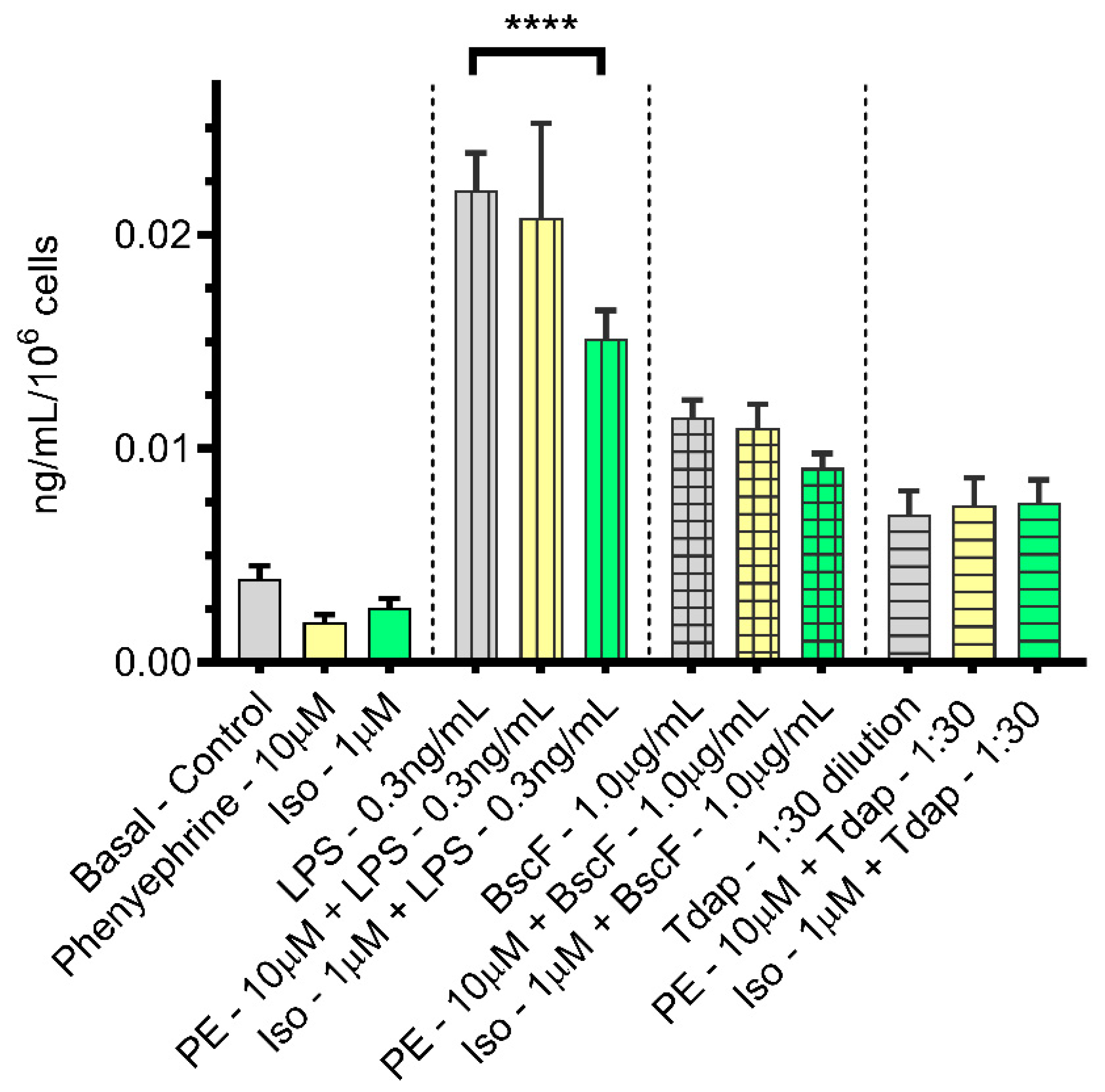
3.4. Immunomodulation of PGF2α Expression in THP-1 Cells Treated with LPS or B. pertussis Antigens in the Presence of Adrenergic Agonists
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Hervé, C.; Laupèze, B.; Del Giudice, G.; Didierlaurent, A.M.; Tavares Da Silva, F. The how’s and what’s of vaccine reactogenicity. NPJ Vaccines 2019, 4, 39. [Google Scholar] [CrossRef] [PubMed]
- Pollard, A.J.; Bijker, E.M. A guide to vaccinology: From basic principles to new developments. Nat. Rev. Immunol. 2021, 21, 83–100. [Google Scholar] [CrossRef] [PubMed]
- Burdin, N.; Handy, L.K.; Plotkin, S.A. What Is Wrong with Pertussis Vaccine Immunity? The Problem of Waning Effectiveness of Pertussis Vaccines. Cold Spring Harb. Perspect. Biol. 2017, 9, a029454. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.; He, Q. Immune persistence after pertussis vaccination. Hum. Vaccines Immunother. 2017, 13, 744–756. [Google Scholar] [CrossRef]
- Alvine, T.D.; Bradley, D.S.; Nilles, M.L. Mouse Immunization with Purified Needle Proteins from Type III Secretion Systems and the Characterization of the Immune Response to These Proteins. Methods Mol. Biol. 2017, 1531, 193–201. [Google Scholar]
- Alvine, T.D.; Knopick, P.L.; Kumar, M.A.; Nilles, M.L.; Bradley, D.S. BscF from Bordetella pertussis provides advantageous adjuvant activity when paired with the acellular pertussis vaccine: Enhanced Th1/Th17 pertussis-specific immune response. J. Immunol. 2016, 196 (Suppl. S1), 146.5. [Google Scholar]
- Xiao, T.S. Innate immunity and inflammation. Cell. Mol. Immunol. 2017, 14, 1–3. [Google Scholar] [CrossRef]
- Cronkite, D.A.; Strutt, T.M. The Regulation of Inflammation by Innate and Adaptive Lymphocytes. J. Immunol. Res. 2018, 2018, 1467538. [Google Scholar] [CrossRef]
- Bhavya, B.C.; Haridas, M. Anti-inflammatory Molecules: Immune System Mediators. In Bioresources and Bioprocess in Biotechnology, Volume 2: Exploring Potential Biomolecules; Sugathan, S., Pradeep, N.S., Abdulhameed, S., Eds.; Springer: Singapore, 2017; pp. 235–268. [Google Scholar]
- Dinarello, C.A. Anti-inflammatory Agents: Present and Future. Cell 2010, 140, 935–950. [Google Scholar] [CrossRef]
- Riccardi, C.; Levi-Schaffer, F.; Tiligada, E. (Eds.) Mediators of Inflammation. In Immunopharmacology and Inflammation; Springer International Publishing: Cham, Switzerland, 2018; pp. 3–32. [Google Scholar]
- Hughes, C.E.; Nibbs, R.J.B. A guide to chemokines and their receptors. FEBS J. 2018, 285, 2944–2971. [Google Scholar] [CrossRef]
- Rahimi, R.A.; Luster, A.D. Chemokines: Critical Regulators of Memory T Cell Development, Maintenance, and Function. Adv. Immunol. 2018, 138, 71–98. [Google Scholar] [PubMed]
- Moser, B. T-Cell Memory: The Importance of Chemokine-Mediated Cell Attraction. Curr. Biol. 2006, 16, R504–R507. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Sander, W.J.; O’Neill, H.; Pohl, C.H. Prostaglandin E2 as a Modulator of Viral Infections. Front. Physiol. 2017, 8, 89. [Google Scholar] [CrossRef] [PubMed]
- Harizi, H. The Immunobiology of Prostanoid Receptor Signaling in Connecting Innate and Adaptive Immunity. BioMed Res. Int. 2013, 2013, 683405. [Google Scholar] [CrossRef] [PubMed]
- Hirata, T.; Narumiya, S. Prostanoids as Regulators of Innate and Adaptive Immunity. Adv. Immunol. 2012, 116, 143–174. [Google Scholar]
- Smyth, E.M.; Grosser, T.; Wang, M.; Yu, Y.; FitzGerald, G.A. Prostanoids in health and disease. J. Lipid Res. 2009, 50, S423–S428. [Google Scholar] [CrossRef]
- Leung, K.; Mihich, E. Prostaglandin modulation of development of cell-mediated immunity in culture. Nature 1980, 288, 597–600. [Google Scholar] [CrossRef]
- Sreeramkumar, V.; Fresno, M.; Cuesta, N. Prostaglandin E2 and T cells: Friends or foes? Immunol. Cell Biol. 2012, 90, 579–586. [Google Scholar] [CrossRef]
- Dragoş, D.; Tănăsescu, M.D. The effect of stress on the defense systems. J. Med. Life 2010, 3, 10–18. [Google Scholar]
- Scanzano, A.; Cosentino, M. Adrenergic regulation of innate immunity: A review. Front. Pharmacol. 2015, 6, 171. [Google Scholar] [CrossRef]
- Calcagni, E.; Elenkov, I. Stress system activity, innate and T helper cytokines, and susceptibility to immune-related diseases. Ann. N. Y. Acad. Sci. 2006, 1069, 62–76. [Google Scholar] [CrossRef] [PubMed]
- Sharma, D.; Farrar, J.D. Adrenergic regulation of immune cell function and inflammation. Semin. Immunopathol. 2020, 42, 709–717. [Google Scholar] [CrossRef]
- Sternberg, E.M. Neural regulation of innate immunity: A coordinated nonspecific host response to pathogens. Nat. Rev. Immunol. 2006, 6, 318–328. [Google Scholar] [CrossRef] [PubMed]
- Wieduwild, E.; Girard-Madoux, M.J.; Quatrini, L.; Laprie, C.; Chasson, L.; Rossignol, R.; Bernat, C.; Guia, S.; Ugolini, S. β2-adrenergic signals downregulate the innate immune response and reduce host resistance to viral infection. J. Exp. Med. 2020, 217, e20190554. [Google Scholar] [CrossRef] [PubMed]
- Agac, D.; Estrada, L.D.; Maples, R.; Hooper, L.V.; Farrar, J.D. The β2-adrenergic receptor controls inflammation by driving rapid IL-10 secretion. Brain Behav. Immun. 2018, 74, 176–185. [Google Scholar] [CrossRef] [PubMed]
- Nijhuis, L.E.; Olivier, B.J.; Dhawan, S.; Hilbers, F.W.; Boon, L.; Wolkers, M.C.; Samsom, J.N.; De Jonge, W.J. Adrenergic β2 Receptor Activation Stimulates Anti-Inflammatory Properties of Dendritic Cells In Vitro. PLoS ONE 2014, 9, e85086. [Google Scholar] [CrossRef] [PubMed]
- Grisanti, L.A.; Perez, D.M.; Porter, J.E. Modulation of Immune Cell Function by α1-Adrenergic Receptor Activation. Curr. Top. Membr. 2011, 67, 113–138. [Google Scholar]
- Grisanti, L.A.; Woster, A.P.; Dahlman, J.; Sauter, E.R.; Combs, C.K.; Porter, J.E. α1-Adrenergic Receptors Positively Regulate Toll-Like Receptor Cytokine Production from Human Monocytes and Macrophages. J. Pharmacol. Exp. Ther. 2011, 338, 648–657. [Google Scholar] [CrossRef]
- Grisanti, L.A.; Evanson, J.; Marchus, E.; Jorissen, H.; Woster, A.P.; DeKrey, W.; Sauter, D.R.; Combs, C.K.; Porter, J.E. Pro-inflammatory responses in human monocytes are beta1-adrenergic receptor subtype dependent. Mol. Immunol. 2010, 47, 1244–1254. [Google Scholar] [CrossRef]
- Poolman, J.T.; Hallander, H.O. Acellular pertussis vaccines and the role of pertactin and fimbriae. Expert Rev. Vaccines 2007, 6, 47–56. [Google Scholar] [CrossRef]
- Andreasen, C.; Carbonetti, N.H. Pertussis Toxin Inhibits Early Chemokine Production to Delay Neutrophil Recruitment in Response to Bordetella pertussis Respiratory Tract Infection in Mice. Infect. Immun. 2008, 76, 5139–5148. [Google Scholar] [CrossRef] [PubMed]
- Yougbare, I.; McTague, A.; He, L.; Choy, C.H.; Su, J.; Gajewska, B.; Azizi, A. Anti-FIM and Anti-FHA Antibodies Inhibit Bordetella pertussis Growth and Reduce Epithelial Cell Inflammation Through Bacterial Aggregation. Front. Immunol. 2020, 11, 605273. [Google Scholar] [CrossRef] [PubMed]
- Higgs, R.; Higgins, S.C.; Ross, P.J.; Mills, K.H.G. Immunity to the respiratory pathogen Bordetella pertussis. Mucosal Immunol. 2012, 5, 485–500. [Google Scholar] [CrossRef] [PubMed]
- Osei-Owusu, P.; Condry, D.L.J.; Toosky, M.; Roughead, W.; Bradley, D.S.; Nilles, M.L. The N Terminus of Type III Secretion Needle Protein YscF from Yersinia pestis Functions to Modulate Innate Immune Responses. Infect. Immun. 2015, 83, 1507–1522. [Google Scholar] [CrossRef][Green Version]
- Jessen, D.L.; Osei-Owusu, P.; Toosky, M.; Roughead, W.; Bradley, D.S.; Nilles, M.L. Type III Secretion Needle Proteins Induce Cell Signaling and Cytokine Secretion via Toll-Like Receptors. Infect. Immun. 2014, 82, 2300–2309. [Google Scholar] [CrossRef]
- Matson, J.S.; Durick, K.A.; Bradley, D.S.; Nilles, M.L. Immunization of mice with YscF provides protection from Yersinia pestis infections. BMC Microbiol. 2005, 5, 5–38. [Google Scholar] [CrossRef]
- Brose, S.A.; Baker, A.G.; Golovko, M.Y. A fast one-step extraction and UPLC-MS/MS analysis for E2/D 2 series prostaglandins and isoprostanes. Lipids 2013, 48, 411–419. [Google Scholar] [CrossRef]
- Kim, B.E.; Leung, D.Y.; Streib, J.E.; Boguniewicz, M.; Hamid, Q.A.; Howell, M.D. Macrophage inflammatory protein 3α deficiency in atopic dermatitis skin and role in innate immune response to vaccinia virus. J. Allergy Clin. Immunol. 2007, 119, 457–463. [Google Scholar] [CrossRef]
- Manes, T.D.; Shiao, S.L.; Dengler, T.J.; Pober, J.S. TCR signaling antagonizes rapid IP-10-mediated trans-endothelial migration of effector memory CD4+ T cells. J. Immunol. 2007, 178, 3237–3243. [Google Scholar] [CrossRef]
- Vazirinejad, R.; Ahmadi, Z.; Arababadi, M.K.; Hassanshahi, G.; Kennedy, D. The biological functions, structure and sources of CXCL10 and its outstanding part in the pathophysiology of multiple sclerosis. Neuroimmunomodulation 2014, 21, 322–330. [Google Scholar] [CrossRef]
- Kalinski, P. Regulation of Immune Responses by Prostaglandin E2. J. Immunol. 2012, 188, 21–28. [Google Scholar] [CrossRef] [PubMed]
- Harizi, H. Reciprocal crosstalk between dendritic cells and natural killer cells under the effects of PGE2 in immunity and immunopathology. Cell Mol. Immunol. 2013, 10, 213–221. [Google Scholar] [CrossRef] [PubMed]
- Newson, J.; Motwani, M.P.; Kendall, A.C.; Nicolaou, A.; Muccioli, G.G.; Alhouayek, M.; Bennett, M.; Merwe, R.V.D.; James, S.; De Maeyer, R.P.H.; et al. Inflammatory Resolution Triggers a Prolonged Phase of Immune Suppression through COX-1/mPGES-1-Derived Prostaglandin E(2). Cell Rep. 2017, 20, 3162–3175. [Google Scholar] [CrossRef]
- Agard, M.; Asakrah, S.; Morici, L.A. PGE2 suppression of innate immunity during mucosal bacterial infection. Front. Cell. Infect. Microbiol. 2013, 3, 45. [Google Scholar] [CrossRef] [PubMed]
- Chiappini, E.; Stival, A.; Galli, L.; De Martino, M. Pertussis re-emergence in the post-vaccination era. BMC Infect. Dis. 2013, 13, 151. [Google Scholar] [CrossRef] [PubMed]
- Saso, A.; Kampmann, B.; Roetynck, S. Vaccine-Induced Cellular Immunity against Bordetella pertussis: Harnessing Lessons from Animal and Human Studies to Improve Design and Testing of Novel Pertussis Vaccines. Vaccines 2021, 9, 877. [Google Scholar] [CrossRef]
- Holubová, J.; Staněk, O.; Brázdilová, L.; Mašín, J.; Bumba, L.; Gorringe, A.R.; Alexander, F.; Šebo, P. Acellular Pertussis Vaccine Inhibits Bordetella pertussis Clearance from the Nasal Mucosa of Mice. Vaccines 2020, 8, 695. [Google Scholar] [CrossRef]
- Springer, T.A. Traffic signals for lymphocyte recirculation and leukocyte emigration: The multistep paradigm. Cell 1994, 76, 301–314. [Google Scholar] [CrossRef]
- Xu, W.; Joo, H.; Clayton, S.; Dullaers, M.; Herve, M.C.; Blankenship, D.; De La Morena, M.T.; Balderas, R.; Picard, C.; Casanova, J.L.; et al. Macrophages induce differentiation of plasma cells through CXCL10/IP-10. J. Exp. Med. 2012, 209, 1813–1823. [Google Scholar] [CrossRef]
- Errea, A.; Moreno, G.; Sisti, F.; Fernandez, J.; Rumbo, M.; Hozbor, D.F. Mucosal innate response stimulation induced by lipopolysaccharide protects against Bordetella pertussis colonization. Med. Microbiol. Immunol. 2010, 199, 103–108. [Google Scholar] [CrossRef]
- Pulendran, B.; Ahmed, R. Immunological mechanisms of vaccination. Nat. Immunol. 2011, 12, 509–517. [Google Scholar] [CrossRef] [PubMed]
- Newton, K.; Dixit, V.M. Signaling in Innate Immunity and Inflammation. Cold Spring Harb. Perspect. Biol. 2012, 4, a006049. [Google Scholar] [CrossRef] [PubMed]
- Abdulkhaleq, L.A.; Assi, M.A.; Abdullah, R.; Zamri-Saad, M.; Taufiq-Yap, Y.H.; Hezmee, M.N.M. The crucial roles of inflammatory mediators in inflammation: A review. Veter World 2018, 11, 627–635. [Google Scholar] [CrossRef] [PubMed]
- Rouse, B.T.; Mueller, S.N. Host Defenses to Viruses. In Clinical Immunology; Elsevier: Amsterdam, The Netherlands, 2019; pp. 365–374.e1. [Google Scholar]
- Branco, A.C.C.C.; Yoshikawa, F.S.Y.; Pietrobon, A.J.; Sato, M.N. Role of Histamine in Modulating the Immune Response and Inflammation. Mediat. Inflamm. 2018, 2018, 9524075. [Google Scholar] [CrossRef]
- Turner, M.D.; Nedjai, B.; Hurst, T.; Pennington, D.J. Cytokines and chemokines: At the crossroads of cell signalling and inflammatory disease. Biochim. Biophys. Acta-Mol. Cell Res. 2014, 1843, 2563–2582. [Google Scholar] [CrossRef]
- Cohen, S.; Williamson, G.M. Stress and infectious disease in humans. Psychol. Bull. 1991, 109, 5–24. [Google Scholar] [CrossRef]
- Corbi, G.; Conti, V.; Russomanno, G.; Longobardi, G.; Furgi, G.; Filippelli, A.; Ferrara, N. Adrenergic signaling and oxidative stress: A role for sirtuins? Front. Physiol. 2013, 4, 324. [Google Scholar] [CrossRef]
- Kavelaars, A.; Ballieux, R.E.; Heijnen, C.J. In Vitro beta-adrenergic stimulation of lymphocytes induces the release of immunoreactive beta-endorphin. Endocrinology 1990, 126, 3028–3032. [Google Scholar] [CrossRef]
- Stolk, R.F.; Naumann, F.; van der Pasch, E.; Schouwstra, J.; Bressers, S.; van Herwaarden, A.E.; Gerretsen, J.; Schambergen, R.; Ruth, M.; van der Hoeven, H.G.; et al. Phenylephrine impairs host defence mechanisms to infection: A combined laboratory study in mice and translational human study. Br. J. Anaesth. 2021, 126, 652–664. [Google Scholar] [CrossRef]
- Stolk, R.F.; Van Der Poll, T.; Angus, D.C.; Van Der Hoeven, J.G.; Pickkers, P.; Kox, M. Potentially Inadvertent Immunomodulation: Norepinephrine Use in Sepsis. Am. J. Respir. Crit. Care Med. 2016, 194, 550–558. [Google Scholar] [CrossRef]
- Forte, E.; Panahi, M.; Baxan, N.; Ng, F.S.; Boyle, J.J.; Branca, J.; Bedard, O.; Hasham, M.G.; Benson, L.; Harding, S.E.; et al. Type 2 MI induced by a single high dose of isoproterenol in C57BL/6J mice triggers a persistent adaptive immune response against the heart. J. Cell. Mol. Med. 2020, 25, 229–243. [Google Scholar] [CrossRef] [PubMed]
- Szelenyi, J.; Selmeczy, Z.; Brozik, A.; Medgyesi, D.; Magocsi, M. Dual beta-adrenergic modulation in the immune system: Stimulus-dependent effect of isoproterenol on MAPK activation and inflammatory mediator production in macrophages. Neurochem. Int. 2006, 49, 94–103. [Google Scholar] [CrossRef] [PubMed]
- Etskovitz, H.; Anastasio, N.; Green, E.; May, M. Role of Evolutionary Selection Acting on Vaccine Antigens in the Re-Emergence of Bordetella pertussis. Diseases 2019, 7, 35. [Google Scholar] [CrossRef] [PubMed]
- Luu, L.; Octavia, S.; Zhong, L.; Raftery, M.J.; Sintchenko, V.; Lan, R. Comparison of the Whole Cell Proteome and Secretome of Epidemic Bordetella pertussis Strains From the 2008–2012 Australian Epidemic Under Sulfate-Modulating Conditions. Front. Microbiol. 2018, 9, 2851. [Google Scholar] [CrossRef] [PubMed]
- Luu, L.D.W.; Octavia, S.; Zhong, L.; Raftery, M.J.; Sintchenko, V.; Lan, R. Proteomic Adaptation of Australian Epidemic Bordetella pertussis. Proteomics 2018, 18, e1700237. [Google Scholar] [CrossRef] [PubMed]
- Williams, M.M.; Sen, K.; Weigand, M.; Skoff, T.H.; Cunningham, V.A.; Halse, T.A.; Tondella, M.L. CDC Pertussis Working Group Bordetella pertussis Strain Lacking Pertactin and Pertussis Toxin. Emerg. Infect. Dis. 2016, 22, 319–322. [Google Scholar] [CrossRef]
- Hovingh, E.S.; Mariman, R.; Solans, L.; Hijdra, D.; Hamstra, H.J.; Jongerius, I.; van Gent, M.; Mooi, F.; Locht, C.; Pinelli, E. Bordetella pertussis pertactin knock-out strains reveal immunomodulatory properties of this virulence factor. Emerg. Microbes Infect. 2018, 7, 1–13. [Google Scholar] [CrossRef]
- Lam, C.; Octavia, S.; Ricafort, L.; Sintchenko, V.; Gilbert, G.L.; Wood, N.; McIntyre, P.; Marshall, H.; Guiso, N.; Keil, A.D.; et al. Rapid Increase in Pertactin-deficient Bordetella pertussis Isolates, Australia. Emerg. Infect. Dis. 2014, 20, 626. [Google Scholar] [CrossRef]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Raihan, M.O.; Espelien, B.M.; McGregor, B.A.; Hanson, C.; Brishti, A.; Velaris, N.A.; Alvine, T.D.; Bradley, D.S.; Nilles, M.; Golovko, M.Y.; et al. Modulation of Inflammatory Signaling Molecules in Bordetella pertussis Antigen-Challenged Human Monocytes in Presence of Adrenergic Agonists. Vaccines 2022, 10, 321. https://doi.org/10.3390/vaccines10020321
Raihan MO, Espelien BM, McGregor BA, Hanson C, Brishti A, Velaris NA, Alvine TD, Bradley DS, Nilles M, Golovko MY, et al. Modulation of Inflammatory Signaling Molecules in Bordetella pertussis Antigen-Challenged Human Monocytes in Presence of Adrenergic Agonists. Vaccines. 2022; 10(2):321. https://doi.org/10.3390/vaccines10020321
Chicago/Turabian StyleRaihan, Md. Obayed, Brenna M. Espelien, Brett A. McGregor, Courtney Hanson, Afrina Brishti, Nathan A. Velaris, Travis D. Alvine, David S. Bradley, Matthew Nilles, Mikhail Y. Golovko, and et al. 2022. "Modulation of Inflammatory Signaling Molecules in Bordetella pertussis Antigen-Challenged Human Monocytes in Presence of Adrenergic Agonists" Vaccines 10, no. 2: 321. https://doi.org/10.3390/vaccines10020321
APA StyleRaihan, M. O., Espelien, B. M., McGregor, B. A., Hanson, C., Brishti, A., Velaris, N. A., Alvine, T. D., Bradley, D. S., Nilles, M., Golovko, M. Y., Hur, J., & Porter, J. E. (2022). Modulation of Inflammatory Signaling Molecules in Bordetella pertussis Antigen-Challenged Human Monocytes in Presence of Adrenergic Agonists. Vaccines, 10(2), 321. https://doi.org/10.3390/vaccines10020321







