COVID-19 among Czech Dentistry Students: Higher Vaccination and Lower Prevalence Compared to General Population Counterparts
Abstract
1. Introduction
2. Materials and Methods
2.1. Design
2.2. Instrument
2.3. Sample Size Relevancy
2.4. Data Collection
2.5. Analysis
3. Results
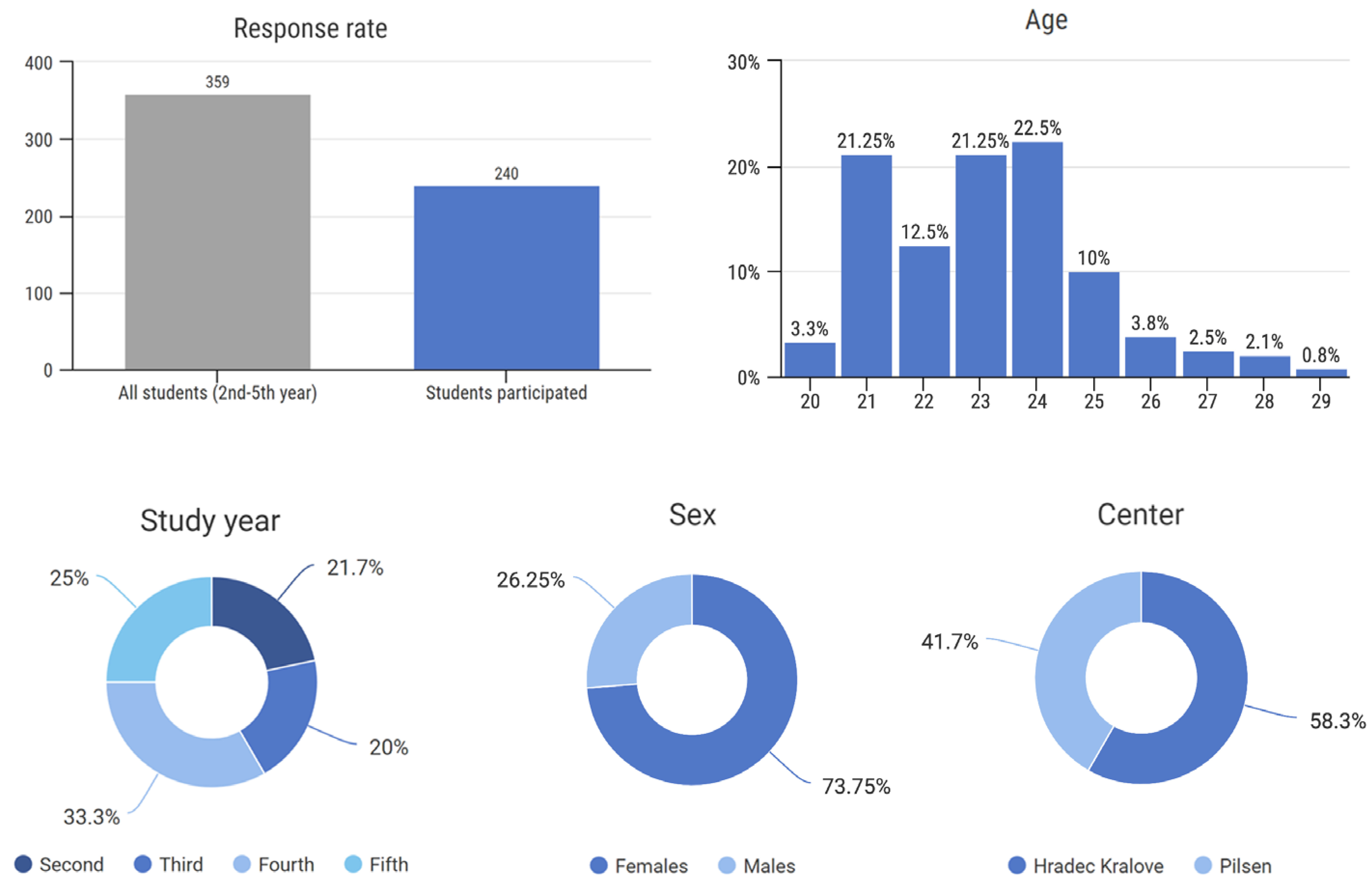
3.1. Response Rate and Center Distribution
3.2. Sex and Age Distribution
3.3. COVID-19 Infection
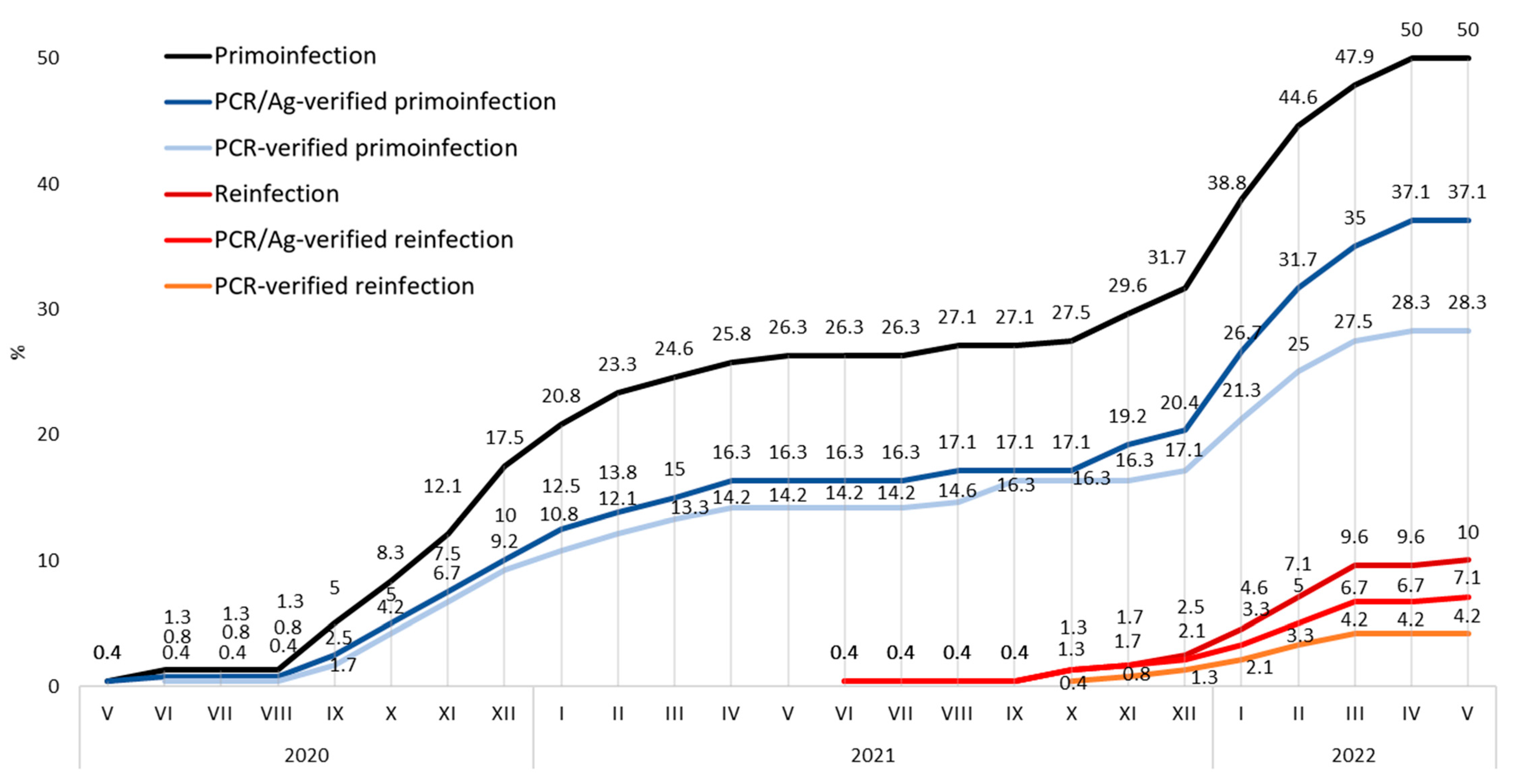
3.3.1. COVID-19 Prevalence
3.3.2. COVID-19 Prevalence Based on the Vaccination Status
3.3.3. COVID-19 Test-Verified Prevalence
3.3.4. Place of Infection
3.3.5. Hospitalization Rate
3.3.6. Incapacity Period
3.3.7. Long-Term Complications
3.3.8. Protective Measures Used during Work with Patients
3.4. COVID-19 Vaccination
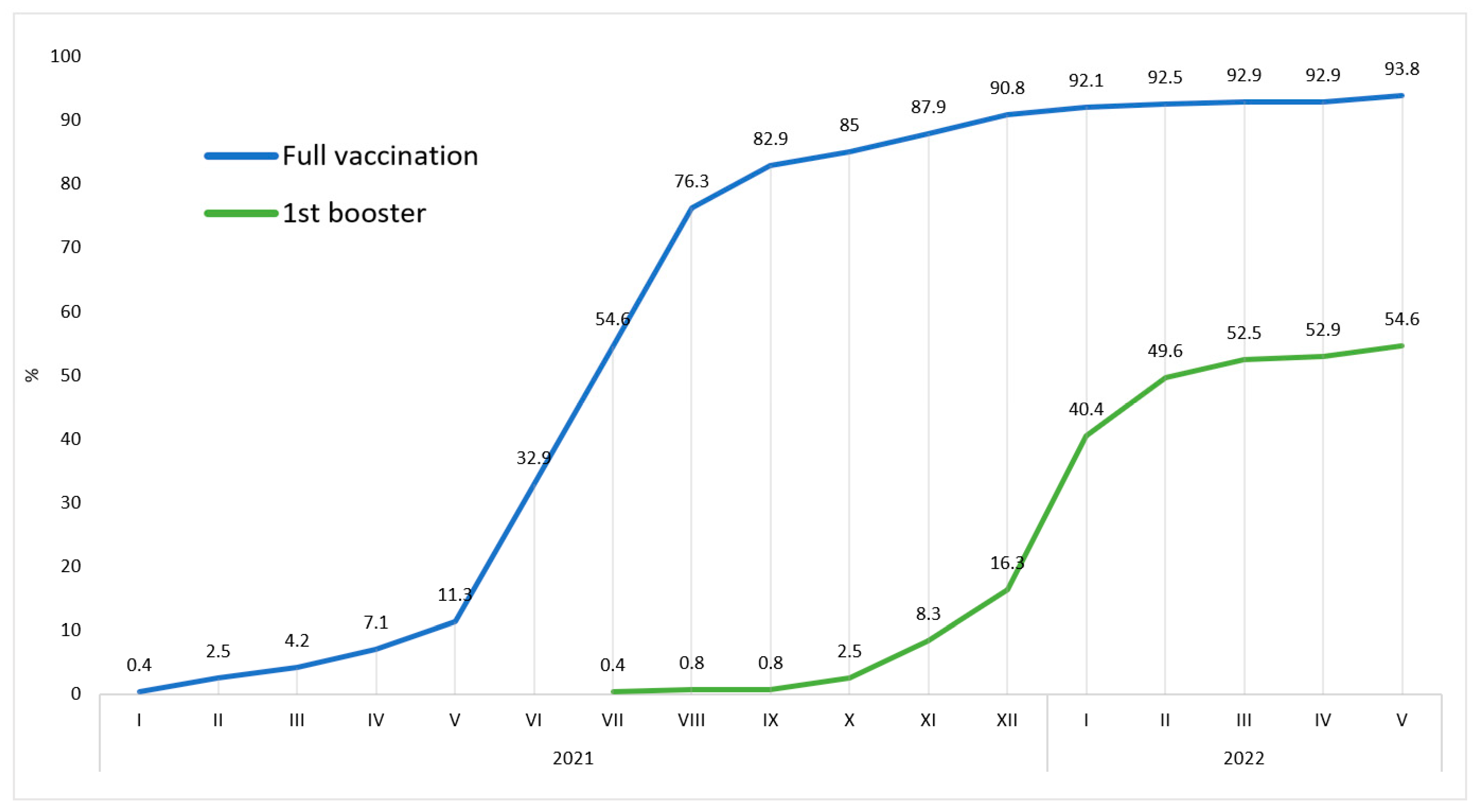
3.4.1. Vaccination Rate
3.4.2. Vaccine Type Used
3.4.3. Vaccination Adverse Effects
3.4.4. Reasons Leading to Avoiding COVID-19 Vaccination
3.4.5. COVID-19 Vaccination Penetration
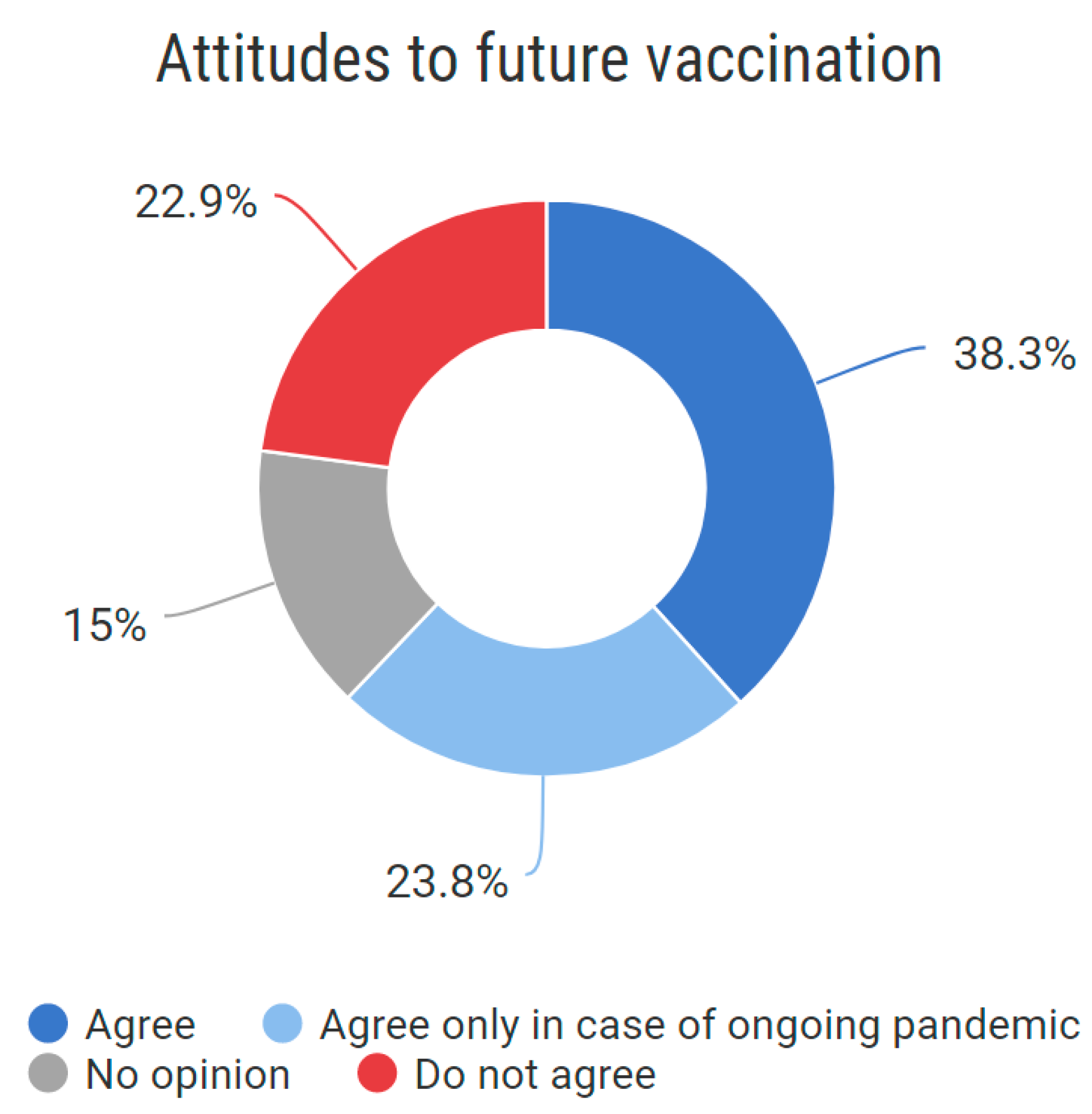
3.4.6. Future Approach to COVID-19 Vaccination
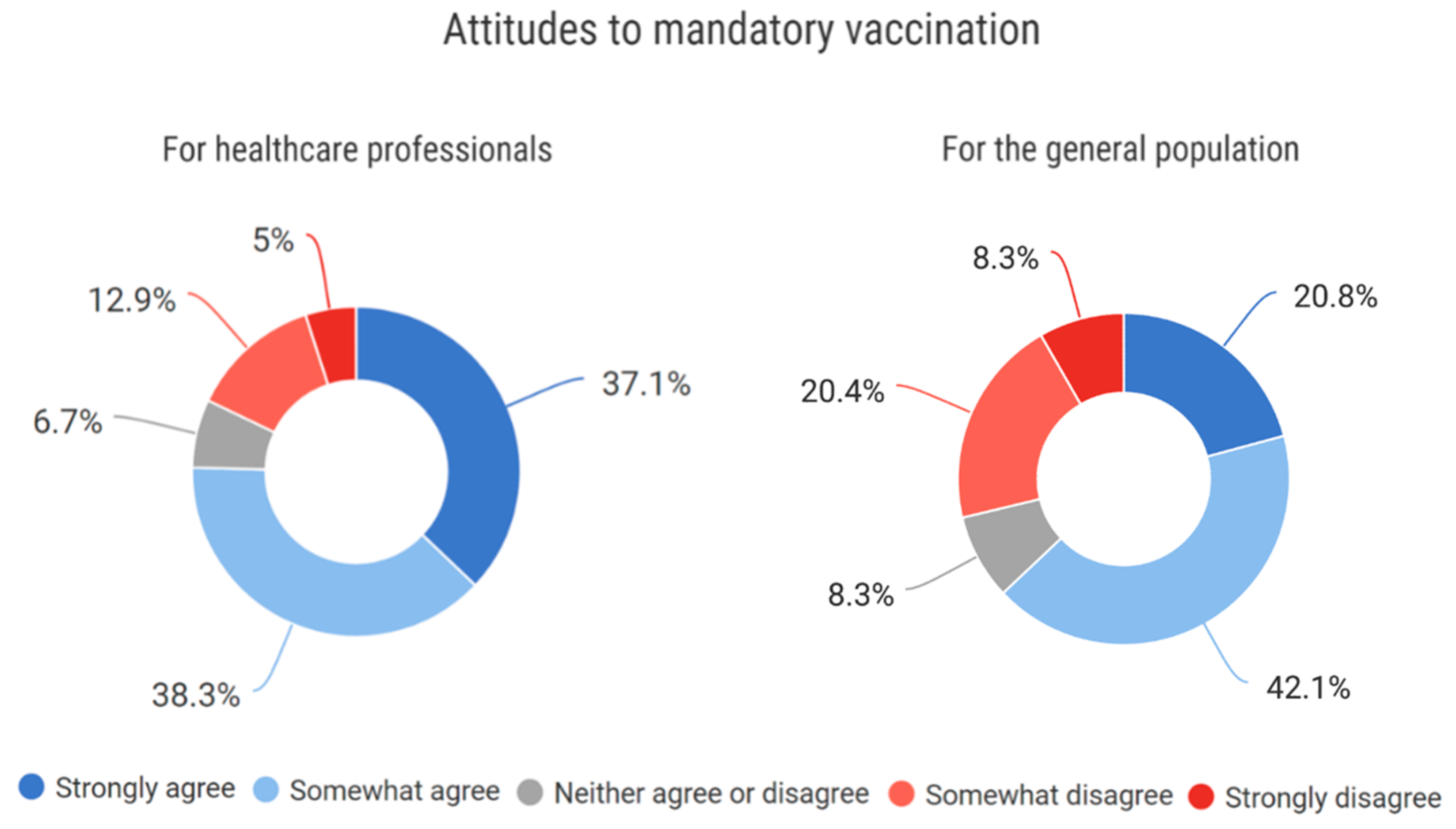
3.4.7. Approach to Mandatory Vaccination for Healthcare Professionals and the General Population
3.5. Comparison to Czech General Population Counterparts
3.5.1. Test-Verified COVID Prevalence
3.5.2. COVID-19 Vaccination Rate
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kaul, V.; Gallo de Moraes, A.; Khateeb, D.; Greenstein, Y.; Winter, G.; Chae, J.; Stewart, N.H.; Qadir, N.; Dangayach, N.S. Medical Education During the COVID-19 Pandemic. Chest 2021, 159, 1949–1960. [Google Scholar] [CrossRef] [PubMed]
- Servin-Rojas, M.; Olivas-Martinez, A.; Dithurbide-Hernandez, M.; Chavez-Vela, J.; Petricevich, V.L.; García-Juárez, I.; Gallo de Moraes, A.; Zendejas, B. Impact of the COVID-19 pandemic on the clinical training of last year medical students in Mexico: A cross-sectional nationwide study. BMC Med. Educ. 2022, 22, 24. [Google Scholar] [CrossRef]
- Turana, Y.; Primatanti, P.A.; Sukarya, W.S.; Wiyanto, M.; Duarsa, A.B.S.; Wratsangka, R.; Adriani, D.; Sasmita, P.K.; Budiyanti, E.; Anditiarina, D.; et al. Impact on Medical Education and the Medical Student’s Attitude, Practice, Mental Health, After One Year of the Covid-19 Pandemic in Indonesia. Front. Educ. 2022, 7, 1–14. [Google Scholar] [CrossRef]
- Wanigasooriya, K.; Beedham, W.; Laloo, R.; Karri, R.S.; Darr, A.; Layton, G.R.; Logan, P.; Tan, Y.; Mittapalli, D.; Patel, T.; et al. The perceived impact of the COVID-19 pandemic on medical student education and training—An international survey. BMC Med. Educ. 2021, 21, 566. [Google Scholar] [CrossRef]
- Shields, A.M.; Faustini, S.E.; Kristunas, C.A.; Cook, A.M.; Backhouse, C.; Dunbar, L.; Ebanks, D.; Emmanuel, B.; Crouch, E.; Kröger, A.; et al. COVID-19: Seroprevalence and Vaccine Responses in UK Dental Care Professionals. J. Dent. Res. 2021, 100, 1220–1227. [Google Scholar] [CrossRef]
- Global Change Data Lab. Czechia, Coronavirus Cases per Capita, December 2021. 2022. Available online: https://ourworldindata.org/explorers/coronavirus-data-explorer?tab=table&zoomToSelection=true&time=earliest..2021-12-31&facet=none&pickerSort=asc&pickerMetric=location&hideControls=true&Metric=Confirmed+cases&Interval=Cumulative&Relative+to+Population=true&Color+by+test+positivity=false&country=~CZE (accessed on 12 September 2022).
- Schmidt, J.; Waldova, E.; Balkova, S.; Suchanek, J.; Smucler, R. Impact of COVID-19 on Czech Dentistry: A Nationwide Cross-Sectional Preliminary Study among Dentists in the Czech Republic. Int. J. Environ. Res. Public Health 2021, 18, 9121. [Google Scholar] [CrossRef]
- Klugar, M.; Riad, A.; Mohanan, L.; Pokorná, A. COVID-19 Vaccine Booster Hesitancy (VBH) of Healthcare Workers in Czechia: National Cross-Sectional Study. Vaccines 2021, 9, 1437. [Google Scholar] [CrossRef]
- Riad, A.; Pokorná, A.; Antalová, N.; Krobot, M.; Zviadadze, N.; Serdiuk, I.; Koščík, M.; Klugar, M. Prevalence and Drivers of COVID-19 Vaccine Hesitancy among Czech University Students: National Cross-Sectional Study. Vaccines 2021, 9, 948. [Google Scholar] [CrossRef]
- Štěpánek, L.; Janošíková, M.; Nakládalová, M.; Štěpánek, L.; Boriková, A.; Vildová, H. Motivation to COVID-19 Vaccination and Reasons for Hesitancy in Employees of a Czech Tertiary Care Hospital: A Cross-Sectional Survey. Vaccines 2021, 9, 863. [Google Scholar] [CrossRef]
- Riad, A.; Jouzová, A.; Üstün, B.; Lagová, E.; Hruban, L.; Janků, P.; Pokorná, A.; Klugarová, J.; Koščík, M.; Klugar, M. COVID-19 Vaccine Acceptance of Pregnant and Lactating Women (PLW) in Czechia: An Analytical Cross-Sectional Study. Int. J. Environ. Res. Public Health 2021, 18, 13373. [Google Scholar] [CrossRef]
- Kosarkova, A.; Malinakova, K.; van Dijk, J.P.; Tavel, P. Vaccine Refusal in the Czech Republic Is Associated with Being Spiritual but Not Religiously Affiliated. Vaccines 2021, 9, 1157. [Google Scholar] [CrossRef] [PubMed]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet 2007, 370, 1453–1457. [Google Scholar] [CrossRef]
- Sample Calculator For Proportions. 2022. Available online: https://www.netquest.com/en/panel/sample-calculator/statistical-calculators (accessed on 20 August 2022).
- Czech Ministry of Health. COVID-19: Demografický Přehled Vykázaných Očkování v Čase/COVID-19: Demographic Overview of Reported Vaccinations over Time; Current up to: 21 February 2022. 2022. Available online: https://onemocneni-aktualne.mzcr.cz/api/v2/covid-19 (accessed on 8 September 2022).
- Czech Ministry of Health. COVID-19 Vaccination in the Czech Republic. 2022. Available online: https://onemocneni-aktualne.mzcr.cz/vakcinace-cr (accessed on 7 September 2022).
- Czech Ministry of Health. SARS-CoV-2 Infection Identification. 2022. Available online: https://onemocneni-aktualne.mzcr.cz/covid-19--napoveda (accessed on 7 September 2022).
- Perina, V.; Schmidt, J. The Effect of Priority Access of Dentists to Covid-Vaccination in the Czech Republic. Vaccines 2022, 10, 1252. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, J.; Perina, V.; Treglerova, J.; Pilbauerova, N.; Suchanek, J.; Smucler, R. COVID-19 Prevalence among Czech Dentists. Int. J. Environ. Res. Public Health 2021, 18, 12488. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, J.; Perina, V.; Treglerova, J.; Pilbauerova, N.; Suchanek, J.; Smucler, R. COVID-19 Vaccination among Czech Dentists. Vaccines 2022, 10, 428. [Google Scholar] [CrossRef] [PubMed]
- Andrejko, K.; Pry, J.; Myers, J.; Fukui, N.; DeGuzman, J.; Openshaw, J.; Watt, J.; Lewnard, J.; Jain, S.; Covid, C.; et al. Effectiveness of Face Mask or Respirator Use in Indoor Public Settings for Prevention of SARS-CoV-2 Infection—California, February–December 2021. MMWR. Morb. Mortal. Wkly. Rep. 2022, 71, 212–216. [Google Scholar] [CrossRef]
- Perencevich, E.N.; Diekema, D.J.; Edmond, M.B. Moving Personal Protective Equipment Into the Community: Face Shields and Containment of COVID-19. JAMA 2020, 323, 2252–2253. [Google Scholar] [CrossRef]
- Levitt, E.E.; Gohari, M.R.; Syan, S.K.; Belisario, K.; Gillard, J.; DeJesus, J.; Levitt, A.; MacKillop, J. Public health guideline compliance and perceived government effectiveness during the COVID-19 pandemic in Canada: Findings from a longitudinal cohort study. Lancet Reg. Health Am. 2022, 9, 100185. [Google Scholar] [CrossRef]
- Rosagemma, C.; Francesca, L.; Barranco, R.; Tettamanti, C.; Bonsignore, A.; Ventura, F. A Survey on Undergraduate Medical Students’ Perception of COVID-19 Vaccination. Vaccines 2022, 10, 1464. [Google Scholar]
- Patwary, M.M.; Bardhan, M.; Haque, M.Z.; Sultana, R.; Alam, M.A.; Browning, M.H.E.M. COVID-19 Vaccine Acceptance Rate and Its Factors among Healthcare Students: A Systematic Review with Meta-Analysis. Vaccines 2022, 10, 806. [Google Scholar] [CrossRef]
- Lucia, V.C.; Kelekar, A.; Afonso, N.M. COVID-19 vaccine hesitancy among medical students. J. Public Health 2021, 43, 445–449. [Google Scholar] [CrossRef] [PubMed]
- Saied, S.M.; Saied, E.M.; Kabbash, I.A.; Abdo, S.A.E. Vaccine hesitancy: Beliefs and barriers associated with COVID-19 vaccination among Egyptian medical students. J. Med. Virol. 2021, 93, 4280–4291. [Google Scholar] [CrossRef] [PubMed]
- Barello, S.; Nania, T.; Dellafiore, F.; Graffigna, G.; Caruso, R. ‘Vaccine hesitancy’ among university students in Italy during the COVID-19 pandemic. Eur. J. Epidemiol. 2020, 35, 781–783. [Google Scholar] [CrossRef] [PubMed]
- Lin, G.S.S.; Lee, H.Y.; Leong, J.Z.; Sulaiman, M.M.; Loo, W.F.; Tan, W.W. COVID-19 vaccination acceptance among dental students and dental practitioners: A systematic review and meta-analysis. PLoS ONE 2022, 17, e0267354. [Google Scholar] [CrossRef]
- Riad, A.; Abdulqader, H.; Morgado, M.; Domnori, S.; Koščík, M.; Mendes, J.J.; Klugar, M.; Kateeb, E.; IADS-SCORE. Global Prevalence and Drivers of Dental Students’ COVID-19 Vaccine Hesitancy. Vaccines 2021, 9, 566. [Google Scholar] [CrossRef]
- Mascarenhas, A.K.; Lucia, V.C.; Kelekar, A.; Afonso, N.M. Dental students’ attitudes and hesitancy toward COVID-19 vaccine. J. Dent. Educ. 2021, 85, 1504–1510. [Google Scholar] [CrossRef]
- Bălan, A.; Bejan, I.; Bonciu, S.; Eni, C.E.; Ruță, S. Romanian Medical Students’ Attitude towards and Perceived Knowledge on COVID-19 Vaccination. Vaccines 2021, 9, 854. [Google Scholar] [CrossRef]
- Kateeb, E.; Danadneh, M.; Pokorná, A.; Klugarová, J.; Abdulqader, H.; Klugar, M.; Riad, A. Predictors of Willingness to Receive COVID-19 Vaccine: Cross-Sectional Study of Palestinian Dental Students. Vaccines 2021, 9, 954. [Google Scholar] [CrossRef]
- Bolatov, A.K.; Seisembekov, T.Z.; Askarova, A.Z.; Pavalkis, D. Barriers to COVID-19 vaccination among medical students in Kazakhstan: Development, validation, and use of a new COVID-19 Vaccine Hesitancy Scale. Hum. Vaccines Immunother. 2021, 17, 4982–4992. [Google Scholar] [CrossRef]
- Peterson, C.J.; Abohelwa, M.; Payne, D.; Mohamed, A.A.; Nugent, K. 2019 Novel Coronavirus Vaccination Among Medical Students. J. Prim. Care Community Health 2021, 12, 21501327211058316. [Google Scholar] [CrossRef]
- Sugawara, N.; Yasui-Furukori, N.; Fukushima, A.; Shimoda, K. Attitudes of Medical Students toward COVID-19 Vaccination: Who Is Willing to Receive a Third Dose of the Vaccine? Vaccines 2021, 9, 1295. [Google Scholar] [CrossRef] [PubMed]
- Sovicova, M.; Zibolenova, J.; Svihrova, V.; Hudeckova, H. Odds Ratio Estimation of Medical Students’ Attitudes towards COVID-19 Vaccination. Int. J. Environ. Res. Public Health 2021, 18, 6815. [Google Scholar] [CrossRef] [PubMed]
- Bani Hani, A.; Alaridah, N.; Abu Abeeleh, M.; Shatarat, A.; Rayyan, R.; Kamal, A.; Alhafez, L.; Odeh, R.; Al-Taher, R.N. Medical students and risk of COVID-19 infection: A descriptive cross-sectional study from the University of Jordan. Ann. Med. Surg. 2021, 70, 102775. [Google Scholar] [CrossRef] [PubMed]
- Silva, G.S.; Avila, G.O.; Lubianca, F.N.; Lubianca, J.P.N.; Michelon, V.M.M.; Kalil, D.P.; Maestri, L.F.; Lengler, A.D.; Lima, G.P.; Lubianca Neto, J.F. Prevalence of COVID-19 in medical school and residency in Porto Alegre, RS. Rev. Da Assoc. Med. Bras. 2022, 68, 206–211. [Google Scholar] [CrossRef]




Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schmidt, J.; Vavrickova, L.; Micopulos, C.; Suchanek, J.; Pilbauerova, N.; Perina, V.; Kapitan, M. COVID-19 among Czech Dentistry Students: Higher Vaccination and Lower Prevalence Compared to General Population Counterparts. Vaccines 2022, 10, 1927. https://doi.org/10.3390/vaccines10111927
Schmidt J, Vavrickova L, Micopulos C, Suchanek J, Pilbauerova N, Perina V, Kapitan M. COVID-19 among Czech Dentistry Students: Higher Vaccination and Lower Prevalence Compared to General Population Counterparts. Vaccines. 2022; 10(11):1927. https://doi.org/10.3390/vaccines10111927
Chicago/Turabian StyleSchmidt, Jan, Lenka Vavrickova, Christos Micopulos, Jakub Suchanek, Nela Pilbauerova, Vojtech Perina, and Martin Kapitan. 2022. "COVID-19 among Czech Dentistry Students: Higher Vaccination and Lower Prevalence Compared to General Population Counterparts" Vaccines 10, no. 11: 1927. https://doi.org/10.3390/vaccines10111927
APA StyleSchmidt, J., Vavrickova, L., Micopulos, C., Suchanek, J., Pilbauerova, N., Perina, V., & Kapitan, M. (2022). COVID-19 among Czech Dentistry Students: Higher Vaccination and Lower Prevalence Compared to General Population Counterparts. Vaccines, 10(11), 1927. https://doi.org/10.3390/vaccines10111927










