Understanding the Photodynamic Therapy Induced Bystander and Abscopal Effects: A Review
Abstract
1. Introduction
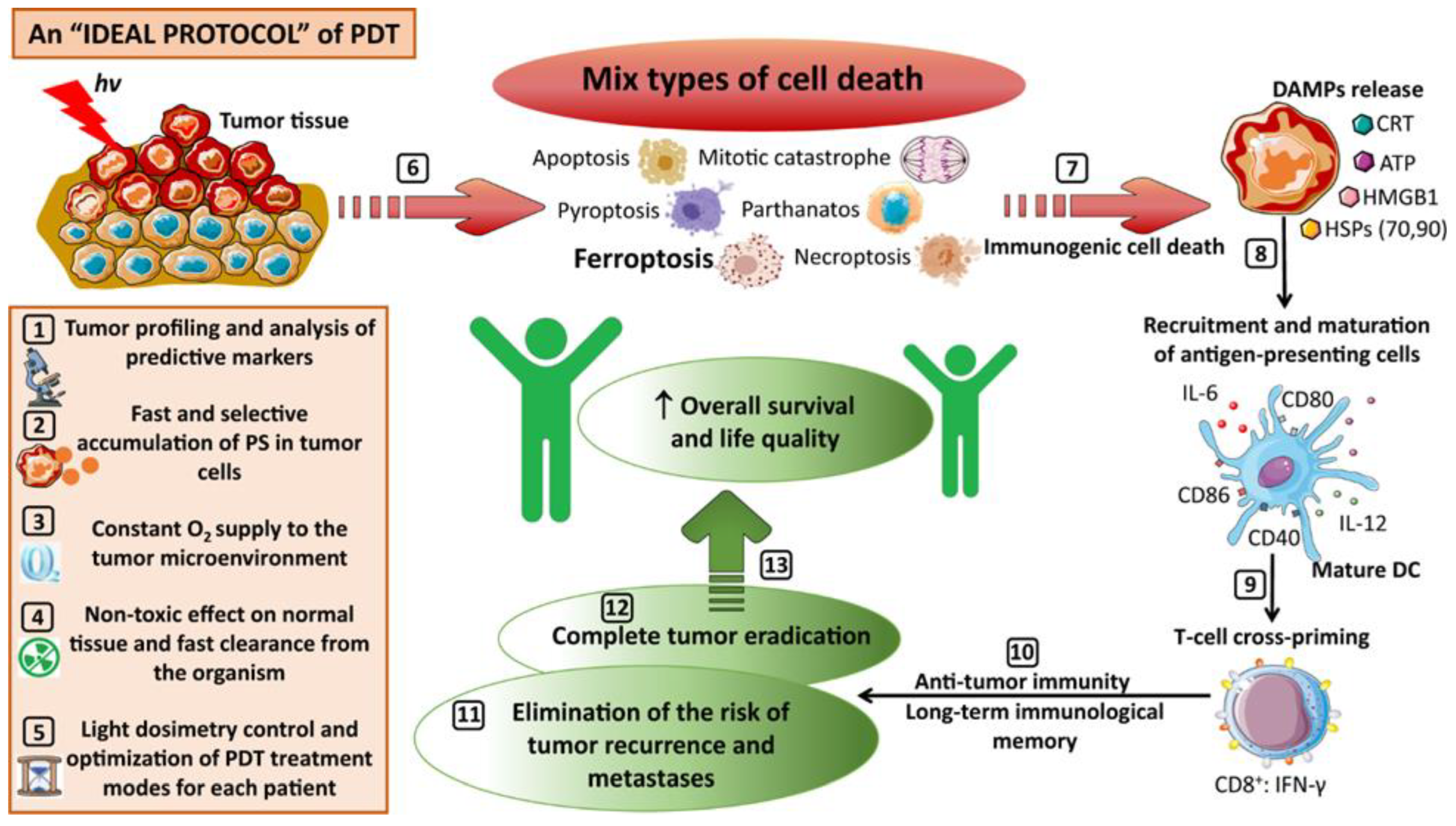
2. PDT-Mediated Anticancer Effects
| Various Kind of ROS/RNS | Biological Activity |
|---|---|
| Superoxide anion (O2•−), hydroperoxide radical (HOO•), peroxides (H2O2, ROOH) and hydroxyl radical (•OH), singlet oxygen (1O2), nitric oxide(•NO) | Mitotic catastrophe (MC), paraptosis, pyroptosis, parthanatos [17], necroptosis, and ferroptosis [16,18], cell signaling, oxidative stress, and immune response [2,4,23] |
3. Biology of Bystander Response in PDT
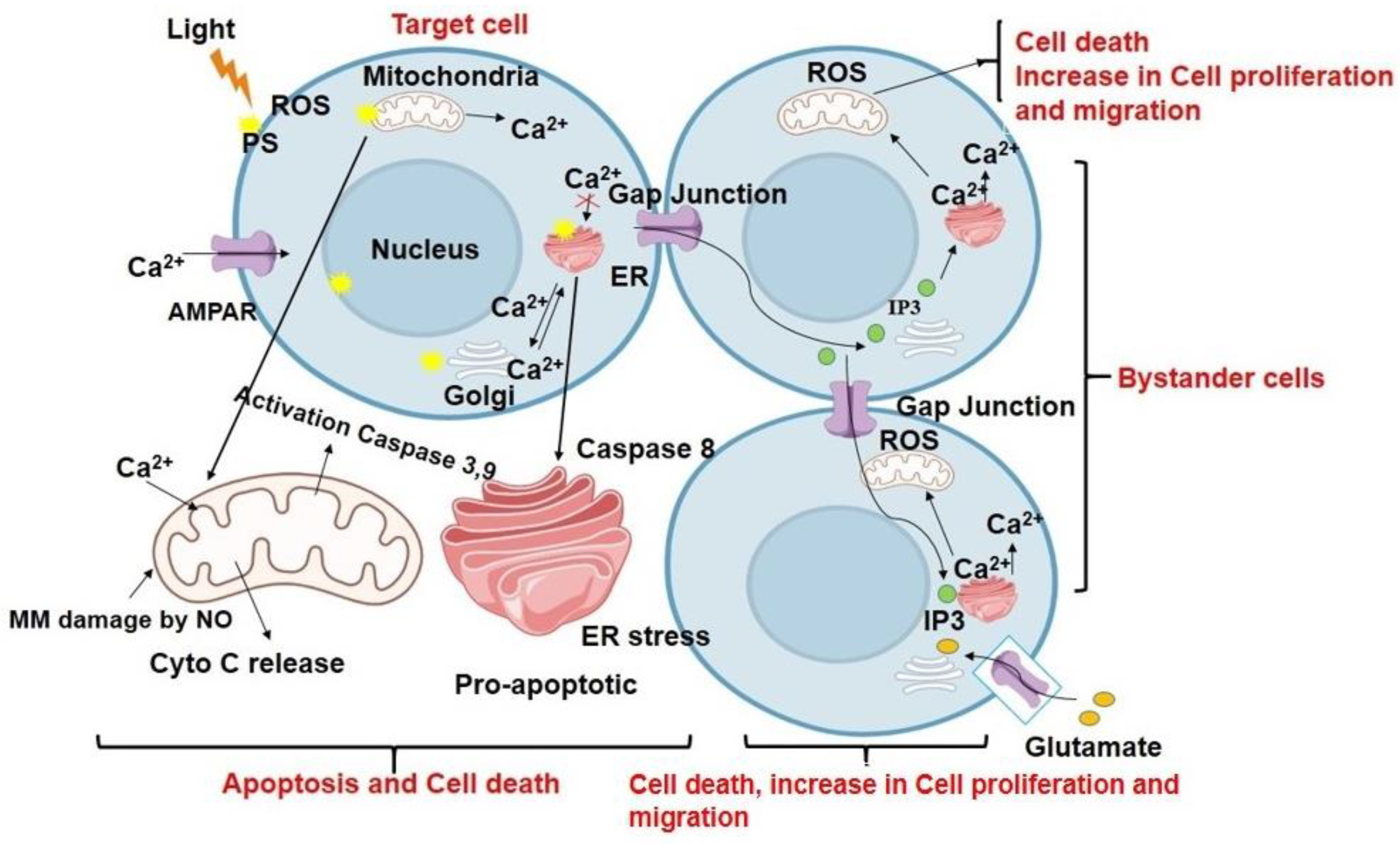
3.1. Contact-Dependent Bystander Effects
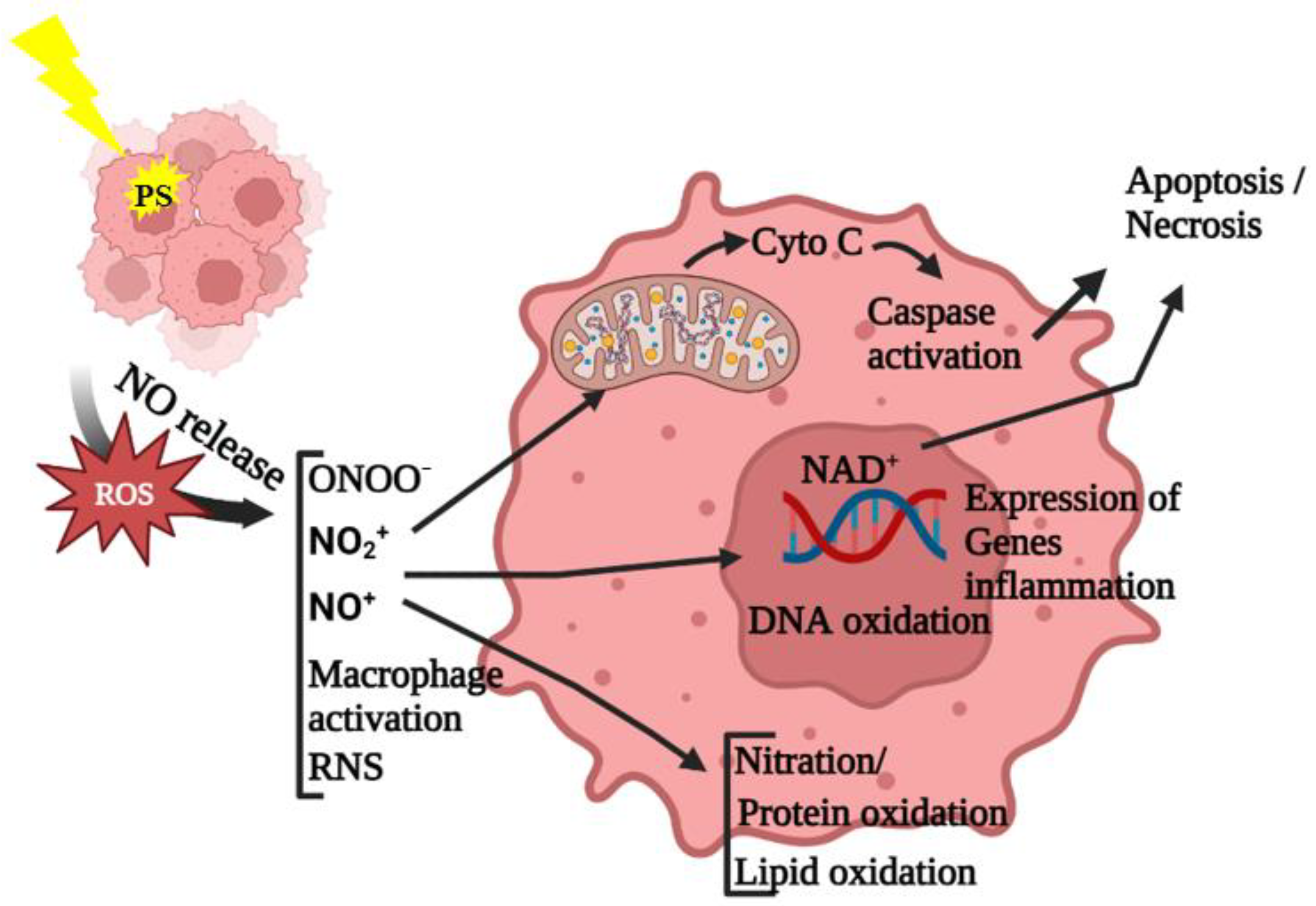
3.2. Diffusing-Mediator-Mediated Bystander Effects
3.2.1. Cytokines
| Types of PS or Other Agent | Cell Lines/Tissue | In Vitro/In Vivo | Effect or Mechanism (Molecular Response) |
|---|---|---|---|
| HPPH | EMT6 | In vivo | Levels of Macrophage inflammatory protein (MIP) and IL-6 increased [64] |
| bPEI25K/DNA-complex | H1299 | In vitro/in vivo | Overexpression of p53 [68] |
| 68Ga-FAP | synovial tissue | ex vivo | Overexpression of caspase-3 [69] |
| Hematoporphyrin derivative (HpD-Arg(2) | OVP10 | In vitro | Reduced mitotic activity and expression of the FAK [51] |
| Tetra(3-hydroxyphenyl)porphyrin | MDCK II | In vitro | Increased necrosis [66] |
| Deuteroporphyrin (DP) | WTK1 | In vitro | DNA damage increased [5] |
3.2.2. Oxidative Species
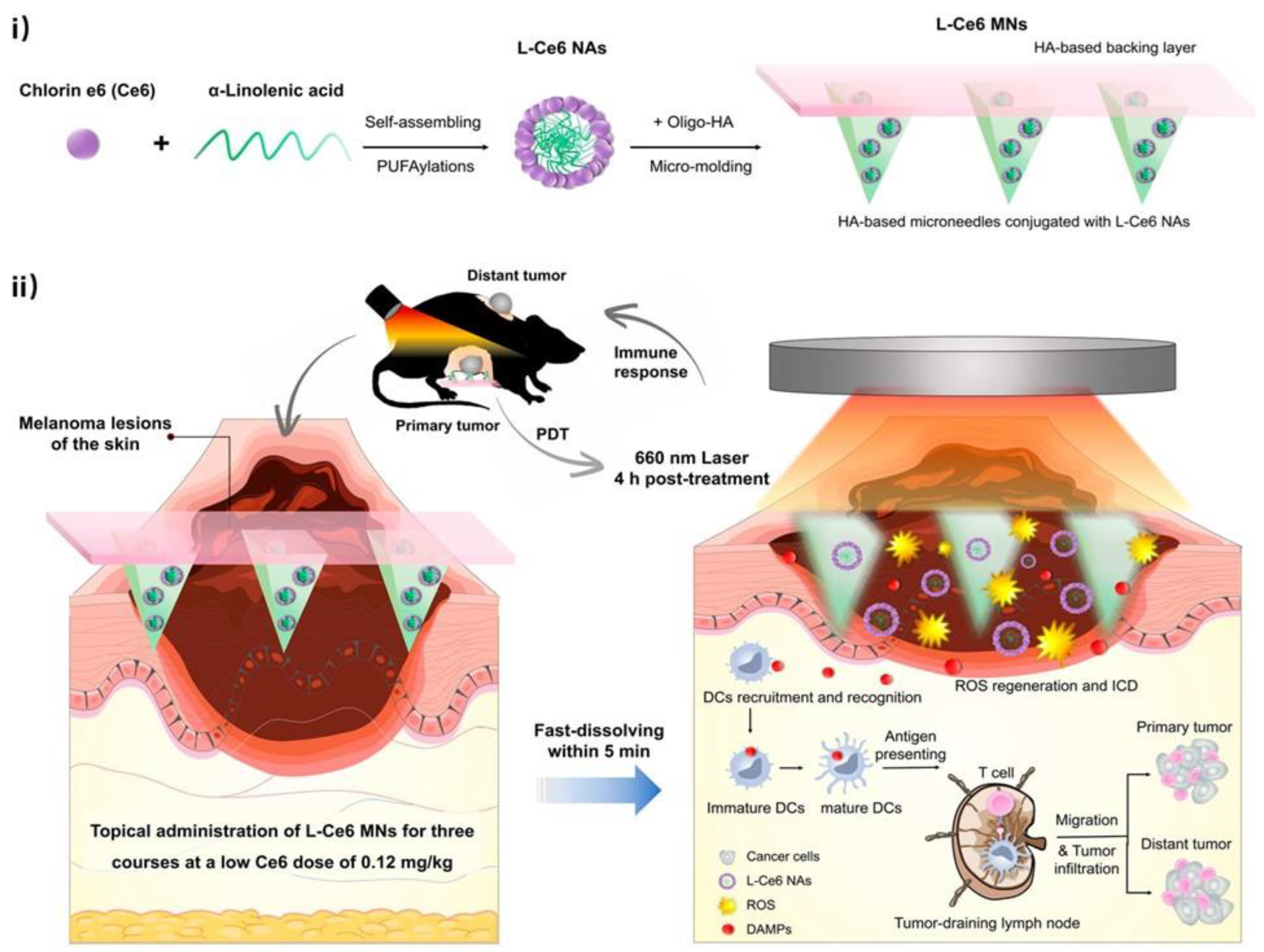
4. Biology of Abscopal Response in PDT
5. Challenges
6. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviation
| PDT | Photodynamic therapy |
| ROS | Reactive oxygen species |
| PS | Photosensitizer |
| ICD | Immunogenic cell death |
| NO | Nitric oxide |
| MC | Mitotic catastrophe |
| DAMPs | Damage-associated molecular patterns |
| RNS | Reactive nitrogen species |
| ALA | 5-aminolevulinic acid |
| HPPH | 2-(1-hexyloxyethyl)-2-devinyl pyropheophorbide |
| Ca2+ | Calcium ion |
| NOS | Nitric oxide synthesis |
| TNF-α | Tumor necrosis factor-alpha |
| FAP | Fibroblast activation protein |
| MIP | Macrophage inflammatory protein |
| MMP-9 | Matrix metalloproteinase-9 |
| COX-2 | Cyclooxygenase-2 |
| GSH | Glutathione |
| PLP | Porphyrin lipoprotein |
| HMGB1 | High-mobility group box-1 |
| ZnP | Zn-pyrophosphate |
References
- Kwiatkowski, S.; Knap, B.; Przystupski, D.; Saczko, J.; Kędzierska, E.; Knap-Czop, K.; Kotlińska, J.; Michel, O.; Kotowski, K.; Kulbacka, J. Photodynamic therapy–mechanisms, photosensitizers and combinations. Biomed. Pharmacother. 2018, 106, 1098–1107. [Google Scholar] [CrossRef]
- Ali Mohammad, S.; Hak, A.; Pogu, S.V.; Rengan, A.K. Radiotherapy, photodynamic therapy, and cryoablation-induced abscopal effect: Challenges and future prospects. Cancer Innov. 2023. [Google Scholar] [CrossRef]
- Bazak, J.; Korytowski, W.; Girotti, A.W. Bystander effects of nitric oxide in cellular models of anti-tumor photodynamic therapy. Cancers 2019, 11, 1674. [Google Scholar] [CrossRef]
- Gani, M.; Xodo, L.E.; Rapozzi, V. Bystander effect in photosensitized prostate cancer cells with a different grade of malignancy: The role of nitric oxide. Nitric Oxide 2022, 128, 25–36. [Google Scholar] [CrossRef] [PubMed]
- Chakraborty, A.; Held, K.D.; Prise, K.M.; Liber, H.L.; Redmond, R.W. Bystander effects induced by diffusing mediators after photodynamic stress. Radiat. Res. 2009, 172, 74–81. [Google Scholar] [CrossRef] [PubMed]
- Daguenet, E.; Louati, S.; Wozny, A.-S.; Vial, N.; Gras, M.; Guy, J.-B.; Vallard, A.; Rodriguez-Lafrasse, C.; Magné, N. Radiation-induced bystander and abscopal effects: Important lessons from preclinical models. Br. J. Cancer 2020, 123, 339–348. [Google Scholar] [CrossRef]
- Abuodeh, Y.; Venkat, P.; Kim, S. Systematic review of case reports on the abscopal effect. Curr. Probl. Cancer 2016, 40, 25–37. [Google Scholar] [CrossRef]
- Demaria, S.; Formenti, S.C. The abscopal effect 67 years later: From a side story to center stage. Br. J. Radiol. 2020, 93, 20200042. [Google Scholar] [CrossRef]
- Wang, D.; Zhang, X.; Gao, Y.; Cui, X.; Yang, Y.; Mao, W.; Li, M.; Zhang, B.; Yu, J. Research progress and existing problems for abscopal effect. Cancer Manag. Res. 2020, 12, 6695. [Google Scholar] [CrossRef]
- Girotti, A.W.; Fahey, J.M.; Korbelik, M. Photodynamic therapy as an oxidative anti-tumor modality: Negative effects of nitric oxide on treatment efficacy. Pharmaceutics 2021, 13, 593. [Google Scholar] [CrossRef] [PubMed]
- Correia, J.H.; Rodrigues, J.A.; Pimenta, S.; Dong, T.; Yang, Z. Photodynamic therapy review: Principles, photosensitizers, applications, and future directions. Pharmaceutics 2021, 13, 1332. [Google Scholar] [CrossRef]
- Macdonald, I.J.; Dougherty, T.J. Basic principles of photodynamic therapy. J. Porphyr. Phthalocyanines 2001, 5, 105–129. [Google Scholar] [CrossRef]
- Henderson, B.W.; Gollnick, S.O. Mechanistic principles of photodynamic therapy. In Biomedical Photonics Handbook; CRC Press: Boca Raton, FL, USA, 2014; pp. 26–53. [Google Scholar]
- Van Den Bergh, H.; Ballini, J. Principles of photodynamic therapy. In Photodynamic Therapy of Ocular Diseases; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2004; pp. 1–9. [Google Scholar]
- Agostinis, P.; Berg, K.; Cengel, K.A.; Foster, T.H.; Girotti, A.W.; Gollnick, S.O.; Hahn, S.M.; Hamblin, M.R.; Juzeniene, A.; Kessel, D. Photodynamic therapy of cancer: An update. CA Cancer J. Clin. 2011, 61, 250–281. [Google Scholar] [CrossRef]
- Mishchenko, T.; Balalaeva, I.; Gorokhova, A.; Vedunova, M.; Krysko, D.V. Which cell death modality wins the contest for photodynamic therapy of cancer? Cell Death Dis. 2022, 13, 455. [Google Scholar] [CrossRef] [PubMed]
- Fatokun, A.A.; Dawson, V.L.; Dawson, T.M. Parthanatos: Mitochondrial-linked mechanisms and therapeutic opportunities. Br. J. Pharmacol. 2014, 171, 2000–2016. [Google Scholar] [CrossRef]
- Mokoena, D.R.; George, B.P.; Abrahamse, H. Photodynamic therapy induced cell death mechanisms in breast cancer. Int. J. Mol. Sci. 2021, 22, 10506. [Google Scholar] [CrossRef] [PubMed]
- Plaetzer, K.; Kiesslich, T.; Verwanger, T.; Krammer, B. The modes of cell death induced by PDT: An overview. Med. Laser Appl. 2003, 18, 7–19. [Google Scholar] [CrossRef]
- Kabingu, E.; Vaughan, L.; Owczarczak, B.; Ramsey, K.; Gollnick, S. CD8+ T cell-mediated control of distant tumours following local photodynamic therapy is independent of CD4+ T cells and dependent on natural killer cells. Br. J. Cancer 2007, 96, 1839–1848. [Google Scholar] [CrossRef]
- Mroz, P.; Szokalska, A.; Wu, M.X.; Hamblin, M.R. Photodynamic therapy of tumors can lead to development of systemic antigen-specific immune response. PLoS ONE 2010, 5, e15194. [Google Scholar] [CrossRef] [PubMed]
- Lou, J.; Aragaki, M.; Bernards, N.; Kinoshita, T.; Mo, J.; Motooka, Y.; Ishiwata, T.; Gregor, A.; Chee, T.; Chen, Z. Repeated porphyrin lipoprotein-based photodynamic therapy controls distant disease in mouse mesothelioma via the abscopal effect. Nanophotonics 2021, 10, 3279–3294. [Google Scholar] [CrossRef]
- Poyer, F.; Thomas, C.D.; Garcia, G.; Croisy, A.; Carrez, D.; Maillard, P.; Lupu, M.; Mispelter, J. PDT induced bystander effect on human xenografted colorectal tumors as evidenced by sodium MRI. Photodiagnosis Photodyn. Ther. 2012, 9, 303–309. [Google Scholar] [CrossRef] [PubMed]
- Dougherty, R.C.; Strain, H.H.; Svec, W.A.; Uphaus, R.A.; Katz, J.J. Structure, properties, and distribution of chlorophyll c. J. Am. Chem. Soc. 1970, 92, 2826–2833. [Google Scholar] [CrossRef]
- Abrahamse, H.; Hamblin, M.R. New photosensitizers for photodynamic therapy. Biochem. J. 2016, 473, 347–364. [Google Scholar] [CrossRef] [PubMed]
- Mfouo-Tynga, I.S.; Dias, L.D.; Inada, N.M.; Kurachi, C. Features of third generation photosensitizers used in anticancer photodynamic therapy. Photodiagnosis Photodyn. Ther. 2021, 34, 102091. [Google Scholar] [CrossRef]
- Dave, D.; Desai, U.; Despande, N. Photodynamic therapy: A view through light. J. Orofac. Res. 2012, 2, 82–86. [Google Scholar] [CrossRef]
- Kataoka, H.; Nishie, H.; Hayashi, N.; Tanaka, M.; Nomoto, A.; Yano, S.; Joh, T. New photodynamic therapy with next-generation photosensitizers. Ann. Transl. Med. 2017, 5, 183. [Google Scholar] [CrossRef]
- Mothersill, C.; Seymour, C. Radiation-induced bystander effects: Past history and future directions. Radiat. Res. 2001, 155, 759–767. [Google Scholar] [CrossRef]
- Najafi, M.; Fardid, R.; Hadadi, G.; Fardid, M. The mechanisms of radiation-induced bystander effect. J. Biomed. Phys. Eng. 2014, 4, 163–172. [Google Scholar]
- Nagasawa, H.; Little, J.B. Induction of sister chromatid exchanges by extremely low doses of α-particles. Cancer Res. 1992, 52, 6394–6396. [Google Scholar]
- Lobachevsky, P.; Forrester, H.B.; Ivashkevich, A.; Mason, J.; Stevenson, A.W.; Hall, C.J.; Sprung, C.N.; Djonov, V.G.; Martin, O.A. Synchrotron X-ray radiation-induced bystander effect: An impact of the scattered radiation, distance from the irradiated site and p53 cell status. Front. Oncol. 2021, 11, 685598. [Google Scholar] [CrossRef]
- Hu, S.; Shao, C. Research progress of radiation induced bystander and abscopal effects in normal tissue. Radiat. Med. Prot. 2020, 1, 69–74. [Google Scholar] [CrossRef]
- Bazak, J.; Fahey, J.M.; Wawak, K.; Korytowski, W.; Girotti, A.W. Enhanced aggressiveness of bystander cells in an anti-tumor photodynamic therapy model: Role of nitric oxide produced by targeted cells. Free. Radic. Biol. Med. 2017, 102, 111–121. [Google Scholar] [CrossRef]
- Calì, B.; Ceolin, S.; Ceriani, F.; Bortolozzi, M.; Agnellini, A.H.; Zorzi, V.; Predonzani, A.; Bronte, V.; Molon, B.; Mammano, F. Critical role of gap junction communication, calcium and nitric oxide signaling in bystander responses to focal photodynamic injury. Oncotarget 2015, 6, 10161. [Google Scholar] [CrossRef]
- Nardin, C.; Peres, C.; Mazzarda, F.; Ziraldo, G.; Salvatore, A.M.; Mammano, F. Photosensitizer activation drives apoptosis by interorganellar Ca2+ transfer and superoxide production in bystander cancer cells. Cells 2019, 8, 1175. [Google Scholar] [CrossRef] [PubMed]
- Baskaran, R.; Lee, J.; Yang, S.-G. Clinical development of photodynamic agents and therapeutic applications. Biomater. Res. 2018, 22, 25. [Google Scholar] [CrossRef] [PubMed]
- Sobhani, N.; Samadani, A.A. Implications of photodynamic cancer therapy: An overview of PDT mechanisms basically and practically. J. Egypt. Natl. Cancer Inst. 2021, 33, 34. [Google Scholar] [CrossRef] [PubMed]
- Deng, X.; Shao, Z.; Zhao, Y. Solutions to the drawbacks of photothermal and photodynamic cancer therapy. Adv. Sci. 2021, 8, 2002504. [Google Scholar] [CrossRef]
- Hei, T.K.; Zhou, H.; Ivanov, V.N.; Hong, M.; Lieberman, H.B.; Brenner, D.J.; Amundson, S.A.; Geard, C.R. Mechanism of radiation-induced bystander effects: A unifying model. J. Pharm. Pharmacol. 2008, 60, 943–950. [Google Scholar] [CrossRef] [PubMed]
- Shao, C.; Folkard, M.; Prise, K. Role of TGF-β1 and nitric oxide in the bystander response of irradiated glioma cells. Oncogene 2008, 27, 434–440. [Google Scholar] [CrossRef]
- Pelle, E.; Mammone, T.; Maes, D.; Frenkel, K. Keratinocytes act as a source of reactive oxygen species by transferring hydrogen peroxide to melanocytes. J. Investig. Dermatol. 2005, 124, 793–797. [Google Scholar] [CrossRef]
- Railkar, R.; Agarwal, P.K. Photodynamic therapy in the treatment of bladder cancer: Past challenges and current innovations. Eur. Urol. Focus 2018, 4, 509–511. [Google Scholar] [CrossRef]
- Castano, A.P.; Demidova, T.N.; Hamblin, M.R. Mechanisms in photodynamic therapy: Part two—Cellular signaling, cell metabolism and modes of cell death. Photodiagnosis Photodyn. Ther. 2005, 2, 1–23. [Google Scholar] [CrossRef]
- Gardlo, K.; Horska, Z.; Enk, C.D.; Rauch, L.; Megahed, M.; Ruzicka, T.; Fritsch, C. Treatment of cutaneous leishmaniasis by photodynamic therapy. J. Am. Acad. Dermatol. 2003, 48, 893–896. [Google Scholar] [CrossRef] [PubMed]
- Wiegell, S.; Hædersdal, M.; Eriksen, P.; Wulf, H. Photodynamic therapy of actinic keratoses with 8% and 16% methyl aminolaevulinate and home-based daylight exposure: A double-blinded randomized clinical trial. Br. J. Dermatol. 2009, 160, 1308–1314. [Google Scholar] [CrossRef] [PubMed]
- Whitaker, I.S.; Shokrollahi, K.; James, W.; Mishra, A.; Lohana, P.; Murison, M.C. Combined CO2 laser with photodynamic therapy for the treatment of nodular basal cell carcinomas. Ann. Plast. Surg. 2007, 59, 484–488. [Google Scholar] [CrossRef] [PubMed]
- Monfrecola, G.; Procaccini, E.M.; D’Onofrio, D.; Roberti, G.; Liuzzi, R.; Staibano, S.; Manco, A.; De Rosa, G.; Santoianni, P. Hyperpigmentation induced by topical 5-aminolaevulinic acid plus visible light. J. Photochem. Photobiol. B Biol. 2002, 68, 147–155. [Google Scholar] [CrossRef]
- Feine, I.; Pinkas, I.; Salomon, Y.; Scherz, A. Local oxidative stress expansion through endothelial cells—A key role for gap junction intercellular communication. PLoS ONE 2012, 7, e41633. [Google Scholar] [CrossRef] [PubMed]
- Rubio, N.; Fleury, S.P.; Redmond, R.W. Spatial and temporal dynamics of in vitro photodynamic cell killing: Extracellular hydrogen peroxide mediates neighbouring cell death. Photochem. Photobiol. Sci. 2009, 8, 457–464. [Google Scholar] [CrossRef]
- DąbrowskaABCDF, A.; GośEF, M.; JanikADG, P. “Bystander effect” induced by photodynamically or heat-injured ovarian carcinoma cells (OVP10) in vitro. Med. Sci. Monit. 2005, 11, BR316–BR324. [Google Scholar]
- Spray, D.C.; Hanstein, R.; Lopez-Quintero, S.V.; Stout, R.F., Jr.; Suadicani, S.O.; Thi, M.M. Gap junctions and bystander effects: Good Samaritans and executioners. Wiley Interdiscip. Rev. Membr. Transp. Signal. 2013, 2, 1–15. [Google Scholar] [CrossRef]
- Dahle, J.; Kaalhus, O.; Moan, J.; Steen, H.B. Cooperative effects of photodynamic treatment of cells in microcolonies. Proc. Natl. Acad. Sci. USA 1997, 94, 1773–1778. [Google Scholar] [CrossRef] [PubMed]
- Dahle, J.; Angell-Petersen, E.; Steen, H.B.; Moan, J. Bystander Effects in Cell Death Induced by Photodynamic Treatment, UVA Radiation and Inhibitors of ATP Synthesis. Photochem. Photobiol. 2001, 73, 378–387. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Wang, Q.; Fan, L.; Wu, D.P.; Zhang, Y.; Liu, L.; Tao, L. Gap junction enhances phototoxicity of photodynamic therapy agent 2-[1-hexyloxyethyl]-2-devinylpyropheophorbide-a (HPPH). Lasers Surg. Med. 2015, 47, 68–76. [Google Scholar] [CrossRef] [PubMed]
- Thomas, C.D.; Poyer, F.; Maillard, P.; Chauvin, B.; Lupu, M.; Mispelter, J. Cellular density, a major factor involved in PDT cytotoxic responses: Study on three different lines of human retinoblastoma grafted on nude mice. Photodiagnosis Photodyn. Ther. 2015, 12, 267–275. [Google Scholar] [CrossRef] [PubMed]
- Hoorelbeke, D.; Decrock, E.; Van Haver, V.; De Bock, M.; Leybaert, L. Calcium, a pivotal player in photodynamic therapy? Biochim. Biophys. Acta Mol. Cell Res. 2018, 1865, 1805–1814. [Google Scholar] [CrossRef] [PubMed]
- Altan-Bonnet, G.; Mukherjee, R. Cytokine-mediated communication: A quantitative appraisal of immune complexity. Nat. Rev. Immunol. 2019, 19, 205–217. [Google Scholar] [CrossRef]
- Tang, S.; Chen, T.; Yang, M.; Wang, L.; Yu, Z.; Xie, B.; Qian, C.; Xu, S.; Li, N.; Cao, X. Extracellular calcium elicits feedforward regulation of the Toll-like receptor-triggered innate immune response. Cell. Mol. Immunol. 2017, 14, 180–191. [Google Scholar] [CrossRef]
- Turner, M.D.; Nedjai, B.; Hurst, T.; Pennington, D.J. Cytokines and chemokines: At the crossroads of cell signalling and inflammatory disease. Biochim. Biophys. Acta Mol. Cell Res. 2014, 1843, 2563–2582. [Google Scholar] [CrossRef]
- Habte-Tsion, H.-M.; Ren, M.; Liu, B.; Ge, X.; Xie, J.; Chen, R. Threonine modulates immune response, antioxidant status and gene expressions of antioxidant enzymes and antioxidant-immune-cytokine-related signaling molecules in juvenile blunt snout bream (Megalobrama amblycephala). Fish Shellfish. Immunol. 2016, 51, 189–199. [Google Scholar] [CrossRef]
- Miller, A.H.; Maletic, V.; Raison, C.L. Inflammation and its discontents: The role of cytokines in the pathophysiology of major depression. Biol. Psychiatry 2009, 65, 732–741. [Google Scholar] [CrossRef]
- Zhang, M.; Zhao, Y.; Ma, H.; Sun, Y.; Cao, J. How to improve photodynamic therapy-induced antitumor immunity for cancer treatment? Theranostics 2022, 12, 4629. [Google Scholar] [CrossRef] [PubMed]
- Gollnick, S.; Evans, S.; Baumann, H.; Owczarczak, B.; Maier, P.; Vaughan, L.; Wang, W.; Unger, E.; Henderson, B. Role of cytokines in photodynamic therapy-induced local and systemic inflammation. Br. J. Cancer 2003, 88, 1772–1779. [Google Scholar] [CrossRef]
- Dahle, J.; Kaalhus, O.; Stokke, T.; Kvam, E. Bystander effects may modulate ultraviolet A and B radiation-induced delayed mutagenesis. Radiat. Res. 2005, 163, 289–295. [Google Scholar] [CrossRef]
- Dahle, J.; Bagdonas, S.; Kaalhus, O.; Olsen, G.; Steen, H.B.; Moan, J. The bystander effect in photodynamic inactivation of cells. Biochim. Biophys. Acta Gen. Subj. 2000, 1475, 273–280. [Google Scholar] [CrossRef]
- Dahle, J.; Mikalsen, S.-O.; Rivedal, E.; Steen, H.B. Gap junctional intercellular communication is not a major mediator in the bystander effect in photodynamic treatment of MDCK II cells. Radiat. Res. 2000, 154, 331–341. [Google Scholar] [CrossRef] [PubMed]
- Tseng, S.-J.; Liao, Z.-X.; Kao, S.-H.; Zeng, Y.-F.; Huang, K.-Y.; Li, H.-J.; Yang, C.-L.; Deng, Y.-F.; Huang, C.-F.; Yang, S.-C. Highly specific in vivo gene delivery for p53-mediated apoptosis and genetic photodynamic therapies of tumour. Nat. Commun. 2015, 6, 6456. [Google Scholar] [CrossRef]
- Dorst, D.N.; Rijpkema, M.; Buitinga, M.; Walgreen, B.; Helsen, M.M.; Brennan, E.; Klein, C.; Laverman, P.; Ramming, A.; Schmidkonz, C. Targeting of fibroblast activation protein in rheumatoid arthritis patients: Imaging and ex vivo photodynamic therapy. Rheumatology 2022, 61, 2999–3009. [Google Scholar] [CrossRef] [PubMed]
- Rubio, N.; Rajadurai, A.; Held, K.D.; Prise, K.M.; Liber, H.L.; Redmond, R.W. Real-time imaging of novel spatial and temporal responses to photodynamic stress. Free. Radic. Biol. Med. 2009, 47, 283–290. [Google Scholar] [CrossRef] [PubMed]
- Leon, L.; Jeannin, J.-F.; Bettaieb, A. Post-translational modifications induced by nitric oxide (NO): Implication in cancer cells apoptosis. Nitric Oxide 2008, 19, 77–83. [Google Scholar] [CrossRef]
- Mocellin, S.; Bronte, V.; Nitti, D. Nitric oxide, a double edged sword in cancer biology: Searching for therapeutic opportunities. Med. Res. Rev. 2007, 27, 317–352. [Google Scholar] [CrossRef]
- Fahey, J.M.; Girotti, A.W. Nitric oxide-mediated resistance to photodynamic therapy in a human breast tumor xenograft model: Improved outcome with NOS2 inhibitors. Nitric Oxide 2017, 62, 52–61. [Google Scholar] [CrossRef]
- Bhowmick, R.; Girotti, A.W. Cytoprotective induction of nitric oxide synthase in a cellular model of 5-aminolevulinic acid-based photodynamic therapy. Free. Radic. Biol. Med. 2010, 48, 1296–1301. [Google Scholar] [CrossRef]
- Fahey, J.M.; Girotti, A.W. Accelerated migration and invasion of prostate cancer cells after a photodynamic therapy-like challenge: Role of nitric oxide. Nitric Oxide 2015, 49, 47–55. [Google Scholar] [CrossRef]
- Fahey, J.M.; Emmer, J.V.; Korytowski, W.; Hogg, N.; Girotti, A.W. Antagonistic effects of endogenous nitric oxide in a glioblastoma photodynamic therapy model. Photochem. Photobiol. 2016, 92, 842–853. [Google Scholar] [CrossRef] [PubMed]
- Fahey, J.M.; Stancill, J.S.; Smith, B.C.; Girotti, A.W. Nitric oxide antagonism to glioblastoma photodynamic therapy and mitigation thereof by BET bromodomain inhibitor JQ1. J. Biol. Chem. 2018, 293, 5345–5359. [Google Scholar] [CrossRef] [PubMed]
- Della Pietra, E.; Simonella, F.; Bonavida, B.; Xodo, L.E.; Rapozzi, V. Repeated sub-optimal photodynamic treatments with pheophorbide a induce an epithelial mesenchymal transition in prostate cancer cells via nitric oxide. Nitric Oxide 2015, 45, 43–53. [Google Scholar] [CrossRef] [PubMed]
- D’Este, F.; Della Pietra, E.; Pazmay, G.V.B.; Xodo, L.E.; Rapozzi, V. Role of nitric oxide in the response to photooxidative stress in prostate cancer cells. Biochem. Pharmacol. 2020, 182, 114205. [Google Scholar] [CrossRef]
- Ferino, A.; Rapozzi, V.; Xodo, L.E. The ROS-KRAS-Nrf2 axis in the control of the redox homeostasis and the intersection with survival-apoptosis pathways: Implications for photodynamic therapy. J. Photochem. Photobiol. B Biol. 2020, 202, 111672. [Google Scholar] [CrossRef]
- Rapozzi, V.; Umezawa, K.; Xodo, L.E. Role of NF-κB/Snail/RKIP loop in the response of tumor cells to photodynamic therapy. Lasers Surg. Med. 2011, 43, 575–585. [Google Scholar] [CrossRef]
- Rapozzi, V.; Della Pietra, E.; Zorzet, S.; Zacchigna, M.; Bonavida, B.; Xodo, L.E. Nitric oxide-mediated activity in anti-cancer photodynamic therapy. Nitric Oxide 2013, 30, 26–35. [Google Scholar] [CrossRef]
- Zhang, Y.-S.; Zhang, Y.-H.; Li, X.-J.; Hu, T.-C.; Chen, W.-Z.; Pan, X.; Chai, H.-Y.; Ye, Y.-C. Bystander effect and abscopal effect in recurrent thymic carcinoma treated with carbon-ion radiation therapy: A case report. World J. Clin. Cases 2021, 9, 6538. [Google Scholar] [CrossRef] [PubMed]
- Peters, M.E.; Shareef, M.M.; Gupta, S.; Zagurovskaya-Sultanov, M.; Kadhim, M.; Mohiuddin, M.; Ahmed, M.M. Potential utilization of bystander/abscopal-mediated signal transduction events in the treatment of solid tumors. Curr. Signal Transduct. Ther. 2007, 2, 129–143. [Google Scholar] [CrossRef]
- Beltrán Hernández, I.; Yu, Y.; Ossendorp, F.; Korbelik, M.; Oliveira, S. Preclinical and clinical evidence of immune responses triggered in oncologic photodynamic therapy: Clinical recommendations. J. Clin. Med. 2020, 9, 333. [Google Scholar] [CrossRef] [PubMed]
- Janopaul-Naylor, J.R.; Shen, Y.; Qian, D.C.; Buchwald, Z.S. The abscopal effect: A review of pre-clinical and clinical advances. Int. J. Mol. Sci. 2021, 22, 11061. [Google Scholar] [CrossRef]
- Nelson, B.E.; Adashek, J.J.; Lin, S.H.; Subbiah, V. On target methods to induce abscopal phenomenon for Off-Target effects: From happenstance to happenings. Cancer Med. 2023, 12, 6451–6465. [Google Scholar] [CrossRef] [PubMed]
- Hendren, S.K.; Hahn, S.M.; Spitz, F.R.; Bauer, T.W.; Rubin, S.C.; Zhu, T.; Glatstein, E.; Fraker, D.L. Phase II trial of debulking surgery and photodynamic therapy for disseminated intraperitoneal tumors. Ann. Surg. Oncol. 2001, 8, 65–71. [Google Scholar] [CrossRef]
- Thong, P.S.-P.; Ong, K.-W.; Goh, N.S.-G.; Kho, K.-W.; Manivasager, V.; Bhuvaneswari, R.; Olivo, M.; Soo, K.-C. Photodynamic-therapy-activated immune response against distant untreated tumours in recurrent angiosarcoma. Lancet Oncol. 2007, 8, 950–952. [Google Scholar] [CrossRef]
- Muhanna, N.; Cui, L.; Chan, H.; Burgess, L.; Jin, C.S.; MacDonald, T.D.; Huynh, E.; Wang, F.; Chen, J.; Irish, J.C. Multimodal Image-Guided Surgical and Photodynamic Interventions in Head and Neck Cancer: From Primary Tumor to Metastatic DrainageImage-Guided Interventions of Head and Neck Cancer. Clin. Cancer Res. 2016, 22, 961–970. [Google Scholar] [CrossRef]
- Rodrigues, M.C.; Vieira, L.G.; Horst, F.H.; de Araújo, E.C.; Ganassin, R.; Merker, C.; Meyer, T.; Böttner, J.; Venus, T.; Longo, J.P.F. Photodynamic therapy mediated by aluminium-phthalocyanine nanoemulsion eliminates primary tumors and pulmonary metastases in a murine 4T1 breast adenocarcinoma model. J. Photochem. Photobiol. B Biol. 2020, 204, 111808. [Google Scholar] [CrossRef]
- Korbelik, M.; Zhang, W.; Merchant, S. Involvement of damage-associated molecular patterns in tumor response to photodynamic therapy: Surface expression of calreticulin and high-mobility group box-1 release. Cancer Immunol. Immunother. 2011, 60, 1431–1437. [Google Scholar] [CrossRef]
- Duan, X.; Chan, C.; Guo, N.; Han, W.; Weichselbaum, R.R.; Lin, W. Photodynamic therapy mediated by nontoxic core–shell nanoparticles synergizes with immune checkpoint blockade to elicit antitumor immunity and antimetastatic effect on breast cancer. J. Am. Chem. Soc. 2016, 138, 16686–16695. [Google Scholar] [CrossRef]
- He, C.; Duan, X.; Guo, N.; Chan, C.; Poon, C.; Weichselbaum, R.R.; Lin, W. Core-shell nanoscale coordination polymers combine chemotherapy and photodynamic therapy to potentiate checkpoint blockade cancer immunotherapy. Nat. Commun. 2016, 7, 12499. [Google Scholar] [CrossRef]
- Sasaki, M.; Tanaka, M.; Kojima, Y.; Nishie, H.; Shimura, T.; Kubota, E.; Kataoka, H. Anti-tumor immunity enhancement by photodynamic therapy with talaporfin sodium and anti-programmed death 1 antibody. Mol. Ther. Oncolytics 2023, 28, 118–131. [Google Scholar] [CrossRef]
- Xie, Q.; Li, Z.; Liu, Y.; Zhang, D.; Su, M.; Niitsu, H.; Lu, Y.; Coffey, R.J.; Bai, M. Translocator protein-targeted photodynamic therapy for direct and abscopal immunogenic cell death in colorectal cancer. Acta Biomater. 2021, 134, 716–729. [Google Scholar] [CrossRef] [PubMed]
- Lou, J.; Aragaki, M.; Bernards, N.; Chee, T.; Gregor, A.; Hiraishi, Y.; Ishiwata, T.; Leung, C.; Ding, L.; Kitazawa, S. Repeated photodynamic therapy mediates the abscopal effect through multiple innate and adaptive immune responses with and without immune checkpoint therapy. Biomaterials 2023, 292, 121918. [Google Scholar] [CrossRef] [PubMed]
- Gurung, P.; Lim, J.; Shrestha, R.; Kim, Y.-W. Chlorin e6-associated photodynamic therapy enhances abscopal antitumor effects via inhibition of PD-1/PD-L1 immune checkpoint. Sci. Rep. 2023, 13, 4647. [Google Scholar] [CrossRef]
- Bian, Q.; Huang, L.; Xu, Y.; Wang, R.; Gu, Y.; Yuan, A.; Ma, X.; Hu, J.; Rao, Y.; Xu, D. A facile low-dose photosensitizer-incorporated dissolving microneedles-based composite system for eliciting antitumor immunity and the abscopal effect. ACS Nano 2021, 15, 19468–19479. [Google Scholar] [CrossRef] [PubMed]
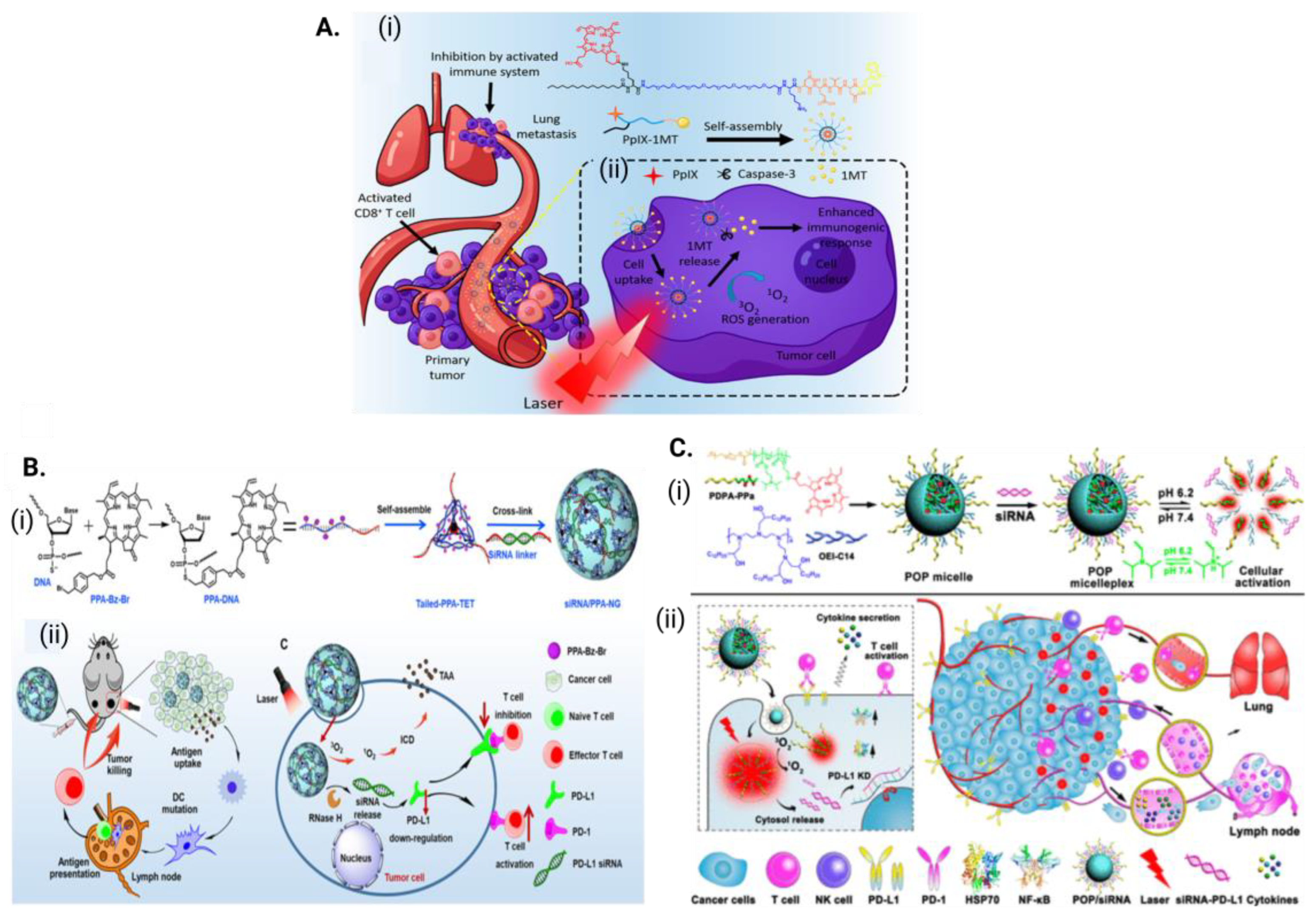
- Song, W.; Kuang, J.; Li, C.-X.; Zhang, M.; Zheng, D.; Zeng, X.; Liu, C.; Zhang, X.-Z. Enhanced immunotherapy based on photodynamic therapy for both primary and lung metastasis tumor eradication. ACS Nano 2018, 12, 1978–1989. [Google Scholar] [CrossRef]
- Wang, D.; Wang, T.; Liu, J.; Yu, H.; Jiao, S.; Feng, B.; Zhou, F.; Fu, Y.; Yin, Q.; Zhang, P. Acid-activatable versatile micelleplexes for PD-L1 blockade-enhanced cancer photodynamic immunotherapy. Nano Lett. 2016, 16, 5503–5513. [Google Scholar] [CrossRef]
- Guo, Y.; Zhang, Q.; Zhu, Q.; Gao, J.; Zhu, X.; Yu, H.; Li, Y.; Zhang, C. Copackaging photosensitizer and PD-L1 siRNA in a nucleic acid nanogel for synergistic cancer photoimmunotherapy. Sci. Adv. 2022, 8, eabn2941. [Google Scholar] [CrossRef]
- Xu, J.; Xu, L.; Wang, C.; Yang, R.; Zhuang, Q.; Han, X.; Dong, Z.; Zhu, W.; Peng, R.; Liu, Z. Near-infrared-triggered photodynamic therapy with multitasking upconversion nanoparticles in combination with checkpoint blockade for immunotherapy of colorectal cancer. ACS Nano 2017, 11, 4463–4474. [Google Scholar] [CrossRef]
- Wang, Z.; Zhang, F.; Shao, D.; Chang, Z.; Wang, L.; Hu, H.; Zheng, X.; Li, X.; Chen, F.; Tu, Z. Janus nanobullets combine photodynamic therapy and magnetic hyperthermia to potentiate synergetic anti-metastatic immunotherapy. Adv. Sci. 2019, 6, 1901690. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Jeon, Y.-H.; Kwon, N.; Park, J.-G.; Guo, T.; Kim, H.-R.; Huang, J.-D.; Lee, D.-S.; Yoon, J. In Vivo-assembled phthalocyanine/albumin supramolecular complexes combined with a hypoxia-activated prodrug for enhanced photodynamic immunotherapy of cancer. Biomaterials 2021, 266, 120430. [Google Scholar] [CrossRef] [PubMed]
- Wang, R.; Kim, K.-H.; Yoo, J.; Li, X.; Kwon, N.; Jeon, Y.-H.; Shin, S.-k.; Han, S.S.; Lee, D.-S.; Yoon, J. A nanostructured phthalocyanine/albumin supramolecular assembly for fluorescence turn-on imaging and photodynamic immunotherapy. ACS Nano 2022, 16, 3045–3058. [Google Scholar] [CrossRef] [PubMed]
- Zhou, S.; Zhen, Z.; Paschall, A.V.; Xue, L.; Yang, X.; Bebin Blackwell, A.G.; Cao, Z.; Zhang, W.; Wang, M.; Teng, Y. FAP-Targeted Photodynamic Therapy Mediated by Ferritin Nanoparticles Elicits an Immune Response against Cancer Cells and Cancer Associated Fibroblasts. Adv. Funct. Mater. 2021, 31, 2007017. [Google Scholar] [CrossRef]
| Generations | Family and Name of PS |
|---|---|
| G1 | Porphyrin family: HpD, BPD (benzoporphyrin derivative), ALA, Texaphyrins [15,25]. |
| G2 | Chlorin family: Temoporfin, Purlytin(tin-ethyl-etiopurpurin), NPe6(mono-L-aspartyl chlorin e6), LS11(Talaporfin sodium), HPPH (Photochlor), 5-aminolevulinic acid (ALA), Benzoporphyrin derivative (BPD), Tinethyletiopurpurin (SnET2), Bacteriochlorins, Methylene blue derivatives, Toluidine blue, Phthalocynine, Curcumin [26,27]. |
| G3 | Dye family: Naphthalocyanine (tin2,3naphthalocyanine), Phthalocyanine [28]. |
| PS/PS-Based Nanostructures/Formulations | Immune Checkpoint Inhibitors | In Vivo Model |
|---|---|---|
| Upconversion nanoparticles loaded with chlorin e6 (PS) and imiquimod (R837) (Toll-like-receptor-7 agonist) | CTLA-4 * | CT26 colorectal cancer murine model [103] |
| Cancer-cell-membrane-cloaked Janus magnetic mesoporous organosilica nanoparticles loaded with chlorin e6 | CTLA-4 | 4T1 breast cancer murine model with lung metastases [104] |
| Phthalocyanine derivative albumin supramolecular complexes | PD-1 * or PD-L1 * | 4T1 breast cancer murine model [105] |
| Supramolecular self-assembly of morpholine-modified silica phthalocyanine (PcM) and serum albumin (SA) | PD-1 | 4T1 breast cancer murine model with lung metastases [106] |
| Zn-pyrophosphate (ZnP) nanoparticles loaded with pyrolipid (photosensitizer) | PD-L1 | 4T1 and TUBO breast cancer murine model with lung metastases [93] |
| Core–shell nanoparticles with oxaliplatin in the core and the PS pyrolipid in the shell | PD-L1 | HT29 and CT26 colorectal cancer murine model [94] |
| Cancer-associated-fibroblast-targeted FAP-specific single-chain variable-fragment (scFv)-conjugated ferritin nanoparticles loaded with ZnF16Pc | PD-1 | 4T1 breast cancer murine model [107] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moloudi, K.; Sarbadhikary, P.; Abrahamse, H.; George, B.P. Understanding the Photodynamic Therapy Induced Bystander and Abscopal Effects: A Review. Antioxidants 2023, 12, 1434. https://doi.org/10.3390/antiox12071434
Moloudi K, Sarbadhikary P, Abrahamse H, George BP. Understanding the Photodynamic Therapy Induced Bystander and Abscopal Effects: A Review. Antioxidants. 2023; 12(7):1434. https://doi.org/10.3390/antiox12071434
Chicago/Turabian StyleMoloudi, Kave, Paromita Sarbadhikary, Heidi Abrahamse, and Blassan P. George. 2023. "Understanding the Photodynamic Therapy Induced Bystander and Abscopal Effects: A Review" Antioxidants 12, no. 7: 1434. https://doi.org/10.3390/antiox12071434
APA StyleMoloudi, K., Sarbadhikary, P., Abrahamse, H., & George, B. P. (2023). Understanding the Photodynamic Therapy Induced Bystander and Abscopal Effects: A Review. Antioxidants, 12(7), 1434. https://doi.org/10.3390/antiox12071434







