Tea Tree Oil: Properties and the Therapeutic Approach to Acne—A Review
Abstract
1. Introduction
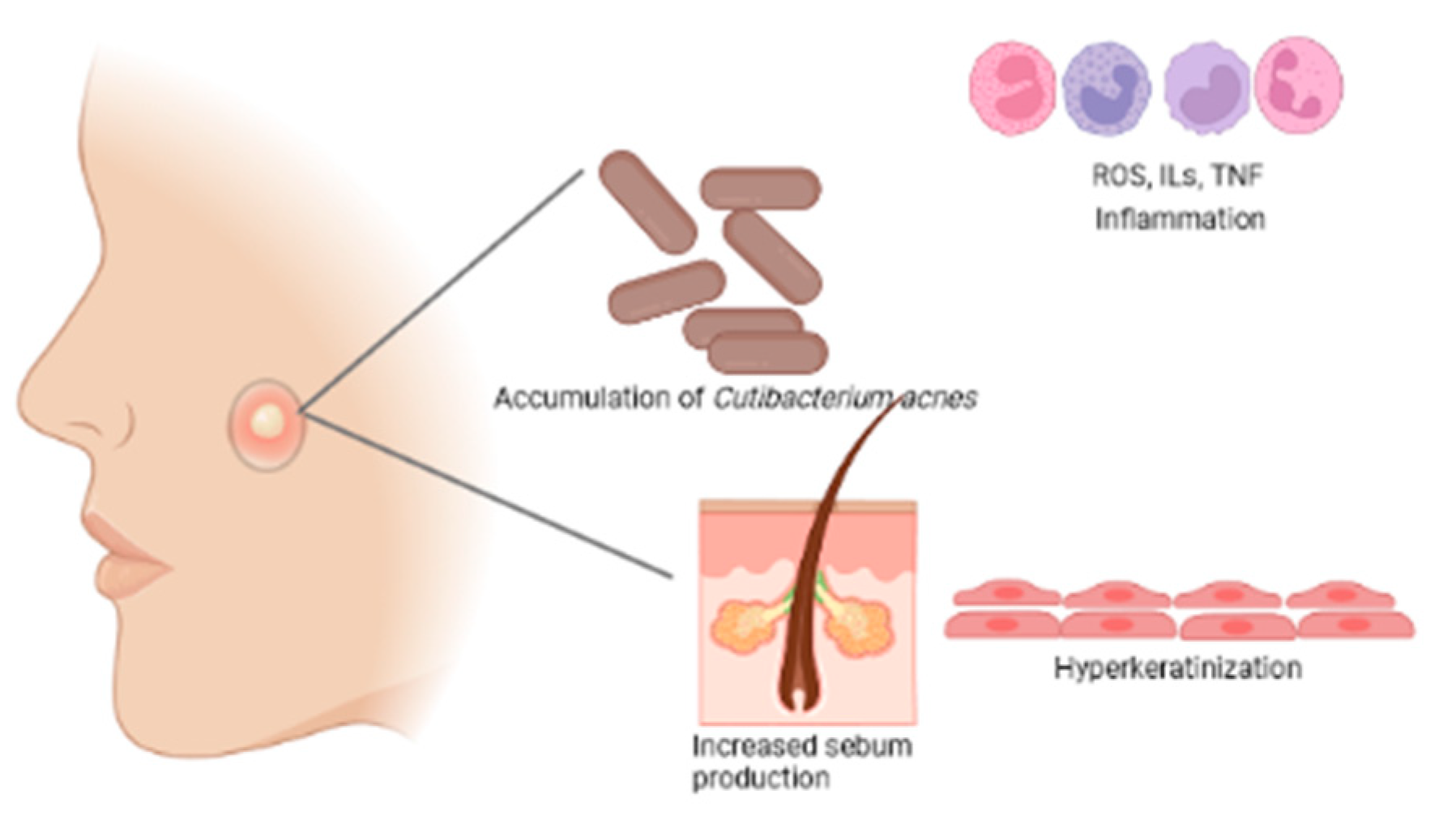
2. Physiopathology of Acne Vulgaris
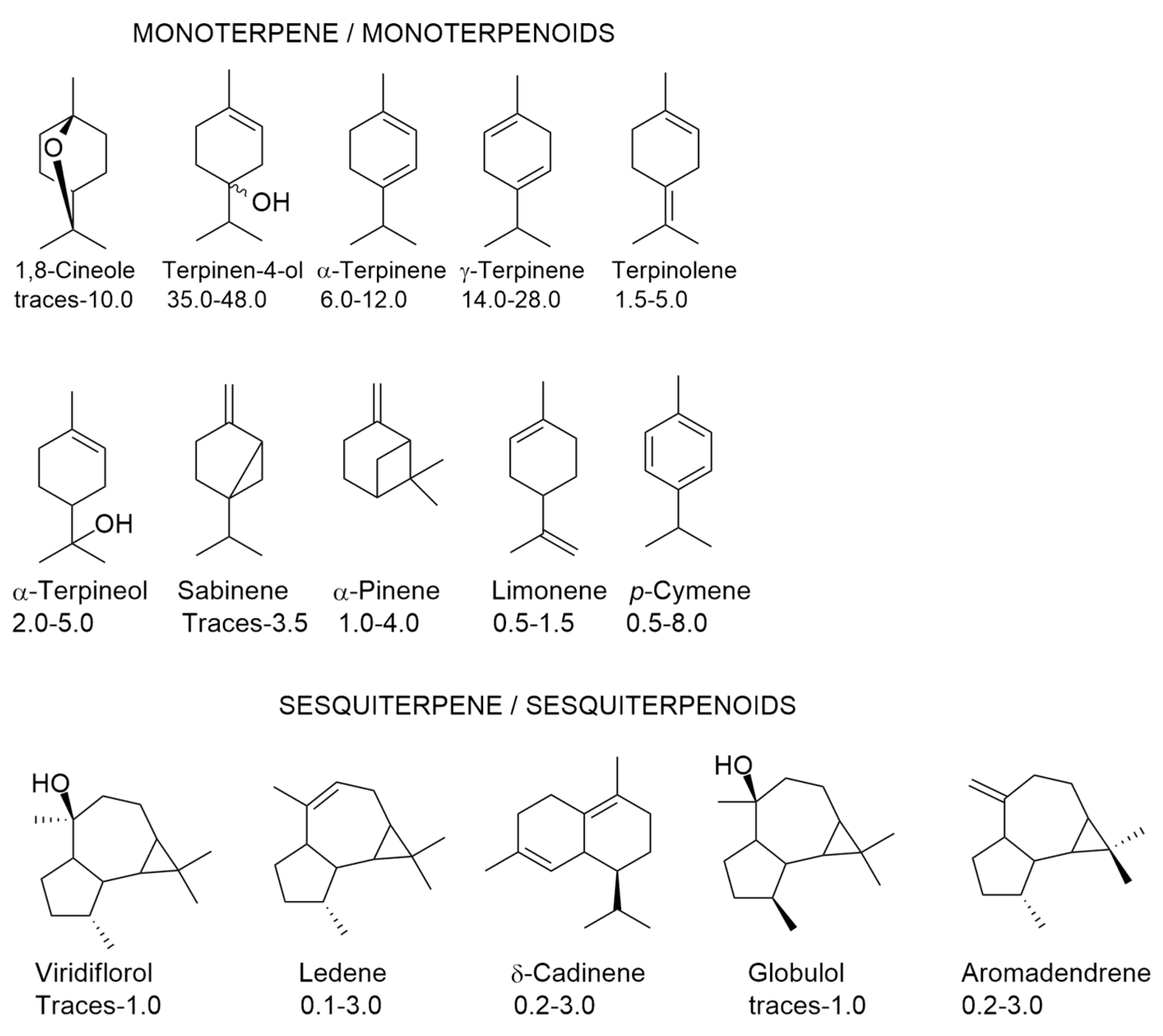
3. Components of Tea Tree Oil (TTO) and Their Variability
4. Biological Properties of TTO
4.1. Antimicrobial Activity of TTO
Tea Tree Oil Formulations with Antimicrobial Activity
5. Anti-Inflammatory Properties of TTO and/or Their Fractions
6. Antioxidant Properties of TTO
6.1. Antioxidant Properties of TTO in Food Matrices
6.2. Antioxidant Properties of TTO in Non-Food Matrices
7. Toxicity of TTO
8. Efficacy of TTO in Acne Therapy—Studies in Humans
9. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Nurzyńska-Wierdak, R.; Pietrasik, D.; Walasek-Janusz, M.W. Essential oils in the treatment of various types of acne—A review. Plants 2023, 12, 90. [Google Scholar] [CrossRef]
- Heng, A.H.S.; Chew, F.T. Systematic Review of the Epidemiology of Acne Vulgaris. Sci Rep. 2020, 10, 5754. [Google Scholar] [CrossRef]
- Nast, A.; Dréno, B.; Bettoli, V.; Degitz, K.; Erdmann, R.; Finlay, A.Y.; Ganceviciene, R.; Haedersdal, M.; Layton, A.; López-Estebaranz, J.L.; et al. European Evidence-Based (S3) Guidelines for the Treatment of Acne. J. Eur. Acad. Dermatol. Venereol. 2012, 26 (Suppl. 1), 1–29. [Google Scholar] [CrossRef]
- Nast, A.; Dréno, B.; Bettoli, V.; Bukvic Mokos, Z.; Degitz, K.; Dressler, C.; Finlay, A.Y.; Haedersdal, M.; Lambert, J.; Layton, A.; et al. European Evidence-Based (S3) Guideline for the Treatment of Acne–Update 2016–Short Version. J. Eur. Acad. Dermatol. Venereol. 2016, 30, 1261–1268. [Google Scholar] [CrossRef]
- Proença, A.C.; Luís, Â.; Duarte, A.P. The Role of Herbal Medicine in the Treatment of Acne Vulgaris: A Systematic Review of Clinical Trials. J. Evid. Based Complement. Altern. Med. 2022, 2022, 2011945. [Google Scholar] [CrossRef]
- Sinha, P.; Srivastava, S.; Mishra, N.; Yadav, N.P. New Perspectives on Antiacne Plant Drugs: Contribution to Modern Therapeutics. Biomed. Res. Int. 2014, 2014, 301304. [Google Scholar] [CrossRef]
- Ogé, L.K.; Broussard, A.; Marshall, M.D. Acne Vulgaris: Diagnosis and Treatment. Am. Fam. Physician 2019, 100, 475–484. [Google Scholar]
- Cha, H.M.; Kim, S.K.; Kook, M.C.; Yi, T.H. Lactobacillus paraplantarum THG-G10 as a Potential Anti-Acne Agent with Anti-Bacterial and Anti-Inflammatory Activities. Anaerobe 2020, 64, 102243. [Google Scholar] [CrossRef]
- Abozeid, D.; Fawzy, G.; Issa, M.; Abdeltawab, N.; Soliman, F. Medicinal Plants and Their Constituents in the Treatment of Acne Vulgaris. Biointerface Res. Appl. Chem. 2023, 13, 189. [Google Scholar] [CrossRef]
- Asnaashari, S.; Kazemnezhad, M.; Masoud, F.; Javadzadeh, Y. An Overview on the Anti-Acne Properties of Herbal Essential Oils. J. Herb. Med. 2023, 38, 100642. [Google Scholar] [CrossRef]
- ISO 9235: 2021; Aromatic Natural Raw Materials—Vocabulary. Technical Committee ISO: Geneva, Switzerland, 2021.
- Dréno, B. What Is New in the Pathophysiology of Acne, an Overview. J. Eur. Acad. Dermatol. Venereol. 2017, 31, 8–12. [Google Scholar] [CrossRef]
- Saurat, J.H. Strategic Targets in Acne: The Comedone Switch in Question. Dermatology 2015, 231, 105–111. [Google Scholar] [CrossRef]
- Kurokawa, I.; Nakase, K. Recent Advances in Understanding and Managing Acne. F1000Research 2020, 9, 792. [Google Scholar] [CrossRef]
- Cunliffe, W.J.; Holland, D.B.; Jeremy, A. Comedone Formation: Etiology, Clinical Presentation, and Treatment. Clin. Dermatol. 2004, 22, 367–374. [Google Scholar] [CrossRef]
- Zouboulis, C.C.; Picardo, M.; Ju, Q.; Kurokawa, I.; Törőcsik, D.; Bíró, T.; Schneider, M.R. Beyond Acne: Current Aspects of Sebaceous Gland Biology and Function. Rev. Endocr. Metab. Disord. 2016, 17, 319–334. [Google Scholar] [CrossRef]
- Josse, G.; Mias, C.; Le Digabel, J.; Filiol, J.; Ipinazar, C.; Villaret, A.; Gomiero, C.; Bevilacqua, M.; Redoules, D.; Nocera, T.; et al. High Bacterial Colonization and Lipase Activity in Microcomedones. Exp. Dermatol. 2020, 29, 168–176. [Google Scholar] [CrossRef]
- Dréno, B.; Dagnelie, M.A.; Khammari, A.; Corvec, S. The Skin Microbiome: A New Actor in Inflammatory Acne. Am. J. Clin. Dermatol. 2020, 21, 18–24. [Google Scholar] [CrossRef]
- Ramasamy, S.; Barnard, E.; Dawson, T.L.; Li, H. The Role of the Skin Microbiota in Acne Pathophysiology. Br. J. Dermatol. 2019, 181, 691–699. [Google Scholar] [CrossRef]
- Chilicka, K.; Dzieńdziora-Urbińska, I.; Szyguła, R.; Asanova, B.; Nowicka, D. Microbiome and Probiotics in Acne Vulgaris—A Narrative Review. Life 2022, 12, 422. [Google Scholar] [CrossRef]
- Yang, J.; Yang, H.; Xu, A.; He, L. A Review of Advancement on Influencing Factors of Acne: An Emphasis on Environment Characteristics. Front. Public Health 2020, 8, 450. [Google Scholar] [CrossRef]
- Borrel, V.; Gannesen, A.V.; Barreau, M.; Gaviard, C.; Duclairoir-Poc, C.; Hardouin, J.; Konto-Ghiorghi, Y.; Lefeuvre, L.; Feuilloley, M.G.J. Adaptation of Acneic and Non Acneic Strains of Cutibacterium acnes to Sebum-like Environment. Microbiologyopen 2019, 8, e841. [Google Scholar] [CrossRef]
- Metiko, B.; Brooks, K.; Burkhart, C.G.; Burkhart, C.N.; Morrell, D. Is the Current Model for Acne Pathogenesis Backwards? J. Am. Acad. Dermatol. 2015, 72, e167. [Google Scholar] [CrossRef]
- Shaheen, B.; Gonzalez, M. Acne sans P. acnes. J. Eur. Acad. Dermatol. Venereol. 2013, 27, 1–10. [Google Scholar] [CrossRef]
- Toyoda, M.; Morohashi, M. An Overview of Topical Antibiotics for Acne Treatment. Dermatology 1998, 196, 130–134. [Google Scholar] [CrossRef]
- Kim, H.J.; Chen, F.; Wu, C.; Wang, X.; Chung, H.Y.; Jin, Z. Evaluation of Antioxidant Activity of Australian Tea Tree (Melaleuca alternifolia) Oil and Its Components. J. Agric. Food Chem. 2004, 52, 2849–2854. [Google Scholar] [CrossRef]
- Noh, H.H.; Shin, S.H.; Roh, Y.J.; Moon, N.J.; Seo, S.J.; Park, K.Y. Particulate Matter Increases Cutibacterium Acnes-Induced Inflammation in Human Epidermal Keratinocytes via the TLR4/NF-ΚB Pathway. PLoS ONE 2022, 17, e0268595. [Google Scholar] [CrossRef]
- Brun, P.; Bernabè, G.; Filippini, R.; Piovan, A. In Vitro Antimicrobial Activities of Commercially Available Tea Tree (Melaleuca alternifolia) Essential Oils. Curr. Microbiol. 2019, 76, 108–116. [Google Scholar] [CrossRef]
- Lwin, S.M.; Kimber, I.; McFadden, J.P. Acne, Quorum Sensing and Danger. Clin. Exp. Dermatol. 2014, 39, 162–167. [Google Scholar] [CrossRef]
- Carson, C.F.; Hammer, K.A.; Riley, T.V. Melaleuca Alternifolia (Tea Tree) Oil: A Review of Antimicrobial and Other Medicinal Properties. Clin. Microbiol. Rev. 2006, 19, 50. [Google Scholar] [CrossRef]
- Zhang, X.; Chen, S.; Zhang, Y.; Xiao, Y.; Qin, Y.; Li, Q.; Liu, L.; Liu, B.; Chai, L.; Yang, H.; et al. Draft Genome of the Medicinal Tea Tree Melaleuca alternifolia. Mol. Biol. Rep. 2023, 50, 1545–1552. [Google Scholar] [CrossRef]
- Caldefie-Chézet, F.; Fusillier, C.; Jarde, T.; Laroye, H.; Damez, M.; Vasson, M.P.; Guillot, J. Potential Anti-Inflammatory Effects of Melaleuca alternifolia Essential Oil on Human Peripheral Blood Leukocytes. Phytother. Res. 2006, 20, 364–370. [Google Scholar] [CrossRef]
- American Botanical Council. Botanical Adulterants Program Publishes Bulletin on Tea Tree Oil Adulteration. Available online: https://www.herbalgram.org/news/press-releases/2017/botanical-adulterants-program-publishes-bulletin-on-tea-tree-oil-adulteration/ (accessed on 20 February 2023).
- Voelker, J.; Mauleon, R.; Shepherd, M. The Terpene Synthase Genes of Melaleuca alternifolia (Tea Tree) and Comparative Gene Family Analysis Among Myrtaceae Essential Oil Crops. Plant Syst. Evol. 2023, 309, 13. [Google Scholar] [CrossRef]
- Homer, L.E.; Leach, D.N.; Lea, D.; Slade Lee, L.; Henry, R.J.; Baverstock, P.R. Natural Variation in the Essential Oil Content of Melaleuca alternifolia Cheel (Myrtaceae). Biochem. Syst. Ecol. 2000, 28, 367–382. [Google Scholar] [CrossRef]
- ISO 4730:2017; Essential Oil of Melaleuca, Terpinen-4-Ol Type (Tea Tree Oil). Technical Committee ISO/TC 54: Geneva, Switzerland, 2017.
- Gloerfelt-Tarp, F.; Micog, J.C.; Bigland, M.; Wheeler, S.; Palmer, W.M.; Kretzschmar, T. Predicting Tea Tree Oil Distillate Composition Using Portable Spectrometric Technology. J. Raman Spectrosc. 2022, 53, 771–784. [Google Scholar] [CrossRef]
- Shelton, D.; Aitken, K.; Doimo, L.; Leach, D.; Baverstock, P.; Henry, R. Genetic Control of Monoterpene Composition in the Essential Oil of Melaleuca alternifolia (Cheel). Theor. Appl. Genet. 2002, 105, 377–383. [Google Scholar] [CrossRef]
- Southwell, I.; Dowell, A.; Morrow, S.; Allen, G.; Savins, D.; Shepherd, M. Monoterpene Chiral Ratios: Chemotype Diversity and Interspecific Commonality in Melaleuca alternifolia and M. linariifolia. Ind. Crops Prod. 2017, 109, 850–856. [Google Scholar] [CrossRef]
- Butcher, P.A.; Doran, J.C.; Slee, M.U. Intraspecific Variation in Leaf Oils of Melaleuca alternifolia (Myrtaceae). Biochem. Syst. Ecol. 1994, 22, 419–430. [Google Scholar] [CrossRef]
- Butcher, P.A.; Matheson, A.C.; Slee, M.U. Potential for Genetic Improvement of Oil Production in Melaleuca alternifolia and M. linariifolia. New For. 1996, 11, 31–51. [Google Scholar] [CrossRef]
- Zabaras, D.; Spooner-hart, R.N.; Wyllie, S.G. Effects of Mechanical Wounding on Concentration and Composition of Essential Oil from Melaleuca alternifolia Leaves. Biochem. Syst. Ecol. 2002, 30, 399–412. [Google Scholar] [CrossRef]
- Figueiredo, M. Chemical Composition and oil Concentration of Tea Tree Leaf Oil Grown in South Africa During a One-Year Vegetative Cycle. J. Essent. Oil Res. 2006, 18, 52–53. [Google Scholar] [CrossRef]
- Silva, C.J.; Barbosa, L.C.A.; Maltha, C.R.A.; Pinheiro, A.L.; Ismail, F.M.D. Comparative Study of the Essential Oils of Seven Melaleuca (Myrtaceae) Species Grown in Brazil. Flavour Fragr. J. 2007, 22, 474–478. [Google Scholar] [CrossRef]
- Baker, G.R.; Lowe, R.F.; Southwell, I.A. Comparison of Oil Recovered from Tea Tree Leaf by Ethanol Extraction and Steam Distillation. J. Agric. Food Chem. 2000, 48, 4041–4043. [Google Scholar] [CrossRef]
- Wong, V.; Wyllie, S.G.; Cornwell, C.P.; Tronson, D. Supercritical Fluid Extraction (SFE) of Monoterpenes from the Leaves of Melaleuca alternifolia (Tea Tree). Molecules 2001, 6, 92–103. [Google Scholar] [CrossRef]
- Carson, C.F.; Riley, T.V. Antimicrobial Activity of the Essential Oil of Melaleuca alternifolia. Lett. Appl. Microbiol. 1993, 16, 49–55. [Google Scholar] [CrossRef]
- Bezabh, S.A.; Tesfaye, W.; Christenson, J.K.; Carson, C.F.; Thomas, J. Antiparasitic Activity of Tea Tree Oil (TTO) and Its Components against Medically Important Ectoparasites: A Systematic Review. Pharmaceutics 2022, 14, 1587. [Google Scholar] [CrossRef]
- Lam, N.S.K.; Long, X.X.; Griffin, R.C.; Chen, M.K.; Doery, J.C.G. Can the Tea Tree Oil (Australian Native Plant: Melaleuca alternifolia Cheel) Be an Alternative Treatment for Human Demodicosis on Skin? Parasitology 2018, 145, 1510–1520. [Google Scholar] [CrossRef]
- Sharifi-Rad, J.; Salehi, B.; Varoni, E.M.; Sharopov, F.; Yousaf, Z.; Ayatollahi, S.A.; Kobarfard, F.; Sharifi-Rad, M.; Afdjei, M.H.; Iriti, M. Plants of the Melaleuca Genus as Antimicrobial Agents: From Farm to Pharmacy. Phytother. Res. 2017, 31, 1475–1494. [Google Scholar] [CrossRef]
- Johnson, J.B.; Thani, P.R.; Mani, J.S.; Cozzolino, D.; Naiker, M. Mid-Infrared Spectroscopy for the Rapid Quantification of Eucalyptus Oil Adulteration in Australian Tea Tree Oil (Melaleuca alternifolia). Spectrochim. Acta Part A Mol. Biomol. Spectrosc. 2022, 283, 121766. [Google Scholar] [CrossRef]
- May, J.; Chan, C.H.; King, A.; Williams, L.; French, G.L. Time-Kill Studies of Tea Tree Oils on Clinical Isolates. J. Antimicrob. Chemother. 2000, 45, 639–643. [Google Scholar] [CrossRef]
- Cox, S.D.; Mann, C.M.; Markham, J.L.; Gustafson, J.E.; Warmington, J.R.; Wyllie, S.G. Determining the Antimicrobial Actions of Tea Tree Oil. Molecules 2001, 6, 87–91. [Google Scholar] [CrossRef]
- Cox, S.D.; Mann, C.M.; Markham, J.L.; Bell, H.C.; Gustafson, J.E.; Warmington, J.R.; Wyllie, S.G. The Mode of Antimicrobial Action of the Essential Oil of Melaleuca alternifolia (Tea Tree Oil). J. Appl. Microbiol. 2000, 88, 170–175. [Google Scholar] [CrossRef]
- Cox, S.D.; Gustafson, J.E.; Mann, C.M.; Markham, J.L.; Liew, Y.C.; Hartland, R.P.; Bell, H.C.; Warmington, J.R.; Wyllie, S.G. Tea Tree Oil Causes K+ Leakage and Inhibits Respiration in Escherichia coli. Lett. Appl. Microbiol. 1998, 26, 355–358. [Google Scholar] [CrossRef]
- Gustafson, J.E.; Liew, Y.C.; Chew, S.; Markham, J.; Bell, H.C.; Wyllie, S.G.; Warmington, J.R. Effects of Tea Tree Oil on Escherichia coli. Lett. Appl. Microbiol. 1998, 26, 194–198. [Google Scholar] [CrossRef]
- Li, W.R.; Li, H.L.; Shi, Q.S.; Sun, T.L.; Xie, X.B.; Song, B.; Huang, X.M. The Dynamics and Mechanism of the Antimicrobial Activity of Tea Tree Oil against Bacteria and Fungi. Appl. Microbiol. Biotechnol. 2016, 100, 8865–8875. [Google Scholar] [CrossRef]
- Cuaron, J.A.; Dulal, S.; Song, Y.; Singh, A.K.; Montelongo, C.E.; Yu, W.; Nagarajan, V.; Jayaswal, R.K.; Wilkinson, B.J.; Gustafson, J.E. Tea Tree Oil-Induced Transcriptional Alterations in Staphylococcus aureus. Phytother. Res. 2013, 27, 390–396. [Google Scholar] [CrossRef]
- Mondello, F.; Fontana, S.; Scaturro, M.; Girolamo, A.; Colone, M.; Stringaro, A.; Di Vito, M.; Ricci, M.L. Terpinen-4-Ol, the Main Bioactive Component of Tea Tree Oil, as an Innovative Antimicrobial Agent against Legionella pneumophila. Pathogens 2022, 11, 682. [Google Scholar] [CrossRef]
- Qi, J.; Gong, M.; Zhang, R.; Song, Y.; Liu, Q.; Zhou, H.; Wang, J.; Mei, Y. Evaluation of the Antibacterial Effect of Tea Tree Oil on Enterococcus faecalis and Biofilm in Vitro. J. Ethnopharmacol. 2021, 281, 114566. [Google Scholar] [CrossRef]
- Iseppi, R.; Mariani, M.; Benvenuti, S.; Truzzi, E.; Messi, P. Effects of Melaleuca alternifolia Chell (Tea Tree) and Eucalyptus globulus Labill. Essential Oils on Antibiotic-Resistant Bacterial Biofilms. Molecules 2023, 28, 1671. [Google Scholar] [CrossRef]
- Brożyna, M.; Paleczny, J.; Kozłowska, W.; Chodaczek, G.; Dudek-Wicher, R.; Felińczak, A.; Gołębiewska, J.; Górniak, A.; Junka, A. The Antimicrobial and Antibiofilm in Vitro Activity of Liquid and Vapour Phases of Selected Essential Oils against Staphylococcus aureus. Pathogens 2021, 10, 1207. [Google Scholar] [CrossRef]
- Oliva, A.; Costantini, S.; de Angelis, M.; Garzoli, S.; Božović, M.; Mascellino, M.T.; Vullo, V.; Ragno, R. High Potency of Melaleuca alternifolia Essential Oil Against Multi-Drug Resistant Gram-Negative Bacteria and Methicillin-Resistant Staphylococcus aureus. Molecules 2018, 23, 2584. [Google Scholar] [CrossRef]
- Borotová, P.; Galovičová, L.; Vukovic, N.L.; Vukic, M.; Tvrdá, E.; Kačániová, M. Chemical and Biological Characterization of Melaleuca alternifolia Essential Oil. Plants 2022, 11, 558. [Google Scholar] [CrossRef]
- Banes-Marshall, L.; Cawley, P.; Phillips, C.A. In Vitro Activity of Melaleuca alternifolia (Tea Tree) Oil against Bacterial and Candida spp. Isolates from Clinical Specimens. Br. J. Biomed. Sci. 2001, 58, 139–145. [Google Scholar]
- Kwieciński, J.; Eick, S.; Wójcik, K. Effects of Tea Tree (Melaleuca alternifolia) Oil on Staphylococcus aureus in Biofilms and Stationary Growth Phase. Int. J. Antimicrob. Agents 2009, 33, 343–347. [Google Scholar] [CrossRef]
- Loughlin, R.; Gilmore, B.F.; McCarron, P.A.; Tunney, M.M. Comparison of the Cidal Activity of Tea Tree Oil and Terpinen-4-Ol against Clinical Bacterial Skin Isolates and Human Fibroblast Cells. Lett. Appl. Microbiol. 2008, 46, 428–433. [Google Scholar] [CrossRef] [PubMed]
- Blejan, E.I.; Popa, D.E.; Costea, T.; Cioacă, A.; Olariu, L.; Ghica, M.; Georgescu, M.; Stancov, G.; Arsene, A.L. The in Vitro Antimicrobial Activity of Some Essential Oils from Aromatic Plants. Farmacia 2021, 69, 290–298. [Google Scholar] [CrossRef]
- Ramadan, M.A.; Shawkey, A.E.; Rabeh, M.A.; Abdellatif, A.O. Promising Antimicrobial Activities of Oil and Silver Nanoparticles Obtained from Melaleuca alternifolia Leaves against Selected Skin-Infecting Pathogens. J. Herb. Med. 2020, 2020, 100289. [Google Scholar] [CrossRef]
- Hammer, K.A.; Carson, C.F.; Riley, T.V. In Vitro Susceptibilities of Lactobacilli and Organisms Associated with Bacterial Vaginosis to Melaleuca alternifolia (Tea Tree) Oil. Antimicrob. Agents Chemother. 1999, 43, 196. [Google Scholar] [CrossRef]
- Ossa-Tabares, J.C.; Llanos, C.J.; García, A.M. Evaluation of Tea Tree Oil Physicochemical Features and Its Antimicrobial Activity against Cutibacterium acnes (Propionibacterium acnes) ATCC 6919. Biomedica 2020, 40, 693–694. [Google Scholar] [CrossRef]
- Nenoff, P.; Haustein, U.F.; Brandt, W. Antifungal Activity of the Essential Oil of Melaleuca alternifolia (Tea Tree Oil) against Pathogenic Fungi in vitro. Ski. Pharmacol. 1996, 9, 388–394. [Google Scholar] [CrossRef] [PubMed]
- Ngenge, A.T.; Kucukaydin, S.; Ceylan, O.; Duru, M.E. Evaluation of Enzyme Inhibition and Anti-Quorum Sensing Potentials of Melaleuca alternifolia and Citrus sinensis Essential Oils. Nat. Prod. Commun. 2021, 16, 1934578X211044565. [Google Scholar] [CrossRef]
- Altun, M.; Yapici, B.M. Determination of Chemical Compositions and Antibacterial Effects of Selected Essential Oils against Human Pathogenic Strains. An. Acad. Bras. Cienc. 2022, 94, e20210074. [Google Scholar] [CrossRef]
- Leigh-de Rapper, S.; Viljoen, A.; van Vuuren, S. Essential Oil Blends: The Potential of Combined Use for Respiratory Tract Infections. Antibiotics 2021, 10, 1517. [Google Scholar] [CrossRef]
- Abdelhamed, F.M.; Abdeltawab, N.F.; ElRakaiby, M.T.; Shamma, R.N.; Moneib, N.A. Antibacterial and Anti-Inflammatory Activities of Thymus vulgaris Essential Oil Nanoemulsion on Acne Vulgaris. Microorganisms 2022, 10, 1874. [Google Scholar] [CrossRef]
- Esmael, A.; Hassan, M.G.; Amer, M.M.; Abdelrahman, S.; Hamed, A.M.; Abd-raboh, H.A.; Foda, M.F. Antimicrobial Activity of Certain Natural-Based Plant Oils against the Antibiotic-Resistant Acne Bacteria. Saudi J. Biol. Sci. 2020, 27, 448–455. [Google Scholar] [CrossRef] [PubMed]
- Homeyer, D.C.; Sanchez, C.J.; Mende, K.; Beckius, M.L.; Murray, C.K.; Wenke, J.C.; Akers, K.S. In Vitro Activity of Melaleuca alternifolia (Tea Tree) Oil on Filamentous Fungi and Toxicity to Human Cells. Med. Mycol. 2015, 53, 285–294. [Google Scholar] [CrossRef] [PubMed]
- Villar Rodríguez, J.; Pérez-Pico, A.M.; Mingorance-Álvarez, E.; Mayordomo Acevedo, R. Meta-Analysis of the Antifungal Activities of Three Essential Oils as Alternative Therapies in Dermatophytosis Infections. J. Appl. Microbiol. 2022, 133, 241–253. [Google Scholar] [CrossRef]
- Pormohammad, A.; Hansen, D.; Turner, R.J. Antibacterial, Antibiofilm, and Antioxidant Activity of 15 Different Plant-Based Natural Compounds in Comparison with Ciprofloxacin and Gentamicin. Antibiotics 2022, 11, 1099. [Google Scholar] [CrossRef]
- Carson, C.F.; Riley, T.V.; Cookson, B.D. Efficacy and Safety of Tea Tree Oil as a Topical Antimicrobial Agent. J. Hosp. Infect. 1998, 40, 175–178. [Google Scholar] [CrossRef] [PubMed]
- Minghetti, P.; Casiraghi, A.; Cilurzo, F.; Gambaro, V.; Montanari, L. Formulation Study of Tea Tree Oil Patches. Nat. Prod. Commun. 2009, 4, 133–137. [Google Scholar] [CrossRef]
- Muta, T.; Parikh, A.; Kathawala, K.; Haidari, H.; Song, Y.; Thomas, J.; Garg, S. Quality-by-Design Approach for the Development of Nano-Sized Tea Tree Oil Formulation-Impregnated Biocompatible Gel with Antimicrobial Properties. Pharmaceutics 2020, 12, 1091. [Google Scholar] [CrossRef]
- Low, W.L.; Kenward, K.; Cairul, M.; Amin, I.M.; Martin, C.; Nahar, L.; Basar, N.; Sarker, S.D.; Adams, J.D. Ionically Crosslinked Chitosan Hydrogels for the Controlled Release of Antimicrobial Essential Oils and Metal Ions for Wound Management Applications. Medicines 2016, 3, 8. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Cid, P.; Jiménez-Rosado, M.; Romero, A.; Pérz-Puyana, V. Novel Trends in Hydrogel Development for Biomedical Applications: A Review. Polymers 2022, 14, 3023. [Google Scholar] [CrossRef]
- Ghosh, B.; Bhattacharya, D.; Mukhopadhyay, M. A Hydrogel Sheet Mask with Tea Tree Essential Oil Entrapment and Targeted Dose Delivery Capability. Mater. Today Proc. 2022, 57, 77–83. [Google Scholar] [CrossRef]
- Catanzano, O.; Straccia, M.C.; Miro, A.; Ungaro, F.; Romano, I.; Mazzarella, G.; Santagata, G.; Quaglia, F.; Laurienzo, P.; Malinconico, M. Spray-by-Spray in Situ Cross-Linking Alginate Hydrogels Delivering a Tea Tree Oil Microemulsion. Eur. J. Pharm. Sci. 2015, 66, 20–28. [Google Scholar] [CrossRef] [PubMed]
- Sinha, P.; Srivastava, S.; Mishra, N.; Singh, D.K.; Luqman, S.; Chanda, D.; Yadav, N.P. Development, Optimization, and Characterization of a Novel Tea Tree Oil Nanogel Using Response Surface Methodology. Drug Dev. Ind. Pharm. 2016, 42, 1434–1445. [Google Scholar] [CrossRef]
- de Assis, K.M.A.; da Silva Leite, J.M.; de Melo, D.F.; Borges, J.C.; Santana, L.M.B.; dos Reis, M.M.L.; Moreira, V.M.; da Rocha, W.R.V.; Catão, R.M.R.; dos Santos, S.G.; et al. Bicontinuous Microemulsions Containing Melaleuca alternifolia Essential Oil as a Therapeutic Agent for Cutaneous Wound Healing. Drug Deliv. Transl. Res. 2020, 10, 1748–1763. [Google Scholar] [CrossRef] [PubMed]
- Bao, X.; Wu, J.; Ma, G. Sprayed Pickering Emulsion with High Antibacterial Activity for Wound Healing. Prog. Nat. Sci. Mater. Int. 2020, 30, 669–676. [Google Scholar] [CrossRef]
- Liu, P.; Chen, G.; Zhang, J. A Review of Liposomes as a Drug Delivery System: Current Status of Approved Products, Regulatory Environments, and Future Perspectives. Molecules 2022, 27, 1372. [Google Scholar] [CrossRef]
- Low, W.L.; Martin, C.; Hill, D.J.; Kenward, M.A. Antimicrobial Efficacy of Liposome-Encapsulated Silver Ions and Tea Tree Oil against Pseudomonas aeruginosa, Staphylococcus aureus and Candida albicans. Lett. Appl. Microbiol. 2013, 57, 33–39. [Google Scholar] [CrossRef]
- Aguilar-Pérez, K.M.; Medina, D.I.; Parra-Saldívar, R.; Iqbal, H.M.N. Nano-Size Characterization and Antifungal Evaluation of Essential Oil Molecules-Loaded Nanoliposomes. Molecules 2022, 27, 5728. [Google Scholar] [CrossRef]
- Ge, Y.; Ge, M. Distribution of Melaleuca alternifolia Essential Oil in Liposomes with Tween 80 Addition and Enhancement of in Vitro Antimicrobial Effect. J. Exp. Nanosci. 2015, 11, 345–358. [Google Scholar] [CrossRef]
- Ge, Y.; Tang, J.; Fu, H.; Fu, Y.; Wu, Y. Characteristics, Controlled-Release and Antimicrobial Properties of Tea Tree Oil Liposomes-Incorporated Chitosan-Based Electrospun Nanofiber Mats. Fibers Polym. 2019, 20, 698–708. [Google Scholar] [CrossRef]
- Esposito, E.; Calderan, L.; Galvan, A.; Cappellozza, E.; Drechsler, M.; Mariani, P.; Pepe, A.; Sguizzato, M.; Vigato, E.; Pozza, E.D.; et al. Ex Vivo Evaluation of Ethosomes and Transethosomes Applied on Human Skin: A Comparative Study. Int. J. Mol. Sci. 2022, 23, 15112. [Google Scholar] [CrossRef]
- Bisht, A.; Hemrajani, C.; Upadhyay, N.; Nidhi, P.; Rolta, R.; Rathore, C.; Gupta, G.; Dua, K.; Chellappan, D.K.; Dev, K.; et al. Azelaic Acid and Melaleuca alternifolia Essential Oil Co-Loaded Vesicular Carrier for Combinational Therapy of Acne. Ther. Deliv. 2022, 13, 13–29. [Google Scholar] [CrossRef]
- da Silva, N.P.; Pereira, E.D.C.R.L.; Duarte, L.M.; de Oliveira Freitas, J.C.; de Almeida, C.G.; da Silva, T.P.; de Melo, R.C.N.; Morais Apolônio, A.C.; de Oliveira, M.A.L.; de Mello Brandão, H.; et al. Improved Anti-Cutibacterium acnes Activity of Tea Tree Oil-Loaded Chitosan-Poly(ε-Caprolactone) Core-Shell Nanocapsules. Colloids Surf. B Biointerfaces 2020, 196, 111371. [Google Scholar] [CrossRef]
- Youn, B.H.; Kim, Y.S.; Yoo, S.; Hur, M.H. Antimicrobial and Hand Hygiene Effects of Tea Tree Essential Oil Disinfectant: A Randomised Control Trial. Int. J. Clin. Pract. 2021, 75, e14206. [Google Scholar] [CrossRef]
- Messager, S.; Hammer, K.A.; Carson, C.F.; Riley, T.V. Assessment of the Antibacterial Activity of Tea Tree Oil Using the European EN 1276 and EN 12054 Standard Suspension Tests. J. Hosp. Infect. 2005, 59, 113–125. [Google Scholar] [CrossRef]
- Filatov, V.A.; Kulyak, O.Y.; Kalenikova, E.I. In Vitro and in Vivo Antimicrobial Activity of an Active Plant-Based Quadrocomplex for Skin Hygiene. J. Pharm. Pharmacogn. Res. 2022, 10, 905–921. [Google Scholar] [CrossRef]
- Kunicka-Styczyńska, A.; Sikora, M.; Kalemba, D. Lavender, Tea Tree and Lemon Oils as Antimicrobials in Washing Liquids and Soft Body Balms. Int. J. Cosmet. Sci. 2011, 33, 53–61. [Google Scholar] [CrossRef] [PubMed]
- Gnatta, J.R.; de Brito Poveda, V.; Padoveze, M.C.; Graziano, K.U.; Turrini, R.N.T.; da Silva, M.J.P. Melaleuca alternifolia Essential Oil Soap: A Potential Alternative for Hand Hygiene. Eur. J. Clin. Microbiol. Infect. Dis. 2021, 40, 1517–1520. [Google Scholar] [CrossRef] [PubMed]
- Sgorbini, B.; Cagliero, C.; Argenziano, M.; Cavalli, R.; Bicchi, C.; Rubiolo, P. In Vitro Release and Permeation Kinetics of Melaleuca alternifolia (Tea Tree) Essential Oil Bioactive Compounds from Topical Formulations. Flavour Fragr. J. 2017, 32, 354–361. [Google Scholar] [CrossRef]
- Del Prado-Audelo, M.L.; Cortés, H.; Caballero-Florán, I.H.; González-Torres, M.; Escutia-Guadarrama, L.; Bernal-Chávez, S.A.; Giraldo-Gomez, D.M.; Magaña, J.J.; Leyva-Gómez, G. Therapeutic Applications of Terpenes on Inflammatory Diseases. Front. Pharmacol. 2021, 12, 2114. [Google Scholar] [CrossRef] [PubMed]
- Miguel, M.G. Antioxidant and Anti-Inflammatory Activities of Essential Oils: A Short Review. Molecules 2010, 15, 9252–9287. [Google Scholar] [CrossRef] [PubMed]
- Mias, C.; Mengeaud, V.; Bessou-Touya, S.; Duplan, H. Recent Advances in Understanding Inflammatory Acne: Deciphering the Relationship between Cutibacterium acnes and Th17 Inflammatory Pathway. J. Eur. Acad. Dermatol. Venereol. 2023, 37 (Suppl. 2), 3–11. [Google Scholar] [CrossRef]
- Ge, Y.; Huang, M.; Yao, Y.M. Biology of Interleukin-17 and Its Pathophysiological Significance in Sepsis. Front. Immunol. 2020, 11, 1558. [Google Scholar] [CrossRef] [PubMed]
- Rai, V.K.; Sinha, P.; Yadav, K.S.; Shukla, A.; Saxena, A.; Bawankule, D.U.; Tandon, S.; Khan, F.; Chanotiya, C.S.; Yadav, N.P. Anti-Psoriatic Effect of Lavandula angustifolia Essential Oil and Its Major Components Linalool and Linalyl Acetate. J. Ethnopharmacol. 2020, 261, 113127. [Google Scholar] [CrossRef] [PubMed]
- Xu, Y.; Shi, Y.; Huang, J.; Gu, H.; Li, C.; Zhang, L.; Liu, G.; Zhou, W.; Du, Z. The Essential Oil Derived from Perilla frutescens (L.) Britt. Attenuates Imiquimod-Induced Psoriasis-like Skin Lesions in BALB/c Mice. Molecules 2022, 27, 2996. [Google Scholar] [CrossRef]
- Pazyar, N.; Yaghoobi, R.; Bagherani, N.; Kazerouni, A. A Review of Applications of Tea Tree Oil in Dermatology. Int. J. Dermatol. 2013, 52, 784–790. [Google Scholar] [CrossRef]
- Kanlayavattanakul, M.; Lourith, N. Therapeutic Agents and Herbs in Topical Application for Acne Treatment. Int. J. Cosmet. Sci. 2011, 33, 289–297. [Google Scholar] [CrossRef]
- Low, P.; Clark, A.M.; Chou, T.C.; Chang, T.C.; Reynolds, M.; Ralph, S.J. Immunomodulatory Activity of Melaleuca alternifolia Concentrate (MAC): Inhibition of LPS-Induced NF-ΚB Activation and Cytokine Production in Myeloid Cell Lines. Int. Immunopharmacol. 2015, 26, 257–264. [Google Scholar] [CrossRef]
- Hart, P.H.; Brand, C.; Carson, C.F.; Riley, T.V.; Prager, R.H.; Finlay-Jones, J.J. Terpinen-4-Ol, the Main Component of the Essential Oil of Melaleuca alternifolia (Tea Tree Oil), Suppresses Inflammatory Mediator Production by Activated Human Monocytes. Inflamm. Res. 2000, 49, 619–626. [Google Scholar] [CrossRef]
- Nogueira, M.N.M.; Aquino, S.G.; Rossa, C.; Spolidorio, D.M.P. Terpinen-4-Ol and Alpha-Terpineol (Tea Tree Oil Components) Inhibit the Production of IL-1β, IL-6 and IL-10 on Human Macrophages. Inflamm. Res. 2014, 63, 769–778. [Google Scholar] [CrossRef] [PubMed]
- Ning, J.; Xu, L.; Zhao, Q.; Zhang, Y.Y.; Shen, C. qing The Protective Effects of Terpinen-4-Ol on LPS-Induced Acute Lung Injury via Activating PPAR-γ. Inflammation 2018, 41, 2012–2017. [Google Scholar] [CrossRef] [PubMed]
- Baldissera, M.D.; Da Silva, A.S.; Oliveira, C.B.; Vaucher, R.A.; Santos, R.C.V.; Duarte, T.; Duarte, M.M.M.F.; França, R.T.; Lopes, S.T.A.; Raffin, R.P.; et al. Effect of Tea Tree Oil (Melaleuca alternifolia) on the Longevity and Immune Response of Rats Infected by Trypanosoma evansi. Res. Vet. Sci. 2014, 96, 501–506. [Google Scholar] [CrossRef] [PubMed]
- Baldissera, M.D.; Souza, C.F.; Doleski, P.H.; de Vargas, A.C.; Duarte, M.M.M.F.; Duarte, T.; Boligon, A.A.; Leal, D.B.R.; Baldisserotto, B. Melaleuca alternifolia Essential Oil Prevents Alterations to Purinergic Enzymes and Ameliorates the Innate Immune Response in Silver Catfish Infected with Aeromonas hydrophila. Microb. Pathog. 2017, 109, 61–66. [Google Scholar] [CrossRef]
- Liu, M.; Sun, C.; Xu, P.; Liu, B.; Zheng, X.; Liu, B.; Zhou, Q. Effects of Dietary Tea Tree (Melaleuca alternifolia) Oil and Feeding Patterns on the Zootechnical Performance and Nonspecific Immune Response of the Giant Freshwater Prawn (Macrobrachium rosenbergii). J. World Aquac. Soc. 2022, 53, 542–557. [Google Scholar] [CrossRef]
- Mohyuddin, S.G.; Qamar, A.; Hu, C.-Y.; Li, Y.; Chen, S.W.; Wen, J.-Y.; Bao, M.L.; Ju, X.H. Terpinen4-Ol Inhibits Heat Stress Induced Inflammation in Colonic Tissue by Activating Occludin, Claudin-2 and TLR4/NF-ΚB Signaling Pathway. Int. Immunopharmacol. 2021, 99, 107727. [Google Scholar] [CrossRef]
- Ergun, S.B.; Saribas, G.S.; Yarayici, S.; Elmazoglu, Z.; Cardak, A.; Ozogul, C.; Ilhan, M.N.; Karasu, C.; Evren Kemer, O. Comparison of Efficacy and Safety of Two Tea Tree Oil-Based Formulations in Patients with Chronic Blepharitis: A Double-Blinded Randomized Clinical Trial. Ocul. Immunol. Inflamm. 2020, 28, 888–897. [Google Scholar] [CrossRef]
- Koh, K.J.; Pearce, A.L.; Marshman, G.; Finlay-Jones, J.J.; Hart, P.H. Tea Tree Oil Reduces Histamine-Induced Skin Inflammation. Br. J. Dermatol. 2002, 147, 1212–1217. [Google Scholar] [CrossRef]
- Azab, A.E.; Adwas, A.A.; Elsayed, A.S.I.; Adwas, A.A.; Elsayed, A.S.I.; Azab, A.E.; Quwaydir, F.A. Oxidative Stress and Antioxidant Mechanisms in Human Body. J. Appl. Biotechnol. Bioeng. 2019, 6, 43–47. [Google Scholar] [CrossRef]
- Losada-Barreiro, S.; Sezgin-Bayindir, Z.; Paiva-Martins, F.; Bravo-Díaz, C. Biochemistry of Antioxidants: Mechanisms and Pharmaceutical Applications. Biomedicines 2022, 10, 3051. [Google Scholar] [CrossRef] [PubMed]
- Vo, T.V.; Truong, T.H.; Chen, B.H. Surfactant-Assisted Extraction of Melaleuca alternifolia (Tea Tree) Oil by Hydrodistillation and Its Application in Microemulsion. J. Chem. Technol. Biotechnol. 2022, 97, 3419–3429. [Google Scholar] [CrossRef]
- Liu, M.; Gao, Q.; Sun, C.; Liu, B.; Liu, X.; Zhou, Q.; Zheng, X.; Xu, P. Effects of Dietary Tea Tree Oil on the Growth, Physiological and Non-Specific Immunity Response in the Giant Freshwater Prawn (Macrobrachium rosenbergii) under High Ammonia Stress. Fish Shellfish Immunol. 2022, 120, 458–469. [Google Scholar] [CrossRef]
- Yang, T.; Feng, F.; Zhan, K.; Ma, X.; Jiang, M.; Datsomor, O.; Zhu, X.; Huo, Y.; Zhao, G. Effect of the Tea Tree Oil on Growth Performance, Meat Quality, Serum Biochemical Indices, and Antioxidant Capacity in Finishing Pigs. Front. Vet. Sci. 2022, 9, 863. [Google Scholar] [CrossRef]
- Chanjirakul, K.; Wang, S.Y.; Wang, C.Y.; Siriphanich, J. Effect of Natural Volatile Compounds on Antioxidant Capacity and Antioxidant Enzymes in Raspberries. Postharvest Biol. Technol. 2006, 40, 106–115. [Google Scholar] [CrossRef]
- Chanjirakul, K.; Wang, S.Y.; Wang, C.Y.; Siriphanich, J. Natural Volatile Treatments Increase Free-Radical Scavenging Capacity of Strawberries and Blackberries. J. Sci. Food Agric. 2007, 87, 1463–1472. [Google Scholar] [CrossRef]
- Ponce, A.G.; Del Valle, C.E.; Roura, S.I. Natural Essential Oils as Reducing Agents of Peroxidase Activity in Leafy Vegetables. LWT-Food Sci. Technol. 2004, 37, 199–204. [Google Scholar] [CrossRef]
- Ponce, A.G.; Del Valle, C.; Roura, S.I. Shelf Life of Leafy Vegetables Treated with Natural Essential Oils. J. Food Sci. 2004, 69, fms50–fms56. [Google Scholar] [CrossRef]
- Cazón, P.; Antoniewska, A.; Rutkowska, J.; Vázquez, M. Evaluation of Easy-Removing Antioxidant Films of Chitosan with Melaleuca alternifolia Essential Oil. Int. J. Biol. Macromol. 2021, 186, 365–376. [Google Scholar] [CrossRef] [PubMed]
- Abdelgawad, K.F.; Awad, A.H.R.; Ali, M.R.; Ludlow, R.A.; Chen, T.; El-Mogy, M.M. Increasing the Storability of Fresh-Cut Green Beans by Using Chitosan as a Carrier for Tea Tree and Peppermint Essential Oils and Ascorbic Acid. Plants 2022, 11, 783. [Google Scholar] [CrossRef]
- Avonto, C.; Chittiboyina, A.G.; Wang, M.; Vasquez, Y.; Rua, D.; Khan, I.A. In Chemico Evaluation of Tea Tree Essential Oils as Skin Sensitizers: Impact of the Chemical Composition on Aging and Generation of Reactive Species. Chem. Res. Toxicol. 2016, 29, 1108–1117. [Google Scholar] [CrossRef]
- Rudbäck, J.; Bergström, M.A.; Börje, A.; Nilsson, U.; Karlberg, A.T. α-Terpinene, an Antioxidant in Tea Tree Oil, Autoxidizes Rapidly to Skin Allergens on Air Exposure. Chem. Res. Toxicol. 2012, 25, 713–721. [Google Scholar] [CrossRef]
- Martiniaková, S.; Ácsová, A.; Hojerová, J.; Krepsová, Z.; Kreps, F. Ceylon Cinnamon and Clove Essential Oils as Promising Free Radical Scavengers for Skin Care Products. Acta Chim. Slovaca 2022, 15, 1–11. [Google Scholar] [CrossRef]
- Zhao, Q.; Bowles, E.J.; Zhang, H.-Y. Antioxidant Activities of Eleven Australian Essential Oils. Nat. Prod. Commun. 2008, 3, 1934578X0800300531. [Google Scholar] [CrossRef]
- Hu, L.; Zou, L.; Liu, Q.; Geng, Y.; Xu, G.; Chen, L.; Pan, P.; Chen, J. Construction of Chitosan-Based Asymmetric Antioxidant and Anti-Inflammatory Repair Film for Acceleration of Wound Healing. Int. J. Biol. Macromol. 2022, 215, 377–386. [Google Scholar] [CrossRef] [PubMed]
- Doustdar, F.; Ramezani, S.; Ghorbani, M.; Mortazavi Moghadam, F. Optimization and Characterization of a Novel Tea Tree Oil-Integrated Poly (ε-Caprolactone)/Soy Protein Isolate Electrospun Mat as a Wound Care System. Int. J. Pharm. 2022, 627, 122218. [Google Scholar] [CrossRef]
- Malik, P.; Upadhyay, P. GC-MS Chemical Profile, Antioxidant Activity, and Sun Protection Factor of Essential Oil of Tea Tree (Melaleuca alternifolia) and Rosemary (Rosmarinus officinalis L.). Orient. J. Chem. 2022, 38, 1266–1275. [Google Scholar] [CrossRef]
- Infante, H.V.; Campos, M.M.P.; Darvin, M.; Lohan, S.; Schleusener, J.; Schanzer, S.; Lademann, J.; Meinke, M. Cosmetic Formulations with Melaleuca alternifolia Essential Oil for the Improvement of Photoaged Skin: A Double-Blind, Randomized, Placebo-Controlled Clinical Study. Photochem. Photobiol. 2023, 99, 176–183. [Google Scholar] [CrossRef]
- Flores, F.C.; De Lima, J.A.; Da Silva, C.R.; Benvegnú, D.; Ferreira, J.; Burger, M.E.; Beck, R.C.R.; Rolim, C.M.B.; Rocha, M.I.U.M.; Da Veiga, M.L.; et al. Hydrogels Containing Nanocapsules and Nanoemulsions of Tea Tree Oil Provide Antiedematogenic Effect and Improved Skin Wound Healing. J. Nanosci. Nanotechnol. 2015, 15, 800–809. [Google Scholar] [CrossRef] [PubMed]
- Yadav, E.; Kumar, S.; Mahant, S.; Khatkar, S.; Rao, R. Tea Tree Oil: A Promising Essential Oil. J. Essent. Oil Res. 2016, 29, 201–213. [Google Scholar] [CrossRef]
- Halcón, L.; Milkus, K. Staphylococcus aureus and Wounds: A Review of Tea Tree Oil as a Promising Antimicrobial. Am. J. Infect. Control 2004, 32, 402–408. [Google Scholar] [CrossRef]
- Stea, S.; Beraudi, A.; de Pasquale, D. Essential Oils for Complementary Treatment of Surgical Patients: State of the Art. Evid.-Based Complement. Atern. Med. 2014, 2014, 726341. [Google Scholar] [CrossRef]
- Carson, C.F.; Riley, T.V. Safety, Efficacy and Provenance of Tea Tree (Melaleuca alternifolia) Oil. Contact Dermat. 2001, 45, 65–67. [Google Scholar] [CrossRef]
- Rutherford, T.; Nixon, R.; Tam, M.; Tate, B. Allergy to Tea Tree Oil: Retrospective Review of 41 Cases with Positive Patch Tests over 4.5 Years. Australas. J. Dermatol. 2007, 48, 83–87. [Google Scholar] [CrossRef]
- de Groot, A.C.; Schmidt, E. Tea Tree Oil: Contact Allergy and Chemical Composition. Contact Dermat. 2016, 75, 129–143. [Google Scholar] [CrossRef]
- Carson, C.F.; Riley, H.T.V. Toxicity of the Essential Oil of Melaleuca alternifolia or Tea Tree Oil. Clin. Toxicol. 1995, 33, 193–194. [Google Scholar]
- Hammer, K.A.; Carson, C.F.; Riley, T.V.; Nielsen, J.B. A Review of the Toxicity of Melaleuca alternifolia (Tea Tree) Oil. Food Chem. Toxicol. 2006, 44, 616–625. [Google Scholar] [CrossRef] [PubMed]
- Vetere, A.; Bertocchi, M.; Pelizzone, I.; Moggia, E.; Travaglino, C.; Grotta, M.D.; Casali, S.; Gerosa, S.; Strada, L.; Filia, K.; et al. Acute Tea Tree Oil Intoxication in a Pet Cockatiel (Nymphicus hollandicus): A Case Report. BMC Veter. Res. 2020, 16, 29. [Google Scholar] [CrossRef]
- Kairey, L.; Agnew, T.; Bowles, E.J.; Barkla, B.J.; Wardle, J.; Lauche, R. Efficacy and Safety of Melaleuca alternifolia (Tea Tree) Oil for Human Health—A Systematic Review of Randomized Controlled Trials. Front. Pharmacol. 2023, 14, 31. [Google Scholar] [CrossRef]
- Bassett, I.B.; Pannowitz, D.L.; Barnetson, R.S.C. A Comparative Study of Tea-Tree Oil versus Benzoylperoxide in the Treatment of Acne. Med. J. Aust. 1990, 153, 455–458. [Google Scholar] [CrossRef] [PubMed]
- Enshaieh, S.; Jooya, A.; Siadat, A.H.; Iraji, F. The Efficacy of 5% Topical Tea Tree Oil Gel in Mild to Moderate Acne Vulgaris: A Randomized, Double-Blind Placebo-Controlled Study. Indian J. Dermatol. Venereol. Leprol. 2007, 73, 22–25. [Google Scholar] [CrossRef]
- Kwon, H.H.; Yoon, J.Y.; Park, S.Y.; Min, S.; Suh, D.H. Comparison of Clinical and Histological Effects between Lactobacillus-Fermented Chamaecyparis obtusa and Tea Tree Oil for the Treatment of Acne: An Eight-Week Double-Blind Randomized Controlled Split-Face Study. Dermatology 2014, 229, 102–109. [Google Scholar] [CrossRef]
- Malhi, H.K.; Tu, J.; Riley, T.V.; Kumarasinghe, S.P.; Hammer, K.A. Tea Tree Oil Gel for Mild to Moderate Acne; a 12 Week Uncontrolled, Open-Label Phase II Pilot Study. Australas. J. Dermatol. 2017, 58, 205–210. [Google Scholar] [CrossRef] [PubMed]
- Lubtikulthum, P.; Kamanamool, N.; Udompataikul, M. A Comparative Study on the Effectiveness of Herbal Extracts vs 2.5% Benzoyl Peroxide in the Treatment of Mild to Moderate Acne Vulgaris. J. Cosmet. Dermatol. 2019, 18, 1767–1775. [Google Scholar] [CrossRef] [PubMed]
- Najafi-Taher, R.; Jafarzadeh kohneloo, A.; Eslami Farsani, V.; Mehdizade Rayeni, N.; Moghimi, H.R.; Ehsani, A.; Amani, A. A Topical Gel of Tea Tree Oil Nanoemulsion Containing Adapalene versus Adapalene Marketed Gel in Patients with Acne Vulgaris: A Randomized Clinical Trial. Arch. Dermatol. Res. 2022, 314, 673–679. [Google Scholar] [CrossRef]
- Mazzarello, V.; Donadu, M.G.; Ferrari, M.; Piga, G.; Usai, D.; Zanetti, S.; Sotgiu, M.A. Treatment of Acne with a Combination of Propolis, Tea Tree Oil, and Aloe Vera Compared to Erythromycin Cream: Two Double-Blind Investigations. Clin. Pharmacol. 2018, 10, 175–181. [Google Scholar] [CrossRef] [PubMed]
- Yadav, N.; Singh, A.; Chatterjee, A.; Belemkar, S. Evaluation of Efficacy and Safety of Perfact Face Gel and Perfact Face Tablets in Management of Acne. J. Clin. Exp. Dermatol. 2011, 2, 1000118. [Google Scholar] [CrossRef]
- Kim, B.Y.; Shin, S. Antimicrobial and Improvement Effects of Tea Tree and Lavender Oils on Acne Lesions. J. Converg. Inf. Technol. 2013, 8, 339–345. [Google Scholar]
- Lupu, M.; Malciu, A.M.; Voiculescu, V.M. Feasibility of Reflectance Confocal Microscopy Monitoring in Oily, Acne-Prone Facial Skin Treated with a Topical Combination of Alpha and Beta-Hydroxy Acids, Anti-Inflammatory Molecules, and Herculane Thermal Water: A Blinded, One-Month Study. Life 2022, 12, 1973. [Google Scholar] [CrossRef]
- Sagransky, M.; Yentzer, B.A.; Feldman, S.R. Benzoyl Peroxide: A Review of Its Current Use in the Treatment of Acne Vulgaris. Expert. Opin. Pharmacother. 2009, 10, 2555–2562. [Google Scholar] [CrossRef]
- Piskin, S.; Uzunali, E. A Review of the Use of Adapalene for the Treatment of Acne Vulgaris. Ther. Clin. Risk Manag. 2007, 3, 621–624. [Google Scholar]
- Baby, A.R.; Freire, T.B.; Marques, G.D.A.; Rijo, P.; Lima, F.V.; de Carvalho, J.C.M.; Rojas, J.; Magalhães, W.V.; Velasco, M.V.R.; Morocho-Jácome, A.L. Azadirachta indica (Neem) as a Potential Natural Active for Dermocosmetic and Topical Products: A Narrative Review. Cosmetics 2022, 9, 58. [Google Scholar] [CrossRef]
- Vaughn, A.R.; Branum, A.; Sivamani, R.K. Effects of Turmeric (Curcuma longa) on Skin Health: A Systematic Review of the Clinical Evidence. Phytother. Res. 2016, 30, 1243–1264. [Google Scholar] [CrossRef] [PubMed]
- Rajaiah Yogesh, H.; Gajjar, T.; Patel, N.; Kumawat, R. Clinical Study to Assess Efficacy and Safety of Purifying Neem Face Wash in Prevention and Reduction of Acne in Healthy Adults. J. Cosmet. Dermatol. 2022, 21, 2849–2858. [Google Scholar] [CrossRef] [PubMed]
- Desai, S. Anti-Acne Activity of Piper Nigrum Fruit Extract. J. Pharm. Sci. Biosci. Res. 2015, 5, 609–612. [Google Scholar]
- Din, M.S.U.; Gohar, U.F.; Hameed, U.; Mukhtar, H.; Morar, A.; Herman, V.; Imre, K. Piper Nigrum Fruit Extract as an Antibiotic Resistance Reversal Agent in MDR Bacteria. Appl. Sci. 2022, 12, 12542. [Google Scholar] [CrossRef]
- Wells, R.; Truong, F.; Adal, A.M.; Sarker, L.S.; Mahmoud, S.S. Lavandula Essential Oils: A Current Review of Applications in Medicinal, Food, and Cosmetic Industries of Lavender. Nat. Prod. Commun. 2018, 13, 1403–1417. [Google Scholar] [CrossRef]
- Kelvin; Wijayadi, L.J. The Role of Herbal Plant Essential Oils in the Treatment of Acne Vulgaris. Sci. Midwifery 2022, 10, 3096–3103. [Google Scholar] [CrossRef]
- Batiha, G.E.S.; Teibo, J.O.; Wasef, L.; Shaheen, H.M.; Akomolafe, A.P.; Teibo, T.K.A.; Al-kuraishy, H.M.; Al-Garbeeb, A.I.; Alexiou, A.; Papadakis, M. A Review of the Bioactive Components and Pharmacological Properties of Lavandula Species. Naunyn-Schmiedeberg’s Arch. Pharmacol. 2023, 396, 877–900. [Google Scholar] [CrossRef]
- Valero Da Silva, M.; Gomes De Moura, N.; Motoyama, A.B.; Ferreira, V.M. A Review of the Potential Therapeutic and Cosmetic Use of Propolis in Topical Formulations. J. Appl. Pharm. Sci. 2019, 10, 131–141. [Google Scholar] [CrossRef]
- Almuhayawi, M.S. Propolis as a Novel Antibacterial Agent. Saudi J. Biol. Sci. 2020, 27, 3079–3086. [Google Scholar] [CrossRef]
- Arung, E.T.; Syafrizal; Kusuma, I.W.; Paramita, S.; Amen, Y.; Kim, Y.U.; Naibaho, N.M.; Ramadhan, R.; Ariyanta, H.A.; Fatriasari, W.; et al. Antioxidant, Anti-Inflammatory and Anti-Acne Activities of Stingless Bee (Tetragonula biroi) Propolis. Fitoterapia 2023, 164, 105375. [Google Scholar] [CrossRef] [PubMed]
- Zhong, H.; Li, X.; Zhang, W.; Shen, X.; Lu, Y.; Li, H. Efficacy of a New Non-Drug Acne Therapy: Aloe Vera Gel Combined With Ultrasound and Soft Mask for the Treatment of Mild to Severe Facial Acne. Front. Med. 2021, 8, 662640. [Google Scholar] [CrossRef] [PubMed]
- Surjushe, A.; Vasani, R.; Saple, D. Aloe vera: A Short Review. Indian J. Dermatol. 2008, 53, 163. [Google Scholar] [CrossRef] [PubMed]
- Orafidiya, L.O.; Agbani, E.O.; Oyedele, A.O.; Babalola, O.O.; Onayemi, O.; Aiyedun, F.F. The Effect of Aloe Vera Gel on the Anti-Acne Properties of the Essential Oil of Ocimum gratissimum Linn Leaf—A Preliminary Clinical Investigation. Int. J. Aromather. 2004, 14, 15–21. [Google Scholar] [CrossRef]
- Zagórska-Dziok, M.; Furman-Toczek, D.; Dudra-Jastrzębska, M.; Zygo, K.; Stanisławek, A.; Kapka-Skrzypczak, L. Evaluation of Clinical Effectiveness of Aloe vera—A Review. J. Pre-Clin. Clin. Res. 2017, 11, 86–93. [Google Scholar] [CrossRef]
- Waranuch, N.; Phimnuan, P.; Yakaew, S.; Nakyai, W.; Grandmottet, F.; Onlom, C.; Srivilai, J.; Viyoch, J. Antiacne and Antiblotch Activities of a Formulated Combination of Aloe barbadensis Leaf Powder, Garcinia mangostana Peel Extract, and Camellia sinensis Leaf Extract. Clin. Cosmet. Investig. Dermatol. 2019, 12, 383–391. [Google Scholar] [CrossRef]
- Lueangarun, S.; Sriviriyakul, K.; Tempark, T.; Managit, C.; Sithisarn, P. Clinical Efficacy of 0.5% Topical Mangosteen Extract in Nanoparticle Loaded Gel in Treatment of Mild-to-Moderate Acne Vulgaris: A 12-Week, Split-Face, Double-Blinded, Randomized, Controlled Trial. J. Cosmet. Dermatol. 2019, 18, 1395–1403. [Google Scholar] [CrossRef]
- Natasha, J.; Ng, C.; Vinna, M.; Crisostomo, N.; Stephanie, M.; Jimenez, L.; Jo, M.; Bunagan, K.S. A Randomized, Comparative Study on the Efficacy and Safety of Mangosteen 1% Extract Gel versus Benzoyl Peroxide 5% Gel in the Treatment of Mild to Moderate Acne Vulgaris. J. Philipp. Dermatol. Soc. 2021, 30, 15–23. [Google Scholar]
- Phumlek, K.; Itharat, A.; Pongcharoen, P.; Chakkavittumrong, P.; Lee, H.Y.; Moon, G.S.; Han, M.H.; Panthong, S.; Ketjinda, W.; Davies, N.M. Garcinia Mangostana Hydrogel Patch: Bactericidal Activity and Clinical Safety for Acne Vulgaris Treatment. Res. Pharm. Sci. 2022, 17, 457. [Google Scholar] [CrossRef]
- Budiman, A.; Praditasari, A.; Rahayu, D.; Aulifa, D.L. Formulation of Antioxidant Gel from Black Mulberry Fruit Extract (Morus Nigra L.). J. Pharm. Bioallied Sci. 2019, 11, 216–222. [Google Scholar] [CrossRef] [PubMed]
- Nangare, S.; Bhatane, D.; Mali, R.; Shitole, M. Development of a Novel Freeze-Dried Mulberry Leaf Extract-Based Transfersome Gel. Turk. J. Pharm. Sci. 2021, 18, 44–55. [Google Scholar] [CrossRef]
- Nguyen, L.T.H. Biological Activities of Paper Mulberry (Broussonetia papyrifera): More than a Skin-Lightening Agent. Cosmetics 2022, 9, 112. [Google Scholar] [CrossRef]
- Solabia Group. Physio-Seboregulator Zincidone; Solabia Group: Pantin, France, 2008. [Google Scholar]
- Solabia Group. ZINCIDONE®-Antibacterial Sebum Regulator; Solabia Group: Pantin, France, 2020. [Google Scholar]
- Abendrot, M.; Kalinowska-Lis, U. Zinc-Containing Compounds for Personal Care Applications. Int. J. Cosmet. Sci. 2018, 40, 319–327. [Google Scholar] [CrossRef]
- Andrade, J.P.; Wagemaker, T.A.L.; Mercurio, D.G.; Maia Campos, P.M.B.G. Benefits of a Dermocosmetic Formulation with Vitamins B3 and a B6 Derivative Combined with Zinc-PCA for Mild Inflammatory Acne and Acne-Prone Skin. J. Biomed. Biopharm. Res. 2018, 15, 214–223. [Google Scholar] [CrossRef]
- Abendrot, M.; Płuciennik, E.; Felczak, A.; Zawadzka, K.; Piątczak, E.; Nowaczyk, P.; Kalinowska-Lis, U. Zinc(II) Complexes of Amino Acids as New Active Ingredients for Anti-Acne Dermatological Preparations. Int. J. Mol. Sci. 2021, 22, 1641. [Google Scholar] [CrossRef]
- Smith, W.P. Epidermal and Dermal Effects of Topical Lactic Acid. J. Am. Acad. Dermatol. 1996, 35, 388–391. [Google Scholar] [CrossRef]
- Garg, T.; Ramam, M.; Pasricha, J.; Verma, K. Long Term Topical Application of Lactic Acid/Lactate Lotion as a Preventive Treatment for Acne Vulgaris. Indian J. Dermatol. Venereol. Leprol. 2002, 68, 137. [Google Scholar]
- Mills, O.; Adler, D.; Verdicchio, R. Pharmacology of Salicylic Acid (SA) in Acne Vulgaris. J. Am. Acad. Dermatol. 2007, 56, AB22. [Google Scholar] [CrossRef]
- Dall’Oglio, F.; Schi, A.T.; Fusto, C.M.; Lacarrubba, F.; Dinotta, F.; Micali, G. A Novel Cosmetic Antifungal/Anti-Inflammatory Topical Gel for the Treatment of Mild to Moderate Seborrheic Dermatitis of the Face: An Open-Label Trial Utilizing Clinical Evaluation and Erythema-Directed Digital Photography. G. Ital. Dermatol. Venereol. 2017, 152, 436–440. [Google Scholar] [CrossRef]
- Piquero-Casals, J.; Hexsel, D.; Mir-Bonafé, J.F.; Rozas-Muñoz, E. Topical Non-Pharmacological Treatment for Facial Seborrheic Dermatitis. Dermatol. Ther. 2019, 9, 469–477. [Google Scholar] [CrossRef]
- Li, W.; Yu, Q.; Shen, Z.; Zhang, L.; Zhang, W.; Li, C. Efficacy and Safety of a Cream Containing Octyl Salicylic Acid, Salicylic Acid, Linoleic Acid, Nicotinamide, and Piroctone Olamine Combined with 5% Benzoyl Peroxide in the Treatment of Acne Vulgaris: A Randomized Controlled Study. Chin. Med. J. 2022, 135, 1381–1382. [Google Scholar] [CrossRef] [PubMed]
- Lucca, A.J.D.; Pauli, A.; Schilcher, H.; Sien, T.; Bhatnagar, D.; Walsh, T.J. Fungicidal and Bactericidal Properties of Bisabolol and Dragosantol. J. Essent. Oil Res. 2011, 23, 47–54. [Google Scholar] [CrossRef]
- Maurya, A.; Singh, M.; Dubey, V.; Srivastava, S.; Luqman, S.; Bawankule, D. α-(-)-Bisabolol Reduces pro-Inflammatory Cytokine Production and Ameliorates Skin Inflammation. Curr. Pharm. Biotechnol. 2014, 15, 173–181. [Google Scholar] [CrossRef] [PubMed]
- Kılıç, S.; Okullu, S.Ö.; Kurt, Ö.; Sevinç, H.; Dündar, C.; Altınordu, F.; Türkoğlu, M. Efficacy of Two Plant Extracts against Acne Vulgaris: Initial Results of Microbiological Tests and Cell Culture Studies. J. Cosmet. Dermatol. 2019, 18, 1061–1065. [Google Scholar] [CrossRef] [PubMed]
- Cao, H.; Yang, G.; Wang, Y.; Liu, J.P.; Smith, C.A.; Luo, H.; Liu, Y. Complementary Therapies for Acne Vulgaris. Cochrane Database of Syst. Rev. 2015, 2017, CD009436. [Google Scholar] [CrossRef]
- European Medicines Agency. European Union Herbal Monograph on Melaleuca alternifolia (Maiden and Betch) Cheel, M. linariifolia Smith, M. dissitiflora F. Mueller and/or Other Species of Melaleuca, aetheroleum; EMA/HMPC/320930/2012; European Medicines Agency: Amsterdam, The Netherlands, 2015. [Google Scholar]


| Main Components, Percentage (>5%) | Microorganism | Diameters of Inhibition Zones (mm) | Minimal Bactericidal Concentration (MBC) TTO | Minimal Inhibitory Concentration (MIC) TTO | Biofilm Reduction (R) or Inhibition (I) (Concentration) | Reference |
|---|---|---|---|---|---|---|
| Terpinen-4-ol, 42 Terpinen-4-ol standard | Legionella pneumophila | - | 0.25–0.5% (v/v) | 0.06–0.125% (v/v) | - | [59] |
| β-Pinene, 9 β-Terpineol, 6 Terpinen-4-ol, 10 α-Terpineol, 20 | Planktonic Enterococcus faecalis E. faecalis biofilm inhibition | - | 0.5% | 0.25% | ≥0.25% (I) | [60] |
| α-Terpinene, 9 γ-Terpinene, 20 Terpinen-4-ol, 43 | Escherichia coli 22BT E. coli 45DT Enterococcus faecium A29 E. faecalis VAN3 Staphylococcus aureus C3 S. aureus O | - | - | 128 μg/mL 1 μg/mL 1 μg/mL 64 μg/mL 8 μg/mL 8 μg/mL | 128 μg/mL (R) 1 μg/mL (R) 1 μg/mL (R) 64 μg/mL (R) 8 μg/mL (R) 8 μg/mL (R) | [61] |
| α-Terpinene, 11 γ-Terpinene, 19 Terpinen-4-ol, 33 | 14 Clinical and 2 references S. aureus strains | Liquid 8–30 Volatile 0–15 | - | Liquid 0.1–0.8% (v/v) Liquid (biofilm) | Liquid (biofilm) 0.8–6.3% (v/v) (minimal biofilm eradication) | [62] |
| Area by standard GC-MS α-Pinene, 12 1,8-Cineole, 15 γ-Terpinene, 10 o-Cymene, 6 Terpinen-4-ol, 35 Area by Head Space GC-MS α-Pinene, 23 1,8-Cineole, 17 γ-Terpinene, 11 o-Cymene, 9 Terpinen-4-ol, 29 | Methicillin-susceptibility Staphylococcus aureus Methicillin-resistant Staphylococcus aureus Escherichia coli Extended Spectrum Beta-Lactamases Carbapenem-Susceptible Kp Extended Spectrum Beta-Lactamases Carbapenem-Resistant Acinetobacter baumannii Pseudomonas aeruginosa Methicillin-susceptibility Staphylococcus aureus + oxacillin Methicillin-resistant Staphylococcus aureus + oxacillin | 2% (v/v) 2% (v/v) 0.25 0.50 0.25 0.25 1 | 1% (v/v) 0.50% (v/v) 0.25% (v/v) 0.50% (v/v) 0.25% (v/v) 0.25% (v/v) 1% (v/v) Fractional inhibitory concentration index 0.32 (synergism) 0.32 (synergism) | [63] | ||
| Terpinen-4-ol, 40 γ-Terpinene, 12 1,8-Cineole, 7 p-Cymene, 6 | Bacillus subtilis Enterococcus faecalis Micrococcus luteus Staphylococcus aureus Pseudomonas aeruginosa Yersinia enterocolitica Salmonella enterica Serratia marcescens Pseudomonas fluorescens (biofilm) Salmonella enterica (biofilm) Candida albicans C. glabrata C. krusei C. tropicalis | 9.33 10.67 7.67 7.33 6.00 6.00 7.33 6.67 6.00 6.00 10.67 7.67 6.33 8.33 | MIC 90 (μL/mL) 18.36 18.45 18.68 14.26 12.32 15.46 16.36 16.24 28.59 25.43 26.76 29.85 26.32 27.46 | [64] | ||
| Terpinen-4-ol, 36 | Staphylococcus aureus Coliform bacilli Proteus spp. Klebsiella spp. Escherichia coli Citrobacter spp. Enterobacter spp. E. coli (NCTC 11560) Fecal streptococci Fecal streptococci β-Hemolytic streptococci GP.2 Enterococcus faecalis (ATC29212) β-Hemolytic streptococci Streptococcus pyogenes Coagulase-negative staphylococci MRSA Staphylococcus aureus (NCTC 6571) Candida spp. P. aeruginosa P. aeruginosa (NCTC10662) | 1 2 4 2 2 2 4 4 4 >8 >8 >8 >8 1–4 4 4 2 1 1–5 >8 | 0.5 1–2 2 1 1 1 2 2 2 >8 >8 8 >8 0.5–2 2 2–4 2 2 0.5 2–6 8 | [65] | ||
| Without a chemical profile, only with the following information: TTO complied with the ISO 4730 and European Pharmacopoeia standards | Twenty-seven clinical isolates of S. aureus and the reference strain S. aureus NCTC 8325-4 | 0.25–1% (v/v) 0.5% (v/v) | 0.125–0.5% (v/v) 0.5% (v/v) | 2% (v/v) 1% (v/v) | [66] | |
| TTO (enterprise 1) TTO (enterprise 2) Terpinen-4-ol (racemic) L-Terpinen-4-ol TTO (enterprise 1) TTO (enterprise 2) Terpinen-4-ol (racemic) L-Terpinen-4-ol | Thirty MRSA isolates Twenty-eight CoNS isolates | 1–8% (v/v) 1->8% (v/v) 0.125–1% (v/v) 0.125–1% (v/v) 0.5–2% (v/v) 0.5–2% (v/v) 0.25–0.5% (v/v) 0.25–0.5% (v/v) | 0.125–1% (v/v) 0.125–1% (v/v) 0.0625–0.5 (v/v) 0.0625–0.5 (v/v) 0.25–0.5% (v/v) 0.125–0.5% (v/v) 0.0625–0.25% (v/v) 0.0625–0.25% (v/v) | [67] | ||
| Terpinen-4-ol, 40 α-Terpinene, 9 γ-Terpinene, 21 | Staphylococcus aureus Escherichia coli Candida albicans | 1 mg/mL (16.57) 0.5 mg/mL (15.54) 0.01 mg/mL (11.08) 1 mg/mL (16.75) 0.5 mg/mL (15.13) 0.01 mg/mL (9.87) 0.01 mg/mL (12.21) | [68] | |||
| Terpinen-4-ol, 44 γ-Terpinene, 22 α-Terpinene, 7 α-Terpineol, 6 | C. albicans Trichophyton mentagrophytes S. aureus S. epidermidis Streptococcus pyogenes MRSA Klebsiella pneumoniae P. aeruginosa C. albicans Trichophyton mentagrophytes S. aureus S. epidermidis Streptococcus pyogenes MRSA Klebsiella pneumoniae P. aeruginosa | TTO 20.3 21.1 19.2 21.7 19.2 19.5 18.1 13.2 AgNO3 17.7 19.2 18.2 19.2 22.4 17.6 24.2 15.3 | [69] | |||
| Not determined | Bacteroides Prevotella Fusobacterium Peptostreptococcus anaerobius Other gram-positive anaerobic cocci | 0.03–0.5% (v/v) 0.03–0.25% (v/v) 0.06–0.55% (v/v) 0.06–0.25% (v/v) 0.03–0.25% (v/v) | [70] | |||
| Three batches Terpinen-4-ol, 41–44 α-Terpinene, 10–11 γ-Terpinene, 21–23 | Cutibacterium acnes | 0.25% (v/v) | [71] | |||
| Terpinen-4-ol, 40 1,8-Cineole, 5 | Trichophyton rubrum T. mentagrophytes Microsporum canis Candida albicans Candida sp. Trichosporon cutaneum Malassezia furfur isolated from patients with Dandruff Seborrheic dermatitis Pityriasis versicolor | 0.11–0.22% (m/v) 0.11–0.44% (m/v) 0.11% (m/v) 0.44% (m/v) 0.22–0.44% (m/v) 0.22% (m/v) 0.05–0.44% (m/v) 0.11–0.22% (m/v) 0.05–0.22% (m/v) | [72] | |||
| α-Terpinene, 9 γ-Terpinene, 19 Terpinen-4-ol, 46 | Chromobacterium violaceum CV026 | At MIC 0.25 mg/mL: 14.3 | 2 mg/mL | [73] | ||
| α-Terpinene, 10 p-Cymene, 24 Terpinen-4-ol, 25 β-Fenchyl alcohol, 9 Oregano + TTO TTO + Cinamom TTO + Lavender TTO + Laurel Oregano + TTO TTO + Cinamom TTO + Lavender TTO + Laurel Oregano + TTO TTO + Cinamom TTO + Lavender TTO + Laurel | Streptococcus pyogenes ATCC 19625 Staphylococcus aureus ATCC 25923 Streptococcus agalactiae ATCC 12386 Streptococcus pyogenes ATCC 19625 S. aureus ATCC 25923 Streptococcus agalactiae ATCC 12386 | 15.00 29.50 26.50 No interaction Additive effect Synergic effect No interaction Synergic effect No interaction No interaction Additive effect Synergic effect No interaction Synergic effect No interaction | 2.00 0.25 Growth | 1.00 0.125 1.00 | [74] | |
| Cupressus sempervirens + TTO Myrtus communis + TTO Origanum marjorana + TTO Origanum vulgare + TTO | Streptococcus agalactiae ATCC 55618 S. pneumoniae ATCC 49619 S. pyogenes ATCC 12344 Mycobacterium smegmatis ATCC 19420 Moraxella catarrhalis ATCC 23246 Cryptococcus neoformans ATCC 14116 Staphylococcus aureus ATCC 25924 Streptococcus agalactiae ATCC 55618 S. pneumoniae ATCC 49619 S. pyogenes ATCC 12344 Mycobacterium smegmatis ATCC 19420 Klebsiella pneumoniae ATCC 13883 Moraxella catarrhalis ATCC 23246 Cryptococcus neoformans ATCC 14116 Staphylococcus aureus ATCC 25924 Streptococcus agalactiae ATCC 55618 S. pneumoniae ATCC 49619 Mycobacterium smegmatis ATCC 19420 Klebsiella pneumoniae ATCC 13883 Moraxella catarrhalis ATCC 23246 Cryptococcus neoformans ATCC 14116 Streptococcus agalactiae ATCC 55618 S. pneumoniae ATCC 49619 Mycobacterium smegmatis ATCC 19420 Klebsiella pneumoniae ATCC 13883 Cryptococcus neoformans ATCC 14116 | Additive effect Additive effect Additive effect Synergic effect Additive effect Synergic effect Synergic effect Additive effect Synergic effect Synergic effect Synergic effect Synergic effect Synergic effect Synergic effect Additive effect Additive effect Additive effect Synergic effect Synergic effect Synergic effect Additive effect Synergic effect Synergic effect Synergic effect Additive effect | 1.00 mg/mL 2.00 mg/mL 1.50 mg/mL 1.00 mg/mL 2.00 mg/mL 0.09 mg/mL 2.00 mg/mL 1.00 mg/mL 1.00 mg/mL 2.00 mg/mL 1.00 mg/mL 1.00 mg/mL 0.25 mg/mL 2.00 mg/mL 1.00 mg/mL 1.50 mg/mL 3.00 mg/mL 1.00 mg/mL 1.00 mg/mL 0.25 mg/mL 1.00 mg/mL 1.00 mg/mL 2.00 mg/mL 1.00 mg/mL 0.50 mg/mL | [75] | ||
| γ-Terpinene, 17 4-Terpinenyl acetate, 67 | Cutibacterium acnes Staphylococcus epidermidis | 0.053 g/mL 0.053 g/mL | 0.053 g/mL 0.053 g/mL | R: No effect I: 0.107 g/mL | [76] | |
| The quantification of the components were not provided | Staphylococcus aureus strain EG-AE1 Staphylococcus epidermidis strain EG-AE2 Cutibacterium acnes Strain EG-AE1 | 15.5 21.02 20.85 | 78 mg/mL 78 mg/mL 39 mg/mL | 78 mg/mL 78 mg/mL 39 mg/mL | [77] |
| Author, Year of Publication | Study | Participants | Acne Severity | Product Application | Duration | Safety | Outcomes (End of Study) |
|---|---|---|---|---|---|---|---|
| Basset et al., 1990 [153] | RCT single-blind | Intervention group (n = 58): tea tree oil (TTO) 5% water-based gel. Control group (n = 61): Benzoyl Peroxide (BP) 5% water-based lotion. Mean age 19.7 years (range 12–35 years) | Mild-moderate acne vulgaris | Unmentioned | 3 months | The control group reported more adverse effects (79%) than the intervention group (44%) (p < 0.001). Adverse effects reported: skin dryness, pruritus, stinging, burning, and redness. Dryness was the most reported. | Inflammatory lesions (IL): BP was significantly better than TTO in the reduction of the number of IL (p < 0.001). However, both treatments were effective in reducing IL. Non-inflammatory lesions (NIL): no significant differences between groups. Both showed a reduction of NIL (TTO group p < 0.05; BP group p < 0.01). Skin oiliness: BP showed increasingly less skin oiliness than the TTO group (p < 0.02). |
| Enshaieh et al., 2007 [154] | RCT double-blind | Intervention group (n = 30): TTO 5% carbomer gel. Mean age = 19.3 ± 3.1 years Control group (n = 30): carbomer gel only Mean age = 19.13 ± 2.64 years | Mild-moderate acne vulgaris | Applied twice daily over the affected area, for 20 min, wash with tap water | 45 days | Minimal pruritus: 10% TTO group; 6.66% control group. Burning sensation on application: 3.33% TTO group; 6.66% control group. Minimal scaling: 3.33% TTO group. | Total Lesion Count (TLC): Intervention group: 43.64% reduction (significant, p = 0.035). Control group: 12.03% reduction (non-significant, p = 0.09). A significant difference between groups (p = 0.000). TTO 5% was 3.55 times more effective. Acne Severity Index (ASI): Intervention group: 40.49% reduction (significant, p = 0.000). Control group: 7.04% reduction (non-significant, p = 0.051). A significant difference between groups (p = 0.000). TTO 5% was 5.75 times more effective. Comedones: Intervention group: 40.24% reduction (significant, p = 0.000). Control group: 12.13% reduction (significant, p = 0.001). A significant difference between groups (p = 0.000). Papules: Intervention group: 46.06% reduction (significant, p = 0.004). Control group: 9.70% reduction (non-significant, p = 0.056). A significant difference between groups (p = 0.022). Pustules: Intervention group: 47.45% reduction (significant, p = 0.001). Control group: 2.37% increase (non-significant, p = 0.45). A significant difference between groups (p = 0.001). |
| Yadav et al., 2011 [160] | RCT uncontrolled, open-label multicentric phase III | Group I (n = 48): Oral tablets (Neem extract 200 mg + Turmeric extract 200 mg + Piper extract 10 mg). Group II (n = 46): Dermatological gel (TTO 5%). Group III (n = 47): Oral tablets + Dermatological gel. Age range: 15–50 years. 139 patients under 30 years | Mild-moderate acne vulgaris | Once daily on the affected area. (Group I and III: one tablet twice a day) | 4 weeks | No serious adverse effects were reported. | Group II (Gel TTO 5%) Blackheads: 78.3% improvement (p < 0.05). Similar in all groups. Papules: 71.4% improvement (p < 0.05). Less improvement compared to other groups. Pustules: 86.4% improvement (p < 0.05). The greater improvement compared to other groups. Cysts: 8.8% improvement (p > 0.05). The greater improvement compared to other groups. Nodules: 13.0% improvement (p > 0.05). Less improvement compared to other groups. Group II showed 17% more improvement in deep inflammatory lesions compared to Group I and over 20% compared to Group III. The improvement observed with gel alone (group II) was slightly lower at the end of the study compared to the other groups. |
| Kim and Shin, 2013 [161] | Experimental pretest-posttest | Intervention group (n = 27): Mixture of TTO 3%, Lavender oil 2% and Jojoba oil + weekly acne treatment Mean age = 21.5 ± 2.2 years Control group (n = 27): weekly acne treatment Mean age = 20.9 ± 1.8 years | Not stated | Twice daily. Subjects were to keep the formulation on their skin for 5 min. | 4 weeks | One subject (n = 1) from the intervention group complained of itch 2–3 days after beginning the treatment, which resolved shortly without subsequent adverse effects. | The number of C. acnes on the foreheads (t = 3.100, p =0.005) and the total number of C. acnes (t = 3.061, p = 0.005) significantly reduced at the end of the intervention. IL: significantly reduced only in the intervention group (t = 5.544, p < 0.001). NIL: significantly reduced in both, intervention (t = 3.406, p = 0.002) and control (t = 3.257, p = 0.003) groups. TLC: significantly reduced in both groups (intervention: t = 6.537, p < 0.001; control: t = 2.947, p =0.007). Sebum excretion: significant reduction in the sebum excretion rate (t = 3.144, p = 0.004) only in the intervention group. |
| Kwon et al., 2014 [155] | RCT double-blind split-face | n = 32 One side: 5% Lactobacillus-fermented Chamaecyparis obtusa (LFCO) Other side: 5% TTO extract to the other side. Mean age = 25.9 ± 5.6 years | Mild-moderate acne vulgaris | Twice daily. | 8 weeks | No severe adverse reactions. TTO side: 12.5% mild dryness and 18.8% mild erythema and desquamation. LFCO side: 6.3% transient mild erythema and 6.3% dryness | IL: significantly reduced on the LFCO side (65.3%, p < 0,01) and TTO side (38.2%, p < 0.01). A significant difference in the mean of IL counts between LFCO and TTO sides (p < 0.05) NIL: significantly reduced on the LFCO side (52.6%, p < 0.01) and TTO side (23.7%, p < 0.05). A significant difference in the mean of NIL counts between LFCO and TTO sides (p < 0.05) Acne Grade (Leeds revised acne grading): significantly decreased on both sides (LFCO side from 4.0 to 1.8, p < 0.01; TTO side from 4.0 to 2.9. p < 0.01). Sebum secretion: LFCO side showed a significant decreased (p < 0.05) but the TTO side did not. Sebaceous gland size: significantly decreased size of the sebaceous gland on the LFCO side (p = 0.03), but not on the TTO side. Proteins related to inflammation: significant decrease on both sides. SREBP-1 and IGF-1R expression showed reductions only on the LFCO side (p < 0.05). IL-8 and TLR-2 mRNA expression were significantly reduced on both sides, but greater on the LFCO side. |
| Malhi et al., 2016 [156] | Dual-centre, open-label, phase II pilot study | n = 14 Tea Tree Medicated Gel (200 mg/g) and Tea Tree Face Wash for Acne (7 mg/g). Mean age = 26 ± 7 years | Mild-moderate acne vulgaris | Twice daily. Wash with one pump of the face wash, then apply a pea-sized gel. Leave the product on for at least 6 h and wash it off only at the next application time. | 12 weeks | No serious adverse reaction. Moderate scaling, peeling, and dryness were recorded at week 4 and reduced at week 12. | TLC: significant decrease of 54% (p < 0.001). IGA Score (Investigator Global Assessment): significant decrease from a mean of 2.4 to 1.9 (p < 0.05). Facial oiliness: mean score significantly decreased from 2.0 to 1.1 (p < 0.01). Clinical efficacy: defined as a reduction in TLC ≥ 40% at the end of the study. Products were clinically effective in 79% of the participants. |
| Mazzarello et al., 2018 [159] | Single-center, randomized, double-blinded, comparative study | Intervention group 1 (n = 20): 20% propolis extract, 3% tea tree oil, and 10% aloe vera leaf juice cream (PTAC). Mean age = 27 ± 7.44 years Intervention group 2 (n = 20): 3% erythromycin cream (EC) Mean age = 23 ± 5.06 years Control group (n = 20): placebo Mean age = 24 ± 6.14 years | Mild-moderate acne vulgaris | Twice daily. | 30 days | Not stated | Sebum, pH, and erythema index values (healthy skin) did not show statistically significant changes in the three groups. The Erythema index of scars and papules showed a statistically significant difference in PTAC and EC groups (p < 0.001). Comedones: Significant reduction (p < 0.001) in PTAC (38.2%) and EC (42.1%) groups. Papules: Significant reduction (p < 0.001) in PTAC (61.4%) and EC (45.4%) groups, and in placebo (4.6%, p < 0.05) Pustules: Significant reduction (p < 0.001) in PTAC (58.7%) and EC (44.1%) groups. ASI: Significant reduction (p < 0.001) in PTAC (66.7%) and EC (49.7%) groups. TLC: Significant reduction (p < 0.001) in PTAC (63.7%) and EC (46.5%) groups, and in placebo (9.9%, p < 0.05) |
| Lubtikulthum et al., 2019 [157] | Observer-blinded, noninferiority randomized controlled study | Intervention group (n = 38): Topical Herbal Extract Formula (HEF). A gel that contains onion, Lavandula, mangosteen, aloe vera, paper mulberry, and tea tree extracts. Mean age = 21.79 ± 2.238 years Control group (n = 36): BP 2.5% cream Mean age = 21.89 ± 2.153 years | Mild-moderate acne vulgaris | Twice daily. Washed off 15 min after application. | 12 weeks | No systemic side effects occurred. The most common adverse effect was skin irritation. Transient itching of acne lesions and burning sensations were reported after the application of both products. Week 2: glazing with peeling and cracking was less common in the intervention group (12.82%) than in the control group (28.95%). Erythema with minimal edema or minimal papular response only was reported in the control group (7.89%). | Comedones: Intervention group: 34.51 ± 31,01%, a significant reduction. Control group: 39.4 ± 2.18%, a significant reduction. IL: Intervention group: 40.54 ± 44.75%, a significant reduction. Control group: 45.3 ± 35.68%, a significant reduction. TLC: Intervention group: 36.47 ± 30.1%, a significant reduction. Control group: 40.9 ± 21.67%, a significant reduction. The mean difference between groups in the percent reduction in comedones, IL and TLC at the end of the study showed an inconclusive result for noninferiority |
| Najafi-Taher, 2022 [158] | RCT, triple-blind | Intervention group (n = 53): tea tree oil (6%) nanoemulsion containing adapalene gel 0.1% (TTO + ADA) Mean age = 26.72 ± 5.231 years Control group (n = 47): adapalene gel 0.1% (ADA) Mean age = 27.36 ± 5.036 years | Mild-moderate acne vulgaris | Once a day (at night). Applied to clean and dry skin on affected areas. | 12 weeks | Mild severity topical adverse reaction was reported in both groups. Dryness was de most frequently reported in both groups. Other reactions reported war irritation, erythema, and burning sensation. | IL and NIL: Decreased in both groups, but a greater decrease in TTO + ADA. Statistically difference between groups (p < 0.001) ASI: Significant reduction (p < 0.001) in both groups, but more obvious for TTO + ADA with 71.69% treatment success compared with 6.38% in the ADA group. TLC: Decreased in both with significant difference between groups (p < 0.001). TTO + ADA showed a greater decrease. |
| Lupu et al., 2022 [162] | Experimental blinded study | Intervention group (n = 35) Application of two products: Ivapur purifying cleansing gel (among other ingredients, zincidone®, glycerine, and Herculane spring thermal water) and Ivapur K cream (among other ingredients, lactic acid, salicylic acid, piroctone olamine, tea tree oil, bisabolol, and Herculane spring thermal water) Mean age = 19.17 ± 6.37 years | Oily, acne-prone skin | Twice daily. Clean with purifying cleansing gel and then applied the cream. | 28 days | No adverse effects were reported. | Facial oiliness: mean score significantly decreased by 2.05 points (p < 0.001). C. acnes colonization: the number of follicles colonized by C. acnes was significantly reduced by an average of 72 (p = 0.003). At the end of the study was observed decrease in the number of infundibula with thickened bright borders (p < 0.001), the follicles with dilated infundibula (p = 0.005), the comedones (p < 0.001), and in the inflammatory infiltrate density (p < 0.001). On the opposite, the number of regular follicles increased (p < 0.001) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nascimento, T.; Gomes, D.; Simões, R.; da Graça Miguel, M. Tea Tree Oil: Properties and the Therapeutic Approach to Acne—A Review. Antioxidants 2023, 12, 1264. https://doi.org/10.3390/antiox12061264
Nascimento T, Gomes D, Simões R, da Graça Miguel M. Tea Tree Oil: Properties and the Therapeutic Approach to Acne—A Review. Antioxidants. 2023; 12(6):1264. https://doi.org/10.3390/antiox12061264
Chicago/Turabian StyleNascimento, Tânia, Diana Gomes, Ricardo Simões, and Maria da Graça Miguel. 2023. "Tea Tree Oil: Properties and the Therapeutic Approach to Acne—A Review" Antioxidants 12, no. 6: 1264. https://doi.org/10.3390/antiox12061264
APA StyleNascimento, T., Gomes, D., Simões, R., & da Graça Miguel, M. (2023). Tea Tree Oil: Properties and the Therapeutic Approach to Acne—A Review. Antioxidants, 12(6), 1264. https://doi.org/10.3390/antiox12061264






