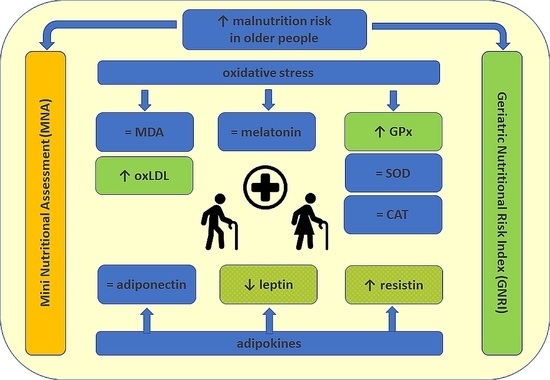
Evaluation of Selected Parameters of Oxidative Stress and Adipokine Levels in Hospitalized Older Patients with Diverse Nutritional Status
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Study Design
2.3. Biochemical Analysis
2.4. Statistical Analysis
3. Results
3.1. Selected Oxidative Stress Parameters and Adipokines According to the MNA
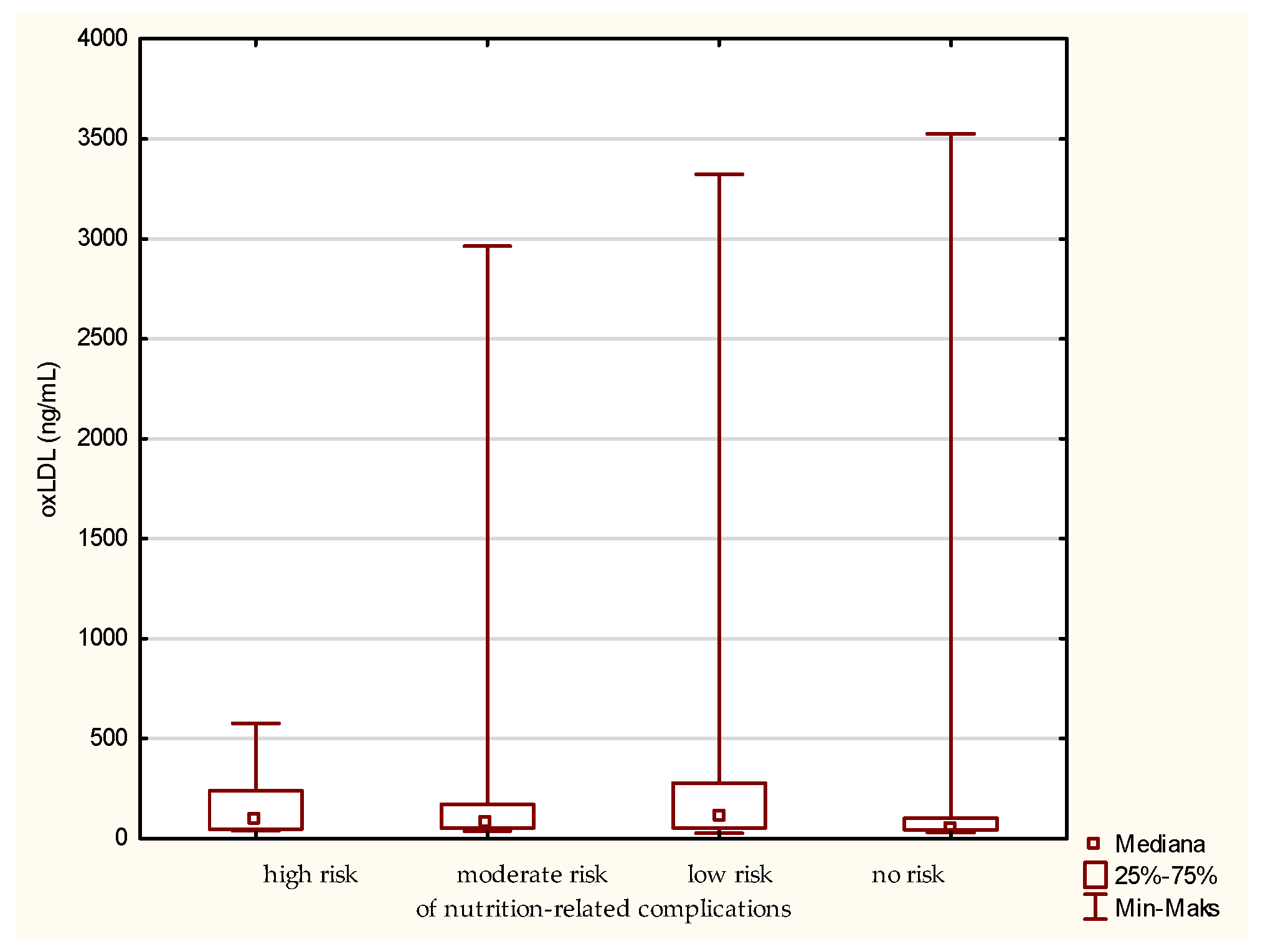
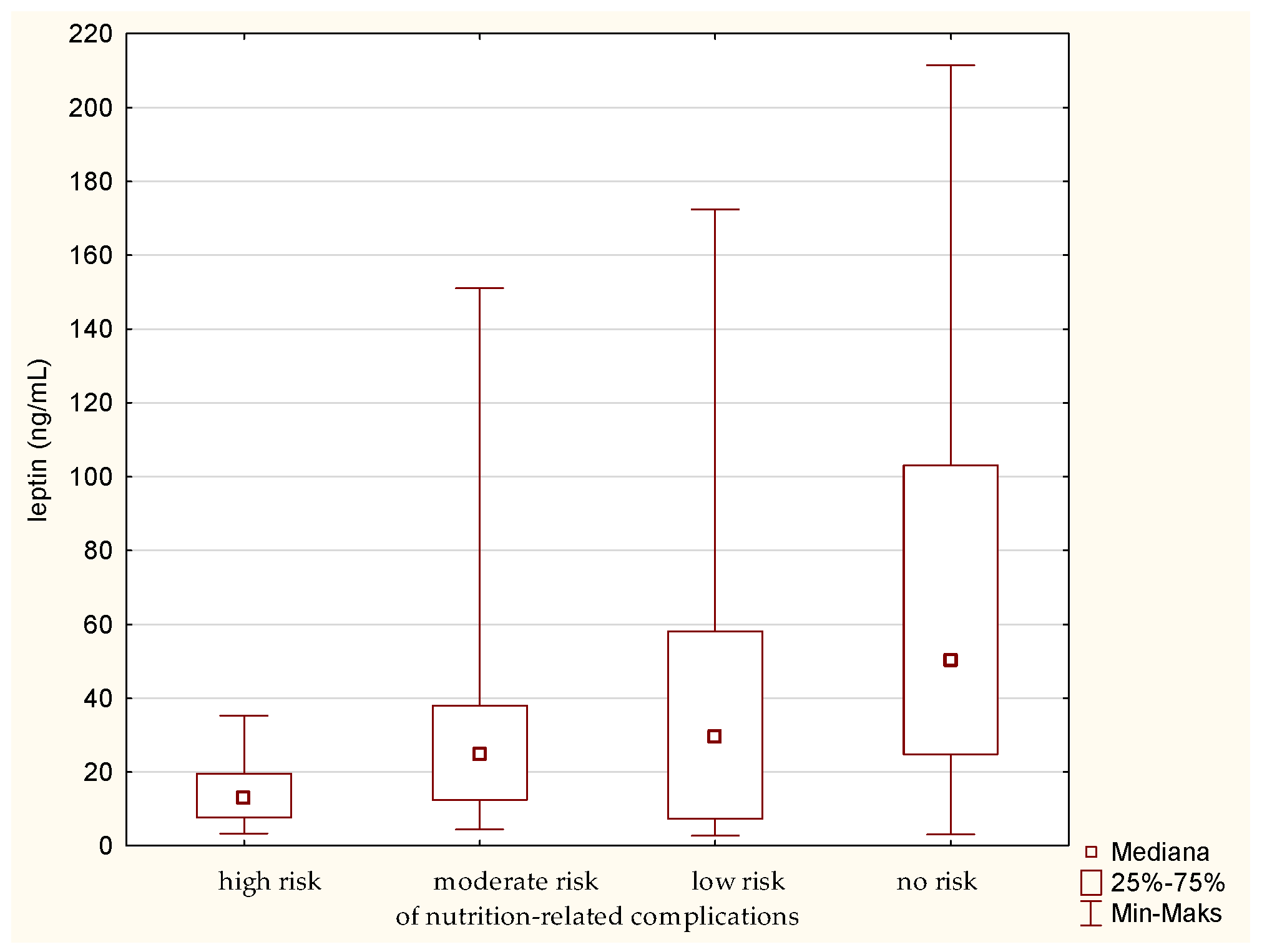
3.2. Selected Oxidative Stress Parameters and Adipokines According to the GNRI
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Adams, N.E.; Bowie, A.J.; Simmance, N.; Murray, M.; Crowe, T.C. Recognition by Medical and Nursing Professionals of Malnutrition and Risk of Malnutrition in Elderly Hospitalised Patients. Nutr. Diet. 2008, 65, 144–150. [Google Scholar] [CrossRef]
- Burks, C.E.; Jones, C.W.; Braz, V.A.; Swor, R.A.; Richmond, N.L.; Hwang, K.S.; Hollowell, A.G.; Weaver, M.A.; Platts-Mills, T.F. Risk Factors for Malnutrition among Older Adults in the Emergency Department: A Multicenter Study. J. Am. Geriatr. Soc. 2017, 65, 1741–1747. [Google Scholar] [CrossRef] [PubMed]
- Raynaud-Simon, A. Virtual Clinical Nutrition University: Malnutrition in the Elderly, Epidemiology and Consequences. e-SPEN 2009, 4, e86–e89. [Google Scholar] [CrossRef] [Green Version]
- Krzymińska-Szymaszko, R.; Lewandowicz, M.; Wieczorowska-Tobis, K. Niedożywienie Jako Wielki Zespół Geriatryczny Malnutrition as a Geriatric Giant. Geriatria 2016, 10, 179–183. [Google Scholar]
- Kaur, B.; Mal, H.K. Association between Malnutrition and Depression among Elderly of Selected Rural Area of District Faridkot, Punjab. Int. J. Com. Health Med. Res. 2017, 3, 41–45. [Google Scholar] [CrossRef]
- Laudisio, A.; Antonelli Incalzi, R.; Gemma, A.; Giovannini, S.; Lo Monaco, M.R.; Vetrano, D.L.; Padua, L.; Bernabei, R.; Zuccalà, G. Use of Proton-Pump Inhibitors Is Associated with Depression: A Population-Based Study. Int. Psychogeriatr. 2018, 30, 153–159. [Google Scholar] [CrossRef]
- Giovannini, S.; Onder, G.; Van Der Roest, H.G.; Topinkova, E.; Gindin, J.; Cipriani, M.C.; Denkinger, M.D.; Bernabei, R.; Liperoti, R. Use of Antidepressant Medications among Older Adults in European Long-Term Care Facilities: A Cross-Sectional Analysis from the SHELTER Study. BMC Geriatr. 2020, 20, 310. [Google Scholar] [CrossRef]
- Mziray, M.; Zuralska, R.; Ksiazek, J.; Domagała, P. Niedożywienie u Osób w Wieku Podeszłym, Metody Jego Oceny, Profilaktyka i Leczenie. Ann. Acad. Medicae Gedanensis 2016, 46, 95–105. [Google Scholar]
- Moreira, P.L.; Boas, P.J.F.V.; Ferreira, A.L.A. Association between Oxidative Stress and Nutritional Status in the Elderly. Rev. Assoc. Med. Bras. 2014, 60, 75–83. [Google Scholar] [CrossRef] [Green Version]
- Egbuna, C. Oxidative Stress and Nutrition. Trop. J. Appl. Nat. Sci. 2017, 2, 110–116. [Google Scholar] [CrossRef]
- Liguori, I.; Russo, G.; Curcio, F.; Bulli, G.; Aran, L.; Della-Morte, D.; Gargiulo, G.; Testa, G.; Cacciatore, F.; Bonaduce, D.; et al. Oxidative Stress, Aging, and Diseases. Clin. Interv. Aging 2018, 13, 757–772. [Google Scholar] [CrossRef] [Green Version]
- Ghone, R.A.; Suryakar, A.N.; Kulhalli, P.M.; Bhagat, S.S.; Padalkar, R.K.; Karnik, A.C.; Hundekar, P.S.; Sangle, D.A. A Study of Oxidative Stress Biomarkers and Effect of Oral Antioxidant Supplementation in Severe Acute Malnutrition. J. Clin. Diagn. Res. 2013, 7, 2146–2148. [Google Scholar] [CrossRef]
- Fuente, M.; Miquel, J. An Update of the Oxidation-Inflammation Theory of Aging: The Involvement of the Immune System in Oxi-Inflamm-Aging. Curr. Pharm. Des. 2009, 15, 3003–3026. [Google Scholar] [CrossRef]
- Bouillanne, O.; Golmard, J.L.; Coussieu, C.; Noël, M.; Durand, D.; Piette, F.; Nivet-Antoine, V. Leptin a New Biological Marker for Evaluating Malnutrition in Elderly Patients. Eur. J. Clin. Nutr. 2007, 61, 647–654. [Google Scholar] [CrossRef]
- Amirkalali, B.; Sharifi, F.; Fakhrzadeh, H.; Mirarefein, M.; Ghaderpanahi, M.; Badamchizadeh, Z.; Larijani, B. Low Serum Leptin Serves as a Biomarker of Malnutrition in Elderly Patients. Nutr. Res. 2010, 30, 314–319. [Google Scholar] [CrossRef]
- Akın, S.; Tufan, F.; Bulut, L.; Genç, S.; Bahat, G.; Saka, B.; Erten, N.; Karan, M.A. Limited Utility of Adipokine Levels in the Diagnosis of Malnutrition in the Elderly. Aging Clin. Exp. Res. 2014, 26, 229–234. [Google Scholar] [CrossRef]
- Paillaud, E.; Poisson, J.; Granier, C.; Ginguay, A.; Plonquet, A.; Conti, C.; Broussier, A.; Raynaud-Simon, A.; Bastuji-Garin, S. Serum Leptin Levels, Nutritional Status, and the Risk of Healthcare-Associated Infections in Hospitalized Older Adults. Nutrients 2022, 14, 226. [Google Scholar] [CrossRef]
- Park, H.K.; Ahima, R.S. Physiology of Leptin: Energy Homeostasis, Neuroendocrine Function and Metabolism. Metabolism 2015, 64, 24–34. [Google Scholar] [CrossRef] [Green Version]
- Góralska, M.; Majewska-Szczepanik, M.; Szczepanik, M. Immunological Mechanisms Involved in Obesity and Their Role in Metabolic Syndrome. Postepy Hig. Med. Dosw. (Online) 2015, 69, 1384–1404. [Google Scholar]
- Smitka, K.; Marešová, D. Adipose Tissue as an Endocrine Organ: An Update on Pro-Inflammatory and Anti-Inflammatory Microenvironment. Prague Med. Rep. 2015, 116, 87–111. [Google Scholar] [CrossRef] [Green Version]
- Kochan, Z.; Karbowska, J. Secretory Function of Adipose Tissue. Postep. Biochem. 2004, 50, 256–271. [Google Scholar]
- Vellas, B.; Guigoz, Y.; Garry, P.J.; Nourhashemi, F.; Bennahum, D.; Lauque, S.; Albarede, J.L.; Vellas, B. The Mini Nutritional Assessment (MNA) for Grading the Nutritional State of Elderly Patients: Presentation of the MNA, History and Validation. Nestle Nutr. Workshop Ser. Clin. Perform. Programme 1999, 1, 3–11. [Google Scholar] [CrossRef] [Green Version]
- Abd Aziz, N.A.S.; Mohd Fahmi Teng, N.I.; Kamarul Zaman, M. Geriatric Nutrition Risk Index Is Comparable to the Mini Nutritional Assessment for Assessing Nutritional Status in Elderly Hospitalized Patients. Clin. Nutr. ESPEN 2019, 29, 77–85. [Google Scholar] [CrossRef] [PubMed]
- Bouillanne, O.; Morineau, G.; Dupont, C.; Coulombel, I.; Vincent, J.-P.; Nicolis, I.; Benazeth, S.; Cynober, L.; Aussel, C. Geriatric Nutritional Risk Index: A New Index for Evaluating at-Risk Elderly Medical Patients. Am. J. Clin. Nutr. 2005, 82, 777–783. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Misra, H.P.; Fridovich, I. The Role of Superoxide Anion in the Autoxidation of Epinephrine and a Simple Assay for Superoxide Dismutase. J. Biol. Chem. 1972, 247, 3170–3175. [Google Scholar] [CrossRef]
- Beers, R.F.J.; Sizer, I.W. A Spectrophotometric Method for Measuring the Breakdown of Hydrogen Peroxide by Catalase. J. Biol. Chem. 1952, 195, 133–140. [Google Scholar] [CrossRef]
- Paglia, D.E.; Valentine, W.N. Studies on the Quantitative and Qualitative Characterization of Erytrocyte Glutathione Peroxidase. J. Lab. Clin. Med. 1967, 70, 158–169. [Google Scholar]
- Buege, J.A.; Aust, S.D. Microsomal Lipid Peroxidation. In Methods in Enzymology; Elsevier: Singapore, 1978; Volume 52, pp. 302–310. ISBN 0121819787. [Google Scholar]
- Esterbauer, H.; Cheeseman, K.H. Determination of Aldehydic Lipid Peroxidation Products: Malonaldehyde and 4-Hydroxynonenal. In Methods in Enzymology; Elsevier: Singapore, 1990; Volume 186, pp. 407–421. ISBN 9780121820879. [Google Scholar]
- Moreira, N.C.F.; Krausch-Hofmann, S.; Matthys, C.; Vereecken, C.; Vanhauwaert, E.; Declercq, A.; Bekkering, G.E.; Duyck, J. Risk Factors for Malnutrition in Older Adults: A Systematic Review of the Literature Based on Longitudinal Data. Adv. Nutr. 2016, 7, 507–522. [Google Scholar] [CrossRef] [Green Version]
- Orrevall, Y.; Tishelman, C.; Permert, J.; Cederholm, T. Nutritional Support and Risk Status among Cancer Patients in Palliative Home Care Services. Support. Care Cancer 2009, 17, 153–161. [Google Scholar] [CrossRef]
- Son, N.; Kavak, B. Evaluation of Nutritional Status of Elderly Patients Presenting to the Family Health Center. Pakistan J. Med. Sci. 2018, 34, 446–451. [Google Scholar] [CrossRef]
- Alzahrani, S.H.; Alamri, S.H. Prevalence of Malnutrition and Associated Factors among Hospitalized Elderly Patients in King Abdulaziz University Hospital, Jeddah, Saudi Arabia. BMC Geriatr. 2017, 17, 136. [Google Scholar] [CrossRef] [Green Version]
- Zhang, Z.; Pereira, S.L.; Luo, M.; Matheson, E.M. Evaluation of Blood Biomarkers Associated with Risk of Malnutrition in Older Adults: A Systematic Review and Meta-Analysis. Nutrients 2017, 9, 829. [Google Scholar] [CrossRef]
- Szewczyk-Golec, K.; Woźniak, A.; Reiter, R.J. Inter-Relationships of the Chronobiotic, Melatonin, with Leptin and Adiponectin: Implications for Obesity. J. Pineal Res. 2015, 59, 277–291. [Google Scholar] [CrossRef]
- Cederholm, T.; Amer, P.; Palmblad, J. Low Circulating Leptin Levels in Protein-Energy Malnourished Chronically Ill Elderly. Clin. Nutr. 1997, 16, 28. [Google Scholar] [CrossRef]
- Jasińska, A.; Diagn, M.P. Adipocytokiny Białka o Wielokierunkowym Działaniu. J. Lab. Diagn. 2010, 46, 331–338. [Google Scholar]
- Dostalova, I.; Kunesova, M.; Duskova, J.; Papezova, H.; Nedvidkova, J. Adipose Tissue Resistin Levels in Patients with Anorexia Nervosa. Nutrition 2006, 22, 977–983. [Google Scholar] [CrossRef]
- Bednarska-Makaruk, M.; Graban, A.; Wiśniewska, A.; Łojkowska, W.; Bochyńska, A.; Gugała-Iwaniuk, M.; Sławińska, K.; Ługowska, A.; Ryglewicz, D.; Wehr, H. Association of Adiponectin, Leptin and Resistin with Inflammatory Markers and Obesity in Dementia. Biogerontology 2017, 18, 561–580. [Google Scholar] [CrossRef] [Green Version]
- Liakopoulos, V.; Mertens, P.R.; Eleftheriadis, T.; Koukoulis, G.; Stefanidis, I. Is There a Link between Inflammation, Plasma Resistin Levels, and Protein Malnutrition in Hemodialysis Patients? Kidney Int. 2006, 70, 1371–1372. [Google Scholar] [CrossRef] [Green Version]
- Marouga, A.; Dalamaga, M.; Kastania, A.N.; Antonakos, G.; Thrasyvoulides, A.; Kontelia, G.; Dimas, C.; Vlahakos, D.V. Correlates of Serum Resistin in Elderly, Non-Diabetic Patients with Chronic Kidney Disease. Clin. Lab. 2013, 59, 1121–1128. [Google Scholar] [CrossRef]
- George, J.; Wexler, D.; Roth, A.; Barak, T.; Sheps, D.; Keren, G. Usefulness of Anti-Oxidized LDL Antibody Determination for Assessment of Clinical Control in Patients with Heart Failure. Eur. J. Heart Fail. 2006, 8, 58–62. [Google Scholar] [CrossRef] [Green Version]
- Dainy, N.C.; Kusharto, C.M.; Madanijah, S.; Nasrun, M.W.S.; Turana, Y. Nutritional Status, Physical Activity, Oxidative Stress, and Cognitive Function in Pre Elderly and Elderly. J. Gizi Pangan 2018, 13, 117–122. [Google Scholar] [CrossRef]
- Raikou, V.; Kardalinos, V.; Kyriaki, D. Oxidized Low-Density Lipoprotein Serum Concentrations and Cardiovascular Morbidity in End Stage of Renal Disease. J. Cardiovasc. Dev. Dis. 2018, 5, 35. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mandas, A.; Congiu, M.G.; Balestrieri, C.; Mereu, A.; Iorio, E.L. Nutritional Status and Oxidative Stress in an Elderly Sardinian Population. Med. J. Nutrition Metab. 2008, 1, 99. [Google Scholar] [CrossRef]
- Sánchez-Rodríguez, M.A.; Martínez-Cruz, M.; Correa-Muñoz, E.; Mendoza-Núñez, V.M. Relationship between Metabolic Syndrome Components and Oxidative Stress in Elderly Community-Dwelling Mexicans. Ann. Nutr. Metab. 2010, 56, 302–307. [Google Scholar] [CrossRef]
- De Ferranti, S.; Mozaffarian, D. The Perfect Storm: Obesity, Adipocyte Dysfunction, and Metabolic Consequences. Clin. Chem. 2008, 54, 945–955. [Google Scholar] [CrossRef] [Green Version]
- Rondanelli, M.; Trotti, R.; Opizzi, A.; Solerte, S.B. Relationship among Nutritional Status, pro/Antioxidant Balance and Cognitive Performance in a Group of Free-Living Healthy Elderly. Minerva Med. 2007, 98, 639–645. [Google Scholar]
- Rahman, K. Studies on Free Radicals, Antioxidants, and Co-Factors. Clin. Interv. Aging 2007, 2, 219–236. [Google Scholar]
- Pinontoan, R.; Sayogo, S.; Roosheroe, A.G. Correlation between Serum Zinc Level and Erythrocyte Superoxide Dismutase (SOD) Activity in Non-Frail and Frail Geriatric Patients. World Nutr. J. 2017, 1, 34. [Google Scholar] [CrossRef] [Green Version]
- Fasna, K.A.; Geetha, N.; Maliekkal, J. Oxidative Stress in Ageing. Int. J. Res. Med. Sci. 2017, 5, 4826. [Google Scholar] [CrossRef]
- Chandran, M.; Phillips, S.A.; Ciaraldi, T.; Henry, R.R. Adiponectin: More than Just Another Fat Cell Hormone? Diabetes Care 2003, 26, 2442–2450. [Google Scholar] [CrossRef] [Green Version]
- Baker, J.F.; Newman, A.B.; Kanaya, A.; Leonard, M.B.; Zemel, B.; Miljkovic, I.; Long, J.; Weber, D.; Harris, T.B. The Adiponectin Paradox in the Elderly: Associations with Body Composition, Physical Functioning, and Mortality. J. Gerontol. Ser. A 2019, 74, 247–253. [Google Scholar] [CrossRef] [Green Version]
- Bobin-Dubigeon, C.; Lefrançois, A.; Vansteene, D.; Dupé, M.; Joalland, M.P.; Bard, J.M. Leptin and Adiponectin as New Markers of Undernutrition in Cancer. Clin. Biochem. 2017, 50, 525–528. [Google Scholar] [CrossRef]
- Huang, C.; Kogure, M.; Tomata, Y.; Sugawara, Y.; Hozawa, A.; Momma, H.; Tsuji, I.; Nagatomi, R. Association of Serum Adiponectin Levels and Body Mass Index with Worsening Depressive Symptoms in Elderly Individuals: A 10-Year Longitudinal Study. Aging Ment. Health 2020, 24, 725–731. [Google Scholar] [CrossRef]
- Soysal, P.; Smith, L.; Dokuzlar, O.; Isik, A.T. Relationship Between Nutritional Status and Insomnia Severity in Older Adults. J. Am. Med. Dir. Assoc. 2019, 20, 1593–1598. [Google Scholar] [CrossRef]




| Nutritional Status | Malnutrition Indicator Score |
|---|---|
| malnutrition | less than 17 points |
| at risk of malnutrition | 17 to 23.5 points |
| adequate nutritional status | 24 to 30 points |
| GNRI Score | Classification |
|---|---|
| <82 | major risk |
| 82–<92 | moderate risk |
| 92–≤98 | low risk |
| >98 | no risk |
| Parameter | Malnutrition | Range | At Risk of Malnutrition | Range | Adequate Nutritional Status | Range | Total Average | Range | Kruskal–Wallis Test | p Value |
|---|---|---|---|---|---|---|---|---|---|---|
| MDApl 1 [nmol/mL] | 0.5 | 0.5 | 0.5 | 0.3 | 0.5 | 0.5 | 0.5 | 0.5 | H (2. N = 136) = 1.821581 | 0.4022 |
| MDAer 2 [nmol/g Hb] | 21.8 | 27.9 | 22.6 | 47.0 | 21.5 | 51.3 | 21.7 | 55.2 | H (2. N = 137) = 0.7760118 | 0.6784 |
| oxLDL 3 [ng/mL] | 82.5 | 3295.2 | 50.7 | 391.3 | 55.8 | 3495.7 | 58.4 | 3498.8 | H (2. N = 136) = 4.469296 | 0.1070 |
| SOD 4 [U/gHb] | 722.9 | 471.1 | 727.2 | 217.3 | 721.1 | 371.1 | 725.1 | 471.1 | H (2. N = 137) = 0.0239938 | 0.9881 |
| GPx 5 [U/gHb] | 7.3 | 12.0 | 6.7 | 9.8 | 6.0 | 13.9 | 6.5 | 15.1 | H (2. N = 137) = 1.293940 | 0.5236 |
| CAT 6 [IU/gHb] | 492,700.0 | 456,900.0 | 504,450.0 | 249,600.0 | 530,200.0 | 462,700.0 | 514,500.0 | 471000.0 | H (2. N = 137) = 2.523735 | 0.2831 |
| adiponectin [ng/mL] | 14.6 | 34.0 | 14.1 | 29.5 | 12.8 | 32.4 | 13.5 | 35.6 | H (2. N = 136) = 4.973683 | 0.0832 |
| leptin [ng/mL] | 18.5 | 169.7 | 29.7 | 198.6 | 52.5 | 208.4 | 35.8 | 208.8 | H (2. N = 132) = 21.36475 | 0.0000 |
| resistin [ng/mL] | 21.2 | 102.2 | 23.7 | 26.1 | 15.9 | 73.6 | 18.5 | 106.1 | H (2. N = 133) = 16.65061 | 0.0002 |
| melatonin [pg/mL] | 81.4 | 196.0 | 81.4 | 247.2 | 86.0 | 246.6 | 84.0 | 258.9 | H (2. N = 136) = 0.3805290 | 0.8267 |
| Parameter | High Risk | Range | Moderate Risk | Range | Low Risk | Range | No Risk | Range | Total Average | Range | Kruskal–Wallis Test | p |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MDApl 1 [nmol/g Hb] | 0.5 | 0.5 | 0.5 | 0.3 | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 | H (3. N = 136) = 4.754880 | 0.1907 |
| MDAer 2 [nmol/g Hb] | 22.2 | 21.6 | 20.2 | 18.0 | 21.8 | 48.7 | 21.6 | 51.3 | 21.7 | 55.2 | H (3. N = 137) = 0.6137224 | 0.8933 |
| oxLDL 3 [ng/mL] | 96.9 | 536.8 | 77.9 | 2926.9 | 105.6 | 3295.2 | 55.4 | 3495.7 | 58.4 | 3498.8 | H (3. N = 136) = 8.611890 | 0.0349 |
| SOD 4 [U/gHb] | 743.2 | 287.3 | 740.6 | 401.6 | 725.1 | 337.7 | 714.5 | 399.2 | 725.1 | 471.1 | H (3. N = 137) = 1.634320 | 0.6516 |
| GPx 5 [U/gHb] | 7.8 | 5.5 | 8.7 | 10.5 | 5.7 | 11.5 | 6.0 | 13.9 | 6.5 | 15.1 | H (3. N = 137) = 9.038221 | 0.0288 |
| CAT 6 [IU/gHb] | 511,850.0 | 319,200.0 | 525,000.0 | 335,600.0 | 484,900.0 | 456,900.0 | 524,000.0 | 462,700.0 | 514,500.0 | 471,000.0 | H (3. N = 137) = 3.183901 | 0.3641 |
| adiponectin [ng/mL] | 20.6 | 34.0 | 14.6 | 27.0 | 10.5 | 24.4 | 13.4 | 35.0 | 13.5 | 35.6 | H (3. N = 136) = 5.996740 | 0.1118 |
| leptin [ng/mL] | 13.0 | 31.9 | 24.8 | 146.6 | 29.5 | 169.7 | 50.2 | 208.4 | 35.8 | 208.8 | H (3. N = 132) = 18.53068 | 0.0003 |
| resistin [ng/mL] | 35.0 | 97.7 | 21.5 | 34.5 | 17.5 | 58.8 | 16.6 | 73.6 | 18.5 | 106.1 | H (3. N = 133) = 17.29766 | 0.0006 |
| melatonin [pg/mL] | 13.0 | 31.9 | 24.8 | 146.6 | 29.5 | 169.7 | 50.2 | 208.4 | 35.8 | 208.8 | H (3. N = 132) = 18.53068 | 0.0003 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mądra-Gackowska, K.; Szewczyk-Golec, K.; Gackowski, M.; Woźniak, A.; Kędziora-Kornatowska, K. Evaluation of Selected Parameters of Oxidative Stress and Adipokine Levels in Hospitalized Older Patients with Diverse Nutritional Status. Antioxidants 2023, 12, 569. https://doi.org/10.3390/antiox12030569
Mądra-Gackowska K, Szewczyk-Golec K, Gackowski M, Woźniak A, Kędziora-Kornatowska K. Evaluation of Selected Parameters of Oxidative Stress and Adipokine Levels in Hospitalized Older Patients with Diverse Nutritional Status. Antioxidants. 2023; 12(3):569. https://doi.org/10.3390/antiox12030569
Chicago/Turabian StyleMądra-Gackowska, Katarzyna, Karolina Szewczyk-Golec, Marcin Gackowski, Alina Woźniak, and Kornelia Kędziora-Kornatowska. 2023. "Evaluation of Selected Parameters of Oxidative Stress and Adipokine Levels in Hospitalized Older Patients with Diverse Nutritional Status" Antioxidants 12, no. 3: 569. https://doi.org/10.3390/antiox12030569
APA StyleMądra-Gackowska, K., Szewczyk-Golec, K., Gackowski, M., Woźniak, A., & Kędziora-Kornatowska, K. (2023). Evaluation of Selected Parameters of Oxidative Stress and Adipokine Levels in Hospitalized Older Patients with Diverse Nutritional Status. Antioxidants, 12(3), 569. https://doi.org/10.3390/antiox12030569