Antioxidant Effects of a Polyphenol-Rich Dietary Supplement Incorporating Pinus massoniana Bark Extract in Healthy Older Adults: A Two-Arm, Parallel Group, Randomized Placebo-Controlled Trial
Abstract
1. Introduction
2. Materials and Methods
2.1. Recruitment
2.2. Study Design
2.3. Clinical Assessments
2.4. Medical History, Dietary Intake and Physical Activity
2.5. Blood Sampling and Analyses
2.6. Statistical Analysis and Sample Size Determination
3. Results
3.1. Baseline Characteristics
3.2. Nutrient Intake, Physical Activity and Compliance
3.3. Anthropometry and Physical Activity
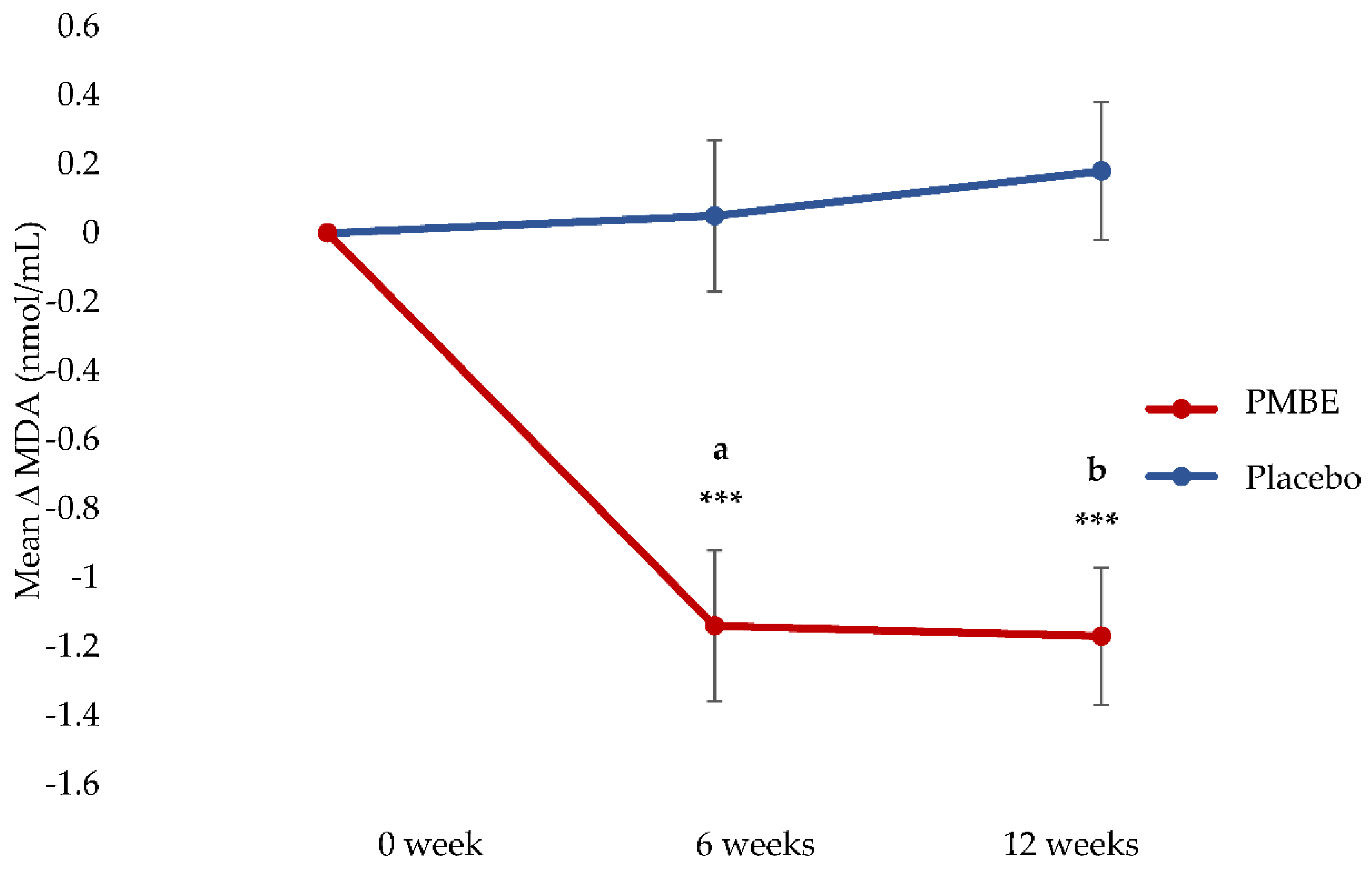
3.4. Primary Outcome: Plasma MDA Concentrations
3.5. Inflammatory Markers
3.6. Liver Function
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Australian Institute of Health and Welfare. Older Clients of Specialist Homelessness Services. Cat. no. HOU 314; AIHM: Canberra, Australia, 2019. Available online: https://www.aihw.gov.au/reports/homelessness-services/older-clients-of-specialist-homelessness-services (accessed on 15 September 2021).
- Australian Institute of Health and Welfare. Older Australia at a Glance. Australian Government. 2018. Available online: https://www.aihw.gov.au/reports/older-people/older-australia-at-a-glance/report-editions (accessed on 21 March 2022).
- Calder, P.C.; Bosco, N.; Bourdet-Sicard, R.; Capuron, L.; Delzenne, N.; Dore, J.; Franceschi, C.; Lehtinen, M.J.; Recker, T.; Salvioli, S.; et al. Health relevance of the modification of low grade inflammation in ageing (inflammageing) and the role of nutrition. Ageing Res. Rev. 2017, 40, 95–119. [Google Scholar] [CrossRef] [PubMed]
- Liguori, I.; Russo, G.; Curcio, F.; Bulli, G.; Della-Morte, D.; Gargiulo, G.; Cacciatore, F. Oxidative stress, aging, and diseases. Clin. Interv. Aging 2018, 13, 757–772. [Google Scholar] [CrossRef] [PubMed]
- Mosoni, L.; Breuille, D.; Buffiere, C.; Obled, C.; Mirand, P.P. Age-related changes in glutathione availability and skeletal muscle carbonyl content in healthy rats. Exp. Gerontol. 2004, 39, 203–210. [Google Scholar] [CrossRef]
- Reid, M.B.; Li, Y.P. Cytokines and oxidative signalling in skeletal muscle. Acta Physiol. Scand. 2001, 171, 225–232. [Google Scholar] [CrossRef]
- Giera, M.; Lingeman, H.; Niessen, W.M.A. Recent advancements in the LC- and GC-based analysis of malondialdehyde (MDA): A brief overview. Chromatographia 2012, 75, 433–440. [Google Scholar] [CrossRef] [PubMed]
- Inal, M.E.; Kanbak, G.; Sunal, E. Antioxidant enzyme activities and malondialdehyde levels related to aging. Clin. Chim. Acta 2001, 305, 75–80. [Google Scholar] [CrossRef]
- Mutlu-Türkoğlu, Ü.; İlhan, E.; Öztezcan, S.; Kuru, A.; Aykaç-Toker, G.; Uysal, M. Age-related increases in plasma malondialdehyde and protein carbonyl levels and lymphocyte DNA damage in elderly subjects. Clin. Biochem. 2003, 36, 397–400. [Google Scholar] [CrossRef]
- Walston, J.D. Sarcopenia in older adults. Curr. Opin. Rheumatol. 2012, 24, 623–627. [Google Scholar] [CrossRef]
- Van Roie, E.; Bautmans, I.; Coudyzer, W.; Boen, F.; Delecluse, C. Low- and High-Resistance Exercise: Long-Term Adherence and Motivation among Older Adults. Gerontology 2015, 61, 551–560. [Google Scholar] [CrossRef]
- Wang, Y.; Chung, S.J.; Song, W.O.; Chun, O.K. Estimation of daily proanthocyanidin intake and major food sources in the U.S. diet. J. Nutr. 2011, 141, 447–452. [Google Scholar] [CrossRef]
- Crozier, A.; Jaganath, I.B.; Clifford, M.N. Dietary phenolics: Chemistry, bioavailability and effects on health. Nat. Prod. Rep. 2009, 26, 1001–1043. [Google Scholar] [CrossRef] [PubMed]
- Gabetta, B.; Fuzzati, N.; Griffini, A.; Lolla, E.; Pace, R.; Ruffilli, T.; Peterlongo, F. Characterization of proanthocyanidins from grape seeds. Fitoterapia 2000, 71, 162–175. [Google Scholar] [CrossRef]
- Shahat, A.A.; Cos, P.; Bruyne, T.D.; Apers, S.; Hammouda, F.M.; Ismail, S.I.; Azzam, S.; Claeys, M.; Goovaerts, E. Antiviral and antioxidant activity of flavonoids and proanthocyanidins from Crataegus sinaica. Planta Med. 2002, 68, 539–541. [Google Scholar] [CrossRef] [PubMed]
- Hatano, T.; Miyatakea, H.; Natsumeb, M.; Osakabeb, N.; Takizawab, T.; Itoa, H.; Yoshida, T. Proanthocyanidin glycosides and related polyphenols from cacao liquor and their antioxidant effects. Phytochemistry 2002, 59, 749–758. [Google Scholar] [CrossRef]
- Bagchi, D.; Bagchi, M.; Stohs, S.J.; Das, D.K.; Ray, S.D.; Kuszynski, C.A.; Joshi, S.S.; Pruess, H.G. Free radicals and grape seed proanthocyanidin extract: Importance in human health and disease prevention. Toxicology 2000, 148, 187–197. [Google Scholar] [CrossRef]
- Garbacki, N.; Kinet, M.; Nusgens, B.; Desmecht, D.; Damas, J. Roantho-cyanidins, from Ribes nigrum leaves, reduce endothelial adhesion molecules ICAM-1 and VCAM-1. J. Inflamm. 2005, 2, 9. [Google Scholar] [CrossRef][Green Version]
- Yang, F.; Villiers, W.J.S.; McClain, C.J.; Varilek, G.W. Green tea polyphenols block endotoxin-induced tumor necrosis factor-production and lethality in a murine model. J. Nutr. 1998, 128, 2334–2340. [Google Scholar] [CrossRef]
- Nandakumar, V.; Singha, T.; Katiyar, S.K. Multi-targeted prevention and therapy of cancer by proanthocyanidins. Cancer Lett. 2008, 269, 378–387. [Google Scholar] [CrossRef]
- Holt, R.R.; Schramm, D.D.; Keen, C.L.; Lazarus, S.A.; Schmitz, H.H. Chocolate consumption and platelet function. JAMA 2002, 287, 2212–2213. [Google Scholar] [CrossRef]
- Ren, J.; An, J.; Chen, M.; Yang, H.; Ma, Y. Effect of proanthocyanidins on blood pressure: A systematic review and meta-analysis of randomized controlled trials. Pharmacol. Res. 2021, 165, 105329. [Google Scholar] [CrossRef]
- Santos-Buelga, C.; Scalbert, A. Proanthocyanidins and tannin-like compounds-nature, occurrence, dietary intake and effects on nutrition and health. J. Sci. Food. Agric. 2000, 80, 1094–1117. [Google Scholar] [CrossRef]
- D’Andrea, G. Pycnogenol: A blend of procyanidins with multifacetedtherapeutic applications? Fitoterapia 2010, 81, 724–736. [Google Scholar] [CrossRef] [PubMed]
- Rauf, A.; Imran, M.; Abu-Izneid, T.; Iahtisham Ul, H.; Patel, S.; Pan, X.; Naz, S.; Sanches Silva, A.; Saeed, F.; Rasul Suleria, H.A. Proanthocyanidins: A comprehensive review. Biomed. Pharmacother. 2019, 116, 108999. [Google Scholar] [CrossRef] [PubMed]
- Malekahmadi, M.; Moradi Moghaddam, O.; Firouzi, S.; Daryabeygi-Khotbehsara, R.; Shariful Islam, S.M.; Norouzy, A.; Soltani, S. Effects of pycnogenol on cardiometabolic health: A systematic review and meta-analysis of randomized controlled trials. Pharmacol. Res. 2019, 150, 104472. [Google Scholar] [CrossRef]
- Cretu, E.; Karonen, M.; Salminen, J.; Mircea, C.; Trifan, A.; Charalambous, C.; Constantinou, A.I.; Miron, A. In Vitro Study on the Antioxidant Activity of a Polyphenol-Rich Extract from Pinus brutia Bark and Its Fractions. J. Med. Food 2013, 16, 984–991. [Google Scholar] [CrossRef]
- Zhang, H.Y.; Zhang, Z.Y. Pinus massoniana Lamb. In Key Records of Chinese Traditional Medicine in China; Zeng, M.Y., Zeng, J.F., Eds.; Science Press: Peking, China, 1994. [Google Scholar]
- Cui, Y.; Xie, H.; Wang, J. Potential biomedical properties of Pinus massoniana bark extract. Phytother. Res. 2005, 19, 34–38. [Google Scholar] [CrossRef] [PubMed]
- Wu, D.C.; Li, S.; Yang, D.Q.; Cui, Y.Y. Effects of Pinus massoniana bark extract on the adhesion and migration capabilities of HeLa cells. Fitoterapia 2011, 82, 1202–1205. [Google Scholar] [CrossRef] [PubMed]
- Yu, L.; Zhao, M.; Wang, J.S.; Cui, C.; Yang, B.; Zhao, Q. Antioxidant, immunomodulatory and anti-breast cancer activities of phenolic extract from pine (Pinus massoniana Lamb) bark. Innov. Food Sci. Emerg. Technol. 2008, 9, 122–128. [Google Scholar] [CrossRef]
- Wang, M.; Ma, H.; Liu, B.; Wang, H.; Xie, H.; Li, R.; Wang, J. Pinus massoniana bark extract protects against oxidative damage in L-02 hepatic cells and mice. Am. J. Chin. Med. 2010, 38, 909–919. [Google Scholar] [CrossRef]
- National Health and Medical Research Council. Australian guidelines to reduce health risks from drinking alcohol. In Australia; Research Council and Universities Australia, Ed.; Commonwealth of Australia: Canberra, Australia, 2020. [Google Scholar]
- Amagase, H.; Sun, B.; Borek, C. Lycium barbarum (goji) juice improves in vivo antioxidant biomarkers in serum of healthy adults. Nutr. Res. 2009, 29, 19–25. [Google Scholar] [CrossRef]
- The Royal College of Pathologists of Australia. Liver Function Tests. The Royal College of Pathologists of Australia. 2019. Available online: https://www.rcpa.edu.au/Manuals/RCPA-Manual/Pathology-Tests/L/Liver-function-tests (accessed on 3 February 2022).
- Clarke, E.D.; Collins, C.; Rollo, M.; Kroon, P.; Philo, M.; Haslam, R. The relationship between urinary polyphenol metabolites and dietary polyphenol intakes in young adults. Br. J. Nutr. 2022, 127, 589–598. [Google Scholar] [CrossRef] [PubMed]
- Del Bo, C.; Bernardi, S.; Marino, M.; Porrini, M.; Tucci, M.; Guglielmetti, S.; Cherubini, A.; Carrieri, B.; Kirkup, B.; Kroon, P.; et al. Systematic Review on Polyphenol Intake and Health Outcomes: Is there Sufficient Evidence to Define a Health-Promoting Polyphenol-Rich Dietary Pattern? Nutrients 2019, 11, 1355. [Google Scholar]
- Amiot, M.J.; Riva, C.; Vinet, A. Effects of dietary polyphenols on metabolic syndrome features in humans: A systematic review. Obes. Rev. 2016, 17, 573–586. [Google Scholar] [CrossRef] [PubMed]
- Devaraj, S.; Vega-Lopez, S.; Kaul, N.; Schonlau, F.; Rohdewald, P.; Jialal, I. Supplementation with a Pine Bark Extract Rich in Polyphenols Increases Plasma Antioxidant Capacity and Alters the Plasma Lipoprotein Profile. Lipids 2002, 37, 931–934. [Google Scholar] [CrossRef]
- Li, S.; Xu, M.; Niu, Q.; Xu, S.; Ding, Y.; Yan, Y.; Guo, S.; Li, F. Efficacy of Procyanidins against In Vivo Cellular Oxidative Damage: A Systematic Review and Meta-Analysis. PLoS ONE 2015, 10, e0139455. [Google Scholar] [CrossRef] [PubMed]
- Gulgun, M.; Erdem, O.; Oxtas, E.; Kesik, V.; Balamtekin, N.; Sebahattin, V.; Kul, M.; Kismet, E.; Koseoglu, V. Proanthocyanidin prevents methotrexate-induced intestinal damage and oxidative stress. Exp. Toxicol. Pathol. 2010, 62, 109–115. [Google Scholar] [CrossRef] [PubMed]
- Guler, A.; Sahin, M.A.; Yucel, O.; Yokusoglu, M.; Gamsizkan, M.; Ozal, E.; Demirkilic, U.; Arslan, M. Proanthocyanidin prevents myocardial ischemic injury in adult rats. Med. Sci. Monit. 2011, 17, BR326. [Google Scholar] [CrossRef]
- Yamakoshi, J.; Kataoka, S.; Koga, T.; Ariga, T. Proanthocyanidin-rich extract from grape seeds attenuates the development of aortic atherosclerosis in cholesterol-fed rabbits. Atherosclerosis 1999, 142, 139–149. [Google Scholar] [CrossRef]
- Sano, A.; Uchida, R.; Saito, M.; Shioya, N.; Komori, Y.; Tho, Y.; Hashizume, N. Beneficial effects of grape seed extract on malondialdehyde-modeified LDL. J. Nutr. Sci. Vitaminol. 2007, 53, 174–182. [Google Scholar] [CrossRef]
- Maurya, P.K.; Rizvi, S.I. Protective role of tea catechins on erythrocytes subjected to oxidative stress during human aging. Nat. Prod. Res. 2009, 23, 1072–1079. [Google Scholar] [CrossRef]
- Ottaviani, J.; Borges, G.; Momma, T.; Spencer, J.P.E.; Keen, C.L.; Crozier, A.; Schroeter, H. The metabolome of [2-14C](−)-epicatechin in humans: Implications for the assessment of efficacy, safety and mechanisms of action of polyphenolic bioactives. Sci. Rep. 2016, 6, 29034. [Google Scholar] [CrossRef] [PubMed]
- Manosroi, A.; Chankhampan, C.; Pattamapun, K.; Manosroi, W.; Manosroi, J. Antioxidant and Gelatinolytic Activities of Papain from Papaya Latex and Bromelain from Pineapple Fruits. Chang. Mai. J. Sci. 2014, 41, 635–648. [Google Scholar]
- Richardson, D.P.; Ansell, J.; Drummond, L.N. The nutritional and health attributes of kiwifruit: A review. Eur. J. Nutr. 2018, 57, 2659–2676. [Google Scholar] [CrossRef]
- Brevik, A.; Gaivão, I.; Medin, T.; Jørgenesen, A.; Piasek, A.; Elilasson, J.; Karlsen, A.; Blomhoff, R.; Veggan, T.; Duttaroy, A.K.; et al. Supplementation of a western diet with golden kiwifruits (Actinidia chinensis var.’Hort 16A’:) effects on biomarkers of oxidation damage and antioxidant protection. Nutr. J. 2011, 10, 54. [Google Scholar] [CrossRef]
- Campanella, L.; Gatta, T.; Gregori, E.; Tomassetti, M. Determination of antioxidant capacity of papaya fruit and papaya-based food and drug integrators, using a biosensor device and other analytical methods. Monatsh. Chem. 2008, 140, 965–972. [Google Scholar] [CrossRef]
- Álvarez-Satta, M.; Berna-Erro, A.; Carrasco-Garcia, E.; Alberro, A.; Saenz-Antoñanzas, A.; Vergara, I.; Otaegui, D.; Matheu, A. Relevance of oxidative stress and inflammation in frailty based on human studies and mouse models. Aging 2020, 12, 9982–9999. [Google Scholar] [CrossRef]
- García, N.; Zazueta, C.; Aguilera-Aguirre, L. Oxidative Stress and Inflammation in Cardiovascular Disease. Oxid. Med. Cell. Longev. 2017, 2017, 5853238. [Google Scholar] [CrossRef]
- De Almeida, A.J.P.O.; de Almeida Rezende, M.S.; Dantas, S.H.; de Lima Silva, S.; de Oliveira, J.C.P.L.; de Lourdes Assunção Araújo de Azevedo, F.; Alves, R.M.F.R.; de Menezes, G.M.S.; dos Santos, P.F.; Gonçalves, T.A.F.; et al. Unveiling the Role of Inflammation and Oxidative Stress on Age-Related Cardiovascular Diseases. Oxid. Med. Cell. Longev. 2020, 2020, 1954398. [Google Scholar] [CrossRef]
- Signorelli, S.; Katsiki, N. Oxidative stress and inflammation: Their role in the pathogenesis of peripheral artery disease with or without type 2 diabetes mellitus. Curr. Vasc. Pharmacol. 2018, 16, 547–554. [Google Scholar] [CrossRef]
- Masoudkabir, F.; Sarrafzadegan, N. The interplay of endothelial dysfunction, cardiovascular disease, and cancer: What we should know beyond inflammation and oxidative stress. Eur. J. Prev. Cardiol. 2020, 27, 2075–2076. [Google Scholar] [CrossRef]
- Rojas-Gutierrez, E.; Muñoz-Arenas, G.; Treviño, S.; Espinosa, B.; Chavez, R.; Rojas, K.; Flores, G.; Díaz, A.; Guevara, J. Alzheimer’s disease and metabolic syndrome: A link from oxidative stress and inflammation to neurodegeneration. Synapse 2017, 71, e21990. [Google Scholar] [CrossRef] [PubMed]
- Kakafika, A.I.; Liberopoulos, E.N.; Mikhailidis, D.P. Fibrinogen: A predictor of vascular disease. Curr. Pharm. Des. 2007, 13, 1647–1659. [Google Scholar] [CrossRef] [PubMed]
- Belcaro, G.; Cesarone, M.R.; Errichi, S.; Zulli, C.; Errichi, B.M.; Vinciguerra, G.; Ledda, A.; Di Renzo, A.; Stuard, S.; Dugall, M.; et al. Variations in C-reactive protein, plasma free radicals and fibrinogen values in patients with osteoarthritis treated with Pycnogenol. Redox Rep. 2008, 13, 271–276. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.; Huang, S.; Zhao, L.; Zhang, J.; Ji, C.; Ma, Q. Pine (Pinus massoniana Lamb.) Needle Extract Supplementation Improves Performance, Egg Quality, Serum Parameters, and the Gut Microbiome in Laying Hens. Front. Nutr. 2022, 9, 810462. [Google Scholar] [CrossRef]
- Probst, Y.; Guan, V.; Kent, K. A systematic review of food composition tools used for determining dietary polyphenol intake in estimated intake studies. Food. Chem. 2018, 1, 146–152. [Google Scholar] [CrossRef]
- Pourmasoumi, M.; Hadi, A.; Mohammadi, H.; Rouhani, M.H. Effect of pycnogenol supplementation on blood pressure: A systematic review and meta-analysis of clinical trials. Phytother. Res. 2020, 34, 67–76. [Google Scholar] [CrossRef]
- Gulati, O.P. Pycnogenol® in Metabolic Syndrome and Related Disorders. Phytother. Res. 2015, 29, 949–968. [Google Scholar] [CrossRef]
- Vinciguerra, G.; Belcaro, G.; Cesarone, M.R.; Rohdewald, P.; Stuard, S.; di Renzo, A.; Hosoi, M.; Dugall, M.; Ledda, A.; Cacchio, M.; et al. Cramps and Muscular Pain-Prevention with pycnogenol in normal subjects, venous patients, athletes, claudicants and in diabetic microangiopathy. Angiology 2006, 57, 331–339. [Google Scholar] [CrossRef]

| Placebo (mg/Day) | PMBE (mg/Day) | |
|---|---|---|
| Polyphenolics (CE) | 32.0 | 431.5 |
| Monomeric (free) catechins | 2 | 29.5 |
| Total PACs | 10.5 | 59.5 |
| Total anthocyanosides | nd | 0.25 |
| Placebo (n = 30) | PMBE (n = 32) | p | |
|---|---|---|---|
| Sex, n (%) | 0.960 | ||
| Male | 12 (40.0) | 13 (40.6) | |
| Female | 18 (60.0) | 19 (59.4) | |
| Ethnicity, n (%) | 0.681 | ||
| Oceanian | 17 (56.7) | 15 (46.9) | |
| Oceanian/North-west European | 5 (16.7) | 6 (18.8) | |
| North-west European | 5 (16.7) | 9 (28.1) | |
| South-east European | 1 (3.3) | 0 (0) | |
| Other 2 | 2 (6.7) | 2 (6.3) | |
| Age (y) | 63.85 ± 0.92 | 65.22 ± 0.90 | 0.293 |
| Height (cm) | 166.90 ± 1.68 | 166.7 ± 1.78 | 0.941 |
| Weight (kg) | 71.50 ± 2.36 | 70.83 ± 2.64 | 0.851 |
| BMI (kg/m2) | 25.33 ± 0.58 | 25.06 ± 0.59 | 0.746 |
| Medication use for: | |||
| High blood pressure | 4 (13.3) | 5 (15.6) | 0.798 |
| High cholesterol | 1 (3.3) | 5 (15.6) | 0.102 |
| GORD | 2 (6.7) | 4 (12.5) | 0.438 |
| Anxiety | 4 (13.3) | 1 (3.1) | 0.140 |
| Other 3 | 8 (26.7) | 5 (15.6) | 0.286 |
| MET (min/week) 4 | 4329.6 (2493, 6456) | 4452 (1983, 6698) | 0.822 |
| Compliance 5 | 98.85 ± 0.52 | 98.61 ± 0.31 | 0.596 |
| Time | ∆ | |||
|---|---|---|---|---|
| Nutrients | Baseline | 6-Weeks | 12-Weeks | |
| Energy (kJ) | ||||
| Placebo | 8554.9 (391.5) | 8489.3 (373.6) | 8452.4 (421.1) | −102.4 (327.3) |
| PMBE | 8307.1 (359.2) | 8364.8 (434.8) | 8689.8 (356.8) | 371.3 (318.8) |
| Protein (%E) 2 | ||||
| Placebo | 18.8 (0.8) | 19.0 (0.9) | 19.1 (0.9) | 0.2 (0.9) |
| PMBE | 18.7 (0.5) | 17.4 (0.8) | 17.5 (0.7) | −1.2 (0.6) |
| CHO (%E) | ||||
| Placebo | 39.1 (1.4) | 38.3 (1.4) | 39.1 (1.6) | 0.08 (1.3) |
| PMBE | 39.3 (1.4) | 39.9 (1.3) | 40.0 (1.3) | 1.0 (1.4) |
| Fat (%E) | ||||
| Placebo | 36.1 (1.3) | 35.9 (1.5) | 35.7 (1.5) | −0.5 (1.3) |
| PMBE | 36.0 (1.1) | 35.2 (1.1) | 35.4 (0.9) | −0.7 (1.2) |
| Sat Fat (%E) | ||||
| Placebo | 13.0 (0.7) | 13.3 (0.8) | 13.2 (0.8) | 0.2 (0.8) |
| PMBE | 13.5 (0.6) | 13.0 (0.6) | 13.1 (0.5) | −0.5 (0.6) |
| Trans fat (%E) | ||||
| Placebo | 0.6 (0.08) | 0.5 (0.05) | 0.6 (0.04) | −0.04 (0.08) |
| PMBE | 0.6 (0.04) | 0.6 (0.04) | 0.6 (0.04) | −0.05 (0.05) |
| Cholesterol (mg) | ||||
| Placebo | 328.1 (41.1) | 288.7 (31.6) | 306.3 (27.5) | −21.8 (42.9) |
| PMBE | 363.3 (26.9) | 288.4 (29.3) | 314.7 (26.3) | −32.9 (27.7) |
| Sugars (g) | ||||
| Placebo | 91.6 (6.9) | 91.3 (5.2) | 90.4 (5.7) | −1.2 (6.3) |
| PMBE | 90.9 (6.3) | 93.3 (7.0) | 93.7 (6.8) | 3.5 (6.1) |
| Fibre (g) | ||||
| Placebo | 29.0 (1.9) | 28.9 (1.9) | 29.1 (2.4) | 0.06 (1.5) |
| PMBE | 28.0 (1.6) | 27.6 (1.5) | 28.2 (1.5) | 0.2 (1.7) |
| Sodium (mg) | ||||
| Placebo | 2417.9 (164.3) | 1984.1 (116.4) | 2094.7 (133.3) | −323.1 (197.4) |
| PMBE | 2365.9 (118.8) | 2247.3 (167.9) | 2520.6 (192.3) | 174.8 (213.5) |
| Alcohol (g) | ||||
| Placebo | 7.6 (2.8) | 9.9 (3.0) | 8.4 (2.3) | 0.8 (1.5) |
| PMBE | 7.7 (1.8) | 10.9 (2.5) | 10.5 (1.9) | 2.3 (2.0) |
| Time | Change 2 | ||||||
|---|---|---|---|---|---|---|---|
| Outcomes | Baseline | 6-Weeks | n | 12-Weeks | n | ∆1 (95% CI) 2 | ∆2 (95% CI) 3 |
| MDA (nmol/mL) | |||||||
| Placebo | 7.58 (0.12) | 7.57 (0.12) | 22 | 7.75 (0.14) | 0.05 (−0.39, −0.48) | 0.18 (−0.22, 0.57) | |
| PMBE | 8.23 (0.19) | 7.02 (0.27) | 22 | 6.85 (0.14) | 30 | −1.19 (−1.62, −0.75) *** | −1.35 (−1.74, −0.96) *** |
| Difference 4 | −1.23 (−1.84, −0.62) *** | −1.53 (−2.09, −0.98) *** | |||||
| hsCRP (mg/dL) 5 | |||||||
| Placebo | 1.26 (0.71. 2.21) | 1.44 (0.89, 2.45) | 22 | 1.43 (0.86, 3.22) | 0.01 (−0.23, 0.26) | 0.18 (−0.04, 0.40) | |
| PMBE | 0.92 (0.53, 1.72) | 0.68 (0.42, 1.34) | 22 | 0.75 (0.49, 1.36) | 30 | −0.20 (−0.44, 0.05) | −0.10 (−0.32, 0.12) |
| Difference | −0.21 (−0.56, 0.14) | −0.28 (−0.59, 0.03) | |||||
| IL-6 (pg/mL) | |||||||
| Placebo | 1.00 (0.63, 1.56) | 0.85 (0.58, 1.27) | 22 | 0.83 (0.58, 1.27) | −0.21 (−0.44, 0.01) | −0.13 (−0.33, 0.07) | |
| PMBE | 0.93 (0.51, 1.41) | 0.91 (0.65, 1.19) | 22 | 1.04 (0.62, 1.46) | 30 | 0.05 (−0.18, 0.27) | 0.17 (−0.03, 0.37) |
| Difference | 0.26 (−0.06, 0.58) | 0.30 (0.02, 0.59) * | |||||
| IL-10 (pg/mL) | |||||||
| Placebo | 0.49 (0.23, 1.21) | 0.65 (0.29, 1.26) | 22 | 0.65 (0.38, 0.97) | 0.12 (−0.09, 0.34) | 0.02 (−0.19, 0.23) | |
| PMBE | 1.13 (1.06, 1.18) | 1.17 (1.03, 1.22) | 22 | 1.16 (1.11, 1.31) | 30 | 0.01 (−0.03, 0.06) | 0.02 (−0.03, 0.08) |
| Difference | −0.11 (−0.33, 0.10) | 0.001 (−0.22, 0.22) | |||||
| ICAM-1 (ng/mL) | |||||||
| Placebo | 11.66 (0.35) | 11.67 (0.46) | 22 | 11.80 (0.41) | −0.23 (−0.71, 0.25) | 0.16 (−0.26, 0.59) | |
| PMBE | 11.03 (0.46) | 11.80 (0.49) | 22 | 11.13 (0.53) | 30 | 0.11 (−0.36, 0.57) | 0.12 (−0.23, 0.47) |
| Difference | 0.34 (−0.34, 1.01) | −0.04 (−0.64, 0.56) | |||||
| Fibrinogen (g/L) | |||||||
| Placebo | 3.56 (0.09) | 3.55 (0.12) | 22 | 3.37 (0.11) | −0.05 (−0.19, 0.09) | −0.18 (−0.38, −0.009) | |
| PMBE | 3.17 (0.08) | 3.22 (0.08) | 22 | 2.90 (0.09) | 30 | −0.02 (−0.14, 0.10) | −0.25 (−0.39, −0.11) *** |
| Difference | 0.03 (−0.16, 0.21) | −0.07 (−0.31, 0.17) | |||||
| Time | Reference Intervals 1 | |||
|---|---|---|---|---|
| Outcomes | Baseline | 6-Weeks | 12-Weeks | |
| Calc Glob (g/L) | ||||
| Placebo | 28.73 (0.36) | 28.64 (0.38) | 29.07 (0.42) | 25–35 |
| PMBE | 29.59 (0.50) | 29.68 (0.62) | 29.50 (0.56) | |
| T. Bilirubin (umol/L) | ||||
| Placebo | 10 (8, 12) | 9 (7, 12) | 10 (9, 13) | <20 |
| PMBE | 13 (9, 19) | 12 (11, 20) | 13 (8, 23) | |
| GGT (U/L) | ||||
| Placebo | 16 (13, 21) | 17.5 (13, 24) | 17.5 (13, 26) | <50 (male) |
| PMBE | 18 (13, 24.5) | 17.5 (14, 27) | 17.5 (14. 24) | <30 (female) |
| ALP (U/L) | ||||
| Placebo | 74.10 (2.82) | 77.14 (2.53) | 74.83 (3.15) | 30–110 |
| PMBE | 65.44 (2.62) | 67.95 (3.41) | 68.00 (3.19) * | |
| ALT (U/L) | ||||
| Placebo | 23.5 (20, 32) | 25 (22, 33) | 24 (21, 30) | <35 |
| PMBE | 23 (21, 27.5) | 24.5 (21, 30) | 24.5 (20, 30) | |
| AST (U/L) | ||||
| Placebo | 26 (23, 29) | 26 (24, 29) | 25.5 (24, 29) | <40 |
| PMBE | 25 (23, 30) | 26 (24, 29) | 25 (22, 29) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ferguson, J.J.A.; Oldmeadow, C.; Bentley, D.; Garg, M.L. Antioxidant Effects of a Polyphenol-Rich Dietary Supplement Incorporating Pinus massoniana Bark Extract in Healthy Older Adults: A Two-Arm, Parallel Group, Randomized Placebo-Controlled Trial. Antioxidants 2022, 11, 1560. https://doi.org/10.3390/antiox11081560
Ferguson JJA, Oldmeadow C, Bentley D, Garg ML. Antioxidant Effects of a Polyphenol-Rich Dietary Supplement Incorporating Pinus massoniana Bark Extract in Healthy Older Adults: A Two-Arm, Parallel Group, Randomized Placebo-Controlled Trial. Antioxidants. 2022; 11(8):1560. https://doi.org/10.3390/antiox11081560
Chicago/Turabian StyleFerguson, Jessica J. A., Christopher Oldmeadow, David Bentley, and Manohar L. Garg. 2022. "Antioxidant Effects of a Polyphenol-Rich Dietary Supplement Incorporating Pinus massoniana Bark Extract in Healthy Older Adults: A Two-Arm, Parallel Group, Randomized Placebo-Controlled Trial" Antioxidants 11, no. 8: 1560. https://doi.org/10.3390/antiox11081560
APA StyleFerguson, J. J. A., Oldmeadow, C., Bentley, D., & Garg, M. L. (2022). Antioxidant Effects of a Polyphenol-Rich Dietary Supplement Incorporating Pinus massoniana Bark Extract in Healthy Older Adults: A Two-Arm, Parallel Group, Randomized Placebo-Controlled Trial. Antioxidants, 11(8), 1560. https://doi.org/10.3390/antiox11081560








