Abstract
Several studies have shown that blood vitamin levels are low in alcoholic patients. In effect, alcohol use abuse is considered a chronic disease that promotes the pathogenesis of many fatal diseases, such as cancer and liver cirrhosis. The alcohol effects in the liver can be prevented by antioxidant mechanisms, which induces enzymatic as well as other nonenzymatic pathways. The effectiveness of several antioxidants has been evaluated. However, these studies have been accompanied by uncertainty as mixed results were reported. Thus, the aim of the present review article was to examine the current knowledge on vitamin deficiency and its role in chronic liver disease. Our review found that deficiencies in nutritional vitamins could develop rapidly during chronic liver disease due to diminished hepatic storage and that inadequate vitamins intake and alcohol consumption may interact to deplete vitamin levels. Numerous studies have described that vitamin supplementation could reduce hepatotoxicity. However, further studies with reference to the changes in vitamin status and the nutritional management of chronic liver disease are in demand.
1. Introduction
In the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) of the American Psychiatric Association, problematic alcohol use is classified as an alcohol use disorder (AUD), which goes from mild to severe depending on the number of diagnostic criteria involved [1]. A range of genetic, behavioral, and environmental variables contribute to alcoholism [2].
Alcoholic drinks are extensively consumed worldwide. Drinking alcohol has negative and positive consequences. The health consequences of alcohol intake vary depending on the amount and pattern of consumption. Although many investigations have provided a correlation between light to moderate alcohol intake and a lower risk of cardiovascular mortality [3,4], some studies found that the link between alcohol consumption and a variety of cardiovascular diseases is ambiguous or negative also at modest intakes [5,6,7].
Ethanol ranks first on the list of abused drugs worldwide. Alcohol use disorder affects about 7.2% of people older than 12 years old, including 6.9% of males and 7.8% of females [8]. It has been described that excessive alcohol drinking promotes the pathogenesis of many diseases, such as cancer, liver cirrhosis, cardiovascular diseases, diabetes, and neuropsychiatric disorders [9,10,11,12].
Several associated conditions, such as liver dysfunction, malnutrition, and deficiency in antioxidant vitamins and trace elements, also contribute to the pathogenesis of alcoholic liver disease (ALD). Furthermore, the evidence summarizing the importance of vitamins, their role during ALD, and their possible pathways of action into the disease development is still contradictory. Therefore, the goal of this review is to update the relevance of vitamins and their deficiency during ALD and their potential modes of action during the illness. The flow chart for the study selection process is shown in Figure 1.
Figure 1.
Flow diagram for the review process.
2. The Pathophysiology of Alcohol Drinking
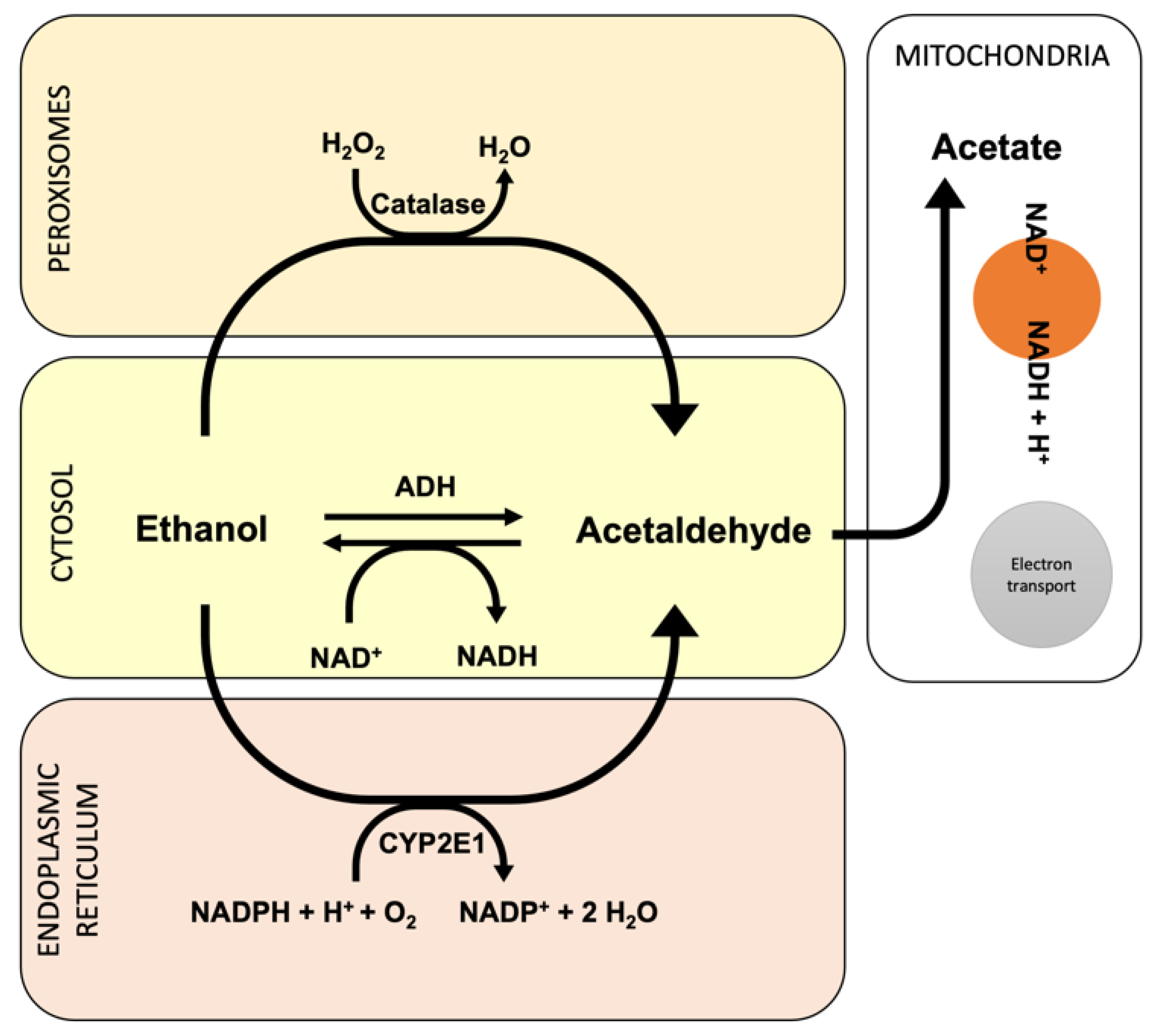
Ethanol is harmful to the human body and can cause toxicity and death when ingested in excessive amounts. Ethanol metabolism produces an alcoholic fatty liver, alcoholic hepatitis, or cirrhosis [13,14]. The major pathway of ethanol metabolism is the oxidative pathway that involves alcohol dehydrogenase (ADH) present in the cytosol of hepatocytes [15]. This ADH produces acetaldehyde, which is toxic due to its high reactivity and may form DNA or protein adducts [16,17]. Some of the alcohol that is ingested orally does not enter the systemic circulation but may be oxidized in the stomach by ADH and their isoforms. Since the Km of most ADH isozymes for ethanol is low (about 1 mM), ADH is saturated at low concentrations of alcohol, and the MEOS system is activated [18].
Another quantity of ethanol is metabolized by the cytochrome P450 2E1 (CYP2E1) in the microsomal ethanol oxidizing system (MEOS) located within the smooth endoplasmic reticulum of hepatocytes, which leads to lipid peroxidation and to the mitochondrial glutathione and S-adenosylmethionine depletion, producing increased oxidative stress and liver injury [19,20,21]. In addition, fatty acid ethyl esters (FAEE) synthase produces FAEEs via nonoxidative metabolism [22].
Through alcohol intoxication, the CYP2E1-dependent system and the microsomal respiratory chain are the principal sources of reactive oxygen species (ROS) within the hepatocytes. Because of its propensity to metabolize and activate a variety of hepatotoxic substrates in the liver, CYP2E1 is of particular interest. Ethanol, carbon tetrachloride, acetaminophen, and N-nitrosodimethylamine, as well as several hazardous compounds, are among these substrates. [23,24]. In this view, the ethanol-induced activation of cytochrome CYP2E1 appears to be one of the main mechanisms by which ethanol causes oxidative stress. Furthermore, when ethanol is oxidized by CYP2E1, it creates acetaldehyde, a highly reactive molecule that may contribute to ethanol’s toxicity [25].
Alcohol-induced liver damage, extracellular matrix changes, and inflammation have all been linked to acetaldehyde [26,27]. Its actions are triggered by the formation of ROS and a redox imbalance (NAD/NADH). It also creates protein clumps in hepatocytes, limiting protein secretion and encouraging hepatomegaly; it combines with dopamine to form salsolinol, which can lead to alcoholism, and it binds to DNA to generate carcinogenic products, such as 1,N 2-propano-2′-desoxyguanosine [12,28].
Several research articles have linked alcohol-mediated oxidative stress and ethanol-inducible CYP2E1 with oxidative stress and their toxicity, both in in vitro and in vivo models. In effect, new pathophysiological focuses that could be used against ALD have been described using in vitro studies [29,30]. Nonetheless, hepatocytes’ antioxidant defense can counteract this damage through enzymatic as well as nonenzymatic mechanisms [31,32,33,34,35,36]. Recent clinical trials have examined the efficacy of numerous antioxidants, including S-adenosylmethionine (SAMe) and vitamin E. However, the conclusions drawn by these have been conflicting [31,32,37,38]. As a result, the current study focuses on what we know about antioxidant deficiency and its involvement in AUD and provides suggestions for future trials. Figure 2 shows the oxidative pathway during ethanol metabolism into the hepatocytes.
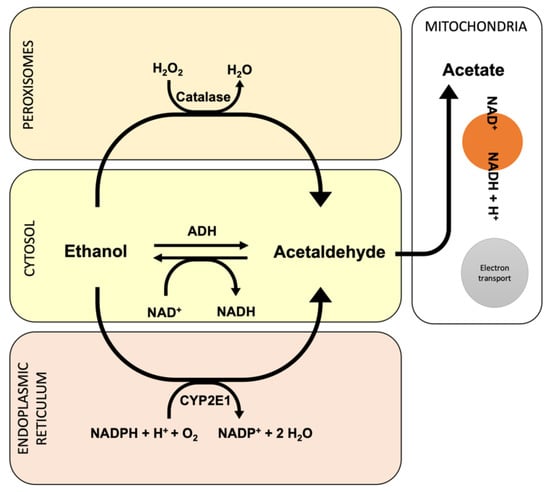
Figure 2.
Oxidative pathway involved during ethanol metabolism.
3. Recommended Dietary Allowances
Recommended dietary allowances (RDA) are population statistics, and they represent rough estimates of the average requirement of individuals within a population. However, for most micronutrients, part of the information that is required to accurately calculate the daily intake is either unknown or incomplete. Thus, the recommendations are made based on several assumptions and considerations that could lead to large variations in the eventual RDA [39,40]. In addition, notwithstanding emerging evidence of the remarkable individual differences in the absorption and excretion of vitamins, these values have changed little over the years. It is known that eating requirement values can vary substantially because of several factors, which include genetic polymorphisms, obesity, total energy intake, exercise, and age [41,42,43,44,45,46,47].
The major dietary recommendations for cirrhotic patients are to avoid hepatotoxic substances and to provide enough macronutrient and micronutrient supply in terms of calories, protein, carbs, vitamins supplements, and minerals [48,49].
4. Vitamin B
Previous studies have described that vitamin B (vitamin B1, vitamin B2 and vitamin B6) deficiency in ALD is caused by different factors, such as inadequate dietary intake, increased use of vitamin B, decreased hepatic storage, impairment of intestinal absorption by ethanol, or abnormal metabolism of the vitamins [50,51].
Due to decreased hepatic storage, vitamin B9 and vitamin B12 deficiencies can develop quickly in chronic liver illness. However, alcohol consumption affects the metabolism of homocysteine (tHcy) because the enzyme cofactor for the conversion of tHcy to methionine is vitamin B12. Decreased levels of vitamin B12 levels were shown to be adversely connected with tHcy and significantly linked with indicators of alcohol-related liver impairment in recent research [52]. Another research found that individuals with severe chronic liver disease had high vitamin B12 plasma levels but decreased vitamin B9 plasma levels [53]. Conversely, Gibson et al. [54] has shown that two weeks of moderate consumption of alcohol (i.e., red wine, or vodka) increased tHcy and reduced the statuses of both vitamin B9 and B12. In addition, other studies have studied vitamin B status as well [55,56,57]. For example, Van der Gaag et al. [55] showed that type-dependent alcohol had no effect on vitamin B12, but a fall in folate with spirits consumption and an increase in vitamin B6 with all alcohol types were observed. In contrast, Laufer et al. [56] only showed an effect of ethanol on vitamin B12, with no effect on vitamin B9. However, in another study, Beulens et al. [57] showed that beer drinking raised vitamin B6 and appeared to reduce vitamin B12 levels while having no effect on vitamin B9 levels. In this regard, Laufer et al. [56] noted that a lack of vitamins and alcohol use may interact to deplete vitamin B9 and vitamin B12 status and that if nutritional intake matches recommended levels, a decreasing impact of alcohol on vitamin B9 may not be detected. However, further studies are required to clarify the relationship between alcohol consumption and the intake of vitamin B to be able to provide nutritional management strategies for chronic liver disease.
5. Vitamin C
One of the many risk factors for vitamin C (including the three forms of vitamin C) and E insufficiency is excessive alcohol intake [58,59]. Vitamin C and E levels are decreased in alcoholics [60]. When compared to those who do not consume alcohol, urine ascorbic acid excretion increased by 47% after acute alcohol consumption of up to 0.58 g ethanol/kg body weight [61]. In effect, pretreatment with vitamin C (doses of 5 g, 1000 mg five times daily for two weeks) significantly improved blood ethanol elimination [62] whereas pretreatment with vitamin C (doses of 2 g, 500 mg four times daily for two weeks) significantly improved alcohol elimination in plasma in the short and long term, implying that vitamin C plays a role in ethanol oxidation [63]. Furthermore, short-term intravenous vitamin C therapy (500 mg/day for five days) significantly improved serum vitamin C levels in chronic alcoholics with hypovitaminosis C [64]. Despite these findings, a previous study indicated that chronic drinkers’ blood levels can take up to three months to restore to normal after taking oral vitamin C supplements [65,66].
Hepatocytes metabolize around 90% of ethanol, which is transformed to acetaldehyde by the enzyme ADH. Once the ADH has exhausted its ability to metabolize alcohol, cytochrome P450 isoenzymes take over and convert the molecule to acetaldehyde [67]. This has been found in tissues, including the liver and brain, that have poor ADH activity. By acting as an electron donor and, thereby, unleashing the NAD/NADH pathway, vitamin C is theorized to speed up alcohol metabolism [68]. A positive relationship between ADH activity and leukocyte ascorbic acid concentration has been discovered in people with liver disease [69]. Furthermore, the acetaldehyde produced has been associated with ethanol-induced hepatotoxicity [70,71], and when paired with hepatic CYP2E1 activation, these factors enhance oxidative stress in hepatocytes [12,33,72,73]. On the other hand, vitamin C has been demonstrated to protect against the detrimental effects of acetaldehyde in animal experiments [74]. Given the function of acetaldehyde in the brain’s dopaminergic stimulation of opiate receptors, this could reduce hepatotoxicity and possibly the biochemical basis of addiction [64].
6. Vitamin D
Calcium homeostasis and bone metabolism require vitamin D to function properly [75]. It is well known for its role in immune response control as well as its anticancer activities [76,77]. Vitamin D deficiency, less than 50 nmol/L of 25-hydroxy vitamin D (25(OH)D) is increasingly being recognized as a global public health issue [78]. According to published studies, the activities and functions of important vitamins and minerals including vitamin B9 and vitamins D, C and E are impaired by chronic ethanol consumption [51,79]. In effect, chronic alcohol consumption has been demonstrated to lower vitamin D levels (inactive vitamin D (25(OH)D3) and active vitamin D (1,25(OH)2D3) as well as cathelicidin/LL-37 expression [80].
Immune system deficiency, muscle weakness, osteopenia, osteoporosis, severe upper respiratory tract infections, community-acquired pneumonia, and acute respiratory distress syndrome have all been associated with vitamin D deficiency [81,82,83,84,85]. Furthermore, epidemiologic data linking vitamin D insufficiency to autoimmune disorders, such as multiple sclerosis (MS), rheumatoid arthritis (RA), diabetes mellitus (DM), inflammatory bowel disease, and systemic lupus erythematosus (SLE), have been raised [86]. Vitamin D deficiency, in effect, has been found to hasten the course of existing autoimmune disorders [87]. Reduced immunological function and responsiveness can be caused by lower amounts of inactive vitamin D and active vitamin D. As a result, the frequency of community-acquired and bacterial pneumonia has increased among susceptible populations, such as those with alcoholism [88,89]. Furthermore, in a mouse model of alcoholic myopathy, low vitamin D levels were associated with muscle fiber atrophy [90] where changes in muscular antioxidant enzyme levels may play a key role in the alcoholic etiology.
CYP2E1, an enzyme engaged in ethanol metabolism directly or by creating reactive oxidative metabolites, is implicated in ethanol disruption of enzymes involved in vitamin D metabolism [83,91]. The elevated levels of CYP2E1 seen in broncho-alveolar lavage fluid or liver samples of people with alcohol use disorder are likely due to this [80,92].
7. Vitamin E
Antioxidants are necessary for avoiding free radical-induced cellular damage. Vitamin E is a lipid-soluble vitamin that is carried as a component of lipoprotein, and efficiently reduces peroxidation susceptibility both in in vivo and in vitro assays [93,94].
Vitamin E insufficiency has long been linked to ALD [95]. Vitamin E levels in the liver of alcoholics with cirrhosis are frequently low [96]. Vitamin E deficiency, according to earlier research, makes the liver more sensitive to alcohol [97]. In this sense, vitamin E has been demonstrated to have hepatoprotective characteristics in rat models, including membrane stability, reduced nuclear factor-kappa B activation, decreased TNF-α generation, and suppressed hepatic stellate cell activation [12,33,73,95].
There are three histological stages for ALD, and they could be classified into the following: (1) simple steatosis or fatty liver, (2) alcoholic hepatitis (AH), and (3) chronic hepatitis with hepatic fibrosis or cirrhosis [98]. The first-line treatment for severe AH is the administration of corticosteroids [99]. However, some patients with severe AH are refractory to corticosteroids. Nonetheless, Miyashima et al. [100] have reported that vitamin E, as a supplement to corticosteroids therapy, may be a new therapeutic option for these patients.
By raising ROS and lowering endogenous antioxidant levels, alcohol promotes oxidative stress [101]. In this sense, Prakash et al. [102] have demonstrated that prognostic factors, including the Child−Pugh score and the Model for End-Stage Liver Disease (MELD) score, increased significantly, demonstrating that vitamin E treatment improves short-term mortality more than long-term mortality. In addition, Kaur et al. [103] studied examined vitamin E supplementation in ethanol-treated mice and found that it restored redox state, decreased apoptosis, and lowered oxidative stress markers. However, as compared to the placebo, 1000 IU of vitamin E per day improved serum hyaluronic acid but had no favorable impact on liver function tests or mortality in individuals with mild to severe alcoholic hepatitis [104].
8. Possible Mechanisms of Action for Vitamins
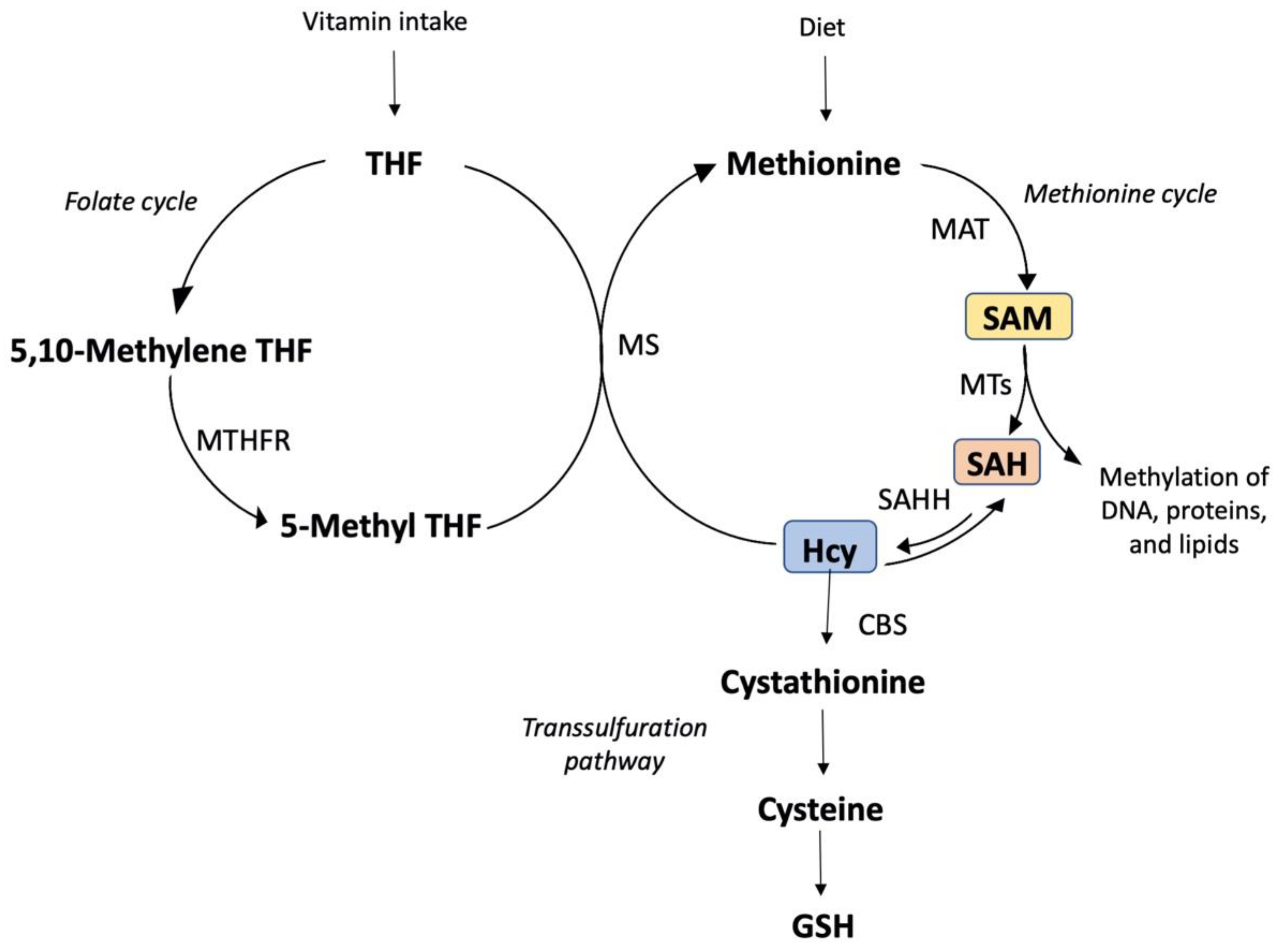
Due to ROS being formed naturally, cells have evolved several enzymatic and nonenzymatic ways to protect them [105,106]. In effect, ethanol or its derivatives impairs several of these defensive mechanisms, which could change the redox status, causing the antioxidant cell defenses to be compromised [107]. Nonenzymatic barriers, such as GSH and vitamins, play a key role in several cellular processes. Reduced glutathione (GSH) and vitamins are probably the most important nonenzymatic antioxidants and participate in a wide range of cellular functions. Furthermore, internal redox buffers, such as Hcy, cysteine (Cys), and cysteinyl glycine (CysGly), play an important role in the extracellular redox system [108,109]. Chronic alcohol intake produces altered Hcy metabolism, which leads to fat storage, inflammation, and hepatocyte damage [110,111]. Hyperhomocysteinemia induced by ethanol and linked to oxidative endoplasmic reticulum stress triggers apoptosis and increases lipid production [112].
Previous research has linked alterations in methionine metabolism to ethanol-induced alcoholic liver damage [113,114,115]. In animals and humans, chronic ethanol abuse reduces plasma levels of vitamins such as vitamin B9 and hepatic levels of SAMe [116] and raises plasma Hcy and hepatic S-adenosylhomocysteine (SAH) concentrations [110,114,115].
There were also associations between both vitamin C and vitamin B9 [117,118] while the molecular basis is unknown. Vitamin B9 is required for the transformation of Hcy into methionine as well as the generation of deoxythymidine monophosphate (dTMP) from deoxyuridine monophosphate (dUMP) [119]. Even though vitamin C consumption has been shown to raise circulation levels of vitamin B9 and lower Hcy levels [118,120,121], the relationship between them remains unknown. Figure 3 summarizes the vitamins and their possible mechanisms of action against the liver injury caused by alcohol consumption.
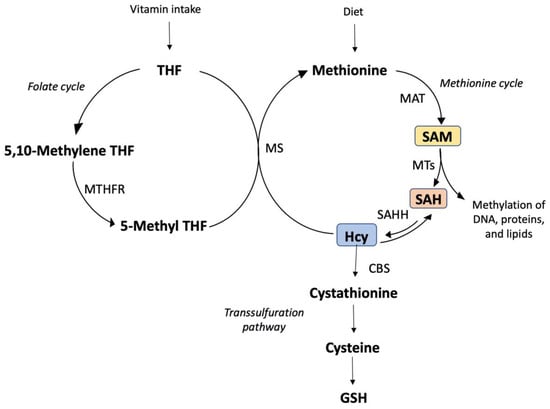
Figure 3.
Vitamins and their possible mechanisms of action against the liver injury caused by al-cohol consumption. Tetrahydrofolate (THF), 5,10-methylenetetrahydrofolate (5,10-Methylene THF), methylenetetrahydrofolate reductase (MTHFR), and 5-methyltetrahydrofolate (5-Methyl THF), the initial methyl donor for transmethylation processes, are all involved in vitamin metabolism. 5-Methyl THF and homocysteine (Hcy) are substrates for methionine synthase (MS) in the synthesis of methionine, which is converted to S-adenosylmethionine (SAM) by methionine adenosyltransferase (MAT) in transmethylation processes. S-adenosylhomocysteine (SAH) is a product and inhibitor of methyltransferase reaction (MTs) as well as a substrate for the bidirectional enzyme SAH hydrolase (SAHH), which creates homocysteine or SAH when SAH is in excess. Hcy is metabolized by cystathionine beta-synthase (CBS) and cystathionase to produce cysteine and glutathione (GSH) in transsulfuration processes. It is also important to note that SAM inhibits MTHFR while promoting CBS expression. As a result, a SAM shortage boosts 5-Methyl THF production while lowering 5,10-Methyl THF and GSH production.
9. Conclusions
The WHO guidelines for withdrawal state the use of multivitamin supplements [122] while another international guideline, published by the World Federation of Societies of Biological Psychiatry, makes mention of the state of hypovitaminosis in the alcoholic but makes no mention of vitamins or their replacement [123].
These antioxidants probably execute their effects through their ability to eliminate reactive oxygen species. However, there is still mixed evidence on the effect of dietary nutrients on the severity of chronic alcohol intake. While the current findings suggest that taking fiber-rich food, consuming water, or eating fat-rich meals could reduce the severity of alcohol hangovers, the last studies have supported the used of vitamins and antioxidants against oxidative alcohol damage. Therefore, new studies are required to elucidate cellular and molecular pathways involved, the mechanisms of action, and the histopathological changes produced after vitamin supplementation.
10. Perspectives
Our review updates the existing relationship between vitamins and their mechanism of action during the pathogenesis of ALD. From this viewpoint, we can see that while vitamins perform an important role in the prevention of alcoholic liver disease, other aspects, such as the amount of alcohol consumed, time of exposure (acute or chronic), administration route (oral or intravenous), and administration pre- or post-alcohol drinking, should all be considered when evaluating the effectiveness of vitamin supplementation. Therefore, these variables should be addressed in future studies.
Author Contributions
C.S. conceived of the presented idea. C.S., J.F., M.Z. and C.H. conducted the database research and wrote the paper. C.S. and J.F. drew the figures and flow gram. C.S. and C.H. edited the paper. C.S. supervised the project. All authors have read and agreed to the published version of the manuscript.
Funding
DIUFRO No DI22-0007 Project, Universidad de La Frontera.
Acknowledgments
We acknowledge the support and advice given by Mario Rivera Meza from Departamento de Ciencias Químicas y Farmacéuticas, Universidad de Chile.
Conflicts of Interest
The authors declare no conflict of interest.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Publishing: Washington, DC, USA, 2013. [Google Scholar]
- Swift, R.M. Drug therapy for alcohol dependence. N. Engl. J. Med. 1999, 340, 1482–1490. [Google Scholar] [CrossRef] [PubMed]
- Costanzo, S.; di Castelnuovo, A.; Donati, M.B.; Iacoviello, L.; de Gaetano, G. Alcohol consumption and mortality in patients with cardiovascular disease a meta-analysis. J. Am. Coll. Cardiol. 2010, 55, 1339–1347. [Google Scholar] [CrossRef]
- Fernandez-Sola, J. Cardiovascular risks and benefits of moderate and heavy alcohol consumption. Nat. Rev. Cardiol. 2015, 12, 576–587. [Google Scholar] [CrossRef]
- Lippi, G.; Mattiuzzi, C.; Franchini, M. Alcohol consumption and venous thromboembolism: Friend or foe? Intern. Emerg. Med. 2015, 10, 907–913. [Google Scholar] [CrossRef] [PubMed]
- Larsson, S.C.; Drca, N.; Wolk, A. Alcohol consumption and risk of atrial fibrillation a prospective study and dose-response meta-analysis. J. Am. Coll. Cardiol. 2014, 64, 282–289. [Google Scholar] [CrossRef] [PubMed]
- Holmes, M.V.; Dale, C.E.; Zuccolo, L.; Silverwood, R.J.; Guo, Y.; Ye, Z.; Prieto-Merino, D.; Dehghan, A.; Trompet, S.; Wong, A.; et al. Association between alcohol and cardiovascular disease: Mendelian randomisation analysis based on individual participant data. BMJ 2014, 349, g4164. [Google Scholar] [CrossRef] [PubMed]
- Substance Abuse and Mental Health Data Archive (SAMHSA). National Survey on Drug Use and Health (NSDUH); Department of Health and Human Services: Washington, DC, USA, 2019.
- Haber, P.S.; Apte, M.V.; Moran, C.; Applegate, T.L.; Pirola, R.C.; Korsten, M.A.; McCaughan, G.W.; Wilson, J.S. Non-oxidative metabolism of ethanol by rat pancreatic acini. Pancreatology 2004, 4, 82–89. [Google Scholar] [CrossRef]
- Brust, J.C.M. Ethanol and cognition: Indirect effects, neurotoxicity and neuroprotection: A review. Int. J. Environ. Res. Public Health. 2010, 7, 1540–1557. [Google Scholar] [CrossRef]
- World Health Organization. Alcohol. Descriptive Note N° 349; World Health Organization: New York, NY, USA, 2011. [Google Scholar]
- Sandoval, C.; Vásquez, B.; Mandarim-de-Lacerda, C.; del Sol, M. Ethanol intake and toxicity: In search of new treatments. Int. J. Morphol. 2017, 35, 942–949. [Google Scholar] [CrossRef]
- García Gutiérrez, E.; Lima Mompó, G.; Aldana Vilas, L.; Casanova Carrillo, P.; Feliciano Álvarez, V. Alcoholismo y sociedad, tendencias actuales. Rev. Cuba. Med. Mil. 2004, 33, 1–10. [Google Scholar]
- Arias, D.R. Reacciones fisiológicas y neuroquímicas del alcoholismo. Diversitas 2005, 1, 138–147. [Google Scholar] [CrossRef]
- Lakshman, R.; Cederbaum, A.I.; Hoek, J.B.; Konishi, M.; Koop, D.; Donohue, T.M. Use of CYP2E1-transfected human liver cell lines in elucidating the actions of ethanol. Alcohol Clin. Exp. Res. 2006, 29, 1726–1734. [Google Scholar] [CrossRef] [PubMed]
- Setshedi, M.; Wands, J.R.; Monte, S.M. Acetaldehyde adducts in alcoholic liver disease. Oxid. Med. Cell Longev. 2010, 3, 178–185. [Google Scholar] [CrossRef] [PubMed]
- Robinson, K.E.; Shah, V.H. Pathogenesis and pathways: Nonalcoholic fatty liver disease & alcoholic liver disease. Transl. Gastroenterol. Hepatol. 2020, 5, 49. [Google Scholar] [PubMed]
- Cederbaum, A.I. Alcohol metabolism. Clin. Liver Dis. 2012, 16, 667–685. [Google Scholar] [CrossRef]
- Zima, T.; Kalousová, M. Oxidative stress and signal transduction pathways in alcoholic liver disease. Alcohol Clin. Exp. Res. 2005, 29, 110S–115S. [Google Scholar] [CrossRef]
- Dunn, W.; Shah, V.H. Pathogenesis of Alcoholic Liver Disease. Clin. Liver Dis. 2016, 20, 445–456. [Google Scholar] [CrossRef]
- Peeraphatdit, T.B.; Kamath, P.S.; Karpyak, V.M.; Davis, B.; Desai, V.; Liangpunsakul, S.; Sanyal, A.; Chalasani, N.; Shah, V.H.; Simonetto, D.A. Alcohol Rehabilitation Within 30 Days of Hospital Discharge is Associated with Reduced Readmission, Relapse, and Death in Patients with Alcoholic Hepatitis. Clin. Gastroenterol Hepatol. 2019, 18, 477–485. [Google Scholar] [CrossRef]
- Wu, H.; Cai, P.; Clemens, D.L.; Jerrells, T.R.; Shakeel Ansari, G.A.; Kaphalia, B.S. Metabolic basis of ethanol-induced cytotoxicity in recombinant HepG2 Cells: Role of nonoxidative metabolism. Toxicol. Appl. Pharmacol. 2006, 216, 238–247. [Google Scholar] [CrossRef]
- Lu, Y.; Cederbaum, A.I. CYP2E1 and oxidative liver injury by alcohol. Free Rad. Biol. Med. 2008, 44, 723–738. [Google Scholar] [CrossRef]
- Carrasco, C.; Carrasco, C.; Souza-Mello, V.; Sandoval, C. Effectiveness of antioxidant treatments on cytochrome P450 2E1 (CYP2E1) activity after alcohol exposure in humans and in vitro models: A systematic review. Int. J. Food Prop. 2021, 24, 1300–1317. [Google Scholar] [CrossRef]
- Yang, Z.; Klionsky, D.J. Eaten alive: A history of macroautophagy. Nat. Cell Biol. 2010, 12, 814–822. [Google Scholar] [CrossRef] [PubMed]
- Bailey, S.M.; Cunningham, C.C. Contribution of mitochondria to oxidative stress associated with alcoholic liver disease. Free Rad. Biol. Med. 2002, 32, 11–16. [Google Scholar] [CrossRef]
- Hoek, J.B.; Cahill, A.; Pastorino, J.G. Alcohol and mitochondria: A dysfunctional relationship. Gastroenterology 2002, 122, 2049–2063. [Google Scholar] [CrossRef] [PubMed]
- Tuma, D.J.; Casey, C.A. Dangerous byproducts of alcohol breakdown: Focus on adducts. Alcohol Res. Health 2003, 27, 285–290. [Google Scholar] [PubMed]
- Schattenberg, J.M.; Czaja, M.J. Regulation of the effects of CYP2E1-induced oxidative stress by JNK signaling. Redox Biol. 2014, 3, 7–15. [Google Scholar] [CrossRef] [PubMed]
- Diesinger, T.; Buko, V.; Lautwein, A.; Dvorsky, R.; Belonovskaya, E.; Lukivskaya, O.; Naruta, E.; Kirko, S.; Andreev, V.; Buckert, D.; et al. Drug targeting CYP2E1 for the treatment of early-stage alcoholic steatohepatitis. PLoS ONE 2020, 15, e0235990. [Google Scholar] [CrossRef]
- Zelko, I.N.; Mariani, T.J.; Folz, R.J. Superoxide dismutase multigene family: A comparison of the CuZn-SOD (SOD1), Mn-SOD (SOD2), and EC-SOD (SOD3) gene structures, evolution, and expression. Free Rad. Biol. Med. 2002, 33, 337–349. [Google Scholar] [CrossRef]
- Chang, P.; Cheng, E.; Brooke, S.; Sapolsky, R. Marked differences in the efficacy of post-insult gene therapy with catalase versus glutathione peroxidase. Brain Res. 2005, 1063, 27–31. [Google Scholar] [CrossRef]
- Sandoval, C.; Vásquez, B.; Souza-Mello, V.; Adeli, K.; Mandarim-de-Lacerda, C.; del Sol, M. Morphoquantitative effects of oral b-carotene supplementation on liver of C57BL/6 mice exposed to ethanol consumption. Int. J. Clin. Exp. Pathol. 2019, 12, 1713–1722. [Google Scholar]
- Sandoval, C.; Vásquez, B.; Vasconcellos, A.; Souza-Mello, V.; Adeli, K.; Mandarim-de-Lacerda, C.; del Sol, M. Oral supplementation of b-carotene benefits the hepatic structure and metabolism in mice exposed to chronic ethanol consumption. Sains Malays. 2022, 51, 285–296. [Google Scholar] [CrossRef]
- Nieto, N.; Friedman, S.L.; Cederbaum, A.I. Cytochrome P450 2E1-derived reactive oxygen species mediate paracrine stimulation of collagen I protein synthesis by hepatic stellate cells. J. Biol. Chem. 2002, 277, 9853–9864. [Google Scholar] [CrossRef] [PubMed]
- Nieto, N. Ethanol and fish oil induce NFkappaB transactivation of the collagen alpha2(I) promoter through lipid peroxidation-driven activation of the PKC-PI3K-Akt pathway. Hepatology 2007, 45, 1433–1445. [Google Scholar] [CrossRef] [PubMed]
- Schott, M.B.; Rasineni, K.; Weller, S.G.; Schulze, R.J.; Sletten, A.C.; Casey, C.A.; McNiven, M.A. Œ≤-Adrenergic induction of lipolysis in hepatocytes is inhibited by ethanol exposure. J. Biol. Chem. 2017, 292, 11815–11828. [Google Scholar] [CrossRef]
- Werling, K. A májbetegségek kialakulásának új szempontjai—különös tekintettel az autophagiára és a mikro-RNS szerepére. Orvosi Hetilap. 2020, 161, 1449–1455. [Google Scholar] [CrossRef]
- Levine, M.; Conry-Cantilena, C.; Wang, Y.; Welch, R.W.; Washko, P.W.; Dhariwal, K.R.; Park, J.B.; Lazarev, A.; Graumlich, J.F.; King, J.; et al. Vitamin C pharmacokinetics in healthy volunteers: Evidence for a recommended dietary allowance. Proc. Natl. Acad. Sci. USA 1996, 93, 3704–3709. [Google Scholar] [CrossRef]
- Young, V.R. Evidence for a recommended dietary allowance for vitamin C from pharmacokinetics: A comment and analysis. Proc. Natl. Acad. Sci. USA 1996, 93, 14344–14348. [Google Scholar] [CrossRef]
- Kauwell, G.P.A.; Wilsky, C.E.; Cerda, J.J.; Herrlinger-Garcia, K.; Hutson, A.D.; Theriaque, D.W.; Boddie, A.; Rampersaud, G.C.; Bailey, L.B. Methylenetetrahydrofolate reductase mutation (677C→T) negatively influences plasma homocysteine response to marginal folate intake in elderly women. Metab. Clin. Exp. 2000, 49, 1440–1443. [Google Scholar] [CrossRef]
- Shibata, K.; Fukuwatari, T.; Ohta, M.; Okamoto, H.; Watanabe, T.; Fukui, T.; Nishimuta, M.; Totani, M.; Kimura, M.; Ohishi, N.; et al. Values of water-soluble vitamins in blood and urine of Japanese young men and women consuming a semi-purified diet based on the Japanese dietary reference intakes. J. Nutr. Sci. Vitaminol. 2005, 51, 319–328. [Google Scholar] [CrossRef]
- Shibata, K.; Fukuwatari, T.; Watanabe, T.; Nishimuta, M. Intra- and inter-individual variations of blood and urinary water-soluble vitamins in japanese young adults consuming a semi-purified diet for 7 days. J. Nutr. Sci. Vitaminol. 2009, 55, 459–470. [Google Scholar] [CrossRef]
- Bailey, L.B. Folic acid. In Handbook of Vitamins, 4th ed.; Zempleni, J., Rucker, R.B., McCormick, D.B., Suttie, J.W., Eds.; CRC Press: Boca Raton, FL, USA, 2007. [Google Scholar]
- Caudill, M.A. Folate bioavailability: Implications for establishing dietary recommendations and optimizing status. Am. J. Clin. Nutr. 2009, 91, 1455S–1460S. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, E.S.; Conus, N.; Kaput, J. B vitamin polymorphisms and behavior: Evidence of associations with neurodevelopment, depression, schizophrenia, bipolar disorder and cognitive decline. Neurosci. Biobehav. Rev. 2014, 47, 307–320. [Google Scholar] [CrossRef] [PubMed]
- Kerns, J.C.; Arundel, C.; Chawla, L.S. Thiamin deficiency in people with obesity. Adv. Nutr. Int. Rev. J. 2015, 6, 147–153. [Google Scholar] [CrossRef] [PubMed]
- Bianchi, G.; Marzocchi, R.; Lorusso, C.; Ridolfi, V.; Marchesini, G. Nutritional treatment of chronic liver failure. Hepatol Res. 2008, 38 (Suppl. 1), S93–S101. [Google Scholar] [CrossRef]
- Amodio, P.; Bemeur, C.; Butterworth, R.; Cordoba, J.; Kato, A.; Montagnese, S.; Uribe, M.; Vilstrup, H.; Morgan, M.Y. The nutritional management of hepatic encephalopathy in patients with cirrhosis: International Society for Hepatic Encephalopathy and Nitrogen Metabolism Consensus. Hepatology 2013, 58, 325–336. [Google Scholar] [CrossRef]
- Roongpisuthipong, C.; Sobhonslidsuk, A.; Nantiruj, K.; Songchitsomboon, S. Nutritional assessment in various stages of liver cirrhosis. Nutrition 2001, 17, 761–765. [Google Scholar] [CrossRef]
- Leevy, C.M.; Moroianu, S.A. Nutritional aspects of alcoholic liver disease. Clin. Liver Dis. 2005, 9, 67–81. [Google Scholar] [CrossRef]
- Cylwik, B.; Czygier, M.; Daniluk, M.; Chrostek, L.; Szmitkowski, M. Vitamin B12 concentration in the blood of alcoholics. Pol. Merkur. Lek. 2010, 28, 122–125. [Google Scholar]
- Muro, N.; Bujanda, L.; Sarasqueta, C. Plasma levels of folate and vitamin B(12) in patients with chronic liver disease. Gastroenterol. Hepatol. 2010, 33, 280–287. [Google Scholar] [CrossRef]
- Gibson, A.; Woodside, J.V.; Young, I.S.; Sharpe, P.C.; Mercer, C.; Patterson, C.C.; Mckinley, M.C.; Kluijtmans, L.A.J.; Whitehead, A.S.; Evans, A. Alcohol increases homocysteine and reduces B vitamin concentration in healthy male volunteers-a randomized, crossover intervention study. QJM 2008, 101, 881–887. [Google Scholar] [CrossRef]
- Van der Gaag, M.S.; Ubbink, J.B.; Sillanaukee, P.; Nikkari, S.; Hendriks, H.F. Effect of consumption of red wine, spirits, and beer on serum homocysteine. Lancet 2000, 355, 1522. [Google Scholar] [CrossRef]
- Laufer, E.M.; Hartman, T.J.; Baer, D.J.; Gunter, E.W.; Dorgan, J.F.; Campbell, W.S.; Clevidence, B.A.; Brown, E.D.; Albanes, D.; Judd, J.T.; et al. Effects of moderate alcohol consumption on folate and vitamin B(12) status in postmenopausal women. Eur. J. Clin. Nutr. 2004, 58, 1518–1524. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Beulens, J.W.; Sierksma, A.; Schaafsma, G.; Kok, F.J.; Struys, E.A.; Jakobs, C.; Hendriks, H.F. Kinetics of homocysteine metabolism after moderate alcohol consumption. Alcohol Clin. Exp. Res. 2005, 29, 739–745. [Google Scholar] [CrossRef]
- Navasumrit, P.; Ward, T.H.; Dodd, N.C.F.; O’Connor, P.J. Ethanol-induced free radicals and hepatic DNA strand breaks are prevented in vivo by antioxidants: Effects of acute and chronic ethanol exposure. Carcinogenesis 2000, 21, 93–99. [Google Scholar] [CrossRef] [PubMed]
- Hercberg, S.; Galan, P.; Preziosi, P.; Bertrais, S.; Mennen, L.; Malvy, D.; Roussel, A.M.; Favier, A.; Briançon, S. The SU.VI.MAX Study: A randomized, placebo-controlled trial of the health effects of antioxidant vitamins and minerals. Arch. Intern. Med. 2004, 164, 2335–2342. [Google Scholar] [CrossRef]
- Suresh, M.V.; Sreeranjit Kumar, C.V.; Lal, J.J.; Indira, M. Impact of massive ascorbic acid supplementation on alcohol induced oxidative stress in guinea pigs. Toxicol. Lett. 1999, 104, 221–229. [Google Scholar] [CrossRef]
- Faizallah, R.; Morris, A.I.; Krasner, N.; Walker, R.J. Alcohol enhances vitamin C excretion in the urine. Alcohol Alcohol. 1986, 21, 81–84. [Google Scholar]
- Susick, R.L.; Zannoni, V.G. Effect of ascorbic acid on the consequences of acute alcohol consumption in humans. Clin. Pharmacol. Ther. 1987, 41, 502–509. [Google Scholar] [CrossRef]
- Chen, M.F.; Boyce, H.W.; Hsu, J.M. Effect of ascorbic acid on plasma alcohol clearance. J. Am. Coll. Nutr. 1990, 9, 185–189. [Google Scholar] [CrossRef]
- Majumdar, S.K.; Patel, S.; Shaw, G.K.; O’Gorman, P.; Thomson, A.D. Vitamin C utilization status in chronic alcoholic patients after short-term intravenous therapy. Int. J. Vitam. Nutr. Res. 1981, 51, 274–278. [Google Scholar]
- Sviripa, E.V. Vitamin C metabolism in alcoholism and alcoholic psychoses. Zh. Nevrol. Psikhiatr. im. S.S. Korsakova 1971, 71, 422–425. [Google Scholar]
- Lim, D.J.; Sharma, Y.; Thompson, C.H. Vitamin C and alcohol: A call to action. BMJ Nutr. Prev. Health 2018, 1, 17–22. [Google Scholar] [CrossRef] [PubMed]
- Hansson, T.; Tindberg, N.; Ingelman-Sundberg, M.; Köhler, C. Regional distribution of ethanol-inducible cytochrome P450 IIE1 in the rat central nervous system. Neuroscience 1990, 34, 451–463. [Google Scholar] [CrossRef]
- Dow, J.; Goldberg, A. Ethanol metabolism in the vitamin C deficient guinea-pig. Biochem. Pharmacol. 1975, 24, 863–866. [Google Scholar] [CrossRef]
- Dow, J.; Krasner, N.; Goldberg, A. Relationship between hepatic alcohol dehydrogenase activity and the ascorbic acid in leucocytes of patients with liver disease. Clin. Sci. Mol. Med. 1975, 49, 603–608. [Google Scholar]
- Ghorbani, Z.; Hajizadeh, M.; Hekmatdoost, A. Dietary supplementation in patients with alcoholic liver disease: A review on current evidence. Hepatobiliary Pancreat. Dis. Int. 2016, 15, 348–360. [Google Scholar] [CrossRef]
- Fuster, D.; Samet, J.H. Alcohol use in patients with chronic liver disease. N. Engl. J. Med. 2018, 379, 1251–1261. [Google Scholar] [CrossRef]
- Abhilash, P.A.; Harikrishnan, R.; Indira, M. Ascorbic acid supplementation down- regulates the alcohol induced oxidative stress, hepatic stellate cell activation, cytotoxicity and mRNA levels of selected fibrotic genes in guinea pigs. Free Radic. Res. 2012, 46, 204–213. [Google Scholar] [CrossRef]
- Sandoval, C.; Vásquez, B.; Souza-Mello, V.; Mandarim-de-Lacerda, C.A.; del Sol, M. Rol del consumo de alcohol y antioxidantes sobre la metilación global del ADN y cáncer. Int. J. Morphol. 2018, 36, 367–372. [Google Scholar] [CrossRef]
- Sprince, H.; Parker, C.M.; Smith, G.G. L-Ascorbic Acid in Alcoholism and Smoking: Protection against Acetaldehyde Toxicity as an Experimental model. Int. J. Vitam. Nutr. Res. 1977, 47, 185–217. [Google Scholar]
- Veldurthy, V.; Wei, R.; Oz, L.; Dhawan, P.; Jeon, Y.H.; Christakos, S. Vitamin D, calcium homeostasis and aging. Bone Res. 2016, 4, 16041. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.C.; Chen, Y.; Liu, W.; Thadhani, R. MicroRNA-mediated mechanism of vitamin D regulation of innate immune response. J. Steroid. Biochem. Mol. Biol. 2014, 144 Pt A, 81–86. [Google Scholar] [CrossRef]
- Jiménez-Sousa, M.A.; Martínez, I.; Medrano, L.M.; Fernández-Rodríguez, A.; Resino, S. Vitamin D in Human Immunodeficiency Virus Infection: Influence on Immunity and Disease. Front. Immunol. 2018, 12, 458. [Google Scholar] [CrossRef] [PubMed]
- Holick, M.F.; Binkley, N.C.; Bischoff-Ferrari, H.A.; Gordon, C.M.; Hanley, D.A.; Heaney, R.P.; Hassan Murad, M.; Weaver, C.M. Evaluation, treatment, and prevention of vitamin D deficiency: An Endocrine Society Clinical Practice Guideline. J. Clin. Endocrinol. Metab. 2011, 96, 1911–1930. [Google Scholar] [CrossRef]
- Kent, J.C.; Devlin, R.D.; Gutteridge, D.H.; Retallack, R.W. Effect of alcohol on renal vitamin D metabolism in chickens. Biochem. Biophys. Res. Commun. 1979, 89, 155–161. [Google Scholar] [CrossRef]
- Ogunsakin, O.; Hottor, T.; Mehta, A.; Lichtveld, M.; McCaskill, M. Chronic Ethanol Exposure Effects on Vitamin D Levels Among Subjects with Alcohol Use Disorder. Environ. Health Insights 2016, 10, 191–199. [Google Scholar] [CrossRef] [PubMed]
- Engs, R.C.; Aldo-Benson, M. The association of alcohol consumption with selfreported illness in university students. Psychol. Rep. 1995, 76, 727–736. [Google Scholar] [CrossRef]
- Fernandez-Sola, J.; Junque, A.; Estruch, R.; Monforte, R.; Torres, A.; Urbano-Marquez, A. High alcohol intake as a risk and prognostic factor for community-acquired pneumonia. Arch. Intern. Med. 1995, 155, 1649–1654. [Google Scholar] [CrossRef]
- McCaskill, M.L.; Hottor, H.T.; Sapkota, M.; Wyatt, T.A. Dietary diallyl disulfide supplementation attenuates ethanol-mediated pulmonary vitamin D speciate depletion in C57Bl/6 mice. BMC Nutr. 2015, 1, 18. [Google Scholar] [CrossRef]
- Wijnia, J.W.; Wielders, J.P.M.; Lips, P.; van de Wiel, A.; Mulder, C.L.; Nieuwenhuis, K.G.A. Is Vitamin D Deficiency a Confounder in Alcoholic Skeletal Muscle Myopathy? Alcohol Clin Exp Res. 2013, 37 (Suppl. 1), E209–E215. [Google Scholar] [CrossRef]
- Tardelli, V.S.; Lago, M.P.P.D.; Silveira, D.X.D.; Fidalgo, T.M. Vitamin D and alcohol: A review of the current literature. Psychiatry Res. 2017, 248, 83–86. [Google Scholar] [CrossRef] [PubMed]
- Adorini, L. Intervention in autoimmunity: The potential of vitamin D receptor agonists. Cell Immunol. 2005, 233, 115–124. [Google Scholar] [CrossRef] [PubMed]
- Zold, E.; Szodoray, P.; Gaal, J.; Kappelmayer, J.; Csathy, L.; Gyimesi, E.; Zeher, M.; Szegedi, G.; Bodolay, E. Vitamin D deficiency in undifferentiated connective tissue disease. Arthritis Res. Ther. 2008, 10, R123. [Google Scholar] [CrossRef] [PubMed]
- White, M.; Mankan, A.; Lawless, M.W.; O’Dwyer, M.J.; McManus, R.; Ryan, T. Mortality in humans with pneumonia and sepsis is related to an uncompensated anti-inflammatory response to infection. Arch Intern Med. 2008, 168, 1468–1469. [Google Scholar] [PubMed]
- Gombart, A.F. The vitamin D-antimicrobial peptide pathway and its role in protection against infection. Future Microbiol. 2009, 4, 1151–1165. [Google Scholar] [CrossRef]
- González-Reimers, E.; Durán-Castellón, M.C.; López-Lirola, A.; Santolaria Fernández, F.; Abreu-González, P.; Alvisa-Negrón, J.; Sánchez-Pérez, M.J. Alcoholic myopathy: Vitamin D deficiency is related to muscle fibre atrophy in a murine model. Alcohol Alcohol. 2010, 45, 223–230. [Google Scholar] [CrossRef][Green Version]
- Niemelä, O.; Parkkila, S.; Pasanen, M.; Viitala, K.; Villanueva, J.A.; Halsted, C.H. Induction of cytochrome P450 enzymes and generation of protein-aldehyde adducts are associated with sex-dependent sensitivity to alcohol-induced liver disease in micropigs. Hepatology 1999, 30, 1011–1017. [Google Scholar] [CrossRef]
- Leung, T.M.; Lu, Y. Alcoholic Liver Disease: From CYP2E1 to CYP2A5. Curr. Mol. Pharmacol. 2017, 10, 172–178. [Google Scholar] [CrossRef]
- Pirozhkov, S.V.; Eskelson, C.D.; Watson, R.R.; Hunter, G.C.; Piotrowski, J.J.; Bernhard, V. Effect of chronic consumption of ethanol and vitamin E on fatty acid composition and lipid peroxidation in rat heart tissue. Alcohol 1992, 9, 329–334. [Google Scholar] [CrossRef]
- Brockes, C.; Buchli, C.; Locher, R.; Koch, J.; Vetter, W. Vitamin E prevents extensive lipid peroxidation in patients with hypertension. Br. J. Biomed. Sci. 2003, 60, 5–8. [Google Scholar] [CrossRef]
- Arteel, G.; Marsano, L.; Mendez, C.; Bentley, F.; McClain, C.J. Advances in alcoholic liver disease. Best Pract. Res. Clin. Gastroenterol. 2003, 17, 625–647. [Google Scholar] [CrossRef]
- Leo, M.A.; Rosman, A.S.; Lieber, C.S. Differential depletion of carotenoids and tocopherol in liver disease. Hepatology 1993, 17, 977–986. [Google Scholar] [PubMed]
- Lieber, C.S. Relationships between nutrition, alcohol use, and liver disease. Alcohol Res. Health 2003, 7, 220–231. [Google Scholar]
- O’Shea, R.S.; Dasarathy, S.; McCullough, A.J. Alcoholic liver disease. Hepatology 2010, 51, 307–328. [Google Scholar] [CrossRef] [PubMed]
- Lucey, M.R.; Mathurin, P.; Morgan, T.R. Alcoholic hepatitis. N. Engl. J. Med. 2009, 360, 2758–2769. [Google Scholar] [CrossRef] [PubMed]
- Miyashima, Y.; Shibata, M.; Honma, Y.; Matsuoka, H.; Hiura, M.; Abe, S.; Harada, M. Severe Alcoholic Hepatitis Effectively Treated with Vitamin E as an Add-on to Corticosteroids. Intern Med. 2017, 56, 3293–3297. [Google Scholar] [CrossRef][Green Version]
- Dey, A.; Cederbaum, A.I. Alcohol and oxidative liver injury. Hepatology 2006, 43, S63–S74. [Google Scholar] [CrossRef]
- Prakash, K.B.; Prasanand, S.; Adithiya, K. Efficacy of Vitamin E supplementation in patients with alcoholic liver disease: An open-label, prospective, randomized comparative study. Int. J. Nutr. Pharmacol. Neurol. Dis. 2016, 6, 101–110. [Google Scholar]
- Kaur, J.; Shalini, S.; Bansal, M.P. Influence of vitamin E on alcohol-induced changes in antioxidant defenses in mice liver. Toxicol. Mech. Methods 2010, 20, 82–89. [Google Scholar] [CrossRef]
- Mezey, E.; Potter, J.J.; Rennie-Tankersley, L.; Caballeria, J.; Pares, A. A randomized placebo-controlled trial of vitamin E for alcoholic hepatitis. J. Hepatol. 2004, 40, 40–46. [Google Scholar] [CrossRef]
- Halliwell, B. Antioxidant defence mechanisms: From the beginning to the end (of the beginning). Free Radic. Res. 1999, 31, 261–272. [Google Scholar] [CrossRef] [PubMed]
- Fernandez-Checa, J.C.; Ookhtens, M.; Kaplowitz, N. Effects of chronic ethanol feeding on rat hepatocytic glutathione. Relationship of cytosolic glutathione to efflux and mitochondrial sequestration. J. Clin. Investig. 1989, 83, 1247–1252. [Google Scholar] [CrossRef] [PubMed]
- Albano, E. Alcohol, oxidative stress and free radical damage. Proc. Nutr. Soc. 2006, 65, 278–290. [Google Scholar] [CrossRef] [PubMed]
- Deneke, S.M. Thiol-based antioxidants. Curr. Top. Cell. Regul. 2000, 36, 151–180. [Google Scholar] [PubMed]
- Munday, R. Toxicity of thiols and disulphides: Involvement of free-radical species. Free Radic. Biol. Med. 1989, 7, 659–673. [Google Scholar] [CrossRef]
- Song, Z.; Zhou, Z.; Chen, T.; Hill, D.; Kang, J.; Barve, S.; McClain, C. S-adenosylmethionine (SAMe) protects against acute alcohol induced hepatotoxicity in mice small star, filled. J. Nutr. Biochem. 2003, 14, 591–597. [Google Scholar] [CrossRef]
- Song, Z.; Zhou, Z.; Deaciuc, I.; Chen, T.; McClain, C.J. Inhibition of adiponectin production by homocysteine: A potential mechanism for alcoholic liver disease. Hepatology 2008, 47, 867–879. [Google Scholar] [CrossRef]
- Ji, C.; Kaplowitz, N. Hyperhomocysteinemia, endoplasmic reticulum stress, and alcoholic liver injury. World J. Gastroenterol. 2004, 10, 1699–1708. [Google Scholar] [CrossRef]
- Barak, A.J.; Beckenhauer, H.C.; Tuma, D.J. S-adenosylmethionine generation and prevention of alcoholic fatty liver by betaine. Alcohol 1994, 11, 501–503. [Google Scholar] [CrossRef]
- Song, Z.; Zhou, Z.; Uriarte, S.; Wang, L.; Kang, Y.J.; Chen, T.; Barve, S.; McClain, C. S-adenosylhomocysteine sensitizes to TNF-alpha hepatotoxicity in mice and liver cells: A possible etiological factor in alcoholic liver disease. Hepatology 2004, 40, 989–997. [Google Scholar] [CrossRef]
- Feo, F.; Pascale, R.; Garcea, R.; Daino, L.; Pirisi, L.; Frassetto, S.; Ruggiu, M.E.; Di Padova, C.; Stramentinoli, G. Effect of the variations of S-adenosyl-L-methionine liver content on fat accumulation and ethanol metabolism in ethanol-intoxicated rats. Toxicol. Appl. Pharmacol. 1986, 83, 331–341. [Google Scholar] [CrossRef]
- Lee, S.J.; Kang, M.H.; Min, H. Folic acid supplementation reduces oxidative stress and hepatic toxicity in rats treated chronically with ethanol. Nutr. Res. Pract. 2011, 5, 520–526. [Google Scholar] [CrossRef] [PubMed]
- Lucock, M.; Yates, Z.; Boyd, L.; Naylor, C.; Choi, J.H.; Ng, X.; Skinner, V.; Wai, R.; Kho, J.; Tang, S.; et al. Vitamin C-related nutrient-nutrient and nutrient-gene interactions that modify folate status. Eur. J. Nutr. 2013, 52, 569–582. [Google Scholar] [CrossRef] [PubMed]
- Cafolla, A.; Dragoni, F.; Girelli, G.; Tosti, M.E.; Costante, A.; De Luca, A.M.; Funaro, D.; Scott, C.S. Effect of folic acid and vitamin C supplementation on folate status and homocysteine level: A randomised controlled trial in Italian smoker-blood donors. Atherosclerosis 2002, 163, 105–111. [Google Scholar] [CrossRef]
- Berg, J.M.; Tymoczko, J.L.; Stryer, L. Biochemistry, 5th ed.; W.H. Freeman and Company: New York, NY, USA, 2001. [Google Scholar]
- Mix, J.A. Do megadoses of vitamin C compromise folic acid’s role in the metabolism of plasma homocysteine? Nutr. Res. 1999, 19, 161–165. [Google Scholar] [CrossRef]
- Alcazar Magana, A.; Reed, R.L.; Koluda, R.; Miranda, C.L.; Maier, C.S.; Stevens, J.F. Vitamin C Activates the Folate-Mediated One-Carbon Cycle in C2C12 Myoblasts. Antioxidants 2020, 9, 217. [Google Scholar] [CrossRef]
- World Health Organization. Clinical Guidelines for Withdrawal Management and Treatment of Drug Dependence in Closed Settings. WHO Guidelines Approved by the Guidelines Review Committee; World Health Organization Press: Geneva, Switzerland, 2009. [Google Scholar]
- Soyka, M.; Kranzler, H.R.; Hesselbrock, V.; Kasper, S.; Mutschler, J.; Möller, H.J.; WFSBP Task Force on Treatment Guidelines for Substance Use Disorders. Guidelines for biological treatment of substance use and related disorders, part 1: Alcoholism, first revision. World J. Biol. Psychiatry 2017, 18, 86–119. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).