Abstract
Biomolecular condensates are membraneless organelles (MLOs) that form dynamic, chemically distinct subcellular compartments organizing macromolecules such as proteins, RNA, and DNA in unicellular prokaryotic bacteria and complex eukaryotic cells. Separated from surrounding environments, MLOs in the nucleoplasm, cytoplasm, and mitochondria assemble by liquid–liquid phase separation (LLPS) into transient, non-static, liquid-like droplets that regulate essential molecular functions. LLPS is primarily controlled by post-translational modifications (PTMs) that fine-tune the balance between attractive and repulsive charge states and/or binding motifs of proteins. Aberrant phase separation due to dysregulated membrane lipid rafts and/or PTMs, as well as the absence of adequate hydrotropic small molecules such as ATP, or the presence of specific RNA proteins can cause pathological protein aggregation in neurodegenerative disorders. Melatonin may exert a dominant influence over phase separation in biomolecular condensates by optimizing membrane and MLO interdependent reactions through stabilizing lipid raft domains, reducing line tension, and maintaining negative membrane curvature and fluidity. As a potent antioxidant, melatonin protects cardiolipin and other membrane lipids from peroxidation cascades, supporting protein trafficking, signaling, ion channel activities, and ATPase functionality during condensate coacervation or dissolution. Melatonin may even control condensate LLPS through PTM and balance mRNA- and RNA-binding protein composition by regulating N6-methyladenosine (m6A) modifications. There is currently a lack of pharmaceuticals targeting neurodegenerative disorders via the regulation of phase separation. The potential of melatonin in the modulation of biomolecular condensate in the attenuation of aberrant condensate aggregation in neurodegenerative disorders is discussed in this review.
1. Introduction
Present in all cells, biomolecular condensates are membraneless organelles (MLOs) containing proteins, ribonucleic acids (RNAs), and other nucleic acids [1]. These micron-scale macromolecules that can assemble into liquid-like droplets have been proposed to be the origin of life [2]. Current cell and molecular biology reveal that liquid–liquid phase separation (LLPS) is the driving force behind the assembly or dissolution of biomolecules in energy-efficient, rapid, essential reactions to changing endogenous or exogenous conditions including stress response [3] and signal transduction [4,5], as well as genome expression, organization, and repair [6]. LLPS creates distinct compartments that enhance or restrict biochemical reactions by enriching or excluding biomolecules from their environment [7]. Increasing evidence associates diseases such as neurodegeneration and cancer with the formation of protein aggregates from dysregulated, aberrant transitions in phase separation [8,9,10,11,12].
Phase separation at its core is a thermodynamic process driven by the reduction or a negative change in global free energy [1,13]. LLPS is entropically unfavorable; therefore, multivalent protein–protein interactions that are energetically favorable may be necessary to offset energetic costs [14]. Adenosine triphosphate (ATP) is the molecule favored by most organisms for capturing and transferring free energy. During hydrolysis, ATP is transformed into adenosine diphosphate (ADP) and inorganic phosphate (Pi). The change in free energy of −7.3 kcal/mol associated with this chemical reaction is used by cells to perform energetically favorable reactions [15], including relevant post-translational modification (PTM) such as phosphorylation [16], ubiquitination [17,18], and SUMOylation that may regulate condensate nucleation, composition, and growth [19,20]. It is understood that most proteins in the human proteome can undergo LLPS, assembling into dense liquid-like, reversible droplets under most physiological conditions [21]. Thermodynamic non-equilibrium processes facilitate the constant exchange of substrates and information that allow these condensates to perform important biological functions [22]. The phase transition of these functionally relevant proteins from their native to droplet states are often mediated and stabilized by ATP-dependent factors such as PTM and RNA. RNAs are critical architectural components that can fine-tune biophysical properties such as viscosity and dynamics in the regulation of spatiotemporal distribution of condensates [23,24].
Mutation, mis-regulated RNA processing, and the altered binding of RNA in MLOs that are enriched with RNA and RNA-binding proteins (RBPs) [25] often result in cytotoxicity and the development of neurodegenerative diseases. Aberrant phase separation leading to the pathological amyloid fibrillation of fused in sarcoma (FUS), TAR DNA-binding protein 43 (TDP-43), tau, and α-synuclein (α-Syn} are now associated with neurodegenerative disorders such as amyotrophic lateral sclerosis (ALS), frontotemporal dementia (FTD), Alzheimer’s disease (AD), and Parkinson’s disorder (PD) [26,27,28,29]. The timely dissolution of pathological amyloid fibrils may be dependent on cellular levels of ATP, which has recently been identified as a biological hydrotrope [30]—an amphiphilic molecule that may behave as a surfactant [31] which can reduce tension between solute and solvent, and increase solubility in an energy-independent manner.
2. ATP Regulates Biomolecular Condensates
At micromolar concentrations in cells, the hydrolysis of ATP phosphoanhydride bonds provides substantial free energy to fuel chemical processes such as post-translational modifications that may maintain fluid phases or facilitate phase separation by generating supersaturation gradients that can induce droplet segregation [13,15,32,33]. At higher physiological concentrations between 2 and 8 mM, ATP becomes a biological hydrotrope that can solubilize proteins to prevent abnormal aggregation and the formation of pathological amyloid fibrils often associated with neurodegenerative disorders such as Alzheimer’s disease (AD) [30]. Recent extensive all-atom molecular dynamics studies showed that at higher millimolar concentrations (150 mM), ATP prevented the aggregation of amyloid-beta peptide Aβ16−22 and disrupted prefibril formations [34], supporting earlier observations of decreased ATP levels in the brain and whole blood of AD transgenic mouse models [35]. Other experimental studies determined that mechanisms such as the suppressed fibrillation of disordered protein by the adenosine moiety of ATP leading to increased protein stability and reduced thermal aggregation may not be typical of hydrotrope-type reactions. Instead, ATP could be viewed as a kosmotropic anion [36] that can increase the solubility of the hydrophobic adenine part [37]; thus, the term “biological aggregation inhibitor” may be more appropriate [38].
Even though ATP is produced mainly in mitochondria, ATP levels in the mitochondrial matrix are significantly lower than those found in the cytoplasm and nucleus [39,40]. Voltage-dependent anion channels (VDACs) located in the mitochondrial outer membrane (MOM) [41] and adenine nucleotide translocators (ANTs) on the inner mitochondrial membranes (IMM) [42,43] facilitate the export of ATP into cytosol where ATP accumulation has been observed to be the highest [44]. The high physiological concentration of ATP in cytoplasm may be used to control the pathological aggregation of macromolecules that coacervate as a result of transient interactions during LLPS in the cytoplasm and nucleus [45,46]. A major hallmark of ALS/FTD is the presence of FUS inclusion in the cytoplasm. FUS are prosurvivor molecules that re-localize from the nucleus to cytoplasm under stress conditions to form reversible, survival-promoting stress granules via LLPS [47,48]. Stress granules contain important ATP-dependent RNA helicases that function as ATPases to hydrolyze ATP during assembly and disassembly [49]. Stress granules could not be formed without the presence of ATP, and the presence of ATP was required to maintain the liquid-like behavior of assembled droplets [32]. A recent in vitro study showed that aggregate disassembly is also an ATP-dependent process.
During metabolic stress such as nutrient deprivation that causes ATP depletion, cells compartmentalize and sequester misfolded proteins into stress granules to protect cellular fitness. Budding yeast subjected to 0.02% glucose starvation showed a 5-fold ATP decline to ~1.1 mM within 10 min, accompanied by a ~4.4-fold increase in median aggregate diameter, whereas the addition of glucose restored ATP levels, quickly reducing aggregate size and abundance back to control values [50]. Mutants with abolished ATP hydrolysis failed to dissolve aggregates even when placed back in 2% glucose solutions after starvation [50]. In the same manner, ATP has been shown to enhance the LLPS of FUS at low concentrations but dissolves FUS aggregates at higher concentrations [51]. Moreover, 8 mM of ATP complexed with Mg2+ ions prevented the LLPS of FUS and dissolved previously formed FUS condensates [30]. The presence of ATP facilitates the essential phase transition of FUS into stress granule droplets, yet prevents further transition into irreversible aggregation and the fibrillation of FUS to cause cytotoxicity by binding to the RNA-recognition motif (RRM) domain of FUS, kinetically inhibiting the fibrillization of FUS [52]. Similarly, through binding to arginine-containing domains in TDP-43, ATP altered physicochemical properties to induce LLPS, causing droplet formation at molar ratios as low as 1:100 (protein to ATP); by contrast, increasing ATP concentrations could reduce droplet formation, with TDP-43 droplets completely dissolving at a molar ratio of 1:1000 [53]. Nevertheless, in order to completely dissolve the amyloid-beta peptide Aβ-42 associated with AD, supraphysiological concentrations of ATP in excess of 100 mM were found to be necessary [30].
Tau is the major constituent of fibrillar tangles in AD. Phase-separated tau forms droplets that serve as intermediates toward aggregation [29]. Physiological concentrations of ATP at 0.1–10 mM enhanced the fibrillation of 10 μM tau K18 (equivalent to 10–1000-fold molar ratio) by accelerating aggregation in a concentration-dependent manner [54] through energy-independent binding to tau proteins [55]. It may seem paradoxical that ATP would enhance the formation of amyloids and prions that are associated with diseases. As a matter of fact, prion-like mechanisms are functional biological processes ubiquitously present from bacteria to humans [56]. The nucleation and growth of amyloid fibrils in FUS, TDP-43, tau and α-synuclein are dependent upon intermolecular interactions of intrinsically disordered regions (IDRs) and proteins (IDPs) such as prion-like domains and low-complexity sequence domains [57].
Proteins that undergo LLPS often contain long segments that are intrinsically disordered and lack well-defined three-dimensional structure [58]. The relatively low concentration of hydrophobic amino acids in IDPs enables the rapid exchange between multiple conformations where condensates form without altering the affinity of binding interactions during LLPS [59,60,61]. Although the formation of biomolecular condensates can potentially accelerate amyloid aggregation, condensates can also inhibit fibril formation by the sequestration of aggregation-prone, prion-like IDPs. Biomolecular condensates derived from proteins associated with the formation of processing bodies (P-bodies) prevented aberrant amyloid aggregation despite local increase in concentration of aggregate-prone proteins [62].
P-bodies are conserved eukaryotic cytoplasmic ribonucleoprotein (RNP) membraneless organelles that regulate protein homeostasis in non-stressed cells through LLPS involving messenger RNAs (mRNAs) and low-complexity sequence domains [63,64,65,66]. P-bodies respond to cellular stress, especially DNA replication stress, by increasing their sizes and numbers [67,68]. The disassembly of P-bodies in yeast is an ATP-dependent process involving ATP hydrolysis by DEAD-box ATPases [69]. The formation of P-bodies is dependent upon RNA and non-translating mRNAs [67]; therefore, it is not surprising to find P-bodies located very close to endoplasmic reticulum (ER) membranes [70] enriched with membrane-associated mRNAs [71,72,73]. Native tau proteins are stable, highly soluble, and resistant to aggregation. When these intrinsically disordered proteins interact with anionic lipid monolayers in plasma membranes, they will undergo LLPS, transitioning from a disordered monomeric state to a pathogenic fibrillar state [74,75]. Phase-separated tau easily aggregates to form highly ordered β-sheets often associated with neurodegeneration [76,77]. The dynamic crosstalk between membranes and membraneless organelles highlights important features critical to the functions and maintenance of biomolecular condensates in health and disease [78,79].
3. The Interdependence between Membranes and Membraneless Organelles
Efficient cellular compartmentalization with or without membranes is indispensable for organic and prebiotic inorganic life [80,81]. There exists a tight interdependence between membranes and MLOs. Since its first discovery in the 1830s, MLOs have been found not only in the nucleus and cytoplasm, but on the membranes of almost all eukaryotic cells [82]. In eukaryotes, lipid bilayer plasma membranes form dynamic trafficking networks with the elaborate endomembrane systems comprising membrane-bound organelles such as the endoplasmic reticulum, Golgi apparatus, endosomes and lysosomes [80,83]. However, exact mechanisms that regulate signaling events and control cargo protein movements within this complex membrane network are not fully understood [84,85]. MLOs formed at membrane surfaces may regulate receptor/transmembrane protein signaling by increasing protein binding affinity and modulating local environments [86]. Recent discoveries revealed that the cluster stoichiometry of condensates formed at plasma membranes could fine-tune signaling proteins such as Ras by increasing dwell time to facilitate kinetic proofreading receptor-mediated activation [87,88]. Conversely, membranes are major regulatory platforms for LLPS due to their ability to concentrate and change protein thresholds during phase separation [79]. Membrane surfaces acted as catalytic sites where alterations in membrane fluidity and lipid composition increased Aβ-42 peptide aggregation and facilitated the binding and internalization of pathogenic amyloid fibrils [89]. β-amyloid peptide (Aβ) featured in AD are derived from amyloid precursor proteins (APPs) where APP cleavage by β-secretase or α-secretase will initiate the amyloidogenic or nonamyloidogenic processing of APP, respectively [90]. Conversely, alterations in membrane fluidity from lipid composition fluctuations such as the reduction in cholesterol and increased membrane fluidity induced nonamyloidogenic APP cleavage by α-secretase [91]. The two distinct pools of APP cleaved by α- and β-secretase that were discovered to exist outside and inside of lipid rafts, respectively [90], may be the result of interactions between lipid rafts and biomolecular condensates.
3.1. Lipid Rafts and Biomolecular Condensates in Health and Disease
Since K. Simons first presented the concept of lipid rafts in 1997 as clusterings of sphingolipids and cholesterol-forming mobile microdomain platforms responsible for signal transduction and protein transport [92], these phase-separated regions in lipid bilayers have been associated with relevant biological functions, including signal transduction [93], trafficking, and the sorting of proteins and lipids [94,95]. Lipid raft signaling is implicated in the pathogenesis of numerous diseases [96], including neurodegenerative disorders [90,97], cardiovascular disease [98], prion disease [99,100], systemic lupus erythematosus [101], viral replication [102], and tumorigenesis [103]. Numerous cancer-related proteins that may be involved in migration, invasion, and metastasis are localized in lipid rafts, understood to be signaling hubs for these proteins [104,105,106]. Gene transcription has been shown to be regulated by biomolecular condensates [107,108,109]; therefore, the recent association of mutations in cancer-related genes with aberrant phase-separated biomolecular condensates [10,110] emphasizes essential relationships between membranes, lipid rafts, and ATP that may not be fully elucidated.
Membrane surfaces offer many advantages in the formation of condensates such as increased pi–pi and cation–pi interactions imposed by geometrical constraints on a two-dimensional flat surface [111], which can reduce the requirements for critical the concentration of molecules necessary for phase separation [112] and enhance biochemical reactions that may take place within biomolecular condensates [113]. Many MLOs form near lipid membrane surfaces because they may rely on lipid-anchored proteins, including H-ras [87,114] which are often found in lipid rafts, for spontaneous thermodynamic phase separation into distinct domains [5,115]. Lipid rafts may enhance phase separation; lipid-driven phase separation within lipid rafts has been demonstrated to dynamically interact with the phase separation of membrane-anchored proteins, resulting in combined effects that change the final phase separation outcome of both systems while enhancing protein-driven phase separation [116]. Indeed, the formation of linker for activation of T cells (LAT) condensates on membrane surfaces induced lipid phase separation into distinct liquid-ordered (Lo) lipid raft domains [117]. To remain in functional states, bimolecular condensates may require energy to support the continuous active restructuring and rearrangement of molecular components. Insufficient or the depletion of ATP can directly impact the physical and functional properties of biomolecular condensates [32,33,79,118].
3.2. Non-Mitochondrial Dimerized ATP Synthase and ATPase Are Localized in High-Curvature Lipid Rafts/Caveolae
First isolated in 1960 [119,120], F1F0 ATP synthases are found localized in the inner membrane invaginations of mitochondria [121]. Eukaryotes and prokaryotes use four major types of ATPases localized in cell membranes to release energy during hydrolysis of ATP for the maintenance of critical transmembrane ionic electrochemical potential differences [122]. In the ubiquitous intracellular powerhouses of eukaryotes, F1F0 ATP synthase is complex V of the electron transport chain responsible for chemiosmotic oxidative phosphorylation (OXPHOS) that couples ATP synthesis to the inner membrane proton gradient [123,124,125]. Of the four types of ATPases—F1F0, P [126], V [127], and ABC [128]—only F1F0 ATPase can reverse the rotation direction of its γ-subunit to function as ATP synthase, binding inorganic phosphate (Pi) to adenosine diphosphate (ADP) to form ATP [129,130], whereas P-type ATPases are mostly found on plasma membranes [126], and V-type ATPases are located on plasma membranes as well as the membranes of intracellular organelles including endosomes, lysosomes, and the Golgi network [127,131]. Once believed to be exclusive to inner membranes of mitochondria, since 1994, non-mitochondrial extracellular F1F0 ATP synthases have been discovered on plasma membrane surfaces of a variety of cell types, including numerous tumor cell lines [132,133], endothelial cells [134], human umbilical vein endothelial cells [135], HepG2 [136,137] and hepatocytes [138], HaCaT keratinocytes [139], and even in neurofibrillary tangles associated with AD [140].
Although the F0 domain of both bacterial and eukaryotic ATP synthase is embedded within the plasma membrane, the hydrophilic, water-soluble catalytic F1 domain of eukaryotes is oriented towards extracellular space, whereas that of bacteria is directed inwards toward the cytoplasm [130,141]. Both bacteria and eukaryotes use membrane-bound, non-mitochondrial ATPase/ATP synthase to calibrate the homeostasis of intracellular pH [141,142,143,144,145,146]. Intracellular pH is an important regulator of biomolecular condensates because macromolecules including RNA and proteins undergo LLPS as adaptive, reversible, quick responses to subtle environmental stimuli that may include changes in pH, salt concentration, and temperature [3,147,148,149]. The localization of ATP synthase in caveolae, which are uniform, bulb-shaped, specialized lipid raft invaginations in plasma membranes, may confer protection to the proton gradient required for the transfer of protons into extracellular space to maintain intracellular pH and to power F1F0 rotors during ATP synthesis [141,150].
For the first time, in 2004, ATP synthase alpha and beta were discovered to be expressed in lipid rafts isolated from rat HepG2 hepatocytes by immunofluorescence [136], and a functionally active F1F0 ATP synthase on isolated rat hepatocytes plasma membrane was independently confirmed a few years later [151]. In the same year (2004), significant levels of ATP synthase complex capable of generating extracellular ATP and regulating plasma membrane proton gradient were found in lipid rafts of human adipocytes [152]. P-type Ca2+-ATPases [153] such as plasma membrane Ca2+ ATPase (PMCA) were found to be exclusively localized to cholesterol/sphingomyelin-rich lipid raft domains of caveolae in pig cerebellum synaptic plasma membranes [154], and sarco/endoplasmic reticulum Ca2+ ATPases (SERCA) were similarly identified in caveolae/lipid rafts in human uterine cells [155], rat hepatocytes [156], and human Müller glial cells of the retina [157]. Capable of dynamic responses to stimuli through rapid formation and dissipation [158], caveolae are subsets of lipid rafts enriched in glycosphingolipids, cholesterol, sphingomyelin, and lipid-anchored membrane proteins [159,160,161]. Cholesterol is a high-curvature lipid that creates spontaneous negative curvature in lipid bilayers [162,163,164], and naturally accumulates in high-curvature regions of lipid domains such as caveolae invaginations and lipid rafts [165]. In order to maintain curvature and their unique invaginations, caveolae recruit caveolins to bind and increase cholesterol concentration in a 1:1 ratio [166,167]. The fact that most non-mitochondrial ATP synthases and ATPases are highly localized in caveolae and lipid raft domains [136,152] is reminiscent of ATP synthase dimers that exclusively localize in high-curvature cristae invaginations of inner mitochondrial membranes (IMMs).
3.2.1. Dimerized ATP Synthase/ATPase Require High-Curvature Lipid Domains
The ATP synthases of mammalian mitochondria are usually arranged in rows of dimeric complexes of two identical monomers located at the highly curved apex of deep IMM invaginations known as cristae [168]. Dimerized ATP synthases are seven times more active than monomers [169]. Dimerization of ATP synthase may be a major determinant in cristae formation [170], because extreme cristae membrane curvature is shaped by the self-assembly of ATP monomers into dimerized rows [171]. Inability to form dimers resulted in reduced or deformed cristae invaginations [172] that impacted ATP production from decreased OXPHOS activity as a result of defective cristae morphology [173,174]. Experimentally purified ATP synthase reconstituted with membrane lipids revealed that dimerized rows of ATP synthases were formed only on curved surfaces and not on flat membrane areas [175]. Extracellular F1F0 ATP synthases have been observed to translocate from mitochondria to lipid raft domains of various cell types, including plasma membranes of gonadotropes [176], and the sarcolemma of muscle fibers [177].
3.2.2. Translocation of ATP Dimers to Lipid Rafts Are Cellular Responses to Stress and Stimuli
Biomolecular condensates adapt to changing endogenous or exogenous conditions [3] by continuously fine-tuning biochemical reactions, enriching or excluding biomolecules from their environment [7]. The rapid translocation of mitochondrial ATP synthase to lipid rafts may be integral to these adaptive responses because ATP functions not only as a biological hydrotrope [30,178], increasing the solubility of positively charged, intrinsically disordered proteins [179], but may act as a universal and specific regulator of intrinsically disordered regions (IDRs) capable of altering physicochemical properties, conformation dynamics, assembly, and aggregation [45], in addition to providing phosphates as an energy source to fuel post-translational modifications that regulate the fluctuation of biomolecule phase separation during condensate formation [79,178].
LLPS is further regulated by lipid raft membrane-anchored proteins that support the continuous restructuring and rearrangement of molecular components in condensates [116]. Cell surfaces from six different cell lines, including human umbilical vein endothelial cells (HUVECs), human hepatocellular liver carcinoma cells (HepG2), hepatic cells (L-02), human highly metastatic lung cancer cells (95-D), human lung cancer cells (A549), and human embryonic kidney cells (293), revealed that there were significant ATP synthase translocations from mitochondria and an upregulation of catalytic activities under tumor-like acidic and hypoxic conditions compared to normal conditions [180]. Upon edelfosine-induced membrane permeability resulting in the depolarization and disruption of IMM proton gradients, mitochondrial F1F0 ATP synthases in various human cancer cell lines translocated to cell surface lipid rafts or to lipid raft domains present in mitochondria [181]. The presence of redox signaling [182,183] and cancer-related [104,105] proteins in lipid rafts/caveolae further emphasizes the importance of lipid raft domains in health and disease [96,184]. Failure to maintain nanoscopic lipid raft domains with appropriate line tension and membrane elasticity [185] to functionally host dimerized ATPase [186], ATP synthase [175] may contribute to aberrant phase separation, resulting in pathogenic protein aggregates in neurodegeneration [11] and cancer [10,12].
3.3. Physiological Nanoscopic Lipid Raft Domains Are Stabilized by Intrinsic Negative Membrane Curvature and Reduced Line Tension
Lipid bilayers in cell membranes are composed of hundreds of different lipid species with a propensity to segregate laterally into subcompartmentalized raft domains [187,188]. Found in plasma membranes, intracellular membranes, and extracellular vesicles, lipid rafts are dynamic, nanoscopic (10–200 nm), transient, mobile, liquid-ordered (Lo) domains formed as a result of thermodynamically driven LLPS [189,190,191,192,193]. Compared to non-raft domains, the lower-fluidity transient lipid rafts serve as signaling hotspots that respond to external stimuli by modulating their composition and size, and increasing or lowering the concentration of signal transduction proteins [93,194,195]. When formed under pathological inflammatory conditions, lipid rafts become enlarged inflammarafts (i-rafts), signaling platforms that contain activated receptors and adaptor molecules associated with inflammatory cellular processes in diseased states [196,197,198]. Enlarged lipid rafts often serve as scaffolding platforms that aggregate pro-inflammatory NLRP3 inflammasome [196] and cluster pro-apoptotic signaling molecules (CASMER) commonly found in many types of cancer [104,199]. The important roles played by lipid rafts in neurological disorders such as Alzheimer’s disease have long been appreciated [200,201,202,203]. The destabilization and changes in the lipid composition of rafts due to elevations of lipid peroxidation from natural aging [204] offer additional insight into the important relationship between membranes and MLOs in the molecular pathophysiology of neurodegenerative disorders.
Line tension, or the energy required to create boundaries between lipid raft domains and the surrounding membranes, is one of the key drivers that can determine the size, form, and shape of physiological nanoscopic lipid compartments [185]. The hydrophobic mismatch between lipids in raft domains increases the energy and line tension required to maintain rafts as separate compartments [205]; therefore, a reduction in line tension will minimize the free energy between ordered and disordered liquid phases and contribute to the more efficient formation of physiological nanoscopic rafts [188]. Interestingly, the intrinsic, spontaneous curvature of membranes has been demonstrated to be able to reduce line tension [185,206]. Nanoscopic lipid raft domains are generated and stabilized by coupling lipid monolayers with different spontaneous curvatures in liquid-ordered (Lo) and liquid-disordered (Ld) phases to induce elastic interactions by reducing line tension between Lo and Ld phases [207]; in addition, lowering line tension through enrichment with high-curvature lipids such as cholesterol successfully induced the transition from macroscopic to nanoscopic Lo phase lipid raft domains [208]. Furthermore, the in vitro loading of cholesterol enhanced both the abundance of cholesterol in the caveolae/lipid rafts of human umbilical vein endothelial cells (HUVECs) and translocation of the ATP synthase beta chain responsible for catalysis in F1 domains to cell surfaces while significantly doubling the degree of extracellular ATP production within 30 min of exposure [209,210].
The ability of ATP synthase/ATPase to form dimerized rows on the IMM of mitochondria and other membrane surfaces may be highly dependent upon membrane lipid composition [211] and curvature [175]. Uncontrolled, excess oxidative stress can cause lipid peroxidation [212] which induces pathological changes to membrane lipid composition, including alterations of cardiolipin in IMMs [211,213], as well as changes in membrane curvature that prevent optimal dimerization and the subsequent functioning of ATP synthase/ATPase [214,215]. Insufficient or depletion of ATP can directly impact the physical and functional properties of biomolecular condensates [32,33,79,118]. ATP is not only a biological hydrotrope capable of inhibiting protein LLPS and aggregation at high mM concentrations; it has recently been observed to act as a universal and specific regulator of IDRs, altering their physicochemical properties, conformation dynamics, assembly, and aggregation [45]. Furthermore, ATP has been documented to associate with phospholipid bilayers, forming aggregates at high mM concentrations in the aqueous phase. In fact, the endogenous heterogeneity of lipid membranes was seen to selectively enhance the diffusion restriction of ATP in the cytosol [216].
3.4. Oxidative Stress Alters Lipid Molecular Structures in Rafts and Membranes, Resulting in the Accumulation of Pathological MLOs
Inability to neutralize excess reactive oxygen species (ROS) accumulated as products of normal cellular functions results in a state of imbalance often referred to as oxidative stress [217]. Oxidation of lipids in membranes disrupts functionality by inducing changes in lipid molecular structure that leads to diminished negative intrinsic membrane curvature, lowered membrane fluidity, and increased membrane permeability [214,218,219,220]. Phase separation of biomolecular condensates such as FUS takes place in the cytoplasm. The presence of high levels of ATP in cytoplasm can ensure proper dissolution of FUS aggregates [51,52]. Even though mitochondria are major ATP-producing organelles in eukaryotes, ATP concentration in mitochondria is maintained at significantly lower levels than that of cytoplasm [40] by voltage-dependent anion channels (VDACs) located in the mitochondrial outer membrane (MOM) [41] and adenine nucleotide translocators (ANTs) on the IMM [43] that transport ATP from mitochondria into cytoplasm. Therefore, mitochondrial ATP production exerts a direct influence on the formation and dissolution of MLOs in cytoplasm. Importantly, the amount of ATP produced in mitochondria is, in large part, determined by cristae morphology [221].
Cristae are dynamic, independent, bioenergetic IMM invaginations capable of remodeling in seconds to organize respiratory chain supercomplex assembly and ATP synthase for efficient ATP production [221,222]. Mitochondrial membrane lipid composition may contain up to 24–25% of cardiolipin (CL) [223,224,225]—an anionic, high-curvature, four-acyl chain lipid with a unique cone shape that can stabilize negative membrane curvatures in cristae and increase bending elasticity of the IMM [226,227,228,229,230,231]. Embedded in the IMM cristae, the F0 motor of the ATP synthase controls proton flux that powers the rotation of the F1 subunit protruding into the mitochondrial matrix, driving the synthesis of ATP [232]. CL is required for the proper docking and insertion of OXPHOS proteins into the IMM, as well as the formation and maintenance of structural integrity of the mitochondrial respiratory chain supercomplexes [233,234]. This is probably why CL binds to the F1F0 ATP synthase with higher affinity than all other mitochondrial phospholipids [235]. ATP synthesis could be significantly enhanced when proton translocation is increased by the non-bilayer structures at the apex of IMM cristae formed during CL interactions with the F0 section of ATP synthase [236], whereas CL deficiency can result in compromised mitochondrial energetic and coupling efficiency in skeletal muscles [237]. Mitochondrial bioenergetics are heavily dependent upon optimal CL lipid composition, content, and structure [238]; therefore, mitochondrial dysfunction as a result of CL peroxidation and depletion is associated with numerous pathophysiological conditions [239], including myocardial ischemia [240], nonalcoholic fatty liver disease [241], thyroid dysfunctions [242], diabetes, obesity and other metabolic diseases [243,244], cancer [245], as well as a wide range of neurological disorders including Alzheimer’s disease [246], Parkinson’s disease [247,248], amyotrophic lateral sclerosis [249], Barth syndrome [250,251], and traumatic brain injury [252,253]. The highly unsaturated phospholipids in CL are extremely sensitive to ROS attack. CL oxidation products in animal models may be used as effective biomarkers for oxidative stress in mitochondria [254,255]. Alterations in lipid composition and molecular structure, as well as membrane curvature and line tension as a result of ROS attacks, often initiate signaling events that recruit MLOs to membrane sites, whereas pathological amyloidogenic MLO aggregates at membranes, in turn, alter membrane structures [256,257].
3.5. ROS-Externalized Cardiolipin Facilitates the Accumulation of Amyloid/Prionoid Aggregates and Activates Autophagic and Inflammatory Signaling
Cardiolipin (CL) is a mitochondria signature lipid distinctly attracted to membrane lipid domains with strong negative curvatures, such as the apex of IMM cristae [226,228]. CL is often externalized to the outer mitochondrial membrane (OMM) upon mitochondrial distress from ROS attacks [258,259], whereas oxidized CL in OMM initiates apoptotic signaling processes [260] that can lead to opening of the mitochondrial permeability transition pore (mPTP) and the release of cytochrome c (Cyt c) [261,262]. Externalized CL, whether oxidized or not, becomes an essential signaling platform that binds and interacts with important mitophagic, autophagic, and inflammatory enzymes [259,263], including Beclin 1 [264], tBid, Bax [262,265], caspase-8 [266], and the NLR pyrin domain containing 3 (NLRP3) inflammasomes [267]. A major source of extremely inflammatory cytokines IL-1β and IL-18 [268], NLRP3 inflammasome is a phase-separated supramolecular complex that mediates immune responses upon the detection of cellular stress and dysfunction [269,270,271]. The activation of the NLRP3 inflammasome in macrophages is induced by oxidized phospholipids [272], whereas the docking of externalized CL to NLRP3 inflammasome primes its assembly and subsequent activation in mitochondria [267] as well as mitochondria-associated membranes (MAMs), a region comprising highly specialized proteins which is tethered to the endoplasmic reticulum (ER) [273,274]. ER stress and MAM dysfunction are increasingly associated with the aggregation of misfolded proteins as a result of aberrant phase separation [275,276,277]. The conversion of the phase-separated presynaptic neuronal protein α-syn from a physiological liquid-like droplet state into the pathological amyloid hydrogel aggregated state may also be facilitated by binding with externalized CL at OMM, ultimately disrupting mitochondrial membrane integrity and enhancing neurotoxicity [278,279,280]. Neurodegenerative disorders such as AD and PD have been associated with aberrant CL content, structure, and localization [281].
α-syn demonstrates a high affinity for mitochondrial membranes, interacting in close proximity with mitochondrial OXPHOS proteins, including lipid raft-like domains at MAMs that are high in phospholipids [282,283]. Native, unfolded, monomeric α-syn improves ATP synthase efficiency and increases ATP levels [284,285], whereas the pathological aggregation of α-syn can generate ROS to cause lipid peroxidation and the oxidation of ATP synthase beta subunits, inhibiting mitochondrial respiration [286], opening mPTP, and resulting in apoptosis [287]. CL has been observed to enhance the formation of ion-permeable pore structures with channel-like properties by α-syn oligomers in lipid membranes [288]. MAMs, IMM, and OMM, with their lipid raft-like domains enriched with CL, easily form pores large enough to allow the transit of water and other small molecules that could cause mitochondrial swelling and Cyt c release [288,289,290]. Intriguingly, most ion channels preferentially reside in membrane raft-like microdomains [291].
Physiological lipid rafts function optimally at nanoscopic sizes [292,293,294]. ROS that attack anionic lipid headgroups at membrane interface [295] can cause lipid peroxidation cascades, creating products that alter raft properties, and increasing line tension [206] to grow nanometer-scale rafts into enlarged, micron-sized inflammarafts [196,197,296] that carry pro-inflammatory signaling molecules [104,198,199]. Melatonin, known for its modulatory effects on various ion channels [297,298,299], has recently been observed to directly inhibit cryopreservation-induced mPTP opening, increasing ATP production, counteracting OXPHOS inhibition, as well as upregulating glycolysis [300]. The fact that oxidized CL, whether exogenously added [261] or endogenously induced [301], causes mPTP opening in mitochondria, further accentuates the necessity for the timely resolution of oxidative stress by appropriate antioxidants.
3.6. Melatonin Inhibits Cardiolipin Peroxidation to Prevent the Aggregation of Pathological MLOs at Membranes
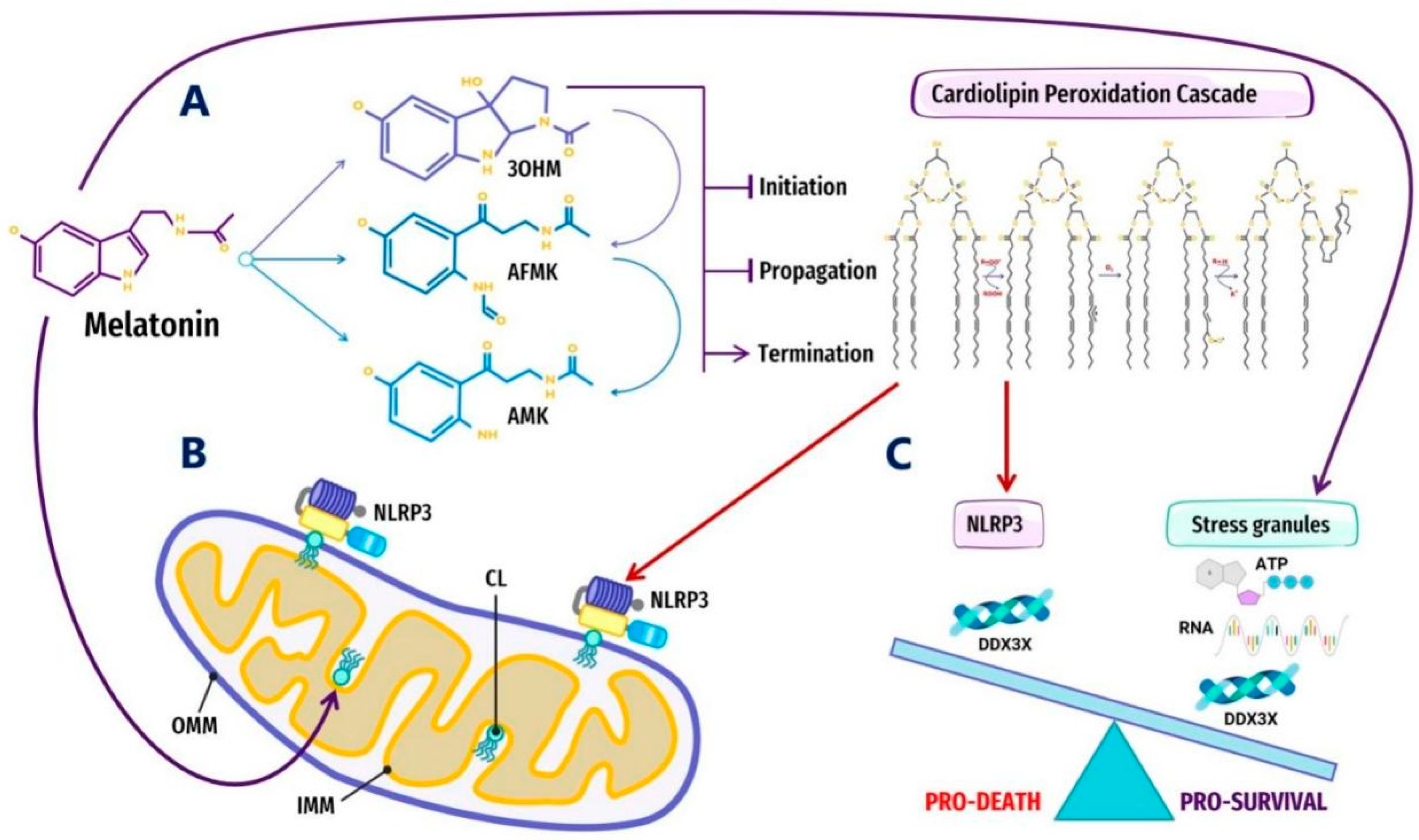
Melatonin is a potent antioxidant that has been shown to inhibit CL peroxidation in mitochondria, preventing mPTP opening and Cyt c release [301] by inhibiting peroxidation cascades initiated by specific ROS that accumulate in lipid headgroups at membrane–water interfaces [295] (Figure 1). The suppression of oxidative stress and lipid peroxidation may halt the externalization or oxidation of CL, effectively preventing potential pathological interactions with MLOs such as α-syn and the NLRP3 inflammasome. The interaction between pathological α-syn oligomers and externalized CL can result in increased ROS, lipid peroxidation, and mitochondrial dysfunction; therefore, it is not surprising that melatonin has been demonstrated to block α-syn fibril formation and oligomerization, decreasing cytotoxicity in primary neuronal cells [302], as well as rescuing impaired mitochondrial respiration induced by α-syn in Saccharomyces cerevisiae under ROS attack [303]. The NLRP3 inflammasome must be primed by externalized CL upon ROS stimulation before activation [258,267,273]. The regulation of the next phase where the NLRP3 inflammasome transitions into stable, prionoid-like complexes is mediated by DDX3X, one of the ATP-bound forms of DEAD-box RNA helicases responsible for the scaffolding of prionoid, self-oligomerizing specks known as apoptosis-associated speck-like protein containing a C-terminal caspase recruitment domain (ASC) which cannot be easily disassembled once they are formed [304,305,306] (Figure 2).
Figure 1.
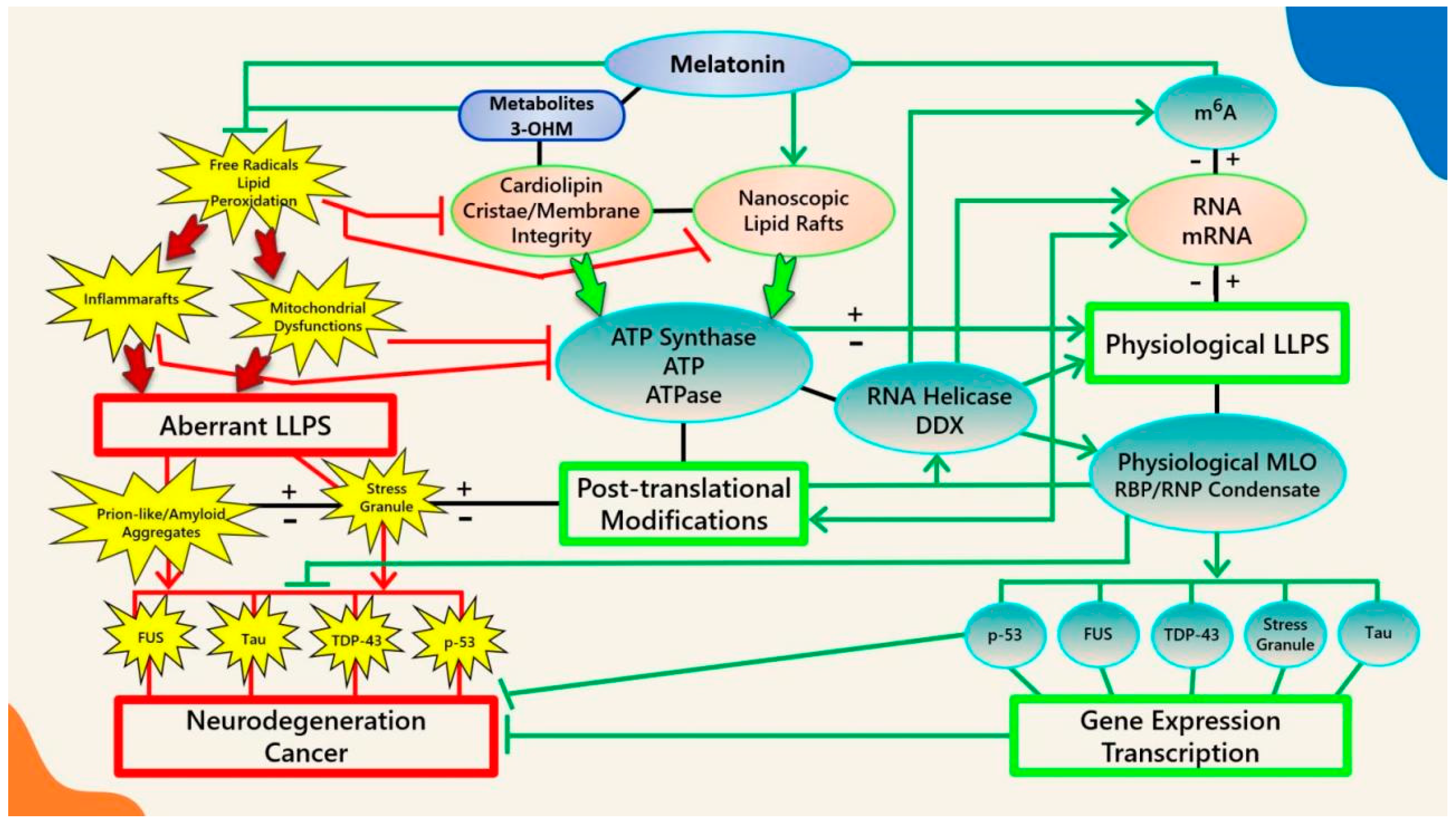
Schematic illustrating the regulation of biomolecular condensates by melatonin represented through observations reported in antioxidant protection against lipid peroxidation to maintain membrane/lipid raft composition/stability that serves to maintain adequate ATP levels in all cellular compartments to fuel, support, and regulate post-translational/m6A modifications that may fine-tune RNA dynamics in the assembly and disassembly of MLOs to prevent pathological aggregations in neurodegenerative disorders. LLPS: liquid–liquid phase separation; DDX: Dead-box RNA helicase; m6A: N6-methyladenosine; MLO: membraneless organelle; RBP: RNA-binding protein; RNP: ribonucleoprotein; PTM: post-translational modification (See Abbreviations for additional acronyms).
Figure 2.
Overview of melatonin regulation of NLRP3 inflammasome (NLRP3) formation, assembly and activation: (A) Summary of melatonin and metabolite antioxidant cascade inhibiting the initiation and propagation of cardiolipin (CL) peroxidation, effectively terminating the CL peroxidation cascade; (B) Oxidized CL is externalized from the cristae/inner mitochondrial membrane (IMM) to the outer mitochondrial membrane (OMM) where it docks and primes NLRP3 inflammasome assembly prior to activation in mitochondria; (C) DDX3X, an ATP-dependent DEAD-box RNA helicase, is the mediator that selects the formation of “Pro-Survival” stress granules or the transition of the NLRP3 inflammasome into “Pro-Death”, stable, prionoid-like complexes. The successful formation of stress granules is also dependent upon the availability of ATP and RNA, both of which may be regulated by melatonin (See Abbreviations for additional acronyms).
ATP-dependent DEAD-box RNA helicases (DDXs) are ATPases that regulate RNA-containing phase-separated organelles in prokaryotes and eukaryotes [307,308]. DDXs promote phase separation in their ATP-bound form, but can also release RNA and induce compartment turnover using ATP hydrolysis. Inhibition of DDX ATPase activity can disrupt the disassembly of physiological MLOs such as P-bodies and stress granules [69,309] (Figure 1). It is presently unknown what prompts DDX3X to select the aggregation of pro-survival stress granules over pro-death NLRP3 inflammasomes or vice versa [304,310]. It would not be unreasonable to assume that an excessive oxidative local environment with pathological i-rafts in membranes could exert a decisive influence over the selection process (Figure 2).
The activation of the NLRP3 inflammasome is now associated with major neurodegenerative disorders such as AD, PD and ALS, where positive correlations have been found to exist between NLRP3 levels and abnormal protein aggregations such as Aβ and α-Syn, whereas the inhibition of the NLRP3 pathway attenuates pathological protein aggregations [311]. Melatonin inhibited NLRP3 inflammasome activation and reduced the aggregation of ASC specks in the mice hippocampus with major depressive disorder induced by inflammatory liposaccharides [312]; melatonin also inhibited the formation of hypoxia-induced inflammasome protein complexes and reduced the aggregation of ASC specks in macrophages of Sugen/hypoxia pulmonary arterial hypertension (PAH) mouse models [313]. Melatonin attenuated the progression of intervertebral disc degeneration in vitro and in vivo by reducing mitochondrial ROS products to inhibit NLRP3 inflammasome priming and activation, effectively terminating pro-inflammatory cytokine expression [314]. The ability of melatonin to prevent the opening of mPTP and release of Cyt c [301], inhibit NLRP3 inflammasome priming, activation, and ASC speck aggregation [312,313], block α-syn fibrillation [302], and improve mitochondrial respiration [303] could be directly related to its ability to stabilize nanoscopic lipid raft domains and suppress lipid peroxidation, which can alter the composition and molecular structures of lipid rafts.
3.7. Melatonin Regulates Membrane Lipid Dynamics and Composition via Phase Separation
Nanoscopic transient lipid raft domains in biological membranes are formed by phase separation in response to external stimuli [92,93,188]. Even though cells may alter lipid constituents to control the composition and size of lipid rafts [315], the propagation of molecular stress, lipid raft rattling dynamics and relaxation are some of the basic mechanisms underlying phase separation on the molecular level [195]. The presence of hydrophobic molecules such as melatonin can modulate viscoelastic dynamics through the accumulation and propagation of stress in lipid–lipid interactions [195,316]. Adding melatonin to membrane models led to a breakdown of out-of-phase membrane displacement patterns and the disruption of the vibrational landing platform of lipid biomolecules at the water–membrane interface, effectively slowing the permeation of ROS and other small molecules [195,317].
In 2005, melatonin was first observed to induce phase-separation in DPPC lipid bilayers [318]; recently, melatonin has been observed to modify lipid hydrocarbon chain order to promote phase separation in ternary membrane models [319]. Due to a preference to localize at membrane interfaces [320], melatonin can form strong hydrogen bonds with membrane lipid anionic headgroups that could significantly modulate lipid acyl chain flexibility and lipid dynamics [318]. Melatonin is able to directly interact with cholesterol [321] and displaced cholesterol due to competitive binding to lipid molecules, increasing disorder in the Ld phase to drive cholesterol into the ordered Lo phase [319]. These subtle changes in lipid nanodomains can profoundly affect amyloid processing at membrane sites. Aβ1–40 and Aβ1–42 peptides are known to interact strongly with negatively charged lipids by binding to anionic, negatively charged membranes [322,323,324,325,326]. Increasing cholesterol content lowered the surface charge of lipid membranes in saline solution from positive to negative [327]. Although cholesterol is an indispensable constituent of lipid rafts [92,162], its electrostatic properties altered interactions of charged or polar biomolecules on lipid membrane surfaces and attracted the targeted binding of Aβ deposits at lipid membranes [328,329,330,331].
In animal and in vitro studies, melatonin was able to prevent or ameliorate tau and Aβ pathology in AD [332,333,334,335] and inhibit Aβ production and assembly while enhancing non-amyloidogenic APP processing [336]. As early as 1998, melatonin was documented to inhibit amyloid fibrillation through modifications of Aβ peptide secondary structures. It was hypothesized that the observed changes could have been due to the unique structural characteristics as well as antioxidant properties of melatonin [337]. As a result of deficient melatonin from natural aging, Aβ25–35 peptides embedded in hydrocarbon cores of anionic lipid bilayers may further displace cholesterol molecules to increase oligomerization or fibrillation [338], but the addition of 30 mol% melatonin to anionic membranes strikingly reduced membrane-embedded Aβ peptides [338]. Melatonin behavior in membrane systems was affected by the competitive binding dynamics between melatonin and cholesterol to membrane phospholipids via hydrogen bonds. The presence of cholesterol could also change melatonin configuration from folded to extended, whereas increasing cholesterol levels to 50% drove melatonin from the membrane interface to become fully solvated by lipid headgroups or bulk water [339]. On the other hand, a single, intraperitoneal, pharmacological dose of melatonin at 100 mg/kg strengthened hydrogen bonding in the polar zone and increased disordering in the non-polar zone of phospholipids in rat brain membranes [340].
Local variations in melatonin concentration also affected the re-ordering of lipids in membranes. At 0.5 mol% concentration, melatonin was documented to penetrate lipid bilayers to form fluid domains that enriched lipid membranes where melatonin molecules aligned parallel to phospholipid tails with the electron-dense regions slightly below hydrophilic headgroups; however, at 30 mol% concentration, melatonin molecules aligned parallel to the lipid bilayer, close to the headgroup regions where one melatonin molecule was associated with two lipid molecules to form an ordered, uniform, lateral membrane structure distributed evenly throughout the membrane model [341]. Variations in local concentration and conformational changes in melatonin molecules can directly impact the lipid phase transition, line tension, size, health, and functions of lipid rafts.
3.8. Melatonin Increases Membrane Fluidity and Reduces Line Tension to Stabilize and Maintain Nanoscopic Lipid Raft Domains
Membrane fluidity reveals the degree of molecular disorder and motion within lipids in membrane bilayers [342]. There are hundreds of different lipid species in lipid bilayers that have a high propensity to segregate laterally into subcompartmentalized lipid raft domains [187]. Oxidative stress can increase membrane rigidity, altering lipid raft formation rates as a response to cellular stress [343,344]. Oxidation of lipids in membranes can also alter molecular structures by creating amphiphilic subpopulations leading to significant changes in the phase behavior of lipid membranes that can affect the integrity and structure of membranes [214]. When under ROS attack, cells form cubic lipid structures in the smooth endoplasmic reticulum and IMM [214,345,346].
It is believed that lipid rafts function optimally as nanodomains [114,293], whereas rafts that are enlarged under inflammatory conditions assemble pathological MLOs associated with cellular processes in diseased states [104,196,197,198,199]. Essentially, lipid peroxidation alters the organization, assembly, and structure of membrane lipids [256,347,348], where lipid peroxides often induce nanometer-scale rafts to grow to micron sizes, accompanied by increased line tension in the order of several piconewtons [206,218,296]. Lipid peroxidation also prevents the formation of lipid rafts at room temperature by enhancing phase separation that favors significant increases in the fraction of the non-raft Ld phase [349]. Interestingly, melatonin was observed to stabilize lipid Lo–Ld phase separation over a range of temperatures and domain sizes, effectively preventing the formation of a non-raft Ld phase, possibly by reducing line tension or acting as a surfactant at Lo–Ld interfaces [350]. ATP is possibly a surfactant [30,31] capable of reducing the interfacial free energy penalty during the formation of smaller-sized multiple coexisting MLOs, whereas larger droplets may form as a result of lower surfactant ratios [351]. Whether melatonin can also act as a surfactant [350] to induce the formation of small, multiple coexisting droplets may require further validation while increasing evidence is being reported [352]. Nonetheless, by stabilizing and maintaining optimal nanoscopic lipid domains, melatonin is perfectly capable of preserving the high level of cytosolic ATP concentration requisite for proper biomolecular condensate formation and dissolution through its features as a potent antioxidant.
During lipid peroxidation events, oxidized moieties were found to mainly reside close to the lipid headgroups forming hydrogen bonds with water. These oxidized lipids can perturb membrane bilayer structures and modify membrane properties, including decreasing the membrane fluidity [318,353,354,355]. The preferential location of melatonin in bilayer lipid headgroups allows dynamic interactions that lead to reductions in bilayer thickness and increased bilayer fluidity [338,341,356]. Eukaryotes and prokaryotes use ATPases localized in cell membranes and lipid raft domains to produce and release ATP energy [122,127,136,152]; therefore, increased ATPase activities from enhanced membrane fluidity [357,358] can impact how ATP interacts with phospholipids in bilayers [216] and modulate the LLPS of MLOs formed at membrane surfaces [45]. Moreover, lipid peroxidation is believed to be associated with the reduction in mitochondrial membrane fluidity during aging in animals [359]. Membranes themselves can affect local protein concentrations [360] where high-curvature lipids that form rafts may attract specific proteins that form aggregates to further enhance membrane curvature [361,362,363,364]. Increasingly, neurodegenerative diseases such as AD are viewed as membrane disorders [203]. The size of MLOs that aggregate at membrane surfaces can be tuned through PTMs such as phosphorylation, which is ATP-dependent [365]. The amount of ATP available at membrane surfaces and cytosol drives the formation, tuning, and dissolution of MLOs, and is regulated by oxidative-stress-sensitive ion channels that reside in lipid rafts (Figure 1).
3.9. Melatonin Maintains a High Cytosolic ATP:ADP Ratio through the Optimization of VDAC-CYB5R3 Redox Complexes in Lipid Rafts
Lipid rafts are phase-separated regions in lipid bilayers responsible for important biological functions including signal transduction [92,93] as well as the trafficking and sorting of proteins and lipids [94,95]. The fact that lipid rafts are also important redox signaling platforms that assemble, recruit, and activate redox regulatory multiprotein complex NADPH oxidase [182,366], and host the quintessential plasma membrane redox enzyme complex VDAC-CYB5R3 [367,368], emphasizes the relevance of melatonin as an antioxidant in the protection and stabilization of lipid raft domains.
Present in all eukaryotes [369], CYB5R3 encodes for a NADH-cytochrome b5 reductase 3 flavoprotein that is engaged in the one-electron transfer from NADH to cytochrome b5 or plasma membrane coenzyme Q, producing NAD+ as a result [370,371]. The soluble isoform of CYB5R3 is exclusive to erythrocytes [372], whereas the membrane-bound isoform is anchored to MOM, ER, and plasma membrane lipid rafts [368,373,374]. Importantly, the OMM-bound CYB5R3 enzyme, ubiquitously expressed in all mammalian cells, is functionally attached to the voltage-dependent anion channel 1 (VDAC1), one of the most prevalent proteins located in the OMM [375,376].
Originally known as mitochondrial porin after its identification in yeast (1985) [377] and humans (1989) [378], VDAC was subsequently observed as a resident protein of lipid rafts in the plasma membranes of animal hearts, brains, and lungs [379] from different human cell lines, including epithelial cells, astrocytes, and neurons [380,381]. Aberrant lipid composition in neuronal lipid rafts disturbs physiological VDAC protein interactions that can affect the opening and closing of VDAC channels, resulting in oxidative stress and neuronal impairments prominent in most AD pathologies [380]. The force-from-lipid principle dictates that the opening and closing of membrane embedded channels can be propelled by the mechanical properties of surrounding lipids [382,383,384,385] and their composition. Changes to raft thickness, curvature and elasticity [291] as a result of lipid peroxidation can therefore affect physiological functions of the VDAC and CYB5R3 redox complex.
CYB5R3 enzymes form large redox centers in lipid rafts that enhance mitochondrial respiration rate and ATP production, albeit resulting in increased production of ROS [368,373,374]. Over stimulation and clustering of CYB5R3 induced oxidative stress-mediated apoptosis of cerebellar granule neurons [386]. Independent of respiratory chain activities, the ascorbate-dependent NADH: cytochrome c oxidoreductase oxidation of NADH at CYB5R3 centers in lipid rafts is also a major source of extracellular superoxide [376,387,388,389,390] that can initiate lipid peroxidation. In Wistar rats, the deregulation of CYB5R3 promptly triggers apoptosis due to the overproduction of superoxide anions at neuronal plasma membranes [368,387]. Excess NADH due to CYB5R3 redox dysfunction can close VDAC, suppressing OXPHOS and increasing glycolysis [376,391], whereas the opening of VDAC also elevates ROS from increased OXPHOS activities [41]. As the most abundant protein in the MOM, VDAC is regarded as a dynamic regulator of mitochondrial functions, interacting with over 100 proteins in health and disease [392]. VDAC opening is believed to globally control mitochondrial metabolism and ROS formation, modulating mitochondria and cellular bioenergetics [41,393]. Nevertheless, the question of whether apoptosis is associated with the opening [394] or closure [395,396] of VDAC has been highly debated [397], further emphasizing the important role of this protein in the regulation of cell life and death [392,398].
VDAC is the gatekeeper which controls the export of ATP out of mitochondria into cytosol and the import of essential respiratory substrates such as ADP and Pi into mitochondria [395,399]; therefore, VDAC opening may be instrumental in determining the fate of MLO formation, regulation, and dissolution. ATP is not only a biological hydrotrope capable of inhibiting protein LLPS and aggregation at high mM concentrations, but it has recently been observed to act as a universal and specific regulator of IDRs capable of altering physicochemical properties, conformation dynamics, assembly, and the aggregation of MLOs [45]. Not only is the preservation of lipid raft structure and composition essential for maintaining specific ion channel properties [380], the amount of cytosolic ATP is dependent upon mitochondrial synthesis and the integrity of CL enriched raft-like lipid domains in mitochondria [367,400,401,402].
The mitochondrial electron transport chain is a major ROS-generating site where complex III and mitochondrial glycerol 3-phosphate dehydrogenase can produce large amounts of redox signaling molecules such as superoxide and hydrogen peroxide to the external side of the IMM as well as the matrix [403,404]. Bis-allylic methylenes and abundant double-bonds in CL lipid chains are vulnerable targets of ROS attacks [239,405,406,407]; therefore, the lipid monolayer leaflets facing the crista lumen enriched in CL in mitochondria [228] may be subject to intense peroxidation events. Peroxidized CL could not support mitochondrial OXPHOS enzyme activities [239,408], leading to the depletion of ATP [409] that can potentiate and exacerbate the aggregation of pathological MLOs.
Melatonin is an ancient, potent antioxidant that protects lipid nanodomains from peroxidation caused by excess oxidative stress. The addition of micromolar concentrations of melatonin to rat heart mitochondria dramatically inhibited CL oxidation by tert-Butylhydroperoxide (t-BuOOH), a peroxidation promoting peroxide, reversing cytochrome c release, matrix swelling, and proton motive force (ΔΨ) collapse in treated cells [301]. The melatonin molecule is uncharged in the entire pH range [410] and contains both hydrophilic and lipophilic moieties that support its easy accumulation in all internal membranes of cells as well as other hydrophobic sites [411,412]. The exogenous supplementation of melatonin in rodents results in dose-dependent increases in all subcellular compartments, with lipid membranes exhibiting 10-fold increases compared to mitochondria [413]. The presence of both hydrophilic and lipophilic moieties in melatonin not only facilitates the efficacious scavenging of both aqueous and lipophilic free radicals [411], but also places the molecule in a unique position during evolution to protect membrane lipids from oxidative damage and potentially regulate MLOs that form at membrane surfaces in an ATP-dependent manner (Figure 1).
4. Melatonin Is a Potent Ancient Antioxidant That Protects ATP Levels to Regulate the Formation and Dissolution of MLOs
Melatonin (N-acetyl-5-methoxytryptamine) is a mitochondria-targeted molecule found in cells of all tested eukarya and bacteria [414]. Effective distribution via horizontal gene transfers may explain the discovery of ancient homologs of arylalkylamine N-acetyltransferase (AANAT), the enzyme responsible for the rhythmic production and release of melatonin in bacteria, fungi, unicellular green algae, and chordates [415,416,417]. In present-day vertebrates, it is estimated that ~99% of melatonin is likely not produced in the pineal gland, nor released into circulation upon pineal production [418], but is mainly synthesized and localized in mitochondria [419,420]. Photosynthetic cyanobacteria responsible for filling the earth with oxygen that led to the extinction of obligate anaerobes produce melatonin [421,422]. The presence of melatonin in primitive unicellular organisms including Rhodospirillum rubrum and cyanobacteria, precursors to mitochondria and chloroplasts, respectively [415,423,424,425], may have conferred protection against endogenous and exogenous oxidative stress that could readily damage biomolecules and disrupt ATP production at plasma membranes [421,425,426,427]. This unique feature implies that melatonin may have an intrinsic modulatory effect over phase separation in early organisms.
As in all eukaryotic cells of plants and animals, LLPS is also believed to be the organizing principle behind the subcellular compartmentalization of membraneless organelles (MLOs) in prokaryotic bacteria [277,428], where condensate formation is tightly correlated with ATP levels. Impaired ATP hydrolysis from reduced ATPase activity in bacteria causes droplet formation by phase separation [429,430]. Cyanobacteria, the only known prokaryote capable of water oxidation [431], has recently been shown to exhibit circadian rhythm in the formation and dissolution of MLOs that remained soluble during daylight, but became reversible, insoluble condensates at night. The formation of aggregates allows cyanobacteria to conserve energy when metabolic activities and ATP levels are lowered at night [432,433,434,435]. It is therefore not unexpected that when ATP production was disrupted, insoluble aggregates could be induced to form in cyanobacteria even during daylight by suppressing F1F0-ATP synthase or uncoupling OXPHOS with mitochondrial proton gradient inhibitors [432].
The gene sequences of cyanobacteria ATP synthase subunits are extremely similar to those in chloroplasts [436]. Embedded in the thylakoid membrane, both ATP synthase in cyanobacteria and chloroplasts (CF0CF1) control transmembrane electrochemical proton gradients for the production of ATP [437,438,439]. Similar to CL, which is synthesized from phosphatidylglycerol (PG) in all organisms [440], PG is the primary phospholipid associated with photosystem complexes that carry out electron transport reactions during oxygenic photosynthesis [441]. Both CL and PG are essential for maintaining the proper lipid composition that supports electron transport and ATP production in eukarya and prokarya, although these lipids are easily subjected to damage via lipid peroxidation [213,234,442,443,444,445,446]. The antioxidant effects of melatonin and its metabolites become particularly meaningful when the prevention of CL peroxidation by hydroperoxyl in mitochondrial membranes can affect the formation and dissolution of biomolecular condensates (Figure 1).
4.1. Melatonin Metabolite 3-OHM Inhibits Lipid Peroxidation by Hydroperoxyl Radical
Melatonin and its secondary, tertiary, and quaternary metabolites actively scavenge potent free radicals [317,426,447] including hydroxyl radicals [448], singlet oxygen [449,450], hydrogen peroxide [451], nitric oxide [452,453,454], and peroxynitrite anions [455] via different antioxidant mechanisms such as direct radical trapping in Type I antioxidant reactions and inactivating hydroxyl radicals (•OH) through the sequestration of metal ions and deactivating •OH during Fenton-like reactions in Type II antioxidant reactions [456]. In addition, melatonin and its metabolites collectively preserve the chemical integrity of biomolecules from oxidative stress via Type III antioxidant cellular repair processes and Type IV antioxidant reactions that can enhance antioxidant enzymes and inhibit pro-oxidant enzymes [456].
A recent study that analyzed the mechanistic interactions between melatonin and •OH employing density functional theory found that one molecule of melatonin effectively scavenged two •OH radicals to produce the stable footprint metabolite, cyclic 3-hydroxymelatonin (3-OHM) [457], in perfect agreement with mechanisms reported in prior experimental and theoretical studies [448,458,459,460]. 3-OHM has been shown to react with hydroperoxyl radicals (•OOH) at rates 98.4 times faster than Trolox in aqueous solution [459]. Trolox is a water-soluble, cell-permeable analog of vitamin E with high radical scavenging potential often used as a yardstick for measuring antioxidant capacities in vitro. Trolox resides mainly in the aqueous phase; therefore, it has been observed that Trolox and other water-soluble antioxidants exhibit reduced scavenging activity if radicals are produced within hydrophobic cores of lipid membranes [461]. Melatonin accumulates in all of the internal membranes of cells as well as other hydrophobic sites [412]; therefore, this antioxidant may be uniquely positioned for quenching lipid peroxidation by •OOH and other free radicals that penetrate deep into lipid molecules.
4.2. Melatonin Is Preferentially Located at Hydrophilic/Hydrophobic Membrane Interfaces
All biological cell membranes comprise amphipathic lipid molecules with hydrophilic heads and hydrophobic tails that naturally form bilayers with headgroups oriented towards an aqueous environment and tails facing each other [462]. The melatonin molecule is uncharged in the entire pH range [410] and, accordingly, in laboratory environment, the “hydrophobic” molecule is dissolved poorly in water [463] except when solubilized in pure aqueous medium by specific methodology that polarized the pyrrole ring to facilitate hydrogen bonding of the N–H group [464]. The unique ability to form strong H-bonds with hydrophilic lipid headgroups allowed nonpolar melatonin to be preferentially located at hydrophilic/hydrophobic interfaces, with complete solubility observed at the interfaces between polar and lipophilic nanodomains in reversed micelles [320]. The presence of both hydrophilic and lipophilic moieties in melatonin facilitates the scavenging of both aqueous and lipophilic free radicals [411], especially •OH [448] and •OOH, the two most prevalent ROS responsible for the chain oxidation of unsaturated phospholipids [465,466] in the membranes of cells and mitochondria [467,468].
4.3. Melatonin Metabolite Free Radical Scavenging Cascades Rescue Cardiolipin from Hydroperoxyl Radicals (•OOH)
Lipid peroxidation, a physiological process in all aerobic cells [469], is a cascading chain reaction that begins with the abstraction of allylic hydrogen from adjacent lipid molecules by free radicals such as •OOH and •OH and terminates with reactive aldehyde end products such as malondialdehyde (MDA) and 4-hydroxynonenal (HNE) [212,470,471,472,473]. Both •OOH and •OH are derived from ubiquitous superoxide radicals (O2•−) generated from the one-electron reduction of oxygen (O2) that may be catalyzed by nicotinamide adenine dinucleotide phosphate oxidase (NADPH oxidase) during respiratory bursts [474] and/or electron leakage during mitochondrial electron transport [403]. Due to its low rate constant values below ~102 L·mol−1·s−1 [475], O2•− behaves more similarly to an unimpressive reductant (E°′(O2/O2•−) = −0.33 V) than an oxidant (E°′(O2•−/H2O2) = 0.93 V) [472,476,477,478] which reacts at a much slower pace with the tested phospholipids compared to •OOH [466,479]. Hydroperoxyl (•OOH or HO2•), also known as a perhydroxyl radical, is a chemically active, protonated form of superoxide radicals (O2•−) [480], engaged predominantly as intermediates for the disproportionation of O2•− into hydrogen peroxide (H2O2) which then can further be transformed via Fenton’s/Haber–Weiss reactions [481] into •OH, possibly the most reactive and mobile species of oxygen that interacts with almost all molecules in cells [212,481]. Even though at neutral pH •OOH exists primarily as the less reactive O2•−, where the ratio of protonated •OOH to anionic O2•− is ~130:1 (less than 1%), •OOH can be a potent initiator of lipid peroxidation [465,466].
When reacting with phospholipids, the advantageous free energy profile of −8.5 kJ/mol free energy minimum relative to the aqueous phase allowed •OOH to accumulate at lipid headgroup membrane–water interface at concentration enhancement of over one order of magnitude [295]. Multi-level atomistic simulations for interactions of •OH, •OOH, and H2O2 with polar headgroups of phospholipid bilayer revealed that all three species traveled deep into the water layer to reach phospholipid biomolecules, oxidizing hydrophilic headgroups before hydrophobic tails [482], with •OOH staying adsorbed for the longest duration at headgroup regions [295]. The headgroup of CL is fully ionized as a dianion in the physiological pH range [483], supporting its unique, optimal functionality as a “proton trap” that promotes mitochondrial respiratory enzyme activities [484].
The strong negative curvature of cristae in the IMM is primarily sustained by the distinct molecular geometry of CL with its smaller, elongated, conical-shaped, double-phosphate dianonic headgroups that increase lateral pressure within the acyl chain regions and stabilize cylindrically curved, tubular cristae structures [223,485,486]. In large unilamellar vesicles (LUVs) comprising similar lipid properties as the IMM, the addition of a typical concentration of 25% negatively charged, dianonic CL lowered pH at the membrane interface to ~3.9, compared to the bulk pH of 6.8 normally found in mitochondrial intermembrane space [487] and 7.7 in the matrix space [488]; in contrast, LUVs with mono-anionic lipids only reduced the pH to ~5.3 at the membrane interface [487]. The reduced pH at the membrane interface from CL, linearly associated with increased proton (H+) concentration (~700 to ~800) [487], is the reason why ATP production is doubled in mitochondrial models with cristae compared to those without [409]. At the same time, the increased H+ concentration at membrane surfaces may cause accumulation of •OOH, the protonated form of O2•− [480].
•OOH remains adsorbed at polar headgroups longer than other ROS tested [295]; therefore, a low pH at membrane interface that is favorable for enhanced ATP synthesis could also initiate peroxidation cascades. As such, even though the proper functioning of CL is prerequisite for optimal mitochondrial respiration and ATP production, peroxidation of CL in mitochondria is an inevitable, natural, physiological process that can deteriorate pathologically [239,241,405,489,490,491,492,493,494,495,496,497,498] unless properly counterbalanced by the continuous synthesis [420] and/or uptake of high levels of melatonin. Melatonin is known for its role in maintaining systemic energy homeostasis [499]. In the mitochondria of brown and beige adipose tissue, CL biosynthesis is robustly induced upon cold exposure [500,501] because CL can bind tightly to uncoupling protein 1 (UCP1), stabilizing its conformation and enhancing functionality [502]. The ability of melatonin to protect CL from peroxidation may account for the increased thermogenic response in Zücker diabetic fatty (ZDF) rats via the restoration of UCP1 mRNA expression, increased mitochondrial mass and brown adipose tissue (BAT) weight, as well as enhanced mitochondrial OXPHOS activities in complex I and IV [503].
4.4. Melatonin May Regulate Glycolytic G Bodies by Increasing ATP
As early as 2002, melatonin was found to increase mitochondria OXPHOS activity and elevate the production of ATP [504]. Recent experimental and theoretical studies have presented different mechanisms explaining how melatonin may function as a glycolytic, such as stimulating the SIRT3/PDH axis in vitro to reverse the Warburg phenotype in lung cancer cells [505], converting cells to a healthy phenotype by inhibiting hypoxia-inducible factor-1α to encourage OXPHOS over glycolysis induced by hypoxic conditions [506], downregulating pyruvate dehydrogenase kinase (PDK) to increase acetyl CoA synthesis [507,508], or elevating α-ketoglutarate (α-KG) levels in macrophages to promote M2 polarization that favors OXPHOS over glycolysis [509,510].
Interestingly, in Saccharomyces cerevisiae and human hepatocarcinoma cells challenged with hypoxic stress, the non-canonical RNA-binding proteins in glycolytic enzymes have been observed to promote phase separation [511] that facilitate and maintain the assembly of glycolysis enzymes into cytoplasmic, membraneless glycolytic G bodies that increased glycolytic output during hypoxia [512]. Melatonin is able to increase ATP concentration in cells [503,504,505]; therefore, the switch between OXPHOS and glycolysis could possibly be part of the effect where high ATP concentration dissolves MLO aggregations. Molecular dynamics simulation experiments revealed that the propensity for self-aggregation enhanced the role of ATP as a hydrotrope, preferentially binding to polymers to unfold hydrophobic macromolecules and disrupting the aggregation process of hydrophobic assemblies via the introduction of charges to the macromolecules [513]. These results may explain previous observations where a high cytosolic ATP:ADP ratio readily suppressed glycolysis, whereas the closure of VDAC channels resulting in lower ATP:ADP ratios in cytosol activated glycolysis in vitro [514]. Alterations to the glycolytic pathways are often observed during the early stages of neurodegenerative diseases where mitochondrial dysfunction and reduced ATP levels may contribute to protein aggregation [515]. Increasingly, the pathogenic aggregation of MLOs such as stress granules, p53, FUS, TDP-43, and tau exhibiting dysregulated LLPS is believed to play a major part in the development of neurodegeneration and cancer [12,516,517,518].
5. Melatonin May Attenuate the Stress-Induced Aggregation of Pathological MLOs via Post-Translational Modification and RNA Modification in an ATP-Dependent Manner
Biomolecular condensates containing protein, RNA, and other nucleic acids [1] are formed by LLPS under changing endogenous or exogenous conditions, including stress responses [3] and signal transduction [4,5], as well as genome expression, organization and repair [6]. In eukaryotes, gene transcription is executed by transcription factors, including p53 [519,520], TDP-43 [521,522], and FUS [523], containing IDRs that form condensates to compartmentalize and assemble necessary factors [6,524]. Transcription is essentially a nonequilibrium process that employs RNA products to provide a two-way dynamic feedback control in the regulation of electrostatic interactions in transcriptional condensates [108,525,526] where RNA products recruit proteins to form molecular scaffolds driving phase separation, whereas many essential RNA processes such as transcription, transport, and metabolism are regulated by phase separation [527]. Under stress, different RNA species are often incorporated by different MLOs because unique RNA–protein interactions can define biophysical properties of MLOs such as stress granules [528,529]. Cells rely upon RNA to regulate condensates because RNA molecules contain powerful electrostatic forces due to the high negative charge densities buried in their phosphate backbones [530,531,532]. Therefore, a low level of RNA with a negative charge could interact with positively charged proteins to promote phase separation and the formation of transcriptional condensates, whereas high levels of negatively charged RNA could repel proteins with a positive charge to dissolve condensates [525].
Cells also employ post-translational modifications (PTMs) to induce non-equilibrium thermodynamic chemical reactions in order to tune the molecular interactions of key condensate components where external energy input drives reactions out of equilibrium to control the size and number of MLOs [533]. PTMs, including phosphorylation, acetylation, glycosylation, methylation, ubiquitination, and SUMOylation [11,79], may function as phase-separation on–off switches [60,534] or rheostats that actively adjust the dynamics of LLPS during condensate formation [79,535]. Under different cellular conditions, including stress, PTMs can either promote or suppress LLPS by modulating protein valency and interaction intensities [79,351,536], as well as recruit or exclude proteins from condensates [537,538].
5.1. Cellular Stress and Mutations Drive Dysregulated LLPS to Form Pathological Aggregates in Neurodegenerative Disorders
Cellular stress in eukaryotes activates defense mechanisms such as stress granules (SGs) that can promote either survival or apoptosis [539]. Integral to cellular stress management adaptations [540], SGs are membraneless, cytoplasmic complexes comprising non-translating mRNA and RNA-binding proteins (RBPs) [541] assembled from RNA–RNA interactions [542]. Type I stress, including hypoxia, heat-shock, and arsenite [539], can induce the formation of SGs to increase cell survival by reprogramming cellular metabolism through the modulation of cytoplasmic mRNA functions [540,541]. Oxidative stress induced by tellurite has recently been documented to assemble bona fide cytoplasmic and nuclear SGs in vitro [543]. Under oxidative stress, increased SGs in senescent cells is one of the key post-transcriptional gene expression regulators [544]. The rapid and dynamic range of gene expressions in immune cells may also be regulated by mRNA translation control modulated by SGs [545]. Interestingly, SGs have been found to host many of the proteins that contain long segments which are intrinsically disordered [546,547] and capable of LLPS to form pathological aggregates [548,549] associated with diseases such as neurodegeneration [550,551] and cancer [552]. It has been proposed that the aggregation of pathological TDP-43, FUS, and tau is processed through the stress granule pathway [553]. The fact that degenerative diseases have been associated with IDR-containing pathological aggregates of p53, tau, TDP-43, and FUS [554,555,556,557], which are also important transcription factors [519,520,521,523] associated with SGs, emphasizes the relevance in the interactions between these MLOs for the dynamic assembly of SGs under stress conditions inhibiting the initiation of mRNA translations, and the necessity of their timely, rapid disassembly upon stress removal [558].
Under cellular stress conditions, phosphorylation can initiate the formation of SGs [559] and also increase tau-phosphorylation which, in turn, appears to increase SG formation [560,561]. Once formed, the subsequent colocalization and interactions between phosphorylated tau and RNA-binding proteins abundantly present in SGs could further enhance the aggregation of insoluble cytotoxic neurofibrillary tangles (NFTs) [553,562,563]. Under cellular stress, TDP-43 and FUS are released from the nucleus where they reside under physiological conditions into the cytoplasm and assemble with SGs [562]. The aggregation of RBPs such as FUS, TDP-43, and even p53 [564] in the cytoplasm has been reported to be linked to phase separation which is regulated by RNA concentration. Both FUS and TDP-43 contain intrinsically disordered, prion-like, low-complexity domains that are soluble in the nucleus due to high levels of RNA, but phase-separate into aggregates driven by lower RNA concentrations in cytoplasm [28,57,565,566]. In the same manner, a low RNA:protein ratio (1:50) caused the formation of large amorphous p53 aggregates in vitro, whereas a higher ratio of 1:8 inhibited aggregation [567,568]. If stress is not resolved in a timely manner, aggregations may become irreversible and insoluble [569]. Prolonged physiological stress and/or mutations in genes coding for TDP-43 [570,571] and FUS [572,573] can lead to enhanced stress granule formation, which could accelerate the pathological aggregation of these proteins in neurodegenerative diseases [553,574,575]. A single substitution of only one residue in a protein sequence, commonly referred to as missense mutation, can also affect macromolecular stability, cellular localization, and perturb macromolecular interactions [576] during LLPS.
Missense mutations associated with diseases are found mostly within IDRs [577]. These mutations in IDRs can cause the dysregulation of LLPS by changing the threshold concentration for condensate formation [578,579,580], modulating the exposure of the aggregation-prone regions [577], and interfering with RNA interactions [27]. IDR mutations are capable of disrupting phase separation in important cellular processes, turning dynamic liquid droplets into aberrant fibril aggregates [581,582,583] to cause mislocalization or the gain/loss of functions [27,584]. TDP-43, an important RNA-binding protein, is the major disease protein where the pathological form is hyperphosphorylated and ubiquitinated in ALS [585]. The C-terminal domain of TDP-43 is a prion-like domain (PLD) [586] which is intrinsically disordered [587] and harbors almost all ALS-causing mutations that drive the LLPS of TDP-43 to associate with stress granules to form pathological aggregates or amyloid fibrils [588,589]. These mutations disrupt LLPS by inhibiting interaction and helical stabilization to enhance aggregation and disrupt protein interactions [590,591,592,593].
Intriguingly, ATP has recently been reported to exhibit a unique biphasic relationship with TDP-43 PLD. At a molar ratio of only 1:25 (PLD:ATP), TDP-43 PLD was induced to undergo LLPS to start forming liquid droplets in a dose-dependent manner where many droplets could be produced at a 1:100 molar ratio. Further increases in ATP, in contrast, led to a reduction in droplet formation. At 1:750, only a few droplets could be detected, and at 1:1000, all droplets were disassembled by ATP. Importantly, in the absence of ATP, TDP-43 PLD was unable to phase-separate into droplets [53]. Neurons have been reported to produce up to 5 mM of ATP in cytoplasm through glycolysis [594], whereas the cytoplasmic concentration of TDP-43 in neurons may be several thousand times lower [53,569,595,596]. Therefore, under physiological conditions, ATP could regulate most IDRs by modulating physicochemical properties, conformations, dynamics, LLPS and aggregation [53]. At physiologically relevant concentrations, ATP has been reported to bind tightly with TDP-43, enhancing thermodynamic stability and prohibiting LLPS-induced pathological fibrillation [597].
Mutations in fused in sarcoma (FUS) are associated with ALS pathology, and are believed to be a major cause behind familial ALS [598,599]. Under physiological conditions, FUS is a multifunctional, DNA-/RNA-binding protein responsible for maintaining genomic stability, RNA metabolism, and stress responses [600]. Under stress conditions, wild-type (WT) FUS may remain nuclear whereas mutant mislocalized FUS in cytoplasm are assembled into stress granules [47,600]. WT FUS exhibit dynamic RNA interactions whereas mutants display altered, static interactions with RNA, leading to a buildup of aggregates in aberrant phase separations [27]. In addition, mutant FUS exhibit a gain-of-toxic mechanism that delay the assembly and alter the structure and dynamics of SGs [572].
Physiological FUS is a transcription factor [523] which has been identified to regulate circadian gene expression via a novel feedback effect [601]. FUS mutations interfere with RNA metabolic pathways and suppress protein translation [602]. Mutant FUS (R52aC) disrupted the feedback effect to lower the expression of the E box-containing core circadian gene Per2 by binding to RNA-/DNA-binding splicing factor protein (PSF) [601]. Similarly to TDP-43, ATP has also been identified to enhance the LLPS of FUS at low concentrations, but dissolves FUS aggregates at higher concentrations [51]. Phosphorylation is an important post-translational modification used by cells to regulate transcription factors [603,604,605] including FUS. In yeast models, phosphorylation of the low-complexity domain in FUS not only disrupted phase separation, but reduced toxicity and the prion-like aggregation propensity of FUS [580]. The synthesis of melatonin in neuronal mitochondrial [420] fulfils a range of important functions, including balancing oxidative stress to maintain relevant physiological levels of ATP and possibly to ensure the proper execution of PTMs such as the increase in phosphorylation to enhance neurogenesis in the mouse subventricular zone (SVZ) that has been reported in experimental studies [606,607].
5.2. Melatonin Inhibits/Disaggregates Pathological Tau Neurofibrillary Tangles and May Regulate the Phosphorylation of Tau in Neurodegenerative Disorders
Phosphorylation is one of the most important PTMs that can control the assembly/disassembly of MLOs [608] as well as stabilize or destabilize MLOs including G bodies [512] and p53 [609]. Cells rely on phosphorylation as rapid, reversible responses to different stimuli by changing the physicochemical properties of proteins during phase separation multivalent interactions [79,538]. Phosphorylation establishes covalent bonds between phosphoryl and amino acid hydroxyl groups using the terminal phosphate group in ATP [610]. The phosphoryl group is negatively charged; therefore, the attachment turns the polar, uncharged residue into a negatively charged amino acid [60]. In theory, charged residues can prevent protein aggregation and increase the solubility of water-soluble proteins [611]. Indeed, phosphorylation has been observed to modulate the size of MLOs [361,535], disassembling synapsin 1 droplets [612] and preventing membrane-attached zona occludens (ZO1) from phase-separating into droplets that form tight junctions in tissues [613]. Similarly, in C. elegans, phosphorylation also promoted IDR granule disassembly, whereas dephosphorylation promoted granule assembly [614]. Under different cellular conditions including stress, PTMs can either promote or suppress LLPS by modulating protein valency and interaction strengths [79,351,536], as well as recruit or exclude proteins from condensates [537,538].
The ATP-dependent DEAD-box helicase [307] DDX3X responsible for initiating NLRP3 inflammasome aggregation is dependent upon phosphorylation-associated IFN promoter stimulation [304,310,615,616]. When the conserved, eukaryotic, integrated stress response (ISR) pathway is activated by external stress stimuli including hypoxia, nutrient deprivation, viral infections, as well as intrinsic ER stress [617], the phosphorylation of eukaryotic translation initiation factor 2 alpha (eIF2a) on Ser51 [618,619] triggers the formation of stress granules as adaptive homeostatic responses to promote survival and restore homeostasis [620,621,622,623] via mRNA translational modification that may involve the repression of protein synthesis [541,624,625,626]; however, dephosphorylation of eIF2a blocks the ISR pathway [627]. The formation of SGs via eIF2a-dependent and -independent pathways [628] during stressful conditions allows cells to conserve energy by reducing global protein synthesis that may prevent the accumulation of harmful misfolded proteins, while preserving the selective translation of genes that assist in survival and recovery [629]. Results from in vitro experiments suggest that SGs form phase-separated, dynamic structures from IDR-containing proteins that can mature over time into stable structures [26,581,582,622,630]. The clearance of stress granules may be carried out by autophagy [631] or the disassembly of shells and cores via an ATP-dependent process [622]. In AD pathology, the hyperphosphorylation of tau proteins thermodynamically facilitates the oligomerization of pathological intracellular neurofibrillary tangles [632,633].
AD is associated with the aggregation of Aβ as well as the intracellular deposition of neurofibrillary tangles (NFTs) of tau, a major neuronal protein with important physiological functions of stabilizing and promoting the assembly of microtubules (MTs) in the central nervous system (CNS) [634,635]. The intrinsically disordered, highly soluble nature of tau in solution facilitates binding to MTs [636]. Under physiological conditions, tau readily converts between soluble monomers and phase-separated droplets that disassemble quickly. Physiological tau droplets support important biological functions specific to the cellular compartments where they are formed [637,638], such as myelination [639,640], axonal transport [639,641], motor function [642], learning and memory [643], neuronal excitability [644], as well as glucose metabolism [645,646,647], DNA protection [648], and gene transcription [520]. In neurons, phase-separated tau droplets enhance the nucleation of MTs, promoting tubulin polymerization by decreasing critical concentration [649,650]. Physiological tau condensates not only stabilize dynamically unstable MTs [651], but can form islands on the surfaces of MTs, protecting them from severing enzymes [652,653]. However, phosphorylation-dependent LLPS that forms physiological tau droplets can also initiate the production of tau amyloids upon the coacervation of positively charged microtubule-binding domains with negatively charged molecules [29,636,637,654]. The deposition of fibrillar hyperphosphorylated misfolded tau aggregates in the brain is accepted as a key biomarker for AD and tauopathies [655,656].
LLPS of tau has been demonstrated to promote amyloid aggregation [657]. Tau can undergo electrostatically propelled LLPS with itself in simple coacervation or with a large number of RNA polyanions in complex coacervation [657,658,659,660]. Experimental model systems have revealed that the pathological aggregation of tau is predominantly mediated by hydrophobically driven LLPS which leads to the dehydration of interfacial water, further amplifying hydrophobic associations [661]. Such strong hydrophobic attractions are believed to be the cause for hyperphosphorylated tau in tauopathies [662,663,664,665]. Even though the hyperphosphorylation of tau is a transient, reversible physiological process, in neurodegenerative disorders such as AD, abnormal hyperphosphorylation of tau is resistant to dephosphorylation and proteolysis [666,667], often resulting in a 3–4-fold increase in accumulation compared to normal brains [668,669,670]. Abnormally hyperphosphorylated tau is disassociated from MTs and loses its MT-stabilizing physiological functions [662,671]. The pathogenic phosphorylation of tau may also be site-specific; the phosphorylation of multiple tyrosine residues including Tyr-310 has been demonstrated to inhibit tau aggregation [672]. Even though hyperphosphorylated tau precedes the appearance of NFTs [673], altering its important physiological role in DNA protection [648,665,674,675], there are unanswered questions surrounding the phosphorylation and hyperphosphorylation of tau [676].
Tau phosphorylation has been proposed as a neuroprotective mechanism [677] where phosphorylated tau sequesters redox active heavy metals [678,679] and NFTs may provide antioxidant defense against oxidative damage [680,681], whereas hyperphosphorylated tau protects neurons from apoptosis [682,683]. An experimental study that phosphorylated specific microtubule binding sites of tau, including K18 and pS356/pS262 and employing a total chemical synthetic approach, discovered that the hyperphosphorylation of K18 inhibited aggregation, seeding activity, binding to microtubules, and microtubule polymerization [684]. These results support the hypothesis that the phosphorylation of tau may be a protective mechanism, and contradict the prevailing concept of the pathogenic nature of hyperphosphorylated tau [685,686,687] which could impair cell viability [688] and accelerate the progression of cognitive impairments [655,689,690,691].
The use of melatonin in neurodegenerative disorders has been extensively studied and reviewed [333,692,693]. Numerous experimental and theoretical studies successfully demonstrated the high efficacy of melatonin in attenuating various pathological effects of tau hyperphosphorylation, employing different mechanisms, including: activating the phosphorylation of p-Akt-Ser473 in a PI3K-dependent manner [694,695]; inhibiting GSK3β-activated tau hyperphosphorylation [696,697,698] to decrease Aβ1–42-induced memory impairment, synaptic disorder, and tau hyperphosphorylation-associated neurotoxicity in C57BL/6N mice [699]; restoring autophagic flux, inhibiting caspase-3 activation, and reducing abnormal protein aggregation to ameliorate tau-pathology-related symptoms such as oxidative stress, neuroinflammation, cognitive impairment, cell death, and tau hyperphosphorylation in experiments using humans/rats ex vivo (10 μmol/L melatonin) and mice in vivo (10 mg/kg melatonin) models [700]; and decreasing calpain expression/activation, GSK-3β activation [697]. Melatonin decreased ER stress induced by kainic acid, easing tau hyperphosphorylation and memory impairment in mouse models, although substitution with vitamin E did not produce the anticipated antioxidant effects on the reduction in ER stress [701]. Even the use of the melatonin receptor agonist agomelatonin was able to prevent tau protein phosphorylation and oxidative damages induced by Aβ25–35 in pheochromocytoma (PC12) cells by activating melatonin-PTEN/Akt/GSK3β signaling [702]. The majority of these experiments showed an association between the reduction in tau hyperphosphorylation-related neurotoxicity and activation of the Akt-PI3K/GSK3β signaling pathway by melatonin. The fact that PI3K is a pro-survival, pro-stress-granule kinase that promotes the assembly of stress granules [703] adds an additional layer of complexity to the mechanisms employed by melatonin in the attenuation of tauopathies.
Even though melatonin is able to ameliorate tau-pathology-related symptoms such as oxidative stress, neuroinflammation, cognitive impairment, cell death, and tau hyperphosphorylation in vivo [700], the fact that Luengo and colleagues supplemented C57BL/6J male/female mice with melatonin only after all symptoms of tauopathy were firmly established (7–28 days) may imply that a further promotion of SG formation via activation of AKT-PI3K was possible, potentially increasing the additional pathological aggregation of tau because the colocalization and interactions between phosphorylated tau and RNA-binding proteins abundantly present in SGs may enhance the assembly of insoluble cytotoxic NFTs [553,562,563]. Similar to the multiple pathways and mechanisms employed by melatonin in effecting the switch from glycolysis to OXPHOS [506,507,508,509,510], there may yet be another compelling reason that could explain how melatonin at pharmacological doses (10 mg/kg in vivo) [700] exerts neuroprotective effects in tauopathy.
An in vitro study on Neuro2A cells reported that melatonin at 10 μM concentration reduced intracellular ROS levels induced by tau aggregate treatment, and at 50 μM, melatonin reduced phospho-tau as well as GSK3β mRNA and subsequent protein levels. Melatonin increased cell viability in tau-exposed neurons in a dose-dependent manner, with 80% viability observed at 20 μM melatonin and a complete reversal at 200 μM, compared to only a 60% viability in controls without melatonin [704]. In an earlier study, the same group had reported that melatonin at strengths between 200 and 5000 μM failed to deter the aggregation of full-length tau. However, distinct morphology of small, broken tau fibrils were seen in the presence of either 1000 [705] or 5000 μM [352] melatonin. Furthermore, 5000 μM melatonin disaggregated tau fibrils by 54%, whereas 100 μM achieved only a ~14% effect [352]. It is possible that melatonin interacts with histidine residues to destabilize the assembly of aggregates [352] in a manner similar to how it disrupts salt bridges in Aβ, because tau phosphorylation alters side chain conformations through the formation of a network of salt bridges [706]. Salt bridge interactions were also observed in Aβ-mutated tau complexes assembled from Aβ peptides and mutated tau [707]. Earlier studies have reported that 300 μM melatonin interacted with hydrophobic segments in Aβ1–40 and Aβ1–42 to inhibit the formation of β-sheet and/or amyloid fibrils [708], and the inhibition of β-sheet and amyloid fibrils in samples containing 250 μM of Aβ1–40 and Aβ1–42 with only 100 μM of melatonin could not be replicated in control experiments using a potent free radical scavenger N-t-butyl-a-phenylnitrone (PBN), or a melatonin analog 5-hydroxy-N-acetyl-tryptamine (NAT) [337]. Even though melatonin could dissolve fibrils [709] by disrupting inter-peptide salt bridges between side chains Asp23 and ly28 [710,711] critical to β-sheet formation [712], the concentrations of 1000 [705] or 5000 μM [352] required to disassemble tau fibrils are significantly higher than the 100–300 μM melatonin used to inhibit β-sheet and amyloid fibrils [337,708], or the complete reversal of cell viability in tau-exposed neurons achieved with only 200 μM melatonin [704]. More importantly, if PI3K-induced SG activation and tau hyperphosphorylation serve pro-survival functions, then there should yet be another mechanism that could convert physiological phase-separated tau droplets into highly ordered pathogenic fibrils implicated in various neurodegenerative disorders that may be rescued by the presence of melatonin.
5.3. Melatonin May Ameliorate Pathological Tau Fibrillation by Protecting Lipid Composition in Membranes and Lipid Rafts
MLOs are found abundantly in the nucleus, cytoplasm, and on the membranes of almost all eukaryotic cells [82], where they perform important biological functions that may regulate receptor/transmembrane protein signaling via the alteration of protein binding affinity and the modulation of local environments [86]. As such, membranes become indispensable to LLPS due to their ability to concentrate and change protein thresholds during phase separation [79], facilitated largely by lipid raft signaling [96]. Alterations in membrane fluidity and lipid composition that cause dysfunctional signaling in lipid rafts have been associated with neurodegenerative disorders [89,90,97,713]. Neuronal membrane lipid rafts, co-localized with several microtubule proteins, have been observed to maintain stability and integrity in mature cortical neurons, where the disruption of raft signaling by exogenous agents (MBC, D-PDMP) causes rapid neuritic retraction that precedes neuronal death [714]. The association of tau with plasma membranes appears to be regulated by phosphorylation [715,716], where underphosphorylated tau-proline-rich regions induce membrane localization [717], and increase the phosphorylation-initiated disassociation of tau from membranes, potentially resulting in tau hyperphosphorylation and the eventual assembly of insoluble pathogenic fibrils [718].
Mutations in the Niemann–Pick type C (NPC) gene cause disturbances in cholesterol metabolism in lipid rafts [719], where a dramatic reduction in membrane raft cholesterol in NPC1-deficient cells leads to the hyperphosphorylation of tau at multiple sites [720]. Experimental evidence from a mutant human tau and APOe knockout (htau-apoe−/−) mouse model demonstrated the formation of tau filaments elevated intraneuronal unesterified cholesterol, which may result in a vicious circle where tau fibrils alter cholesterol homeostasis and disturb cholesterol metabolism which continues to promote tau pathology [721]. Physiological tau proteins are flexible, highly charged, and soluble, and can be extremely active on membrane surfaces, interacting favorably with anionic lipids at air–water interfaces [74]. A recent in vitro study revealed that tau–anionic lipid membrane interactions catalyzed the misfolding and assembly of tau, transitioning from random coil conformations into β-sheet aggregates that fueled tau fibrillation and deposition [74]. The binding and insertion of tau into anionic lipid membranes not only structurally compacted and misfolded tau into extended β-sheet aggregates, but disrupted lipid packing, inducing membrane morphological changes [74] including membrane roughness [722]. As a result of tau association, well-defined circular liquid-condensed (ordered) Lc domains [723] in anionic 1,2-dimyristoyl-sn-glycero-3-phospho-(1′-rac-glycerol) (DMPG) monolayers used as mimics for anionic lipids in neuronal cells became less defined and subsequently fused with other Lc domains [74]. Increased unesterified cholesterol in membranes from tau fibrillation [721] may cause Lc domains to become more fluid, mechanistically deforming membrane bilayer structure [724]. Melatonin has been reported to interact with cholesterol [321], binding competitively to lipid molecules to displace cholesterol [319]. Lc domains that have become more fluid will transition into Lo lipid raft domains [721,724] that could potentially potentiate the formation of enlarged lipid rafts (inflammarafts) [196,198].
Melatonin may regulate lipid dynamics and composition, modifying the lipid hydrocarbon chain order to promote phase separation in ternary membrane models [318,319], as well as preserving nanoscopic lipid raft domains by stabilizing lipid Lo–Ld phase separation over a range of temperatures [350]. The ability of melatonin to penetrate and re-order lipids in membranes provides insight into its neuroprotective effects against tauopathy. Tau interacts favorably with anionic lipids at membrane interfaces [74]; therefore, the accumulation of melatonin in electron-dense anionic headgroup regions to form fluid domains that enrich lipid membranes [341] can potentially disrupt tau–lipid interactions. Indeed, in addition to dissolving tau fibrils, the addition of 1000 μM melatonin reversed all membrane roughness induced by tau aggregates in neuro2A cells in vitro [705,722,725].
The tumor suppressor p53 has been found to interact with tau and Aβ, forming pathological aggregates that result in the mislocation and impairment of its essential physiological DNA repair functions [726,727,728]. p53 has been seen to cause a shift in membrane phospholipids from mono-unsaturated acyl chains towards saturated phospholipid species that may potentially contribute to cell survival [729]. However, gain of function in p53 has also been observed in tumor cells with altered lipid raft composition comprising higher cholesterol levels [730]. The influence of melatonin over tumor-suppressor p53 may also explain its effectiveness against tauopathies.
5.4. Melatonin Regulates p53 and Other Biomolecular Condensates through the ATP-Dependent Ubiquitin–Protease System in Neurodegenerative Disorders
Often called the “guardian of the genome” [731], p53 is arguably the most studied mammalian transcription factor [732,733] because it maintains genomic stability by inducing the transcription of thousands of genes that may regulate the cell cycle in heterogeneous responses to different stimuli, allowing cells to adapt to varying types and levels of stress [733,734,735]. After its initial discovery in 1979 [736], p53 was intensely studied for the loss of its apoptotic, tumor-suppressing capacities [737,738,739] through inactivation by frequent mutations detected in different cancers [740,741,742]. Continued explorations of this gene have led to increased understanding of the complexity in its ability to promote survival and growth [743] through the regulation of metabolic and antioxidant pathways [744] in addition to cell elimination [745]. p53 was found to induce the expression of glutaminase 2 (GLS2) under physiological conditions to enhance mitochondrial respiration, ATP production, and antioxidant defense that protected cells from oxidative stress [746]. However, under a highly stressed environment with increased ROS that induced DNA damage, p53 suppressed the Nrf2-dependent activation of antioxidant genes, initiating cell cycle arrest and apoptosis to eliminate unrepairable damages [747]. p53 has been found to be enriched in DNA damage response effectors such as 53BP1, and the aberrant phase separation of 53BP1 impaired the activation of p53, preventing proper DNA recognition and repair [748]. Mechanisms including transcription [519], PTM [749,750,751], and degradation by the ubiquitin–protease system (UPS) [752,753,754,755,756] can fine-tune the regulation of p53 [757].
More than 50% of all human cancers have been associated with missense [758] and/or synonymous mutations of the p53 gene [742,759,760,761], where close to 95% of these mutations are located in the DNA-binding domain (DBD) [12,742,762,763,764,765] which is regulated by interactions with the extensive intrinsically disordered regions of the C- and N-termini that flank the DBD [547,766,767,768]. IDRs are believed to modulate LLPS [557]; therefore, it is not surprising that aggregates of both wild-type and mutant p53 have been observed in cancer cells and tissues and are regarded as a hallmark for p53 inactivation [769]. In addition, the formation of amyloid oligomers and fibrils in the DBD of p53 may produce prion-like characteristics [770,771,772] that can result in the gain or loss of functions [773]. More importantly, p53 stabilization through activation is tightly regulated by the UPS, which degrades p53 by default. Nevertheless, this “default degradation” process can be evaded through stabilization of the intrinsically disordered C- and N-termini of p53 [754].
5.4.1. Aberrant Phase Separation/Droplet Formation May Cause Pathological Prion-like Aggregation and Inactivation of p53 in Neurodegenerative Disorders
Recent in vitro studies have demonstrated that formation of highly fluid p53 droplets at neutral and slightly acidic pH, and a low-salt environment is mediated by its N- and C-termini disordered domains [609]. The DNA binding domain (p53C) of p53 mutants also undergoes LLPS but evolves at a faster speed than wild-type p53C into solid-like phase transitions, resulting in the formation of amyloid-like aggregates [517]. Molecular crowding agents such as polyethylene glycol (PEG) can promote LLPS droplet formation in both wild-type and mutant p53; however, phosphorylation, DNA, and ATP can suppress the process and dissolve p53 droplets [517,609]. It has been proposed that LLPS droplet formation acts as a functional “on-off” switch for p53, where the compartmentalization of p53 into droplets prevents p53 transcriptional functions such as gene targeting and binding. Upon stress or PTM modification (phosphorylation) activation, p53 is released from the droplets to execute its physiological functions [609].
A recent study demonstrated that wild-type p53 expressed in living yeast not only had the capacity to form liquid-like, dynamic, unstable droplets that appeared and disappeared in response to the presence or absence of stress, respectively, but when overexpressed, was able to propagate into true amyloid-like prions that could seed other molecules, and at the same time suppressed p53 transcription activities to precipitate tumorigenesis [774], confirming earlier experimental observations where a seed of mutant p53C oligomers and fibrils accelerated wild-type p53C in a prion-like manner [770]. Both wild-type and mutant p53 proteins exhibited aggregation kinetics and morphology, closely resembling classical amyloidogenic proteins such as Aβ and α-syn, with mutants displaying enhanced amyloidogenicity and accelerated aggregation [775] which contribute to functional loss [770,773,776] and gain [777,778] associated with tumorigenesis [775,779].
In AD human brain tissues and animal models, the interaction between p53, pathological tau oligomers, and Aβ form aggregates resulting in the mislocalization and impairment of its important physiological functions in DNA repair [726,727,728]. Compared to healthy elderly controls, p53 in AD patients exhibited a 100% increase in p53 in the superior temporal gyrus, and induced the phosphorylation of tau in HEK293a cells in vitro [728]. Dysregulation of p53 such as unfolded p53 caused by oxidative stress [780] is a reliable biomarker for AD [781,782], whereas overexpression of the truncated p53 isoform p47 (Δ40p53 or p44) [783] in mice accelerated aging and increased tau fibrillation [782,784,785]. Tau was recently reported to have increased wild-type p53 expression post-translationally through the abnormal modification of MDM2, the E3 ubiquitin ligase which negatively regulates p53 [786,787,788,789]. Since the discovery of ubiquitin-positive aggregates in various neurodegenerative diseases, there has not been any clear consensus on the exact nature of the involvement of the ubiquitin–protease system (UPS) in neurodegenerative disorders [790].
5.4.2. The Potential Regulation of Ubiquitination/SUMOylation in MLO Assembly and Dissolution by Melatonin in an ATP-Dependent Manner
The main function of UPS is to degrade and eliminate abnormal proteins damaged by oxidative stress and/or mutations after they are covalently bound to ubiquitin in an ATP-dependent pathway [791]. Many MLOs, such as stress granules formed as a result of RNA interactions, rely on ATP-dependent UPS-associated proteins such as ubiquitin complexed within their structures for proper assembly and disassembly [32,792,793,794,795]. Ubiquitin (Ub) is a highly conserved protein that targets proteins for degradation via covalent binding, and ubiquitination is an enzymatic cascade involving ubiquitin-activation (E1), ubiquitin-conjugation (E2), and ubiquitin-ligation (E3) which relies on ATP to provide energy to ultimately form an isopeptide bond between Ub and the targeted substrate [18,796]. LLPS can promote and enhance ubiquitination by providing a scaffolding of necessary proteins to accelerate ubiquitination processing, and aberrant LLPS may result in dysfunction of the UPS in neurodegenerative disorders [797]. Ubiquitin-positive protein aggregates have been identified in many neurodegenerative diseases [798]; therefore, it is believed that the failure to eliminate ubiquitinated proteins in the brain is one of the major causes of neurodegeneration [799]. Alternatively, it is possible that neurotoxicity arises from a deficiency of free Ub that could reduce proteasome activity rather than the accumulation of ubiquitinated aggregates often observed in neurodegenerative diseases [800]. Even though Ub can bind to Aβ peptides, interfering with clearance pathways, Ub bound non-covalently to Aβ has been observed to exhibit a lower tendency to aggregate, significantly reducing fibril formation and delaying amyloid fibril aggregation in a dose-dependent manner [801].
In eukaryotes, the UPS may be the most complex, extensive, cytosolic proteolytic enzyme system that performs essential functions [802] including cell growth and cycle control [803], apoptosis [804,805,806], inflammation [807,808], transcription [809,810], and signal transduction [811]. The UPS exerts a critical influence over protein quality control in neurodegeneration [812], mediating the degradation of more than 80% of normal and abnormal intracellular proteins in the human body [813,814]. The proteasome is the only known ATP- and ubiquitin-dependent protease in both eukaryotes and bacteria [815,816,817], and ubiquitin-related molecules have been reported to participate in the regulation of LLPS in the formation of MLOs [795,818,819]. The proteasome contains six distinct ATPase subunits that cooperatively coordinate substrate binding, deubiquitination, unfolding, and translocation [820]. The failure of a single mutated ATPase decreased the overall rate of ATP hydrolysis by 66%, and reduced the 2–3-fold ubiquitinated substrate stimulation of ATPase activity to zero [821]. Substrate degradation is directly linked and is proportional to ATP hydrolysis; therefore, it is not unreasonable to assume that ATP hydrolysis may be the rate-limiting step in UPS [821]. Thus, the maintenance of high cytosolic levels of ATP in the millimolar range by mitochondria [39,40] is not only requisite for the proper assembly and disassembly of MLOs; it is potentially indispensable for substrate degradation by UPS [821].
The theoretical maximum of ATP calculated from simultaneous measurements of extracellular acidification and oxygen consumption indicated that OXPHOS ATP production was close to or more than 16 times above glycolysis, at 31.45 ATP/glucose (maximum total yield 33.45) and 2 ATP/glucose, respectively [822]. Whether mitochondria can use OXPHOS to generate ATP is dictated by the fate of pyruvate upon glucose oxidation [823]. In mitochondria, pyruvate drives ATP production by OXPHOS and the TCA cycle via different enzymes. Pyruvate dehydrogenase complex (PDC) irreversibly converts pyruvate, NAD+, CoA into acetyl-coA, NADH and CO2. The phosphorylation of the E1α subunit of pyruvate dehydrogenase complex (PDC) by pyruvate dehydrogenase kinase 2 (PDK2) blocks the entrance of acetyl-coA into the tricarboxylic acid (TCA) cycle, inhibiting the OXPHOS production of higher ATP [824,825,826]. OXPHOS is believed to be the main initial energy production pathway used by neurons to fuel activities [827]; thus, alterations in PDK enzymes and/or their interactions with neurons and glial cell metabolism may affect the development of neurological disorders [828]. Decreased expression of PDC has been observed in post-mortem brain tissues from AD patients [829] as well as transgenic female AD mice [830].
VDAC is the gatekeeper that controls the export of ATP out of mitochondria into cytosol and the import of essential respiratory substrates such as ADP and Pi into mitochondria [395,399]; therefore, it is not surprising that VDAC has been demonstrated to be neuroprotective against Aβ-induced neuronal mortality [831] and essential for neurite maintenance and the prevention of demyelination after spinal cord injury [832]. The interactions between VDAC, APP, and Aβ in lipid rafts of neurons from the frontal and entorhinal cortex of human brains affected by AD showed enhanced dephosphorylation of the enzyme that correlated with cell death [833]. As discussed in Section 3.9, melatonin protects the functionality of the VDAC–CYB5R3 complex by reducing oxidative stress, lowering ROS that may induce lipid peroxidation, which can alter raft composition, thickness, curvature and elasticity [291] that may impact VDAC ion-channel opening/closure according to the force-from-lipid principle [382,383,384,385]. VDAC expressed in the plasma membranes of HT22 mouse hippocampal neuronal cells were quiescent under control conditions with normal ATP and an absence of apoptotic signals. Serum deprivation increased ROS and induced VDAC opening in the plasma membranes of hippocampal HT22 cells, resulting in mitochondrial dysfunction and increased apoptosis and autophagy. HT22 cells pre-loaded with 200 μM melatonin prior to serum deprivation did not exhibit VDAC activities. In the same manner, the addition of 4 mM ATP blocked the activation of VDAC channels [834]. The fact that both ATP and melatonin rescue neuronal cytotoxicity from VDAC-associated mitochondrial dysfunction may offer an explanation as to why p53 is found to be elevated in AD patients [728], and why tau increases wild-type p53 expression through the modulation of MDM2 [788,789,835], the E3 ubiquitin ligase which is also used by melatonin to activate p53 [836].
p53 is a transcription factor [519] that responds to a diverse range of stress signals [837] where it may promote survival and growth through the regulation of metabolic pathways [745], controlling protein synthesis and mRNA translation [838], and mediating energy metabolism under physiological and pathological conditions [839]. Mutant p53 has been reported to increase aerobic glycolysis and suppress mitochondrial OXPHOS, driving the “Warburg Effect” [840]. However, wild-type (WT) p53 has been reported to inhibit glycolysis and promote mitochondrial OXPHOS via the mediation of microRNA-34a and the IKK-NF-kappaB pathway [841,842,843]. WT p53 can regulate pyruvate metabolism in a manner that favors the conversion of pyruvate into acetyl-CoA, which then enters the TCA cycle that fuels ATP production in OXPHOS [844]. In irradiated mice, activation of wild-type p53 decreased PDK2 mRNA concentration in the colon and spleen, and increased the active, unphosphorylated form of PDC; by contrast, irradiated p53-null mice did not exhibit any decrease in PDK2 mRNA [844]. Active, unphosphorylated PDC converts pyruvate, NAD+, CoA into acetyl-coA, NADH and CO2, supporting the TCA cycle in OXPHOS to generate higher levels of ATP [824,825]. AD patients and transgenic AD mice show decreased PDC expression [829,830]; therefore, the regulation of PDK2/PDC by p53 may play an integral role in neuroprotection. Melatonin has been studied extensively for its ability to activate p53 [845,846,847] through phosphorylation [836,848,849,850,851,852], which is an ATP-dependent post-translational modification [365].
Breast cancer (MCF-7) and human colorectal carcinoma cells (HCT116) treated with 1 μM melatonin exhibited p53 activation and accumulation which inhibited proliferation and protected against DNA damage through the ATP-dependent phosphorylation of p53 at serine 15 (Ser15) [848]. Phosphorylation of p53 at Ser15 suppresses the inhibitive effect of MDM2 on p53 [853] and is also required for the maintenance of p53 physiological functions [854]. MDM2 is an E3 ubiquitin ligase that both inhibits the p53 transcription of target genes and acts as a molecular scaffold to promote p53 ubiquitination and the proteasome-dependent degradation of p53 [855]. Thus, MDM2 is often seen to be overexpressed in human tumors retaining wild-type p53 [856]. MCF-7 cells treated for 3 h with only 1 nM melatonin showed a dramatic overall cellular decrease in MDM2 content compared to control values [850]. The mechanisms involved that were observed [850] included the inhibition of Akt-PI3K-dependent MDM2 phosphorylation [851,857] together with the increase in p300 [858] via Sirt1 suppression [859]. In addition, a twofold increase in the concentration of ribosomal protein (RP) L11 was observed [850]. Aside from L11 [860,861], other RPs including S7 [862], L23 [863,864] and L5 [861,865] have also been reported to inhibit MDM2-mediated ubiquitination by binding to MDM2 to promote the activation and stabilization of p53 [866]. Intriguingly, the inhibition of ubiquitin was reported to cause a corresponding increase or decrease in SUMOylated proteins, with the implication that when the UPS cannot efficiently degrade targeted substrates, the proteins may be SUMO-modified and accumulate in MLOs [867]. Early studies have indicated the existence of an intricate interplay between SUMO and ubiquitin in response to genotoxic stress and DNA damage [868,869,870,871].
As part of the complex PTM/UPS modification system, SUMO modification, similarly to ubiquitination, is an ATP-dependent enzymatic cascade involving activating, conjugating, and ligating E1, E2, and E3 enzymes, respectively [872,873]. Small ubiquitin-like modifiers (SUMO) recognize and conjugate many protein substrates that may also be targeted by ubiquitin [874,875,876], but often with different effects [877]. The SUMOylation of proteins can alter interaction properties that may change subcellular localization, function and stability [878,879]. SUMOylation mediates the intranuclear and nucleo-cytoplasmic translocation of proteins regulating circadian rhythm [880], neuronal and synaptic functions [881,882,883], apoptosis [884], and protein degradation [875,885]. Unlike ubiquitin, SUMO-binding proteins involve covalent [886] as well as non-covalent [887] interactions that are believed to exert great influence over nuclear processes such as transcription, replication, and the maintenance of genomic integrity [888]. Embryos of mice bred without the SUMO-conjugating enzyme E2 did not survive beyond the early postimplantation stage [889]. The interplay between ubiquitin and SUMO in the nucleolar compartment may be driven by LLPS [890,891], because the inhibition of ubiquitination leads to an accumulation of SUMOylated proteins that condense into MLOs known as promyelocytic leukemia proteins (PMLs) in nucleoli [867,892].
Nucleoli PMLs are phase-separated quality control MLOs that compartmentalize misfolded proteins for clearance [893]. In mammalian cells, defective ribosomal products [894] may misfold as a result of DNA mutations [895] and damage to mRNA responsible for transcription and/or translation during protein synthesis [896,897,898,899]. The defective clearance of misfolded proteins often aggregates into protein structures in either an amyloid or amorphous state. Amyloid aggregates are insoluble, structured, higher-order assemblies [900,901,902], whereas amorphous aggregates are disordered and may contain soluble proteins [903]. Many neurodegenerative diseases, including Alzheimer’s, Parkinson’s, and Huntington’s, are associated with amyloid aggregates [904]. Failure of SUMOylation may result in the ineffective clearance of defective proteins that affect neurodegenerative disorders [905,906]. It is believed that most familial PD is caused by mutations in parkin, a ubiquitin E3 ligase that regulates the turnover of RanBP2, the SUMO E3 ligase, by catalyzing its ubiquitination to promote proteasome degradation and clearance [907].
In the cytoplasm, exposure to heat [908,909], oxidative stress [910], and osmotic stress [819,911] can cause the misfolding of proteins often associated with neurodegenerative disorders. Cells respond to various stress factors by forming cytoplasmic stress granules which are dynamic MLOs that can conserve energy and limit protein synthesis by transiently sequestering ribonucleoproteins (RNPs) such as non-translating mRNAs and RNA-binding proteins to downregulate bulk translation. Upon the removal of stress conditions, these dynamic SG MLOs in the cytoplasm are disassembled, releasing stored RNPs to reassume protein synthesis [541,542,912,913]. SG components include RBPs such as TDP-43, FUS, tau, and p53; therefore, mutations and aberrant SG dynamics may significantly contribute to neurodegenerative disorders [540,837,914]. Both ubiquitination and SUMOylation have been reported to regulate SG dynamics, where the ubiquitination–protease system [915] and SUMO-primed ubiquitination facilitate the timely resolution and disassembly of SG upon stress release, preventing aberrant SGs that may result in disease-linked pathological aggregates [915,916]. Consequently, failure to SUMOylate eIF4A2 (or DDX2B), a DEAD-box RNA helicase that acts as a scaffolding protein, impairs stress granule formation [917]. Melatonin has been reported to induce and enhance SUMOylation for the effective degradation of Aβ in AD mice models [918].
Frontal cortex tissues of double-transgenic APP/PS1 AD mice that were given daily intraperitoneal injections of melatonin at pharmacological concentration of ~10 mg/kg (0.3 mL, 10 µg/µL) for 3 weeks exhibited a significant degradation of Aβ as a result of the SUMOylation of the amyloid precursor protein (APP) intracellular domain (AICD) at lysine 43 by the SUMO E3 ligase protein inhibitor of activated STAT1 (PIAS1) [918]. AICD SUMOylation not only enhanced the clearance of Aβ and amyloid plaque in vivo [918], but the covalent SUMO-modification of amyloid precursor protein (APP) at lysines 587 and 595 by SUMO E2 ligase has also been observed to reduce Aβ aggregates in vitro [919]. Compared to wild-type AICD, SUMOylated AICD was actually more effective in the reduction in Aβ levels and the suppression of amyloid plaque accumulation [918]. APP/PS1 double-transgenic AD mice treated with melatonin exhibited an enhanced expression of AICD accompanied by marked improvements in both spatial learning and memory deficits, possibly due to the induction of AICD SUMOylation by melatonin [918].
Stress granules are formed in response to external stress factors; therefore, hypoxia, heat, oxidative, osmotic, and genotoxic stress can also significantly increase SUMO conjugate levels as a protective response [920]. Under severe oxygen and glucose deprivation, overexpression of SUMO-1 or SUMO-2 in human neuroblastoma SHSY5Y cells increased survival and ischemic tolerance [921]. SUMO conjugation may be correlated to intracellular ROS levels in a dose-dependent manner. In HeLa cells, high levels of H2O2 increased SUMO conjugation, but exposure to low levels of H2O2 (1 mM) induced a severe, rapid deSUMOylation within 5 min, resulting in the disappearance of SUMO conjugates including transcription factors [922]. Even though SUMOylation may exert neuroprotective functions [923], a dysregulated SUMO system can also negatively impact Aβ and tau aggregates in AD [924] due to the fact that SUMOylation not only controls protein–protein interactions [886] but also regulates the transcriptional control of RNA through various post-transcriptional modifications [925].
5.5. Post-Transcriptional Modifications of RNA by m6A Regulate Phase-Separated MLOs
Ribonucleic acid (RNA) is a single-stranded molecule with alternating ribose and phosphate groups attached to adenine, uracil, cytosine or guanine bases. The evolution of RNA is believed to precede that of DNA; nonetheless, the origin of the “RNA World” has not been resolved to date [926,927,928]. Perhaps due to its earlier evolution, RNA controls gene regulation at multiple levels [929,930,931]. Gene expression is essentially the transfer of genetic information from deoxyribonucleic acid (DNA) to proteins by RNA using both coding messenger RNA [932,933] and non-coding RNA [934,935,936,937]. Abnormal gene transcription may alter gene expression which often results in neurodegenerative diseases. During healthy aging, changes in the expression of key switch genes in the brain may cause neurodegenerative disorders [938]. Post-transcriptional RNA modifications are believed to have important roles in gene expression and regulation [939,940].
Phase-separated MLOs are enriched in RNA and RNA-binding proteins with IDRs [527,630,941]. RNA can be considered as an architectural element that not only seeds the nucleation of condensates but affects the size and composition of condensate phases [23]. Both the transcriptional regulation and post-transcriptional regulation of genes are now believed to be directly associated with phase separation [942]. Activation domains of transcription factors undergo phase separation to facilitate gene activation [109]. Henninger and colleagues (2021) revealed that at gene transcription sites, optimal condensate formation and transcription are co-dependent, where low levels of RNA enhanced condensate formation, supporting transcription; however, high levels of RNA dissolved condensates, terminating transcription. Control of condensate formation and dissolution during transcription processes are dependent upon fluctuations in RNA abundance that alter the electrostatic charge balance in condensates that contain transcription factors [525].
Transcription factors (TFs) can undergo LLPS to form dynamic regions that compartmentalize and concentrate other TFs, enriching transcription-related proteins to activate the transcription of target genes [527]. RNA properties such as composition, length, structure, modification, and expression level can modulate the size, shape, viscosity, liquidity, surface tension, and composition of these condensates [529,943,944]. Experimental studies have showed that longer, more structured RNA prevents the aggregation of the p53 DNA-binding core domain (p53C) in vitro [567]; therefore, it has been proposed that the larger surface area and charge of structured RNAs could potentially act as globular nanoparticles that induce changes in bound proteins to initiate fibrillation [945] or suppress aggregation [946].
Aberrant RNA–RNA interactions leading to the sequestration and/or dysregulation of RNA-binding proteins in MLOs may be one of the major driving forces behind neurodegenerative diseases [11,542,947,948,949]. Aberrant LLPS as a result of deficient RNA-binding in TDP-43 can form pathogenic, insoluble aggregates that are excluded from physiological SGs. On the other hand, with RNA-binding, TDP-43 phase-separated into dynamic inclusions that were recruited into RNA-rich, fluid compartments within SGs [28]. The formation of SGs in response to various stress conditions, including oxidative stress, involves the sequestration of translationally stalled mRNA and RNA-binding proteins to conserve energy and downregulate bulk translation [541,542,912,913].
The mechanism of selection for mRNA inclusion in SGs is determined by mRNA modification mediated by a prevalent methylation at position 6 of adenosine (m6A) in the 5′ UTRs of mRNA [950]. m6A mRNA modification is dynamic, reversible, and has been observed to be oxidative-stress-dependent. Stress-induced methylation is recognized by the m6A cytoplasmic “reader” protein, YTH domain family 3 (YTHDF3) [951], which then relocates the selected mRNA transcripts into SGs [950]. The ability of m6A to affect heterogeneous RNA and protein contents of SGs resulting from stress-specific differentiation in composition, dynamics of assembly and disassembly may ultimately determine the viability or pathology of cells in neurodegenerative diseases [540].
RNA Regulation by N6-Methyladenosine (m6A) in Neurodegenerative Disorders
Modification of eukaryotic messenger RNAs (mRNAs) occurs mostly via N6-methyladenosine (m6A), which involves the transfer of a methyl group to the sixth position of the purine ring in RNA adenosine [952]. m6A is installed by m6A methyltransferases and removed by m6A demethylases. RNA splicing, transcription, stability, and metabolism are all regulated by RNA m6A modifications [953,954,955,956]. m6A mediates structural switches that affect RNA stability and activity, regulating the access of RNA-binding proteins to their RNA binding motifs [957]. Among hundreds of types of RNA modifications identified [958], m6A is possibly the most prevalent internal, dynamic, reversible chemical modification identified to date, and plays critical roles in the growth, differentiation, and metabolism of cells [952,959]. An evolutionarily conserved RNA modification, m6A RNA methylation is involved in most aspects of RNA processing that may affect the regulation of cellular processes [960] such as immune modulation [961,962,963], fat metabolism [964], circadian rhythm [965], fertility [966,967,968,969], and brain plasticity and development [970].
The m6A RNA modification of eukaryotic RNAs is dynamic and reversible, where the methylation of mRNAs, tRNAs, rRNAs, and long non-coding RNAs by “writers” (RNA methyltransferases) such as METTL3 [971] is removed by “erasers” (RNA demethylases) such as FTO and ALKBH5 [972,973], and recognized by “readers” (m6A-binding proteins) such as YTH domain proteins [974,975]. Dysregulations of these m6A “writers”, “readers”, and “erasers” are increasingly associated with degenerative and metabolic diseases. Fat mass and obesity-associated (FTO) protein, the m6A “eraser” associated with human obesity and energy homeostasis [976,977,978,979], was found to be upregulated in breast cancer [980], hepatocellular carcinoma [981], melanoma [982], and acute myeloid leukemia (AML) [983]; however, the downregulation of FTO in vivo and in vitro enhanced invasion and metastasis in epithelial cancers [984]. ALKBH5, another m6A “eraser”, was found to be overexpressed in the tumorigenesis of glioblastoma stem-like cells [985]. The METTL3 m6A “writer” was also identified as a critical regulator of a chromatin-based pathway that maintained cells in a leukemic state, where the inhibition of METTL3 removed the myeloid differentiation block in human and mouse AML cells [986]. Depletion of YTHDF1, the m6A “reader”, was able to enhance antitumor immune responses in the dendritic cells of tumor-bearing mice [987]. The dysregulation of m6A is increasingly associated with tumorigenesis [955,959,988,989] and neurodegenerative disorders [990,991,992,993].
m6A methylation may be highest in the brain, regulating embryonic stem cell differentiation and brain development [992,994,995,996,997,998,999]; however, dysregulated m6A methylation potentially drives neurodevelopmental disorders [993]. Investigations employing high-throughput sequencing comparing m6A RNA methylation in the brains of double-transgenic APP/PS1 with those of control mice revealed statistically significant elevations of m6A methyltransferase METTL3 and downregulations of m6A demethylase FTO in the cortex and hippocampus of AD mice [991]. Post-mortem human AD brain samples showed distinct aberrant expression of m6A methyltransferases where METTL3 and the RNA-binding motif protein 15B (RBM15B) were downregulated and upregulated in the hippocampus, respectively. METTL3 was observed to be accumulated in the insoluble fractions of tau proteins, possibly implying an epitranscriptomic mechanism in altered gene expression in neurodegenerative disorders [990]. RNA epitranscriptomics regulation [1000] may provide additional speed and specificity [1001] to facilitate the transcriptional regulation of gene expression by epigenetic mechanisms [1002].
Dysregulation of m6A modifiers can lead to changes in the regulation of gene expression, affecting cancer [1003,1004], neurodegenerative diseases [990,991,1005], aortic dissection [1006], blood pressure regulation [1007], and cardiac function [1008]. More than 50% of all human cancers have been associated with missense [758] and/or synonymous mutations of the p53 gene [759,760,761]. An analysis of datasets from the Cancer Genome Atlas Research Network (TCGA) acute myeloid leukemia (AML) study revealed that mutations and/or copy number variations in genes that write, read, or erase m6A methylations, such as METTL3, METTL14, YTHDF1, YTHDF2, FTO, and ALKBH5, are significantly correlated with p53 mutations in AML patients [1009]. Most (93.6%) AML patients with mutated p53 have ≥1 genetic alteration(s) of these m6A regulatory genes. In addition, their overall and event-free survival is worse than patients without m6A genetic alterations [1009]. The loss of the m6A methyltransferase METTL3 in hepatocellular carcinoma cells (HepG2) caused alterations in gene expression and alternative splicing in more than 20 genes, including MDM2, MDM4, and p21, involved in the signaling of p53 [1010]. R273H is a hot-spot missense mutation in the p53 gene [1011,1012] which can promote cellular malignancy [1013], migration and metastasis [1014]. m6A methylation by METTL3 at the point-mutated codon 273 (G > A) of p53 pre-mRNA promoted a preferential pre-mRNA splicing that produced p53 R273H mutant genes that were resistant to multiple anticancer drugs in colon cancer cells [1015]. However, silencing METTL3 expression or inhibiting RNA methylation substantially increased the level of phosphorylated p53 protein (Ser15), allowing cells with heterozygous R273H mutations to respond normally to anticancer drugs [1015].
Aberrant RNA–RNA interactions leading to the sequestration and/or dysregulation of RNA-binding proteins in MLOs may be one of the major driving forces behind neurodegenerative diseases [11,542,947,948,949]. Section 5.5 discussed the formation of SGs in response to various stress conditions involving the sequestration of translationally stalled mRNA and RNA-binding proteins [541,542,912,913], where the mechanism of selection for mRNA inclusion in SGs is determined by oxidative stress-dependent m6A mRNA modifications by “reader” YTHDF3 [950,951]. The formation of MLOs such as SGs and P-bodies [63] enriched in translationally stalled mRNAs is dependent upon m6A-binding protein YTHDF. Depletion of YTHDF1/3 in human bone osteosarcoma epithelial cells (U-2 OS) inhibited SG formation and the recruitment of mRNAs into SGs [1016]. YTH proteins themselves undergo LLPS, and must bind to m6A-RNA before they can be complexed into stress granules, implying that polymethylated m6A-RNA may act as a scaffold for YTH proteins, causing them to undergo LLPS through interactions within their own low-complexity domains [1017,1018]. Therefore, m6A can be regarded as a beacon that attracts YTH proteins into stress granules [1019]. PTMs such as ubiquitination and SUMOylation have been reported to regulate SG dynamics, where the ubiquitination–protease system [915] and SUMO-primed ubiquitination facilitates the timely resolution and disassembly of SG upon stress release [915,916]. Melatonin has been reported to enhance AICD SUMOylation in APP/PS1 AD mice, improving spatial learning and memory deficits; therefore, melatonin may regulate biomolecular condensates via RNA and RNA m6A modifications.
5.6. Potential Regulation of RNA and RNA m6A Modifications by Melatonin
Even though AICD SUMOylation has been shown to exert beneficial effects in transgenic AD mice models, the study of SUMOylation in neurodegenerative disorders and other diseases has led to controversial and often contradictory observations, because pathways can undergo SUMOylation at different sites, yielding conflicting consequences. For example, the SUMOylation of many important proteins in AD, including APP and tau, have been associated with the pathogenesis of AD [1020,1021] and PD [1022]. On the other hand, SUMOylated misfolded proteins are targeted for ubiquitination by ubiquitin ligase RNF4, then subsequently degraded by UPS [1023]. In vitro experiments have reported that the overexpression of SUMO-1 and SUMO E2 enzyme ubc9 decreased Aβ aggregates [919], and only 10% SUMOylated α-synuclein was enough to prevent aggregation [1024]. Interestingly, fibroblasts exposed to staurosporine-induced oxidative stress exhibited reduced apoptosis as a result of α-synuclein aggregates promoted by SUMOylation [1025]. SUMOylation is essentially a stress-responsive PTM which is rapidly increased upon cellular stress to reprogram cells [1026,1027,1028] and mitochondria [1029] for survival. SUMO is also known for its inhibition of transcription factors [1030]. Upon stimulation by oxidative stress, transcription factor E2F1 was efficiently SUMOylated to initiate cell cycle arrest to increase survival [1031]. Therefore, the association of SUMO with proteins implicated in neurodegenerative disorders which are also transcription factors such as SOD1 [1032], p53 [519], tau [520], TDP-43 [521], and FUS [523] would not be unexpected, although the occasional negative outcomes may require further elucidation [1033,1034,1035,1036,1037,1038]. It is therefore not surprising to find that the SUMOylation of m6A “writers” and “readers” is also associated with the progression of cancer.
The SUMOylation of METTL3 was found to promote tumor growth and colony formation in human non-small cell lung carcinoma (NSCLC) cells (H1299) [1039], where the SUMO1 modification of METTL3 at lysine residues K177, K211, K212, and K215 dramatically repressed methylation that decreased mRNA m6A levels in vitro and in vivo—a process that can be reduced by deSUMOylation enzyme sentrin/SUMO-specific protease 1 (SENP1) [1039,1040]. In a study of liver cancer, the SUMO1 modification of METTL3 promoted tumor progression with high metastatic potential [1041]. However, in lung cancer, the SUMOylation of m6A “reader” YTHDF2 by SUMO1 at lysine residue K571 in vitro and in vivo increased the binding affinity of YTHDF2 to m6A-modified mRNAs, altering gene expression profiles, resulting in the increased proliferation, migration, colony formation and tumor growth of lung cancer H1299 cells [1042].
The YTHDF2 m6A “reader” targets and destabilizes m6A-modified mRNAs, facilitating the localization and degradation of m6A mRNA in MLOs such as P-bodies [63,953]. Ultimately, the amount of RNA released into cytoplasm could be the factor that determines the assembly and disassembly of MLOs, where a low level of negatively charged RNA could interact with positively charged proteins to promote phase separation and the formation of condensates, whereas high levels have the opposite effect in repelling proteins with a positive charge to dissolve condensates [525]. The promotion of an mRNA nuclear export is controlled by m5C, a ubiquitous post-translational RNA modification found in mRNAs [1043]. YTHDF2 has been observed to bind directly to m5C in RNA, significantly regulating 208 out of 1350 identified m5C sites that may affect pre-rRNA processing through the modification of m5C levels in rRNA [1044]. More importantly, melatonin has also been found to modulate YTHDF2 as well as METTL3.
Stimulation of oncogene Ras led to the suppression of YTHDF2 that stabilized the transcription of MAP2K4 and MAP4K4, upregulating the senescence-associated secretory phenotype (SASP) in human ovarian surface epithelial cells (HOSEpiC). Treating HOSEpiC cells with 1 μM of melatonin enhanced the expression of YTHDF2, reversed telomere shortening, and blocked Ras-induced growth arrest [1045]. The activation of cytoplasmic YTH domain “readers” [951] has been inversely correlated with oxidative stress. Upon the induction of oxidative stress, YTHDF1 increases localization to SGs to lower the activation energy barrier and reduce the critical size for SG condensate formation [1016]. Substituting 1 μM melatonin with 10 mM N-acetyl-l-cysteine (NAC), an antioxidant, also augments YTHDF2 expression in oxidative-stress-induced senescent cells; therefore, it is believed that oxidative pathways may negatively regulate YTHDF2 expression [1045]. On the other hand, the mechanism(s) involved in the modulation of METTL3 by melatonin may not be as straightforward.
Adult male C57BL/6J mice pretreated with melatonin intraperitoneal injections (25 mg/kg b.w./day × 14 days) exhibited attenuated cell viability loss, ROS generation, mitochondrial dynamics imbalance, and mitophagy in spermatogonial stem cells (SSCs) induced by daily intraperitoneal injections with chromium (VI) (16.2 mg/kg b.w./day × 14 days), an environmental toxin and carcinogen that can cause male infertility by damaging SSCs [1046,1047,1048]. In vitro mouse SSCs/progenitor cells treated with 10 μM chromium (VI) exhibited decreased METTL3 mRNA levels, but cells pretreated with 50 μM melatonin were able to attenuate the downregulation of METTL3 [1046]. An interesting observation was the significant elevation of METTL3 to levels above controls in the melatonin-only samples, whereas YTHDF2 levels were significantly elevated above the control samples in the melatonin + chromium (VI) cells after 4 h, which again supports the theory that the expression of YTHDF2 may be correlated with stress levels [1016], and can be increased by the presence of melatonin, and perhaps other antioxidants [1045].
On the other hand, melatonin was found to decrease METTL3 expression and modification in another report. m6A regulates the pluripotency of embryonic stem cells (ESCs) [1049]. Treatment with 10 μM melatonin maintained the stemness features of ESCs for more than 90 days (45 passages) via the marked suppression of global m6A modification and significant reduction in m6A “writer” METTL3 [1050]. Melatonin treatment decreased m6A mRNA methylation and altered the subcellular location of METTL3, preventing m6A-dependent mRNA decay to stabilize key pluripotency factors Nanog, Sox2, Klf4, and c-Myc [1050], known to be destabilized by m6A methylation [1051]. It has been proposed that melatonin could decrease METTL3, increasing ESC pluripotency via the MT1-JAK2/STAT3-Zfp217 signal axis. Zinc finger protein 217 (ZFP217) has been reported to activate pluripotency genes and sequester METTL3 [1052]. Using doxycycline to induce an 85% knockdown of ZFP217 in ESCs treated with melatonin, or the depletion of melatonin receptor 1 (MT1), failed to produce similar effects of m6A modification compared to wild-type ESCs treated with melatonin [1050]. However, if knocking down ZFP217 (reduction in ATP by 25% in prostate cancer cells [1053]) and/or using doxycycline (~80% reduction in ATP in hypoxic stem-like prostate cancer cells [1054]) lowered ATP production in ESCs used in the experiment [1050], then it is possible that even in the presence of melatonin, the lack of ATP led to the failure of DDX3, an ATP-dependent helicase that regulates m6A mRNA methylation.
m6A mRNA methylation can be oxidatively reversed or “erased” by m6A demethylases such as FTO [976,1055] and ALKBH5 [973,1056]. Just as the suppression of METTL3 enhances ESC pluripotency [1050], the deficiency of “erasers” such as ALKBH5 is associated with testicular dysfunction, resulting in compromised spermatogenesis [1056]. In addition, the aberrant overexpression of ALKBH5 in AML enhances the self-renewal of leukemia stem/initiating cells, often resulting in poor prognosis in AML patients [1057]. In fact, the demethylation of mRNAs by ALKBH5 in stem cells is mediated by DEAD-Box Helicase 3 (DDX3 or DDX3X), an ATP-dependent RNA helicase. DDX3 was found to modulate the demethylation of mRNAs via interactions between the DDX3 ATP domain and the DSBH domain of ALKBH5 [1058]. DDX3 is expressed in adult germ cells, whereas the expression of DDX3 in embryonic stem cells is the highest during early development [1059]. DDX3 was found to be overexpressed in undifferentiated pluripotent stem cells, compared to differentiated cells, and the abrogation of DDX3 expression in multiple stem cells resulted in reduced proliferation but increased differentiation, while at the same time, lowered potency to induce teratoma formation [1059].
NLRP3 inflammasome, a widely documented target of melatonin associated with pathological protein aggregates in neurodegenerative disorders [311,312,313,314], is a stress-induced supramolecular complex formed by phase separation [269,270,271] (Section 3.6). DDX3 is the determining factor that could favor the transition of NLRP3 into pro-death, stable, prionoid-like complexes containing self-oligomerizing specks that cannot be easily disassembled once they are formed [304,305] over the formation of reversible, pro-survival stress granules [304,310] (Figure 2). Melatonin has been widely reported to inhibit NLRP3 inflammasome inactivation; therefore, the connection between melatonin, DDX3, and other ATP-dependent RNA helicases may simply originate from the two most basic but quintessential elements that have been shaping and defining MLOs since the very beginning of life—ATP and RNA.
5.7. The Ancient Relationships between Melatonin, ATP, RNA, and Membraneless Organelles
When life originated, LLPS driven by multivalent macromolecular interactions might have been the organizing principle behind the subcellular compartmentalization of MLOS in eukaryotes and prokaryotes [2,82,277,428]. The assembly and disassembly of dynamic, transient MLOs containing RNAs, nucleic acids, and proteins [1] is tightly correlated with ATP. DEAD-box (DDX) proteins are RNA-binding ATPases that couple cycles of ATP binding and hydrolysis to changes in affinity for single-stranded RNA [1060,1061], where ATP-bound DDXs exhibit a tight affinity for RNA [1062]. DDX is involved in all aspects of RNA metabolism, from translation initiation, pre-mRNA splicing, mRNA export and decay, and ribosome biogenesis [1063]. DDX can promote RNA–protein complex remodeling, RNA duplex unwinding, and duplex annealing [1061,1063] (Figure 1).
Adenosine triphosphate (ATP) is one of the four nucleotide monomers used during RNA synthesis [1064]. RNA has been demonstrated to bind to ATP with high affinity and specificity [1065]. The tight relationship between ATP and RNA may date as far back as the “RNA world”, when ATP existed as an important cofactor of a metabolic system composed of nucleic acid enzymes prior to the evolution of ribosomal protein synthesis [1066,1067]. The addition of an unstable, third phosphate onto adenosine diphosphate (ADP) produces ATP. The transfer of the third phosphate released during hydrolysis drives energetically unfavorable but essential metabolic reactions in living organisms [1067,1068]. When RNA substrates are engaged during RNA rearrangement and unwinding processes, DEAD-box RNA helicases can display different open or closed conformations when bound to ADP or ATP, respectively [1069,1070,1071]. DDXs have also been reported to form stable, persistent complexes with RNA during RNA clamping [1072].
Cells rely upon RNA to regulate condensates because RNA molecules contain powerful electrostatic forces due to the high negative charge densities buried in their phosphate backbones [530,531,532]. Therefore, a low level of RNA with negative charge could interact with positively charged proteins to promote phase separation and the formation of transcriptional condensates, whereas high levels of negatively charged RNA could repel proteins with positive charges to dissolve condensates [525]. In the regulation of MLO assembly and disassembly dynamics, DDXs such as DDX3, DDX4, and DDX6 may function as molecular switches that direct mRNA into RNA granules such as P-bodies and stress granules for transient storage or decay, as well as the timely, necessary resolution and disassembly of these granules [49,1073,1074,1075,1076,1077]. It is important to note that the export of nuclear mRNA into cytoplasm is regulated by DDX19, an ATP-dependent RNA helicase with many important functions [1078].
Since its discovery in Saccharomyces cerevisiae in 1999, DX19 (human)/Dbp5 (yeast) [1079] has been associated with important functions involving mRNA export and remodeling [1062,1079,1080,1081], mRNA expression [1082], and translation [1076], as well as DNA transcription and metabolism [1083,1084]. One of the most important functions of DDX19 in the context of MLO dynamics is the export of nuclear mRNA via nuclear pore complexes (NPCs). NPCs are huge, highly conserved, macromolecular structures comprising ~1000 protein subunits (nucleoporins) that perforate the nuclear envelope, fusing inner and outer nuclear membranes to create pores as well as a passive diffusion barrier of disordered proteins [1085]. NPCs not only mediate mRNA export into the cytosol and bidirectional protein transport, but they may also be transcription regulators which are spatial organizers of the genome due to their ability to interact with chromosomal loci to promote transcriptional activation, repression, and poising [1086].
It has been proposed that the ATP-dependent catalytic cycle of DDX19 involves the cycling between open and closed conformations to bind RNA for export into cytoplasm [1085]. Even though mutant Dbp5/DDX19 which could not bind RNA are unable to export mRNA in both yeast and human cells [1080], ATP binding and hydrolysis are also necessary for Dbp5/DDX19 to engage nuclear pore complexes for the optimal transport of mRNA into cytoplasm [1085]. DDXs have been shown to regulate the formation of phase-separated condensates such as stress granules and P-bodies in vivo and in vitro [69]; therefore, the overexpression of DDX19 may actually prevent the formation of SGs, as reported by an experimental study showing that the overexpression of DDX eIF4A [1087] together with ATP prevented drug-induced RNA condensate formation in vitro [1088]. The nuclear export of mRNA by DDX19 is reliant upon functional NPCs; therefore, the relationship between RNA and lipid domains in nuclear envelopes presents a deeper perspective into the role of melatonin in MLO dynamics.
NPCs can be visualized as thousands of toroid-shaped “ultradonut”-like pores with extremely high curvatures generated by nanoscale buckling instabilities triggered by membrane stresses during nuclei growth [1089]. These “ultradonuts” fuse the outer (ONM) and inner (INM) nuclear envelope (NE) membranes, which are lipid bilayers [1090,1091]. The NE ONM faces the cytoplasm and is a continuation of the ER [1092,1093]. It has been proposed that the ER is the source of the membrane for NE assembly [1094]. The fact that ER membranes are enriched with membrane-associated mRNAs and RNAs [71,72,73] may explain why MLOs such as P-bodies are formed at close proximity to ER membranes [70], because the assembly of MLOs such as P-bodies are dependent upon mRNAs and RNAs [67]. The composition of lipids in the NE is dominated by phosphatidylcholine with extremely high levels of negatively charged lipids and cholesterol, and reconstituted nuclear membrane vesicles have been seen to be more ordered than classical POPC membranes [1095]. Compared to classical plasma membranes, human nuclear envelopes are at least two orders of magnitude more elastic, with exceptionally high fluidity to stabilize large, dynamic, deep-penetrating invaginations that deform the membranes. The functions of these invaginations are as-yet unclear, although appear to be involved in calcium signaling and gene expression [1095]. Morphological changes to NEs due to the dysregulation of membrane lipid composition may lead to pathological outcomes [1095,1096].
As early as 1979, the regulation of nuclear RNA release was found to be directly correlated with nuclear membrane fluidity where a reduction in membrane fluidity caused a linear decrease in RNA release [1097]. It has been proposed that NPC biogenesis may be dependent upon the fluidity of NE membranes [1098]. Cells of Saccharomyces cerevisiae with defects in regulating membrane fluidity assembled NPCs that were defective, whereas the restoration of membrane fluidity via the addition of membrane-fluidizing agents attenuated defects in NPC biogenesis and normalized mRNA export [1099]. The peroxidation of lipids in NE [1100,1101] may reduce membrane fluidity. Lipid peroxidation can alter molecular structures, creating amphiphilic subpopulations and leading to significant changes in the phase behavior of lipid membranes that can affect the integrity and fluidity of membranes [214,318,343,344,353,354,355]. The preferential location of melatonin in bilayer lipid headgroups enables dynamic interactions that reduce bilayer thickness and increase bilayer fluidity [338,341,356]. The presence of both hydrophilic and lipophilic moieties in melatonin also facilitates the scavenging of both aqueous and lipophilic free radicals [411], especially •OH [448] and •OOH, the two most prevalent ROS responsible for the chain oxidation of unsaturated phospholipids [465,466] such as phosphatidylcholine, the dominant lipid in NE [1095] (Figure 1).
Membranes of NE must be tightly curved to support NPCs [1102]. Lipid components of the nuclear pore membrane may promote membrane curvature, maintaining a convex (positive) curvature along the surface of the membrane connecting the outer and inner membranes, and a concave (negative) curvature in the central plane of the pore membrane [1103,1104]. Despite the fact that many NPC proteins have been proposed to induce and/or stabilize membrane curvature by amphipathic helix insertion into the lipid bilayer [1105,1106], key questions on how NPCs promote membrane curvature remain unresolved [1107]. It is possible that nuclear lipid domains play an important role in the generation and stabilization of membrane curvature and fluidity in NE, because membranes themselves can affect local protein concentrations [360] where high curvature lipids that form rafts may attract specific proteins that can further enhance membrane curvature [361,362,363,364]. Adsorption of proteins onto membranes can modulate composition of the lipid bilayers because lipids may potentially flow to accommodate changes in membrane curvature during protein adsorption. These changes result in alterations to membrane tension that reflect the residual local tension that adjusts the difference between the actual mean curvature and the imposed spontaneous curvature [1108].
During protein membrane adsorption, the complex interactions between lateral membrane organization and proteins often enhance the propensity of membrane lipids to form domains or to phase-separate [1109]. These domains may, in turn, act as anchors for the adsorbed proteins [116]. The formation of nuclear lipid microdomains is especially relevant because NPCs are believed to be transcription regulators [1086]. An in vivo experiment using Sprague Dawley female rats discovered the existence of nuclear lipid raft microdomains that acted as platforms for transcription processes during RNA synthesis. Compared to sham-operated animals, lipid microdomains isolated from nuclei exhibited a lipid composition that was associated with DNA replication and transcription during cellular proliferation in liver regeneration, and these nuclear raft domains were especially enriched in labeled uridine when there was increased RNA synthesis [1110]. RNA and phospholipids may have a long-standing relationship; the two molecules have been shown to form heteromeric weak bonds that could regulate membrane permeability [1111,1112]. Human tRNASec was demonstrated to show increased binding affinity for lipid rafts [1113], and free RNA 10 molecules would preferentially associate with Lo lipid raft domains at 18 °C with ~80% binding, whereas increasing the temperature to 23 °C lowered the binding affinity to ~58% due to a corresponding increase in the non-raft Ld phase that discouraged binding [1114]. Cells may use melatonin to control temperature fluctuations that could affect RNA binding affinities. Melatonin stabilized lipid Lo–Ld phase separation over a range of temperatures (tested up to 45 °C), preserving nanoscopic lipid domain structure and composition, possibly by reducing membrane line tension [350]. Lipid peroxides often induced nanometer-scale rafts to grow to micron sizes, accompanied by increased line tension in the order of several piconewtons [206,218,296]. As a potent antioxidant, melatonin may also be used by organisms to preserve membrane tension and fluidity, and stabilize Lo-phase lipid rafts in cells and nuclei (Figure 1).
The relationship between melatonin and RNA is likely an ancient one that might date as far back as ~4 billion years ago, possibly after the height of the “RNA world” [1115,1116,1117], when a proposed gene duplication event at ~3.5 Ga involving CP43 and CP47, enzymes unique to photosystem II (PSII), marked the beginning of water oxidation [431]. Regulation of the synthesis and degradation of the evolutionarily conserved PSII D1 reaction center is mediated by post-translational RNA modulations [1118,1119,1120] and the presence of ATP [1121] in a light-dependent manner, where synthesis and/or degradation is induced by light but ceased in the dark. Unlike animals [1122], melatonin in plants is increased by the presence of light [1123,1124], and treatment with melatonin enhanced the synthesis of PSII D1 reaction centers in tomato seedlings under salt stress [1125]. Cyanobacteria, the only known prokaryote capable of water oxidation [431] which also produces melatonin [421,422], has recently been shown to exhibit circadian rhythm in the formation and dissolution of MLOs that remained soluble during daylight, but became reversible, insoluble condensates at night in an ATP-dependent manner [432]; therefore, it is not unreasonable to hypothesize that the relationship between melatonin, MLOs, ATP, and RNA was already in existence at ~3.5 Ga. The presence of melatonin in primitive unicellular organisms including Rhodospirillum rubrum and cyanobacteria, precursors to mitochondria and chloroplasts, respectively [415,423,424,425], may have conferred protection against endogenous and exogenous oxidative stress that could readily damage macromolecules and disrupt ATP production at membrane lipid domains [421,426,427]. This unique feature implies that melatonin may have an intrinsic modulatory effect over phase separation, not only in early but present-day organisms (Figure 1).
6. Conclusions
The physiological and pathological functions of biomolecular condensates in neurodegenerative disorders are shaped by powerful, complex, interdependent relationships between membraneless organelles, membranes/lipid rafts, ATP, RNA, and most of all, stress and its timely resolution. Melatonin’s intimate association with each of these decisive influencers may position the potent, ancient antioxidant as an important mediator of the phase separation of condensates in health and disease via principal ATP-dependent mechanisms including post-translational modifications and RNA m6A modifications (Figure 1). This novel theoretical review is presented with the intention to spur further research interest and exploration in the full, multi-faceted potential of melatonin in the regulation of biomolecular condensates that could provide solutions and answers to existing and future challenges and questions in this exciting and promising field of study.
Author Contributions
D.L.: Conceptualization and manuscript preparation. R.J.R.: Review and final version editing. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Acknowledgments
Special thanks to Allan Lenon Cura for the preparation and design of the graphic illustrations, and Elizabeth Martorana for proofreading the initial draft.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
| 3-OHM | 3-hydroxymelatonin |
| Aβ | β-amyloid peptide |
| AD | Alzheimer’s disease |
| ADP | adenosine diphosphate |
| AICD | amyloid precursor protein intracellular domain |
| ALS | amyotrophic lateral sclerosis |
| ANT | adenine nucleotide translocator |
| APP | amyloid precursor protein |
| ASC | apoptosis-associated speck-like protein containing a C-terminal caspase recruitment domain |
| ATP | adenosine triphosphate |
| CL | cardiolipin |
| CYB5R3 | NADH-cytochrome b5 reductase 3 |
| Cyt | c cytochrome c |
| DDX3(X) | DEAD-box RNA helicase |
| DNA | deoxyribonucleic acid |
| eIF2a | eukaryotic translation initiation factor 2 alpha |
| ER | endoplasmic reticulum |
| FTO | frontotemporal dementia |
| FUS | fused in sarcoma |
| H+ | proton |
| H2O2 | hydrogen peroxide |
| IDP | intrinsically disordered protein |
| IDR | intrinsically disordered region |
| IMM | inner mitochondrial membrane |
| Lo | liquid-ordered |
| Lc | circular liquid-condensed |
| Ld | liquid-disordered |
| LLPS | liquid–liquid phase separation |
| m6A | N6-methyladenosine |
| mM | millimolar |
| μM | micromolar |
| MDM2 | mouse double minute 2 homolog |
| MLO | membraneless organelle |
| MAM | mitochondria-associated membrane |
| MOM | mitochondrial outer membrane |
| mPTP | mitochondrial permeability transition pore |
| mRNA | messenger RNA |
| MT | microtubule |
| NE | nuclear envelope |
| NFT | neurofibrillary tangles |
| NLRP3 | NLR pyrin domain containing 3 (inflammasome) |
| nM | nanomolar |
| NPC | nuclear pore complex |
| O2•− | superoxide radical |
| •OH | hydroxyl radical |
| •OOH | hydroperoxyl radical |
| OXPHOS | oxidative phosphorylation |
| PD | Parkinson’s disorder |
| PDC | pyruvate dehydrogenase complex |
| PDK | pyruvate dehydrogenase kinase |
| Pi | inorganic phosphate |
| PLD | prion-like domain |
| PML | promyelocytic leukemia proteins |
| PTM | post-translational modification |
| RNA | ribonucleic acid |
| RBP | RNA-binding protein |
| RNP | ribonucleoprotein |
| ROS | reactive oxygen species |
| RP | ribosomal protein |
| SG | stress granule |
| SUMO | small ubiquitin-like modifier |
| TCA | tricarboxylic acid (cycle) |
| TDP-43 | TAR DNA-binding protein 43 |
| Ub | ubiquitin |
| UCP1 | uncoupling protein 1 |
| UPS | ubiquitin-protease system |
| VDAC | voltage-dependent anion channel |
| ZFP217 | zinc finger protein 217 |
References
- Feng, Z.; Chen, X.; Wu, X.; Zhang, M. Formation of Biological Condensates via Phase Separation: Characteristics, Analytical Methods, and Physiological Implications. J. Biol. Chem. 2019, 294, 14823–14835. [Google Scholar] [CrossRef]
- Oparin, A.I.; Synge, A. The Origin of Life on the Earth/Translated from the Russian by Ann Synge; Elsevier Science Ltd.: Amsterdam, The Netherlands, 1957. [Google Scholar] [CrossRef]
- Riback, J.A.; Katanski, C.D.; Kear-Scott, J.L.; Pilipenko, E.V.; Rojek, A.E.; Sosnick, T.R.; Drummond, D.A. Stress-Triggered Phase Separation is an Adaptive, Evolutionarily Tuned Response. Cell 2017, 168, 1028–1040.e19. [Google Scholar] [CrossRef] [PubMed]
- Li, P.; Banjade, S.; Cheng, H.-C.; Kim, S.; Chen, B.; Guo, L.; Llaguno, M.; Hollingsworth, J.V.; King, D.S.; Banani, S.F.; et al. Phase Transitions in the Assembly of Multivalent Signalling Proteins. Nature 2012, 483, 336–340. [Google Scholar] [CrossRef]
- Su, X.; Ditlev, J.A.; Hui, E.; Xing, W.; Banjade, S.; Okrut, J.; King, D.S.; Taunton, J.; Rosen, M.K.; Vale, R.D. Phase Separation of Signaling Molecules Promotes T Cell Receptor Signal Transduction. Science 2016, 352, 595–599. [Google Scholar] [CrossRef]
- Laflamme, G.; Mekhail, K. Biomolecular Condensates as Arbiters of Biochemical Reactions inside the Nucleus. Commun. Biol. 2020, 3, 773. [Google Scholar] [CrossRef] [PubMed]
- Ditlev, J.A.; Case, L.B.; Rosen, M.K. Who’s In and Who’s Out-Compositional Control of Biomolecular Condensates. J. Mol. Biol. 2018, 430, 4666–4684. [Google Scholar] [CrossRef] [PubMed]
- Shin, Y.; Brangwynne, C.P. Liquid Phase Condensation in Cell Physiology and Disease. Science 2017, 357, eaaf4382. [Google Scholar] [CrossRef] [PubMed]
- Alberti, S.; Dormann, D. Liquid-Liquid Phase Separation in Disease. Annu. Rev. Genet. 2019, 53, 171–194. [Google Scholar] [CrossRef]
- Boija, A.; Klein, I.A.; Young, R.A. Biomolecular Condensates and Cancer. Cancer Cell 2021, 39, 174–192. [Google Scholar] [CrossRef]
- Zbinden, A.; Pérez-Berlanga, M.; De Rossi, P.; Polymenidou, M. Phase Separation and Neurodegenerative Diseases: A Disturbance in the Force. Dev. Cell 2020, 55, 45–68. [Google Scholar] [CrossRef]
- Taniue, K.; Akimitsu, N. Aberrant Phase Separation and Cancer. FEBS J. 2021. [Google Scholar] [CrossRef]
- Hyman, A.A.; Weber, C.A.; Jülicher, F. Liquid-Liquid Phase Separation in Biology. Annu. Rev. Cell Dev. Biol. 2014, 30, 39–58. [Google Scholar] [CrossRef]
- Ahlers, J.; Adams, E.M.; Bader, V.; Pezzotti, S.; Winklhofer, K.F.; Tatzelt, J.; Havenith, M. The Key Role of Solvent in Condensation: Mapping Water in Liquid-Liquid Phase-Separated FUS. Biophys. J. 2021, 120, 1266–1275. [Google Scholar] [CrossRef] [PubMed]
- Lodish, H.; Berk, A.; Lawrence Zipursky, S.; Matsudaira, P.; Baltimore, D.; Darnell, J. Biochemical Energetics; W. H. Freeman: New York, NY, USA, 2000. [Google Scholar]
- Manchester, K.L. Free Energy ATP Hydrolysis and Phosphorylation Potential. Biochem. Educ. 1980, 8, 70–72. [Google Scholar] [CrossRef]
- Peth, A.; Uchiki, T.; Goldberg, A.L. ATP-Dependent Steps in the Binding of Ubiquitin Conjugates to the 26S Proteasome That Commit to Degradation. Mol. Cell 2010, 40, 671–681. [Google Scholar] [CrossRef]
- Callis, J. The Ubiquitination Machinery of the Ubiquitin System. Arab. Book 2014, 12, e0174. [Google Scholar] [CrossRef]
- Zhao, X. SUMO-Mediated Regulation of Nuclear Functions and Signaling Processes. Mol. Cell 2018, 71, 409–418. [Google Scholar] [CrossRef] [PubMed]
- Van Damme, E.; Laukens, K.; Dang, T.H.; Van Ostade, X. A Manually Curated Network of the PML Nuclear Body Interactome Reveals an Important Role for PML-NBs in SUMOylation Dynamics. Int. J. Biol. Sci. 2010, 6, 51–67. [Google Scholar] [CrossRef] [PubMed]
- Hardenberg, M.; Horvath, A.; Ambrus, V.; Fuxreiter, M.; Vendruscolo, M. Widespread Occurrence of the Droplet State of Proteins in the Human Proteome. Proc. Natl. Acad. Sci. USA 2020, 117, 33254–33262. [Google Scholar] [CrossRef]
- Hondele, M.; Heinrich, S.; De Los Rios, P.; Weis, K. Membraneless Organelles: Phasing out of Equilibrium. Emerg. Top Life Sci. 2020, 4, 331–342. [Google Scholar] [CrossRef]
- Garcia-Jove Navarro, M.; Kashida, S.; Chouaib, R.; Souquere, S.; Pierron, G.; Weil, D.; Gueroui, Z. RNA Is a Critical Element for the Sizing and the Composition of Phase-Separated RNA-Protein Condensates. Nat. Commun. 2019, 10, 3230. [Google Scholar] [CrossRef]
- Elbaum-Garfinkle, S.; Kim, Y.; Szczepaniak, K.; Chen, C.C.-H.; Eckmann, C.R.; Myong, S.; Brangwynne, C.P. The Disordered P Granule Protein LAF-1 Drives Phase Separation into Droplets with Tunable Viscosity and Dynamics. Proc. Natl. Acad. Sci. USA 2015, 112, 7189–7194. [Google Scholar] [CrossRef]
- Lunde, B.M.; Moore, C.; Varani, G. RNA-Binding Proteins: Modular Design for Efficient Function. Nat. Rev. Mol. Cell Biol. 2007, 8, 479–490. [Google Scholar] [CrossRef]
- Patel, A.; Lee, H.O.; Jawerth, L.; Maharana, S.; Jahnel, M.; Hein, M.Y.; Stoynov, S.; Mahamid, J.; Saha, S.; Franzmann, T.M.; et al. A Liquid-to-Solid Phase Transition of the ALS Protein FUS Accelerated by Disease Mutation. Cell 2015, 162, 1066–1077. [Google Scholar] [CrossRef]
- Niaki, A.G.; Sarkar, J.; Cai, X.; Rhine, K.; Vidaurre, V.; Guy, B.; Hurst, M.; Lee, J.C.; Koh, H.R.; Guo, L.; et al. Loss of Dynamic RNA Interaction and Aberrant Phase Separation Induced by Two Distinct Types of ALS/FTD-Linked FUS Mutations. Mol. Cell 2020, 77, 82–94.e4. [Google Scholar] [CrossRef] [PubMed]
- Mann, J.R.; Gleixner, A.M.; Mauna, J.C.; Gomes, E.; DeChellis-Marks, M.R.; Needham, P.G.; Copley, K.E.; Hurtle, B.; Portz, B.; Pyles, N.J.; et al. RNA Binding Antagonizes Neurotoxic Phase Transitions of TDP-43. Neuron 2019, 102, 321–338.e8. [Google Scholar] [CrossRef] [PubMed]
- Wegmann, S.; Eftekharzadeh, B.; Tepper, K.; Zoltowska, K.M.; Bennett, R.E.; Dujardin, S.; Laskowski, P.R.; MacKenzie, D.; Kamath, T.; Commins, C.; et al. Tau Protein Liquid-Liquid Phase Separation Can Initiate Tau Aggregation. EMBO J. 2018, 37, e98049. [Google Scholar] [CrossRef]
- Patel, A.; Malinovska, L.; Saha, S.; Wang, J.; Alberti, S.; Krishnan, Y.; Hyman, A.A. ATP as a Biological Hydrotrope. Science 2017, 356, 753–756. [Google Scholar] [CrossRef]
- Hatzopoulos, M.H.; Eastoe, J.; Dowding, P.J.; Rogers, S.E.; Heenan, R.; Dyer, R. Are Hydrotropes Distinct from Surfactants? Langmuir 2011, 27, 12346–12353. [Google Scholar] [CrossRef] [PubMed]
- Jain, S.; Wheeler, J.R.; Walters, R.W.; Agrawal, A.; Barsic, A.; Parker, R. ATPase-Modulated Stress Granules Contain a Diverse Proteome and Substructure. Cell 2016, 164, 487–498. [Google Scholar] [CrossRef] [PubMed]
- Brangwynne, C.P.; Mitchison, T.J.; Hyman, A.A. Active Liquid-like Behavior of Nucleoli Determines Their Size and Shape in Xenopus Laevis Oocytes. Proc. Natl. Acad. Sci. USA 2011, 108, 4334–4339. [Google Scholar] [CrossRef]
- Pal, S.; Paul, S. ATP Controls the Aggregation of Aβ16-22 Peptides. J. Phys. Chem. B 2020, 124, 210–223. [Google Scholar] [CrossRef]
- Zhang, C.; Rissman, R.A.; Feng, J. Characterization of ATP Alternations in an Alzheimer’s Disease Transgenic Mouse Model. J. Alzheimers. Dis. 2015, 44, 375–378. [Google Scholar] [CrossRef]
- Salis, A.; Ninham, B.W. Models and Mechanisms of Hofmeister Effects in Electrolyte Solutions, and Colloid and Protein Systems Revisited. Chem. Soc. Rev. 2014, 43, 7358–7377. [Google Scholar] [CrossRef] [PubMed]
- Mandl, I.; Grauer, A.; Neuberg, C. Solubilization of Insoluble Matter in Nature; I. The Part Played by Salts of Adenosinetriphosphate. Biochim. Biophys. Acta 1952, 8, 654–663. [Google Scholar] [CrossRef]
- Mehringer, J.; Do, T.-M.; Touraud, D.; Hohenschutz, M.; Khoshsima, A.; Horinek, D.; Kunz, W. Hofmeister versus Neuberg: Is ATP Really a Biological Hydrotrope? Cell Rep. Phys. Science 2021, 2, 100343. [Google Scholar] [CrossRef]
- Schwenke, W.D.; Soboll, S.; Seitz, H.J.; Sies, H. Mitochondrial and Cytosolic ATP/ADP Ratios in Rat Liver in Vivo. Biochem. J 1981, 200, 405–408. [Google Scholar] [CrossRef] [PubMed]
- Imamura, H.; Nhat, K.P.H.; Togawa, H.; Saito, K.; Iino, R.; Kato-Yamada, Y.; Nagai, T.; Noji, H. Visualization of ATP Levels inside Single Living Cells with Fluorescence Resonance Energy Transfer-Based Genetically Encoded Indicators. Proc. Natl. Acad. Sci. USA 2009, 106, 15651–15656. [Google Scholar] [CrossRef]
- Fang, D.; Maldonado, E.N. VDAC Regulation: A Mitochondrial Target to Stop Cell Proliferation. Adv. Cancer Res. 2018, 138, 41–69. [Google Scholar] [CrossRef] [PubMed]
- Ruprecht, J.J.; King, M.S.; Zögg, T.; Aleksandrova, A.A.; Pardon, E.; Crichton, P.G.; Steyaert, J.; Kunji, E.R.S. The Molecular Mechanism of Transport by the Mitochondrial ADP/ATP Carrier. Cell 2019, 176, 435–447.e15. [Google Scholar] [CrossRef]
- Liu, Y.; Chen, X.J. Adenine Nucleotide Translocase, Mitochondrial Stress, and Degenerative Cell Death. Oxid. Med. Cell. Longev. 2013, 2013, 146860. [Google Scholar] [CrossRef] [PubMed]
- Depaoli, M.R.; Karsten, F.; Madreiter-Sokolowski, C.T.; Klec, C.; Gottschalk, B.; Bischof, H.; Eroglu, E.; Waldeck-Weiermair, M.; Simmen, T.; Graier, W.F.; et al. Real-Time Imaging of Mitochondrial ATP Dynamics Reveals the Metabolic Setting of Single Cells. Cell Rep. 2018, 25, 501–512.e3. [Google Scholar] [CrossRef] [PubMed]
- Song, J. Adenosine Triphosphate Energy-Independently Controls Protein Homeostasis with Unique Structure and Diverse Mechanisms. Protein Sci. 2021, 30, 1277–1293. [Google Scholar] [CrossRef] [PubMed]
- Takaine, M.; Imamura, H.; Yoshida, S. High and Stable ATP Levels Prevent Aberrant Intracellular Protein Aggregation. bioRxiv 2021, 2021, 801738. [Google Scholar] [CrossRef]
- Sama, R.R.K.; Ward, C.L.; Kaushansky, L.J.; Lemay, N.; Ishigaki, S.; Urano, F.; Bosco, D.A. FUS/TLS Assembles into Stress Granules and Is a Prosurvival Factor during Hyperosmolar Stress. J. Cell. Physiol. 2013, 228, 2222–2231. [Google Scholar] [CrossRef]
- Mahboubi, H.; Stochaj, U. Cytoplasmic Stress Granules: Dynamic Modulators of Cell Signaling and Disease. Biochim. Biophys. Acta Mol. Basis Dis. 2017, 1863, 884–895. [Google Scholar] [CrossRef]
- Hilliker, A. Analysis of RNA Helicases in P-Bodies and Stress Granules. Methods Enzymol. 2012, 511, 323–346. [Google Scholar] [CrossRef]
- Sathyanarayanan, U.; Musa, M.; Bou Dib, P.; Raimundo, N.; Milosevic, I.; Krisko, A. ATP Hydrolysis by Yeast Hsp104 Determines Protein Aggregate Dissolution and Size in Vivo. Nat. Commun. 2020, 11, 5226. [Google Scholar] [CrossRef]
- Kang, J.; Lim, L.; Song, J. ATP Enhances at Low Concentrations but Dissolves at High Concentrations Liquid-Liquid Phase Separation (LLPS) of ALS/FTD-Causing FUS. Biochem. Biophys. Res. Commun. 2018, 504, 545–551. [Google Scholar] [CrossRef]
- Kang, J.; Lim, L.; Song, J. ATP Binds and Inhibits the Neurodegeneration-Associated Fibrillization of the FUS RRM Domain. Commun. Biol. 2019, 2, 223. [Google Scholar] [CrossRef]
- Dang, M.; Lim, L.; Kang, J.; Song, J. ATP Biphasically Modulates LLPS of TDP-43 PLD by Specifically Binding Arginine Residues. Commun. Biol. 2021, 4, 714. [Google Scholar] [CrossRef]
- Heo, C.E.; Han, J.Y.; Lim, S.; Lee, J.; Im, D.; Lee, M.J.; Kim, Y.K.; Kim, H.I. ATP Kinetically Modulates Pathogenic Tau Fibrillations. ACS Chem. Neurosci. 2020, 11, 3144–3152. [Google Scholar] [CrossRef]
- Farid, M.; Corbo, C.P.; Alonso, A.D.C. Tau Binds ATP and Induces Its Aggregation. Microsc. Res. Tech. 2014, 77, 133–137. [Google Scholar] [CrossRef]
- Newby, G.A.; Lindquist, S. Blessings in Disguise: Biological Benefits of Prion-like Mechanisms. Trends Cell Biol. 2013, 23, 251–259. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; McGinnis, J.P.; Si, K. Translational Control by Prion-like Proteins. Trends Cell Biol. 2018, 28, 494–505. [Google Scholar] [CrossRef]
- Schuster, B.S.; Dignon, G.L.; Tang, W.S.; Kelley, F.M.; Ranganath, A.K.; Jahnke, C.N.; Simpkins, A.G.; Regy, R.M.; Hammer, D.A.; Good, M.C.; et al. Identifying Sequence Perturbations to an Intrinsically Disordered Protein That Determine Its Phase-Separation Behavior. Proc. Natl. Acad. Sci. USA 2020, 117, 11421–11431. [Google Scholar] [CrossRef] [PubMed]
- Harmon, T.S.; Holehouse, A.S.; Rosen, M.K.; Pappu, R.V. Intrinsically Disordered Linkers Determine the Interplay between Phase Separation and Gelation in Multivalent Proteins. Elife 2017, 6, e30294. [Google Scholar] [CrossRef] [PubMed]
- Owen, I.; Shewmaker, F. The Role of Post-Translational Modifications in the Phase Transitions of Intrinsically Disordered Proteins. Int. J. Mol. Sci. 2019, 20, 5501. [Google Scholar] [CrossRef]
- Van der Lee, R.; Buljan, M.; Lang, B.; Weatheritt, R.J.; Daughdrill, G.W.; Dunker, A.K.; Fuxreiter, M.; Gough, J.; Gsponer, J.; Jones, D.T.; et al. Classification of Intrinsically Disordered Regions and Proteins. Chem. Rev. 2014, 114, 6589–6631. [Google Scholar] [CrossRef]
- Küffner, A.M.; Linsenmeier, M.; Grigolato, F.; Prodan, M.; Zuccarini, R.; Capasso Palmiero, U.; Faltova, L.; Arosio, P. Sequestration within Biomolecular Condensates Inhibits Aβ-42 Amyloid Formation. Chem. Sci. 2021, 12, 4373–4382. [Google Scholar] [CrossRef]
- Luo, Y.; Na, Z.; Slavoff, S.A. P-Bodies: Composition, Properties, and Functions. Biochemistry 2018, 57, 2424–2431. [Google Scholar] [CrossRef] [PubMed]
- Stoecklin, G.; Kedersha, N. Relationship of GW/P-Bodies with Stress Granules. Adv. Exp. Med. Biol. 2013, 768, 197–211. [Google Scholar] [CrossRef] [PubMed]
- Kedersha, N.; Stoecklin, G.; Ayodele, M.; Yacono, P.; Lykke-Andersen, J.; Fritzler, M.J.; Scheuner, D.; Kaufman, R.J.; Golan, D.E.; Anderson, P. Stress Granules and Processing Bodies Are Dynamically Linked Sites of mRNP Remodeling. J. Cell Biol. 2005, 169, 871–884. [Google Scholar] [CrossRef]
- Nostramo, R.; Xing, S.; Zhang, B.; Herman, P.K. Insights into the Role of P-Bodies and Stress Granules in Protein Quality Control. Genetics 2019, 213, 251–265. [Google Scholar] [CrossRef] [PubMed]
- Teixeira, D.; Sheth, U.; Valencia-Sanchez, M.A.; Brengues, M.; Parker, R. Processing Bodies Require RNA for Assembly and Contain Nontranslating mRNAs. RNA 2005, 11, 371–382. [Google Scholar] [CrossRef]
- Loll-Krippleber, R.; Brown, G.W. P-Body Proteins Regulate Transcriptional Rewiring to Promote DNA Replication Stress Resistance. Nat. Commun. 2017, 8, 558. [Google Scholar] [CrossRef] [PubMed]
- Mugler, C.F.; Hondele, M.; Heinrich, S.; Sachdev, R.; Vallotton, P.; Koek, A.Y.; Chan, L.Y.; Weis, K. ATPase Activity of the DEAD-Box Protein Dhh1 Controls Processing Body Formation. Elife 2016, 5, e18746. [Google Scholar] [CrossRef]
- Wang, C.; Schmich, F.; Srivatsa, S.; Weidner, J.; Beerenwinkel, N.; Spang, A. Context-Dependent Deposition and Regulation of mRNAs in P-Bodies. Elife 2018, 7, e29815. [Google Scholar] [CrossRef]
- Hermesh, O.; Jansen, R.-P. Take the (RN)A-Train: Localization of mRNA to the Endoplasmic Reticulum. Biochim. Biophys. Acta 2013, 1833, 2519–2525. [Google Scholar] [CrossRef] [PubMed]
- Cui, X.A.; Palazzo, A.F. Localization of mRNAs to the Endoplasmic Reticulum. Wiley Interdiscip. Rev. RNA 2014, 5, 481–492. [Google Scholar] [CrossRef]
- Reid, D.W.; Nicchitta, C.V. Primary Role for Endoplasmic Reticulum-Bound Ribosomes in Cellular Translation Identified by Ribosome Profiling. J. Biol. Chem. 2012, 287, 5518–5527. [Google Scholar] [CrossRef]
- Majewski, J.; Jones, E.M.; Vander Zanden, C.M.; Biernat, J.; Mandelkow, E.; Chi, E.Y. Lipid Membrane Templated Misfolding and Self-Assembly of Intrinsically Disordered Tau Protein. Sci. Rep. 2020, 10, 13324. [Google Scholar] [CrossRef] [PubMed]
- Zhao, H.; Tuominen, E.K.J.; Kinnunen, P.K.J. Formation of Amyloid Fibers Triggered by Phosphatidylserine-Containing Membranes. Biochemistry 2004, 43, 10302–10307. [Google Scholar] [CrossRef]
- Goñi, F.; Martá-Ariza, M.; Herline, K.; Peyser, D.; Boutajangout, A.; Mehta, P.; Drummond, E.; Prelli, F.; Wisniewski, T. Anti-β-Sheet Conformation Monoclonal Antibody Reduces Tau and Aβ Oligomer Pathology in an Alzheimer’s Disease Model. Alzheimers. Res. Ther. 2018, 10, 10. [Google Scholar] [CrossRef] [PubMed]
- Dregni, A.J.; Mandala, V.S.; Wu, H.; Elkins, M.R.; Wang, H.K.; Hung, I.; DeGrado, W.F.; Hong, M. In Vitro 0N4R Tau Fibrils Contain a Monomorphic β-Sheet Core Enclosed by Dynamically Heterogeneous Fuzzy Coat Segments. Proc. Natl. Acad. Sci. USA 2019, 116, 16357–16366. [Google Scholar] [CrossRef] [PubMed]
- Koppers, M.; Özkan, N.; Farías, G.G. Complex Interactions between Membrane-Bound Organelles, Biomolecular Condensates and the Cytoskeleton. Front. Cell Dev. Biol. 2020, 8, 618733. [Google Scholar] [CrossRef] [PubMed]
- Snead, W.T.; Gladfelter, A.S. The Control Centers of Biomolecular Phase Separation: How Membrane Surfaces, PTMs, and Active Processes Regulate Condensation. Mol. Cell 2019, 76, 295–305. [Google Scholar] [CrossRef]
- Alberts, B.; Johnson, A.; Lewis, J.; Raff, M.; Roberts, K.; Walter, P. The Compartmentalization of Cells; Garland Science: New York, NY, USA, 2002. [Google Scholar]
- Mizuuchi, R.; Ichihashi, N. Primitive Compartmentalization for the Sustainable Replication of Genetic Molecules. Life 2021, 11, 191. [Google Scholar] [CrossRef]
- Banani, S.F.; Lee, H.O.; Hyman, A.A.; Rosen, M.K. Biomolecular Condensates: Organizers of Cellular Biochemistry. Nat. Rev. Mol. Cell Biol. 2017, 18, 285–298. [Google Scholar] [CrossRef]
- Pucadyil, T.J. Chapter 2—Dynamic Remodeling of Membranes Catalyzed by Dynamin. In Current Topics in Membranes; Chernomordik, L.V., Kozlov, M.M., Eds.; Academic Press: Cambridge, MA, USA, 2011; Volume 68. [Google Scholar] [CrossRef]
- Scorrano, L.; De Matteis, M.A.; Emr, S.; Giordano, F.; Hajnóczky, G.; Kornmann, B.; Lackner, L.L.; Levine, T.P.; Pellegrini, L.; Reinisch, K.; et al. Coming Together to Define Membrane Contact Sites. Nat. Commun. 2019, 10, 1287. [Google Scholar] [CrossRef]
- Sallese, M.; Pulvirenti, T.; Luini, A. The Physiology of Membrane Transport and Endomembrane-Based Signalling. EMBO J. 2006, 25, 2663–2673. [Google Scholar] [CrossRef]
- Jaqaman, K.; Ditlev, J.A. Biomolecular Condensates in Membrane Receptor Signaling. Curr. Opin. Cell Biol. 2021, 69, 48–54. [Google Scholar] [CrossRef]
- Case, L.B.; Zhang, X.; Ditlev, J.A.; Rosen, M.K. Stoichiometry Controls Activity of Phase-Separated Clusters of Actin Signaling Proteins. Science 2019, 363, 1093–1097. [Google Scholar] [CrossRef] [PubMed]
- Huang, W.Y.C.; Alvarez, S.; Kondo, Y.; Lee, Y.K.; Chung, J.K.; Lam, H.Y.M.; Biswas, K.H.; Kuriyan, J.; Groves, J.T. A Molecular Assembly Phase Transition and Kinetic Proofreading Modulate Ras Activation by SOS. Science 2019, 363, 1098–1103. [Google Scholar] [CrossRef] [PubMed]
- Bharadwaj, P.; Solomon, T.; Malajczuk, C.J.; Mancera, R.L.; Howard, M.; Arrigan, D.W.M.; Newsholme, P.; Martins, R.N. Role of the Cell Membrane Interface in Modulating Production and Uptake of Alzheimer’s Beta Amyloid Protein. Biochim. Biophys. Acta Biomembr. 2018, 1860, 1639–1651. [Google Scholar] [CrossRef]
- Ehehalt, R.; Keller, P.; Haass, C.; Thiele, C.; Simons, K. Amyloidogenic Processing of the Alzheimer Beta-Amyloid Precursor Protein Depends on Lipid Rafts. J. Cell Biol. 2003, 160, 113–123. [Google Scholar] [CrossRef]
- Kojro, E.; Gimpl, G.; Lammich, S.; Marz, W.; Fahrenholz, F. Low Cholesterol Stimulates the Nonamyloidogenic Pathway by Its Effect on the Alpha -Secretase ADAM 10. Proc. Natl. Acad. Sci. USA 2001, 98, 5815–5820. [Google Scholar] [CrossRef]
- Simons, K.; Ikonen, E. Functional Rafts in Cell Membranes. Nature 1997, 387, 569–572. [Google Scholar] [CrossRef] [PubMed]
- Simons, K.; Toomre, D. Lipid Rafts and Signal Transduction. Nat. Rev. Mol. Cell Biol. 2000, 1, 31–39. [Google Scholar] [CrossRef] [PubMed]
- Bagnat, M.; Keränen, S.; Shevchenko, A.; Shevchenko, A.; Simons, K. Lipid Rafts Function in Biosynthetic Delivery of Proteins to the Cell Surface in Yeast. Proc. Natl. Acad. Sci. USA 2000, 97, 3254–3259. [Google Scholar] [CrossRef]
- Ikonen, E. Roles of Lipid Rafts in Membrane Transport. Curr. Opin. Cell Biol. 2001, 13, 470–477. [Google Scholar] [CrossRef]
- Michel, V.; Bakovic, M. Lipid Rafts in Health and Disease. Biol. Cell 2007, 99, 129–140. [Google Scholar] [CrossRef] [PubMed]
- Schengrund, C.-L. Lipid Rafts: Keys to Neurodegeneration. Brain Res. Bull. 2010, 82, 7–17. [Google Scholar] [CrossRef] [PubMed]
- Maguy, A.; Hebert, T.E.; Nattel, S. Involvement of Lipid Rafts and Caveolae in Cardiac Ion Channel Function. Cardiovasc. Res. 2006, 69, 798–807. [Google Scholar] [CrossRef]
- Vey, M.; Pilkuhn, S.; Wille, H.; Nixon, R.; DeArmond, S.J.; Smart, E.J.; Anderson, R.G.; Taraboulos, A.; Prusiner, S.B. Subcellular Colocalization of the Cellular and Scrapie Prion Proteins in Caveolae-like Membranous Domains. Proc. Natl. Acad. Sci. USA 1996, 93, 14945–14949. [Google Scholar] [CrossRef]
- Taylor, D.R.; Hooper, N.M. The Prion Protein and Lipid Rafts. Mol. Membr. Biol. 2006, 23, 89–99. [Google Scholar] [CrossRef] [PubMed]
- Jury, E.C.; Kabouridis, P.S.; Flores-Borja, F.; Mageed, R.A.; Isenberg, D.A. Altered Lipid Raft-Associated Signaling and Ganglioside Expression in T Lymphocytes from Patients with Systemic Lupus Erythematosus. J. Clin. Investig. 2004, 113, 1176–1187. [Google Scholar] [CrossRef]
- Chazal, N.; Gerlier, D. Virus Entry, Assembly, Budding, and Membrane Rafts. Microbiol. Mol. Biol. Rev. 2003, 67, 226–237. [Google Scholar] [CrossRef]
- Murai, T. The Role of Lipid Rafts in Cancer Cell Adhesion and Migration. Int. J. Cell Biol. 2012, 2012, 763283. [Google Scholar] [CrossRef]
- Mollinedo, F.; Gajate, C. Lipid Rafts as Signaling Hubs in Cancer Cell Survival/death and Invasion: Implications in Tumor Progression and Therapy: Thematic Review Series: Biology of Lipid Rafts. J. Lipid Res. 2020, 61, 611–635. [Google Scholar] [CrossRef]
- Greenlee, J.D.; Subramanian, T.; Liu, K.; King, M.R. Rafting Down the Metastatic Cascade: The Role of Lipid Rafts in Cancer Metastasis, Cell Death, and Clinical Outcomes. Cancer Res. 2021, 81, 5–17. [Google Scholar] [CrossRef]
- Codini, M.; Garcia-Gil, M.; Albi, E. Cholesterol and Sphingolipid Enriched Lipid Rafts as Therapeutic Targets in Cancer. Int. J. Mol. Sci. 2021, 22, 726. [Google Scholar] [CrossRef] [PubMed]
- Wei, M.-T.; Chang, Y.-C.; Shimobayashi, S.F.; Shin, Y.; Strom, A.R.; Brangwynne, C.P. Nucleated Transcriptional Condensates Amplify Gene Expression. Nat. Cell Biol. 2020, 22, 1187–1196. [Google Scholar] [CrossRef]
- Shrinivas, K.; Sabari, B.R.; Coffey, E.L.; Klein, I.A.; Boija, A.; Zamudio, A.V.; Schuijers, J.; Hannett, N.M.; Sharp, P.A.; Young, R.A.; et al. Enhancer Features That Drive Formation of Transcriptional Condensates. Mol. Cell 2019, 75, 549–561.e7. [Google Scholar] [CrossRef] [PubMed]
- Boija, A.; Klein, I.A.; Sabari, B.R.; Dall’Agnese, A.; Coffey, E.L.; Zamudio, A.V.; Li, C.H.; Shrinivas, K.; Manteiga, J.C.; Hannett, N.M.; et al. Transcription Factors Activate Genes through the Phase-Separation Capacity of Their Activation Domains. Cell 2018, 175, 1842–1855.e16. [Google Scholar] [CrossRef] [PubMed]
- Jiang, S.; Fagman, J.B.; Chen, C.; Alberti, S.; Liu, B. Protein Phase Separation and Its Role in Tumorigenesis. Elife 2020, 9, e60264. [Google Scholar] [CrossRef]
- Vernon, R.M.; Chong, P.A.; Tsang, B.; Kim, T.H.; Bah, A.; Farber, P.; Lin, H.; Forman-Kay, J.D. Pi-Pi Contacts Are an Overlooked Protein Feature Relevant to Phase Separation. Elife 2018, 7, e31486. [Google Scholar] [CrossRef]
- Ditlev, J.A. Membrane-Associated Phase Separation: Organization and Function Emerge from a Two-Dimensional Milieu. J. Mol. Cell Biol. 2021, 13, 319–324. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Rabouille, C. Membrane-Bound Meet Membraneless in Health and Disease. Cells 2019, 8, 1000. [Google Scholar] [CrossRef]
- Plowman, S.J.; Muncke, C.; Parton, R.G.; Hancock, J.F. H-Ras, K-Ras, and Inner Plasma Membrane Raft Proteins Operate in Nanoclusters with Differential Dependence on the Actin Cytoskeleton. Proc. Natl. Acad. Sci. USA 2005, 102, 15500–15505. [Google Scholar] [CrossRef] [PubMed]
- Banjade, S.; Rosen, M.K. Phase Transitions of Multivalent Proteins Can Promote Clustering of Membrane Receptors. Elife 2014, 3, e04123. [Google Scholar] [CrossRef]
- Lee, I.-H.; Imanaka, M.Y.; Modahl, E.H.; Torres-Ocampo, A.P. Lipid Raft Phase Modulation by Membrane-Anchored Proteins with Inherent Phase Separation Properties. ACS Omega. 2019, 4, 6551–6559. [Google Scholar] [CrossRef] [PubMed]
- Chung, J.K.; Huang, W.Y.C.; Carbone, C.B.; Nocka, L.M.; Parikh, A.N.; Vale, R.D.; Groves, J.T. Coupled Membrane Lipid Miscibility and Phosphotyrosine-Driven Protein Condensation Phase Transitions. Biophys. J. 2021, 120, 1257–1265. [Google Scholar] [CrossRef] [PubMed]
- Feric, M.; Vaidya, N.; Harmon, T.S.; Mitrea, D.M.; Zhu, L.; Richardson, T.M.; Kriwacki, R.W.; Pappu, R.V.; Brangwynne, C.P. Coexisting Liquid Phases Underlie Nucleolar Subcompartments. Cell 2016, 165, 1686–1697. [Google Scholar] [CrossRef]
- Pullman, M.E.; Penefsky, H.S.; Datta, A.; Racker, E. Partial Resolution of the Enzymes Catalyzing Oxidative Phosphorylation. I. Purification and Properties of Soluble Dinitrophenol-Stimulated Adenosine Triphosphatase. J. Biol. Chem. 1960, 235, 3322–3329. [Google Scholar] [CrossRef]
- Ernster, L.; Schatz, G. Mitochondria: A Historical Review. J. Cell Biol. 1981, 91, 227s–255s. [Google Scholar] [CrossRef]
- Abrahams, J.P.; Leslie, A.G.; Lutter, R.; Walker, J.E. Structure at 2.8 A Resolution of F1-ATPase from Bovine Heart Mitochondria. Nature 1994, 370, 621–628. [Google Scholar] [CrossRef] [PubMed]
- Grüber, G.; Wieczorek, H.; Harvey, W.R.; Müller, V. Structure–function Relationships of A-, F- and V-ATPases. J. Exp. Biol. 2001, 204, 2597–2605. [Google Scholar] [CrossRef]
- Mitchell, P. Chemiosmotic Coupling in Oxidative and Photosynthetic Phosphorylation. Biol. Rev. Camb. Philos. Soc. 1966, 41, 445–502. [Google Scholar] [CrossRef]
- Boyer, P.D. The ATP Synthase--a Splendid Molecular Machine. Annu. Rev. Biochem. 1997, 66, 717–749. [Google Scholar] [CrossRef]
- Jonckheere, A.I.; Smeitink, J.A.M.; Rodenburg, R.J.T. Mitochondrial ATP Synthase: Architecture, Function and Pathology. J. Inherit. Metab. Dis. 2012, 35, 211–225. [Google Scholar] [CrossRef]
- Kühlbrandt, W. Biology, Structure and Mechanism of P-Type ATPases. Nat. Rev. Mol. Cell Biol. 2004, 5, 282–295. [Google Scholar] [CrossRef]
- Beyenbach, K.W.; Wieczorek, H. The V-Type H+ ATPase: Molecular Structure and Function, Physiological Roles and Regulation. J. Exp. Biol. 2006, 209 Pt 4, 577–589. [Google Scholar] [CrossRef]
- Gaudet, R.; Wiley, D.C. Structure of the ABC ATPase Domain of Human TAP1, the Transporter Associated with Antigen Processing. EMBO J. 2001, 20, 4964–4972. [Google Scholar] [CrossRef] [PubMed]
- Adachi, K.; Oiwa, K.; Nishizaka, T.; Furuike, S.; Noji, H.; Itoh, H.; Yoshida, M.; Kinosita Jr, K. Coupling of Rotation and Catalysis in F(1)-ATPase Revealed by Single-Molecule Imaging and Manipulation. Cell 2007, 130, 309–321. [Google Scholar] [CrossRef] [PubMed]
- Okuno, D.; Iino, R.; Noji, H. Rotation and Structure of FoF1-ATP Synthase. J. Biochem. 2011, 149, 655–664. [Google Scholar] [CrossRef]
- Cotter, K.; Stransky, L.; McGuire, C.; Forgac, M. Recent Insights into the Structure, Regulation, and Function of the V-ATPases. Trends Biochem. Sci. 2015, 40, 611–622. [Google Scholar] [CrossRef]
- Das, B.; Mondragon, M.O.; Sadeghian, M.; Hatcher, V.B.; Norin, A.J. A Novel Ligand in Lymphocyte-Mediated Cytotoxicity: Expression of the Beta Subunit of H+ Transporting ATP Synthase on the Surface of Tumor Cell Lines. J. Exp. Med. 1994, 180, 273–281. [Google Scholar] [CrossRef] [PubMed]
- Qian, Y.; Wang, X.; Li, Y.; Cao, Y.; Chen, X. Extracellular ATP a New Player in Cancer Metabolism: NSCLC Cells Internalize ATP In Vitro and In Vivo Using Multiple Endocytic Mechanisms. Mol. Cancer Res. 2016, 14, 1087–1096. [Google Scholar] [CrossRef] [PubMed]
- Moser, T.L.; Kenan, D.J.; Ashley, T.A.; Roy, J.A.; Goodman, M.D.; Misra, U.K.; Cheek, D.J.; Pizzo, S.V. Endothelial Cell Surface F1-F0 ATP Synthase Is Active in ATP Synthesis and Is Inhibited by Angiostatin. Proc. Natl. Acad. Sci. USA 2001, 98, 6656–6661. [Google Scholar] [CrossRef]
- Arakaki, N.; Nagao, T.; Niki, R.; Toyofuku, A.; Tanaka, H.; Kuramoto, Y.; Emoto, Y.; Shibata, H.; Magota, K.; Higuti, T. Possible Role of Cell Surface H+ -ATP Synthase in the Extracellular ATP Synthesis and Proliferation of Human Umbilical Vein Endothelial Cells. Mol. Cancer Res. 2003, 1, 931–939. [Google Scholar] [PubMed]
- Bae, T.-J.; Kim, M.-S.; Kim, J.-W.; Kim, B.-W.; Choo, H.-J.; Lee, J.-W.; Kim, K.-B.; Lee, C.S.; Kim, J.-H.; Chang, S.Y.; et al. Lipid Raft Proteome Reveals ATP Synthase Complex in the Cell Surface. Proteomics 2004, 4, 3536–3548. [Google Scholar] [CrossRef]
- Zhang, L.-H.; Kamanna, V.S.; Zhang, M.C.; Kashyap, M.L. Niacin Inhibits Surface Expression of ATP Synthase Beta Chain in HepG2 Cells: Implications for Raising HDL. J. Lipid Res. 2008, 49, 1195–1201. [Google Scholar] [CrossRef] [PubMed]
- Martinez, L.O.; Jacquet, S.; Esteve, J.-P.; Rolland, C.; Cabezón, E.; Champagne, E.; Pineau, T.; Georgeaud, V.; Walker, J.E.; Tercé, F.; et al. Ectopic Beta-Chain of ATP Synthase Is an Apolipoprotein A-I Receptor in Hepatic HDL Endocytosis. Nature 2003, 421, 75–79. [Google Scholar] [CrossRef] [PubMed]
- Burrell, H.E.; Wlodarski, B.; Foster, B.J.; Buckley, K.A.; Sharpe, G.R.; Quayle, J.M.; Simpson, A.W.M.; Gallagher, J.A. Human Keratinocytes Release ATP and Utilize Three Mechanisms for Nucleotide Interconversion at the Cell Surface. J. Biol. Chem. 2005, 280, 29667–29676. [Google Scholar] [CrossRef] [PubMed]
- Sergeant, N.; Wattez, A.; Galván-valencia, M.; Ghestem, A.; David, J.-P.; Lemoine, J.; Sautiére, P.-E.; Dachary, J.; Mazat, J.-P.; Michalski, J.-C.; et al. Association of ATP Synthase Alpha-Chain with Neurofibrillary Degeneration in Alzheimer’s Disease. Neuroscience 2003, 117, 293–303. [Google Scholar] [CrossRef]
- Chi, S.L.; Pizzo, S.V. Cell Surface F1Fo ATP Synthase: A New Paradigm? Ann. Med. 2006, 38, 429–438. [Google Scholar] [CrossRef]
- Abrams, A. Structure and Function of Membrane-Bound ATPase in Bacteria. In The Enzymes of Biological Membranes: Volume 3 Membrane Transport (FIRST EDITION); Martonosi, A., Ed.; Springer: Boston, MA, USA, 1976. [Google Scholar] [CrossRef]
- Guo, H.; Suzuki, T.; Rubinstein, J.L. Structure of a Bacterial ATP Synthase. Elife 2019, 8, e43128. [Google Scholar] [CrossRef]
- Krulwich, T.A.; Sachs, G.; Padan, E. Molecular Aspects of Bacterial pH Sensing and Homeostasis. Nat. Rev. Microbiol. 2011, 9, 330–343. [Google Scholar] [CrossRef]
- Xing, S.-L.; Yan, J.; Yu, Z.-H.; Zhu, C.-Q. Neuronal Cell Surface ATP Synthase Mediates Synthesis of Extracellular ATP and Regulation of Intracellular pH. Cell Biol. Int. 2011, 35, 81–86. [Google Scholar] [CrossRef]
- Murakami, T.; Shibuya, I.; Ise, T.; Chen, Z.S.; Akiyama, S.; Nakagawa, M.; Izumi, H.; Nakamura, T.; Matsuo, K.; Yamada, Y.; et al. Elevated Expression of Vacuolar Proton Pump Genes and Cellular PH in Cisplatin Resistance. Int. J. Cancer 2001, 93, 869–874. [Google Scholar] [CrossRef]
- Nott, T.J.; Petsalaki, E.; Farber, P.; Jervis, D.; Fussner, E.; Plochowietz, A.; Craggs, T.D.; Bazett-Jones, D.P.; Pawson, T.; Forman-Kay, J.D.; et al. Phase Transition of a Disordered Nuage Protein Generates Environmentally Responsive Membraneless Organelles. Mol. Cell 2015, 57, 936–947. [Google Scholar] [CrossRef] [PubMed]
- Ruff, K.M.; Roberts, S.; Chilkoti, A.; Pappu, R.V. Advances in Understanding Stimulus-Responsive Phase Behavior of Intrinsically Disordered Protein Polymers. J. Mol. Biol. 2018, 430, 4619–4635. [Google Scholar] [CrossRef]
- Alberti, S.; Gladfelter, A.; Mittag, T. Considerations and Challenges in Studying Liquid-Liquid Phase Separation and Biomolecular Condensates. Cell 2019, 176, 419–434. [Google Scholar] [CrossRef] [PubMed]
- Chidlow Jr, J.H.; Sessa, W.C. Caveolae, Caveolins, and Cavins: Complex Control of Cellular Signalling and Inflammation. Cardiovasc. Res. 2010, 86, 219–225. [Google Scholar] [CrossRef] [PubMed]
- Mangiullo, R.; Gnoni, A.; Leone, A.; Gnoni, G.V.; Papa, S.; Zanotti, F. Structural and Functional Characterization of FoF1-ATP Synthase on the Extracellular Surface of Rat Hepatocytes. BBA—Bioenerg. 2008, 1777, 1326–1335. [Google Scholar] [CrossRef]
- Kim, B.-W.; Choo, H.-J.; Lee, J.-W.; Kim, J.-H.; Ko, Y.-G. Extracellular ATP Is Generated by ATP Synthase Complex in Adipocyte Lipid Rafts. Exp. Mol. Med. 2004, 36, 476–485. [Google Scholar] [CrossRef] [PubMed]
- Brini, M.; Carafoli, E. The Plasma Membrane Ca2+ ATPase and the Plasma Membrane Sodium Calcium Exchanger Cooperate in the Regulation of Cell Calcium. Cold Spring Harb. Perspect. Biol. 2011, 3, a004168. [Google Scholar] [CrossRef] [PubMed]
- Sepúlveda, M.R.; Berrocal-Carrillo, M.; Gasset, M.; Mata, A.M. The Plasma Membrane Ca2+-ATPase Isoform 4 Is Localized in Lipid Rafts of Cerebellum Synaptic Plasma Membranes. J. Biol. Chem. 2006, 281, 447–453. [Google Scholar] [CrossRef]
- Noble, K.; Zhang, J.; Wray, S. Lipid Rafts, the Sarcoplasmic Reticulum and Uterine Calcium Signalling: An Integrated Approach. J. Physiol. 2006, 570 Pt 1, 29–35. [Google Scholar] [CrossRef]
- Nagata, J.; Guerra, M.T.; Shugrue, C.A.; Gomes, D.A.; Nagata, N.; Nathanson, M.H. Lipid Rafts Establish Calcium Waves in Hepatocytes. Gastroenterology 2007, 133, 256–267. [Google Scholar] [CrossRef]
- Krishnan, G.; Chatterjee, N. Detergent Resistant Membrane Fractions Are Involved in Calcium Signaling in Müller Glial Cells of Retina. Int. J. Biochem. Cell Biol. 2013, 45, 1758–1766. [Google Scholar] [CrossRef]
- Tsutsumi, Y.M.; Horikawa, Y.T.; Jennings, M.M.; Kidd, M.W.; Niesman, I.R.; Yokoyama, U.; Head, B.P.; Hagiwara, Y.; Ishikawa, Y.; Miyanohara, A.; et al. Cardiac-Specific Overexpression of Caveolin-3 Induces Endogenous Cardiac Protection by Mimicking Ischemic Preconditioning. Circulation 2008, 118, 1979–1988. [Google Scholar] [CrossRef]
- Shaul, P.W.; Anderson, R.G. Role of Plasmalemmal Caveolae in Signal Transduction. Am. J. Physiol. 1998, 275, L843–L851. [Google Scholar] [CrossRef]
- Parton, R.G.; del Pozo, M.A. Caveolae as Plasma Membrane Sensors, Protectors and Organizers. Nat. Rev. Mol. Cell Biol. 2013, 14, 98–112. [Google Scholar] [CrossRef] [PubMed]
- Galbiati, F.; Razani, B.; Lisanti, M.P. Emerging Themes in Lipid Rafts and Caveolae. Cell 2001, 106, 403–411. [Google Scholar] [CrossRef]
- Chen, Z.; Rand, R.P. The Influence of Cholesterol on Phospholipid Membrane Curvature and Bending Elasticity. Biophys. J. 1997, 73, 267–276. [Google Scholar] [CrossRef]
- Wang, W.; Yang, L.; Huang, H.W. Evidence of Cholesterol Accumulated in High Curvature Regions: Implication to the Curvature Elastic Energy for Lipid Mixtures. Biophys. J. 2007, 92, 2819–2830. [Google Scholar] [CrossRef] [PubMed]
- Yesylevskyy, S.O.; Rivel, T.; Ramseyer, C. The Influence of Curvature on the Properties of the Plasma Membrane. Insights from Atomistic Molecular Dynamics Simulations. Sci. Rep. 2017, 7, 16078. [Google Scholar] [CrossRef] [PubMed]
- Krishna, A.; Sengupta, D. Interplay between Membrane Curvature and Cholesterol: Role of Palmitoylated Caveolin-1. Biophys. J. 2019, 116, 69–78. [Google Scholar] [CrossRef]
- Smart, E.J.; Graf, G.A.; McNiven, M.A.; Sessa, W.C.; Engelman, J.A.; Scherer, P.E.; Okamoto, T.; Lisanti, M.P. Caveolins, Liquid-Ordered Domains, and Signal Transduction. Mol. Cell Biol. 1999, 19, 7289–7304. [Google Scholar] [CrossRef]
- Murata, M.; Peränen, J.; Schreiner, R.; Wieland, F.; Kurzchalia, T.V.; Simons, K. VIP21/caveolin Is a Cholesterol-Binding Protein. Proc. Natl. Acad. Sci. USA 1995, 92, 10339–10343. [Google Scholar] [CrossRef] [PubMed]
- Strauss, M.; Hofhaus, G.; Schröder, R.R.; Kühlbrandt, W. Dimer Ribbons of ATP Synthase Shape the Inner Mitochondrial Membrane. EMBO J. 2008, 27, 1154–1160. [Google Scholar] [CrossRef]
- Esparza-Perusquía, M.; Olvera-Sánchez, S.; Pardo, J.P.; Mendoza-Hernández, G.; Martínez, F.; Flores-Herrera, O. Structural and Kinetics Characterization of the F1F0-ATP Synthase Dimer. New Repercussion of Monomer-Monomer Contact. Biochim. Biophys. Acta Bioenerg. 2017, 1858, 975–981. [Google Scholar] [CrossRef]
- Spikes, T.E.; Montgomery, M.G.; Walker, J.E. Interface Mobility between Monomers in Dimeric Bovine ATP Synthase Participates in the Ultrastructure of Inner Mitochondrial Membranes. Proc. Natl. Acad. Sci. USA 2021, 118, e2021012118. [Google Scholar] [CrossRef] [PubMed]
- Paumard, P.; Vaillier, J.; Coulary, B.; Schaeffer, J.; Soubannier, V.; Mueller, D.M.; Brèthes, D.; di Rago, J.-P.; Velours, J. The ATP Synthase Is Involved in Generating Mitochondrial Cristae Morphology. EMBO J. 2002, 21, 221–230. [Google Scholar] [CrossRef] [PubMed]
- Davies, K.M.; Anselmi, C.; Wittig, I.; Faraldo-Gómez, J.D.; Kühlbrandt, W. Structure of the Yeast F1Fo-ATP Synthase Dimer and Its Role in Shaping the Mitochondrial Cristae. Proc. Natl. Acad. Sci. USA 2012, 109, 13602–13607. [Google Scholar] [CrossRef] [PubMed]
- Habersetzer, J.; Larrieu, I.; Priault, M.; Salin, B.; Rossignol, R.; Brèthes, D.; Paumard, P. Human F1F0 ATP Synthase, Mitochondrial Ultrastructure and OXPHOS Impairment: A (super-)complex Matter? PLoS ONE 2013, 8, e75429. [Google Scholar] [CrossRef]
- Mannella, C.A. The Relevance of Mitochondrial Membrane Topology to Mitochondrial Function. Biochim. Biophys. Acta 2006, 1762, 140–147. [Google Scholar] [CrossRef] [PubMed]
- Blum, T.B.; Hahn, A.; Meier, T.; Davies, K.M.; Kühlbrandt, W. Dimers of Mitochondrial ATP Synthase Induce Membrane Curvature and Self-Assemble into Rows. Proc. Natl. Acad. Sci. USA 2019, 116, 4250–4255. [Google Scholar] [CrossRef]
- Allen-Worthington, K.; Xie, J.; Brown, J.L.; Edmunson, A.M.; Dowling, A.; Navratil, A.M.; Scavelli, K.; Yoon, H.; Kim, D.-G.; Bynoe, M.S.; et al. The F0F1 ATP Synthase Complex Localizes to Membrane Rafts in Gonadotrope Cells. Mol. Endocrinol. 2016, 30, 996–1011. [Google Scholar] [CrossRef][Green Version]
- Kim, B.-W.; Lee, J.-W.; Choo, H.-J.; Lee, C.S.; Jung, S.-Y.; Yi, J.-S.; Ham, Y.-M.; Lee, J.-H.; Hong, J.; Kang, M.-J.; et al. Mitochondrial Oxidative Phosphorylation System Is Recruited to Detergent-Resistant Lipid Rafts during Myogenesis. Proteomics 2010, 10, 2498–2515. [Google Scholar] [CrossRef] [PubMed]
- Hayes, M.H.; Peuchen, E.H.; Dovichi, N.J.; Weeks, D.L. Dual Roles for ATP in the Regulation of Phase Separated Protein Aggregates in Xenopus Oocyte Nucleoli. Elife 2018, 7, e35224. [Google Scholar] [CrossRef] [PubMed]
- Sridharan, S.; Kurzawa, N.; Werner, T.; Günthner, I.; Helm, D.; Huber, W.; Bantscheff, M.; Savitski, M.M. Proteome-Wide Solubility and Thermal Stability Profiling Reveals Distinct Regulatory Roles for ATP. Nat. Commun. 2019, 10, 1155. [Google Scholar] [CrossRef]
- Ma, Z.; Cao, M.; Liu, Y.; He, Y.; Wang, Y.; Yang, C.; Wang, W.; Du, Y.; Zhou, M.; Gao, F. Mitochondrial F1Fo-ATP Synthase Translocates to Cell Surface in Hepatocytes and Has High Activity in Tumor-like Acidic and Hypoxic Environment. Acta Biochim. Biophys. Sin. 2010, 42, 530–537. [Google Scholar] [CrossRef]
- Villa-Pulgarín, J.A.; Gajate, C.; Botet, J.; Jimenez, A.; Justies, N.; Varela-M, R.E.; Cuesta-Marbán, Á.; Müller, I.; Modolell, M.; Revuelta, J.L.; et al. Mitochondria and Lipid Raft-Located FOF1-ATP Synthase as Major Therapeutic Targets in the Antileishmanial and Anticancer Activities of Ether Lipid Edelfosine. PLoS Negl. Trop. Dis. 2017, 11, e0005805. [Google Scholar] [CrossRef]
- Jin, S.; Zhou, F.; Katirai, F.; Li, P.-L. Lipid Raft Redox Signaling: Molecular Mechanisms in Health and Disease. Antioxid. Redox Signal. 2011, 15, 1043–1083. [Google Scholar] [CrossRef] [PubMed]
- Patel, H.H.; Insel, P.A. Lipid Rafts and Caveolae and Their Role in Compartmentation of Redox Signaling. Antioxid. Redox Signal. 2009, 11, 1357–1372. [Google Scholar] [CrossRef]
- Koneru, S.; Penumathsa, S.V.; Thirunavukkarasu, M.; Samuel, S.M.; Zhan, L.; Han, Z.; Maulik, G.; Das, D.K.; Maulik, N. Redox Regulation of Ischemic Preconditioning Is Mediated by the Differential Activation of Caveolins and Their Association with eNOS and GLUT-4. Am. J. Physiol. Heart Circ. Physiol. 2007, 292, H2060–H2072. [Google Scholar] [CrossRef]
- Kuzmin, P.I.; Akimov, S.A.; Chizmadzhev, Y.A.; Zimmerberg, J.; Cohen, F.S. Line Tension and Interaction Energies of Membrane Rafts Calculated from Lipid Splay and Tilt. Biophys. J. 2005, 88, 1120–1133. [Google Scholar] [CrossRef] [PubMed]
- Blackwell, D.J.; Zak, T.J.; Robia, S.L. Cardiac Calcium ATPase Dimerization Measured by Cross-Linking and Fluorescence Energy Transfer. Biophys. J. 2016, 111, 1192–1202. [Google Scholar] [CrossRef]
- Simons, K.; Sampaio, J.L. Membrane Organization and Lipid Rafts. Cold Spring Harb. Perspect. Biol. 2011, 3, a004697. [Google Scholar] [CrossRef] [PubMed]
- Kinnun, J.J.; Bolmatov, D.; Lavrentovich, M.O.; Katsaras, J. Lateral Heterogeneity and Domain Formation in Cellular Membranes. Chem. Phys. Lipids 2020, 232, 104976. [Google Scholar] [CrossRef] [PubMed]
- Pike, L.J. Rafts Defined: A Report on the Keystone Symposium on Lipid Rafts and Cell Function. J. Lipid Res. 2006, 47, 1597–1598. [Google Scholar] [CrossRef]
- Sezgin, E.; Levental, I.; Mayor, S.; Eggeling, C. The Mystery of Membrane Organization: Composition, Regulation and Roles of Lipid Rafts. Nat. Rev. Mol. Cell Biol. 2017, 18, 361–374. [Google Scholar] [CrossRef]
- Ouweneel, A.B.; Thomas, M.J.; Sorci-Thomas, M.G. The Ins and Outs of Lipid Rafts: Functions in Intracellular Cholesterol Homeostasis, Microparticles, and Cell Membranes: Thematic Review Series: Biology of Lipid Rafts. J. Lipid Res. 2020, 61, 676–686. [Google Scholar] [CrossRef]
- Armstrong, C.L.; Marquardt, D.; Dies, H.; Kučerka, N.; Yamani, Z.; Harroun, T.A.; Katsaras, J.; Shi, A.-C.; Rheinstädter, M.C. The Observation of Highly Ordered Domains in Membranes with Cholesterol. PLoS ONE 2013, 8, e66162. [Google Scholar] [CrossRef] [PubMed]
- Almeida, P.F.F.; Pokorny, A.; Hinderliter, A. Thermodynamics of Membrane Domains. Biochim. Biophys. Acta 2005, 1720, 1–13. [Google Scholar] [CrossRef]
- Igarashi, M.; Honda, A.; Kawasaki, A.; Nozumi, M. Neuronal Signaling Involved in Neuronal Polarization and Growth: Lipid Rafts and Phosphorylation. Front. Mol. Neurosci. 2020, 13, 150. [Google Scholar] [CrossRef] [PubMed]
- Bolmatov, D.; Soloviov, D.; Zhernenkov, M.; Zav’yalov, D.; Mamontov, E.; Suvorov, A.; Cai, Y.Q.; Katsaras, J. Molecular Picture of the Transient Nature of Lipid Rafts. Langmuir 2020, 36, 4887–4896. [Google Scholar] [CrossRef]
- Miller, Y.I.; Navia-Pelaez, J.M.; Corr, M.; Yaksh, T.L. Lipid Rafts in Glial Cells: Role in Neuroinflammation and Pain Processing: Thematic Review Series: Biology of Lipid Rafts. J. Lipid Res. 2020, 61, 655–666. [Google Scholar] [CrossRef]
- Sviridov, D.; Mukhamedova, N.; Miller, Y.I. Lipid Rafts as a Therapeutic Target: Thematic Review Series: Biology of Lipid Rafts. J. Lipid Res. 2020, 61, 687–695. [Google Scholar] [CrossRef]
- Li, Y.C.; Park, M.J.; Ye, S.-K.; Kim, C.-W.; Kim, Y.-N. Elevated Levels of Cholesterol-Rich Lipid Rafts in Cancer Cells Are Correlated with Apoptosis Sensitivity Induced by Cholesterol-Depleting Agents. Am. J. Pathol. 2006, 168, 1107–1118; quiz 1404–1405. [Google Scholar] [CrossRef]
- Mollinedo, F.; Gajate, C. Lipid Rafts and Clusters of Apoptotic Signaling Molecule-Enriched Rafts in Cancer Therapy. Future Oncol. 2010, 6, 811–821. [Google Scholar] [CrossRef] [PubMed]
- Cordy, J.M.; Hooper, N.M.; Turner, A.J. The Involvement of Lipid Rafts in Alzheimer’s Disease. Mol. Membr. Biol. 2006, 23, 111–122. [Google Scholar] [CrossRef]
- Rushworth, J.V.; Hooper, N.M. Lipid Rafts: Linking Alzheimer’s Amyloid-β Production, Aggregation, and Toxicity at Neuronal Membranes. Int. J. Alzheimers. Dis. 2011, 2011, 603052. [Google Scholar] [CrossRef] [PubMed]
- Hicks, D.A.; Nalivaeva, N.N.; Turner, A.J. Lipid Rafts and Alzheimer’s Disease: Protein-Lipid Interactions and Perturbation of Signaling. Front. Physiol. 2012, 3, 189. [Google Scholar] [CrossRef]
- Fabiani, C.; Antollini, S.S. Alzheimer’s Disease as a Membrane Disorder: Spatial Cross-Talk Among Beta-Amyloid Peptides, Nicotinic Acetylcholine Receptors and Lipid Rafts. Front. Cell Neurosci. 2019, 13, 309. [Google Scholar] [CrossRef]
- Mesa-Herrera, F.; Taoro-González, L.; Valdés-Baizabal, C.; Diaz, M.; Marín, R. Lipid and Lipid Raft Alteration in Aging and Neurodegenerative Diseases: A Window for the Development of New Biomarkers. Int. J. Mol. Sci. 2019, 20, 3810. [Google Scholar] [CrossRef] [PubMed]
- Pike, L.J. The Challenge of Lipid Rafts. J. Lipid Res. 2009, 50, S323–S328. [Google Scholar] [CrossRef] [PubMed]
- Baumgart, T.; Hess, S.T.; Webb, W.W. Imaging Coexisting Fluid Domains in Biomembrane Models Coupling Curvature and Line Tension. Nature 2003, 425, 821–824. [Google Scholar] [CrossRef]
- Meinhardt, S.; Vink, R.L.C.; Schmid, F. Monolayer Curvature Stabilizes Nanoscale Raft Domains in Mixed Lipid Bilayers. Proc. Natl. Acad. Sci. USA 2013, 110, 4476–4481. [Google Scholar] [CrossRef]
- Tsai, W.-C.; Feigenson, G.W. Lowering Line Tension with High Cholesterol Content Induces a Transition from Macroscopic to Nanoscopic Phase Domains in Model Biomembranes. BBA—Biomembr. 2019, 1861, 478–485. [Google Scholar] [CrossRef]
- Wang, T.; Chen, Z.; Wang, X.; Shyy, J.Y.-J.; Zhu, Y. Cholesterol Loading Increases the Translocation of ATP Synthase Beta Chain into Membrane Caveolae in Vascular Endothelial Cells. Biochim. Biophys. Acta 2006, 1761, 1182–1190. [Google Scholar] [CrossRef] [PubMed]
- Leyva, J.A.; Bianchet, M.A.; Amzel, L.M. Understanding ATP Synthesis: Structure and Mechanism of the F1-ATPase (Review). Mol. Membr. Biol. 2003, 20, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Houtkooper, R.H.; Vaz, F.M. Cardiolipin, the Heart of Mitochondrial Metabolism. Cell. Mol. Life Sci. 2008, 65, 2493–2506. [Google Scholar] [CrossRef] [PubMed]
- Ayala, A.; Muñoz, M.F.; Argüelles, S. Lipid Peroxidation: Production, Metabolism, and Signaling Mechanisms of Malondialdehyde and 4-Hydroxy-2-Nonenal. Oxid. Med. Cell. Longev. 2014, 2014, 360438. [Google Scholar] [CrossRef] [PubMed]
- Vähäheikkilä, M.; Peltomaa, T.; Róg, T.; Vazdar, M.; Pöyry, S.; Vattulainen, I. How Cardiolipin Peroxidation Alters the Properties of the Inner Mitochondrial Membrane? Chem. Phys. Lipids 2018, 214, 15–23. [Google Scholar] [CrossRef] [PubMed]
- Sankhagowit, S.; Lee, E.Y.; Wong, G.C.L.; Malmstadt, N. Oxidation of Membrane Curvature-Regulating Phosphatidylethanolamine Lipid Results in Formation of Bilayer and Cubic Structures. Langmuir 2016, 32, 2450–2457. [Google Scholar] [CrossRef]
- Acehan, D.; Malhotra, A.; Xu, Y.; Ren, M.; Stokes, D.L.; Schlame, M. Cardiolipin Affects the Supramolecular Organization of ATP Synthase in Mitochondria. Biophys. J. 2011, 100, 2184–2192. [Google Scholar] [CrossRef]
- Garcia, A.; Pochinda, S.; Elgaard-Jørgensen, P.N.; Khandelia, H.; Clarke, R.J. Evidence for ATP Interaction with Phosphatidylcholine Bilayers. Langmuir 2019, 35, 9944–9953. [Google Scholar] [CrossRef] [PubMed]
- Pizzino, G.; Irrera, N.; Cucinotta, M.; Pallio, G.; Mannino, F.; Arcoraci, V.; Squadrito, F.; Altavilla, D.; Bitto, A. Oxidative Stress: Harms and Benefits for Human Health. Oxid. Med. Cell. Longev. 2017, 2017, 8416763. [Google Scholar] [CrossRef] [PubMed]
- Coban, O.; Popov, J.; Burger, M.; Vobornik, D.; Johnston, L.J. Transition from Nanodomains to Microdomains Induced by Exposure of Lipid Monolayers to Air. Biophys. J. 2007, 92, 2842–2853. [Google Scholar] [CrossRef] [PubMed]
- Borst, J.W.; Visser, N.V.; Kouptsova, O.; Visser, A.J. Oxidation of Unsaturated Phospholipids in Membrane Bilayer Mixtures Is Accompanied by Membrane Fluidity Changes. Biochim. Biophys. Acta 2000, 1487, 61–73. [Google Scholar] [CrossRef]
- Runas, K.A.; Malmstadt, N. Low Levels of Lipid Oxidation Radically Increase the Passive Permeability of Lipid Bilayers. Soft Matter. 2015, 11, 499–505. [Google Scholar] [CrossRef]
- Cogliati, S.; Enriquez, J.A.; Scorrano, L. Mitochondrial Cristae: Where Beauty Meets Functionality. Trends Biochem. Sci. 2016, 41, 261–273. [Google Scholar] [CrossRef]
- Kondadi, A.K.; Anand, R.; Reichert, A.S. Cristae Membrane Dynamics—A Paradigm Change. Trends Cell Biol. 2020, 30, 923–936. [Google Scholar] [CrossRef] [PubMed]
- Horvath, S.E.; Daum, G. Lipids of Mitochondria. Prog. Lipid Res. 2013, 52, 590–614. [Google Scholar] [CrossRef]
- Agrawal, A.; Ramachandran, R. Exploring the Links between Lipid Geometry and Mitochondrial Fission: Emerging Concepts. Mitochondrion 2019, 49, 305–313. [Google Scholar] [CrossRef] [PubMed]
- Vetica, F.; Sansone, A.; Meliota, C.; Batani, G.; Roberti, M.; Chatgilialoglu, C.; Ferreri, C. Free-Radical-Mediated Formation of Trans-Cardiolipin Isomers, Analytical Approaches for Lipidomics and Consequences of the Structural Organization of Membranes. Biomolecules 2020, 10, 1189. [Google Scholar] [CrossRef]
- Elías-Wolff, F.; Lindén, M.; Lyubartsev, A.P.; Brandt, E.G. Curvature Sensing by Cardiolipin in Simulated Buckled Membranes. Soft Matter 2019, 15, 792–802. [Google Scholar] [CrossRef] [PubMed]
- Wilson, B.A.; Ramanathan, A.; Lopez, C.F. Cardiolipin-Dependent Properties of Model Mitochondrial Membranes from Molecular Simulations. Biophys. J. 2019, 117, 429–444. [Google Scholar] [CrossRef] [PubMed]
- Ikon, N.; Ryan, R.O. Cardiolipin and Mitochondrial Cristae Organization. Biochim. Biophys. Acta Biomembr. 2017, 1859, 1156–1163. [Google Scholar] [CrossRef]
- Beltrán-Heredia, E.; Tsai, F.-C.; Salinas-Almaguer, S.; Cao, F.J.; Bassereau, P.; Monroy, F. Membrane Curvature Induces Cardiolipin Sorting. Commun Biol 2019, 2, 225. [Google Scholar] [CrossRef]
- Mileykovskaya, E.; Dowhan, W. Cardiolipin Membrane Domains in Prokaryotes and Eukaryotes. Biochim. Biophys. Acta 2009, 1788, 2084–2091. [Google Scholar] [CrossRef] [PubMed]
- Mukhopadhyay, R.; Huang, K.C.; Wingreen, N.S. Lipid Localization in Bacterial Cells through Curvature-Mediated Microphase Separation. Biophys. J. 2008, 95, 1034–1049. [Google Scholar] [CrossRef]
- Xu, T.; Pagadala, V.; Mueller, D.M. Understanding Structure, Function, and Mutations in the Mitochondrial ATP Synthase. Microb. Cell Fact. 2015, 2, 105–125. [Google Scholar] [CrossRef] [PubMed]
- Lee, R.G.; Gao, J.; Siira, S.J.; Shearwood, A.-M.; Ermer, J.A.; Hofferek, V.; Mathews, J.C.; Zheng, M.; Reid, G.E.; Rackham, O.; et al. Cardiolipin is Required for Membrane Docking of Mitochondrial Ribosomes and Protein Synthesis. J. Cell Sci. 2020, 133, jcs240374. [Google Scholar] [CrossRef]
- Basu Ball, W.; Neff, J.K.; Gohil, V.M. The Role of Nonbilayer Phospholipids in Mitochondrial Structure and Function. FEBS Lett. 2018, 592, 1273–1290. [Google Scholar] [CrossRef]
- Eble, K.S.; Coleman, W.B.; Hantgan, R.R.; Cunningham, C.C. Tightly Associated Cardiolipin in the Bovine Heart Mitochondrial ATP Synthase as Analyzed by 31P Nuclear Magnetic Resonance Spectroscopy. J. Biol. Chem. 1990, 265, 19434–19440. [Google Scholar] [CrossRef]
- Gasanov, S.E.; Kim, A.A.; Yaguzhinsky, L.S.; Dagda, R.K. Non-Bilayer Structures in Mitochondrial Membranes Regulate ATP Synthase Activity. Biochim. Biophys. Acta Biomembr. 2018, 1860, 586–599. [Google Scholar] [CrossRef]
- Prola, A.; Blondelle, J.; Vandestienne, A.; Piquereau, J.; Denis, R.G.P.; Guyot, S.; Chauvin, H.; Mourier, A.; Maurer, M.; Henry, C.; et al. Cardiolipin Content Controls Mitochondrial Coupling and Energetic Efficiency in Muscle. Sci. Adv. 2021, 7, eabd6322. [Google Scholar] [CrossRef]
- Paradies, G.; Paradies, V.; De Benedictis, V.; Ruggiero, F.M.; Petrosillo, G. Functional Role of Cardiolipin in Mitochondrial Bioenergetics. Biochim. Biophys. Acta 2014, 1837, 408–417. [Google Scholar] [CrossRef]
- Chicco, A.J.; Sparagna, G.C. Role of Cardiolipin Alterations in Mitochondrial Dysfunction and Disease. Am. J. Physiol. Cell Physiol. 2007, 292, C33–C44. [Google Scholar] [CrossRef] [PubMed]
- Lesnefsky, E.J.; Slabe, T.J.; Stoll, M.S.; Minkler, P.E.; Hoppel, C.L. Myocardial Ischemia Selectively Depletes Cardiolipin in Rabbit Heart Subsarcolemmal Mitochondria. Am. J. Physiol. Heart Circ. Physiol. 2001, 280, H2770–H2778. [Google Scholar] [CrossRef] [PubMed]
- Paradies, G.; Paradies, V.; Ruggiero, F.M.; Petrosillo, G. Oxidative Stress, Cardiolipin and Mitochondrial Dysfunction in Nonalcoholic Fatty Liver Disease. World J. Gastroenterol. 2014, 20, 14205–14218. [Google Scholar] [CrossRef] [PubMed]
- Gredilla, R.; López Torres, M.; Portero-Otín, M.; Pamplona, R.; Barja, G. Influence of Hyper- and Hypothyroidism on Lipid Peroxidation, Unsaturation of Phospholipids, Glutathione System and Oxidative Damage to Nuclear and Mitochondrial DNA in Mice Skeletal Muscle. Mol. Cell Biochem. 2001, 221, 41–48. [Google Scholar] [CrossRef]
- Li, J.; Romestaing, C.; Han, X.; Li, Y.; Hao, X.; Wu, Y.; Sun, C.; Liu, X.; Jefferson, L.S.; Xiong, J.; et al. Cardiolipin Remodeling by ALCAT1 Links Oxidative Stress and Mitochondrial Dysfunction to Obesity. Cell Metab. 2010, 12, 154–165. [Google Scholar] [CrossRef] [PubMed]
- Shi, Y. Emerging Roles of Cardiolipin Remodeling in Mitochondrial Dysfunction Associated with Diabetes, Obesity, and Cardiovascular Diseases. J. Biomed. Res. 2010, 24, 6–15. [Google Scholar] [CrossRef]
- Ahmadpour, S.T.; Mahéo, K.; Servais, S.; Brisson, L.; Dumas, J.-F. Cardiolipin, the Mitochondrial Signature Lipid: Implication in Cancer. Int. J. Mol. Sci. 2020, 21, 8031. [Google Scholar] [CrossRef]
- Monteiro-Cardoso, V.F.; Oliveira, M.M.; Melo, T.; Domingues, M.R.M.; Moreira, P.I.; Ferreiro, E.; Peixoto, F.; Videira, R.A. Cardiolipin Profile Changes Are Associated to the Early Synaptic Mitochondrial Dysfunction in Alzheimer’s Disease. J. Alzheimers. Dis. 2015, 43, 1375–1392. [Google Scholar] [CrossRef]
- Gaudioso, A.; Garcia-Rozas, P.; Casarejos, M.J.; Pastor, O.; Rodriguez-Navarro, J.A. Lipidomic Alterations in the Mitochondria of Aged Parkin Null Mice Relevant to Autophagy. Front. Neurosci. 2019, 13, 329. [Google Scholar] [CrossRef] [PubMed]
- Tyurina, Y.Y.; Polimova, A.M.; Maciel, E.; Tyurin, V.A.; Kapralova, V.I.; Winnica, D.E.; Vikulina, A.S.; Domingues, M.R.M.; McCoy, J.; Sanders, L.H.; et al. LC/MS Analysis of Cardiolipins in Substantia Nigra and Plasma of Rotenone-Treated Rats: Implication for Mitochondrial Dysfunction in Parkinson’s Disease. Free Radic. Res. 2015, 49, 681–691. [Google Scholar] [CrossRef]
- Chaves-Filho, A.B.; Pinto, I.F.D.; Dantas, L.S.; Xavier, A.M.; Inague, A.; Faria, R.L.; Medeiros, M.H.G.; Glezer, I.; Yoshinaga, M.Y.; Miyamoto, S. Alterations in Lipid Metabolism of Spinal Cord Linked to Amyotrophic Lateral Sclerosis. Sci. Rep. 2019, 9, 11642. [Google Scholar] [CrossRef] [PubMed]
- Zegallai, H.M.; Hatch, G.M. Barth Syndrome: Cardiolipin, Cellular Pathophysiology, Management, and Novel Therapeutic Targets. Mol. Cell Biochem. 2021, 476, 1605–1629. [Google Scholar] [CrossRef]
- Cole, L.K.; Kim, J.H.; Amoscato, A.A.; Tyurina, Y.Y.; Bay, R.H.; Karimi, B.; Siddiqui, T.J.; Kagan, V.E.; Hatch, G.M.; Kauppinen, T.M. Aberrant Cardiolipin Metabolism is Associated with Cognitive Deficiency and Hippocampal Alteration in Tafazzin Knockdown Mice. Biochim. Biophys. Acta Mol. Basis Dis. 2018, 1864, 3353–3367. [Google Scholar] [CrossRef] [PubMed]
- Sparvero, L.J.; Amoscato, A.A.; Fink, A.B.; Anthonymuthu, T.; New, L.A.; Kochanek, P.M.; Watkins, S.; Kagan, V.E.; Bayır, H. Imaging Mass Spectrometry Reveals Loss of Polyunsaturated Cardiolipins in the Cortical Contusion, Hippocampus, and Thalamus after Traumatic Brain Injury. J. Neurochem. 2016, 139, 659–675. [Google Scholar] [CrossRef]
- Anthonymuthu, T.S.; Kenny, E.M.; Hier, Z.E.; Clark, R.S.B.; Kochanek, P.M.; Kagan, V.E.; Bayır, H. Detection of Brain Specific Cardiolipins in Plasma after Experimental Pediatric Head Injury. Exp. Neurol. 2019, 316, 63–73. [Google Scholar] [CrossRef]
- Helmer, P.O.; Wienken, C.M.; Korf, A.; Hayen, H. Mass Spectrometric Investigation of Cardiolipins and Their Oxidation Products after Two-Dimensional Heart-Cut Liquid Chromatography. J. Chromatogr. A 2020, 1619, 460918. [Google Scholar] [CrossRef]
- Helmer, P.O.; Nicolai, M.M.; Schwantes, V.; Bornhorst, J.; Hayen, H. Investigation of Cardiolipin Oxidation Products as a New Endpoint for Oxidative Stress in C. Elegans by Means of Online Two-Dimensional Liquid Chromatography and High-Resolution Mass Spectrometry. Free Radic. Biol. Med. 2021, 162, 216–224. [Google Scholar] [CrossRef]
- Jacob, R.F.; Mason, R.P. Lipid Peroxidation Induces Cholesterol Domain Formation in Model Membranes. J. Biol. Chem. 2005, 280, 39380–39387. [Google Scholar] [CrossRef] [PubMed]
- Munishkina, L.A.; Fink, A.L. Fluorescence as a Method to Reveal Structures and Membrane-Interactions of Amyloidogenic Proteins. Biochim. Biophys. Acta 2007, 1768, 1862–1885. [Google Scholar] [CrossRef] [PubMed]
- Huang, Z.; Tyurina, Y.Y.; Jiang, J.; Tokarska-Schlattner, M.; Boissan, M.; Lacombe, M.-L.; Epand, R.; Schlattner, U.; Epand, R.M.; Kagan, V.E. Externalization of Cardiolipin as an “Eat-Me” Mitophageal Signal Is Facilitated by NDPK-D. Biophys. J. 2014, 106, 184a. [Google Scholar] [CrossRef]
- Manganelli, V.; Capozzi, A.; Recalchi, S.; Riitano, G.; Mattei, V.; Longo, A.; Misasi, R.; Garofalo, T.; Sorice, M. The Role of Cardiolipin as a Scaffold Mitochondrial Phospholipid in Autophagosome Formation: In Vitro Evidence. Biomolecules 2021, 11, 222. [Google Scholar] [CrossRef] [PubMed]
- Kagan, V.E.; Tyurin, V.A.; Jiang, J.; Tyurina, Y.Y.; Ritov, V.B.; Amoscato, A.A.; Osipov, A.N.; Belikova, N.A.; Kapralov, A.A.; Kini, V.; et al. Cytochrome c Acts as a Cardiolipin Oxygenase Required for Release of Proapoptotic Factors. Nat. Chem. Biol. 2005, 1, 223–232. [Google Scholar] [CrossRef]
- Petrosillo, G.; Casanova, G.; Matera, M.; Ruggiero, F.M.; Paradies, G. Interaction of Peroxidized Cardiolipin with Rat-Heart Mitochondrial Membranes: Induction of Permeability Transition and Cytochrome c Release. FEBS Lett. 2006, 580, 6311–6316. [Google Scholar] [CrossRef]
- Li, X.-X.; Tsoi, B.; Li, Y.-F.; Kurihara, H.; He, R.-R. Cardiolipin and Its Different Properties in Mitophagy and Apoptosis. J. Histochem. Cytochem. 2015, 63, 301–311. [Google Scholar] [CrossRef]
- Dudek, J. Role of Cardiolipin in Mitochondrial Signaling Pathways. Front. Cell Dev. Biol. 2017, 5, 90. [Google Scholar] [CrossRef]
- Huang, W.; Choi, W.; Hu, W.; Mi, N.; Guo, Q.; Ma, M.; Liu, M.; Tian, Y.; Lu, P.; Wang, F.-L.; et al. Crystal Structure and Biochemical Analyses Reveal Beclin 1 as a Novel Membrane Binding Protein. Cell Res. 2012, 22, 473–489. [Google Scholar] [CrossRef]
- Gonzalvez, F.; Pariselli, F.; Dupaigne, P.; Budihardjo, I.; Lutter, M.; Antonsson, B.; Diolez, P.; Manon, S.; Martinou, J.-C.; Goubern, M.; et al. tBid Interaction with Cardiolipin Primarily Orchestrates Mitochondrial Dysfunctions and Subsequently Activates Bax and Bak. Cell Death Differ. 2005, 12, 614–626. [Google Scholar] [CrossRef]
- Gonzalvez, F.; Schug, Z.T.; Houtkooper, R.H.; MacKenzie, E.D.; Brooks, D.G.; Wanders, R.J.A.; Petit, P.X.; Vaz, F.M.; Gottlieb, E. Cardiolipin Provides an Essential Activating Platform for Caspase-8 on Mitochondria. J. Cell Biol. 2008, 183, 681–696. [Google Scholar] [CrossRef]
- Iyer, S.S.; He, Q.; Janczy, J.R.; Elliott, E.I.; Zhong, Z.; Olivier, A.K.; Sadler, J.J.; Knepper-Adrian, V.; Han, R.; Qiao, L.; et al. Mitochondrial Cardiolipin is Required for Nlrp3 Inflammasome Activation. Immunity 2013, 39, 311–323. [Google Scholar] [CrossRef] [PubMed]
- De Zoete, M.R.; Palm, N.W.; Zhu, S.; Flavell, R.A. Inflammasomes. Cold Spring Harb. Perspect. Biol. 2014, 6, a016287. [Google Scholar] [CrossRef]
- Sharif, H.; Wang, L.; Wang, W.L.; Magupalli, V.G.; Andreeva, L.; Qiao, Q.; Hauenstein, A.V.; Wu, Z.; Núñez, G.; Mao, Y.; et al. Structural Mechanism for NEK7-Licensed Activation of NLRP3 Inflammasome. Nature 2019, 570, 338–343. [Google Scholar] [CrossRef] [PubMed]
- He, Y.; Hara, H.; Núñez, G. Mechanism and Regulation of NLRP3 Inflammasome Activation. Trends Biochem. Sci. 2016, 41, 1012–1021. [Google Scholar] [CrossRef] [PubMed]
- Seoane, P.I.; Lee, B.; Hoyle, C.; Yu, S.; Lopez-Castejon, G.; Lowe, M.; Brough, D. The NLRP3-Inflammasome as a Sensor of Organelle Dysfunction. J. Cell Biol. 2020, 219. [Google Scholar] [CrossRef]
- Yeon, S.H.; Yang, G.; Lee, H.E.; Lee, J.Y. Oxidized Phosphatidylcholine Induces the Activation of NLRP3 Inflammasome in Macrophages. J. Leukoc. Biol. 2017, 101, 205–215. [Google Scholar] [CrossRef]
- Elliott, E.I.; Miller, A.N.; Banoth, B.; Iyer, S.S.; Stotland, A.; Weiss, J.P.; Gottlieb, R.A.; Sutterwala, F.S.; Cassel, S.L. Cutting Edge: Mitochondrial Assembly of the NLRP3 Inflammasome Complex Is Initiated at Priming. J. Immunol. 2018, 200, 3047–3052. [Google Scholar] [CrossRef]
- Raturi, A.; Simmen, T. Where the Endoplasmic Reticulum and the Mitochondrion Tie the Knot: The Mitochondria-Associated Membrane (MAM). Biochim. Biophys. Acta 2013, 1833, 213–224. [Google Scholar] [CrossRef]
- Wang, P.; Li, J.; Sha, B. The ER Stress Sensor PERK Luminal Domain Functions as a Molecular Chaperone to Interact with Misfolded Proteins. Acta Cryst. D Struct. Biol. 2016, 72 Pt 12, 1290–1297. [Google Scholar] [CrossRef] [PubMed]
- Kumar, V.; Maity, S. ER Stress-Sensor Proteins and ER-Mitochondrial Crosstalk-Signaling Beyond (ER) Stress Response. Biomolecules 2021, 11, 173. [Google Scholar] [CrossRef]
- Gomes, E.; Shorter, J. The Molecular Language of Membraneless Organelles. J. Biol. Chem. 2019, 294, 7115–7127. [Google Scholar] [CrossRef]
- Gilmozzi, V.; Gentile, G.; Castelo Rueda, M.P.; Hicks, A.A.; Pramstaller, P.P.; Zanon, A.; Lévesque, M.; Pichler, I. Interaction of Alpha-Synuclein with Lipids: Mitochondrial Cardiolipin as a Critical Player in the Pathogenesis of Parkinson’s Disease. Front. Neurosci. 2020, 14, 578993. [Google Scholar] [CrossRef] [PubMed]
- Ray, S.; Singh, N.; Kumar, R.; Patel, K.; Pandey, S.; Datta, D.; Mahato, J.; Panigrahi, R.; Navalkar, A.; Mehra, S.; et al. α-Synuclein Aggregation Nucleates through Liquid-Liquid Phase Separation. Nat. Chem. 2020, 12, 705–716. [Google Scholar] [CrossRef]
- Stefanis, L. α-Synuclein in Parkinson’s Disease. Cold Spring Harb. Perspect. Med. 2012, 2, a009399. [Google Scholar] [CrossRef]
- Falabella, M.; Vernon, H.J.; Hanna, M.G.; Claypool, S.M.; Pitceathly, R.D.S. Cardiolipin, Mitochondria, and Neurological Disease. Trends Endocrinol. Metab. 2021, 32, 224–237. [Google Scholar] [CrossRef] [PubMed]
- Vicario, M.; Cieri, D.; Brini, M.; Calì, T. The Close Encounter between Alpha-Synuclein and Mitochondria. Front. Neurosci. 2018, 12, 388. [Google Scholar] [CrossRef]
- Fortin, D.L.; Troyer, M.D.; Nakamura, K.; Kubo, S.-I.; Anthony, M.D.; Edwards, R.H. Lipid Rafts Mediate the Synaptic Localization of Alpha-Synuclein. J. Neurosci. 2004, 24, 6715–6723. [Google Scholar] [CrossRef] [PubMed]
- Ludtmann, M.H.R.; Angelova, P.R.; Ninkina, N.N.; Gandhi, S.; Buchman, V.L.; Abramov, A.Y. Monomeric Alpha-Synuclein Exerts a Physiological Role on Brain ATP Synthase. J. Neurosci. 2016, 36, 10510–10521. [Google Scholar] [CrossRef]
- Ludtmann, M.; Angelova, P.; Ninkina, N.; Gandhi, S.; Buchman, V.; Abramov, A. A Physiological Role for Alpha-Synuclein in the Regulation of ATP Synthesis. Biophys. J. 2016, 110, 471a. [Google Scholar] [CrossRef]
- Wang, X.; Becker, K.; Levine, N.; Zhang, M.; Lieberman, A.P.; Moore, D.J.; Ma, J. Pathogenic Alpha-Synuclein Aggregates Preferentially Bind to Mitochondria and Affect Cellular Respiration. Acta Neuropathol. Commun. 2019, 7, 41. [Google Scholar] [CrossRef]
- Ludtmann, M.H.R.; Angelova, P.R.; Horrocks, M.H.; Choi, M.L.; Rodrigues, M.; Baev, A.Y.; Berezhnov, A.V.; Yao, Z.; Little, D.; Banushi, B.; et al. α-Synuclein Oligomers Interact with ATP Synthase and Open the Permeability Transition Pore in Parkinson’s Disease. Nat. Commun. 2018, 9, 2293. [Google Scholar] [CrossRef]
- Ghio, S.; Camilleri, A.; Caruana, M.; Ruf, V.C.; Schmidt, F.; Leonov, A.; Ryazanov, S.; Griesinger, C.; Cauchi, R.J.; Kamp, F.; et al. Cardiolipin Promotes Pore-Forming Activity of Alpha-Synuclein Oligomers in Mitochondrial Membranes. ACS Chem. Neurosci. 2019, 10, 3815–3829. [Google Scholar] [CrossRef]
- Annunziata, I.; Sano, R.; d’Azzo, A. Mitochondria-Associated ER Membranes (MAMs) and Lysosomal Storage Diseases. Cell Death Dis. 2018, 9, 328. [Google Scholar] [CrossRef]
- Faustino Mollinedo, C.G. Mitochondrial Targeting Involving Cholesterol-Rich Lipid Rafts in the Mechanism of Action of the Antitumor Ether Lipid and Alkylphospholipid Analog Edelfosine. Pharmaceutics 2021, 13, 763. [Google Scholar] [CrossRef] [PubMed]
- Dart, C. Lipid Microdomains and the Regulation of Ion Channel Function. J. Physiol. 2010, 588 Pt 17, 3169–3178. [Google Scholar] [CrossRef] [PubMed]
- Pathak, P.; London, E. Measurement of Lipid Nanodomain (raft) Formation and Size in sphingomyelin/POPC/cholesterol Vesicles Shows TX-100 and Transmembrane Helices Increase Domain Size by Coalescing Preexisting Nanodomains but Do Not Induce Domain Formation. Biophys. J. 2011, 101, 2417–2425. [Google Scholar] [CrossRef] [PubMed]
- Sharma, P.; Varma, R.; Sarasij, R.C.; Gousset, K.; Krishnamoorthy, G.; Rao, M.; Mayor, S. Nanoscale Organization of Multiple GPI-Anchored Proteins in Living Cell Membranes. Cell 2004, 116, 577–589. [Google Scholar] [CrossRef]
- Ma, Y.; Hinde, E.; Gaus, K. Nanodomains in Biological Membranes. Essays Biochem. 2015, 57, 93–107. [Google Scholar] [CrossRef] [PubMed]
- Cordeiro, R.M. Reactive Oxygen Species at Phospholipid Bilayers: Distribution, Mobility and Permeation. Biochim. Biophys. Acta 2014, 1838, 438–444. [Google Scholar] [CrossRef]
- Ayuyan, A.G.; Cohen, F.S. Lipid Peroxides Promote Large Rafts: Effects of Excitation of Probes in Fluorescence Microscopy and Electrochemical Reactions during Vesicle Formation. Biophys. J. 2006, 91, 2172–2183. [Google Scholar] [CrossRef]
- Squecco, R.; Tani, A.; Zecchi-Orlandini, S.; Formigli, L.; Francini, F. Melatonin Affects Voltage-Dependent Calcium and Potassium Currents in MCF-7 Cell Line Cultured Either in Growth or Differentiation Medium. Eur. J. Pharmacol. 2015, 758, 40–52. [Google Scholar] [CrossRef] [PubMed]
- Hiroki, M.; Suzuki, Y.; Yamamura, H. Inhibitory Effect of Melatonin on Voltage-Dependent Potassium (Kv4.2) Channels. Proc. Annu. Meet. Jpn. Pharmacol. Soc. 2020, 93, 1. [Google Scholar] [CrossRef]
- Acuna-Castroviejo, D.; Escames, G.; Rodriguez, M.I.; Lopez, L.C. Melatonin Role in the Mitochondrial Function. Front. Biosci. 2007, 12, 947–963. [Google Scholar] [CrossRef] [PubMed]
- Fang, Y.; Zhao, C.; Xiang, H.; Zhao, X.; Zhong, R. Melatonin Inhibits Formation of Mitochondrial Permeability Transition Pores and Improves Oxidative Phosphorylation of Frozen-Thawed Ram Sperm. Front. Endocrinol. 2019, 10, 896. [Google Scholar] [CrossRef]
- Petrosillo, G.; Moro, N.; Ruggiero, F.M.; Paradies, G. Melatonin Inhibits Cardiolipin Peroxidation in Mitochondria and Prevents the Mitochondrial Permeability Transition and Cytochrome c Release. Free Radic. Biol. Med. 2009, 47, 969–974. [Google Scholar] [CrossRef]
- Ono, K.; Mochizuki, H.; Ikeda, T.; Nihira, T.; Takasaki, J.-I.; Teplow, D.B.; Yamada, M. Effect of Melatonin on α-Synuclein Self-Assembly and Cytotoxicity. Neurobiol. Aging. 2012, 33, 2172–2185. [Google Scholar] [CrossRef]
- Zampol, M.A.; Barros, M.H. Melatonin Improves Survival and Respiratory Activity of Yeast Cells Challenged by Alpha-Synuclein and Menadione. Yeast 2018, 35, 281–290. [Google Scholar] [CrossRef]
- Samir, P.; Kanneganti, T.-D. DDX3X Sits at the Crossroads of Liquid-Liquid and Prionoid Phase Transitions Arbitrating Life and Death Cell Fate Decisions in Stressed Cells. DNA Cell Biol. 2020, 39, 1091–1095. [Google Scholar] [CrossRef]
- Compan, V.; Martín-Sánchez, F.; Baroja-Mazo, A.; López-Castejón, G.; Gomez, A.I.; Verkhratsky, A.; Brough, D.; Pelegrín, P. Apoptosis-Associated Speck-like Protein Containing a CARD Forms Specks but Does Not Activate Caspase-1 in the Absence of NLRP3 during Macrophage Swelling. J. Immunol. 2015, 194, 1261–1273. [Google Scholar] [CrossRef]
- Stehlik, C.; Lee, S.H.; Dorfleutner, A.; Stassinopoulos, A.; Sagara, J.; Reed, J.C. Apoptosis-Associated Speck-like Protein Containing a Caspase Recruitment Domain Is a Regulator of Procaspase-1 Activation. J. Immunol. 2003, 171, 6154–6163. [Google Scholar] [CrossRef]
- Ozgur, S.; Buchwald, G.; Falk, S.; Chakrabarti, S.; Prabu, J.R.; Conti, E. The Conformational Plasticity of Eukaryotic RNA-Dependent ATPases. FEBS J. 2015, 282, 850–863. [Google Scholar] [CrossRef]
- Owttrim, G.W. RNA Helicases: Diverse Roles in Prokaryotic Response to Abiotic Stress. RNA Biol. 2013, 10, 96–110. [Google Scholar] [CrossRef]
- Hondele, M.; Sachdev, R.; Heinrich, S.; Wang, J.; Vallotton, P.; Fontoura, B.M.A.; Weis, K. DEAD-Box ATPases Are Global Regulators of Phase-Separated Organelles. Nature 2019, 573, 144–148. [Google Scholar] [CrossRef]
- Fox, D.; Man, S.M. DDX3X: Stressing the NLRP3 Inflammasome. Cell Res. 2019, 29, 969–970. [Google Scholar] [CrossRef]
- Guan, Y.; Han, F. Key Mechanisms and Potential Targets of the NLRP3 Inflammasome in Neurodegenerative Diseases. Front. Integr. Neurosci. 2020, 14, 37. [Google Scholar] [CrossRef] [PubMed]
- Arioz, B.I.; Tastan, B.; Tarakcioglu, E.; Tufekci, K.U.; Olcum, M.; Ersoy, N.; Bagriyanik, A.; Genc, K.; Genc, S. Melatonin Attenuates LPS-Induced Acute Depressive-Like Behaviors and Microglial NLRP3 Inflammasome Activation Through the SIRT1/Nrf2 Pathway. Front. Immunol. 2019, 10, 1511. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Lu, X.; Liu, M.; Fan, H.; Zheng, H.; Zhang, S.; Rahman, N.; Wołczyński, S.; Kretowski, A.; Li, X. Melatonin Inhibits Inflammasome-Associated Activation of Endothelium and Macrophages Attenuating Pulmonary Arterial Hypertension. Cardiovasc. Res. 2020, 116, 2156–2169. [Google Scholar] [CrossRef] [PubMed]
- Chen, F.; Jiang, G.; Liu, H.; Li, Z.; Pei, Y.; Wang, H.; Pan, H.; Cui, H.; Long, J.; Wang, J.; et al. Melatonin Alleviates Intervertebral Disc Degeneration by Disrupting the IL-1β/NF-κB-NLRP3 Inflammasome Positive Feedback Loop. Bone Res. 2020, 8, 10. [Google Scholar] [CrossRef]
- Heerklotz, H. Triton Promotes Domain Formation in Lipid Raft Mixtures. Biophys. J. 2002, 83, 2693–2701. [Google Scholar] [CrossRef]
- Aponte-Santamaría, C.; Brunken, J.; Gräter, F. Stress Propagation through Biological Lipid Bilayers in Silico. J. Am. Chem. Soc. 2017, 139, 13588–13591. [Google Scholar] [CrossRef]
- Reiter, R.J. Melatonin: Lowering the High Price of Free Radicals. News Physiol. Sci. 2000, 15, 246–250. [Google Scholar] [CrossRef]
- Severcan, F.; Sahin, I.; Kazanci, N. Melatonin Strongly Interacts with Zwitterionic Model Membranes--Evidence from Fourier Transform Infrared Spectroscopy and Differential Scanning Calorimetry. Biochim. Biophys. Acta 2005, 1668, 215–222. [Google Scholar] [CrossRef]
- Mei, N.; Robinson, M.; Davis, J.H.; Leonenko, Z. Melatonin Alters Fluid Phase Co-Existence in POPC/DPPC/cholesterol Membranes. Biophys. J. 2020, 119, 2391–2402. [Google Scholar] [CrossRef]
- Bongiorno, D.; Ceraulo, L.; Ferrugia, M.; Filizzola, F.; Giordano, C.; Ruggirello, A.; Liveri, V.T. H-NMR and FT-IR Study of the State of Melatonin Confined in Membrane Models: Location and Interactions of Melatonin in Water Free Lecithin and AOT Reversed Micelles. Arkivoc 2004, 2004, 251–262. [Google Scholar] [CrossRef]
- Choi, Y.; Attwood, S.J.; Hoopes, M.I.; Drolle, E.; Karttunen, M.; Leonenko, Z. Melatonin Directly Interacts with Cholesterol and Alleviates Cholesterol Effects in Dipalmitoylphosphatidylcholine Monolayers. Soft Matter 2014, 10, 206–213. [Google Scholar] [CrossRef] [PubMed]
- Del Mar Martínez-Senac, M.; Villalaín, J.; Gómez-Fernández, J.C. Structure of the Alzheimer Beta-Amyloid Peptide (25-35) and Its Interaction with Negatively Charged Phospholipid Vesicles. Eur. J. Biochem. 1999, 265, 744–753. [Google Scholar] [CrossRef] [PubMed]
- Sani, M.-A.; Gehman, J.D.; Separovic, F. Lipid Matrix Plays a Role in Abeta Fibril Kinetics and Morphology. FEBS Lett. 2011, 585, 749–754. [Google Scholar] [CrossRef] [PubMed]
- Hane, F.; Drolle, E.; Gaikwad, R.; Faught, E.; Leonenko, Z. Amyloid-β Aggregation on Model Lipid Membranes: An Atomic Force Microscopy Study. J. Alzheimers. Dis. 2011, 26, 485–494. [Google Scholar] [CrossRef] [PubMed]
- Ahyayauch, H.; Raab, M.; Busto, J.V.; Andraka, N.; Arrondo, J.-L.R.; Masserini, M.; Tvaroska, I.; Goñi, F.M. Binding of β-Amyloid (1-42) Peptide to Negatively Charged Phospholipid Membranes in the Liquid-Ordered State: Modeling and Experimental Studies. Biophys. J. 2012, 103, 453–463. [Google Scholar] [CrossRef] [PubMed]
- Ding, H.; Schauerte, J.A.; Steel, D.G.; Gafni, A. β-Amyloid (1-40) Peptide Interactions with Supported Phospholipid Membranes: A Single-Molecule Study. Biophys. J. 2012, 103, 1500–1509. [Google Scholar] [CrossRef]
- Magarkar, A.; Dhawan, V.; Kallinteri, P.; Viitala, T.; Elmowafy, M.; Róg, T.; Bunker, A. Cholesterol Level Affects Surface Charge of Lipid Membranes in Saline Solution. Sci. Rep. 2014, 4, 5005. [Google Scholar] [CrossRef]
- Drolle, E.; Gaikwad, R.M.; Leonenko, Z. Nanoscale Electrostatic Domains in Cholesterol-Laden Lipid Membranes Create a Target for Amyloid Binding. Biophys. J. 2012, 103, L27–L29. [Google Scholar] [CrossRef]
- Finot, E.; Leonenko, Y.; Moores, B.; Eng, L.; Amrein, M.; Leonenko, Z. Effect of Cholesterol on Electrostatics in Lipid-Protein Films of a Pulmonary Surfactant. Langmuir 2010, 26, 1929–1935. [Google Scholar] [CrossRef]
- Eckert, G.P.; Kirsch, C.; Leutz, S.; Wood, W.G.; Müller, W.E. Cholesterol Modulates Amyloid Beta-Peptide’s Membrane Interactions. Pharmacopsychiatry 2003, 36 (Suppl. 2), S136–S143. [Google Scholar] [CrossRef] [PubMed]
- Gibson Wood, W.; Eckert, G.P.; Igbavboa, U.; Müller, W.E. Amyloid Beta-Protein Interactions with Membranes and Cholesterol: Causes or Casualties of Alzheimer’s Disease. Biochim. Biophys. Acta 2003, 1610, 281–290. [Google Scholar] [CrossRef]
- Matsubara, E.; Bryant-Thomas, T.; Pacheco Quinto, J.; Henry, T.L.; Poeggeler, B.; Herbert, D.; Cruz-Sanchez, F.; Chyan, Y.-J.; Smith, M.A.; Perry, G.; et al. Melatonin Increases Survival and Inhibits Oxidative and Amyloid Pathology in a Transgenic Model of Alzheimer’s Disease. J. Neurochem. 2003, 85, 1101–1108. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.-Z.; Wang, Z.-F. Role of Melatonin in Alzheimer-like Neurodegeneration. Acta Pharmacol. Sin. 2006, 27, 41–49. [Google Scholar] [CrossRef]
- Vincent, B. Protective Roles of Melatonin against the Amyloid-Dependent Development of Alzheimer’s Disease: A Critical Review. Pharmacol. Res. 2018, 134, 223–237. [Google Scholar] [CrossRef]
- Chinchalongporn, V.; Shukla, M.; Govitrapong, P. Melatonin Ameliorates Aβ42 -Induced Alteration of βAPP-Processing Secretases via the Melatonin Receptor through the Pin1/GSK3β/NF-κB Pathway in SH-SY5Y Cells. J. Pineal Res. 2018, 64, e12470. [Google Scholar] [CrossRef]
- Li, Y.; Zhang, J.; Wan, J.; Liu, A.; Sun, J. Melatonin Regulates Aβ Production/clearance Balance and Aβ Neurotoxicity: A Potential Therapeutic Molecule for Alzheimer’s Disease. Biomed. Pharmacother. 2020, 132, 110887. [Google Scholar] [CrossRef]
- Pappolla, M.; Bozner, P.; Soto, C.; Shao, H.; Robakis, N.K.; Zagorski, M.; Frangione, B.; Ghiso, J. Inhibition of Alzheimer Beta-Fibrillogenesis by Melatonin. J. Biol. Chem. 1998, 273, 7185–7188. [Google Scholar] [CrossRef] [PubMed]
- Dies, H.; Toppozini, L.; Rheinstädter, M.C. The Interaction between Amyloid-β Peptides and Anionic Lipid Membranes Containing Cholesterol and Melatonin. PLoS ONE 2014, 9, e99124. [Google Scholar] [CrossRef]
- Lu, H.; Martí, J. Binding and Dynamics of Melatonin at the Interface of Phosphatidylcholine-Cholesterol Membranes. PLoS ONE 2019, 14, e0224624. [Google Scholar] [CrossRef] [PubMed]
- Akkas, S.B.; Inci, S.; Zorlu, F.; Severcan, F. Melatonin Affects the Order, Dynamics and Hydration of Brain Membrane Lipids. J. Mol. Struct. 2007, 834–836, 207–215. [Google Scholar] [CrossRef]
- Dies, H.; Cheung, B.; Tang, J.; Rheinstädter, M.C. The Organization of Melatonin in Lipid Membranes. Biochim. Biophys. Acta 2015, 1848, 1032–1040. [Google Scholar] [CrossRef] [PubMed]
- Los, D.A.; Murata, N. Membrane Fluidity and Its Roles in the Perception of Environmental Signals. Biochim. Biophys. Acta 2004, 1666, 142–157. [Google Scholar] [CrossRef] [PubMed]
- Choe, M.; Jackson, C.; Yu, B.P. Lipid Peroxidation Contributes to Age-Related Membrane Rigidity. Free Radic. Biol. Med. 1995, 18, 977–984. [Google Scholar] [CrossRef]
- De la Haba, C.; Palacio, J.R.; Martínez, P.; Morros, A. Effect of Oxidative Stress on Plasma Membrane Fluidity of THP-1 Induced Macrophages. Biochim. Biophys. Acta 2013, 1828, 357–364. [Google Scholar] [CrossRef]
- Tenchov, B.; Koynova, R. Cubic Phases in Membrane Lipids. Eur. Biophys. J. 2012, 41, 841–850. [Google Scholar] [CrossRef]
- Landh, T. From Entangled Membranes to Eclectic Morphologies: Cubic Membranes as Subcellular Space Organizers. FEBS Lett. 1995, 369, 13–17. [Google Scholar] [CrossRef]
- Catalá, Á. Lipid Peroxidation Modifies the Assembly of Biological Membranes “The Lipid Whisker Model”. Front. Physiol. 2014, 5, 520. [Google Scholar] [CrossRef] [PubMed]
- Volinsky, R.; Paananen, R.; Kinnunen, P.K.J. Oxidized Phosphatidylcholines Promote Phase Separation of Cholesterol-Sphingomyelin Domains. Biophys. J. 2012, 103, 247–254. [Google Scholar] [CrossRef] [PubMed]
- Balakrishnan, M.; Kenworthy, A.K. Lipid Peroxidation Enhances LO/LD Domain Phase Separation in Giant Plasma Membrane Vesicles. Biophys. J. 2021, 120, 324a. [Google Scholar] [CrossRef]
- Bolmatov, D.; McClintic, W.T.; Taylor, G.; Stanley, C.B.; Do, C.; Collier, C.P.; Leonenko, Z.; Lavrentovich, M.O.; Katsaras, J. Deciphering Melatonin-Stabilized Phase Separation in Phospholipid Bilayers. Langmuir 2019, 35, 12236–12245. [Google Scholar] [CrossRef] [PubMed]
- Sanchez-Burgos, I.; Espinosa, J.R.; Joseph, J.A.; Collepardo-Guevara, R. Valency and Binding Affinity Variations Can Regulate the Multilayered Organization of Protein Condensates with Many Components. Biomolecules 2021, 11, 278. [Google Scholar] [CrossRef]
- Balmik, A.A.; Das, R.; Dangi, A.; Gorantla, N.V.; Marelli, U.K.; Chinnathambi, S. Melatonin Interacts with Repeat Domain of Tau to Mediate Disaggregation of Paired Helical Filaments. Biochim. Biophys. Acta Gen. Subj. 2020, 1864, 129467. [Google Scholar] [CrossRef]
- Wong-Ekkabut, J.; Xu, Z.; Triampo, W.; Tang, I.-M.; Tieleman, D.P.; Monticelli, L. Effect of Lipid Peroxidation on the Properties of Lipid Bilayers: A Molecular Dynamics Study. Biophys. J. 2007, 93, 4225–4236. [Google Scholar] [CrossRef]
- Kaplán, P.; Racay, P.; Lehotský, J.; Mézesová, V. Change in Fluidity of Brain Endoplasmic Reticulum Membranes by Oxygen Free Radicals: A Protective Effect of Stobadine, Alpha-Tocopherol Acetate, and Butylated Hydroxytoluene. Neurochem. Res. 1995, 20, 815–820. [Google Scholar] [CrossRef]
- Yu, B.P.; Suescun, E.A.; Yang, S.Y. Effect of Age-Related Lipid Peroxidation on Membrane Fluidity and Phospholipase A2: Modulation by Dietary Restriction. Mech. Ageing. Dev. 1992, 65, 17–33. [Google Scholar] [CrossRef]
- Rudzite, V.; Jurika, E.; Jirgensons, J. Changes in Membrane Fluidity Induced by Tryptophan and Its Metabolites. In Tryptophan, Serotonin, and Melatonin: Basic Aspects and Applications; Huether, G., Kochen, W., Simat, T.J., Steinhart, H., Eds.; Springer: Boston, MA, USA, 1999. [Google Scholar] [CrossRef]
- Alexandre, H.; Mathieu, B.; Charpentier, C. Alteration in Membrane Fluidity and Lipid Composition, and Modulation of H+-ATPase Activity in Saccharomyces Cerevisiae Caused by Decanoic Acid. Available online: https://www.microbiologyresearch.org/docserver/fulltext/micro/142/3/mic-142-3-469.pdf?expires=1616871084&id=id&accname=guest&checksum=6688BACF19B736B01B5100ACDEA617F6 (accessed on 27 March 2021).
- Keeffe, E.B.; Blankenship, N.M.; Scharschmidt, B.F. Alteration of Rat Liver Plasma Membrane Fluidity and ATPase Activity by Chlorpromazine Hydrochloride and Its Metabolites. Gastroenterology 1980, 79, 222–231. [Google Scholar] [CrossRef]
- Chen, J.J.; Yu, B.P. Alterations in Mitochondrial Membrane Fluidity by Lipid Peroxidation Products. Free Radic. Biol. Med. 1994, 17, 411–418. [Google Scholar] [CrossRef]
- Kholodenko, B.N.; Hoek, J.B.; Westerhoff, H.V. Why Cytoplasmic Signalling Proteins Should Be Recruited to Cell Membranes. Trends Cell Biol. 2000, 10, 173–178. [Google Scholar] [CrossRef]
- Botterbusch, S.; Baumgart, T. Interactions between Phase-Separated Liquids and Membrane Surfaces. NATO Adv. Sci. Inst. Ser. E Appl. Sci. 2021, 11, 1288. [Google Scholar] [CrossRef]
- Alimohamadi, H.; Rangamani, P. Modeling Membrane Curvature Generation due to Membrane−Protein Interactions. Biomolecules 2018, 8, 120. [Google Scholar] [CrossRef]
- Prévost, C.; Zhao, H.; Manzi, J.; Lemichez, E.; Lappalainen, P.; Callan-Jones, A.; Bassereau, P. IRSp53 Senses Negative Membrane Curvature and Phase Separates along Membrane Tubules. Nat. Commun. 2015, 6, 8529. [Google Scholar] [CrossRef]
- Gallop, J.L.; McMahon, H.T. BAR Domains and Membrane Curvature: Bringing Your Curves to the BAR. Biochem. Soc. Symp. 2005, 72, 223–231. [Google Scholar] [CrossRef]
- Lu, S.; Deng, R.; Jiang, H.; Song, H.; Li, S.; Shen, Q.; Huang, W.; Nussinov, R.; Yu, J.; Zhang, J. The Mechanism of ATP-Dependent Allosteric Protection of Akt Kinase Phosphorylation. Structure 2015, 23, 1725–1734. [Google Scholar] [CrossRef]
- Jiang, F.; Zhang, Y.; Dusting, G.J. NADPH Oxidase-Mediated Redox Signaling: Roles in Cellular Stress Response, Stress Tolerance, and Tissue Repair. Pharmacol. Rev. 2011, 63, 218–242. [Google Scholar] [CrossRef]
- Garofalo, T.; Manganelli, V.; Grasso, M.; Mattei, V.; Ferri, A.; Misasi, R.; Sorice, M. Role of Mitochondrial Raft-like Microdomains in the Regulation of Cell Apoptosis. Apoptosis 2015, 20, 621–634. [Google Scholar] [CrossRef]
- Samhan-Arias, A.K.; Garcia-Bereguiain, M.A.; Martin-Romero, F.J.; Gutierrez-Merino, C. Clustering of Plasma Membrane-Bound Cytochrome b5 Reductase within “Lipid Raft” Microdomains of the Neuronal Plasma Membrane. Mol. Cell. Neurosci. 2009, 40, 14–26. [Google Scholar] [CrossRef]
- Gostincar, C.; Turk, M.; Gunde-Cimerman, N. The Evolution of Fatty Acid Desaturases and Cytochrome b5 in Eukaryotes. J. Membr. Biol. 2010, 233, 63–72. [Google Scholar] [CrossRef] [PubMed]
- Ito, A.; Hayashi, S.; Yoshida, T. Participation of a Cytochrome b5-like Hemoprotein of Outer Mitochondrial Membrane (OM Cytochrome B) in NADH-Semidehydroascorbic Acid Reductase Activity of Rat Liver. Biochem. Biophys. Res. Commun. 1981, 101, 591–598. [Google Scholar] [CrossRef]
- Navarro, F.; Villalba, J.M.; Crane, F.L.; Mackellar, W.C.; Navas, P. A Phospholipid-Dependent NADH-Coenzyme Q Reductase from Liver Plasma Membrane. Biochem. Biophys. Res. Commun. 1995, 212, 138–143. [Google Scholar] [CrossRef] [PubMed]
- Percy, M.J.; Lappin, T.R. Recessive Congenital Methaemoglobinaemia: Cytochrome b(5) Reductase Deficiency. Br. J. Haematol. 2008, 141, 298–308. [Google Scholar] [CrossRef] [PubMed]
- Siendones, E.; SantaCruz-Calvo, S.; Martín-Montalvo, A.; Cascajo, M.V.; Ariza, J.; López-Lluch, G.; Villalba, J.M.; Acquaviva-Bourdain, C.; Roze, E.; Bernier, M.; et al. Membrane-Bound CYB5R3 Is a Common Effector of Nutritional and Oxidative Stress Response through FOXO3a and Nrf2. Antioxid. Redox Signal. 2014, 21, 1708–1725. [Google Scholar] [CrossRef] [PubMed]
- Marques-da-Silva, D.; Samhan-Arias, A.K.; Tiago, T.; Gutierrez-Merino, C. L-Type Calcium Channels and Cytochrome b5 Reductase Are Components of Protein Complexes Tightly Associated with Lipid Rafts Microdomains of the Neuronal Plasma Membrane. J. Proteom. 2010, 73, 1502–1510. [Google Scholar] [CrossRef]
- Nikiforova, A.B.; Saris, N.-E.L.; Kruglov, A.G. External Mitochondrial NADH-Dependent Reductase of Redox Cyclers: VDAC1 or Cyb5R3? Free Radic. Biol. Med. 2014, 74, 74–84. [Google Scholar] [CrossRef]
- Bakalova, R.; Zhelev, Z.; Miller, T.; Aoki, I.; Higashi, T. New Potential Biomarker for Stratification of Patients for Pharmacological Vitamin C in Adjuvant Settings of Cancer Therapy. Redox Biol. 2020, 28, 101357. [Google Scholar] [CrossRef]
- Mihara, K.; Sato, R. Molecular Cloning and Sequencing of cDNA for Yeast Porin, an Outer Mitochondrial Membrane Protein: A Search for Targeting Signal in the Primary Structure. EMBO J. 1985, 4, 769–774. [Google Scholar] [CrossRef]
- Thinnes, F.P.; Götz, H.; Kayser, H.; Benz, R.; Schmidt, W.E.; Kratzin, H.D.; Hilschmann, N. Identification of human porins. I. Purification of a porin from human B-lymphocytes (Porin 31HL) and the topochemical proof of its expression on the plasmalemma of the progenitor cell. Biol. Chem. Hoppe Seyler 1989, 370, 1253–1264. [Google Scholar]
- Bàthori, G.; Parolini, I.; Tombola, F.; Szabò, I.; Messina, A.; Oliva, M.; De Pinto, V.; Lisanti, M.; Sargiacomo, M.; Zoratti, M. Porin Is Present in the Plasma Membrane Where It Is Concentrated in Caveolae and Caveolae-Related Domains. J. Biol. Chem. 1999, 274, 29607–29612. [Google Scholar] [CrossRef]
- Herrera, J.L.; Diaz, M.; Hernández-Fernaud, J.R.; Salido, E.; Alonso, R.; Fernández, C.; Morales, A.; Marin, R. Voltage-Dependent Anion Channel as a Resident Protein of Lipid Rafts: Post-Transductional Regulation by Estrogens and Involvement in Neuronal Preservation against Alzheimer’s Disease. J. Neurochem. 2011, 116, 820–827. [Google Scholar] [CrossRef]
- De Pinto, V.; Messina, A.; Lane, D.J.R.; Lawen, A. Voltage-Dependent Anion-Selective Channel (VDAC) in the Plasma Membrane. FEBS Lett. 2010, 584, 1793–1799. [Google Scholar] [CrossRef]
- Anishkin, A.; Loukin, S.H.; Teng, J.; Kung, C. Feeling the Hidden Mechanical Forces in Lipid Bilayer Is an Original Sense. Proc. Natl. Acad. Sci. USA 2014, 111, 7898–7905. [Google Scholar] [CrossRef] [PubMed]
- Anishkin, A.; Kung, C. Stiffened Lipid Platforms at Molecular Force Foci. Proc. Natl. Acad. Sci. USA 2013, 110, 4886–4892. [Google Scholar] [CrossRef]
- Martinac, B.; Adler, J.; Kung, C. Mechanosensitive Ion Channels of E. Coli Activated by Amphipaths. Nature 1990, 348, 261–263. [Google Scholar] [CrossRef] [PubMed]
- Markin, V.S.; Martinac, B. Mechanosensitive Ion Channels as Reporters of Bilayer Expansion. A Theoretical Model. Biophys. J. 1991, 60, 1120–1127. [Google Scholar] [CrossRef]
- Samhan-Arias, A.K.; Marques-da-Silva, D.; Yanamala, N.; Gutierrez-Merino, C. Stimulation and Clustering of Cytochrome b5 Reductase in Caveolin-Rich Lipid Microdomains Is an Early Event in Oxidative Stress-Mediated Apoptosis of Cerebellar Granule Neurons. J. Proteom. 2012, 75, 2934–2949. [Google Scholar] [CrossRef] [PubMed]
- Samhan-Arias, A.K.; Fortalezas, S.; Cordas, C.M.; Moura, I.; Moura, J.J.G.; Gutierrez-Merino, C. Cytochrome b5 Reductase Is the Component from Neuronal Synaptic Plasma Membrane Vesicles That Generates Superoxide Anion upon Stimulation by Cytochrome c. Redox Biol. 2018, 15, 109–114. [Google Scholar] [CrossRef] [PubMed]
- Samhan-Arias, A.K.; Gutierrez-Merino, C. Purified NADH-Cytochrome b5 Reductase Is a Novel Superoxide Anion Source Inhibited by Apocynin: Sensitivity to Nitric Oxide and Peroxynitrite. Free Radic. Biol. Med. 2014, 73, 174–189. [Google Scholar] [CrossRef]
- La Piana, G.; Marzulli, D.; Gorgoglione, V.; Lofrumento, N.E. Porin and Cytochrome Oxidase Containing Contact Sites Involved in the Oxidation of Cytosolic NADH. Arch. Biochem. Biophys. 2005, 436, 91–100. [Google Scholar] [CrossRef] [PubMed]
- Martín-Romero, F.J.; Gutiérrez-Martín, Y.; Henao, F.; Gutiérrez-Merino, C. The NADH Oxidase Activity of the Plasma Membrane of Synaptosomes Is a Major Source of Superoxide Anion and Is Inhibited by Peroxynitrite. J. Neurochem. 2002, 82, 604–614. [Google Scholar] [CrossRef]
- Zizi, M.; Forte, M.; Blachly-Dyson, E.; Colombini, M. NADH Regulates the Gating of VDAC, the Mitochondrial Outer Membrane Channel. J. Biol. Chem. 1994, 269, 1614–1616. [Google Scholar] [CrossRef]
- Shoshan-Barmatz, V.; Shteinfer-Kuzmine, A.; Verma, A. VDAC1 at the Intersection of Cell Metabolism, Apoptosis, and Diseases. Biomolecules 2020, 10, 1485. [Google Scholar] [CrossRef] [PubMed]
- Lemasters, J.J. Evolution of Voltage-Dependent Anion Channel Function: From Molecular Sieve to Governator to Actuator of Ferroptosis. Front. Oncol. 2017, 7, 303. [Google Scholar] [CrossRef]
- Elinder, F.; Akanda, N.; Tofighi, R.; Shimizu, S.; Tsujimoto, Y.; Orrenius, S.; Ceccatelli, S. Opening of Plasma Membrane Voltage-Dependent Anion Channels (VDAC) Precedes Caspase Activation in Neuronal Apoptosis Induced by Toxic Stimuli. Cell Death Differ. 2005, 12, 1134–1140. [Google Scholar] [CrossRef]
- Rostovtseva, T.; Colombini, M. VDAC Channels Mediate and Gate the Flow of ATP: Implications for the Regulation of Mitochondrial Function. Biophys. J. 1997, 72, 1954–1962. [Google Scholar] [CrossRef]
- Rostovtseva, T.K.; Tan, W.; Colombini, M. On the Role of VDAC in Apoptosis: Fact and Fiction. J. Bioenerg. Biomembr. 2005, 37, 129–142. [Google Scholar] [CrossRef]
- McCommis, K.S.; Baines, C.P. The Role of VDAC in Cell Death: Friend or Foe? Biochim. Biophys. Acta 2012, 1818, 1444–1450. [Google Scholar] [CrossRef]
- Shoshan-Barmatz, V.; Maldonado, E.N.; Krelin, Y. VDAC1 at the Crossroads of Cell Metabolism, Apoptosis and Cell Stress. Cell Stress Chaperones 2017, 1, 11–36. [Google Scholar] [CrossRef] [PubMed]
- Camara, A.K.S.; Zhou, Y.; Wen, P.-C.; Tajkhorshid, E.; Kwok, W.-M. Mitochondrial VDAC1: A Key Gatekeeper as Potential Therapeutic Target. Front. Physiol. 2017, 8, 460. [Google Scholar] [CrossRef] [PubMed]
- Sorice, M.; Manganelli, V.; Matarrese, P.; Tinari, A.; Misasi, R.; Malorni, W.; Garofalo, T. Cardiolipin-Enriched Raft-like Microdomains Are Essential Activating Platforms for Apoptotic Signals on Mitochondria. FEBS Lett. 2009, 583, 2447–2450. [Google Scholar] [CrossRef] [PubMed]
- Sorice, M.; Mattei, V.; Matarrese, P.; Garofalo, T.; Tinari, A.; Gambardella, L.; Ciarlo, L.; Manganelli, V.; Tasciotti, V.; Misasi, R.; et al. Dynamics of Mitochondrial Raft-like Microdomains in Cell Life and Death. Commun. Integr. Biol. 2012, 5, 217–219. [Google Scholar] [CrossRef] [PubMed]
- Malorni, W.; Giammarioli, A.M.; Garofalo, T.; Sorice, M. Dynamics of Lipid Raft Components during Lymphocyte Apoptosis: The Paradigmatic Role of GD3. Apoptosis 2007, 12, 941–949. [Google Scholar] [CrossRef]
- Wong, H.-S.; Dighe, P.A.; Mezera, V.; Monternier, P.-A.; Brand, M.D. Production of Superoxide and Hydrogen Peroxide from Specific Mitochondrial Sites under Different Bioenergetic Conditions. J. Biol. Chem. 2017, 292, 16804–16809. [Google Scholar] [CrossRef]
- Brand, M.D. Mitochondrial Generation of Superoxide and Hydrogen Peroxide as the Source of Mitochondrial Redox Signaling. Free Radic. Biol. Med. 2016, 100, 14–31. [Google Scholar] [CrossRef]
- Kim, J.; Minkler, P.E.; Salomon, R.G.; Anderson, V.E.; Hoppel, C.L. Cardiolipin: Characterization of Distinct Oxidized Molecular Species. J. Lipid Res. 2011, 52, 125–135. [Google Scholar] [CrossRef]
- Schneider, C. An Update on Products and Mechanisms of Lipid Peroxidation. Mol. Nutr. Food Res. 2009, 53, 315–321. [Google Scholar] [CrossRef]
- Ting, H.-C.; Chen, L.-T.; Chen, J.-Y.; Huang, Y.-L.; Xin, R.-C.; Chan, J.-F.; Hsu, Y.-H.H. Double Bonds of Unsaturated Fatty Acids Differentially Regulate Mitochondrial Cardiolipin Remodeling. Lipids Health Dis. 2019, 18, 53. [Google Scholar] [CrossRef]
- Musatov, A. Contribution of Peroxidized Cardiolipin to Inactivation of Bovine Heart Cytochrome c Oxidase. Free Radic. Biol. Med. 2006, 41, 238–246. [Google Scholar] [CrossRef]
- Afzal, N.; Lederer, W.J.; Jafri, M.S.; Mannella, C.A. Effect of Crista Morphology on Mitochondrial ATP Output: A Computational Study. Curr. Res. Physiol. 2021, 4, 163–176. [Google Scholar] [CrossRef] [PubMed]
- Römsing, S. Development and Validation of Bioanalytical Methods: Application to Melatonin and Selected Anti-Infective Drugs; Acta Universitatis Upsaliensis: Uppsala, Sweden, 2010. [Google Scholar]
- Ceraulo, L.; Ferrugia, M.; Tesoriere, L.; Segreto, S.; Livrea, M.A.; Turco Liveri, V. Interactions of Melatonin with Membrane Models: Portioning of Melatonin in AOT and Lecithin Reversed Micelles. J. Pineal Res. 1999, 26, 108–112. [Google Scholar] [CrossRef]
- Yu, H.; Dickson, E.J.; Jung, S.-R.; Koh, D.-S.; Hille, B. High Membrane Permeability for Melatonin. J. Gen. Physiol. 2016, 147, 63–76. [Google Scholar] [CrossRef]
- Venegas, C.; García, J.A.; Escames, G.; Ortiz, F.; López, A.; Doerrier, C.; García-Corzo, L.; López, L.C.; Reiter, R.J.; Acuña-Castroviejo, D. Extrapineal Melatonin: Analysis of Its Subcellular Distribution and Daily Fluctuations. J. Pineal Res. 2012, 52, 217–227. [Google Scholar] [CrossRef]
- Reiter, R.J.; Rosales-Corral, S.; Tan, D.X.; Jou, M.J.; Galano, A.; Xu, B. Melatonin as a Mitochondria-Targeted Antioxidant: One of Evolution’s Best Ideas. Cell. Mol. Life Sci. 2017, 74, 3863–3881. [Google Scholar] [CrossRef]
- Coon, S.L.; Klein, D.C. Evolution of Arylalkylamine N-Acetyltransferase: Emergence and Divergence. Mol. Cell. Endocrinol. 2006, 252, 2–10. [Google Scholar] [CrossRef] [PubMed]
- Klein, D.C. Arylalkylamine N-Acetyltransferase: The Timezyme. J. Biol. Chem. 2007, 282, 4233–4237. [Google Scholar] [CrossRef]
- Ganguly, S.; Weller, J.L.; Ho, A.; Chemineau, P.; Malpaux, B.; Klein, D.C. Melatonin Synthesis: 14-3-3-Dependent Activation and Inhibition of Arylalkylamine N-Acetyltransferase Mediated by Phosphoserine-205. Proc. Natl. Acad. Sci. USA 2005, 102, 1222–1227. [Google Scholar] [CrossRef]
- Martín, M.; Macías, M.; Escames, G.; León, J.; Acuña-Castroviejo, D. Melatonin but Not Vitamins C and E Maintains Glutathione Homeostasis in T-Butyl Hydroperoxide-Induced Mitochondrial Oxidative Stress. FASEB J. 2000, 14, 1677–1679. [Google Scholar] [CrossRef]
- Tan, D.-X.; Manchester, L.C.; Qin, L.; Reiter, R.J. Melatonin: A Mitochondrial Targeting Molecule Involving Mitochondrial Protection and Dynamics. Int. J. Mol. Sci. 2016, 17, 2124. [Google Scholar] [CrossRef]
- Suofu, Y.; Li, W.; Jean-Alphonse, F.G.; Jia, J.; Khattar, N.K.; Li, J.; Baranov, S.V.; Leronni, D.; Mihalik, A.C.; He, Y.; et al. Dual Role of Mitochondria in Producing Melatonin and Driving GPCR Signaling to Block Cytochrome c Release. Proc. Natl. Acad. Sci. USA 2017, 114, E7997–E8006. [Google Scholar] [CrossRef]
- Manchester, L.C.; Coto-Montes, A.; Boga, J.A.; Andersen, L.P.H.; Zhou, Z.; Galano, A.; Vriend, J.; Tan, D.-X.; Reiter, R.J. Melatonin: An Ancient Molecule That Makes Oxygen Metabolically Tolerable. J. Pineal. Res. 2015, 59, 403–419. [Google Scholar] [CrossRef]
- Byeon, Y.; Lee, K.; Park, Y.-I.; Park, S.; Back, K. Molecular Cloning and Functional Analysis of Serotonin N-Acetyltransferase from the Cyanobacterium Synechocystis Sp. PCC 6803. J. Pineal. Res. 2013, 55, 371–376. [Google Scholar] [CrossRef]
- Tan, D.-X.; Manchester, L.C.; Liu, X.; Rosales-Corral, S.A.; Acuna-Castroviejo, D.; Reiter, R.J. Mitochondria and Chloroplasts as the Original Sites of Melatonin Synthesis: A Hypothesis Related to Melatonin’s Primary Function and Evolution in Eukaryotes. J. Pineal. Res. 2013, 54, 127–138. [Google Scholar] [CrossRef]
- Abhishek, A.; Bavishi, A.; Bavishi, A.; Choudhary, M. Bacterial Genome Chimaerism and the Origin of Mitochondria. Can. J. Microbiol. 2011, 57, 49–61. [Google Scholar] [CrossRef] [PubMed]
- Raven, J.A.; Allen, J.F. Genomics and Chloroplast Evolution: What Did Cyanobacteria Do for Plants? Genome Biol. 2003, 4, 209. [Google Scholar] [CrossRef] [PubMed]
- Tan, D.-X.; Manchester, L.C.; Terron, M.P.; Flores, L.J.; Reiter, R.J. One Molecule, Many Derivatives: A Never-Ending Interaction of Melatonin with Reactive Oxygen and Nitrogen Species? J. Pineal. Res. 2007, 42, 28–42. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.-N. Distribution and Dynamics of Electron Transport Complexes in Cyanobacterial Thylakoid Membranes. Biochim. Biophys. Acta 2016, 1857, 256–265. [Google Scholar] [CrossRef]
- Azaldegui, C.A.; Vecchiarelli, A.G.; Biteen, J.S. The Emergence of Phase Separation as an Organizing Principle in Bacteria. Biophys. J. 2021, 120, 1123–1138. [Google Scholar] [CrossRef]
- Guilhas, B.; Walter, J.-C.; Rech, J.; David, G.; Walliser, N.O.; Palmeri, J.; Mathieu-Demaziere, C.; Parmeggiani, A.; Bouet, J.-Y.; Le Gall, A.; et al. ATP-Driven Separation of Liquid Phase Condensates in Bacteria. Mol. Cell 2020, 79, 293–303.e4. [Google Scholar] [CrossRef] [PubMed]
- Muthunayake, N.S.; Tomares, D.T.; Childers, W.S.; Schrader, J.M. Phase-Separated Bacterial Ribonucleoprotein Bodies Organize mRNA Decay. Wiley Interdiscip. Rev. RNA 2020, 11, e1599. [Google Scholar] [CrossRef] [PubMed]
- Oliver, T.; Sánchez-Baracaldo, P.; Larkum, A.W.; Rutherford, A.W.; Cardona, T. Time-Resolved Comparative Molecular Evolution of Oxygenic Photosynthesis. Biochim. Biophys. Acta Bioenerg. 2021, 1862, 148400. [Google Scholar] [CrossRef]
- Pattanayak, G.K.; Liao, Y.; Wallace, E.W.J.; Budnik, B.; Drummond, D.A.; Rust, M.J. Daily Cycles of Reversible Protein Condensation in Cyanobacteria. Cell Rep. 2020, 32, 108032. [Google Scholar] [CrossRef]
- Bar Eyal, L.; Ranjbar Choubeh, R.; Cohen, E.; Eisenberg, I.; Tamburu, C.; Dorogi, M.; Ünnep, R.; Appavou, M.-S.; Nevo, R.; Raviv, U.; et al. Changes in Aggregation States of Light-Harvesting Complexes as a Mechanism for Modulating Energy Transfer in Desert Crust Cyanobacteria. Proc. Natl. Acad. Sci. USA 2017, 114, 9481–9486. [Google Scholar] [CrossRef]
- Wang, H.; Yan, X.; Aigner, H.; Bracher, A.; Nguyen, N.D.; Hee, W.Y.; Long, B.M.; Price, G.D.; Hartl, F.U.; Hayer-Hartl, M. Rubisco Condensate Formation by CcmM in β-Carboxysome Biogenesis. Nature 2019, 566, 131–135. [Google Scholar] [CrossRef]
- McKinney, D.W.; Buchanan, B.B.; Wolosiuk, R.A. Activation of Chloroplast ATPase by Reduced Thioredoxin. Phytochemistry 1978, 17, 794–795. [Google Scholar] [CrossRef]
- Curtis, S.E. Structure, Organization and Expression of Cyanobacterial ATP Synthase Genes. Photosynth. Res. 1988, 18, 223–244. [Google Scholar] [CrossRef]
- Pogoryelov, D.; Reichen, C.; Klyszejko, A.L.; Brunisholz, R.; Muller, D.J.; Dimroth, P.; Meier, T. The Oligomeric State of c Rings from Cyanobacterial F-ATP Synthases Varies from 13 to 15. J. Bacteriol. 2007, 189, 5895–5902. [Google Scholar] [CrossRef]
- Walraven, H.S.; Bakels, R.H.A. Function, Structure and Regulation of Cyanobacterial and Chloroplast ATP Synthase. Physiol. Plant 1996, 96, 526–532. [Google Scholar] [CrossRef]
- Buchert, F.E. Chapter Three—Chloroplast ATP Synthase from Green Microalgae. In Advances in Botanical Research; Hisabori, T., Ed.; Academic Press: Cambridge, MA, USA, 2020; Volume 96, pp. 75–118. [Google Scholar] [CrossRef]
- Carman, G.M. An Unusual Phosphatidylethanolamine-Utilizing Cardiolipin Synthase Is Discovered in Bacteria. Proc. Natl. Acad. Sci. USA 2012, 109, 16402–16403. [Google Scholar] [CrossRef]
- Kobayashi, K.; Endo, K.; Wada, H. Specific Distribution of Phosphatidylglycerol to Photosystem Complexes in the Thylakoid Membrane. Front. Plant Sci. 2017, 8, 1991. [Google Scholar] [CrossRef]
- Shadyro, O.I.; Yurkova, I.L.; Kisel, M.A. Radiation-Induced Peroxidation and Fragmentation of Lipids in a Model Membrane. Int. J. Radiat. Biol. 2002, 78, 211–217. [Google Scholar] [CrossRef]
- Althoff, T.; Mills, D.J.; Popot, J.-L.; Kühlbrandt, W. Arrangement of Electron Transport Chain Components in Bovine Mitochondrial Supercomplex I1III2IV1. EMBO J. 2011, 30, 4652–4664. [Google Scholar] [CrossRef]
- Ostrander, D.B.; Zhang, M.; Mileykovskaya, E.; Rho, M.; Dowhan, W. Lack of Mitochondrial Anionic Phospholipids Causes an Inhibition of Translation of Protein Components of the Electron Transport Chain. A Yeast Genetic Model System for the Study of Anionic Phospholipid Function in Mitochondria. J. Biol. Chem. 2001, 276, 25262–25272. [Google Scholar] [CrossRef]
- Yoshioka-Nishimura, M. Close Relationships Between the PSII Repair Cycle and Thylakoid Membrane Dynamics. Plant Cell Physiol. 2016, 57, 1115–1122. [Google Scholar] [CrossRef]
- Megiatto, J.D.; Antoniuk-Pablant, A.; Sherman, B.D.; Kodis, G.; Gervaldo, M.; Moore, T.A.; Moore, A.L.; Gust, D. Mimicking the Electron Transfer Chain in Photosystem II with a Molecular Triad Thermodynamically Capable of Water Oxidation. Proc. Natl. Acad. Sci. USA 2012, 109, 15578–15583. [Google Scholar] [CrossRef]
- Reiter, R.J.; Tan, D.-X.; Terron, M.P.; Flores, L.J.; Czarnocki, Z. Melatonin and Its Metabolites: New Findings Regarding Their Production and Their Radical Scavenging Actions. Acta Biochim. Pol. 2007, 54, 1–9. [Google Scholar] [CrossRef]
- Tan, D.X.; Manchester, L.C.; Reiter, R.J.; Plummer, B.F. Cyclic 3-Hydroxymelatonin: A Melatonin Metabolite Generated as a Result of Hydroxyl Radical Scavenging. Biol. Signals Recept. 1999, 8, 70–74. [Google Scholar] [CrossRef] [PubMed]
- De Almeida, E.A.; Martinez, G.R.; Klitzke, C.F.; de Medeiros, M.H.G.; Di Mascio, P. Oxidation of Melatonin by Singlet Molecular Oxygen (O2(1deltag)) Produces N1-Acetyl-N2-Formyl-5-Methoxykynurenine. J. Pineal. Res. 2003, 35, 131–137. [Google Scholar] [CrossRef] [PubMed]
- Matuszak, Z.; Bilska, M.A.; Reszka, K.J.; Chignell, C.F.; Bilski, P. Interaction of Singlet Molecular Oxygen with Melatonin and Related Indoles. Photochem. Photobiol. 2003, 78, 449–455. [Google Scholar] [CrossRef]
- Tan, D.X.; Manchester, L.C.; Reiter, R.J.; Plummer, B.F.; Limson, J.; Weintraub, S.T.; Qi, W. Melatonin Directly Scavenges Hydrogen Peroxide: A Potentially New Metabolic Pathway of Melatonin Biotransformation. Free Radic. Biol. Med. 2000, 29, 1177–1185. [Google Scholar] [CrossRef]
- Noda, Y.; Mori, A.; Liburdy, R.; Packer, L. Melatonin and Its Precursors Scavenge Nitric Oxide. J. Pineal. Res. 1999, 27, 159–163. [Google Scholar] [CrossRef]
- Aydogan, S.; Yerer, M.B.; Goktas, A. Melatonin and Nitric Oxide. J. Endocrinol. Investig. 2006, 29, 281–287. [Google Scholar] [CrossRef]
- Hardeland, R. Melatonin, Its Metabolites and Their Interference with Reactive Nitrogen Compounds. Molecules 2021, 26, 4105. [Google Scholar] [CrossRef] [PubMed]
- Gilad, E.; Cuzzocrea, S.; Zingarelli, B.; Salzman, A.L.; Szabó, C. Melatonin Is a Scavenger of Peroxynitrite. Life Sci. 1997, 60, PL169–PL174. [Google Scholar] [CrossRef]
- Galano, A.; Reiter, R.J. Melatonin and Its Metabolites vs. Oxidative Stress: From Individual Actions to Collective Protection. J. Pineal Res. 2018, 65, e12514. [Google Scholar] [CrossRef]
- Purushothaman, A.; Sheeja, A.A.; Janardanan, D. Hydroxyl Radical Scavenging Activity of Melatonin and Its Related Indolamines. Free Radic. Res. 2020, 54, 373–383. [Google Scholar] [CrossRef]
- Galano, A. On the Direct Scavenging Activity of Melatonin towards Hydroxyl and a Series of Peroxyl Radicals. Phys. Chem. Chem. Phys. 2011, 13, 7178–7188. [Google Scholar] [CrossRef]
- Galano, A.; Tan, D.X.; Reiter, R.J. Cyclic 3-Hydroxymelatonin, a Key Metabolite Enhancing the Peroxyl Radical Scavenging Activity of Melatonin. RSC Adv. 2014, 4, 5220. [Google Scholar] [CrossRef]
- Galano, A.; Medina, M.E.; Tan, D.X.; Reiter, R.J. Melatonin and Its Metabolites as Copper Chelating Agents and Their Role in Inhibiting Oxidative Stress: A Physicochemical Analysis. J. Pineal. Res. 2015, 58, 107–116. [Google Scholar] [CrossRef]
- Lúcio, M.; Nunes, C.; Gaspar, D.; Ferreira, H.; Lima, J.L.F.C.; Reis, S. Antioxidant Activity of Vitamin E and Trolox: Understanding of the Factors That Govern Lipid Peroxidation Studies In Vitro. Food Biophys. 2009, 4, 312–320. [Google Scholar] [CrossRef]
- Watson, H. Biological Membranes. Essays Biochem. 2015, 59, 43–69. [Google Scholar] [CrossRef]
- Zhang, J.; Yan, X.; Tian, Y.; Li, W.; Wang, H.; Li, Q.; Li, Y.; Li, Z.; Wu, T. Synthesis of a New Water-Soluble Melatonin Derivative with Low Toxicity and a Strong Effect on Sleep Aid. ACS Omega. 2020, 5, 6494–6499. [Google Scholar] [CrossRef]
- Shida, C.S.; Castrucci, A.M.; Lamy-Freund, M.T. High Melatonin Solubility in Aqueous Medium. J. Pineal. Res. 1994, 16, 198–201. [Google Scholar] [CrossRef]
- Aikens, J.; Dix, T.A. Perhydroxyl Radical (HOO.) Initiated Lipid Peroxidation. The Role of Fatty Acid Hydroperoxides. J. Biol. Chem. 1991, 266, 15091–15098. [Google Scholar] [CrossRef]
- Bielski, B.H.; Arudi, R.L.; Sutherland, M.W. A Study of the Reactivity of HO2/O2- with Unsaturated Fatty Acids. J. Biol. Chem. 1983, 258, 4759–4761. [Google Scholar] [CrossRef]
- Repetto, M.; Semprine, J.; Boveris, A. Lipid Peroxidation: Chemical Mechanism, Biological Implications and Analytical Determination. In Lipid Peroxidation; Catala, A., Ed.; IntechOpen: London, UK, 2012. [Google Scholar] [CrossRef]
- Ademowo, O.S.; Dias, H.K.I.; Burton, D.G.A.; Griffiths, H.R. Lipid (per) Oxidation in Mitochondria: An Emerging Target in the Ageing Process? Biogerontology 2017, 18, 859–879. [Google Scholar] [CrossRef] [PubMed]
- Niki, E. Lipid Peroxidation: Physiological Levels and Dual Biological Effects. Free Radic. Biol. Med. 2009, 47, 469–484. [Google Scholar] [CrossRef]
- Esterbauer, H.; Schaur, R.J.; Zollner, H. Chemistry and Biochemistry of 4-Hydroxynonenal, Malonaldehyde and Related Aldehydes. Free Radic. Biol. Med. 1991, 11, 81–128. [Google Scholar] [CrossRef]
- Kanner, J.; German, J.B.; Kinsella, J.E. Initiation of Lipid Peroxidation in Biological Systems. Crit. Rev. Food Sci. Nutr. 1987, 25, 317–364. [Google Scholar] [CrossRef] [PubMed]
- Southorn, P.A.; Powis, G. Free Radicals in Medicine. I. Chemical Nature and Biologic Reactions. Mayo Clin. Proc. 1988, 63, 381–389. [Google Scholar] [CrossRef]
- Yin, H.; Xu, L.; Porter, N.A. Free Radical Lipid Peroxidation: Mechanisms and Analysis. Chem. Rev. 2011, 111, 5944–5972. [Google Scholar] [CrossRef] [PubMed]
- Wientjes, F.B.; Segal, A.W. NADPH Oxidase and the Respiratory Burst. Semin. Cell Biol. 1995, 6, 357–365. [Google Scholar] [CrossRef]
- Bielski, B.H.J.; Cabelli, D.E.; Arudi, R.L.; Ross, A.B. Reactivity of HO2/O−2 Radicals in Aqueous Solution. J. Phys. Chem. Ref. Data 1985, 14, 1041–1100. [Google Scholar] [CrossRef]
- Wardman, P. Reduction Potentials of One-Electron Couples Involving Free Radicals in Aqueous Solution. J. Phys. Chem. Ref. Data 1989, 18, 1637–1755. [Google Scholar] [CrossRef]
- Hayyan, M.; Hashim, M.A.; AlNashef, I.M. Superoxide Ion: Generation and Chemical Implications. Chem. Rev. 2016, 116, 3029–3085. [Google Scholar] [CrossRef]
- Collin, F. Chemical Basis of Reactive Oxygen Species Reactivity and Involvement in Neurodegenerative Diseases. Int. J. Mol. Sci. 2019, 20, 2407. [Google Scholar] [CrossRef]
- Gebicki, J.M.; Bielski, B.H.J. Comparison of the Capacities of the Perhydroxyl and the Superoxide Radicals to Initiate Chain Oxidation of Linoleic Acid. J. Am. Chem. Soc. 1981, 103, 7020–7022. [Google Scholar] [CrossRef]
- De Grey, A.D.N.J. HO2*: The Forgotten Radical. DNA Cell Biol. 2002, 21, 251–257. [Google Scholar] [CrossRef] [PubMed]
- Halliwell, B.; Gutteridge, J.M. Oxygen Toxicity, Oxygen Radicals, Transition Metals and Disease. Biochem. J. 1984, 219, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Yusupov, M.; Wende, K.; Kupsch, S.; Neyts, E.C.; Reuter, S.; Bogaerts, A. Effect of Head Group and Lipid Tail Oxidation in the Cell Membrane Revealed through Integrated Simulations and Experiments. Sci. Rep. 2017, 7, 5761. [Google Scholar] [CrossRef]
- Sathappa, M.; Alder, N.N. The Ionization Properties of Cardiolipin and Its Variants in Model Bilayers. Biochim. Biophys. Acta 2016, 1858, 1362–1372. [Google Scholar] [CrossRef] [PubMed]
- Haines, T.H.; Dencher, N.A. Cardiolipin: A Proton Trap for Oxidative Phosphorylation. FEBS Lett. 2002, 528, 35–39. [Google Scholar] [CrossRef]
- Van den Brink-van der Laan, E.; Killian, J.A.; de Kruijff, B. Nonbilayer Lipids Affect Peripheral and Integral Membrane Proteins via Changes in the Lateral Pressure Profile. Biochim. Biophys. Acta 2004, 1666, 275–288. [Google Scholar] [CrossRef]
- Khalifat, N.; Puff, N.; Bonneau, S.; Fournier, J.-B.; Angelova, M.I. Membrane Deformation under Local pH Gradient: Mimicking Mitochondrial Cristae Dynamics. Biophys. J. 2008, 95, 4924–4933. [Google Scholar] [CrossRef]
- Parui, P.P.; Sarakar, Y.; Majumder, R.; Das, S.; Yang, H.; Yasuhara, K.; Hirota, S. Determination of Proton Concentration at Cardiolipin-Containing Membrane Interfaces and Its Relation with the Peroxidase Activity of Cytochrome c. Chem. Sci. 2019, 10, 9140–9151. [Google Scholar] [CrossRef]
- Porcelli, A.M.; Ghelli, A.; Zanna, C.; Pinton, P.; Rizzuto, R.; Rugolo, M. pH Difference across the Outer Mitochondrial Membrane Measured with a Green Fluorescent Protein Mutant. Biochem. Biophys. Res. Commun. 2005, 326, 799–804. [Google Scholar] [CrossRef]
- Paradies, G.; Ruggiero, F.M.; Petrosillo, G.; Quagliariello, E. Age-Dependent Decline in the Cytochrome c Oxidase Activity in Rat Heart Mitochondria: Role of Cardiolipin. FEBS Lett. 1997, 406, 136–138. [Google Scholar] [CrossRef]
- Paradies, G.; Ruggiero, F.M.; Petrosillo, G.; Quagliariello, E. Peroxidative Damage to Cardiac Mitochondria: Cytochrome Oxidase and Cardiolipin Alterations. FEBS Lett. 1998, 424, 155–158. [Google Scholar] [CrossRef]
- Paradies, G.; Petrosillo, G.; Pistolese, M.; Ruggiero, F.M. Reactive Oxygen Species Generated by the Mitochondrial Respiratory Chain Affect the Complex III Activity via Cardiolipin Peroxidation in Beef-Heart Submitochondrial Particles. Mitochondrion 2001, 1, 151–159. [Google Scholar] [CrossRef]
- Petrosillo, G.; Ruggiero, F.M.; Pistolese, M.; Paradies, G. Reactive Oxygen Species Generated from the Mitochondrial Electron Transport Chain Induce Cytochrome c Dissociation from Beef-Heart Submitochondrial Particles via Cardiolipin Peroxidation. Possible Role in the Apoptosis. FEBS Lett. 2001, 509, 435–438. [Google Scholar] [CrossRef]
- Paradies, G.; Petrosillo, G.; Pistolese, M.; Ruggiero, F.M. Reactive Oxygen Species Affect Mitochondrial Electron Transport Complex I Activity through Oxidative Cardiolipin Damage. Gene 2002, 286, 135–141. [Google Scholar] [CrossRef]
- Paradies, G.; Petrosillo, G.; Pistolese, M.; Di Venosa, N.; Federici, A.; Ruggiero, F.M. Decrease in Mitochondrial Complex I Activity in Ischemic/reperfused Rat Heart: Involvement of Reactive Oxygen Species and Cardiolipin. Circ. Res. 2004, 94, 53–59. [Google Scholar] [CrossRef] [PubMed]
- Paradies, G.; Petrosillo, G.; Paradies, V.; Ruggiero, F.M. Role of Cardiolipin Peroxidation and Ca2+ in Mitochondrial Dysfunction and Disease. Cell Calcium. 2009, 45, 643–650. [Google Scholar] [CrossRef] [PubMed]
- Arnarez, C.; Mazat, J.-P.; Elezgaray, J.; Marrink, S.-J.; Periole, X. Evidence for Cardiolipin Binding Sites on the Membrane-Exposed Surface of the Cytochrome bc1. J. Am. Chem. Soc. 2013, 135, 3112–3120. [Google Scholar] [CrossRef]
- Panov, A. Perhydroxyl Radical (HO2•) as Inducer of the Isoprostane Lipid Peroxidation in Mitochondria. Mol. Biol. 2018, 52, 295–305. [Google Scholar] [CrossRef]
- Miranda, É.G.A.; Araujo-Chaves, J.C.; Kawai, C.; Brito, A.M.M.; Dias, I.W.R.; Arantes, J.T.; Nantes-Cardoso, I.L. Cardiolipin Structure and Oxidation Are Affected by Ca2+ at the Interface of Lipid Bilayers. Front. Chem. 2019, 7, 930. [Google Scholar] [CrossRef] [PubMed]
- Cipolla-Neto, J.; Amaral, F.G.; Afeche, S.C.; Tan, D.X.; Reiter, R.J. Melatonin, Energy Metabolism, and Obesity: A Review. J. Pineal. Res. 2014, 56, 371–381. [Google Scholar] [CrossRef]
- Sustarsic, E.G.; Ma, T.; Lynes, M.D.; Larsen, M.; Karavaeva, I.; Havelund, J.F.; Nielsen, C.H.; Jedrychowski, M.P.; Moreno-Torres, M.; Lundh, M.; et al. Cardiolipin Synthesis in Brown and Beige Fat Mitochondria Is Essential for Systemic Energy Homeostasis. Cell Metab. 2018, 28, 159–174.e11. [Google Scholar] [CrossRef]
- Von Bank, H.; Hurtado-Thiele, M.; Oshimura, N.; Simcox, J. Mitochondrial Lipid Signaling and Adaptive Thermogenesis. Metabolites 2021, 11, 124. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.; Willers, C.; Kunji, E.R.S.; Crichton, P.G. Uncoupling Protein 1 Binds One Nucleotide per Monomer and Is Stabilized by Tightly Bound Cardiolipin. Proc. Natl. Acad. Sci. USA 2015, 112, 6973–6978. [Google Scholar] [CrossRef]
- Fernández Vázquez, G.; Reiter, R.J.; Agil, A. Melatonin Increases Brown Adipose Tissue Mass and Function in Zücker Diabetic Fatty Rats: Implications for Obesity Control. J. Pineal. Res. 2018, 64, e12472. [Google Scholar] [CrossRef] [PubMed]
- Martín, M.; Macías, M.; León, J.; Escames, G.; Khaldy, H.; Acuña-Castroviejo, D. Melatonin Increases the Activity of the Oxidative Phosphorylation Enzymes and the Production of ATP in Rat Brain and Liver Mitochondria. Int. J. Biochem. Cell Biol. 2002, 34, 348–357. [Google Scholar] [CrossRef]
- Chen, X.; Hao, B.; Li, D.; Reiter, R.J.; Bai, Y.; Abay, B.; Chen, G.; Lin, S.; Zheng, T.; Ren, Y.; et al. Melatonin Inhibits Lung Cancer Development by Reversing the Warburg Effect via Stimulating the SIRT3/PDH Axis. J. Pineal. Res. 2021, e12755. [Google Scholar] [CrossRef]
- Reiter, R.J.; Sharma, R.; Rosales-Corral, S. Anti-Warburg Effect of Melatonin: A Proposed Mechanism to Explain Its Inhibition of Multiple Diseases. Int. J. Mol. Sci. 2021, 22, 764. [Google Scholar] [CrossRef] [PubMed]
- Reiter, R.J.; Sharma, R.; Ma, Q.; Rorsales-Corral, S.; de Almeida Chuffa, L.G. Melatonin Inhibits Warburg-Dependent Cancer by Redirecting Glucose Oxidation to the Mitochondria: A Mechanistic Hypothesis. Cell. Mol. Life Sci. 2020, 77, 2527–2542. [Google Scholar] [CrossRef]
- Reiter, R.J.; Sharma, R.; Pires de Campos Zuccari, D.A.; de Almeida Chuffa, L.G.; Manucha, W.; Rodriguez, C. Melatonin Synthesis in and Uptake by Mitochondria: Implications for Diseased Cells with Dysfunctional Mitochondria. Future Med. Chem. 2021, 13, 335–339. [Google Scholar] [CrossRef]
- Xia, Y.; Chen, S.; Zeng, S.; Zhao, Y.; Zhu, C.; Deng, B.; Zhu, G.; Yin, Y.; Wang, W.; Hardeland, R.; et al. Melatonin in Macrophage Biology: Current Understanding and Future Perspectives. J. Pineal. Res. 2019, 66, e12547. [Google Scholar] [CrossRef]
- Reiter, R.J.; Sharma, R.; Ma, Q. Switching Diseased Cells from Cytosolic Aerobic Glycolysis to Mitochondrial Oxidative Phosphorylation: A Metabolic Rhythm Regulated by Melatonin? J. Pineal. Res. 2021, 70, e12677. [Google Scholar] [CrossRef]
- Fuller, G.G.; Han, T.; Freeberg, M.A.; Moresco, J.J.; Ghanbari Niaki, A.; Roach, N.P.; Yates, J.R.; Myong, S.; Kim, J.K. RNA Promotes Phase Separation of Glycolysis Enzymes into Yeast G Bodies in Hypoxia. Elife 2020, 9, e48480. [Google Scholar] [CrossRef]
- Jin, M.; Fuller, G.G.; Han, T.; Yao, Y.; Alessi, A.F.; Freeberg, M.A.; Roach, N.P.; Moresco, J.J.; Karnovsky, A.; Baba, M.; et al. Glycolytic Enzymes Coalesce in G Bodies under Hypoxic Stress. Cell Rep. 2017, 20, 895–908. [Google Scholar] [CrossRef] [PubMed]
- Sarkar, S.; Mondal, J. Mechanistic Insights on ATP’s Role as a Hydrotrope. J. Phys. Chem. B 2021, 125, 7717–7731. [Google Scholar] [CrossRef] [PubMed]
- Maldonado, E.N.; Lemasters, J.J. ATP/ADP Ratio, the Missed Connection between Mitochondria and the Warburg Effect. Mitochondrion 2014, 19 Pt A, 78–84. [Google Scholar] [CrossRef]
- Bell, S.M.; Burgess, T.; Lee, J.; Blackburn, D.J.; Allen, S.P.; Mortiboys, H. Peripheral Glycolysis in Neurodegenerative Diseases. Int. J. Mol. Sci. 2020, 21, 8924. [Google Scholar] [CrossRef]
- Lu, J.; Qian, J.; Xu, Z.; Yin, S.; Zhou, L.; Zheng, S.; Zhang, W. Emerging Roles of Liquid-Liquid Phase Separation in Cancer: From Protein Aggregation to Immune-Associated Signaling. Front. Cell Dev. Biol. 2021, 9, 631486. [Google Scholar] [CrossRef] [PubMed]
- Petronilho, E.C.; Pedrote, M.M.; Marques, M.A.; Passos, Y.M.; Mota, M.F.; Jakobus, B.; de Sousa, G.D.S.; Pereira da Costa, F.; Felix, A.L.; Ferretti, G.D.S.; et al. Phase Separation of p53 Precedes Aggregation and Is Affected by Oncogenic Mutations and Ligands. Chem. Sci. 2021, 12, 7334–7349. [Google Scholar] [CrossRef] [PubMed]
- Gargini, R.; Segura-Collar, B.; Sánchez-Gómez, P. Novel Functions of the Neurodegenerative-Related Gene Tau in Cancer. Front. Aging Neurosci. 2019, 11, 231. [Google Scholar] [CrossRef]
- Sullivan, K.D.; Galbraith, M.D.; Andrysik, Z.; Espinosa, J.M. Mechanisms of Transcriptional Regulation by p53. Cell Death Differ. 2018, 25, 133–143. [Google Scholar] [CrossRef]
- Maina, M.B.; Bailey, L.J.; Wagih, S.; Biasetti, L.; Pollack, S.J.; Quinn, J.P.; Thorpe, J.R.; Doherty, A.J.; Serpell, L.C. The Involvement of Tau in Nucleolar Transcription and the Stress Response. Acta Neuropathol. Commun. 2018, 6, 70. [Google Scholar] [CrossRef] [PubMed]
- Reddi, P.P. Transcription and Splicing Factor TDP-43: Role in Regulation of Gene Expression in Testis. Semin. Reprod. Med. 2017, 35, 167–172. [Google Scholar] [CrossRef]
- Morera, A.A.; Ahmed, N.S.; Schwartz, J.C. TDP-43 Regulates Transcription at Protein-Coding Genes and Alu Retrotransposons. Biochim. Biophys. Acta Gene Regul. Mech. 2019, 1862, 194434. [Google Scholar] [CrossRef]
- Yang, L.; Gal, J.; Chen, J.; Zhu, H. Self-Assembled FUS Binds Active Chromatin and Regulates Gene Transcription. Proc. Natl. Acad. Sci. USA 2014, 111, 17809–17814. [Google Scholar] [CrossRef] [PubMed]
- Cramer, P. Organization and Regulation of Gene Transcription. Nature 2019, 573, 45–54. [Google Scholar] [CrossRef]
- Henninger, J.E.; Oksuz, O.; Shrinivas, K.; Sagi, I.; LeRoy, G.; Zheng, M.M.; Andrews, J.O.; Zamudio, A.V.; Lazaris, C.; Hannett, N.M.; et al. RNA-Mediated Feedback Control of Transcriptional Condensates. Cell 2021, 184, 207–225.e24. [Google Scholar] [CrossRef] [PubMed]
- Das, R.K.; Pappu, R.V. Conformations of Intrinsically Disordered Proteins Are Influenced by Linear Sequence Distributions of Oppositely Charged Residues. Proc. Natl. Acad. Sci. USA 2013, 110, 13392–13397. [Google Scholar] [CrossRef] [PubMed]
- Guo, Q.; Shi, X.; Wang, X. RNA and Liquid-Liquid Phase Separation. Noncoding RNA Res. 2021, 6, 92–99. [Google Scholar] [CrossRef]
- Fay, M.M.; Anderson, P.J. The Role of RNA in Biological Phase Separations. J. Mol. Biol. 2018, 430, 4685–4701. [Google Scholar] [CrossRef] [PubMed]
- Roden, C.; Gladfelter, A.S. RNA Contributions to the Form and Function of Biomolecular Condensates. Nat. Rev. Mol. Cell Biol. 2021, 22, 183–195. [Google Scholar] [CrossRef] [PubMed]
- Conn, G.L.; Gittis, A.G.; Lattman, E.E.; Misra, V.K.; Draper, D.E. A Compact RNA Tertiary Structure Contains a Buried Backbone-K+ Complex. J. Mol. Biol. 2002, 318, 963–973. [Google Scholar] [CrossRef]
- Drobot, B.; Iglesias-Artola, J.M.; Le Vay, K.; Mayr, V.; Kar, M.; Kreysing, M.; Mutschler, H.; Tang, T.-Y.D. Compartmentalised RNA Catalysis in Membrane-Free Coacervate Protocells. Nat. Commun. 2018, 9, 3643. [Google Scholar] [CrossRef] [PubMed]
- Frankel, E.A.; Bevilacqua, P.C.; Keating, C.D. Polyamine/Nucleotide Coacervates Provide Strong Compartmentalization of Mg2+, Nucleotides, and RNA. Langmuir 2016, 32, 2041–2049. [Google Scholar] [CrossRef]
- Kirschbaum, J.; Zwicker, D. Controlling Biomolecular Condensates via Chemical Reactions. arXiv 2021, arXiv:2103.02921. [Google Scholar]
- Bah, A.; Forman-Kay, J.D. Modulation of Intrinsically Disordered Protein Function by Post-Translational Modifications. J. Biol. Chem. 2016, 291, 6696–6705. [Google Scholar] [CrossRef] [PubMed]
- Söding, J.; Zwicker, D.; Sohrabi-Jahromi, S.; Boehning, M.; Kirschbaum, J. Mechanisms for Active Regulation of Biomolecular Condensates. Trends Cell Biol. 2020, 30, 4–14. [Google Scholar] [CrossRef]
- Brangwynne, C.P.; Tompa, P.; Pappu, R.V. Polymer Physics of Intracellular Phase Transitions. Nat. Phys. 2015, 11, 899–904. [Google Scholar] [CrossRef]
- Schisa, J.A.; Elaswad, M.T. An Emerging Role for Post-Translational Modifications in Regulating RNP Condensates in the Germ Line. Frontiers in Molecular Biosciences 2021, 8, 230. [Google Scholar] [CrossRef]
- Hofweber, M.; Dormann, D. Friend or Foe-Post-Translational Modifications as Regulators of Phase Separation and RNP Granule Dynamics. J. Biol. Chem. 2019, 294, 7137–7150. [Google Scholar] [CrossRef] [PubMed]
- Arimoto, K.; Fukuda, H.; Imajoh-Ohmi, S.; Saito, H.; Takekawa, M. Formation of Stress Granules Inhibits Apoptosis by Suppressing Stress-Responsive MAPK Pathways. Nat. Cell Biol. 2008, 10, 1324–1332. [Google Scholar] [CrossRef] [PubMed]
- Advani, V.M.; Ivanov, P. Stress Granule Subtypes: An Emerging Link to Neurodegeneration. Cell. Mol. Life Sci. 2020, 77, 4827–4845. [Google Scholar] [CrossRef]
- Buchan, J.R.; Parker, R. Eukaryotic Stress Granules: The Ins and Outs of Translation. Mol. Cell 2009, 36, 932–941. [Google Scholar] [CrossRef]
- Van Treeck, B.; Protter, D.S.W.; Matheny, T.; Khong, A.; Link, C.D.; Parker, R. RNA Self-Assembly Contributes to Stress Granule Formation and Defining the Stress Granule Transcriptome. Proc. Natl. Acad. Sci. USA 2018, 115, 2734–2739. [Google Scholar] [CrossRef]
- Gaete-Argel, A.; Velásquez, F.; Márquez, C.L.; Rojas-Araya, B.; Bueno-Nieto, C.; Marín-Rojas, J.; Cuevas-Zúñiga, M.; Soto-Rifo, R.; Valiente-Echeverría, F. Tellurite Promotes Stress Granules and Nuclear SG-Like Assembly in Response to Oxidative Stress and DNA Damage. Front. Cell Dev. Biol. 2021, 9, 622057. [Google Scholar] [CrossRef]
- Lian, X.J.; Gallouzi, I.-E. Oxidative Stress Increases the Number of Stress Granules in Senescent Cells and Triggers a Rapid Decrease in p21waf1/cip1 Translation. J. Biol. Chem. 2009, 284, 8877–8887. [Google Scholar] [CrossRef]
- Curdy, N.; Lanvin, O.; Cadot, S.; Laurent, C.; Fournié, J.-J.; Franchini, D.-M. Stress Granules in the Post-Transcriptional Regulation of Immune Cells. Front. Cell Dev. Biol. 2020, 8, 611185. [Google Scholar] [CrossRef] [PubMed]
- Uversky, V.N. Intrinsically Disordered Proteins in Overcrowded Milieu: Membrane-Less Organelles, Phase Separation, and Intrinsic Disorder. Curr. Opin. Struct. Biol. 2017, 44, 18–30. [Google Scholar] [CrossRef]
- Wells, M.; Tidow, H.; Rutherford, T.J.; Markwick, P.; Jensen, M.R.; Mylonas, E.; Svergun, D.I.; Blackledge, M.; Fersht, A.R. Structure of Tumor Suppressor p53 and Its Intrinsically Disordered N-Terminal Transactivation Domain. Proc. Natl. Acad. Sci. USA 2008, 105, 5762–5767. [Google Scholar] [CrossRef]
- Gilks, N.; Kedersha, N.; Ayodele, M.; Shen, L.; Stoecklin, G.; Dember, L.M.; Anderson, P. Stress Granule Assembly Is Mediated by Prion-like Aggregation of TIA-1. Mol. Biol. Cell 2004, 15, 5383–5398. [Google Scholar] [CrossRef]
- Ryan, V.H.; Fawzi, N.L. Physiological, Pathological, and Targetable Membraneless Organelles in Neurons. Trends Neurosci. 2019, 42, 693–708. [Google Scholar] [CrossRef]
- Ash, P.E.A.; Vanderweyde, T.E.; Youmans, K.L.; Apicco, D.J.; Wolozin, B. Pathological Stress Granules in Alzheimer’s Disease. Brain Res. 2014, 1584, 52–58. [Google Scholar] [CrossRef]
- Elbaum-Garfinkle, S. Matter over Mind: Liquid Phase Separation and Neurodegeneration. J. Biol. Chem. 2019, 294, 7160–7168. [Google Scholar] [CrossRef]
- Santofimia-Castaño, P.; Rizzuti, B.; Xia, Y.; Abian, O.; Peng, L.; Velázquez-Campoy, A.; Neira, J.L.; Iovanna, J. Targeting Intrinsically Disordered Proteins Involved in Cancer. Cell. Mol. Life Sci. 2020, 77, 1695–1707. [Google Scholar] [CrossRef]
- Wolozin, B. Regulated Protein Aggregation: Stress Granules and Neurodegeneration. Mol. Neurodegener. 2012, 7, 56. [Google Scholar] [CrossRef] [PubMed]
- Xue, B.; Brown, C.J.; Dunker, A.K.; Uversky, V.N. Intrinsically Disordered Regions of p53 Family Are Highly Diversified in Evolution. Biochim. Biophys. Acta 2013, 1834, 725–738. [Google Scholar] [CrossRef]
- Ash, P.E.A.; Lei, S.; Shattuck, J.; Boudeau, S.; Carlomagno, Y.; Medalla, M.; Mashimo, B.L.; Socorro, G.; Al-Mohanna, L.F.A.; Jiang, L.; et al. TIA1 Potentiates Tau Phase Separation and Promotes Generation of Toxic Oligomeric Tau. Proc. Natl. Acad. Sci. USA 2021, 118, e2014188118. [Google Scholar] [CrossRef]
- Asakawa, K.; Handa, H.; Kawakami, K. Optogenetic Modulation of TDP-43 Oligomerization Accelerates ALS-Related Pathologies in the Spinal Motor Neurons. Nat. Commun. 2020, 11, 1004. [Google Scholar] [CrossRef]
- Lin, Y.; Currie, S.L.; Rosen, M.K. Intrinsically Disordered Sequences Enable Modulation of Protein Phase Separation through Distributed Tyrosine Motifs. J. Biol. Chem. 2017, 292, 19110–19120. [Google Scholar] [CrossRef]
- Jeon, P.; Lee, J.A. Dr. Jekyll and Mr. Hyde? Physiology and Pathology of Neuronal Stress Granules. Front Cell Dev. Biol. 2021, 9, 609698. [Google Scholar] [CrossRef] [PubMed]
- Farny, N.G.; Kedersha, N.L.; Silver, P.A. Metazoan Stress Granule Assembly Is Mediated by P-eIF2alpha-Dependent and -Independent Mechanisms. RNA 2009, 15, 1814–1821. [Google Scholar] [CrossRef] [PubMed]
- Vanderweyde, T.; Yu, H.; Varnum, M.; Liu-Yesucevitz, L.; Citro, A.; Ikezu, T.; Duff, K.; Wolozin, B. Contrasting Pathology of the Stress Granule Proteins TIA-1 and G3BP in Tauopathies. J. Neurosci. 2012, 32, 8270–8283. [Google Scholar] [CrossRef]
- Jenkins, S.M.; Zinnerman, M.; Garner, C.; Johnson, G.V. Modulation of Tau Phosphorylation and Intracellular Localization by Cellular Stress. Biochem. J. 2000, 345 Pt 2, 263–270. [Google Scholar] [CrossRef]
- Cruz, A.; Verma, M.; Wolozin, B. The Pathophysiology of Tau and Stress Granules in Disease. In Tau Biology; Takashima, A., Wolozin, B., Buee, L., Eds.; Springer: Singapore, 2019; pp. 359–372. [Google Scholar] [CrossRef]
- Dobra, I.; Pankivskyi, S.; Samsonova, A.; Pastre, D.; Hamon, L. Relation Between Stress Granules and Cytoplasmic Protein Aggregates Linked to Neurodegenerative Diseases. Curr. Neurol. Neurosci. Rep. 2018, 18, 107. [Google Scholar] [CrossRef]
- Yoshida, Y.; Izumi, H.; Torigoe, T.; Ishiguchi, H.; Yoshida, T.; Itoh, H.; Kohno, K. Binding of RNA to p53 Regulates Its Oligomerization and DNA-Binding Activity. Oncogene 2004, 23, 4371–4379. [Google Scholar] [CrossRef]
- Maharana, S.; Wang, J.; Papadopoulos, D.K.; Richter, D.; Pozniakovsky, A.; Poser, I.; Bickle, M.; Rizk, S.; Guillén-Boixet, J.; Franzmann, T.M.; et al. RNA Buffers the Phase Separation Behavior of Prion-like RNA Binding Proteins. Science 2018, 360, 918–921. [Google Scholar] [CrossRef] [PubMed]
- Burke, K.A.; Janke, A.M.; Rhine, C.L.; Fawzi, N.L. Residue-by-Residue View of In Vitro FUS Granules That Bind the C-Terminal Domain of RNA Polymerase II. Mol. Cell 2015, 60, 231–241. [Google Scholar] [CrossRef]
- Kovachev, P.S.; Banerjee, D.; Rangel, L.P.; Eriksson, J.; Pedrote, M.M.; Martins-Dinis, M.M.D.C.; Edwards, K.; Cordeiro, Y.; Silva, J.L.; Sanyal, S. Distinct Modulatory Role of RNA in the Aggregation of the Tumor Suppressor Protein p53 Core Domain. J. Biol. Chem. 2017, 292, 9345–9357. [Google Scholar] [CrossRef] [PubMed]
- Safari, M.S.; Wang, Z.; Tailor, K.; Kolomeisky, A.B.; Conrad, J.C.; Vekilov, P.G. Anomalous Dense Liquid Condensates Host the Nucleation of Tumor Suppressor p53 Fibrils. Science 2019, 12, 342–355. [Google Scholar] [CrossRef]
- Gasset-Rosa, F.; Lu, S.; Yu, H.; Chen, C.; Melamed, Z.; Guo, L.; Shorter, J.; Da Cruz, S.; Cleveland, D.W. Cytoplasmic TDP-43 De-Mixing Independent of Stress Granules Drives Inhibition of Nuclear Import, Loss of Nuclear TDP-43, and Cell Death. Neuron 2019, 102, 339–357.e7. [Google Scholar] [CrossRef]
- Ding, Q.; Chaplin, J.; Morris, M.J.; Hilliard, M.A.; Wolvetang, E.; Ng, D.C.H.; Noakes, P.G. TDP-43 Mutation Affects Stress Granule Dynamics in Differentiated NSC-34 Motoneuron-Like Cells. Front. Cell Dev. Biol. 2021, 9, 611601. [Google Scholar] [CrossRef]
- Aulas, A.; Vande Velde, C. Alterations in Stress Granule Dynamics Driven by TDP-43 and FUS: A Link to Pathological Inclusions in ALS? Front. Cell Neurosci. 2015, 9, 423. [Google Scholar] [CrossRef] [PubMed]
- Baron, D.M.; Kaushansky, L.J.; Ward, C.L.; Sama, R.R.K.; Chian, R.-J.; Boggio, K.J.; Quaresma, A.J.C.; Nickerson, J.A.; Bosco, D.A. Amyotrophic Lateral Sclerosis-Linked FUS/TLS Alters Stress Granule Assembly and Dynamics. Mol. Neurodegener. 2013, 8, 30. [Google Scholar] [CrossRef] [PubMed]
- Lenzi, J.; De Santis, R.; de Turris, V.; Morlando, M.; Laneve, P.; Calvo, A.; Caliendo, V.; Chiò, A.; Rosa, A.; Bozzoni, I. ALS Mutant FUS Proteins Are Recruited into Stress Granules in Induced Pluripotent Stem Cell-Derived Motoneurons. Dis. Model. Mech. 2015, 8, 755–766. [Google Scholar] [CrossRef] [PubMed]
- Khalfallah, Y.; Kuta, R.; Grasmuck, C.; Prat, A.; Durham, H.D.; Vande Velde, C. TDP-43 Regulation of Stress Granule Dynamics in Neurodegenerative Disease-Relevant Cell Types. Sci. Rep. 2018, 8, 7551. [Google Scholar] [CrossRef]
- Liu-Yesucevitz, L.; Bilgutay, A.; Zhang, Y.-J.; Vanderweyde, T.; Citro, A.; Mehta, T.; Zaarur, N.; McKee, A.; Bowser, R.; Sherman, M.; et al. Tar DNA Binding Protein-43 (TDP-43) Associates with Stress Granules: Analysis of Cultured Cells and Pathological Brain Tissue. PLoS ONE 2010, 5, e13250. [Google Scholar] [CrossRef] [PubMed]
- Stefl, S.; Nishi, H.; Petukh, M.; Panchenko, A.R.; Alexov, E. Molecular Mechanisms of Disease-Causing Missense Mutations. J. Mol. Biol. 2013, 425, 3919–3936. [Google Scholar] [CrossRef] [PubMed]
- Kolonko-Adamska, M.; Uversky, V.N.; Greb-Markiewicz, B. The Participation of the Intrinsically Disordered Regions of the bHLH-PAS Transcription Factors in Disease Development. Int. J. Mol. Sci. 2021, 22, 2868. [Google Scholar] [CrossRef] [PubMed]
- Portz, B.; Lee, B.L.; Shorter, J. FUS and TDP-43 Phases in Health and Disease. Trends Biochem. Sci. 2021, 46, 550–563. [Google Scholar] [CrossRef]
- Tsang, B.; Pritišanac, I.; Scherer, S.W.; Moses, A.M.; Forman-Kay, J.D. Phase Separation as a Missing Mechanism for Interpretation of Disease Mutations. Cell 2020, 183, 1742–1756. [Google Scholar] [CrossRef] [PubMed]
- Monahan, Z.; Ryan, V.H.; Janke, A.M.; Burke, K.A.; Rhoads, S.N.; Zerze, G.H.; O’Meally, R.; Dignon, G.L.; Conicella, A.E.; Zheng, W.; et al. Phosphorylation of the FUS Low-Complexity Domain Disrupts Phase Separation, Aggregation, and Toxicity. EMBO J. 2017, 36, 2951–2967. [Google Scholar] [CrossRef]
- Molliex, A.; Temirov, J.; Lee, J.; Coughlin, M.; Kanagaraj, A.P.; Kim, H.J.; Mittag, T.; Taylor, J.P. Phase Separation by Low Complexity Domains Promotes Stress Granule Assembly and Drives Pathological Fibrillization. Cell 2015, 163, 123–133. [Google Scholar] [CrossRef]
- Murakami, T.; Qamar, S.; Lin, J.Q.; Schierle, G.S.K.; Rees, E.; Miyashita, A.; Costa, A.R.; Dodd, R.B.; Chan, F.T.S.; Michel, C.H.; et al. ALS/FTD Mutation-Induced Phase Transition of FUS Liquid Droplets and Reversible Hydrogels into Irreversible Hydrogels Impairs RNP Granule Function. Neuron 2015, 88, 678–690. [Google Scholar] [CrossRef] [PubMed]
- Gopal, P.P.; Nirschl, J.J.; Klinman, E.; Holzbaur, E.L.F. Amyotrophic Lateral Sclerosis-Linked Mutations Increase the Viscosity of Liquid-like TDP-43 RNP Granules in Neurons. Proc. Natl. Acad. Sci. USA 2017, 114, E2466–E2475. [Google Scholar] [CrossRef]
- Hofweber, M.; Hutten, S.; Bourgeois, B.; Spreitzer, E.; Niedner-Boblenz, A.; Schifferer, M.; Ruepp, M.-D.; Simons, M.; Niessing, D.; Madl, T.; et al. Phase Separation of FUS Is Suppressed by Its Nuclear Import Receptor and Arginine Methylation. Cell 2018, 173, 706–719.e13. [Google Scholar] [CrossRef]
- Neumann, M.; Sampathu, D.M.; Kwong, L.K.; Truax, A.C.; Micsenyi, M.C.; Chou, T.T.; Bruce, J.; Schuck, T.; Grossman, M.; Clark, C.M.; et al. Ubiquitinated TDP-43 in Frontotemporal Lobar Degeneration and Amyotrophic Lateral Sclerosis. Science 2006, 314, 130–133. [Google Scholar] [CrossRef] [PubMed]
- King, O.D.; Gitler, A.D.; Shorter, J. The Tip of the Iceberg: RNA-Binding Proteins with Prion-like Domains in Neurodegenerative Disease. Brain Res. 2012, 1462, 61–80. [Google Scholar] [CrossRef]
- Lim, L.; Wei, Y.; Lu, Y.; Song, J. ALS-Causing Mutations Significantly Perturb the Self-Assembly and Interaction with Nucleic Acid of the Intrinsically Disordered Prion-Like Domain of TDP-43. PLoS Biol. 2016, 14, e1002338. [Google Scholar] [CrossRef]
- Taylor, J.P.; Brown, R.H.; Cleveland, D.W. Decoding ALS: From Genes to Mechanism. Nature 2016, 539, 197–206. [Google Scholar] [CrossRef]
- Johnson, B.S.; Snead, D.; Lee, J.J.; McCaffery, J.M.; Shorter, J.; Gitler, A.D. TDP-43 Is Intrinsically Aggregation-Prone, and Amyotrophic Lateral Sclerosis-Linked Mutations Accelerate Aggregation and Increase Toxicity. J. Biol. Chem. 2009, 284, 20329–20339. [Google Scholar] [CrossRef] [PubMed]
- Conicella, A.E.; Dignon, G.L.; Zerze, G.H.; Schmidt, H.B.; D’Ordine, A.M.; Kim, Y.C.; Rohatgi, R.; Ayala, Y.M.; Mittal, J.; Fawzi, N.L. TDP-43 α-Helical Structure Tunes Liquid-Liquid Phase Separation and Function. Proc. Natl. Acad. Sci. USA 2020, 117, 5883–5894. [Google Scholar] [CrossRef] [PubMed]
- Jiang, L.-L.; Zhao, J.; Yin, X.-F.; He, W.-T.; Yang, H.; Che, M.-X.; Hu, H.-Y. Two Mutations G335D and Q343R within the Amyloidogenic Core Region of TDP-43 Influence Its Aggregation and Inclusion Formation. Sci. Rep. 2016, 6, 23928. [Google Scholar] [CrossRef]
- Conicella, A.E.; Zerze, G.H.; Mittal, J.; Fawzi, N.L. ALS Mutations Disrupt Phase Separation Mediated by α-Helical Structure in the TDP-43 Low-Complexity C-Terminal Domain. Structure 2016, 24, 1537–1549. [Google Scholar] [CrossRef]
- Pesiridis, G.S.; Lee, V.M.-Y.; Trojanowski, J.Q. Mutations in TDP-43 Link Glycine-Rich Domain Functions to Amyotrophic Lateral Sclerosis. Hum. Mol. Genet. 2009, 18, R156–R162. [Google Scholar] [CrossRef]
- Genc, S.; Kurnaz, I.A.; Ozilgen, M. Astrocyte-Neuron Lactate Shuttle May Boost More ATP Supply to the Neuron under Hypoxic Conditions--in Silico Study Supported by in Vitro Expression Data. BMC Syst. Biol. 2011, 5, 162. [Google Scholar] [CrossRef] [PubMed]
- Smethurst, P.; Risse, E.; Tyzack, G.E.; Mitchell, J.S.; Taha, D.M.; Chen, Y.-R.; Newcombe, J.; Collinge, J.; Sidle, K.; Patani, R. Distinct Responses of Neurons and Astrocytes to TDP-43 Proteinopathy in Amyotrophic Lateral Sclerosis. Brain 2020, 143, 430–440. [Google Scholar] [CrossRef]
- Fallini, C.; Bassell, G.J.; Rossoll, W. The ALS Disease Protein TDP-43 Is Actively Transported in Motor Neuron Axons and Regulates Axon Outgrowth. Hum. Mol. Genet. 2012, 21, 3703–3718. [Google Scholar] [CrossRef]
- Dang, M.; Kang, J.; Lim, L.; Li, Y.; Wang, L.; Song, J. ATP Is a Cryptic Binder of TDP-43 RRM Domains to Enhance Stability and Inhibit ALS/AD-Associated Fibrillation. Biochem. Biophys. Res. Commun. 2020, 522, 247–253. [Google Scholar] [CrossRef] [PubMed]
- Corrado, L.; Del Bo, R.; Castellotti, B.; Ratti, A.; Cereda, C.; Penco, S.; Sorarù, G.; Carlomagno, Y.; Ghezzi, S.; Pensato, V.; et al. Mutations of FUS Gene in Sporadic Amyotrophic Lateral Sclerosis. J. Med. Genet. 2010, 47, 190–194. [Google Scholar] [CrossRef]
- Ticozzi, N.; Silani, V.; LeClerc, A.L.; Keagle, P.; Gellera, C.; Ratti, A.; Taroni, F.; Kwiatkowski, T.J.; McKenna-Yasek, D.M.; Sapp, P.C.; et al. Analysis of FUS Gene Mutation in Familial Amyotrophic Lateral Sclerosis within an Italian Cohort. Neurology 2009, 73, 1180–1185. [Google Scholar] [CrossRef]
- Sama, R.R.K.; Ward, C.L.; Bosco, D.A. Functions of FUS/TLS from DNA Repair to Stress Response: Implications for ALS. ASN Neuro 2014, 6, 1759091414544472. [Google Scholar] [CrossRef]
- Jiang, X.; Zhang, T.; Wang, H.; Wang, T.; Qin, M.; Bao, P.; Wang, R.; Liu, Y.; Chang, H.-C.; Yan, J.; et al. Neurodegeneration-Associated FUS Is a Novel Regulator of Circadian Gene Expression. Transl. Neurodegener. 2018, 7, 24. [Google Scholar] [CrossRef] [PubMed]
- Kamelgarn, M.; Chen, J.; Kuang, L.; Jin, H.; Kasarskis, E.J.; Zhu, H. ALS Mutations of FUS Suppress Protein Translation and Disrupt the Regulation of Nonsense-Mediated Decay. Proc. Natl. Acad. Sci. USA 2018, 115, E11904–E11913. [Google Scholar] [CrossRef]
- Holmberg, C.I.; Tran, S.E.F.; Eriksson, J.E.; Sistonen, L. Multisite Phosphorylation Provides Sophisticated Regulation of Transcription Factors. Trends Biochem. Sci. 2002, 27, 619–627. [Google Scholar] [CrossRef]
- Filtz, T.M.; Vogel, W.K.; Leid, M. Regulation of Transcription Factor Activity by Interconnected Post-Translational Modifications. Trends Pharmacol. Sci. 2014, 35, 76–85. [Google Scholar] [CrossRef] [PubMed]
- Whitmarsh, A.J.; Davis, R.J. Regulation of Transcription Factor Function by Phosphorylation. Cell. Mol. Life Sci. 2000, 57, 1172–1183. [Google Scholar] [CrossRef]
- Sotthibundhu, A.; Ekthuwapranee, K.; Govitrapong, P. Comparison of Melatonin with Growth Factors in Promoting Precursor Cells Proliferation in Adult Mouse Subventricular Zone. EXCLI J. 2016, 15, 829–841. [Google Scholar] [CrossRef]
- Onaolapo, O.J.; Onaolapo, A.Y.; Olowe, O.A.; Udoh, M.O.; Udoh, D.O.; Nathaniel, T.I. Melatonin and Melatonergic Influence on Neuronal Transcription Factors: Implications for the Development of Novel Therapies for Neurodegenerative Disorders. Curr. Neuropharmacol. 2020, 18, 563–577. [Google Scholar] [CrossRef] [PubMed]
- Aumiller, W.M.; Keating, C.D. Phosphorylation-Mediated RNA/peptide Complex Coacervation as a Model for Intracellular Liquid Organelles. Nat. Chem. 2016, 8, 129–137. [Google Scholar] [CrossRef]
- Kamagata, K.; Kanbayashi, S.; Honda, M.; Itoh, Y.; Takahashi, H.; Kameda, T.; Nagatsugi, F.; Takahashi, S. Liquid-like Droplet Formation by Tumor Suppressor p53 Induced by Multivalent Electrostatic Interactions between Two Disordered Domains. Sci. Rep. 2020, 10, 580. [Google Scholar] [CrossRef]
- Ardito, F.; Giuliani, M.; Perrone, D.; Troiano, G.; Lo Muzio, L. The Crucial Role of Protein Phosphorylation in Cell Signaling and Its Use as Targeted Therapy (Review). Int. J. Mol. Med. 2017, 40, 271–280. [Google Scholar] [CrossRef]
- Zhou, H.-X.; Pang, X. Electrostatic Interactions in Protein Structure, Folding, Binding, and Condensation. Chem. Rev. 2018, 118, 1691–1741. [Google Scholar] [CrossRef]
- Milovanovic, D.; Wu, Y.; Bian, X.; De Camilli, P. A Liquid Phase of Synapsin and Lipid Vesicles. Science 2018, 361, 604–607. [Google Scholar] [CrossRef]
- Beutel, O.; Maraspini, R.; Pombo-García, K.; Martin-Lemaitre, C.; Honigmann, A. Phase Separation of Zonula Occludens Proteins Drives Formation of Tight Junctions. Cell 2019, 179, 923–936.e11. [Google Scholar] [CrossRef]
- Wang, J.T.; Smith, J.; Chen, B.-C.; Schmidt, H.; Rasoloson, D.; Paix, A.; Lambrus, B.G.; Calidas, D.; Betzig, E.; Seydoux, G. Regulation of RNA Granule Dynamics by Phosphorylation of Serine-Rich, Intrinsically Disordered Proteins in C. Elegans. Elife 2014, 3, e04591. [Google Scholar] [CrossRef] [PubMed]
- Gustafson, E.A.; Wessel, G.M. DEAD-Box Helicases: Posttranslational Regulation and Function. Biochem. Biophys. Res. Commun. 2010, 395, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Soulat, D.; Bürckstümmer, T.; Westermayer, S.; Goncalves, A.; Bauch, A.; Stefanovic, A.; Hantschel, O.; Bennett, K.L.; Decker, T.; Superti-Furga, G. The DEAD-Box Helicase DDX3X Is a Critical Component of the TANK-Binding Kinase 1-Dependent Innate Immune Response. EMBO J. 2008, 27, 2135–2146. [Google Scholar] [CrossRef]
- Ron, D. Translational Control in the Endoplasmic Reticulum Stress Response. J. Clin. Investig. 2002, 110, 1383–1388. [Google Scholar] [CrossRef] [PubMed]
- Wek, R.C.; Jiang, H.-Y.; Anthony, T.G. Coping with Stress: eIF2 Kinases and Translational Control. Biochem. Soc. Trans. 2006, 34, 7–11. [Google Scholar] [CrossRef] [PubMed]
- Donnelly, N.; Gorman, A.M.; Gupta, S.; Samali, A. The eIF2α Kinases: Their Structures and Functions. Cell. Mol. Life Sci. 2013, 70, 3493–3511. [Google Scholar] [CrossRef]
- Pakos-Zebrucka, K.; Koryga, I.; Mnich, K.; Ljujic, M.; Samali, A.; Gorman, A.M. The Integrated Stress Response. EMBO Rep. 2016, 17, 1374–1395. [Google Scholar] [CrossRef]
- Sidrauski, C.; McGeachy, A.M.; Ingolia, N.T.; Walter, P. The Small Molecule ISRIB Reverses the Effects of eIF2α Phosphorylation on Translation and Stress Granule Assembly. Elife 2015, 4, e05033. [Google Scholar] [CrossRef] [PubMed]
- Wheeler, J.R.; Matheny, T.; Jain, S.; Abrisch, R.; Parker, R. Distinct Stages in Stress Granule Assembly and Disassembly. Elife 2016, 5, e18413. [Google Scholar] [CrossRef]
- Anderson, P.; Kedersha, N. Visibly Stressed: The Role of eIF2, TIA-1, and Stress Granules in Protein Translation. Cell Stress Chaperones 2002, 7, 213–221. [Google Scholar] [CrossRef]
- Mateju, D.; Eichenberger, B.; Voigt, F.; Eglinger, J.; Roth, G.; Chao, J.A. Single-Molecule Imaging Reveals Translation of mRNAs Localized to Stress Granules. Cell 2020, 183, 1801–1812.e13. [Google Scholar] [CrossRef]
- Baumann, K. mRNA Translation in Stress Granules Is Not Uncommon. Nat. Rev. Mol. Cell Biol. 2021, 22, 164. [Google Scholar] [CrossRef] [PubMed]
- Ivanov, P.; Kedersha, N.; Anderson, P. Stress Granules and Processing Bodies in Translational Control. Cold Spring Harb. Perspect. Biol. 2019, 11, a032813. [Google Scholar] [CrossRef]
- Novoa, I.; Zeng, H.; Harding, H.P.; Ron, D. Feedback Inhibition of the Unfolded Protein Response by GADD34-Mediated Dephosphorylation of eIF2alpha. J. Cell Biol. 2001, 153, 1011–1022. [Google Scholar] [CrossRef] [PubMed]
- Mazroui, R.; Sukarieh, R.; Bordeleau, M.-E.; Kaufman, R.J.; Northcote, P.; Tanaka, J.; Gallouzi, I.; Pelletier, J. Inhibition of Ribosome Recruitment Induces Stress Granule Formation Independently of Eukaryotic Initiation Factor 2alpha Phosphorylation. Mol. Biol. Cell 2006, 17, 4212–4219. [Google Scholar] [CrossRef] [PubMed]
- Lu, P.D.; Harding, H.P.; Ron, D. Translation Reinitiation at Alternative Open Reading Frames Regulates Gene Expression in an Integrated Stress Response. J. Cell Biol. 2004, 167, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.; Protter, D.S.W.; Rosen, M.K.; Parker, R. Formation and Maturation of Phase-Separated Liquid Droplets by RNA-Binding Proteins. Mol. Cell 2015, 60, 208–219. [Google Scholar] [CrossRef]
- Buchan, J.R.; Kolaitis, R.-M.; Taylor, J.P.; Parker, R. Eukaryotic Stress Granules Are Cleared by Autophagy and Cdc48/VCP Function. Cell 2013, 153, 1461–1474. [Google Scholar] [CrossRef]
- Chen, X.; Chen, M.; Schafer, N.P.; Wolynes, P.G. Exploring the Interplay between Fibrillization and Amorphous Aggregation Channels on the Energy Landscapes of Tau Repeat Isoforms. Proc. Natl. Acad. Sci. USA 2020, 117, 4125–4130. [Google Scholar] [CrossRef] [PubMed]
- Shafiei, S.S.; Guerrero-Muñoz, M.J.; Castillo-Carranza, D.L. Tau Oligomers: Cytotoxicity, Propagation, and Mitochondrial Damage. Front. Aging. Neurosci. 2017, 9, 83. [Google Scholar] [CrossRef] [PubMed]
- Kadavath, H.; Hofele, R.V.; Biernat, J.; Kumar, S.; Tepper, K.; Urlaub, H.; Mandelkow, E.; Zweckstetter, M. Tau Stabilizes Microtubules by Binding at the Interface between Tubulin Heterodimers. Proc. Natl. Acad. Sci. USA 2015, 112, 7501–7506. [Google Scholar] [CrossRef] [PubMed]
- Johnson, G.V.; Hartigan, J.A. Tau Protein in Normal and Alzheimer’s Disease Brain: An Update. J. Alzheimers. Dis. 1999, 1, 329–351. [Google Scholar] [CrossRef]
- Ambadipudi, S.; Biernat, J.; Riedel, D.; Mandelkow, E.; Zweckstetter, M. Liquid-Liquid Phase Separation of the Microtubule-Binding Repeats of the Alzheimer-Related Protein Tau. Nat. Commun. 2017, 8, 275. [Google Scholar] [CrossRef]
- Kanaan, N.M.; Hamel, C.; Grabinski, T.; Combs, B. Liquid-Liquid Phase Separation Induces Pathogenic Tau Conformations in Vitro. Nat. Commun. 2020, 11, 2809. [Google Scholar] [CrossRef]
- Kent, S.A.; Spires-Jones, T.L.; Durrant, C.S. The Physiological Roles of Tau and Aβ: Implications for Alzheimer’s Disease Pathology and Therapeutics. Acta Neuropathol. 2020, 140, 417–447. [Google Scholar] [CrossRef]
- Ferrer, I.; Andrés-Benito, P.; Zelaya, M.V.; Aguirre, M.E.E.; Carmona, M.; Ausín, K.; Lachén-Montes, M.; Fernández-Irigoyen, J.; Santamaría, E.; Del Rio, J.A. Familial Globular Glial Tauopathy Linked to MAPT Mutations: Molecular Neuropathology and Seeding Capacity of a Prototypical Mixed Neuronal and Glial Tauopathy. Acta Neuropathol. 2020, 139, 735–771. [Google Scholar] [CrossRef]
- McAleese, K.E.; Firbank, M.; Dey, M.; Colloby, S.J.; Walker, L.; Johnson, M.; Beverley, J.R.; Taylor, J.P.; Thomas, A.J.; O’Brien, J.T.; et al. Cortical Tau Load Is Associated with White Matter Hyperintensities. Acta Neuropathol. Commun. 2015, 3, 60. [Google Scholar] [CrossRef]
- Kanaan, N.M.; Morfini, G.A.; LaPointe, N.E.; Pigino, G.F.; Patterson, K.R.; Song, Y.; Andreadis, A.; Fu, Y.; Brady, S.T.; Binder, L.I. Pathogenic Forms of Tau Inhibit Kinesin-Dependent Axonal Transport through a Mechanism Involving Activation of Axonal Phosphotransferases. J. Neurosci. 2011, 31, 9858–9868. [Google Scholar] [CrossRef]
- Lei, P.; Ayton, S.; Moon, S.; Zhang, Q.; Volitakis, I.; Finkelstein, D.I.; Bush, A.I. Motor and Cognitive Deficits in Aged Tau Knockout Mice in Two Background Strains. Mol. Neurodegener. 2014, 9, 29. [Google Scholar] [CrossRef] [PubMed]
- Velazquez, R.; Ferreira, E.; Tran, A.; Turner, E.C.; Belfiore, R.; Branca, C.; Oddo, S. Acute Tau Knockdown in the Hippocampus of Adult Mice Causes Learning and Memory Deficits. Aging Cell 2018, 17, e12775. [Google Scholar] [CrossRef]
- Kobayashi, S.; Tanaka, T.; Soeda, Y.; Takashima, A. Enhanced Tau Protein Translation by Hyper-Excitation. Front. Aging. Neurosci. 2019, 11, 322. [Google Scholar] [CrossRef]
- Marciniak, E.; Leboucher, A.; Caron, E.; Ahmed, T.; Tailleux, A.; Dumont, J.; Issad, T.; Gerhardt, E.; Pagesy, P.; Vileno, M.; et al. Tau Deletion Promotes Brain Insulin Resistance. J. Exp. Med. 2017, 214, 2257–2269. [Google Scholar] [CrossRef]
- Wijesekara, N.; Gonçalves, R.A.; Ahrens, R.; De Felice, F.G.; Fraser, P.E. Tau Ablation in Mice Leads to Pancreatic β Cell Dysfunction and Glucose Intolerance. FASEB J. 2018, 32, 3166–3173. [Google Scholar] [CrossRef]
- Adams, J.N.; Lockhart, S.N.; Li, L.; Jagust, W.J. Relationships Between Tau and Glucose Metabolism Reflect Alzheimer’s Disease Pathology in Cognitively Normal Older Adults. Cereb. Cortex 2019, 29, 1997–2009. [Google Scholar] [CrossRef] [PubMed]
- Sultan, A.; Nesslany, F.; Violet, M.; Bégard, S.; Loyens, A.; Talahari, S.; Mansuroglu, Z.; Marzin, D.; Sergeant, N.; Humez, S.; et al. Nuclear Tau, a Key Player in Neuronal DNA Protection. J. Biol. Chem. 2011, 286, 4566–4575. [Google Scholar] [CrossRef] [PubMed]
- Rai, S.K.; Savastano, A.; Singh, P.; Mukhopadhyay, S.; Zweckstetter, M. Liquid-Liquid Phase Separation of Tau: From Molecular Biophysics to Physiology and Disease. Protein Sci. 2021, 30, 1294–1314. [Google Scholar] [CrossRef]
- Cleveland, D.W.; Hwo, S.Y.; Kirschner, M.W. Purification of Tau, a Microtubule-Associated Protein That Induces Assembly of Microtubules from Purified Tubulin. J. Mol. Biol. 1977, 116, 207–225. [Google Scholar] [CrossRef]
- Mitchison, T.; Kirschner, M. Dynamic Instability of Microtubule Growth. Nature 1984, 312, 237–242. [Google Scholar] [CrossRef]
- Panda, D.; Daijo, J.E.; Jordan, M.A.; Wilson, L. Kinetic Stabilization of Microtubule Dynamics at Steady State in Vitro by Substoichiometric Concentrations of Tubulin-Colchicine Complex. Biochemistry 1995, 34, 9921–9929. [Google Scholar] [CrossRef]
- Qiang, L.; Yu, W.; Andreadis, A.; Luo, M.; Baas, P.W. Tau Protects Microtubules in the Axon from Severing by Katanin. J. Neurosci. 2006, 26, 3120–3129. [Google Scholar] [CrossRef] [PubMed]
- Boyko, S.; Surewicz, K.; Surewicz, W.K. Regulatory Mechanisms of Tau Protein Fibrillation under the Conditions of Liquid-Liquid Phase Separation. Proc. Natl. Acad. Sci. USA 2020, 117, 31882–31890. [Google Scholar] [CrossRef]
- Liu, M.; Dexheimer, T.; Sui, D.; Hovde, S.; Deng, X.; Kwok, R.; Bochar, D.A.; Kuo, M.-H. Hyperphosphorylated Tau Aggregation and Cytotoxicity Modulators Screen Identified Prescription Drugs Linked to Alzheimer’s Disease and Cognitive Functions. Sci. Rep. 2020, 10, 16551. [Google Scholar] [CrossRef]
- Brunello, C.A.; Merezhko, M.; Uronen, R.-L.; Huttunen, H.J. Mechanisms of Secretion and Spreading of Pathological Tau Protein. Cell Mol. Life Sci. 2020, 77, 1721–1744. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.; Fichou, Y.; Zeng, Z.; Hu, N.Y.; Han, S. Electrostatically Driven Complex Coacervation and Amyloid Aggregation of Tau Are Independent Processes with Overlapping Conditions. ACS Chem. Neurosci. 2020, 11, 615–627. [Google Scholar] [CrossRef]
- Zhang, X.; Lin, Y.; Eschmann, N.A.; Zhou, H.; Rauch, J.N.; Hernandez, I.; Guzman, E.; Kosik, K.S.; Han, S. RNA Stores Tau Reversibly in Complex Coacervates. PLoS Biol. 2017, 15, e2002183. [Google Scholar] [CrossRef]
- Boyko, S.; Qi, X.; Chen, T.-H.; Surewicz, K.; Surewicz, W.K. Liquid-Liquid Phase Separation of Tau Protein: The Crucial Role of Electrostatic Interactions. J. Biol. Chem. 2019, 294, 11054–11059. [Google Scholar] [CrossRef]
- Lin, Y.; McCarty, J.; Rauch, J.N.; Delaney, K.T.; Kosik, K.S.; Fredrickson, G.H.; Shea, J.-E.; Han, S. Narrow Equilibrium Window for Complex Coacervation of Tau and RNA under Cellular Conditions. Elife 2019, 8, e42571. [Google Scholar] [CrossRef]
- Lin, Y.; Fichou, Y.; Longhini, A.P.; Llanes, L.C.; Yin, P.; Bazan, G.C.; Kosik, K.S.; Han, S. Liquid-Liquid Phase Separation of Tau Driven by Hydrophobic Interaction Facilitates Fibrillization of Tau. J. Mol. Biol. 2021, 433, 166731. [Google Scholar] [CrossRef] [PubMed]
- Iqbal, K.; Liu, F.; Gong, C.-X.; Grundke-Iqbal, I. Tau in Alzheimer Disease and Related Tauopathies. Curr. Alzheimer Res. 2010, 7, 656–664. [Google Scholar] [CrossRef] [PubMed]
- Ruben, G.C.; Ciardelli, T.L.; Grundke-Iqbal, I.; Iqbal, K. Alzheimer Disease Hyperphosphorylated Tau Aggregates Hydrophobically. Synapse 1997, 27, 208–229. [Google Scholar] [CrossRef]
- Takashima, A. Hyperphosphorylated Tau Is a Cause of Neuronal Dysfunction in Tauopathy. J. Alzheimers. Dis. 2008, 14, 371–375. [Google Scholar] [CrossRef]
- Alonso, A.D.; Cohen, L.S.; Corbo, C.; Morozova, V.; ElIdrissi, A.; Phillips, G.; Kleiman, F.E. Hyperphosphorylation of Tau Associates With Changes in Its Function Beyond Microtubule Stability. Front. Cell. Neurosci. 2018, 12, 338. [Google Scholar] [CrossRef]
- Wang, J.Z.; Gong, C.X.; Zaidi, T.; Grundke-Iqbal, I.; Iqbal, K. Dephosphorylation of Alzheimer Paired Helical Filaments by Protein Phosphatase-2A and -2B. J. Biol. Chem. 1995, 270, 4854–4860. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.Z.; Grundke-Iqbal, I.; Iqbal, K. Restoration of Biological Activity of Alzheimer Abnormally Phosphorylated Tau by Dephosphorylation with Protein Phosphatase-2A, -2B and -1. Brain Res. Mol. Brain Res. 1996, 38, 200–208. [Google Scholar] [CrossRef]
- Poppek, D.; Keck, S.; Ermak, G.; Jung, T.; Stolzing, A.; Ullrich, O.; Davies, K.J.A.; Grune, T. Phosphorylation Inhibits Turnover of the Tau Protein by the Proteasome: Influence of RCAN1 and Oxidative Stress. Biochem. J. 2006, 400, 511–520. [Google Scholar] [CrossRef] [PubMed]
- Köpke, E.; Tung, Y.C.; Shaikh, S.; Alonso, A.C.; Iqbal, K.; Grundke-Iqbal, I. Microtubule-Associated Protein Tau. Abnormal Phosphorylation of a Non-Paired Helical Filament Pool in Alzheimer Disease. J. Biol. Chem. 1993, 268, 24374–24384. [Google Scholar] [CrossRef]
- Khatoon, S.; Grundke-Iqbal, I.; Iqbal, K. Brain Levels of Microtubule-Associated Protein Tau Are Elevated in Alzheimer’s Disease: A Radioimmuno-Slot-Blot Assay for Nanograms of the Protein. J. Neurochem. 1992, 59, 750–753. [Google Scholar] [CrossRef]
- Gong, C.-X.; Iqbal, K. Hyperphosphorylation of Microtubule-Associated Protein Tau: A Promising Therapeutic Target for Alzheimer Disease. Curr. Med. Chem. 2008, 15, 2321–2328. [Google Scholar] [CrossRef]
- Ait-Bouziad, N.; Chiki, A.; Limorenko, G.; Xiao, S.; Eliezer, D.; Lashuel, H.A. Phosphorylation of the Overlooked Tyrosine 310 Regulates the Structure, Aggregation, and Microtubule- and Lipid-Binding Properties of Tau. J. Biol. Chem. 2020, 295, 7905–7922. [Google Scholar] [CrossRef] [PubMed]
- Bancher, C.; Brunner, C.; Lassmann, H.; Budka, H.; Jellinger, K.; Wiche, G.; Seitelberger, F.; Grundke-Iqbal, I.; Iqbal, K.; Wisniewski, H.M. Accumulation of Abnormally Phosphorylated Tau Precedes the Formation of Neurofibrillary Tangles in Alzheimer’s Disease. Brain Res. 1989, 477, 90–99. [Google Scholar] [CrossRef]
- Qi, H.; Cantrelle, F.-X.; Benhelli-Mokrani, H.; Smet-Nocca, C.; Buée, L.; Lippens, G.; Bonnefoy, E.; Galas, M.-C.; Landrieu, I. Nuclear Magnetic Resonance Spectroscopy Characterization of Interaction of Tau with DNA and Its Regulation by Phosphorylation. Biochemistry 2015, 54, 1525–1533. [Google Scholar] [CrossRef] [PubMed]
- Hua, Q.; He, R.-Q. Tau Could Protect DNA Double Helix Structure. Biochim. Biophys. Acta 2003, 1645, 205–211. [Google Scholar] [CrossRef]
- Castellani, R.J.; Nunomura, A.; Lee, H.-G.; Perry, G.; Smith, M.A. Phosphorylated Tau: Toxic, Protective, or None of the above. J. Alzheimers. Dis. 2008, 14, 377–383. [Google Scholar] [CrossRef]
- Luna-Muñoz, J.; Harrington, C.R.; Wischik, C.M.; Flores-Rodríguez, P.; Avila, J.; Zamudio, S.R.; la Cruz, F.D.; Mena, R.; Meraz-Ríos, M.A.; Floran-Garduño, B. Phosphorylation of Tau Protein Associated as a Protective Mechanism in the Presence of Toxic, C-Terminally Truncated Tau in Alzheimer’s Disease. In Understanding Alzheimer’s Disease; Zerr, I., Ed.; IntechOpen: London, UK, 2013. [Google Scholar] [CrossRef]
- Castellani, R.J.; Honda, K.; Zhu, X.; Cash, A.D.; Nunomura, A.; Perry, G.; Smith, M.A. Contribution of Redox-Active Iron and Copper to Oxidative Damage in Alzheimer Disease. Ageing. Res. Rev. 2004, 3, 319–326. [Google Scholar] [CrossRef]
- Smith, M.A.; Harris, P.L.; Sayre, L.M.; Perry, G. Iron Accumulation in Alzheimer Disease Is a Source of Redox-Generated Free Radicals. Proc. Natl. Acad. Sci. USA 1997, 94, 9866–9868. [Google Scholar] [CrossRef]
- Sayre, L.M.; Perry, G.; Harris, P.L.; Liu, Y.; Schubert, K.A.; Smith, M.A. In Situ Oxidative Catalysis by Neurofibrillary Tangles and Senile Plaques in Alzheimer’s Disease: A Central Role for Bound Transition Metals. J. Neurochem. 2000, 74, 270–279. [Google Scholar] [CrossRef]
- Smith, M.A.; Casadesus, G.; Joseph, J.A.; Perry, G. Amyloid-β and τ Serve Antioxidant Functions in the Aging and Alzheimer Brain. Free. Radic. Biol. Med. 2002, 33, 1194–1199. [Google Scholar] [CrossRef]
- Li, H.-L.; Wang, H.-H.; Liu, S.-J.; Deng, Y.-Q.; Zhang, Y.-J.; Tian, Q.; Wang, X.-C.; Chen, X.-Q.; Yang, Y.; Zhang, J.-Y.; et al. Phosphorylation of Tau Antagonizes Apoptosis by Stabilizing Beta-Catenin, a Mechanism Involved in Alzheimer’s Neurodegeneration. Proc. Natl. Acad. Sci. USA 2007, 104, 3591–3596. [Google Scholar] [CrossRef]
- Wang, H.-H.; Li, H.-L.; Liu, R.; Zhang, Y.; Liao, K.; Wang, Q.; Wang, J.-Z.; Liu, S.-J. Tau Overexpression Inhibits Cell Apoptosis with the Mechanisms Involving Multiple Viability-Related Factors. J. Alzheimers. Dis. 2010, 21, 167–179. [Google Scholar] [CrossRef]
- Haj-Yahya, M.; Gopinath, P.; Rajasekhar, K.; Mirbaha, H.; Diamond, M.I.; Lashuel, H.A. Site-Specific Hyperphosphorylation Inhibits, Rather than Promotes, Tau Fibrillization, Seeding Capacity, and Its Microtubule Binding. Angew. Chem. Int. Ed Engl. 2020, 59, 4059–4067. [Google Scholar] [CrossRef]
- Amir Mishan, M.; Rezaei Kanavi, M.; Shahpasand, K.; Ahmadieh, H. Pathogenic Tau Protein Species: Promising Therapeutic Targets for Ocular Neurodegenerative Diseases. J. Ophthalmic Vis. Res. 2019, 14, 491–505. [Google Scholar] [CrossRef] [PubMed]
- Miao, J.; Shi, R.; Li, L.; Chen, F.; Zhou, Y.; Tung, Y.C.; Hu, W.; Gong, C.-X.; Iqbal, K.; Liu, F. Pathological Tau from Alzheimer’s Brain Induces Site-Specific Hyperphosphorylation and SDS- and Reducing Agent-Resistant Aggregation of Tau in Vivo. Front. Aging Neurosci. 2019, 11, 34. [Google Scholar] [CrossRef]
- Wang, Y.; Mandelkow, E. Tau in Physiology and Pathology. Nat. Rev. Neurosci. 2016, 17, 5–21. [Google Scholar] [CrossRef] [PubMed]
- Fath, T.; Eidenmüller, J.; Brandt, R. Tau-Mediated Cytotoxicity in a Pseudohyperphosphorylation Model of Alzheimer’s Disease. J. Neurosci. 2002, 22, 9733–9741. [Google Scholar] [CrossRef]
- Di, J.; Cohen, L.S.; Corbo, C.P.; Phillips, G.R.; El Idrissi, A.; Alonso, A.D. Abnormal Tau Induces Cognitive Impairment through Two Different Mechanisms: Synaptic Dysfunction and Neuronal Loss. Sci. Rep. 2016, 6, 20833. [Google Scholar] [CrossRef]
- Tai, X.Y.; Koepp, M.; Duncan, J.S.; Fox, N.; Thompson, P.; Baxendale, S.; Liu, J.Y.W.; Reeves, C.; Michalak, Z.; Thom, M. Hyperphosphorylated Tau in Patients with Refractory Epilepsy Correlates with Cognitive Decline: A Study of Temporal Lobe Resections. Brain 2016, 139, 2441–2455. [Google Scholar] [CrossRef] [PubMed]
- Nelson, P.T.; Alafuzoff, I.; Bigio, E.H.; Bouras, C.; Braak, H.; Cairns, N.J.; Castellani, R.J.; Crain, B.J.; Davies, P.; Del Tredici, K.; et al. Correlation of Alzheimer Disease Neuropathologic Changes with Cognitive Status: A Review of the Literature. J. Neuropathol. Exp. Neurol. 2012, 71, 362–381. [Google Scholar] [CrossRef]
- Cardinali, D.P. Melatonin: Clinical Perspectives in Neurodegeneration. Front. Endocrinol. 2019, 10, 480. [Google Scholar] [CrossRef]
- Srinivasan, V.; Pandi-Perumal, S.R.; Maestroni, G.J.; Esquifino, A.I.; Hardeland, R.; Cardinali, D.P. Role of Melatonin in Neurodegenerative Diseases. Neurotox. Res. 2005, 7, 293–318. [Google Scholar] [CrossRef]
- Kong, P.-J.; Byun, J.-S.; Lim, S.-Y.; Lee, J.-J.; Hong, S.-J.; Kwon, K.-J.; Kim, S.-S. Melatonin Induces Akt Phosphorylation through Melatonin Receptor- and PI3K-Dependent Pathways in Primary Astrocytes. Korean J. Physiol. Pharmacol. 2008, 12, 37–41. [Google Scholar] [CrossRef] [PubMed]
- Kilic, U.; Caglayan, A.B.; Beker, M.C.; Gunal, M.Y.; Caglayan, B.; Yalcin, E.; Kelestemur, T.; Gundogdu, R.Z.; Yulug, B.; Yılmaz, B.; et al. Particular Phosphorylation of PI3K/Akt on Thr308 via PDK-1 and PTEN Mediates Melatonin’s Neuroprotective Activity after Focal Cerebral Ischemia in Mice. Redox Biol. 2017, 12, 657–665. [Google Scholar] [CrossRef]
- Hooper, C.; Killick, R.; Lovestone, S. The GSK3 Hypothesis of Alzheimer’s Disease. J. Neurochem. 2008, 104, 1433–1439. [Google Scholar] [CrossRef]
- Hernandez, F.; Lucas, J.J.; Avila, J. GSK3 and Tau: Two Convergence Points in Alzheimer’s Disease. J. Alzheimers. Dis. 2013, 33 (Suppl. 1), S141–S144. [Google Scholar] [CrossRef]
- Toral-Rios, D.; Pichardo-Rojas, P.S.; Alonso-Vanegas, M.; Campos-Peña, V. GSK3β and Tau Protein in Alzheimer’s Disease and Epilepsy. Front. Cell Neurosci. 2020, 14, 19. [Google Scholar] [CrossRef]
- Ali, T.; Kim, M.O. Melatonin Ameliorates Amyloid Beta-Induced Memory Deficits, Tau Hyperphosphorylation and Neurodegeneration via PI3/Akt/GSk3β Pathway in the Mouse Hippocampus. J. Pineal. Res. 2015, 59, 47–59. [Google Scholar] [CrossRef] [PubMed]
- Luengo, E.; Buendia, I.; Fernández-Mendívil, C.; Trigo-Alonso, P.; Negredo, P.; Michalska, P.; Hernández-García, B.; Sánchez-Ramos, C.; Bernal, J.A.; Ikezu, T.; et al. Pharmacological Doses of Melatonin Impede Cognitive Decline in Tau-Related Alzheimer Models, Once Tauopathy Is Initiated, by Restoring the Autophagic Flux. J. Pineal. Res. 2019, 67, e12578. [Google Scholar] [CrossRef]
- Shi, C.; Zeng, J.; Li, Z.; Chen, Q.; Hang, W.; Xia, L.; Wu, Y.; Chen, J.; Shi, A. Melatonin Mitigates Kainic Acid-Induced Neuronal Tau Hyperphosphorylation and Memory Deficits through Alleviating ER Stress. Front. Mol. Neurosci. 2018, 11, 5. [Google Scholar] [CrossRef] [PubMed]
- Yao, K.; Zhao, Y.-F.; Zu, H.-B. Melatonin Receptor Stimulation by Agomelatine Prevents Aβ-Induced Tau Phosphorylation and Oxidative Damage in PC12 Cells. Drug Des. Devel. Ther. 2019, 13, 387–396. [Google Scholar] [CrossRef]
- Heberle, A.M.; Razquin Navas, P.; Langelaar-Makkinje, M.; Kasack, K.; Sadik, A.; Faessler, E.; Hahn, U.; Marx-Stoelting, P.; Opitz, C.A.; Sers, C.; et al. The PI3K and MAPK/p38 Pathways Control Stress Granule Assembly in a Hierarchical Manner. Life Sci. Alliance 2019, 2, e201800257. [Google Scholar] [CrossRef]
- Das, R.; Balmik, A.A.; Chinnathambi, S. Melatonin Reduces GSK3β-Mediated Tau Phosphorylation, Enhances Nrf2 Nuclear Translocation and Anti-Inflammation. ASN Neuro. 2020, 12, 1759091420981204. [Google Scholar] [CrossRef] [PubMed]
- Das, R.; Balmik, A.A.; Chinnathambi, S. Effect of Melatonin on Tau Aggregation and Tau-Mediated Cell Surface Morphology. Int. J. Biol. Macromol. 2020, 152, 30–39. [Google Scholar] [CrossRef]
- Schwalbe, M.; Kadavath, H.; Biernat, J.; Ozenne, V.; Blackledge, M.; Mandelkow, E.; Zweckstetter, M. Structural Impact of Tau Phosphorylation at Threonine 231. Structure 2015, 23, 1448–1458. [Google Scholar] [CrossRef] [PubMed]
- Raz, Y.; Miller, Y. Interactions between Aβ and Mutated Tau Lead to Polymorphism and Induce Aggregation of Aβ-Mutated Tau Oligomeric Complexes. PLoS ONE 2013, 8, e73303. [Google Scholar] [CrossRef]
- Skribanek, Z.; Baláspiri, L.; Mák, M. Interaction between Synthetic Amyloid-Beta-Peptide (1-40) and Its Aggregation Inhibitors Studied by Electrospray Ionization Mass Spectrometry. J. Mass Spectrom. 2001, 36, 1226–1229. [Google Scholar] [CrossRef]
- He, H.; Dong, W.; Huang, F. Anti-Amyloidogenic and Anti-Apoptotic Role of Melatonin in Alzheimer Disease. Curr. Neuropharmacol. 2010, 8, 211–217. [Google Scholar] [CrossRef] [PubMed]
- Berhanu, W.M.; Hansmann, U.H.E. Structure and Dynamics of Amyloid-β Segmental Polymorphisms. PLoS ONE 2012, 7, e41479. [Google Scholar] [CrossRef]
- Fraser, P.E.; Nguyen, J.T.; Surewicz, W.K.; Kirschner, D.A. pH-Dependent Structural Transitions of Alzheimer Amyloid Peptides. Biophys. J. 1991, 60, 1190–1201. [Google Scholar] [CrossRef]
- Huang, T.H.; Fraser, P.E.; Chakrabartty, A. Fibrillogenesis of Alzheimer Abeta Peptides Studied by Fluorescence Energy Transfer. J. Mol. Biol. 1997, 269, 214–224. [Google Scholar] [CrossRef]
- Kawarabayashi, T.; Shoji, M.; Younkin, L.H.; Wen-Lang, L.; Dickson, D.W.; Murakami, T.; Matsubara, E.; Abe, K.; Ashe, K.H.; Younkin, S.G. Dimeric Amyloid Beta Protein Rapidly Accumulates in Lipid Rafts Followed by Apolipoprotein E and Phosphorylated Tau Accumulation in the Tg2576 Mouse Model of Alzheimer’s Disease. J. Neurosci. 2004, 24, 3801–3809. [Google Scholar] [CrossRef]
- Whitehead, S.N.; Gangaraju, S.; Aylsworth, A.; Hou, S.T. Membrane Raft Disruption Results in Neuritic Retraction prior to Neuronal Death in Cortical Neurons. Biosci. Trends 2012, 6, 183–191. [Google Scholar] [CrossRef]
- Pooler, A.M.; Hanger, D.P. Functional Implications of the Association of Tau with the Plasma Membrane. Biochem. Soc. Trans. 2010, 38, 1012–1015. [Google Scholar] [CrossRef] [PubMed]
- Pooler, A.M.; Usardi, A.; Evans, C.J.; Philpott, K.L.; Noble, W.; Hanger, D.P. Dynamic Association of Tau with Neuronal Membranes Is Regulated by Phosphorylation. Neurobiol. Aging. 2012, 33, 431.e27–e38. [Google Scholar] [CrossRef] [PubMed]
- Arrasate, M.; Pérez, M.; Avila, J. Tau Dephosphorylation at Tau-1 Site Correlates with Its Association to Cell Membrane. Neurochem. Res. 2000, 25, 43–50. [Google Scholar] [CrossRef] [PubMed]
- Ekinci, F.J.; Shea, T.B. Phosphorylation of Tau Alters Its Association with the Plasma Membrane. Cell. Mol. Neurobiol. 2000, 20, 497–508. [Google Scholar] [CrossRef]
- Yamauchi, Y.; Reid, P.C.; Sperry, J.B.; Furukawa, K.; Takeya, M.; Chang, C.C.Y.; Chang, T.-Y. Plasma Membrane Rafts Complete Cholesterol Synthesis by Participating in Retrograde Movement of Precursor Sterols. J. Biol. Chem. 2007, 282, 34994–35004. [Google Scholar] [CrossRef] [PubMed]
- Sawamura, N.; Gong, J.-S.; Chang, T.-Y.; Yanagisawa, K.; Michikawa, M. Promotion of Tau Phosphorylation by MAP Kinase Erk1/2 Is Accompanied by Reduced Cholesterol Level in Detergent-Insoluble Membrane Fraction in Niemann-Pick C1-Deficient Cells. J. Neurochem. 2003, 84, 1086–1096. [Google Scholar] [CrossRef]
- Glöckner, F.; Ohm, T.G. Tau Pathology Induces Intraneuronal Cholesterol Accumulation. J. Neuropathol. Exp. Neurol. 2014, 73, 846–854. [Google Scholar] [CrossRef]
- Jones, E.M.; Dubey, M.; Camp, P.J.; Vernon, B.C.; Biernat, J.; Mandelkow, E.; Majewski, J.; Chi, E.Y. Interaction of Tau Protein with Model Lipid Membranes Induces Tau Structural Compaction and Membrane Disruption. Biochemistry 2012, 51, 2539–2550. [Google Scholar] [CrossRef] [PubMed]
- Vogel, S.K.; Greiss, F.; Khmelinskaia, A.; Schwille, P. Control of Lipid Domain Organization by a Biomimetic Contractile Actomyosin Cortex. Elife 2017, 6, e24350. [Google Scholar] [CrossRef] [PubMed]
- Connell, S.D.; Smith, D.A. The Atomic Force Microscope as a Tool for Studying Phase Separation in Lipid Membranes. Mol. Membr. Biol. 2006, 23, 17–28. [Google Scholar] [CrossRef]
- Lee, C.-W.; Jang, L.-L.; Pan, H.-J.; Chen, Y.-R.; Chen, C.-C.; Lee, C.-H. Membrane Roughness as a Sensitive Parameter Reflecting the Status of Neuronal Cells in Response to Chemical and Nanoparticle Treatments. J. Nanobiotechnology 2016, 14, 9. [Google Scholar] [CrossRef] [PubMed]
- Farmer, K.M.; Ghag, G.; Puangmalai, N.; Montalbano, M.; Bhatt, N.; Kayed, R. P53 Aggregation, Interactions with Tau, and Impaired DNA Damage Response in Alzheimer’s Disease. Acta Neuropathol. Commun. 2020, 8, 132. [Google Scholar] [CrossRef] [PubMed]
- Jazvinšćak Jembrek, M.; Slade, N.; Hof, P.R.; Šimić, G. The Interactions of p53 with Tau and Aß as Potential Therapeutic Targets for Alzheimer’s Disease. Prog. Neurobiol. 2018, 168, 104–127. [Google Scholar] [CrossRef]
- Hooper, C.; Meimaridou, E.; Tavassoli, M.; Melino, G.; Lovestone, S.; Killick, R. p53 Is Upregulated in Alzheimer’s Disease and Induces Tau Phosphorylation in HEK293a Cells. Neurosci. Lett. 2007, 418, 34–37. [Google Scholar] [CrossRef]
- Rueda-Rincon, N.; Bloch, K.; Derua, R.; Vyas, R.; Harms, A.; Hankemeier, T.; Khan, N.A.; Dehairs, J.; Bagadi, M.; Binda, M.M.; et al. p53 Attenuates AKT Signaling by Modulating Membrane Phospholipid Composition. Oncotarget 2015, 6, 21240–21254. [Google Scholar] [CrossRef]
- Pascual, A.S.; Espejo, L.S.; Moore, J.L.; Leyva, K.J.; Hull, E.E. Properties of Lipid Rafts in Two Epigenetically Distinct Subtypes of the Oncogenic Cell-line SW13. FASEB J. 2020, 34, 1. [Google Scholar] [CrossRef]
- Lane, D.P. Cancer. p53, Guardian of the Genome. Nature 1992, 358, 15–16. [Google Scholar] [CrossRef]
- Lakin, N.D.; Jackson, S.P. Regulation of p53 in Response to DNA Damage. Oncogene 1999, 18, 7644–7655. [Google Scholar] [CrossRef]
- Reisman, D.; Takahashi, P.; Polson, A.; Boggs, K. Transcriptional Regulation of the p53 Tumor Suppressor Gene in S-Phase of the Cell-Cycle and the Cellular Response to DNA Damage. Biochem. Res. Int. 2012, 2012, 808934. [Google Scholar] [CrossRef]
- Beckerman, R.; Prives, C. Transcriptional Regulation by p53. Cold Spring Harb. Perspect. Biol. 2010, 2, a000935. [Google Scholar] [CrossRef]
- Murray-Zmijewski, F.; Slee, E.A.; Lu, X. A Complex Barcode Underlies the Heterogeneous Response of p53 to Stress. Nat. Rev. Mol. Cell Biol. 2008, 9, 702–712. [Google Scholar] [CrossRef] [PubMed]
- Lane, D.P.; Crawford, L.V. T Antigen Is Bound to a Host Protein in SV40-Transformed Cells. Nature 1979, 278, 261–263. [Google Scholar] [CrossRef] [PubMed]
- Polyak, K.; Xia, Y.; Zweier, J.L.; Kinzler, K.W.; Vogelstein, B. A Model for p53-Induced Apoptosis. Nature 1997, 389, 300–305. [Google Scholar] [CrossRef] [PubMed]
- Pietsch, E.C.; Sykes, S.M.; McMahon, S.B.; Murphy, M.E. The p53 Family and Programmed Cell Death. Oncogene 2008, 27, 6507–6521. [Google Scholar] [CrossRef]
- Aubrey, B.J.; Kelly, G.L.; Janic, A.; Herold, M.J.; Strasser, A. How Does p53 Induce Apoptosis and How Does This Relate to p53-Mediated Tumour Suppression? Cell Death Differ. 2018, 25, 104–113. [Google Scholar] [CrossRef]
- Lane, D.P. p53 and Human Cancers. Br. Med. Bull. 1994, 50, 582–599. [Google Scholar] [CrossRef]
- Rivlin, N.; Brosh, R.; Oren, M.; Rotter, V. Mutations in the p53 Tumor Suppressor Gene: Important Milestones at the Various Steps of Tumorigenesis. Genes Cancer 2011, 2, 466–474. [Google Scholar] [CrossRef]
- Muller, P.A.J.; Vousden, K.H. p53 Mutations in Cancer. Nat. Cell Biol. 2013, 15, 2–8. [Google Scholar] [CrossRef]
- Levine, A.J. p53, the Cellular Gatekeeper for Growth and Division. Cell 1997, 88, 323–331. [Google Scholar] [CrossRef]
- Kruiswijk, F.; Labuschagne, C.F.; Vousden, K.H. p53 in Survival, Death and Metabolic Health: A Lifeguard with a Licence to Kill. Nat. Rev. Mol. Cell Biol. 2015, 16, 393–405. [Google Scholar] [CrossRef] [PubMed]
- Vousden, K.H.; Prives, C. Blinded by the Light: The Growing Complexity of p53. Cell 2009, 137, 413–431. [Google Scholar] [CrossRef]
- Hu, W.; Zhang, C.; Wu, R.; Sun, Y.; Levine, A.; Feng, Z. Glutaminase 2, a Novel p53 Target Gene Regulating Energy Metabolism and Antioxidant Function. Proc. Natl. Acad. Sci. USA 2010, 107, 7455–7460. [Google Scholar] [CrossRef]
- Faraonio, R.; Vergara, P.; Di Marzo, D.; Pierantoni, M.G.; Napolitano, M.; Russo, T.; Cimino, F. p53 Suppresses the Nrf2-Dependent Transcription of Antioxidant Response Genes. J. Biol. Chem. 2006, 281, 39776–39784. [Google Scholar] [CrossRef]
- Kilic, S.; Lezaja, A.; Gatti, M.; Bianco, E.; Michelena, J.; Imhof, R.; Altmeyer, M. Phase Separation of 53BP1 Determines Liquid-like Behavior of DNA Repair Compartments. EMBO J. 2019, 38, e101379. [Google Scholar] [CrossRef]
- Xu, Y. Regulation of p53 Responses by Post-Translational Modifications. Cell Death Differ. 2003, 10, 400–403. [Google Scholar] [CrossRef] [PubMed]
- Meek, D.W.; Anderson, C.W. Posttranslational Modification of p53: Cooperative Integrators of Function. Cold Spring Harb. Perspect. Biol. 2009, 1, a000950. [Google Scholar] [CrossRef]
- Dai, C.; Gu, W. p53 Post-Translational Modification: Deregulated in Tumorigenesis. Trends Mol. Med. 2010, 16, 528–536. [Google Scholar] [CrossRef]
- Asher, G.; Shaul, Y. p53 Proteasomal Degradation: Poly-Ubiquitination Is Not the Whole Story. Cell Cycle 2005, 4, 1015–1018. [Google Scholar] [CrossRef]
- Brooks, C.L.; Gu, W. Dynamics in the p53-Mdm2 Ubiquitination Pathway. Cell Cycle 2004, 3, 895–899. [Google Scholar] [CrossRef] [PubMed]
- Tsvetkov, P.; Reuven, N.; Shaul, Y. Ubiquitin-Independent p53 Proteasomal Degradation. Cell Death Differ. 2010, 17, 103–108. [Google Scholar] [CrossRef]
- Pant, V.; Lozano, G. Limiting the Power of p53 through the Ubiquitin Proteasome Pathway. Genes Dev. 2014, 28, 1739–1751. [Google Scholar] [CrossRef] [PubMed]
- Hock, A.K.; Vousden, K.H. The Role of Ubiquitin Modification in the Regulation of p53. Biochim. Biophys. Acta 2014, 1843, 137–149. [Google Scholar] [CrossRef]
- Kruse, J.-P.; Gu, W. Modes of p53 Regulation. Cell 2009, 137, 609–622. [Google Scholar] [CrossRef]
- Perri, F.; Pisconti, S.; Della Vittoria Scarpati, G. P53 Mutations and Cancer: A Tight Linkage. Ann. Transl. Med. 2016, 4, 522. [Google Scholar] [CrossRef] [PubMed]
- Kotler, E.; Shani, O.; Goldfeld, G.; Lotan-Pompan, M.; Tarcic, O.; Gershoni, A.; Hopf, T.A.; Marks, D.S.; Oren, M.; Segal, E. A Systematic p53 Mutation Library Links Differential Functional Impact to Cancer Mutation Pattern and Evolutionary Conservation. Mol. Cell 2018, 71, 178–190.e8. [Google Scholar] [CrossRef] [PubMed]
- Supek, F.; Miñana, B.; Valcárcel, J.; Gabaldón, T.; Lehner, B. Synonymous Mutations Frequently Act as Driver Mutations in Human Cancers. Cell 2014, 156, 1324–1335. [Google Scholar] [CrossRef]
- Royds, J.A.; Iacopetta, B. p53 and Disease: When the Guardian Angel Fails. Cell Death Differ. 2006, 13, 1017–1026. [Google Scholar] [CrossRef]
- Hainaut, P.; Butcher, S.; Milner, J. Temperature Sensitivity for Conformation Is an Intrinsic Property of Wild-Type p53. Br. J. Cancer 1995, 71, 227–231. [Google Scholar] [CrossRef]
- Joerger, A.C.; Fersht, A.R. Structural Biology of the Tumor Suppressor p53. Annu. Rev. Biochem. 2008, 77, 557–582. [Google Scholar] [CrossRef]
- Brown, C.J.; Lain, S.; Verma, C.S.; Fersht, A.R.; Lane, D.P. Awakening Guardian Angels: Drugging the p53 Pathway. Nat. Rev. Cancer 2009, 9, 862–873. [Google Scholar] [CrossRef] [PubMed]
- Muller, P.A.J.; Vousden, K.H. Mutant p53 in Cancer: New Functions and Therapeutic Opportunities. Cancer Cell 2014, 25, 304–317. [Google Scholar] [CrossRef]
- Krois, A.S.; Dyson, H.J.; Wright, P.E. Long-Range Regulation of p53 DNA Binding by Its Intrinsically Disordered N-Terminal Transactivation Domain. Proc. Natl. Acad. Sci. USA 2018, 115, E11302–E11310. [Google Scholar] [CrossRef]
- Laptenko, O.; Shiff, I.; Freed-Pastor, W.; Zupnick, A.; Mattia, M.; Freulich, E.; Shamir, I.; Kadouri, N.; Kahan, T.; Manfredi, J.; et al. The p53 C Terminus Controls Site-Specific DNA Binding and Promotes Structural Changes within the Central DNA Binding Domain. Mol. Cell 2015, 57, 1034–1046. [Google Scholar] [CrossRef]
- Kim, H.; Kim, K.; Choi, J.; Heo, K.; Baek, H.J.; Roeder, R.G.; An, W. p53 Requires an Intact C-Terminal Domain for DNA Binding and Transactivation. J. Mol. Biol. 2012, 415, 843–854. [Google Scholar] [CrossRef] [PubMed]
- De Smet, F.; Saiz Rubio, M.; Hompes, D.; Naus, E.; De Baets, G.; Langenberg, T.; Hipp, M.S.; Houben, B.; Claes, F.; Charbonneau, S.; et al. Nuclear Inclusion Bodies of Mutant and Wild-Type p53 in Cancer: A Hallmark of p53 Inactivation and Proteostasis Remodelling by p53 Aggregation. J. Pathol. 2017, 242, 24–38. [Google Scholar] [CrossRef] [PubMed]
- Ano Bom, A.P.D.; Rangel, L.P.; Costa, D.C.F.; de Oliveira, G.A.P.; Sanches, D.; Braga, C.A.; Gava, L.M.; Ramos, C.H.I.; Cepeda, A.O.T.; Stumbo, A.C.; et al. Mutant p53 Aggregates into Prion-like Amyloid Oligomers and Fibrils: Implications for Cancer. J. Biol. Chem. 2012, 287, 28152–28162. [Google Scholar] [CrossRef]
- Rangel, L.P.; Costa, D.C.F.; Vieira, T.C.R.G.; Silva, J.L. The Aggregation of Mutant p53 Produces Prion-like Properties in Cancer. Prion 2014, 8, 75–84. [Google Scholar] [CrossRef]
- Silva, J.L.; De Moura Gallo, C.V.; Costa, D.C.F.; Rangel, L.P. Prion-like Aggregation of Mutant p53 in Cancer. Trends Biochem. Sci. 2014, 39, 260–267. [Google Scholar] [CrossRef]
- Ghosh, S.; Salot, S.; Sengupta, S.; Navalkar, A.; Ghosh, D.; Jacob, R.; Das, S.; Kumar, R.; Jha, N.N.; Sahay, S.; et al. p53 Amyloid Formation Leading to Its Loss of Function: Implications in Cancer Pathogenesis. Cell Death Differ. 2017, 24, 1784–1798. [Google Scholar] [CrossRef]
- Park, S.-K.; Park, S.; Pentek, C.; Liebman, S.W. Tumor Suppressor Protein p53 Expressed in Yeast Can Remain Diffuse, Form a Prion, or Form Unstable Liquid-like Droplets. iScience 2021, 24, 102000. [Google Scholar] [CrossRef] [PubMed]
- Gong, H.; Yang, X.; Zhao, Y.; Petersen, R.B.; Liu, X.; Liu, Y.; Huang, K. Amyloidogenicity of p53: A Hidden Link between Protein Misfolding and Cancer. Curr. Protein Pept. Sci. 2015, 16, 135–146. [Google Scholar] [CrossRef]
- Ishimaru, D.; Andrade, L.R.; Teixeira, L.S.P.; Quesado, P.A.; Maiolino, L.M.; Lopez, P.M.; Cordeiro, Y.; Costa, L.T.; Heckl, W.M.; Weissmüller, G.; et al. Fibrillar Aggregates of the Tumor Suppressor p53 Core Domain. Biochemistry 2003, 42, 9022–9027. [Google Scholar] [CrossRef]
- Xu, J.; Reumers, J.; Couceiro, J.R.; De Smet, F.; Gallardo, R.; Rudyak, S.; Cornelis, A.; Rozenski, J.; Zwolinska, A.; Marine, J.-C.; et al. Gain of Function of Mutant p53 by Coaggregation with Multiple Tumor Suppressors. Nat. Chem. Biol. 2011, 7, 285–295. [Google Scholar] [CrossRef] [PubMed]
- Pedrote, M.M.; Motta, M.F.; Ferretti, G.D.S.; Norberto, D.R.; Spohr, T.C.L.S.; Lima, F.R.S.; Gratton, E.; Silva, J.L.; de Oliveira, G.A.P. Oncogenic Gain of Function in Glioblastoma Is Linked to Mutant p53 Amyloid Oligomers. iScience 2020, 23, 100820. [Google Scholar] [CrossRef]
- Navalkar, A.; Ghosh, S.; Pandey, S.; Paul, A.; Datta, D.; Maji, S.K. Prion-like p53 Amyloids in Cancer. Biochemistry 2020, 59, 146–155. [Google Scholar] [CrossRef] [PubMed]
- Buizza, L.; Cenini, G.; Lanni, C.; Ferrari-Toninelli, G.; Prandelli, C.; Govoni, S.; Buoso, E.; Racchi, M.; Barcikowska, M.; Styczynska, M.; et al. Conformational Altered p53 as an Early Marker of Oxidative Stress in Alzheimer’s Disease. PLoS ONE 2012, 7, e29789. [Google Scholar] [CrossRef]
- Amor-Gutiérrez, O.; Costa-Rama, E.; Arce-Varas, N.; Martínez-Rodríguez, C.; Novelli, A.; Fernández-Sánchez, M.T.; Costa-García, A. Competitive Electrochemical Immunosensor for the Detection of Unfolded p53 Protein in Blood as Biomarker for Alzheimer’s Disease. Anal. Chim. Acta 2020, 1093, 28–34. [Google Scholar] [CrossRef]
- Abate, G.; Frisoni, G.B.; Bourdon, J.-C.; Piccirella, S.; Memo, M.; Uberti, D. The Pleiotropic Role of p53 in Functional/dysfunctional Neurons: Focus on Pathogenesis and Diagnosis of Alzheimer’s Disease. Alzheimers. Res. Ther. 2020, 12, 1–10. [Google Scholar] [CrossRef]
- Fusée, L.T.S.; Marín, M.; Fåhraeus, R.; López, I. Alternative Mechanisms of p53 Action During the Unfolded Protein Response. Cancers 2020, 12, 401. [Google Scholar] [CrossRef]
- Pehar, M.; O’Riordan, K.J.; Burns-Cusato, M.; Andrzejewski, M.E.; del Alcazar, C.G.; Burger, C.; Scrable, H.; Puglielli, L. Altered Longevity-Assurance Activity of p53:p44 in the Mouse Causes Memory Loss, Neurodegeneration and Premature Death. Aging Cell 2010, 9, 174–190. [Google Scholar] [CrossRef] [PubMed]
- Pehar, M.; Ko, M.H.; Li, M.; Scrable, H.; Puglielli, L. P44, the “Longevity-Assurance” Isoform of P53, Regulates Tau Phosphorylation and Is Activated in an Age-Dependent Fashion. Aging Cell 2014, 13, 449–456. [Google Scholar] [CrossRef] [PubMed]
- Kubbutat, M.H.; Jones, S.N.; Vousden, K.H. Regulation of p53 Stability by Mdm2. Nature 1997, 387, 299–303. [Google Scholar] [CrossRef] [PubMed]
- Honda, R.; Tanaka, H.; Yasuda, H. Oncoprotein MDM2 Is a Ubiquitin Ligase E3 for Tumor Suppressor p53. FEBS Lett. 1997, 420, 25–27. [Google Scholar] [CrossRef]
- Sola, M.; Magrin, C.; Pedrioli, G.; Pinton, S.; Salvadè, A.; Papin, S.; Paganetti, P. Tau Affects P53 Function and Cell Fate during the DNA Damage Response. Commun. Biol. 2020, 3, 245. [Google Scholar] [CrossRef] [PubMed]
- Moll, U.M.; Petrenko, O. The MDM2-p53 Interaction. Mol. Cancer Res. 2003, 1, 1001–1008. [Google Scholar] [PubMed]
- Ciechanover, A.; Brundin, P. The Ubiquitin Proteasome System in Neurodegenerative Diseases: Sometimes the Chicken, Sometimes the Egg. Neuron 2003, 40, 427–446. [Google Scholar] [CrossRef]
- Alves-Rodrigues, A.; Gregori, L.; Figueiredo-Pereira, M.E. Ubiquitin, Cellular Inclusions and Their Role in Neurodegeneration. Trends Neurosci. 1998, 21, 516–520. [Google Scholar] [CrossRef]
- Youn, J.-Y.; Dunham, W.H.; Hong, S.J.; Knight, J.D.R.; Bashkurov, M.; Chen, G.I.; Bagci, H.; Rathod, B.; MacLeod, G.; Eng, S.W.M.; et al. High-Density Proximity Mapping Reveals the Subcellular Organization of mRNA-Associated Granules and Bodies. Mol. Cell 2018, 69, 517–532.e11. [Google Scholar] [CrossRef]
- Markmiller, S.; Soltanieh, S.; Server, K.L.; Mak, R.; Jin, W.; Fang, M.Y.; Luo, E.-C.; Krach, F.; Yang, D.; Sen, A.; et al. Context-Dependent and Disease-Specific Diversity in Protein Interactions within Stress Granules. Cell 2018, 172, 590–604.e13. [Google Scholar] [CrossRef]
- Markmiller, S.; Fulzele, A.; Higgins, R.; Leonard, M.; Yeo, G.W.; Bennett, E.J. Active Protein Neddylation or Ubiquitylation Is Dispensable for Stress Granule Dynamics. Cell Rep. 2019, 27, 1356–1363.e3. [Google Scholar] [CrossRef]
- Dao, T.P.; Kolaitis, R.-M.; Kim, H.J.; O’Donovan, K.; Martyniak, B.; Colicino, E.; Hehnly, H.; Taylor, J.P.; Castañeda, C.A. Ubiquitin Modulates Liquid-Liquid Phase Separation of UBQLN2 via Disruption of Multivalent Interactions. Mol. Cell 2018, 69, 965–978.e6. [Google Scholar] [CrossRef] [PubMed]
- Bedford, L.; Lowe, J.; Dick, L.R.; Mayer, R.J.; Brownell, J.E. Ubiquitin-like Protein Conjugation and the Ubiquitin-Proteasome System as Drug Targets. Nat. Rev. Drug Discov. 2011, 10, 29–46. [Google Scholar] [CrossRef] [PubMed]
- Gallego, L.D.; Schneider, M.; Mittal, C.; Romanauska, A.; Gudino Carrillo, R.M.; Schubert, T.; Pugh, B.F.; Köhler, A. Phase Separation Directs Ubiquitination of Gene-Body Nucleosomes. Nature 2020, 579, 592–597. [Google Scholar] [CrossRef] [PubMed]
- Tai, H.-C.; Schuman, E.M. Ubiquitin, the Proteasome and Protein Degradation in Neuronal Function and Dysfunction. Nat. Rev. Neurosci. 2008, 9, 826–838. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, Y.; Taguchi, K.; Tanaka, M. Ubiquitin, Autophagy and Neurodegenerative Diseases. Cells 2020, 9, 2022. [Google Scholar] [CrossRef]
- Park, C.-W.; Jung, B.-K.; Ryu, K.-Y. Reduced Free Ubiquitin Levels and Proteasome Activity in Cultured Neurons and Brain Tissues Treated with Amyloid Beta Aggregates. Mol. Brain 2020, 13, 89. [Google Scholar] [CrossRef] [PubMed]
- Bellia, F.; Lanza, V.; García-Viñuales, S.; Ahmed, I.M.M.; Pietropaolo, A.; Iacobucci, C.; Malgieri, G.; D’Abrosca, G.; Fattorusso, R.; Nicoletti, V.G.; et al. Ubiquitin Binds the Amyloid β Peptide and Interferes with Its Clearance Pathways. Chem. Sci. 2019, 10, 2732–2742. [Google Scholar] [CrossRef] [PubMed]
- Finley, D. Recognition and Processing of Ubiquitin-Protein Conjugates by the Proteasome. Annu. Rev. Biochem. 2009, 78, 477–513. [Google Scholar] [CrossRef]
- Benanti, J.A. Coordination of Cell Growth and Division by the Ubiquitin-Proteasome System. Semin. Cell Dev. Biol. 2012, 23, 492–498. [Google Scholar] [CrossRef] [PubMed]
- Orlowski, R.Z. The Role of the Ubiquitin-Proteasome Pathway in Apoptosis. Cell Death Differ. 1999, 6, 303–313. [Google Scholar] [CrossRef]
- Wójcik, C. Regulation of Apoptosis by the Ubiquitin and Proteasome Pathway. J. Cell Mol. Med. 2002, 6, 25–48. [Google Scholar] [CrossRef] [PubMed]
- Sharma, A.; Trivedi, A.K. Regulation of Apoptosis by E3 Ubiquitin Ligases in Ubiquitin Proteasome System. Cell Biol. Int. 2020, 44, 721–734. [Google Scholar] [CrossRef]
- Marfella, R.; D’Amico, M.; Esposito, K.; Baldi, A.; Di Filippo, C.; Siniscalchi, M.; Sasso, F.C.; Portoghese, M.; Cirillo, F.; Cacciapuoti, F.; et al. The Ubiquitin-Proteasome System and Inflammatory Activity in Diabetic Atherosclerotic Plaques: Effects of Rosiglitazone Treatment. Diabetes 2006, 55, 622–632. [Google Scholar] [CrossRef]
- Goetzke, C.C.; Ebstein, F.; Kallinich, T. Role of Proteasomes in Inflammation. J. Clin. Med. Res. 2021, 10, 1783. [Google Scholar] [CrossRef]
- Muratani, M.; Tansey, W.P. How the Ubiquitin-Proteasome System Controls Transcription. Nat. Rev. Mol. Cell Biol. 2003, 4, 192–201. [Google Scholar] [CrossRef] [PubMed]
- Geng, F.; Wenzel, S.; Tansey, W.P. Ubiquitin and Proteasomes in Transcription. Annu. Rev. Biochem. 2012, 81, 177–201. [Google Scholar] [CrossRef] [PubMed]
- Voutsadakis, I.A. The Ubiquitin-Proteasome System and Signal Transduction Pathways Regulating Epithelial Mesenchymal Transition of Cancer. J. Biomed. Sci. 2012, 19, 67. [Google Scholar] [CrossRef] [PubMed]
- Ciechanover, A.; Kwon, Y.T. Protein Quality Control by Molecular Chaperones in Neurodegeneration. Front. Neurosci. 2017, 11, 185. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Maldonado, M.A. The Ubiquitin-Proteasome System and Its Role in Inflammatory and Autoimmune Diseases. Cell Mol. Immunol. 2006, 3, 255–261. [Google Scholar] [PubMed]
- Hershko, A. The Ubiquitin System for Protein Degradation and Some of Its Roles in the Control of the Cell Division Cycle. Cell Death Differ. 2005, 12, 1191–1197. [Google Scholar] [CrossRef] [PubMed]
- Goldberg, A.L. ATP-Dependent Proteases in Prokaryotic and Eukaryotic Cells. Semin. Cell Biol. 1990, 1, 423–432. [Google Scholar]
- Baker, T.A.; Sauer, R.T. ATP-Dependent Proteases of Bacteria: Recognition Logic and Operating Principles. Trends Biochem. Sci. 2006, 31, 647–653. [Google Scholar] [CrossRef]
- Tomko Jr, R.J.; Hochstrasser, M. Molecular Architecture and Assembly of the Eukaryotic Proteasome. Annu. Rev. Biochem. 2013, 82, 415–445. [Google Scholar] [CrossRef]
- Sun, D.; Wu, R.; Zheng, J.; Li, P.; Yu, L. Polyubiquitin Chain-Induced p62 Phase Separation Drives Autophagic Cargo Segregation. Cell Res. 2018, 28, 405–415. [Google Scholar] [CrossRef] [PubMed]
- Yasuda, S.; Tsuchiya, H.; Kaiho, A.; Guo, Q.; Ikeuchi, K.; Endo, A.; Arai, N.; Ohtake, F.; Murata, S.; Inada, T.; et al. Stress- and Ubiquitylation-Dependent Phase Separation of the Proteasome. Nature 2020, 578, 296–300. [Google Scholar] [CrossRef]
- Dong, Y.; Zhang, S.; Wu, Z.; Li, X.; Wang, W.L.; Zhu, Y.; Stoilova-McPhie, S.; Lu, Y.; Finley, D.; Mao, Y. Cryo-EM Structures and Dynamics of Substrate-Engaged Human 26S Proteasome. Nature 2019, 565, 49–55. [Google Scholar] [CrossRef]
- Peth, A.; Nathan, J.A.; Goldberg, A.L. The ATP Costs and Time Required to Degrade Ubiquitinated Proteins by the 26 S Proteasome. J. Biol. Chem. 2013, 288, 29215–29222. [Google Scholar] [CrossRef]
- Mookerjee, S.A.; Gerencser, A.A.; Nicholls, D.G.; Brand, M.D. Quantifying Intracellular Rates of Glycolytic and Oxidative ATP Production and Consumption Using Extracellular Flux Measurements. J. Biol. Chem. 2017, 292, 7189–7207. [Google Scholar] [CrossRef]
- Schurr, A. Lactate, Not Pyruvate, Is the End Product of Glucose Metabolism via Glycolysis. In Carbohydrate; Caliskan, M., Kavakli, I.H., Oz, G.C., Eds.; IntechOpen: London, UK, 2017. [Google Scholar] [CrossRef]
- Gray, L.R.; Tompkins, S.C.; Taylor, E.B. Regulation of Pyruvate Metabolism and Human Disease. Cell Mol. Life Sci. 2014, 71, 2577–2604. [Google Scholar] [CrossRef]
- Park, S.; Jeon, J.H.; Min, B.K.; Ha, C.M.; Thoudam, T.; Park, B.Y.; Lee, I.K. Role of the Pyruvate Dehydrogenase Complex in Metabolic Remodeling: Differential Pyruvate Dehydrogenase Complex Functions in Metabolism. Diabetes Metab. J. 2018, 42, 270–281. [Google Scholar] [CrossRef]
- Atas, E.; Oberhuber, M.; Kenner, L. The Implications of PDK1-4 on Tumor Energy Metabolism, Aggressiveness and Therapy Resistance. Front. Oncol. 2020, 10, 583217. [Google Scholar] [CrossRef]
- Hall, C.N.; Klein-Flügge, M.C.; Howarth, C.; Attwell, D. Oxidative Phosphorylation, Not Glycolysis, Powers Presynaptic and Postsynaptic Mechanisms Underlying Brain Information Processing. J. Neurosci. 2012, 32, 8940–8951. [Google Scholar] [CrossRef] [PubMed]
- Jha, M.K.; Jeon, S.; Suk, K. Pyruvate Dehydrogenase Kinases in the Nervous System: Their Principal Functions in Neuronal-Glial Metabolic Interaction and Neuro-Metabolic Disorders. Curr. Neuropharmacol. 2012, 10, 393–403. [Google Scholar] [CrossRef]
- Blass, J.P.; Sheu, R.K.; Gibson, G.E. Inherent Abnormalities in Energy Metabolism in Alzheimer Disease. Interaction with Cerebrovascular Compromise. Ann. N. Y. Acad. Sci. 2000, 903, 204–221. [Google Scholar] [CrossRef]
- Yao, J.; Irwin, R.W.; Zhao, L.; Nilsen, J.; Hamilton, R.T.; Brinton, R.D. Mitochondrial Bioenergetic Deficit Precedes Alzheimer’s Pathology in Female Mouse Model of Alzheimer s Disease. Proc. Natl. Acad. Sci. USA 2009, 106, 14670–14675. [Google Scholar] [CrossRef]
- Marin, R.; Ramírez, C.M.; González, M.; González-Muñoz, E.; Zorzano, A.; Camps, M.; Alonso, R.; Díaz, M. Voltage-Dependent Anion Channel (VDAC) Participates in Amyloid Beta-Induced Toxicity and Interacts with Plasma Membrane Estrogen Receptor Alpha in Septal and Hippocampal Neurons. Mol. Membr. Biol. 2007, 24, 148–160. [Google Scholar] [CrossRef] [PubMed]
- Paschon, V.; Morena, B.C.; Correia, F.F.; Beltrame, G.R.; Dos Santos, G.B.; Cristante, A.F.; Kihara, A.H. VDAC1 Is Essential for Neurite Maintenance and the Inhibition of Its Oligomerization Protects Spinal Cord from Demyelination and Facilitates Locomotor Function Recovery after Spinal Cord Injury. Sci. Rep. 2019, 9, 14063. [Google Scholar] [CrossRef] [PubMed]
- Fernandez-Echevarria, C.; Díaz, M.; Ferrer, I.; Canerina-Amaro, A.; Marin, R. Aβ Promotes VDAC1 Channel Dephosphorylation in Neuronal Lipid Rafts. Relevance to the Mechanisms of Neurotoxicity in Alzheimer’s Disease. Neuroscience 2014, 278, 354–366. [Google Scholar] [CrossRef] [PubMed]
- Cesarini, E.; Cerioni, L.; Canonico, B.; Di Sario, G.; Guidarelli, A.; Lattanzi, D.; Savelli, D.; Guescini, M.; Nasoni, M.G.; Bigini, N.; et al. Melatonin Protects Hippocampal HT22 Cells from the Effects of Serum Deprivation Specifically Targeting Mitochondria. PLoS ONE 2018, 13, e0203001. [Google Scholar] [CrossRef]
- Nag, S.; Qin, J.; Srivenugopal, K.S.; Wang, M.; Zhang, R. The MDM2-p53 Pathway Revisited. J. Biomed. Res. 2013, 27, 254–271. [Google Scholar] [CrossRef]
- Song, J.; Ma, S.-J.; Luo, J.-H.; Zhang, H.; Wang, R.-X.; Liu, H.; Li, L.; Zhang, Z.-G.; Zhou, R.-X. Melatonin Induces the Apoptosis and Inhibits the Proliferation of Human Gastric Cancer Cells via Blockade of the AKT/MDM2 Pathway. Oncol. Rep. 2018, 39, 1975–1983. [Google Scholar] [CrossRef] [PubMed]
- Haronikova, L.; Olivares-Illana, V.; Wang, L.; Karakostis, K.; Chen, S.; Fåhraeus, R. The p53 mRNA: An Integral Part of the Cellular Stress Response. Nucleic Acids Res. 2019, 47, 3257–3271. [Google Scholar] [CrossRef]
- Kasteri, J.; Das, D.; Zhong, X.; Persaud, L.; Francis, A.; Muharam, H.; Sauane, M. Translation Control by p53. Cancers 2018, 10, 133. [Google Scholar] [CrossRef]
- Zhang, X.-D.; Qin, Z.-H.; Wang, J. The Role of p53 in Cell Metabolism. Acta Pharmacol. Sin. 2010, 31, 1208–1212. [Google Scholar] [CrossRef]
- Zhang, C.; Liu, J.; Liang, Y.; Wu, R.; Zhao, Y.; Hong, X.; Lin, M.; Yu, H.; Liu, L.; Levine, A.J.; et al. Tumour-Associated Mutant p53 Drives the Warburg Effect. Nat. Commun. 2013, 4, 2935. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.-R.; Roe, J.-S.; Lee, J.-E.; Cho, E.-J.; Youn, H.-D. p53 Regulates Glucose Metabolism by miR-34a. Biochem. Biophys. Res. Commun. 2013, 437, 225–231. [Google Scholar] [CrossRef] [PubMed]
- Kawauchi, K.; Araki, K.; Tobiume, K.; Tanaka, N. p53 Regulates Glucose Metabolism through an IKK-NF-kappaB Pathway and Inhibits Cell Transformation. Nat. Cell Biol. 2008, 10, 611–618. [Google Scholar] [CrossRef] [PubMed]
- Ma, W.; Sung, H.J.; Park, J.Y.; Matoba, S.; Hwang, P.M. A Pivotal Role for p53: Balancing Aerobic Respiration and Glycolysis. J. Bioenerg. Biomembr. 2007, 39, 243–246. [Google Scholar] [CrossRef] [PubMed]
- Contractor, T.; Harris, C.R. p53 Negatively Regulates Transcription of the Pyruvate Dehydrogenase Kinase Pdk2. Cancer Res. 2012, 72, 560–567. [Google Scholar] [CrossRef]
- Mediavilla, M.D.; Cos, S.; Sánchez-Barceló, E.J. Melatonin Increases p53 and p21WAF1 Expression in MCF-7 Human Breast Cancer Cells in Vitro. Life Sci. 1999, 65, 415–420. [Google Scholar] [CrossRef]
- Kim, C.H.; Yoo, Y.-M. Melatonin Induces Apoptotic Cell Death via p53 in LNCaP Cells. Korean J. Physiol. Pharmacol. 2010, 14, 365–369. [Google Scholar] [CrossRef]
- Ma, L.; Liu, Q.; Tian, M.; Tian, X.; Gao, L. Mechanisms of Melatonin in Anti-Aging and Its Regulation Effects in Radiation-Induced Premature Senescence. Radiat. Med. Prot. 2021, 2, 33–37. [Google Scholar] [CrossRef]
- Santoro, R.; Marani, M.; Blandino, G.; Muti, P.; Strano, S. Melatonin Triggers p53Ser Phosphorylation and Prevents DNA Damage Accumulation. Oncogene 2012, 31, 2931–2942. [Google Scholar] [CrossRef]
- Santoro, R.; Mori, F.; Marani, M.; Grasso, G.; Cambria, M.A.; Blandino, G.; Muti, P.; Strano, S. Blockage of Melatonin Receptors Impairs p53-Mediated Prevention of DNA Damage Accumulation. Carcinogenesis 2013, 34, 1051–1061. [Google Scholar] [CrossRef]
- Proietti, S.; Cucina, A.; Dobrowolny, G.; D’Anselmi, F.; Dinicola, S.; Masiello, M.G.; Pasqualato, A.; Palombo, A.; Morini, V.; Reiter, R.J.; et al. Melatonin down-Regulates MDM2 Gene Expression and Enhances p53 Acetylation in MCF-7 Cells. J. Pineal. Res. 2014, 57, 120–129. [Google Scholar] [CrossRef] [PubMed]
- Carr, M.I.; Roderick, J.E.; Gannon, H.S.; Kelliher, M.A.; Jones, S.N. Mdm2 Phosphorylation Regulates Its Stability and Has Contrasting Effects on Oncogene and Radiation-Induced Tumorigenesis. Cell Rep. 2016, 16, 2618–2629. [Google Scholar] [CrossRef] [PubMed]
- Facchin, S.; Ruzzene, M.; Peggion, C.; Sartori, G.; Carignani, G.; Marin, O.; Brustolon, F.; Lopreiato, R.; Pinna, L.A. Phosphorylation and Activation of the Atypical Kinase p53-Related Protein Kinase (PRPK) by Akt/PKB. Cell. Mol. Life Sci. 2007, 64, 2680–2689. [Google Scholar] [CrossRef] [PubMed]
- Shieh, S.Y.; Ikeda, M.; Taya, Y.; Prives, C. DNA Damage-Induced Phosphorylation of p53 Alleviates Inhibition by MDM2. Cell 1997, 91, 325–334. [Google Scholar] [CrossRef]
- Loughery, J.; Cox, M.; Smith, L.M.; Meek, D.W. Critical Role for p53-Serine 15 Phosphorylation in Stimulating Transactivation at p53-Responsive Promoters. Nucleic Acids Res. 2014, 42, 7666–7680. [Google Scholar] [CrossRef]
- Wade, M.; Li, Y.C.; Matani, A.S.; Braun, S.M.G.; Milanesi, F.; Rodewald, L.W.; Wahl, G.M. Functional Analysis and Consequences of Mdm2 E3 Ligase Inhibition in Human Tumor Cells. Oncogene 2012, 31, 4789–4797. [Google Scholar] [CrossRef]
- Hou, H.; Sun, D.; Zhang, X. The Role of MDM2 Amplification and Overexpression in Therapeutic Resistance of Malignant Tumors. Cancer Cell Int. 2019, 19, 216. [Google Scholar] [CrossRef]
- Gottlieb, T.M.; Leal, J.F.M.; Seger, R.; Taya, Y.; Oren, M. Cross-Talk between Akt, p53 and Mdm2: Possible Implications for the Regulation of Apoptosis. Oncogene 2002, 21, 1299–1303. [Google Scholar] [CrossRef] [PubMed]
- Ito, A.; Lai, C.H.; Zhao, X.; Saito, S.; Hamilton, M.H.; Appella, E.; Yao, T.P. p300/CBP-Mediated p53 Acetylation Is Commonly Induced by p53-Activating Agents and Inhibited by MDM2. EMBO J. 2001, 20, 1331–1340. [Google Scholar] [CrossRef] [PubMed]
- Bouras, T.; Fu, M.; Sauve, A.A.; Wang, F.; Quong, A.A.; Perkins, N.D.; Hay, R.T.; Gu, W.; Pestell, R.G. SIRT1 Deacetylation and Repression of p300 Involves Lysine Residues 1020/1024 within the Cell Cycle Regulatory Domain 1. J. Biol. Chem. 2005, 280, 10264–10276. [Google Scholar] [CrossRef]
- Lohrum, M.A.E.; Ludwig, R.L.; Kubbutat, M.H.G.; Hanlon, M.; Vousden, K.H. Regulation of HDM2 Activity by the Ribosomal Protein L11. Cancer Cell 2003, 3, 577–587. [Google Scholar] [CrossRef]
- Bursać, S.; Brdovčak, M.C.; Pfannkuchen, M.; Orsolić, I.; Golomb, L.; Zhu, Y.; Katz, C.; Daftuar, L.; Grabušić, K.; Vukelić, I.; et al. Mutual Protection of Ribosomal Proteins L5 and L11 from Degradation Is Essential for p53 Activation upon Ribosomal Biogenesis Stress. Proc. Natl. Acad. Sci. USA 2012, 109, 20467–20472. [Google Scholar] [CrossRef]
- Zhu, Y.; Poyurovsky, M.V.; Li, Y.; Biderman, L.; Stahl, J.; Jacq, X.; Prives, C. Ribosomal Protein S7 Is Both a Regulator and a Substrate of MDM2. Mol. Cell 2009, 35, 316–326. [Google Scholar] [CrossRef]
- Dai, M.-S.; Zeng, S.X.; Jin, Y.; Sun, X.-X.; David, L.; Lu, H. Ribosomal Protein L23 Activates p53 by Inhibiting MDM2 Function in Response to Ribosomal Perturbation but Not to Translation Inhibition. Mol. Cell. Biol. 2004, 24, 7654–7668. [Google Scholar] [CrossRef] [PubMed]
- Jin, A.; Itahana, K.; O’Keefe, K.; Zhang, Y. Inhibition of HDM2 and Activation of p53 by Ribosomal Protein L23. Mol. Cell. Biol. 2004, 24, 7669–7680. [Google Scholar] [CrossRef]
- Dai, M.-S.; Lu, H. Inhibition of MDM2-Mediated p53 Ubiquitination and Degradation by Ribosomal Protein L5. J. Biol. Chem. 2004, 279, 44475–44482. [Google Scholar] [CrossRef]
- Liu, Y.; Deisenroth, C.; Zhang, Y. RP-MDM2-p53 Pathway: Linking Ribosomal Biogenesis and Tumor Surveillance. Trends Cancer Res. 2016, 2, 191–204. [Google Scholar] [CrossRef] [PubMed]
- Sha, Z.; Blyszcz, T.; González-Prieto, R.; Vertegaal, A.C.O.; Goldberg, A.L. Inhibiting Ubiquitination Causes an Accumulation of SUMOylated Newly Synthesized Nuclear Proteins at PML Bodies. J. Biol. Chem. 2019, 294, 15218–15234. [Google Scholar] [CrossRef] [PubMed]
- Bergink, S.; Jentsch, S. Principles of Ubiquitin and SUMO Modifications in DNA Repair. Nature 2009, 458, 461–467. [Google Scholar] [CrossRef] [PubMed]
- Yang, K.; Moldovan, G.-L.; Vinciguerra, P.; Murai, J.; Takeda, S.; D’Andrea, A.D. Regulation of the Fanconi Anemia Pathway by a SUMO-like Delivery Network. Genes Dev. 2011, 25, 1847–1858. [Google Scholar] [CrossRef]
- Jackson, S.P.; Durocher, D. Regulation of DNA Damage Responses by Ubiquitin and SUMO. Mol. Cell 2013, 49, 795–807. [Google Scholar] [CrossRef]
- Pellegrino, S.; Altmeyer, M. Interplay between Ubiquitin, SUMO, and Poly(ADP-Ribose) in the Cellular Response to Genotoxic Stress. Front. Genet. 2016, 7, 63. [Google Scholar] [CrossRef]
- Lee, C.C.; Li, B.; Yu, H.; Matunis, M.J. A Method for SUMO Modification of Proteins in Vitro. Bio Protoc 2018, 8, e3033. [Google Scholar] [CrossRef]
- Gareau, J.R.; Lima, C.D. The SUMO Pathway: Emerging Mechanisms That Shape Specificity, Conjugation and Recognition. Nat. Rev. Mol. Cell Biol. 2010, 11, 861–871. [Google Scholar] [CrossRef]
- Van Wijk, S.J.L.; Müller, S.; Dikic, I. Shared and Unique Properties of Ubiquitin and SUMO Interaction Networks in DNA Repair. Genes Dev. 2011, 25, 1763–1769. [Google Scholar] [CrossRef][Green Version]
- Lamoliatte, F.; McManus, F.P.; Maarifi, G.; Chelbi-Alix, M.K.; Thibault, P. Uncovering the SUMOylation and Ubiquitylation Crosstalk in Human Cells Using Sequential Peptide Immunopurification. Nat. Commun. 2017, 8, 14109. [Google Scholar] [CrossRef]
- Gill, G. SUMO and Ubiquitin in the Nucleus: Different Functions, Similar Mechanisms? Genes Dev. 2004, 18, 2046–2059. [Google Scholar] [CrossRef]
- Ulrich, H.D. Mutual Interactions between the SUMO and Ubiquitin Systems: A Plea of No Contest. Trends Cell Biol. 2005, 15, 525–532. [Google Scholar] [CrossRef]
- Sriramachandran, A.M.; Dohmen, R.J. SUMO-Targeted Ubiquitin Ligases. Biochim. Biophys. Acta 2014, 1843, 75–85. [Google Scholar] [CrossRef]
- Cubeñas-Potts, C.; Matunis, M.J. SUMO: A Multifaceted Modifier of Chromatin Structure and Function. Dev. Cell 2013, 24, 1–12. [Google Scholar] [CrossRef]
- Cardone, L.; Hirayama, J.; Giordano, F.; Tamaru, T.; Palvimo, J.J.; Sassone-Corsi, P. Circadian Clock Control by SUMOylation of BMAL1. Science 2005, 309, 1390–1394. [Google Scholar] [CrossRef] [PubMed]
- Berndt, A.; Wilkinson, K.A.; Henley, J.M. Regulation of Neuronal Protein Trafficking and Translocation by SUMOylation. Biomolecules 2012, 2, 256–268. [Google Scholar] [CrossRef] [PubMed]
- Wilkinson, K.A.; Nakamura, Y.; Henley, J.M. Targets and Consequences of Protein SUMOylation in Neurons. Brain Res. Rev. 2010, 64, 195–212. [Google Scholar] [CrossRef] [PubMed]
- Luo, J.; Ashikaga, E.; Rubin, P.P.; Heimann, M.J.; Hildick, K.L.; Bishop, P.; Girach, F.; Josa-Prado, F.; Tang, L.T.H.; Carmichael, R.E.; et al. Receptor Trafficking and the Regulation of Synaptic Plasticity by SUMO. Neuromolecular Med. 2013, 15, 692–706. [Google Scholar] [CrossRef]
- Meinecke, I.; Cinski, A.; Baier, A.; Peters, M.A.; Dankbar, B.; Wille, A.; Drynda, A.; Mendoza, H.; Gay, R.E.; Hay, R.T.; et al. Modification of Nuclear PML Protein by SUMO-1 Regulates Fas-Induced Apoptosis in Rheumatoid Arthritis Synovial Fibroblasts. Proc. Natl. Acad. Sci. USA 2007, 104, 5073–5078. [Google Scholar] [CrossRef]
- Liebelt, F.; Vertegaal, A.C.O. Ubiquitin-Dependent and Independent Roles of SUMO in Proteostasis. Am. J. Physiol. Cell Physiol. 2016, 311, C284–C296. [Google Scholar] [CrossRef]
- Song, J.; Durrin, L.K.; Wilkinson, T.A.; Krontiris, T.G.; Chen, Y. Identification of a SUMO-Binding Motif That Recognizes SUMO-Modified Proteins. Proc. Natl. Acad. Sci. USA. 2004, 101, 14373–14378. [Google Scholar] [CrossRef] [PubMed]
- Kerscher, O. SUMO Junction-What’s Your Function? New Insights through SUMO-Interacting Motifs. EMBO Rep. 2007, 8, 550–555. [Google Scholar] [CrossRef] [PubMed]
- González-Prieto, R.; Eifler-Olivi, K.; Claessens, L.A.; Willemstein, E.; Xiao, Z.; Talavera Ormeno, C.M.P.; Ovaa, H.; Ulrich, H.D.; Vertegaal, A.C.O. Global Non-Covalent SUMO Interaction Networks Reveal SUMO-Dependent Stabilization of the Non-Homologous End Joining Complex. Cell Rep. 2021, 34, 108691. [Google Scholar] [CrossRef] [PubMed]
- Nacerddine, K.; Lehembre, F.; Bhaumik, M.; Artus, J.; Cohen-Tannoudji, M.; Babinet, C.; Pandolfi, P.P.; Dejean, A. The SUMO Pathway Is Essential for Nuclear Integrity and Chromosome Segregation in Mice. Dev. Cell 2005, 9, 769–779. [Google Scholar] [CrossRef]
- Jin, J. Interplay between Ubiquitylation and SUMOylation: Empowered by Phase Separation. J. Biol. Chem. 2019, 294, 15235–15236. [Google Scholar] [CrossRef]
- Keiten-Schmitz, J.; Röder, L.; Hornstein, E.; Müller-McNicoll, M.; Müller, S. SUMO: Glue or Solvent for Phase-Separated Ribonucleoprotein Complexes and Molecular Condensates? Front. Mol. Biosci. 2021, 8, 673038. [Google Scholar] [CrossRef]
- Mattsson, K.; Pokrovskaja, K.; Kiss, C.; Klein, G.; Szekely, L. Proteins Associated with the Promyelocytic Leukemia Gene Product (PML)-Containing Nuclear Body Move to the Nucleolus upon Inhibition of Proteasome-Dependent Protein Degradation. Proc. Natl. Acad. Sci. USA 2001, 98, 1012–1017. [Google Scholar] [CrossRef] [PubMed]
- Mediani, L.; Guillén-Boixet, J.; Alberti, S.; Carra, S. Nucleoli and Promyelocytic Leukemia Protein (PML) Bodies Are Phase Separated Nuclear Protein Quality Control Compartments for Misfolded Proteins. Mol. Cell Oncol. 2019, 6, e1415624. [Google Scholar] [CrossRef]
- Schubert, U.; Antón, L.C.; Gibbs, J.; Norbury, C.C.; Yewdell, J.W.; Bennink, J.R. Rapid Degradation of a Large Fraction of Newly Synthesized Proteins by Proteasomes. Nature 2000, 404, 770–774. [Google Scholar] [CrossRef] [PubMed]
- Walsh, I.M.; Bowman, M.A.; Soto Santarriaga, I.F.; Rodriguez, A.; Clark, P.L. Synonymous Codon Substitutions Perturb Cotranslational Protein Folding in Vivo and Impair Cell Fitness. Proc. Natl. Acad. Sci. USA 2020, 117, 3528–3534. [Google Scholar] [CrossRef] [PubMed]
- Drummond, D.A.; Wilke, C.O. The Evolutionary Consequences of Erroneous Protein Synthesis. Nat. Rev. Genet. 2009, 10, 715–724. [Google Scholar] [CrossRef] [PubMed]
- Faure, G.; Ogurtsov, A.Y.; Shabalina, S.A.; Koonin, E.V. Adaptation of mRNA Structure to Control Protein Folding. RNA Biol. 2017, 14, 1649–1654. [Google Scholar] [CrossRef]
- Gout, J.-F.; Li, W.; Fritsch, C.; Li, A.; Haroon, S.; Singh, L.; Hua, D.; Fazelinia, H.; Smith, Z.; Seeholzer, S.; et al. The Landscape of Transcription Errors in Eukaryotic Cells. Sci. Adv. 2017, 3, e1701484. [Google Scholar] [CrossRef]
- Jamar, N.H.; Kritsiligkou, P.; Grant, C.M. Loss of mRNA Surveillance Pathways Results in Widespread Protein Aggregation. Sci. Rep. 2018, 8, 3894. [Google Scholar] [CrossRef]
- Chen, G.-F.; Xu, T.-H.; Yan, Y.; Zhou, Y.-R.; Jiang, Y.; Melcher, K.; Xu, H.E. Amyloid Beta: Structure, Biology and Structure-Based Therapeutic Development. Acta Pharmacol. Sin. 2017, 38, 1205–1235. [Google Scholar] [CrossRef]
- Hipp, M.S.; Park, S.-H.; Hartl, F.U. Proteostasis Impairment in Protein-Misfolding and -Aggregation Diseases. Trends Cell Biol. 2014, 24, 506–514. [Google Scholar] [CrossRef]
- Wu, H. Higher-Order Assemblies in a New Paradigm of Signal Transduction. Cell 2013, 153, 287–292. [Google Scholar] [CrossRef]
- Kuroda, Y. Biophysical Studies of Protein Solubility and Amorphous Aggregation by Systematic Mutational Analysis and a Helical Polymerization Model. Biophys. Rev. 2018, 10, 473–480. [Google Scholar] [CrossRef]
- Koo, E.H.; Lansbury, P.T.; Kelly, J.W. Amyloid Diseases: Abnormal Protein Aggregation in Neurodegeneration. Proc. Natl. Acad. Sci. USA 1999, 96, 9989–9990. [Google Scholar] [CrossRef]
- Dorval, V.; Fraser, P.E. SUMO on the Road to Neurodegeneration. Biochim. Biophys. Acta 2007, 1773, 694–706. [Google Scholar] [CrossRef] [PubMed]
- Yau, T.-Y.; Molina, O.; Courey, A.J. SUMOylation in Development and Neurodegeneration. Development 2020, 147, dev175703. [Google Scholar] [CrossRef] [PubMed]
- Um, J.W.; Min, D.S.; Rhim, H.; Kim, J.; Paik, S.R.; Chung, K.C. Parkin Ubiquitinates and Promotes the Degradation of RanBP2*. J. Biol. Chem. 2006, 281, 3595–3603. [Google Scholar] [CrossRef]
- Vabulas, R.M.; Raychaudhuri, S.; Hayer-Hartl, M.; Hartl, F.U. Protein Folding in the Cytoplasm and the Heat Shock Response. Cold Spring Harb. Perspect. Biol. 2010, 2, a004390. [Google Scholar] [CrossRef]
- Gidalevitz, T.; Prahlad, V.; Morimoto, R.I. The Stress of Protein Misfolding: From Single Cells to Multicellular Organisms. Cold Spring Harb. Perspect. Biol. 2011, 3, a009704. [Google Scholar] [CrossRef]
- Ruddock, L.W.; Klappa, P. Oxidative Stress: Protein Folding with a Novel Redox Switch. Curr. Biol. 1999, 9, R400–R402. [Google Scholar] [CrossRef][Green Version]
- Stadmiller, S.S.; Gorensek-Benitez, A.H.; Guseman, A.J.; Pielak, G.J. Osmotic Shock Induced Protein Destabilization in Living Cells and Its Reversal by Glycine Betaine. J. Mol. Biol. 2017, 429, 1155–1161. [Google Scholar] [CrossRef]
- Protter, D.S.W.; Parker, R. Principles and Properties of Stress Granules. Trends Cell Biol. 2016, 26, 668–679. [Google Scholar] [CrossRef] [PubMed]
- Mittag, T.; Parker, R. Multiple Modes of Protein-Protein Interactions Promote RNP Granule Assembly. J. Mol. Biol. 2018, 430, 4636–4649. [Google Scholar] [CrossRef]
- Boeynaems, S.; Alberti, S.; Fawzi, N.L.; Mittag, T.; Polymenidou, M.; Rousseau, F.; Schymkowitz, J.; Shorter, J.; Wolozin, B.; Van Den Bosch, L.; et al. Protein Phase Separation: A New Phase in Cell Biology. Trends Cell Biol. 2018, 28, 420–435. [Google Scholar] [CrossRef]
- Tolay, N.; Buchberger, A. Comparative Profiling of Stress Granule Clearance Reveals Differential Contributions of the Ubiquitin System. Life Sci Alliance 2021, 4. [Google Scholar] [CrossRef] [PubMed]
- Keiten-Schmitz, J.; Wagner, K.; Piller, T.; Kaulich, M.; Alberti, S.; Müller, S. The Nuclear SUMO-Targeted Ubiquitin Quality Control Network Regulates the Dynamics of Cytoplasmic Stress Granules. Mol. Cell 2020, 79, 54–67.e7. [Google Scholar] [CrossRef] [PubMed]
- Jongjitwimol, J.; Baldock, R.A.; Morley, S.J.; Watts, F.Z. Sumoylation of eIF4A2 Affects Stress Granule Formation. J. Cell Sci. 2016, 129, 2407–2415. [Google Scholar] [CrossRef]
- Liu, Y.-C.; Hsu, W.-L.; Ma, Y.-L.; Lee, E.H.Y. Melatonin Induction of APP Intracellular Domain 50 SUMOylation Alleviates AD through Enhanced Transcriptional Activation and Aβ Degradation. Mol. Ther. 2021, 29, 376–395. [Google Scholar] [CrossRef]
- Zhang, Y.-Q.; Sarge, K.D. Sumoylation of Amyloid Precursor Protein Negatively Regulates Abeta Aggregate Levels. Biochem. Biophys. Res. Commun. 2008, 374, 673–678. [Google Scholar] [CrossRef]
- Agbor, T.A.; Taylor, C.T. SUMO, Hypoxia and the Regulation of Metabolism. Biochem. Soc. Trans. 2008, 36 Pt 3, 445–448. [Google Scholar] [CrossRef]
- Lee, Y.J.; Castri, P.; Bembry, J.; Maric, D.; Auh, S.; Hallenbeck, J.M. SUMOylation Participates in Induction of Ischemic Tolerance. J. Neurochem. 2009, 109, 257–267. [Google Scholar] [CrossRef] [PubMed]
- Bossis, G.; Melchior, F. Regulation of SUMOylation by Reversible Oxidation of SUMO Conjugating Enzymes. Mol. Cell 2006, 21, 349–357. [Google Scholar] [CrossRef]
- Silveirinha, V.; Stephens, G.J.; Cimarosti, H. Molecular Targets Underlying SUMO-Mediated Neuroprotection in Brain Ischemia. J. Neurochem. 2013, 127, 580–591. [Google Scholar] [CrossRef]
- Lee, L.; Sakurai, M.; Matsuzaki, S.; Arancio, O.; Fraser, P. SUMO and Alzheimer’s Disease. Neuromolecular Med. 2013, 15, 720–736. [Google Scholar] [CrossRef]
- Boulanger, M.; Chakraborty, M.; Tempé, D.; Piechaczyk, M.; Bossis, G. SUMO and Transcriptional Regulation: The Lessons of Large-Scale Proteomic, Modifomic and Genomic Studies. Molecules 2021, 26, 828. [Google Scholar] [CrossRef] [PubMed]
- Joyce, G.F. RNA Evolution and the Origins of Life. Nature 1989, 338, 217–224. [Google Scholar] [CrossRef]
- Joyce, G.F. The Antiquity of RNA-Based Evolution. Nature 2002, 418, 214–221. [Google Scholar] [CrossRef] [PubMed]
- Robertson, M.P.; Joyce, G.F. The Origins of the RNA World. Cold Spring Harb. Perspect. Biol. 2012, 4, a003608. [Google Scholar] [CrossRef]
- Hawkins, P.G.; Morris, K.V. RNA and Transcriptional Modulation of Gene Expression. Cell Cycle 2008, 7, 602–607. [Google Scholar] [CrossRef] [PubMed]
- Morris, K.V. The Emerging Role of RNA in the Regulation of Gene Transcription in Human Cells. Semin. Cell Dev. Biol. 2011, 22, 351–358. [Google Scholar] [CrossRef] [PubMed]
- Payne, J.L.; Khalid, F.; Wagner, A. RNA-Mediated Gene Regulation Is Less Evolvable than Transcriptional Regulation. Proc. Natl. Acad. Sci. USA 2018, 115, E3481–E3490. [Google Scholar] [CrossRef]
- Gott, J.M.; Emeson, R.B. Functions and Mechanisms of RNA Editing. Annu. Rev. Genet. 2000, 34, 499–531. [Google Scholar] [CrossRef]
- Gilbert, W.V.; Bell, T.A.; Schaening, C. Messenger RNA Modifications: Form, Distribution, and Function. Science 2016, 352, 1408–1412. [Google Scholar] [CrossRef]
- Szymański, M.; Barciszewska, M.Z.; Zywicki, M.; Barciszewski, J. Noncoding RNA Transcripts. J. Appl. Genet. 2003, 44, 1–19. [Google Scholar] [PubMed]
- Catalanotto, C.; Cogoni, C.; Zardo, G. MicroRNA in Control of Gene Expression: An Overview of Nuclear Functions. Int. J. Mol. Sci. 2016, 17, 1712. [Google Scholar] [CrossRef] [PubMed]
- Patil, V.S.; Zhou, R.; Rana, T.M. Gene Regulation by Non-Coding RNAs. Crit. Rev. Biochem. Mol. Biol. 2014, 49, 16–32. [Google Scholar] [CrossRef]
- Statello, L.; Guo, C.-J.; Chen, L.-L.; Huarte, M. Gene Regulation by Long Non-Coding RNAs and Its Biological Functions. Nat. Rev. Mol. Cell Biol. 2021, 22, 96–118. [Google Scholar] [CrossRef]
- Potashkin, J.A.; Bottero, V.; Santiago, J.A.; Quinn, J.P. Computational Identification of Key Genes That May Regulate Gene Expression Reprogramming in Alzheimer’s Patients. PLoS ONE 2019, 14, e0222921. [Google Scholar] [CrossRef]
- He, C. Grand Challenge Commentary: RNA Epigenetics? Nat. Chem. Biol. 2010, 6, 863–865. [Google Scholar] [CrossRef]
- Seo, K.W.; Kleiner, R.E. Mechanisms of Epitranscriptomic Gene Regulation. Biopolymers 2021, 112, e23403. [Google Scholar] [CrossRef]
- Aumiller, W.M.; Pir Cakmak, F.; Davis, B.W.; Keating, C.D. RNA-Based Coacervates as a Model for Membraneless Organelles: Formation, Properties, and Interfacial Liposome Assembly. Langmuir 2016, 32, 10042–10053. [Google Scholar] [CrossRef]
- Peng, L.; Li, E.-M.; Xu, L.-Y. From Start to End: Phase Separation and Transcriptional Regulation. Biochim. Biophys. Acta Gene Regul. Mech. 2020, 1863, 194641. [Google Scholar] [CrossRef]
- Campos-Melo, D.; Hawley, Z.C.E.; Droppelmann, C.A.; Strong, M.J. The Integral Role of RNA in Stress Granule Formation and Function. Front. Cell Dev. Biol. 2021, 9, 621779. [Google Scholar] [CrossRef] [PubMed]
- Sanchez de Groot, N.; Armaos, A.; Graña-Montes, R.; Alriquet, M.; Calloni, G.; Vabulas, R.M.; Tartaglia, G.G. RNA Structure Drives Interaction with Proteins. Nat. Commun. 2019, 10, 3246. [Google Scholar] [CrossRef] [PubMed]
- Colvin, V.L.; Kulinowski, K.M. Nanoparticles as Catalysts for Protein Fibrillation. Proc. Natl. Acad. Sci. USA 2007, 104, 8679–8680. [Google Scholar] [CrossRef] [PubMed]
- Brambilla, D.; Le Droumaguet, B.; Nicolas, J.; Hashemi, S.H.; Wu, L.-P.; Moghimi, S.M.; Couvreur, P.; Andrieux, K. Nanotechnologies for Alzheimer’s Disease: Diagnosis, Therapy, and Safety Issues. Nanomedicine 2011, 7, 521–540. [Google Scholar] [CrossRef] [PubMed]
- Conlon, E.G.; Manley, J.L. RNA-Binding Proteins in Neurodegeneration: Mechanisms in Aggregate. Genes Dev. 2017, 31, 1509–1528. [Google Scholar] [CrossRef]
- Maziuk, B.; Ballance, H.I.; Wolozin, B. Dysregulation of RNA Binding Protein Aggregation in Neurodegenerative Disorders. Front. Mol. Neurosci. 2017, 10, 89. [Google Scholar] [CrossRef]
- Kinoshita, C.; Kubota, N.; Aoyama, K. Interplay of RNA-Binding Proteins and microRNAs in Neurodegenerative Diseases. Int. J. Mol. Sci. 2021, 22, 5292. [Google Scholar] [CrossRef]
- Anders, M.; Chelysheva, I.; Goebel, I.; Trenkner, T.; Zhou, J.; Mao, Y.; Verzini, S.; Qian, S.-B.; Ignatova, Z. Dynamic m6A Methylation Facilitates mRNA Triaging to Stress Granules. Life Sci. Alliance 2018, 1, e201800113. [Google Scholar] [CrossRef]
- Li, A.; Chen, Y.-S.; Ping, X.-L.; Yang, X.; Xiao, W.; Yang, Y.; Sun, H.-Y.; Zhu, Q.; Baidya, P.; Wang, X.; et al. Cytoplasmic m6A Reader YTHDF3 Promotes mRNA Translation. Cell Res. 2017, 27, 444–447. [Google Scholar] [CrossRef]
- Rajecka, V.; Skalicky, T.; Vanacova, S. The Role of RNA Adenosine Demethylases in the Control of Gene Expression. Biochim. Biophys. Acta Gene Regul. Mech. 2019, 1862, 343–355. [Google Scholar] [CrossRef]
- Wang, X.; Lu, Z.; Gomez, A.; Hon, G.C.; Yue, Y.; Han, D.; Fu, Y.; Parisien, M.; Dai, Q.; Jia, G.; et al. N6-Methyladenosine-Dependent Regulation of Messenger RNA Stability. Nature 2014, 505, 117–120. [Google Scholar] [CrossRef]
- Wang, X.; Zhao, B.S.; Roundtree, I.A.; Lu, Z.; Han, D.; Ma, H.; Weng, X.; Chen, K.; Shi, H.; He, C. N(6)-Methyladenosine Modulates Messenger RNA Translation Efficiency. Cell 2015, 161, 1388–1399. [Google Scholar] [CrossRef] [PubMed]
- He, L.; Li, H.; Wu, A.; Peng, Y.; Shu, G.; Yin, G. Functions of N6-Methyladenosine and Its Role in Cancer. Mol. Cancer 2019, 18, 176. [Google Scholar] [CrossRef]
- Dai, D.; Wang, H.; Zhu, L.; Jin, H.; Wang, X. N6-Methyladenosine Links RNA Metabolism to Cancer Progression. Cell Death Dis. 2018, 9, 124. [Google Scholar] [CrossRef] [PubMed]
- Liu, N.; Dai, Q.; Zheng, G.; He, C.; Parisien, M.; Pan, T. N(6)-Methyladenosine-Dependent RNA Structural Switches Regulate RNA-Protein Interactions. Nature 2015, 518, 560–564. [Google Scholar] [CrossRef]
- Boo, S.H.; Kim, Y.K. The Emerging Role of RNA Modifications in the Regulation of mRNA Stability. Exp. Mol. Med. 2020, 52, 400–408. [Google Scholar] [CrossRef]
- Liu, L.; Wang, Y.; Wu, J.; Liu, J.; Qin, Z.; Fan, H. N6-Methyladenosine: A Potential Breakthrough for Human Cancer. Mol. Ther. Nucleic Acids 2020, 19, 804–813. [Google Scholar] [CrossRef]
- Zhu, Z.-M.; Huo, F.-C.; Pei, D.-S. Function and Evolution of RNA N6-Methyladenosine Modification. Int. J. Biol. Sci. 2020, 16, 1929–1940. [Google Scholar] [CrossRef]
- Winkler, R.; Gillis, E.; Lasman, L.; Safra, M.; Geula, S.; Soyris, C.; Nachshon, A.; Tai-Schmiedel, J.; Friedman, N.; Le-Trilling, V.T.K.; et al. m6A Modification Controls the Innate Immune Response to Infection by Targeting Type I Interferons. Nat. Immunol. 2019, 20, 173–182. [Google Scholar] [CrossRef]
- Gao, Y.; Vasic, R.; Song, Y.; Teng, R.; Liu, C.; Gbyli, R.; Biancon, G.; Nelakanti, R.; Lobben, K.; Kudo, E.; et al. m6A Modification Prevents Formation of Endogenous Double-Stranded RNAs and Deleterious Innate Immune Responses during Hematopoietic Development. Immunity 2020, 52, 1007–1021.e8. [Google Scholar] [CrossRef]
- Liu, C.; Yang, Z.; Li, R.; Wu, Y.; Chi, M.; Gao, S.; Sun, X.; Meng, X.; Wang, B. Potential Roles of N6-Methyladenosine (m6A) in Immune Cells. J. Transl. Med. 2021, 19, 251. [Google Scholar] [CrossRef] [PubMed]
- Yang, Z.; Yu, G.-L.; Zhu, X.; Peng, T.-H.; Lv, Y.-C. Critical Roles of FTO-Mediated mRNA m6A Demethylation in Regulating Adipogenesis and Lipid Metabolism: Implications in Lipid Metabolic Disorders. Genes Dis. 2021. [Google Scholar] [CrossRef]
- Zhong, X.; Yu, J.; Frazier, K.; Weng, X.; Li, Y.; Cham, C.M.; Dolan, K.; Zhu, X.; Hubert, N.; Tao, Y.; et al. Circadian Clock Regulation of Hepatic Lipid Metabolism by Modulation of m6A mRNA Methylation. Cell Rep. 2018, 25, 1816–1828.e4. [Google Scholar] [CrossRef]
- Yang, Y.; Huang, W.; Huang, J.-T.; Shen, F.; Xiong, J.; Yuan, E.-F.; Qin, S.-S.; Zhang, M.; Feng, Y.-Q.; Yuan, B.-F.; et al. Increased N6-Methyladenosine in Human Sperm RNA as a Risk Factor for Asthenozoospermia. Sci. Rep. 2016, 6, 24345. [Google Scholar] [CrossRef]
- Zhao, B.S.; He, C. “Gamete On” for m6A: YTHDF2 Exerts Essential Functions in Female Fertility. Mol. Cell 2017, 67, 903–905. [Google Scholar] [CrossRef]
- Tang, C.; Klukovich, R.; Peng, H.; Wang, Z.; Yu, T.; Zhang, Y.; Zheng, H.; Klungland, A.; Yan, W. ALKBH5-Dependent m6A Demethylation Controls Splicing and Stability of Long 3’-UTR mRNAs in Male Germ Cells. Proc. Natl. Acad. Sci. USA 2018, 115, E325–E333. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Lao, Y.; Wang, Y.; Li, R.; Fang, X.; Wang, Y.; Gao, X.; Dong, Z. Role of RNA N6-Methyladenosine Modification in Male Infertility and Genital System Tumors. Front. Cell Dev. Biol. 2021, 9, 676364. [Google Scholar] [CrossRef] [PubMed]
- Livneh, I.; Moshitch-Moshkovitz, S.; Amariglio, N.; Rechavi, G.; Dominissini, D. The m6A Epitranscriptome: Transcriptome Plasticity in Brain Development and Function. Nat. Rev. Neurosci. 2020, 21, 36–51. [Google Scholar] [CrossRef] [PubMed]
- Wang, P.; Doxtader, K.A.; Nam, Y. Structural Basis for Cooperative Function of Mettl3 and Mettl14 Methyltransferases. Mol. Cell 2016, 63, 306–317. [Google Scholar] [CrossRef]
- Zou, S.; Toh, J.D.W.; Wong, K.H.Q.; Gao, Y.-G.; Hong, W.; Woon, E.C.Y. N(6)-Methyladenosine: A Conformational Marker That Regulates the Substrate Specificity of Human Demethylases FTO and ALKBH5. Sci. Rep. 2016, 6, 25677. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Wang, J.; Gu, Q.; Ma, Y.; Yang, Y.; Zhu, J.; Zhang, Q. The Biological Function of m6A Demethylase ALKBH5 and Its Role in Human Disease. Cancer Cell Int. 2020, 20, 347. [Google Scholar] [CrossRef]
- Liao, S.; Sun, H.; Xu, C. YTH Domain: A Family of N6-Methyladenosine (m6A) Readers. Genom. Proteom. Bioinform. 2018, 16, 99–107. [Google Scholar] [CrossRef]
- Patil, D.P.; Pickering, B.F.; Jaffrey, S.R. Reading m6A in the Transcriptome: m6A-Binding Proteins. Trends Cell Biol. 2018, 28, 113–127. [Google Scholar] [CrossRef]
- Jia, G.; Fu, Y.; Zhao, X.; Dai, Q.; Zheng, G.; Yang, Y.; Yi, C.; Lindahl, T.; Pan, T.; Yang, Y.-G.; et al. N6-Methyladenosine in Nuclear RNA Is a Major Substrate of the Obesity-Associated FTO. Nat. Chem. Biol. 2011, 7, 885–887. [Google Scholar] [CrossRef]
- Church, C.; Moir, L.; McMurray, F.; Girard, C.; Banks, G.T.; Teboul, L.; Wells, S.; Brüning, J.C.; Nolan, P.M.; Ashcroft, F.M.; et al. Overexpression of Fto Leads to Increased Food Intake and Results in Obesity. Nat. Genet. 2010, 42, 1086–1092. [Google Scholar] [CrossRef] [PubMed]
- Church, C.; Lee, S.; Bagg, E.A.L.; McTaggart, J.S.; Deacon, R.; Gerken, T.; Lee, A.; Moir, L.; Mecinović, J.; Quwailid, M.M.; et al. A Mouse Model for the Metabolic Effects of the Human Fat Mass and Obesity Associated FTO Gene. PLoS Genet. 2009, 5, e1000599. [Google Scholar] [CrossRef]
- Barber, T.M.; Bennett, A.J.; Groves, C.J.; Sovio, U.; Ruokonen, A.; Martikainen, H.; Pouta, A.; Hartikainen, A.-L.; Elliott, P.; Lindgren, C.M.; et al. Association of Variants in the Fat Mass and Obesity Associated (FTO) Gene with Polycystic Ovary Syndrome. Diabetologia 2008, 51, 1153–1158. [Google Scholar] [CrossRef] [PubMed]
- Niu, Y.; Lin, Z.; Wan, A.; Chen, H.; Liang, H.; Sun, L.; Wang, Y.; Li, X.; Xiong, X.-F.; Wei, B.; et al. RNA N6-Methyladenosine Demethylase FTO Promotes Breast Tumor Progression through Inhibiting BNIP3. Mol. Cancer 2019, 18, 46. [Google Scholar] [CrossRef]
- Li, J.; Zhu, L.; Shi, Y.; Liu, J.; Lin, L.; Chen, X. m6A Demethylase FTO Promotes Hepatocellular Carcinoma Tumorigenesis via Mediating PKM2 Demethylation. Am. J. Transl. Res. 2019, 11, 6084–6092. [Google Scholar]
- Yang, S.; Wei, J.; Cui, Y.-H.; Park, G.; Shah, P.; Deng, Y.; Aplin, A.E.; Lu, Z.; Hwang, S.; He, C.; et al. m6A mRNA Demethylase FTO Regulates Melanoma Tumorigenicity and Response to Anti-PD-1 Blockade. Nat. Commun. 2019, 10, 2782. [Google Scholar] [CrossRef]
- Li, Z.; Weng, H.; Su, R.; Weng, X.; Zuo, Z.; Li, C.; Huang, H.; Nachtergaele, S.; Dong, L.; Hu, C.; et al. FTO Plays an Oncogenic Role in Acute Myeloid Leukemia as a N6-Methyladenosine RNA Demethylase. Cancer Cell 2017, 31, 127–141. [Google Scholar] [CrossRef]
- Jeschke, J.; Collignon, E.; Al Wardi, C.; Krayem, M.; Bizet, M.; Jia, Y.; Garaud, S.; Wimana, Z.; Calonne, E.; Hassabi, B.; et al. Downregulation of the FTO m6A RNA Demethylase Promotes EMT-Mediated Progression of Epithelial Tumors and Sensitivity to Wnt Inhibitors. Nature Cancer 2021, 2, 611–628. [Google Scholar] [CrossRef]
- Zhang, S.; Zhao, B.S.; Zhou, A.; Lin, K.; Zheng, S.; Lu, Z.; Chen, Y.; Sulman, E.P.; Xie, K.; Bögler, O.; et al. m6A Demethylase ALKBH5 Maintains Tumorigenicity of Glioblastoma Stem-like Cells by Sustaining FOXM1 Expression and Cell Proliferation Program. Cancer Cell 2017, 31, 591–606.e6. [Google Scholar] [CrossRef] [PubMed]
- Barbieri, I.; Tzelepis, K.; Pandolfini, L.; Shi, J.; Millán-Zambrano, G.; Robson, S.C.; Aspris, D.; Migliori, V.; Bannister, A.J.; Han, N.; et al. Promoter-Bound METTL3 Maintains Myeloid Leukaemia by m6A-Dependent Translation Control. Nature 2017, 552, 126–131. [Google Scholar] [CrossRef] [PubMed]
- Han, D.; Liu, J.; Chen, C.; Dong, L.; Liu, Y.; Chang, R.; Huang, X.; Liu, Y.; Wang, J.; Dougherty, U.; et al. Anti-Tumour Immunity Controlled through mRNA m6A Methylation and YTHDF1 in Dendritic Cells. Nature 2019, 566, 270–274. [Google Scholar] [CrossRef]
- Lan, Q.; Liu, P.Y.; Haase, J.; Bell, J.L.; Hüttelmaier, S.; Liu, T. The Critical Role of RNA m6A Methylation in Cancer. Cancer Res. 2019, 79, 1285–1292. [Google Scholar] [CrossRef] [PubMed]
- Sun, T.; Wu, R.; Ming, L. The Role of m6A RNA Methylation in Cancer. Biomed. Pharmacother. 2019, 112, 108613. [Google Scholar] [CrossRef]
- Huang, H.; Camats-Perna, J.; Medeiros, R.; Anggono, V.; Widagdo, J. Altered Expression of the m6A Methyltransferase METTL3 in Alzheimer’s Disease. Eneuro 2020, 7, 5. [Google Scholar] [CrossRef]
- Han, M.; Liu, Z.; Xu, Y.; Liu, X.; Wang, D.; Li, F.; Wang, Y.; Bi, J. Abnormality of m6A mRNA Methylation Is Involved in Alzheimer’s Disease. Front. Neurosci. 2020, 14, 98. [Google Scholar] [CrossRef]
- Shafik, A.M.; Zhang, F.; Guo, Z.; Dai, Q.; Pajdzik, K.; Li, Y.; Kang, Y.; Yao, B.; Wu, H.; He, C.; et al. N6-Methyladenosine Dynamics in Neurodevelopment and Aging, and Its Potential Role in Alzheimer’s Disease. Genome Biol. 2021, 22, 17. [Google Scholar] [CrossRef]
- Yen, Y.-P.; Chen, J.-A. The m6A Epitranscriptome on Neural Development and Degeneration. J. Biomed. Sci. 2021, 28, 40. [Google Scholar] [CrossRef]
- Wang, Y.; Li, Y.; Yue, M.; Wang, J.; Kumar, S.; Wechsler-Reya, R.J.; Zhang, Z.; Ogawa, Y.; Kellis, M.; Duester, G.; et al. N6-Methyladenosine RNA Modification Regulates Embryonic Neural Stem Cell Self-Renewal through Histone Modifications. Nat. Neurosci. 2018, 21, 195–206. [Google Scholar] [CrossRef]
- Wang, C.-X.; Cui, G.-S.; Liu, X.; Xu, K.; Wang, M.; Zhang, X.-X.; Jiang, L.-Y.; Li, A.; Yang, Y.; Lai, W.-Y.; et al. METTL3-Mediated m6A Modification Is Required for Cerebellar Development. PLoS Biol. 2018, 16, e2004880. [Google Scholar] [CrossRef]
- Chen, J.; Zhang, Y.-C.; Huang, C.; Shen, H.; Sun, B.; Cheng, X.; Zhang, Y.-J.; Yang, Y.-G.; Shu, Q.; Yang, Y.; et al. m6A Regulates Neurogenesis and Neuronal Development by Modulating Histone Methyltransferase Ezh2. Genom. Proteom. Bioinform. 2019, 17, 154–168. [Google Scholar] [CrossRef] [PubMed]
- Edens, B.M.; Vissers, C.; Su, J.; Arumugam, S.; Xu, Z.; Shi, H.; Miller, N.; Rojas Ringeling, F.; Ming, G.-L.; He, C.; et al. FMRP Modulates Neural Differentiation through m6A-Dependent mRNA Nuclear Export. Cell Rep. 2019, 28, 845–854.e5. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Zhai, Y.; Zhang, S.; Dai, X.; Li, Z. Roles of N6-Methyladenosine (m6A) in Stem Cell Fate Decisions and Early Embryonic Development in Mammals. Front. Cell Dev. Biol. 2020, 8, 782. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Zang, L.; Zhang, F.; Chen, J.; Shen, H.; Shu, L.; Liang, F.; Feng, C.; Chen, D.; Tao, H.; et al. Fat Mass and Obesity-Associated (FTO) Protein Regulates Adult Neurogenesis. Hum. Mol. Genet. 2017, 26, 2398–2411. [Google Scholar] [CrossRef] [PubMed]
- Xiong, X.; Yi, C.; Peng, J. Epitranscriptomics: Toward A Better Understanding of RNA Modifications. Genom. Proteom. Bioinform. 2017, 15, 147–153. [Google Scholar] [CrossRef]
- Yoon, K.-J.; Ringeling, F.R.; Vissers, C.; Jacob, F.; Pokrass, M.; Jimenez-Cyrus, D.; Su, Y.; Kim, N.-S.; Zhu, Y.; Zheng, L.; et al. Temporal Control of Mammalian Cortical Neurogenesis by m6A Methylation. Cell 2017, 171, 877–889.e17. [Google Scholar] [CrossRef]
- Gibney, E.R.; Nolan, C.M. Epigenetics and Gene Expression. Heredity 2010, 105, 4–13. [Google Scholar] [CrossRef]
- Deng, X.; Su, R.; Weng, H.; Huang, H.; Li, Z.; Chen, J. RNA N6-Methyladenosine Modification in Cancers: Current Status and Perspectives. Cell Res. 2018, 28, 507–517. [Google Scholar] [CrossRef] [PubMed]
- Fitzsimmons, C.M.; Batista, P.J. It’s Complicate m6A-Dependent Regulation of Gene Expression in Cancer. Biochim. Biophys. Acta Gene Regul. Mech. 2019, 1862, 382–393. [Google Scholar] [CrossRef]
- Chen, X.; Yu, C.; Guo, M.; Zheng, X.; Ali, S.; Huang, H.; Zhang, L.; Wang, S.; Huang, Y.; Qie, S.; et al. Down-Regulation of m6A mRNA Methylation Is Involved in Dopaminergic Neuronal Death. ACS Chem. Neurosci. 2019, 10, 2355–2363. [Google Scholar] [CrossRef] [PubMed]
- Zhou, X.; Chen, Z.; Zhou, J.; Liu, Y.; Fan, R.; Sun, T. Transcriptome and N6-Methyladenosine RNA Methylome Analyses in Aortic Dissection and Normal Human Aorta. Front. Cardiovasc. Med. 2021, 8, 627380. [Google Scholar] [CrossRef] [PubMed]
- Mo, X.-B.; Lei, S.-F.; Zhang, Y.-H.; Zhang, H. Examination of the Associations between m6A-Associated Single-Nucleotide Polymorphisms and Blood Pressure. Hypertens. Res. 2019, 42, 1582–1589. [Google Scholar] [CrossRef]
- Kmietczyk, V.; Riechert, E.; Kalinski, L.; Boileau, E.; Malovrh, E.; Malone, B.; Gorska, A.; Hofmann, C.; Varma, E.; Jürgensen, L.; et al. m6A-mRNA Methylation Regulates Cardiac Gene Expression and Cellular Growth. Life Sci. Alliance 2019, 2, e201800233. [Google Scholar] [CrossRef]
- Kwok, C.-T.; Marshall, A.D.; Rasko, J.E.J.; Wong, J.J.L. Genetic Alterations of m6A Regulators Predict Poorer Survival in Acute Myeloid Leukemia. J. Hematol. Oncol. 2017, 10, 39. [Google Scholar] [CrossRef]
- Dominissini, D.; Moshitch-Moshkovitz, S.; Schwartz, S.; Salmon-Divon, M.; Ungar, L.; Osenberg, S.; Cesarkas, K.; Jacob-Hirsch, J.; Amariglio, N.; Kupiec, M.; et al. Topology of the Human and Mouse m6A RNA Methylomes Revealed by m6A-Seq. Nature 2012, 485, 201–206. [Google Scholar] [CrossRef] [PubMed]
- Walerych, D.; Napoli, M.; Collavin, L.; Del Sal, G. The Rebel Angel: Mutant p53 as the Driving Oncogene in Breast Cancer. Carcinogenesis 2012, 33, 2007–2017. [Google Scholar] [CrossRef]
- Baugh, E.H.; Ke, H.; Levine, A.J.; Bonneau, R.A.; Chan, C.S. Why Are There Hotspot Mutations in the TP53 Gene in Human Cancers? Cell Death Differ. 2018, 25, 154–160. [Google Scholar] [CrossRef]
- Kang, N.; Wang, Y.; Guo, S.; Ou, Y.; Wang, G.; Chen, J.; Li, D.; Zhan, Q. Mutant TP53 G245C and R273H Promote Cellular Malignancy in Esophageal Squamous Cell Carcinoma. BMC Cell Biol. 2018, 19, 16. [Google Scholar] [CrossRef]
- Sun, S.; Chen, H.; Sun, L.; Wang, M.; Wu, X.; Xiao, Z.-X.J. Hotspot Mutant p53-R273H Inhibits KLF6 Expression to Promote Cell Migration and Tumor Metastasis. Cell Death Dis. 2020, 11, 595. [Google Scholar] [CrossRef]
- Uddin, M.B.; Roy, K.R.; Hosain, S.B.; Khiste, S.K.; Hill, R.A.; Jois, S.D.; Zhao, Y.; Tackett, A.J.; Liu, Y.-Y. An N6-Methyladenosine at the Transited Codon 273 of p53 Pre-mRNA Promotes the Expression of R273H Mutant Protein and Drug Resistance of Cancer Cells. Biochem. Pharmacol. 2019, 160, 134–145. [Google Scholar] [CrossRef]
- Fu, Y.; Zhuang, X. m6A-Binding YTHDF Proteins Promote Stress Granule Formation. Nat. Chem. Biol. 2020, 16, 955–963. [Google Scholar] [CrossRef] [PubMed]
- Ries, R.J.; Zaccara, S.; Klein, P.; Olarerin-George, A.; Namkoong, S.; Pickering, B.F.; Patil, D.P.; Kwak, H.; Lee, J.H.; Jaffrey, S.R. m6A Enhances the Phase Separation Potential of mRNA. Nature 2019, 571, 424–428. [Google Scholar] [CrossRef]
- Gao, Y.; Pei, G.; Li, D.; Li, R.; Shao, Y.; Zhang, Q.C.; Li, P. Multivalent m6A Motifs Promote Phase Separation of YTHDF Proteins. Cell Res. 2019, 29, 767–769. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.-Y.; Feng, Y.; Wu, J.-J.; Zou, M.-L.; Sun, Z.-L.; Li, X.; Yuan, F.-L. m6 A Facilitates YTHDF-Independent Phase Separation. J. Cell. Mol. Med. 2020, 24, 2070–2072. [Google Scholar] [CrossRef] [PubMed]
- Hoppe, J.B.; Salbego, C.G.; Cimarosti, H. SUMOylation: Novel Neuroprotective Approach for Alzheimer’s Disease? Aging. Dis. 2015, 6, 322–330. [Google Scholar] [CrossRef]
- Celen, A.B.; Sahin, U. Sumoylation on Its 25th Anniversary: Mechanisms, Pathology, and Emerging Concepts. FEBS J. 2020, 287, 3110–3140. [Google Scholar] [CrossRef]
- Eckermann, K. SUMO and Parkinson’s Disease. Neuromolecular Med. 2013, 15, 737–759. [Google Scholar] [CrossRef]
- Guo, L.; Giasson, B.I.; Glavis-Bloom, A.; Brewer, M.D.; Shorter, J.; Gitler, A.D.; Yang, X. A Cellular System That Degrades Misfolded Proteins and Protects against Neurodegeneration. Mol. Cell 2014, 55, 15–30. [Google Scholar] [CrossRef]
- Krumova, P.; Meulmeester, E.; Garrido, M.; Tirard, M.; Hsiao, H.-H.; Bossis, G.; Urlaub, H.; Zweckstetter, M.; Kügler, S.; Melchior, F.; et al. Sumoylation Inhibits Alpha-Synuclein Aggregation and Toxicity. J. Cell Biol. 2011, 194, 49–60. [Google Scholar] [CrossRef] [PubMed]
- Oh, Y.; Kim, Y.M.; Mouradian, M.M.; Chung, K.C. Human Polycomb Protein 2 Promotes α-Synuclein Aggregate Formation through Covalent SUMOylation. Brain Res. 2011, 1381, 78–89. [Google Scholar] [CrossRef]
- Guo, C.; Henley, J.M. Wrestling with Stress: Roles of Protein SUMOylation and deSUMOylation in Cell Stress Response. IUBMB Life 2014, 66, 71–77. [Google Scholar] [CrossRef]
- Enserink, J.M. Sumo and the Cellular Stress Response. Cell Div. 2015, 10, 4. [Google Scholar] [CrossRef] [PubMed]
- Karhausen, J.; Ulloa, L.; Yang, W. SUMOylation Connects Cell Stress Responses and Inflammatory Control: Lessons from the Gut as a Model Organ. Front. Immunol. 2021, 12, 646633. [Google Scholar] [CrossRef]
- He, J.; Cheng, J.; Wang, T. SUMOylation-Mediated Response to Mitochondrial Stress. Int. J. Mol. Sci. 2020, 21, 5657. [Google Scholar] [CrossRef]
- Gill, G. Something about SUMO Inhibits Transcription. Curr. Opin. Genet. Dev. 2005, 15, 536–541. [Google Scholar] [CrossRef] [PubMed]
- Graves, J.D.; Lee, Y.-J.; Liu, K.; Li, G.; Lin, F.-T.; Lin, W.-C. E2F1 Sumoylation as a Protective Cellular Mechanism in Oxidative Stress Response. Proc. Natl. Acad. Sci. USA. 2020, 117, 14958–14969. [Google Scholar] [CrossRef]
- Tsang, C.K.; Liu, Y.; Thomas, J.; Zhang, Y.; Zheng, X.F.S. Superoxide Dismutase 1 Acts as a Nuclear Transcription Factor to Regulate Oxidative Stress Resistance. Nat. Commun. 2014, 5, 3446. [Google Scholar] [CrossRef]
- Fei, E.; Jia, N.; Yan, M.; Ying, Z.; Sun, Q.; Wang, H.; Zhang, T.; Ma, X.; Ding, H.; Yao, X.; et al. SUMO-1 Modification Increases Human SOD1 Stability and Aggregation. Biochem. Biophys. Res. Commun. 2006, 347, 406–412. [Google Scholar] [CrossRef]
- Zhang, H.; Kuai, X.; Ji, Z.; Li, Z.; Shi, R. Over-Expression of Small Ubiquitin-Related Modifier-1 and Sumoylated p53 in Colon Cancer. Cell Biochem. Biophys. 2013, 67, 1081–1087. [Google Scholar] [CrossRef] [PubMed]
- Luo, H.-B.; Xia, Y.-Y.; Shu, X.-J.; Liu, Z.-C.; Feng, Y.; Liu, X.-H.; Yu, G.; Yin, G.; Xiong, Y.-S.; Zeng, K.; et al. SUMOylation at K340 Inhibits Tau Degradation through Deregulating Its Phosphorylation and Ubiquitination. Proc. Natl. Acad. Sci. USA 2014, 111, 16586–16591. [Google Scholar] [CrossRef] [PubMed]
- Seyfried, N.T.; Gozal, Y.M.; Dammer, E.B.; Xia, Q.; Duong, D.M.; Cheng, D.; Lah, J.J.; Levey, A.I.; Peng, J. Multiplex SILAC Analysis of a Cellular TDP-43 Proteinopathy Model Reveals Protein Inclusions Associated with SUMOylation and Diverse Polyubiquitin Chains. Mol. Cell Proteom. 2010, 9, 705–718. [Google Scholar] [CrossRef] [PubMed]
- Dangoumau, A.; Veyrat-Durebex, C.; Blasco, H.; Praline, J.; Corcia, P.; Andres, C.R.; Vourc’h, P. Protein SUMOylation, an Emerging Pathway in Amyotrophic Lateral Sclerosis. Int. J. Neurosci. 2013, 123, 366–374. [Google Scholar] [CrossRef] [PubMed]
- Foran, E.; Rosenblum, L.; Bogush, A.I.; Trotti, D. Sumoylation of Critical Proteins in Amyotrophic Lateral Sclerosis: Emerging Pathways of Pathogenesis. Neuromolecular Med. 2013, 15, 760–770. [Google Scholar] [CrossRef]
- Du, Y.; Hou, G.; Zhang, H.; Dou, J.; He, J.; Guo, Y.; Li, L.; Chen, R.; Wang, Y.; Deng, R.; et al. SUMOylation of the m6A-RNA Methyltransferase METTL3 Modulates Its Function. Nucleic Acids Res. 2018, 46, 5195–5208. [Google Scholar] [CrossRef] [PubMed]
- Maruyama, T.; Abe, Y.; Niikura, T. SENP1 and SENP2 Regulate SUMOylation of Amyloid Precursor Protein. Heliyon 2018, 4, e00601. [Google Scholar] [CrossRef]
- Xu, H.; Wang, H.; Zhao, W.; Fu, S.; Li, Y.; Ni, W.; Xin, Y.; Li, W.; Yang, C.; Bai, Y.; et al. SUMO1 Modification of Methyltransferase-like 3 Promotes Tumor Progression via Regulating Snail mRNA Homeostasis in Hepatocellular Carcinoma. Theranostics 2020, 10, 5671–5686. [Google Scholar] [CrossRef]
- Hou, G.; Zhao, X.; Li, L.; Yang, Q.; Liu, X.; Huang, C.; Lu, R.; Chen, R.; Wang, Y.; Jiang, B.; et al. SUMOylation of YTHDF2 Promotes mRNA Degradation and Cancer Progression by Increasing Its Binding Affinity with m6A-Modified mRNAs. Nucleic Acids Res. 2021, 49, 2859–2877. [Google Scholar] [CrossRef]
- Yang, X.; Yang, Y.; Sun, B.-F.; Chen, Y.-S.; Xu, J.-W.; Lai, W.-Y.; Li, A.; Wang, X.; Bhattarai, D.P.; Xiao, W.; et al. 5-Methylcytosine Promotes mRNA Export—NSUN2 as the Methyltransferase and ALYREF as an m5C Reader. Cell Res. 2017, 27, 606–625. [Google Scholar] [CrossRef]
- Dai, X.; Gonzalez, G.; Li, L.; Li, J.; You, C.; Miao, W.; Hu, J.; Fu, L.; Zhao, Y.; Li, R.; et al. YTHDF2 Binds to 5-Methylcytosine in RNA and Modulates the Maturation of Ribosomal RNA. Anal. Chem. 2020, 92, 1346–1354. [Google Scholar] [CrossRef] [PubMed]
- Zhu, R.; Ji, X.; Wu, X.; Chen, J.; Li, X.; Jiang, H.; Fu, H.; Wang, H.; Lin, Z.; Tang, X.; et al. Melatonin Antagonizes Ovarian Aging via YTHDF2-MAPK-NF-κB Pathway. Genes Dis. 2020. [Google Scholar] [CrossRef]
- Lv, Y.; Li, T.; Yang, M.; Su, L.; Zhu, Z.; Zhao, S.; Zeng, W.; Zheng, Y. Melatonin Attenuates Chromium (VI)-Induced Spermatogonial Stem Cell/Progenitor Mitophagy by Restoration of METTL3-Mediated RNA N6-Methyladenosine Modification. Front. Cell Dev. Biol. 2021, 9, 684398. [Google Scholar] [CrossRef]
- Li, H.; Chen, Q.; Li, S.; Yao, W.; Li, L.; Shi, X.; Wang, L.; Castranova, V.; Vallyathan, V.; Ernst, E.; et al. Effect of Cr(VI) Exposure on Sperm Quality: Human and Animal Studies. Ann. Occup. Hyg. 2001, 45, 505–511. [Google Scholar] [CrossRef]
- Das, J.; Kang, M.-H.; Kim, E.; Kwon, D.-N.; Choi, Y.-J.; Kim, J.-H. Hexavalent Chromium Induces Apoptosis in Male Somatic and Spermatogonial Stem Cells via Redox Imbalance. Sci. Rep. 2015, 5, 13921. [Google Scholar] [CrossRef]
- Zhao, B.S.; He, C. Fate by RNA Methylation: m6A Steers Stem Cell Pluripotency. Genome Biol. 2015, 16, 43. [Google Scholar] [CrossRef]
- Yang, L.; Liu, X.; Song, L.; Su, G.; Di, A.; Bai, C.; Wei, Z.; Li, G. Melatonin Restores the Pluripotency of Long-Term-Cultured Embryonic Stem Cells through Melatonin Receptor-Dependent m6A RNA Regulation. J. Pineal. Res. 2020, 69, e12669. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Li, Y.; Toth, J.I.; Petroski, M.D.; Zhang, Z.; Zhao, J.C. N6-Methyladenosine Modification Destabilizes Developmental Regulators in Embryonic Stem Cells. Nat. Cell Biol. 2014, 16, 191–198. [Google Scholar] [CrossRef]
- Aguilo, F.; Zhang, F.; Sancho, A.; Fidalgo, M.; Di Cecilia, S.; Vashisht, A.; Lee, D.-F.; Chen, C.-H.; Rengasamy, M.; Andino, B.; et al. Coordination of m(6)A mRNA Methylation and Gene Transcription by ZFP217 Regulates Pluripotency and Reprogramming. Cell Stem Cell 2015, 17, 689–704. [Google Scholar] [CrossRef]
- Jiang, X.; Zhang, C.; Qi, S.; Guo, S.; Chen, Y.; Du, E.; Zhang, H.; Wang, X.; Liu, R.; Qiao, B.; et al. Elevated Expression of ZNF217 Promotes Prostate Cancer Growth by Restraining Ferroportin-Conducted Iron Egress. Oncotarget 2016, 7, 84893–84906. [Google Scholar] [CrossRef]
- Matsumoto, T.; Uchiumi, T.; Monji, K.; Yagi, M.; Setoyama, D.; Amamoto, R.; Matsushima, Y.; Shiota, M.; Eto, M.; Kang, D. Doxycycline Induces Apoptosis via ER Stress Selectively to Cells with a Cancer Stem Cell-like Properties: Importance of Stem Cell Plasticity. Oncogenesis 2017, 6, 397. [Google Scholar] [CrossRef] [PubMed]
- Gerken, T.; Girard, C.A.; Tung, Y.-C.L.; Webby, C.J.; Saudek, V.; Hewitson, K.S.; Yeo, G.S.H.; McDonough, M.A.; Cunliffe, S.; McNeill, L.A.; et al. The Obesity-Associated FTO Gene Encodes a 2-Oxoglutarate-Dependent Nucleic Acid Demethylase. Science 2007, 318, 1469–1472. [Google Scholar] [CrossRef] [PubMed]
- Zheng, G.; Dahl, J.A.; Niu, Y.; Fedorcsak, P.; Huang, C.-M.; Li, C.J.; Vågbø, C.B.; Shi, Y.; Wang, W.-L.; Song, S.-H.; et al. ALKBH5 Is a Mammalian RNA Demethylase That Impacts RNA Metabolism and Mouse Fertility. Mol. Cell 2013, 49, 18–29. [Google Scholar] [CrossRef]
- Shen, C.; Sheng, Y.; Zhu, A.C.; Robinson, S.; Jiang, X.; Dong, L.; Chen, H.; Su, R.; Yin, Z.; Li, W.; et al. RNA Demethylase ALKBH5 Selectively Promotes Tumorigenesis and Cancer Stem Cell Self-Renewal in Acute Myeloid Leukemia. Cell Stem Cell 2020, 27, 64–80.e9. [Google Scholar] [CrossRef]
- Shah, A.; Rashid, F.; Awan, H.M.; Hu, S.; Wang, X.; Chen, L.; Shan, G. The DEAD-Box RNA Helicase DDX3 Interacts with m6A RNA Demethylase ALKBH5. Stem Cells Int. 2017, 2017, 8596135. [Google Scholar] [CrossRef]
- Kerr, C.L.; Bol, G.M.; Vesuna, F.; Raman, V. Targeting RNA Helicase DDX3 in Stem Cell Maintenance and Teratoma Formation. Genes Cancer 2019, 10, 11–20. [Google Scholar] [CrossRef][Green Version]
- Hilbert, M.; Karow, A.R.; Klostermeier, D. The Mechanism of ATP-Dependent RNA Unwinding by DEAD Box Proteins. Biol. Chem. 2009, 390, 1237–1250. [Google Scholar] [CrossRef]
- Jarmoskaite, I.; Russell, R. DEAD-Box Proteins as RNA Helicases and Chaperones. Wiley Interdiscip. Rev. RNA 2011, 2, 135–152. [Google Scholar] [CrossRef]
- Ledoux, S.; Guthrie, C. Regulation of the Dbp5 ATPase Cycle in mRNP Remodeling at the Nuclear Pore: A Lively New Paradigm for DEAD-Box Proteins. Genes Dev. 2011, 25, 1109–1114. [Google Scholar] [CrossRef]
- Young, C.L.; Khoshnevis, S.; Karbstein, K. Cofactor-Dependent Specificity of a DEAD-Box Protein. Proc. Natl. Acad. Sci. USA 2013, 110, E2668–E2676. [Google Scholar] [CrossRef] [PubMed]
- Conaway, R.C.; Conaway, J.W. ATP Activates Transcription Initiation from Promoters by RNA Polymerase II in a Reversible Step prior to RNA Synthesis. J. Biol. Chem. 1988, 263, 2962–2968. [Google Scholar] [CrossRef]
- Sassanfar, M.; Szostak, J.W. An RNA Motif That Binds ATP. Nature 1993, 364, 550–553. [Google Scholar] [CrossRef]
- White, H.B. Coenzymes as Fossils of an Earlier Metabolic State. J. Mol. Evol. 1976, 7, 101–104. [Google Scholar] [CrossRef]
- Goldman, A.D.; Kacar, B. Cofactors Are Remnants of Life’s Origin and Early Evolution. J. Mol. Evol. 2021, 89, 127–133. [Google Scholar] [CrossRef] [PubMed]
- Lymn, R.W.; Taylor, E.W. Mechanism of Adenosine Triphosphate Hydrolysis by Actomyosin. Biochemistry 1971, 10, 4617–4624. [Google Scholar] [CrossRef] [PubMed]
- Theissen, B.; Karow, A.R.; Köhler, J.; Gubaev, A.; Klostermeier, D. Cooperative Binding of ATP and RNA Induces a Closed Conformation in a DEAD Box RNA Helicase. Proc. Natl. Acad. Sci. USA 2008, 105, 548–553. [Google Scholar] [CrossRef] [PubMed]
- Henn, A.; Bradley, M.J.; De La Cruz, E.M. ATP Utilization and RNA Conformational Rearrangement by DEAD-Box Proteins. Annu. Rev. Biophys. 2012, 41, 247–267. [Google Scholar] [CrossRef]
- Song, H.; Ji, X. The Mechanism of RNA Duplex Recognition and Unwinding by DEAD-Box Helicase DDX3X. Nat. Commun. 2019, 10, 3085. [Google Scholar] [CrossRef]
- Liu, F.; Putnam, A.A.; Jankowsky, E. DEAD-Box Helicases Form Nucleotide-Dependent, Long-Lived Complexes with RNA. Biochemistry 2014, 53, 423–433. [Google Scholar] [CrossRef]
- Hooper, C.; Hilliker, A. Packing Them up and Dusting Them off: RNA Helicases and mRNA Storage. Biochim. Biophys. Acta 2013, 1829, 824–834. [Google Scholar] [CrossRef]
- Pimentel, J.; Boccaccio, G.L. Translation and Silencing in RNA Granules: A Tale of Sand Grains. Front. Mol. Neurosci. 2014, 7, 68. [Google Scholar] [CrossRef] [PubMed]
- Bourgeois, C.F.; Mortreux, F.; Auboeuf, D. The Multiple Functions of RNA Helicases as Drivers and Regulators of Gene Expression. Nat. Rev. Mol. Cell Biol. 2016, 17, 426–438. [Google Scholar] [CrossRef] [PubMed]
- Beißel, C.; Grosse, S.; Krebber, H. Dbp5/DDX19 between Translational Readthrough and Nonsense Mediated Decay. Int. J. Mol. Sci. 2020, 21, 1085. [Google Scholar] [CrossRef] [PubMed]
- Alluri, R.K.; Li, Z.; McCrae, K.R. Stress Granule-Mediated Oxidized RNA Decay in P-Body: Hypothetical Role of ADAR1, Tudor-SN, and STAU1. Front. Mol. Biosci. 2021, 8, 672988. [Google Scholar] [CrossRef]
- Tseng, S.S.; Weaver, P.L.; Liu, Y.; Hitomi, M.; Tartakoff, A.M.; Chang, T.H. Dbp5p, a Cytosolic RNA Helicase, Is Required for poly(A)+ RNA Export. EMBO J. 1998, 17, 2651–2662. [Google Scholar] [CrossRef] [PubMed]
- Hodge, C.A.; Colot, H.V.; Stafford, P.; Cole, C.N. Rat8p/Dbp5p Is a Shuttling Transport Factor That Interacts with Rat7p/Nup159p and Gle1p and Suppresses the mRNA Export Defect of xpo1-1 Cells. EMBO J. 1999, 18, 5778–5788. [Google Scholar] [CrossRef]
- Hodge, C.A.; Tran, E.J.; Noble, K.N.; Alcazar-Roman, A.R.; Ben-Yishay, R.; Scarcelli, J.J.; Folkmann, A.W.; Shav-Tal, Y.; Wente, S.R.; Cole, C.N. The Dbp5 Cycle at the Nuclear Pore Complex during mRNA Export I: dbp5 Mutants with Defects in RNA Binding and ATP Hydrolysis Define Key Steps for Nup159 and Gle1. Genes Dev. 2011, 25, 1052–1064. [Google Scholar] [CrossRef] [PubMed]
- Noble, K.N.; Tran, E.J.; Alcázar-Román, A.R.; Hodge, C.A.; Cole, C.N.; Wente, S.R. The Dbp5 Cycle at the Nuclear Pore Complex during mRNA Export II: Nucleotide Cycling and mRNP Remodeling by Dbp5 Are Controlled by Nup159 and Gle1. Genes Dev. 2011, 25, 1065–1077. [Google Scholar] [CrossRef]
- Okamura, M.; Yamanaka, Y.; Shigemoto, M.; Kitadani, Y.; Kobayashi, Y.; Kambe, T.; Nagao, M.; Kobayashi, I.; Okumura, K.; Masuda, S. Depletion of mRNA Export Regulator DBP5/DDX19, GLE1 or IPPK That Is a Key Enzyme for the Production of IP6, Resulting in Differentially Altered Cytoplasmic mRNA Expression and Specific Cell Defect. PLoS ONE 2018, 13, e0197165. [Google Scholar] [CrossRef]
- Hodroj, D.; Recolin, B.; Serhal, K.; Martinez, S.; Tsanov, N.; Abou Merhi, R.; Maiorano, D. An ATR-Dependent Function for the Ddx19 RNA Helicase in Nuclear R-Loop Metabolism. EMBO J. 2017, 36, 1182–1198. [Google Scholar] [CrossRef]
- Hodroj, D.; Serhal, K.; Maiorano, D. Ddx19 Links mRNA Nuclear Export with Progression of Transcription and Replication and Suppresses Genomic Instability upon DNA Damage in Proliferating Cells. Nucleus 2017, 8, 489–495. [Google Scholar] [CrossRef]
- Lin, D.H.; Correia, A.R.; Cai, S.W.; Huber, F.M.; Jette, C.A.; Hoelz, A. Structural and Functional Analysis of mRNA Export Regulation by the Nuclear Pore Complex. Nat. Commun. 2018, 9, 2319. [Google Scholar] [CrossRef] [PubMed]
- Sumner, M.C.; Brickner, J. The Nuclear Pore Complex as a Transcription Regulator. Cold Spring Harb. Perspect. Biol. 2021, a039438. [Google Scholar] [CrossRef] [PubMed]
- Andreou, A.Z.; Klostermeier, D. The DEAD-Box Helicase eIF4A: Paradigm or the Odd One Out? RNA Biol. 2013, 10, 19–32. [Google Scholar] [CrossRef] [PubMed]
- Tauber, D.; Tauber, G.; Khong, A.; Van Treeck, B.; Pelletier, J.; Parker, R. Modulation of RNA Condensation by the DEAD-Box Protein eIF4A. Cell 2020, 180, 411–426.e16. [Google Scholar] [CrossRef]
- Torbati, M.; Lele, T.P.; Agrawal, A. Ultradonut Topology of the Nuclear Envelope. Proc. Natl. Acad. Sci. USA 2016, 113, 11094–11099. [Google Scholar] [CrossRef] [PubMed]
- Agrawal, A.; Lele, T.P. Mechanics of Nuclear Membranes. J. Cell Sci. 2019, 132, jcs229245. [Google Scholar] [CrossRef] [PubMed]
- Fiserova, J.; Kiseleva, E.; Goldberg, M.W. Nuclear Envelope and Nuclear Pore Complex Structure and Organization in Tobacco BY-2 Cells. Plant J. 2009, 59, 243–255. [Google Scholar] [CrossRef]
- Mattaj, I.W. Sorting out the Nuclear Envelope from the Endoplasmic Reticulum. Nat. Rev. Mol. Cell Biol. 2004, 5, 65–69. [Google Scholar] [CrossRef]
- De Magistris, P.; Antonin, W. The Dynamic Nature of the Nuclear Envelope. Curr. Biol. 2018, 28, R487–R497. [Google Scholar] [CrossRef]
- Anderson, D.J.; Hetzer, M.W. Shaping the Endoplasmic Reticulum into the Nuclear Envelope. J. Cell Sci. 2008, 121 Pt 2, 137–142. [Google Scholar] [CrossRef] [PubMed]
- Dazzoni, R.; Grélard, A.; Morvan, E.; Bouter, A.; Applebee, C.J.; Loquet, A.; Larijani, B.; Dufourc, E.J. The Unprecedented Membrane Deformation of the Human Nuclear Envelope, in a Magnetic Field, Indicates Formation of Nuclear Membrane Invaginations. Sci. Rep. 2020, 10, 5147. [Google Scholar] [CrossRef] [PubMed]
- Fischer, A.H.; Bardarov, S.; Jiang, Z. Molecular Aspects of Diagnostic Nucleolar and Nuclear Envelope Changes in Prostate Cancer. J. Cell. Biochem. 2004, 91, 170–184. [Google Scholar] [CrossRef]
- Herlan, G.; Giese, G.; Wunderlich, F. Influence of Nuclear Membrane Lipid Fluidity on Nuclear RNA Release. Exp. Cell Res. 1979, 118, 305–309. [Google Scholar] [CrossRef]
- Hodge, C.A.; Choudhary, V.; Wolyniak, M.J.; Scarcelli, J.J.; Schneiter, R.; Cole, C.N. Integral Membrane Proteins Brr6 and Apq12 Link Assembly of the Nuclear Pore Complex to Lipid Homeostasis in the Endoplasmic Reticulum. J. Cell Sci. 2010, 123 Pt 1, 141–151. [Google Scholar] [CrossRef]
- Scarcelli, J.J.; Hodge, C.A.; Cole, C.N. The Yeast Integral Membrane Protein Apq12 Potentially Links Membrane Dynamics to Assembly of Nuclear Pore Complexes. J. Cell Biol. 2007, 178, 799–812. [Google Scholar] [CrossRef]
- Mimnaugh, E.G.; Kennedy, K.A.; Trush, M.A.; Sinha, B.K. Adriamycin-Enhanced Membrane Lipid Peroxidation in Isolated Rat Nuclei. Cancer Res. 1985, 45, 3296–3304. [Google Scholar]
- Vaca, C.E.; Harms-Ringdahl, M. Nuclear Membrane Lipid Peroxidation Products Bind to Nuclear Macromolecules. Arch. Biochem. Biophys. 1989, 269, 548–554. [Google Scholar] [CrossRef]
- Jarsch, I.K.; Daste, F.; Gallop, J.L. Membrane Curvature in Cell Biology: An Integration of Molecular Mechanisms. J. Cell Biol. 2016, 214, 375–387. [Google Scholar] [CrossRef]
- Antonin, W.; Ellenberg, J.; Dultz, E. Nuclear Pore Complex Assembly through the Cell Cycle: Regulation and Membrane Organization. FEBS Lett. 2008, 582, 2004–2016. [Google Scholar] [CrossRef]
- Antonin, W.; Mattaj, I.W. Nuclear Pore Complexes: Round the Bend? Nat. Cell Biol. 2005, 7, 10–12. [Google Scholar] [CrossRef]
- Mészáros, N.; Cibulka, J.; Mendiburo, M.J.; Romanauska, A.; Schneider, M.; Köhler, A. Nuclear Pore Basket Proteins Are Tethered to the Nuclear Envelope and Can Regulate Membrane Curvature. Dev. Cell 2015, 33, 285–298. [Google Scholar] [CrossRef] [PubMed]
- Vollmer, B.; Schooley, A.; Sachdev, R.; Eisenhardt, N.; Schneider, A.M.; Sieverding, C.; Madlung, J.; Gerken, U.; Macek, B.; Antonin, W. Dimerization and Direct Membrane Interaction of Nup53 Contribute to Nuclear Pore Complex Assembly. EMBO J. 2012, 31, 4072–4084. [Google Scholar] [CrossRef] [PubMed]
- Bahmanyar, S.; Schlieker, C. Lipid and Protein Dynamics That Shape Nuclear Envelope Identity. Mol. Biol. Cell 2020, 31, 1315–1323. [Google Scholar] [CrossRef] [PubMed]
- Rangamani, P.; Mandadap, K.K.; Oster, G. Protein-Induced Membrane Curvature Alters Local Membrane Tension. Biophys. J. 2014, 107, 751–762. [Google Scholar] [CrossRef]
- Hinderliter, A.; May, S. Cooperative Adsorption of Proteins onto Lipid Membranes. J. Phys. Condens. Matter 2006, 18, S1257–S1270. [Google Scholar] [CrossRef] [PubMed]
- Cascianelli, G.; Villani, M.; Tosti, M.; Marini, F.; Bartoccini, E.; Magni, M.V.; Albi, E. Lipid Microdomains in Cell Nucleus. Mol. Biol. Cell 2008, 19, 5289–5295. [Google Scholar] [CrossRef]
- Vlassov, A.; Khvorova, A.; Yarus, M. Binding and Disruption of Phospholipid Bilayers by Supramolecular RNA Complexes. Proc. Natl. Acad. Sci. USA 2001, 98, 7706–7711. [Google Scholar] [CrossRef]
- Khvorova, A.; Kwak, Y.G.; Tamkun, M.; Majerfeld, I.; Yarus, M. RNAs That Bind and Change the Permeability of Phospholipid Membranes. Proc. Natl. Acad. Sci. USA 1999, 96, 10649–10654. [Google Scholar] [CrossRef] [PubMed]
- Janas, T.; Janas, T.; Yarus, M. Human tRNA(Sec) Associates with HeLa Membranes, Cell Lipid Liposomes, and Synthetic Lipid Bilayers. RNA 2012, 18, 2260–2268. [Google Scholar] [CrossRef]
- Janas, T.; Janas, T.; Yarus, M. Specific RNA Binding to Ordered Phospholipid Bilayers. Nucleic Acids Res. 2006, 34, 2128–2136. [Google Scholar] [CrossRef]
- Lehman, N. The RNA World: 4,000,000,050 Years Old. Life 2015, 5, 1583–1586. [Google Scholar] [CrossRef]
- Horning, D.P.; Joyce, G.F. Amplification of RNA by an RNA Polymerase Ribozyme. Proc. Natl. Acad. Sci. USA 2016, 113, 9786–9791. [Google Scholar] [CrossRef]
- Xu, J.; Green, N.J.; Gibard, C.; Krishnamurthy, R.; Sutherland, J.D. Prebiotic Phosphorylation of 2-Thiouridine Provides Either Nucleotides or DNA Building Blocks via Photoreduction. Nat. Chem. 2019, 11, 457–462. [Google Scholar] [CrossRef] [PubMed]
- Watkins, K.P.; Williams-Carrier, R.; Chotewutmontri, P.; Friso, G.; Teubner, M.; Belcher, S.; Ruwe, H.; Schmitz-Linneweber, C.; van Wijk, K.J.; Barkan, A. Exploring the Proteome Associated with the mRNA Encoding the D1 Reaction Center Protein of Photosystem II in Plant Chloroplasts. Plant J. 2020, 102, 369–382. [Google Scholar] [CrossRef] [PubMed]
- Zoschke, R.; Bock, R. Chloroplast Translation: Structural and Functional Organization, Operational Control, and Regulation. Plant Cell 2018, 30, 745–770. [Google Scholar] [CrossRef] [PubMed]
- Gawroński, P.; Enroth, C.; Kindgren, P.; Marquardt, S.; Karpiński, S.; Leister, D.; Jensen, P.E.; Vinther, J.; Scharff, L.B. Light-Dependent Translation Change of Arabidopsis psbA Correlates with RNA Structure Alterations at the Translation Initiation Region. Cells 2021, 10, 322. [Google Scholar] [CrossRef]
- Preiss, S.; Schrader, S.; Johanningmeier, U. Rapid, ATP-Dependent Degradation of a Truncated D1 Protein in the Chloroplast. Eur. J. Biochem. 2001, 268, 4562–4569. [Google Scholar] [CrossRef]
- Pévet, P. Melatonin in Animal Models. Dialogues Clin. Neurosci. 2003, 5, 343–352. [Google Scholar]
- Zheng, X.; Tan, D.X.; Allan, A.C.; Zuo, B.; Zhao, Y.; Reiter, R.J.; Wang, L.; Wang, Z.; Guo, Y.; Zhou, J.; et al. Chloroplastic Biosynthesis of Melatonin and Its Involvement in Protection of Plants from Salt Stress. Sci. Rep. 2017, 7, 41236. [Google Scholar] [CrossRef]
- Hwang, O.J.; Kang, K.; Back, K. Effects of Light Quality and Phytochrome Form on Melatonin Biosynthesis in Rice. Biomolecules 2020, 10, 523. [Google Scholar] [CrossRef] [PubMed]
- Zhou, X.; Zhao, H.; Cao, K.; Hu, L.; Du, T.; Baluška, F.; Zou, Z. Beneficial Roles of Melatonin on Redox Regulation of Photosynthetic Electron Transport and Synthesis of D1 Protein in Tomato Seedlings under Salt Stress. Front. Plant Sci. 2016, 7, 1823. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).