The Effects of Nano-Curcumin Supplementation on Risk Factors for Cardiovascular Disease: A GRADE-Assessed Systematic Review and Meta-Analysis of Clinical Trials
Abstract
:1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Inclusion Criteria
2.3. Exclusion Criteria
2.4. Data Extraction
2.5. Quality Assessment
2.6. Statistical Analysis
2.7. Certainty Assessment
3. Results
3.1. Study Characteristics
3.2. Meta-Analysis
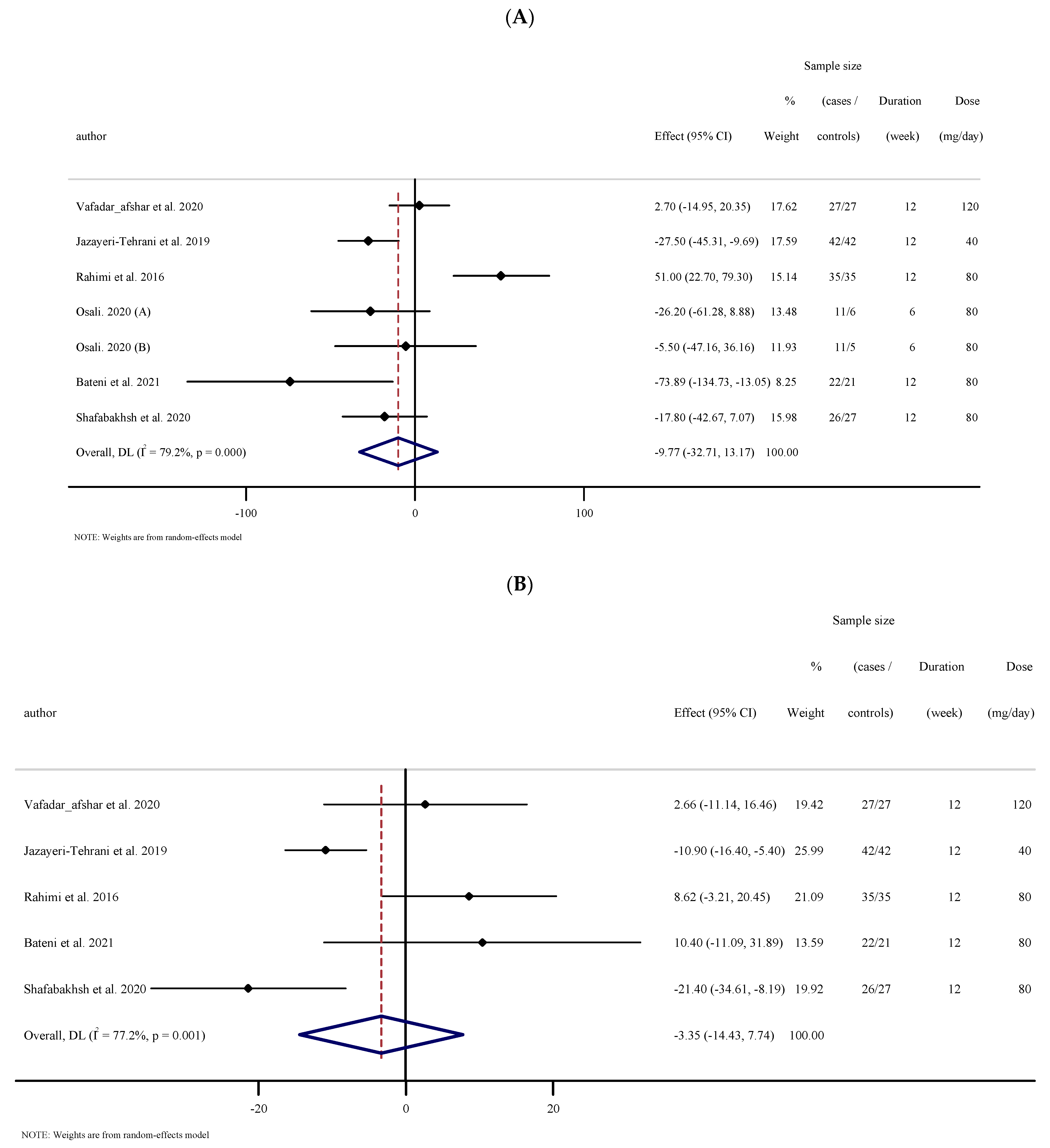
3.2.1. The Effects of Nano-Curcumin Supplementation on Triglyceride (TG)
3.2.2. The Effects of Nano-Curcumin Supplementation on Total Cholesterol (TC)
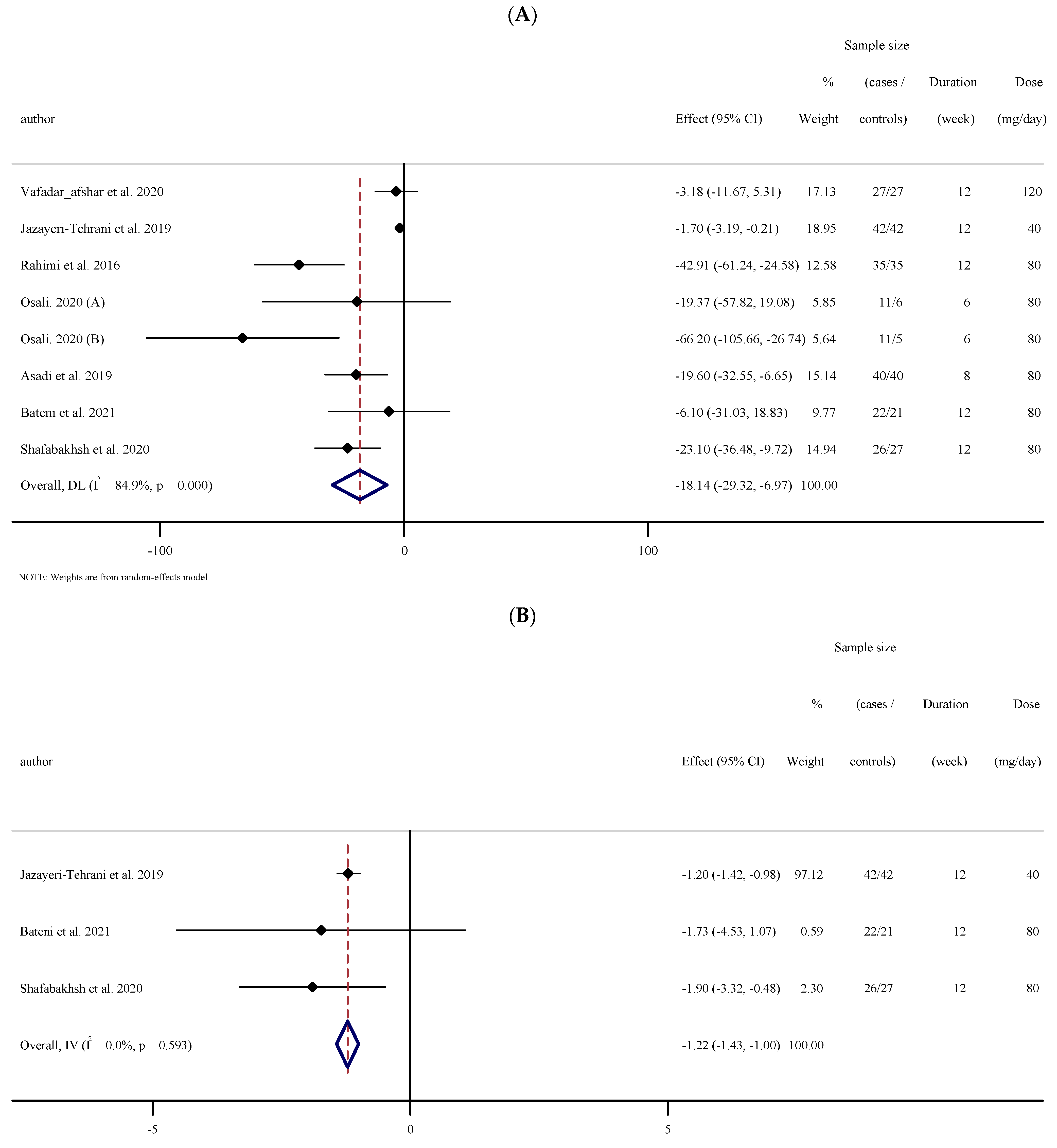
3.2.3. The Effects of Nano-Curcumin Supplementation on LDL-C
3.2.4. The Effects of Nano-Curcumin Supplementation on HDL-C
3.2.5. The Effects of Nano-Curcumin Supplementation on Fasting Blood Sugar (FBS)
3.2.6. The Effects of Nano-Curcumin Supplementation on Fasting Insulin, Homeostatic Model Assessment for Insulin Resistance (HOMA-IR), and Hemoglobin A1c (HbA1c)
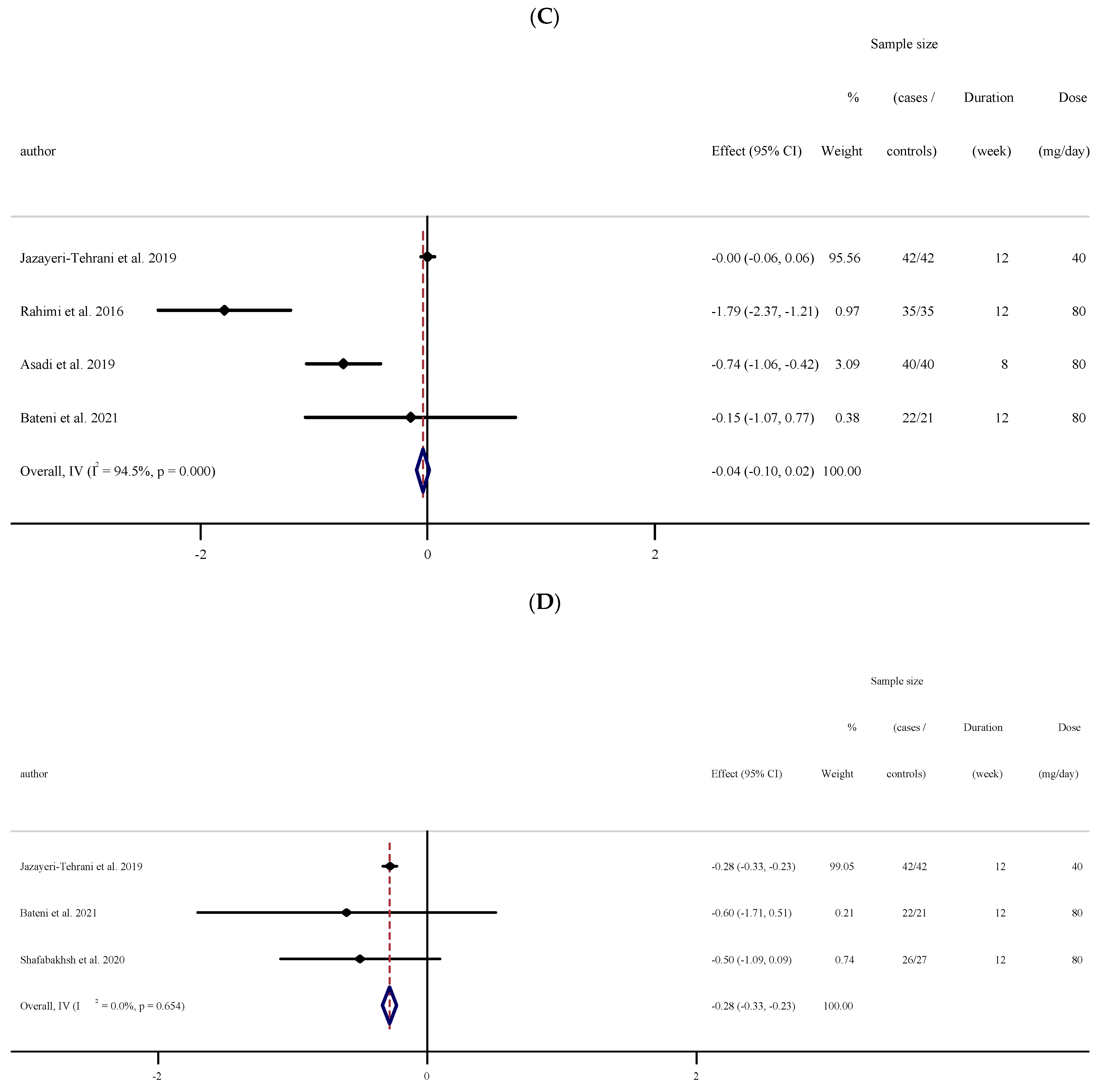
3.2.7. The Effects of Nano-Curcumin Supplementation on BP
3.2.8. The Effects of Nano-Curcumin Supplementation on CRP
3.2.9. The Effects of Nano-Curcumin Supplementation on IL-6 and TNF-α
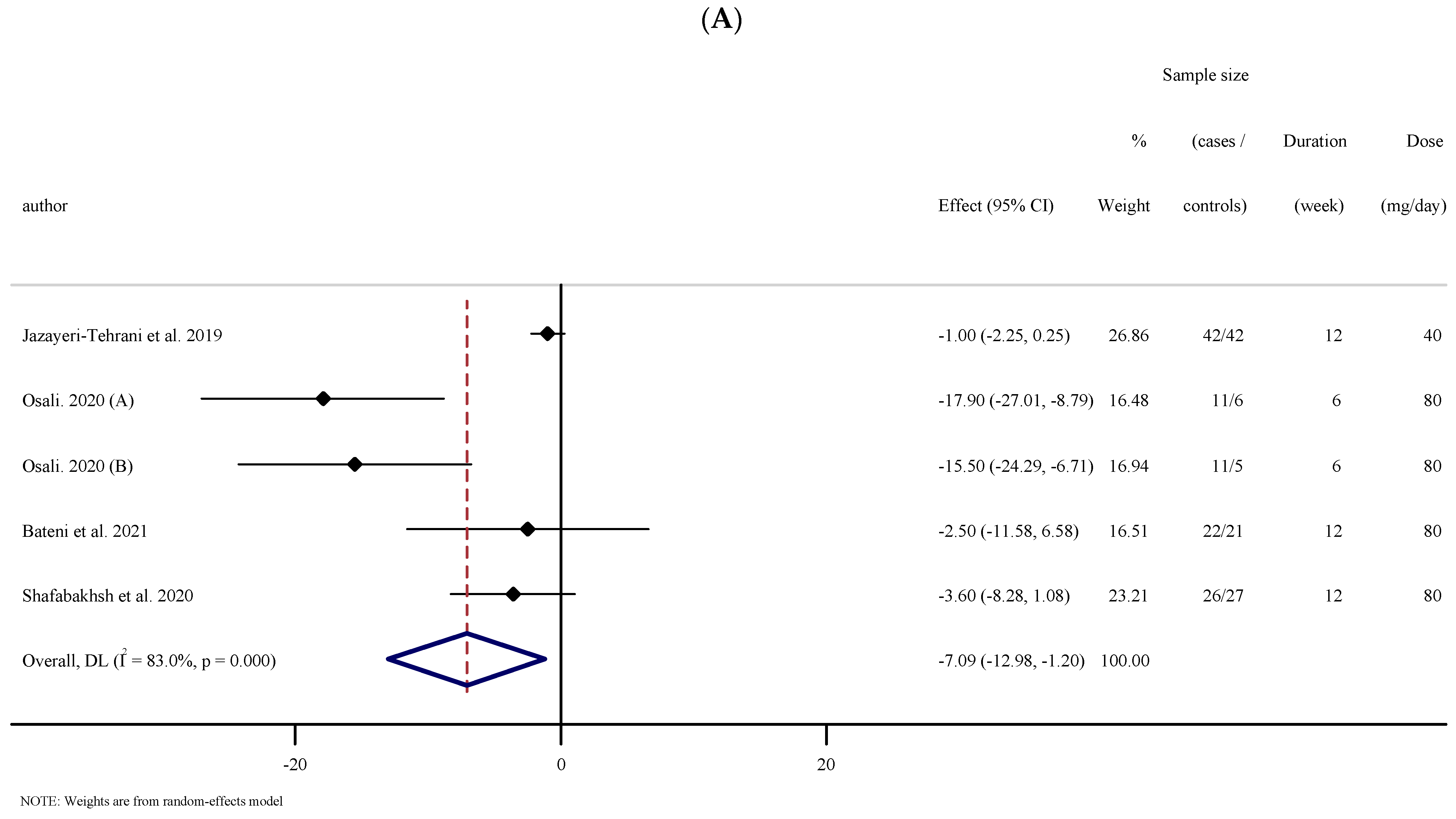
3.2.10. The Effects of Nano-Curcumin Supplementation on the Anthropometric Indices
3.3. Publication Bias
3.4. Sensitivity Analysis
3.5. Grading of Evidence
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Wilkins, E.; Wilson, L.; Wickramasinghe, K.; Bhatnagar, P.; Leal, J.; Luengo-Fernandez, R.; Burns, R.; Rayner, M.; Townsend, N. European Cardiovascular Disease Statistics 2017; European Heart Network: Brussels, Belgium, 2017. [Google Scholar]
- Ashtary-Larky, D.; Bagheri, R.; Ghanavati, M.; Asbaghi, O.; Tinsley, G.M.; Mombaini, D.; Kooti, W.; Kashkooli, S.; Wong, A. Effects of betaine supplementation on cardiovascular markers: A systematic review and Meta-analysis. Crit. Rev. Food Sci. Nutr. 2021, 1–18. [Google Scholar] [CrossRef]
- Asbaghi, O.; Choghakhori, R.; Ashtary-Larky, D.; Abbasnezhad, A. Effects of the Mediterranean diet on cardiovascular risk factors in non-alcoholic fatty liver disease patients: A systematic review and meta-analysis. Clin. Nutr. ESPEN 2020, 37, 148–156. [Google Scholar] [CrossRef] [PubMed]
- Dehbalaei, M.G.; Ashtary-Larky, D.; Mesrkanlou, H.A.; Talebi, S.; Asbaghi, O. The effects of magnesium and vitamin E co-supplementation on some cardiovascular risk factors: A meta-analysis. Clin. Nutr. ESPEN 2021, 41, 110–117. [Google Scholar] [CrossRef]
- Asbaghi, O.; Fatemeh, N.; Mahnaz, R.K.; Ehsan, G.; Elham, E.; Behzad, N.; Damoon, A.-L.; Amirmansour, A. Effects of chromium supplementation on glycemic control in patients with type 2 diabetes: A systematic review and meta-analysis of randomized controlled trials. Pharmacol. Res. 2020, 161, 105098. [Google Scholar] [CrossRef] [PubMed]
- Sahebkar, A. Are curcuminoids effective C-reactive protein-lowering agents in clinical practice? Evidence from a meta-analysis. Phytother. Res. 2014, 28, 633–642. [Google Scholar] [CrossRef]
- Panahi, Y.; Hosseini, M.S.; Khalili, N.; Naimi, E.; Simental-Mendía, L.E.; Majeed, M.; Sahebkar, A. Effects of curcumin on serum cytokine concentrations in subjects with metabolic syndrome: A post-hoc analysis of a randomized controlled trial. Biomed. Pharmacother. 2016, 82, 578–582. [Google Scholar] [CrossRef]
- Hewlings, S.J.; Kalman, D.S. Curcumin: A review of its effects on human health. Foods 2017, 6, 92. [Google Scholar] [CrossRef]
- Pulido-Moran, M.; Moreno-Fernandez, J.; Ramirez-Tortosa, C.; Ramirez-Tortosa, M. Curcumin and health. Molecules 2016, 21, 264. [Google Scholar] [CrossRef]
- Kapakos, G.; Youreva, V.; Srivastava, A.K. Cardiovascular protection by curcumin: Molecular aspects. Indian J. Biochem. Biophys. 2012, 49, 306–315. [Google Scholar]
- Wongcharoen, W.; Phrommintikul, A. The protective role of curcumin in cardiovascular diseases. Int. J. Cardiol. 2009, 133, 145–151. [Google Scholar] [CrossRef]
- Islam, A.; Rebello, L.; Chepyala, S. Review on nanoformulations of curcumin (Curcuma longa Linn.): Special emphasis on Nanocurcumin®. Int. J. Nat. Life Sci. 2019, 3, 1–12. [Google Scholar]
- Flora, G.; Gupta, D.; Tiwari, A. Nanocurcumin: A promising therapeutic advancement over native curcumin. Crit. Rev. Ther. Drug Carr. Syst. 2013, 30, 331–368. [Google Scholar] [CrossRef]
- Rahimi, H.R.; Mohammadpour, A.H.; Dastani, M.; Jaafari, M.R.; Abnous, K.; Mobarhan, M.G.; Oskuee, R.K. The effect of nano-curcumin on HbA1c, fasting blood glucose, and lipid profile in diabetic subjects: A randomized clinical trial. Avicenna J. Phytomed. 2016, 6, 567. [Google Scholar] [PubMed]
- Khosropanah, M.H.; Dinarvand, A.; Nezhadhosseini, A.; Haghighi, A.; Hashemi, S.; Nirouzad, F.; Khatamsaz, S.; Entezari, M.; Hashemi, M.; Dehghani, H. Analysis of the Antiproliferative Effects of Curcumin and Nanocurcumin in MDA-MB231 as a Breast Cancer Cell Line. Iran. J. Pharm. Res. 2016, 15, 231–239. [Google Scholar] [PubMed]
- Dende, C.; Meena, J.; Nagarajan, P.; Nagaraj, V.A.; Panda, A.K.; Padmanaban, G. Nanocurcumin is superior to native curcumin in preventing degenerative changes in Experimental Cerebral Malaria. Sci. Rep. 2017, 7, 10062. [Google Scholar] [CrossRef] [Green Version]
- Basniwal, R.K.; Khosla, R.; Jain, N. Improving the Anticancer Activity of Curcumin Using Nanocurcumin Dispersion in Water. Nutr. Cancer 2014, 66, 1015–1022. [Google Scholar] [CrossRef]
- Shamsi-Goushki, A.; Mortazavi, Z.; Mirshekar, M.A.; Mohammadi, M.; Moradi-Kor, N.; Jafari-Maskouni, S.; Shahraki, M. Comparative Effects of Curcumin versus Nano-Curcumin on Insulin Resistance, Serum Levels of Apelin and Lipid Profile in Type 2 Diabetic Rats. Diabetes Metab. Syndr. Obes. Targets Ther. 2020, 13, 2337–2346. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [Green Version]
- Higgins, J.P.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savovic, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- DerSimonian, R.; Laird, N. Meta-analysis in clinical trials. Control. Clin. Trials 1986, 7, 177–188. [Google Scholar] [CrossRef]
- Borenstein, M.; Hedges, L.V.; Higgins, J.P.; Rothstein, H.R. Introduction to Meta-Analysis; John Wiley & Sons: Hoboken, NJ, USA, 2011. [Google Scholar]
- Hozo, S.P.; Djulbegovic, B.; Hozo, I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med. Res. Methodol. 2005, 5, 1–10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Higgins, J.P.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef] [Green Version]
- Higgins, J.P.; Thompson, S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef]
- Tobias, A. Assessing the influence of a single study in the meta-anyalysis estimate. Stata Tech. Bull. 1999, 8, 1–48. [Google Scholar]
- Egger, M.; Smith, G.D.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997, 315, 629–634. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gordon, H.; Oxman, A.; Vist, G.; Kunz, R.; Falck-Ytter, Y.; Alonso-Coello, P.; Schünemann, H. Rating quality of evidence and strength of recommendations: GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008, 336, 924–926. [Google Scholar]
- Abdolahi, M.; Tafakhori, A.; Togha, M.; Okhovat, A.A.; Siassi, F.; Eshraghian, M.R.; Sedighiyan, M.; Djalali, M.; Honarvar, N.M.; Djalali, M. The synergistic effects of omega-3 fatty acids and nano-curcumin supplementation on tumor necrosis factor (TNF)-alpha gene expression and serum level in migraine patients. Immunogenetics 2017, 69, 371–378. [Google Scholar] [CrossRef] [PubMed]
- Abdolahi, M.; Sarraf, P.; Javanbakht, M.H.; Honarvar, N.M.; Hatami, M.; Soveyd, N.; Tafakhori, A.; Sedighiyan, M.; Djalali, M.; Jafarieh, A.; et al. A Novel Combination of omega-3 Fatty Acids and Nano-Curcumin Modulates Interleukin-6 Gene Expression and High Sensitivity C-reactive Protein Serum Levels in Patients with Migraine: A Randomized Clinical Trial Study. CNS Neurol. Disord. Drug Targets 2018, 17, 430–438. [Google Scholar] [CrossRef] [PubMed]
- Asadi, S.; Gholami, M.S.; Siassi, F.; Qorbani, M.; Khamoshian, K.; Sotoudeh, G. Nano curcumin supplementation reduced the severity of diabetic sensorimotor polyneuropathy in patients with type 2 diabetes mellitus: A randomized double-blind placebo- controlled clinical trial. Complementary Ther. Med. 2019, 43, 253–260. [Google Scholar] [CrossRef]
- Jazayeri-Tehrani, S.A.; Rezayat, S.M.; Mansouri, S.; Qorbani, M.; Alavian, S.M.; Daneshi-Maskooni, M.; Hosseinzadeh-Attar, M.J. Nano-curcumin improves glucose indices, lipids, inflammation, and Nesfatin in overweight and obese patients with non-alcoholic fatty liver disease (NAFLD): A double-blind randomized placebo-controlled clinical trial. Nutr. Metab. 2019, 16, 8. [Google Scholar] [CrossRef]
- Osali, A. Aerobic exercise and nano-curcumin supplementation improve inflammation in elderly females with metabolic syndrome. Diabetol. Metab. Syndr. 2020, 12, 26. [Google Scholar] [CrossRef] [PubMed]
- Shafabakhsh, R.; Asemi, Z.; Reiner, Ž.; Soleimani, A.; Aghadavod, E.; Bahmani, F. The Effects of Nano-curcumin on Metabolic Status in Patients with Diabetes on Hemodialysis, a Randomized, Double Blind, Placebo-controlled Trial. Iran. J. Kidney Dis. 2020, 14, 290–299. [Google Scholar] [PubMed]
- Afshar, G.V.; Rasmi, Y.; Yagmayee, P.; Khadem-Ansari, M.-H.; Makhdomii, K.; Rasooli, J. The Effects of Nano-curcumin Supplementation on Serum Level of hs-CRP, Adhesion Molecules, and Lipid Profiles in Hemodialysis Patients, A Randomized Controlled Clinical Trial. Iran. J. Kidney Dis. 2020, 14, 52–61. [Google Scholar]
- Bateni, Z.; Rahimi, H.R.; Hedayati, M.; Afsharian, S.; Goudarzi, R.; Sohrab, G. The effects of nano-curcumin supplementation on glycemic control, blood pressure, lipid profile, and insulin resistance in patients with the metabolic syndrome: A randomized, double-blind clinical trial. Phytother. Res. 2021. [Google Scholar] [CrossRef]
- Karthikeyan, A.; Senthil, N.; Min, T. Nanocurcumin: A Promising Candidate for Therapeutic Applications. Front. Pharmacol. 2020, 11, 11. [Google Scholar] [CrossRef]
- Aggarwal, B.B.; Sung, B. Pharmacological basis for the role of curcumin in chronic diseases: An age-old spice with modern targets. Trends Pharmacol. Sci. 2009, 30, 85–94. [Google Scholar] [CrossRef]
- Commandeur, J.N.M.; Vermeulen, N.P. Cytotoxicity and cytoprotective activities of natural compounds. The case of curcumin. Xenobiotica 1996, 26, 667–680. [Google Scholar] [CrossRef]
- Basnet, P.; Skalko-Basnet, N. Curcumin: An anti-inflammatory molecule from a curry spice on the path to cancer treatment. Molecules 2011, 16, 4567–4598. [Google Scholar] [CrossRef] [Green Version]
- Rawshani, A.; Rawshani, A.; Franzén, S.; Sattar, N.; Eliasson, B.; Svensson, A.-M.; Zethelius, B.; Miftaraj, M.; McGuire, D.K.; Rosengren, A.; et al. Risk Factors, Mortality, and Cardiovascular Outcomes in Patients with Type 2 Diabetes. N. Engl. J. Med. 2018, 379, 633–644. [Google Scholar] [CrossRef]
- Martín-Timón, I.; Sevillano-Collantes, C.; Segura-Galindo, A.; del Cañizo-Gómez, F.J. Type 2 diabetes and cardiovascular disease: Have all risk factors the same strength? World J. Diabetes 2014, 5, 444. [Google Scholar] [CrossRef]
- Miller, M. Dyslipidemia and cardiovascular risk: The importance of early prevention. QJM Int. J. Med. 2009, 102, 657–667. [Google Scholar] [CrossRef] [Green Version]
- American Diabetes Association. Dyslipidemia management in adults with diabetes. Diabetes Care 2004, 27, s68–s71. [Google Scholar] [CrossRef] [Green Version]
- Piepoli, M.F.; Hoes, A.W.; Agewall, S.; Albus, C.; Brotons, C.; Catapano, A.L.; Cooney, M.-T.; Corra, U.; Cosyns, B.; Deaton, C.; et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts) Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur. J. Prev. Cardiol. 2016, 37, 2315–2381. [Google Scholar]
- Grundy, S.M.; Cleeman, J.I.; Merz, C.N.B.; Brewer, H.B.; Clark, L.T.; Hunninghake, D.B.; Pasternak, R.C.; Smith, S.C.; Stone, N.J. Implications of Recent Clinical Trials for the National Cholesterol Education Program Adult Treatment Panel III Guidelines. J. Am. Coll. Cardiol. 2004, 44, 720–732. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Colhoun, H.M.; Betteridge, D.J.; Durrington, P.N.; Hitman, G.A.; Neil, H.A.W.; Livingstone, S.J.; Thomason, M.; Mackness, M.I.; Charlton-Menys, V.; Fuller, J.H. Primary prevention of cardiovascular disease with atorvastatin in type 2 diabetes in the Collaborative Atorvastatin Diabetes Study (CARDS): Multicentre randomised placebo-controlled trial. Lancet 2004, 364, 685–696. [Google Scholar] [CrossRef]
- Elam, M.B.; Ginsberg, H.N.; Lovato, L.C.; Corson, M.; Largay, J.; Leiter, L.A.; Lopez, C.; O’Connor, P.; Sweeney, M.E.; Weiss, D.; et al. Association of Fenofibrate Therapy With Long-term Cardiovascular Risk in Statin-Treated Patients with Type 2 Diabetes. JAMA Cardiol. 2017, 2, 370–380. [Google Scholar] [CrossRef]
- Brugts, J.J.; Yetgin, T.; Hoeks, S.E.; Gotto, A.M.; Shepherd, J.; Westendorp, R.G.J.; De Craen, A.J.M.; Knopp, R.H.; Nakamura, H.; Ridker, P.; et al. The benefits of statins in people without established cardiovascular disease but with cardiovascular risk factors: Meta-analysis of randomised controlled trials. BMJ 2009, 338, b2376. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abramson, J.D.; Rosenberg, H.G.; Jewell, N.; Wright, J.M. Should people at low risk of cardiovascular disease take a statin? BMJ 2013, 347, f6123. [Google Scholar] [CrossRef] [Green Version]
- Toth, P.P.; Barter, P.J.; Rosenson, R.S.; Boden, W.E.; Chapman, M.J.; Cuchel, M.; D’Agostino Sr, R.B.; Davidson, M.H.; Davidson, W.S.; Heinecke, J.W.; et al. High-density lipoproteins: A consensus statement from the National Lipid Association. J. Clin. Lipidol. 2013, 7, 484–525. [Google Scholar] [CrossRef]
- Goff, D.C.; Lloyd-Jones, D.M.; Bennett, G.; Coady, S.; D’agostino, R.B.; Gibbons, R.; Greenland, P.; Lackland, D.T.; Levy, D.; O’donnell, C.J.; et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J. Am. Coll. Cardiol. 2014, 63, 2935–2959. [Google Scholar] [CrossRef] [Green Version]
- Rader, D.J.; Hovingh, G.K. HDL and cardiovascular disease. Lancet 2014, 384, 618–625. [Google Scholar] [CrossRef]
- Namkhah, Z.; Ashtary-Larky, D.; Naeini, F.; Clark, C.C.; Asbaghi, O. Does vitamin C supplementation exert profitable effects on serum lipid profile in patients with type 2 diabetes? A systematic review and dose-response meta-analysis. Pharmacol. Res. 2021, 169, 105665. [Google Scholar] [CrossRef] [PubMed]
- Asbaghi, O.; Fouladvand, F.; Moradi, S.; Ashtary-Larky, D.; Choghakhori, R.; Abbasnezhad, A. Effect of green tea extract on lipid profile in patients with type 2 diabetes mellitus: A systematic review and meta-analysis. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 293–301. [Google Scholar] [CrossRef] [PubMed]
- Reda, F.M.; El-Saadony, M.T.; ElNesr, S.S.; Alagawany, M.; Tufarelli, V. Effect of Dietary Supplementation of Biological Curcumin Nanoparticles on Growth and Carcass Traits, Antioxidant Status, Immunity and Caecal Microbiota of Japanese Quails. Animals 2020, 10, 754. [Google Scholar] [CrossRef]
- Altobelli, E.; Angeletti, P.M.; Marziliano, C.; Mastrodomenico, M.; Giuliani, A.R.; Petrocelli, R. Potential Therapeutic Effects of Curcumin on Glycemic and Lipid Profile in Uncomplicated Type 2 Diabetes—A Meta-Analysis of Randomized Controlled Trial. Nutrients 2021, 13, 404. [Google Scholar] [CrossRef]
- Gouda, W.; Hafiz, N.A.; Mageed, L.; Alazzouni, A.S.; Khalil, W.K.B.; Afify, M.; Abdelmaksoud, M.D.E. Effects of nano-curcumin on gene expression of insulin and insulin receptor. Bull. Natl. Res. Cent. 2019, 43, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Ganugula, R.; Arora, M.; Jaisamut, P.; Wiwattanapatapee, R.; Jørgensen, H.G.; Venkatpurwar, V.P.; Zhou, B.; Hoffmann, A.R.; Basu, R.; Guo, S.; et al. Nano-curcumin safely prevents streptozotocin-induced inflammation and apoptosis in pancreatic beta cells for effective management of Type 1 diabetes mellitus. Br. J. Pharmacol. 2017, 174, 2074–2084. [Google Scholar] [CrossRef] [Green Version]
- Libby, P. Inflammation and cardiovascular disease mechanisms. Am. J. Clin. Nutr. 2006, 83, 456S–460S. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tracy, R.P. Emerging relationships of inflammation, cardiovascular disease and chronic diseases of aging. Int. J. Obes. 2003, 27, S29–S34. [Google Scholar] [CrossRef] [Green Version]
- Tuomisto, K.; Jousilahti, P.; Sundvall, J.; Pajunen, P.; Salomaa, V. C-reactive protein, interleukin-6 and tumor necrosis factor alpha as predictors of incident coronary and cardiovascular events and total mortality. Thromb. Haemost. 2006, 95, 511–518. [Google Scholar] [CrossRef]
- He, Y.; Yue, Y.; Zheng, X.; Zhang, K.; Chen, S.; Du, Z. Curcumin, Inflammation, and Chronic Diseases: How Are They Linked? Molecules 2015, 20, 9183–9213. [Google Scholar] [CrossRef]
- Shehzad, A.; Rehman, G.; Lee, Y.S. Curcumin in inflammatory diseases. BioFactors 2012, 39, 69–77. [Google Scholar] [CrossRef] [PubMed]
- Deguchi, A. Curcumin Targets in Inflammation and Cancer. Endocr. Metab. Immune Disord. Drug Targets 2015, 15, 88–96. [Google Scholar] [CrossRef]
- Trivedi, M.K.; Mondal, S.C.; Gangwar, M.; Jana, S. Immunomodulatory potential of nanocurcumin-based formulation. Inflammopharmacology 2017, 25, 609–619. [Google Scholar] [CrossRef] [PubMed]
- Dolati, S.; Ahmadi, M.; Aghebti-Maleki, L.; Nikmaram, A.; Marofi, F.; Rikhtegar, R.; Ayromlou, H.; Yousefi, M. Nanocurcumin is a potential novel therapy for multiple sclerosis by influencing inflammatory mediators. Pharmacol. Rep. 2018, 70, 1158–1167. [Google Scholar] [CrossRef] [PubMed]
- Bisht, S.; Feldmann, G.; Soni, S.; Ravi, R.; Karikar, C.; Maitra, A.; Maitra, A. Polymeric nanoparticle-encapsulated curcumin (“nanocurcumin”): A novel strategy for human cancer therapy. J. Nanobiotechnol. 2007, 5, 3–18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kjeldsen, S.E. Hypertension and cardiovascular risk: General aspects. Pharmacol. Res. 2018, 129, 95–99. [Google Scholar] [CrossRef] [PubMed]
- Franklin, S.S.; GustinIV, W.; Wong, N.D.; Larson, M.G.; Weber, M.A.; Kannel, W.B.; Levy, D. Hemodynamic patterns of age-related changes in blood pressure: The Framingham Heart Study. Circulation 1997, 96, 308–315. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vishram, J.K.; Borglykke, A.; Andreasen, A.H.; Jeppesen, J.; Ibsen, H.; Jørgensen, T.; Broda, G.; Palmieri, L.; Giampaoli, S.; Donfrancesco, C.; et al. Impact of Age on the Importance of Systolic and Diastolic Blood Pressures for Stroke Risk. Hypertension 2012, 60, 1117–1123. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hadi, A.; Pourmasoumi, M.; Ghaedi, E.; Sahebkar, A. The effect of Curcumin/Turmeric on blood pressure modulation: A systematic review and meta-analysis. Pharmacol. Res. 2019, 150, 104505. [Google Scholar] [CrossRef]
- Azhdari, M.; Karandish, M.; Mansoori, A. Metabolic benefits of curcumin supplementation in patients with metabolic syndrome: A systematic review and meta-analysis of randomized controlled trials. Phytother. Res. 2019, 33, 1289–1301. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bhawana; Basniwal, R.K.; Buttar, H.S.; Jain, V.K.; Jain, N. Curcumin Nanoparticles: Preparation, Characterization, and Antimicrobial Study. J. Agric. Food Chem. 2011, 59, 2056–2061. [Google Scholar] [CrossRef]
- Aggarwal, B.B.; Harikumar, K.B. Potential therapeutic effects of curcumin, the anti-inflammatory agent, against neurodegenerative, cardiovascular, pulmonary, metabolic, autoimmune and neoplastic diseases. Int. J. Biochem. Cell Biol. 2009, 41, 40–59. [Google Scholar] [CrossRef] [Green Version]
- Suresh, S.; Sankar, P.; Telang, A.G.; Kesavan, M.; Sarkar, S.N. Nanocurcumin ameliorates Staphylococcus aureus-induced mastitis in mouse by suppressing NF-κB signaling and inflammation. Int. Immunopharmacol. 2018, 65, 408–412. [Google Scholar] [CrossRef]
- Rashidian, A.; Ghafari, H.; Chamanara, M.; Dehpour, A.; Muhammadnejad, A.; Akbarian, R.; Mousavi, S.E.; Rezayat, S. The protective effect of nano-curcumin in experimental model of acute pancreatitis: The involvement of TLR4/NF-kB pathway. Nanomed. J. 2018, 5, 138–143. [Google Scholar]
- Agrawal, A.; Cha-Molstad, H.; Samols, D.; Kushner, I. Overexpressed nuclear factor-κB can participate in endogenous C-reactive protein induction, and enhances the effects of C/EBPβ and signal transducer and activator of transcription-3. Immunology 2003, 108, 539–547. [Google Scholar] [CrossRef] [PubMed]
- Menon, V.P.; Sudheer, A.R. Antioxidant and Anti-Inflammatory Properties of Curcumin. Chem. Biol. Pteridines Folates 2007, 595, 105–125. [Google Scholar]
- Potphode, N.D.; Daunde, J.A.; Desai, S.S.; Walvekar, M.V. Nano-curcumin: A Potent Enhancer of Body Antioxidant System in Diabetic Mice. Int. J. Phytomed. 2018, 10, 162–167. [Google Scholar] [CrossRef]
- Accinni, R.; Rosina, M.; Bamonti, F.; Della Noce, C.; Tonini, A.; Bernacchi, F.; Campolo, J.; Caruso, R.; Novembrino, C.; Ghersi, L.; et al. Effects of combined dietary supplementation on oxidative and inflammatory status in dyslipidemic subjects. Nutr. Metab. Cardiovasc. Dis. 2006, 16, 121–127. [Google Scholar] [CrossRef]
- Shin, S.-K.; Ha, T.-Y.; McGregor, R.A.; Choi, M.-S. Long-term curcumin administration protects against atherosclerosis via hepatic regulation of lipoprotein cholesterol metabolism. Mol. Nutr. Food Res. 2011, 55, 1829–1840. [Google Scholar] [CrossRef]
- Jang, E.-M.; Choi, M.-S.; Jung, U.J.; Kim, M.-J.; Kim, H.-J.; Jeon, S.-M.; Shin, S.-K.; Seong, C.-N.; Lee, M.-K. Beneficial effects of curcumin on hyperlipidemia and insulin resistance in high-fat–fed hamsters. Metabolism 2008, 57, 1576–1583. [Google Scholar] [CrossRef]
- Ramírez-Boscá, A.; Soler, A.; A Carrión, M.; Díaz-Alperi, J.; Bernd, A.; Quintanilla, C.; Almagro, E.Q.; Miquel, J. An hydroalcoholic extract of Curcuma longa lowers the apo B/apo A ratio: Implications for atherogenesis prevention. Mech. Ageing Dev. 2000, 119, 41–47. [Google Scholar] [CrossRef]
- Tu, Y.; Sun, D.; Zeng, X.; Yao, N.; Huang, X.; Huang, D.; Chen, Y. Piperine potentiates the hypocholesterolemic effect of curcumin in rats fed on a high fat diet. Exp. Ther. Med. 2014, 8, 260–266. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Clark, C.C.; Ghaedi, E.; Arab, A.; Pourmasoumi, M.; Hadi, A. The effect of curcumin supplementation on circulating adiponectin: A systematic review and meta-analysis of randomized controlled trials. Diabetes Metab. Syndr. Clin. Res. Rev. 2019, 13, 2819–2825. [Google Scholar] [CrossRef] [PubMed]
- Tabrizi, R.; Vakili, S.; Akbari, M.; Mirhosseini, N.; Lankarani, K.B.; Rahimi, M.; Mobini, M.; Jafarnejad, S.; Vahedpoor, Z.; Asemi, Z. The effects of curcumin-containing supplements on biomarkers of inflammation and oxidative stress: A systematic review and meta-analysis of randomized controlled trials. Phytother. Res. 2019, 33, 253–262. [Google Scholar] [CrossRef] [PubMed]
- Parija, S.C.; Jandhyam, H.; Mohanty, B.P. Vasorelaxation to Eugenol, Curcumin and Nanocurcumin is mediated by differential augmentation of Na+, K+-ATPase activity in middle uterine artery of Capra hircus. Indian J. Tradit. Knowl. 2021, 20, 59–67. [Google Scholar]
- Chrissobolis, S.; Ziogas, J.; Chu, Y.; Faraci, F.M.; Sobey, C.G. Role of inwardly rectifying K(+) channels in K(+)-induced cerebral vasodilatation in vivo. Am. J. Physiol. Circ. Physiol. 2000, 279, H2704–H2712. [Google Scholar] [CrossRef]
- Haddy, F.J. The sodium-potassium pump in hypertension. Mechanisms of action of potassium. Arch. Mal. Coeur Vaiss. 1984, 77, 67–72. [Google Scholar]
- Shome, S.; Das Talukdar, A.; Choudhury, M.D.; Bhattacharya, M.K.; Upadhyaya, H. Curcumin as potential therapeutic natural product: A nanobiotechnological perspective. J. Pharm. Pharmacol. 2016, 68, 1481–1500. [Google Scholar] [CrossRef]
- Mozos, I. Crosstalk between Oxidative and Nitrosative Stress and Arterial Stiffness. Curr. Vasc. Pharmacol. 2017, 15, 446–456. [Google Scholar] [CrossRef]
- Nahar, P.P.; Slitt, A.L.; Seeram, N.P. Anti-Inflammatory Effects of Novel Standardized Solid Lipid Curcumin Formulations. J. Med. Food 2015, 18, 786–792. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zaki, S.M.; Algaleel, W.A.A.; Imam, R.A.; Soliman, G.F.; Ghoneim, F.M. Nano-curcumin versus curcumin in amelioration of deltamethrin-induced hippocampal damage. Histochem. Cell Biol. 2020, 154, 157–175. [Google Scholar] [CrossRef] [PubMed]
- Fakhri, S.; Shakeryan, S.; Alizadeh, A.; Shahryari, A. Effect of 6 Weeks of High Intensity Interval Training with Nano curcumin Supplement on Antioxidant Defense and Lipid Peroxidation in Overweight Girls-Clinical Trial. Iran. J. Diabetes Obes. 2020. [Google Scholar] [CrossRef]

| Studies | Country | Study Design | Participant | Sample Size and Sex | Sample Size | Trial Duration (Week) | Means Age | Means BMI | Intervention | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| IG | CG | IG | CG | IG | CG | Intervention Dose (mg/d) | Control Group | ||||||
| Vafadar_afshar et al., 2020 | Iran | Parallel = l, R, PC, DB | Hemodialysis Patients | M/F (F:20, M:34) | 27 | 27 | 12 | 55.33 ± 12.95 | 59.05 ± 7.68 | 26.1 ± 5.19 | 27.19 ± 5.19 | 120 | placebo |
| Jazayeri-Tehrani et al., 2019 | Iran | parallel, R, PC, DB | non-alcoholic fatty liver disease | M/F (F:38, M:46) | 42 | 42 | 12 | 41.8 ± 5.6 | 42.5 ± 6.2 | 30.6 ± 2.14 | 30.7 ± 2.35 | 40 | placebo |
| Abdolahi et al., 2017 | Iran | parallel, R, PC, DB | migraine patients | M/F (F:30, M:8) | 19 | 19 | 8 | 37.36 ± 8.49 | 36.57 ± 8.15 | 27.59 ± 4.57 | 26.94 ± 3.87 | 80 | placebo |
| Rahimi et al., 2016 | Iran | parallel, R, PC, DB | type 2 diabetic | M/F (F:39, M:31) | 35 | 35 | 12 | 56.34 ± 11.17 | 60.95 ±1 0.77 | 26.92 ± 2.71 | 27.27 ± 3.59 | 80 | placebo |
| Osali. 2020 (A) | Iran | parallel, R, PC, DB | metabolic syndrome | F:22 | 11 | 6 | 6 | 62.3 ± 1.23 | 62.3 ± 1.23 | 31.24 ± 3.12 | 32.22 ± 2.46 | 80 | placebo |
| Osali. 2020 (B) | Iran | parallel, R, PC, DB | metabolic syndrome | F:22 | 11 | 5 | 6 | 62.3 ± 1.23 | 62.3 ± 1.23 | 29.54 ± 2.67 | 29.02 ± 1.56 | 80 | placebo |
| Asadi et al., 2019 | Iran | parallel, R, PC, DB | type 2 diabetes | M/F (F:70, M:10) | 40 | 40 | 8 | 53.3 ± 6.5 | 54.6 ± 6.2 | 31.1 ± 4.2 | 30.8 ± 3.8 | 80 | placebo |
| Bateni et al., 2021 | Iran | parallel, R, PC, DB | metabolic syndrome | M/F (F:33, M:10) | 22 | 21 | 12 | 50 ± 9 | 54 ± 7 | 29.9 ± 4.3 | 29.4 ± 4.5 | 80 | placebo |
| Abdolahi et al., 2018 (A) | Iran | parallel, R, PC, DB | Migraine | M/F (F:29, M:7) | 17 | 10 | 8 | 35.82 ± 8.2 | 36.15 ± 8.67 | 26.02 ± 4.04 | 26.16 ± 4.27 | 80 | placebo |
| Abdolahi et al., 2018 (B) | Iran | parallel, R, PC, DB | Migraine | M/F (F:30, M:8) | 19 | 9 | 8 | 37.36 ± 8.5 | 36.57 ± 8.15 | 27.59 ± 4.57 | 26.94 ± 3.87 | 80 | placebo |
| Shafabakhsh et al., 2020 | Iran | parallel, R, PC, DB | Diabetes on Hemodialysis | M/F (F:21, M:32) | 26 | 27 | 12 | 58.3 ± 9.4 | 56.2 ± 9.8 | 27.9 ± 4.9 | 27.1 ± 4.2 | 80 | placebo |
| No | WMD (95%CI) | P within Group | Heterogeneity | ||||
|---|---|---|---|---|---|---|---|
| P Heterogeneity | I2 | P between Subgroups | Tau-Squared | ||||
| Subgroup analyses of nano-curcumin supplementation on TG. | |||||||
| Overall effect | 7 | −9.76 (−32.71, 13.17) | 0.404 | <0.001 | 79.2% | 696.43 | |
| Baseline TG (mg/dL) | |||||||
| <150 | 2 | 25.53 (−21.73, 72.79) | 0.290 | 0.005 | 87.6% | <0.001 | 1000 |
| ≥150 | 5 | −24.87 (−37.34, −12.40) | <0.001 | 0.445 | 0.0% | 0.0 | |
| Trial duration (week) | |||||||
| <12 | 2 | −17.61 (−44.44, 9.21) | 0.198 | 0.456 | 0.0% | 0.454 | 0.0 |
| ≥12 | 5 | −8.05 (−37.44, 21.34) | 0.591 | <0.001 | 85.6% | 893.41 | |
| Health status | |||||||
| Type 2 diabetic | 2 | 16.25 (−51.16, 83.67) | 0.637 | <0.001 | 92.2% | 0.028 | 2200 |
| Metabolic syndrome | 3 | −29.11 (−61.92, 3.68) | 0.082 | 0.191 | 39.5% | 334.45 | |
| Other | 2 | −12.37 (−41.97, 17.22) | 0.412 | 0.018 | 82.1% | 374.19 | |
| BMI baseline | |||||||
| Overweight (25–29.9 kg/m2) | 5 | −2.74 (−32.87, 27.38) | 0.858 | <0.001 | 80.0% | 0.003 | 874.72 |
| Obese (>30 kg/m2) | 2 | −27.23 (−43.11, −11.35) | 0.001 | 0.948 | 0.0% | 0.0 | |
| Overall analyses of nano-curcumin supplementation on TC | |||||||
| Overall effect | 5 | −3.34 (−14.43, 7.73) | 0.554 | 0.001 | 77.2% | 115.21 | |
| Baseline TC (mg/dL) | |||||||
| <200 | 4 | −0.53 (−15.66, 14.60) | 0.945 | 0.005 | 77.0% | 0.033 | 179.57 |
| ≥200 | 1 | −10.90 (−16.40, −5.39) | <0.001 | - | - | 0.0 | |
| Health status | |||||||
| Type 2 diabetic | 2 | −6.24 (−35.65, 23.17) | 0.678 | 0.001 | 90.9% | 0.185 | 409.66 |
| Metabolic syndrome | 1 | 10.40 (−11.09, 31.89) | 0.343 | - | - | 0.0 | |
| Other | 2 | −5.65 (−18.59, 7.28) | 0.392 | 0.074 | 68.8% | 63.22 | |
| BMI baseline | |||||||
| Overweight (25–29.9 kg/m2) | 4 | −0.53 (−15.66, 14.60) | 0.945 | 0.005 | 77.0% | 0.033 | 179.57 |
| Obese (>30 kg/m2) | 1 | −10.90 (−16.40, −5.39) | <0.001 | - | - | 0.0 | |
| Subgroup analyses of nano-curcumin supplementation on LDL-C | |||||||
| Overall effect | 5 | −3.59 (−15.74, 8.56) | 0.562 | <0.001 | 84.8% | 150.46 | |
| Baseline LDL-C (mg/dL) | |||||||
| <100 | 4 | −0.14 (−15.65, 15.37) | 0.986 | 0.001 | 82.8% | 0.003 | 196.19 |
| ≥100 | 1 | −13.70 (−19.26, −8.13) | <0.001 | - | - | 0.0 | |
| Health status | |||||||
| Type 2 diabetic | 2 | −4.72 (−34.37, 24.91) | 0.755 | <0.001 | 93.5% | 0.028 | 427.83 |
| Metabolic syndrome | 1 | 16.50 (−9.06, 42.06) | 0.206 | - | - | 0.0 | |
| Other | 2 | −8.61 (−20.37, 3.13) | 0.151 | 0.056 | 72.7% | 53.72 | |
| BMI baseline | |||||||
| Overweight (25–29.9 kg/m2) | 4 | −0.14 (−15.65, 15.37) | 0.986 | 0.001 | 82.8% | 0.003 | 196.19 |
| Obese (>30 kg/m2) | 1 | −13.70 (−19.26, −8.13) | <0.001 | - | - | 0.0 | |
| Subgroup analyses of nano-curcumin supplementation on HDL-C | |||||||
| Overall effect | 7 | 5.77 (2.90, 8.64) | <0.001 | <0.001 | 83.5% | 11.41 | |
| Baseline HDL-C (mg/dL) | |||||||
| <40 | 2 | 2.01 (0.21, 3.80) | 0.028 | 0.875 | 0.0% | <0.001 | 0.0 |
| ≥40 | 5 | 7.61 (5.34, 9.89) | <0.001 | 0.079 | 52.3% | 3.22 | |
| Trial duration (week) | |||||||
| <12 | 2 | 5.62 (3.06, 8.18) | <0.001 | 0.293 | 9.5% | 0.779 | 0.32 |
| ≥12 | 5 | 5.92 (1.93, 9.90) | 0.004 | <0.001 | 88.6% | 16.57 | |
| Health status | |||||||
| Type 2 diabetic | 2 | 6.84 (−2.85, 16.53) | 0.167 | <0.001 | 93.4% | 0.021 | 45.77 |
| Metabolic syndrome | 3 | 5.66 (3.34, 7.98) | <0.001 | 0.574 | 0.0% | 0.0 | |
| Other | 2 | 5.31 (−1.26, 11.88) | 0.113 | <0.001 | 91.9% | 20.75 | |
| BMI baseline | |||||||
| Overweight (25–29.9 kg/m2) | 5 | 5.42 (1.78, 9.05) | 0.003 | 0.001 | 79.9% | 0.001 | 12.74 |
| Obese (>30 kg/m2) | 2 | 6.66 (2.46, 10.85) | 0.002 | 0.034 | 77.7% | 7.28 | |
| Subgroup analyses of nano-curcumin supplementation on FBS | |||||||
| Overall effect | 8 | −18.14 (−29.31, −6.97) | 0.001 | <0.001 | 84.9% | 170.85 | |
| Baseline FBS (mg/dL) | |||||||
| <100 | 1 | −1.70 (−3.18, −0.21) | 0.025 | - | - | <0.001 | 0.0 |
| ≥100 | 7 | −22.43 (−36.02, −8.84) | 0.001 | <0.001 | 76.2% | 220.96 | |
| Trial duration (week) | |||||||
| <12 | 3 | −31.20 (−57.78, −4.61) | 0.021 | 0.087 | 59.1% | <0.001 | 330.04 |
| ≥12 | 5 | −13.77 (−25.80, −1.73) | 0.025 | <0.001 | 86.2% | 139.70 | |
| Health status | |||||||
| Type 2 diabetic | 3 | −27.07 (−39.61, −14.52) | <0.001 | 0.112 | 54.4% | <0.001 | 66.60 |
| Metabolic syndrome | 3 | −28.29 (−63.34, 6.76) | 0.114 | 0.041 | 68.7% | 655.74 | |
| Other | 2 | −1.74 (−3.20, −0.28) | 0.019 | 0.736 | 0.0% | 0.0 | |
| BMI baseline | |||||||
| Overweight (25–29.9 kg/m2) | 5 | −24.53 (−43.50, −5.55) | 0.011 | <0.001 | 83.8% | <0.001 | 355.24 |
| Obese (>30 kg/m2) | 3 | −10.50 (−25.81, 4.79) | 0.178 | 0.018 | 75.1% | 119.83 | |
| Subgroup analyses of nano-curcumin supplementation on fasting insulin | |||||||
| Overall effect | 3 | −1.21 (−1.43, −1.00) | <0.001 | 0.593 | 0.0% | 0.0 | |
| Subgroup analyses of nano-curcumin supplementation on hemoglubin A1c | |||||||
| Overall effect | 4 | −0.66 (−1.41, 0.08) | 0.081 | <0.001 | 94.5% | 0.51 | |
| Subgroup analyses of nano-curcumin supplementation on HOMA-IR | |||||||
| Overall effect | 3 | −0.28 (−0.33, −0.23) | <0.001 | 0.654 | 0.0% | 0.0 | |
| Subgroup analyses of nano-curcumin supplementation on SBP | |||||||
| Overall effect | 5 | −7.09 (−12.98, −1.20) | <0.001 | 0.018 | 83.0% | 33.22 | |
| Baseline SBP (mmHg) | |||||||
| <120 | 1 | −2.50 (−11.58, 6.58) | 0.590 | - | - | 0.868 | 0.0 |
| ≥120 | 4 | −8.21 (−15.21, −1.22) | 0.021 | <0.001 | 87.2% | 40.64 | |
| Trial duration (week) | |||||||
| <12 | 2 | −16.65 (−22.98, −10.33) | <0.001 | 0.710 | 0.0% | <0.001 | 0.0 |
| ≥12 | 3 | −1.19 (−2.39, 0.00) | 0.050 | 0.552 | 0.0% | 0.0 | |
| Health status | |||||||
| Type 2 diabetic | 1 | −3.60 (−8.27, 1.07) | 0.131 | <0.001 | |||
| Metabolic syndrome | 3 | −11.98 (−21.29, −2.68) | 0.012 | 0.040 | 68.9% | 46.55 | |
| Other | 1 | −1.00 (−2.25, 0.25) | 0.118 | ||||
| BMI baseline | |||||||
| Overweight (25–29.9 kg/m2) | 3 | −6.79 (−14.20, 0.62) | 0.073 | 0.049 | 66.8% | 0.034 | 28.45 |
| Obese (>30 kg/m2) | 2 | −8.82 (−25.33, 7.69) | 0.295 | <0.001 | 92.3% | 131.80 | |
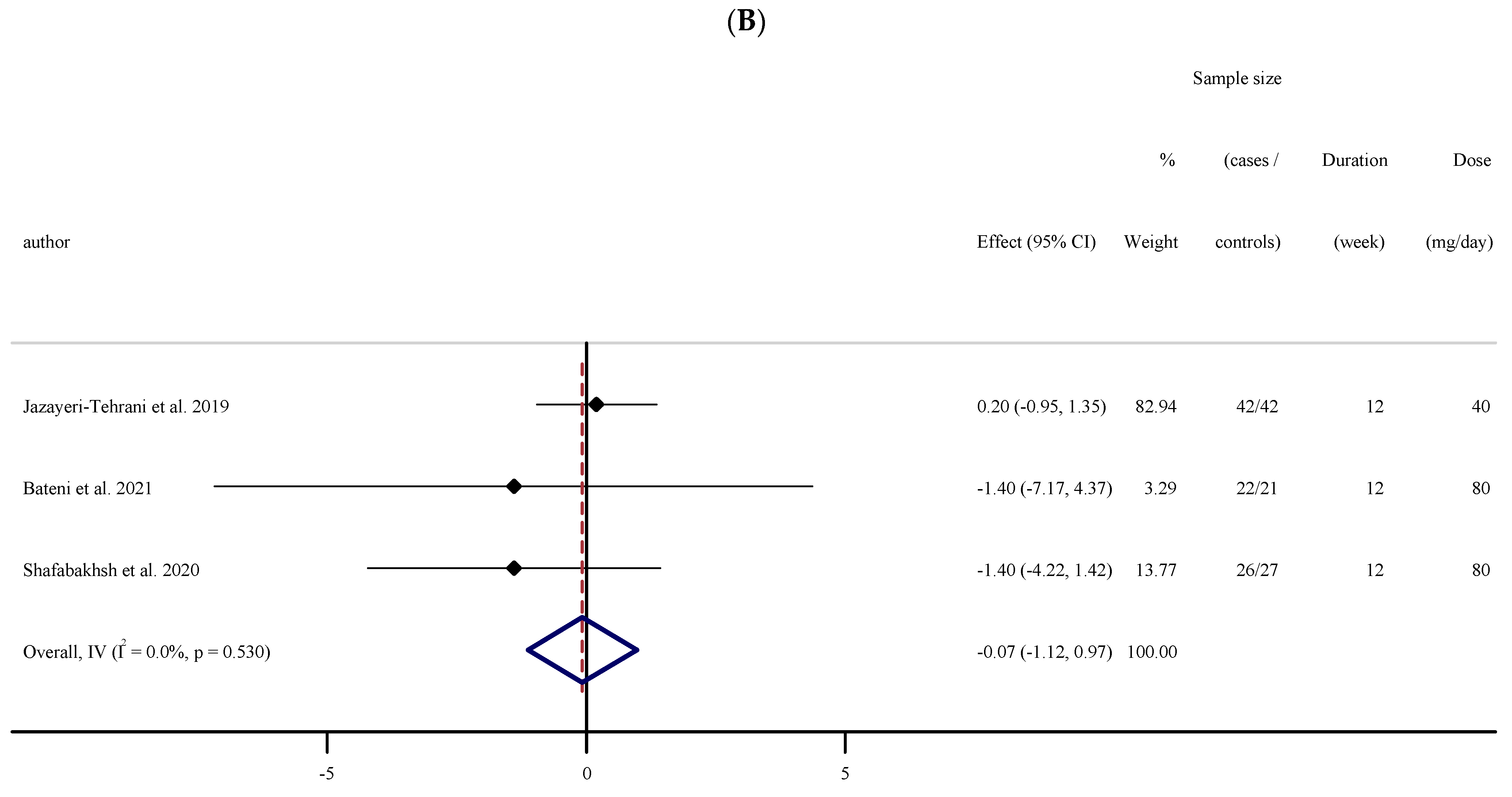
| Subgroup analyses of nano-curcumin supplementation on DBP | |||||||
| Overall effect | 3 | −0.07 (−1.12, 0.97) | 0.891 | 0.530 | 0.0% | 0.0 | |
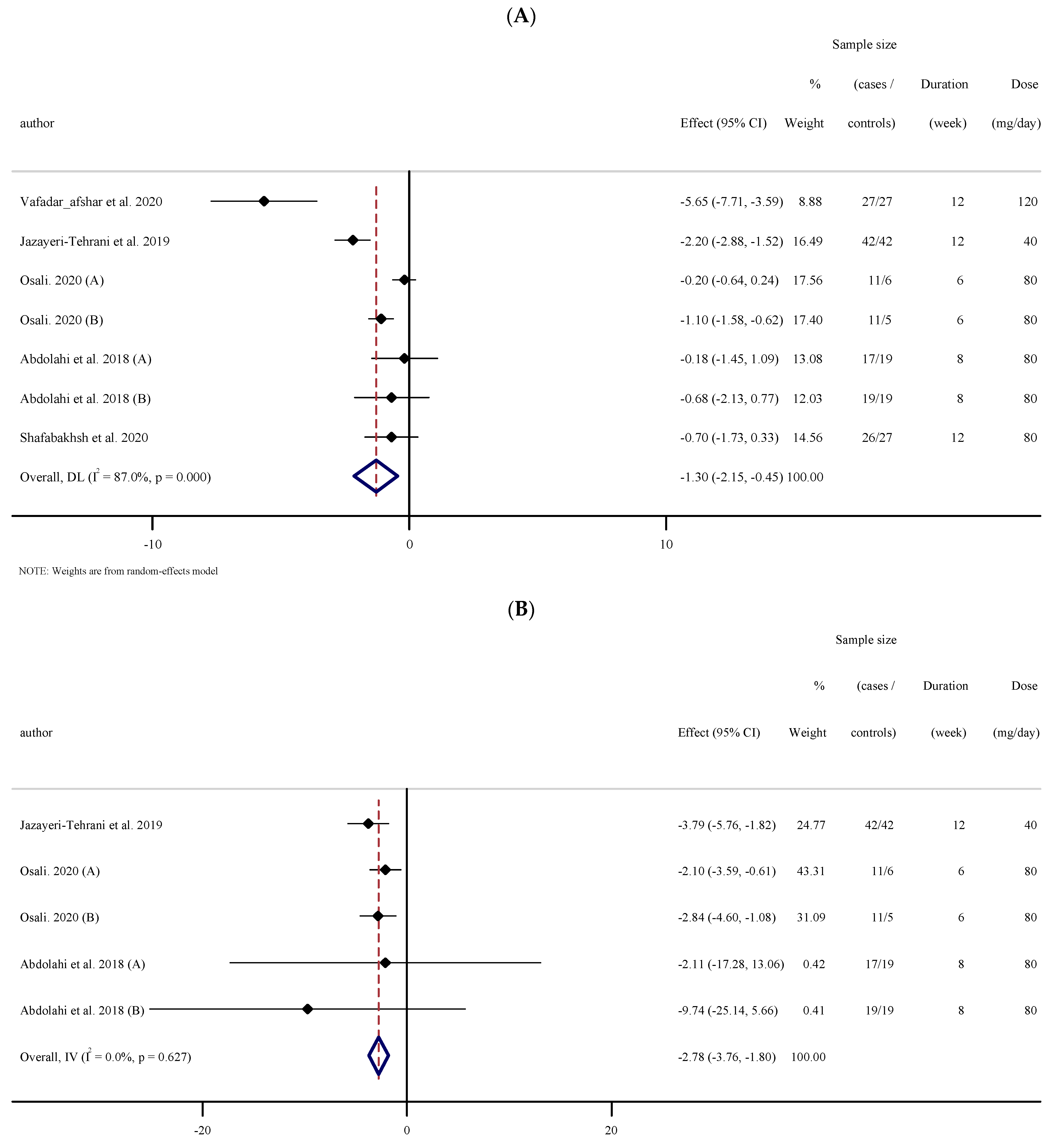
| Subgroup analyses of nano-curcumin supplementation on CRP | |||||||
| Overall effect | 7 | −1.29 (−2.15, −0.44) | 0.003 | <0.001 | 87.0% | 1.02 | |
| Baseline CRP (mg/L) | |||||||
| <3 | 2 | −0.64 (−1.52, 0.23) | 0.152 | 0.007 | 86.2% | 0.001 | 0.34 |
| ≥3 | 5 | −1.71 (−3.08, −0.35) | 0.014 | <0.001 | 85.2% | 1.98 | |
| Trial duration (week) | |||||||
| <12 | 4 | −0.57 (−1.17, 0.01) | 0.057 | 0.054 | 60.8% | <0.001 | 0.19 |
| ≥12 | 3 | −2.61 (−4.58, −0.64) | 0.009 | <0.001 | 89.2% | 2.58 | |
| Health status | |||||||
| Type 2 diabetic | 1 | −0.70 (−1.72, 0.32) | 0.181 | - | - | 0.000 | 0.0 |
| Metabolic syndrome | 2 | −0.64 (−1.52, −1.52) | 0.152 | 0.007 | 86.2% | 0.34 | |
| Migraine | 2 | −0.39 (−1.35, 0.55) | 0.415 | 0.611 | 0.0% | 0.0 | |
| Other | 2 | −3.78 (−7.15, −0.41) | 0.028 | 0.002 | 89.7% | 5.33 | |
| BMI baseline | |||||||
| Overweight (25–29.9 kg/m2) | 5 | −1.40 (−2.55, −0.25) | 0.017 | <0.001 | 81.5% | 0.286 | 1.30 |
| Obese (>30 kg/m2) | 2 | −1.18 (−3.14, 0.77) | 0.237 | <0.001 | 95.7% | 1.91 | |
| Subgroup analyses of nano-curcumin supplementation on IL-6 | |||||||
| Overall effect | 5 | −2.78 (−3.76, −1.79) | <0.001 | 0.627 | 0.0% | 0.0 | |
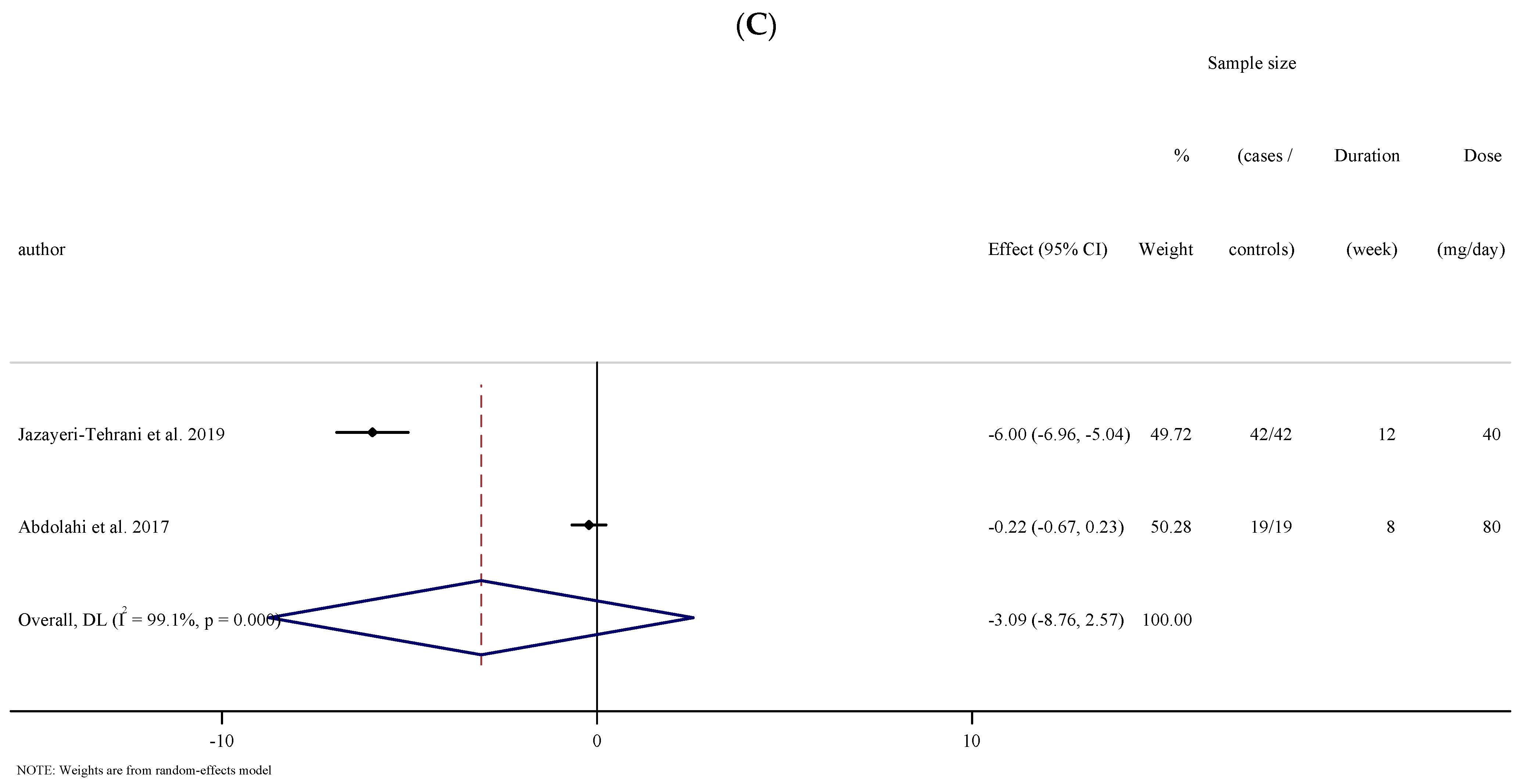
| Subgroup analyses of nano-curcumin supplementation on TNF-α | |||||||
| Overall effect | 2 | −3.09 (−8.75, 2.57) | 0.284 | <0.001 | 99.1% | 16.55 | |
| Subgroup analyses of nano-curcumin supplementation on body mass | |||||||
| Overall effect | 5 | −0.51 (−1.85, 0.82) | 0.449 | 0.974 | 0.0% | 0.0 | |
| Subgroup analyses of nano-curcumin supplementation on BMI | |||||||
| Overall effect | 7 | −0.35 (−0.76, 0.04) | 0.079 | 0.207 | 29.0% | 0.13 | |
| Subgroup analyses of nano-curcumin supplementation on WC | |||||||
| Overall effect | 5 | −1.32 (−3.89, 1.23) | 0.310 | 0.015 | 67.4% | 5.26 | |
| Subgroup analyses of nano-curcumin supplementation on FM | |||||||
| Overall effect | 4 | −0.86 (−1.95, 0.23) | 0.123 | 0.371 | 4.3% | 0.06 | |
| Quality Assessment | Summary of Findings | Quality of Evidence | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Outcomes | Risk of Bias | Inconsistency | Indirectness | Imprecision | Publication Bias | Number of Intervention/Control | WMD (95%CI) | Heterogeneity (I2) | |
| TG | No serious limitations | Very serious Limitations | No serious limitations | Serious Limitations | No serious limitations | 174/163 | −9.76 (−32.71, 13.17) | 79.2% | ⊕◯◯◯ Very low |
| TC | No serious limitations | Very serious Limitations | No serious limitations | Serious Limitations | No serious limitations | 152/152 | −3.34 (−14.43, 7.73) | 77.2% | ⊕◯◯◯ Very low |
| LDL-C | No serious limitations | Very serious Limitations | No serious limitations | Serious Limitations | No serious limitations | 152/152 | −3.59 (−15.74, 8.56) | 84.8% | ⊕◯◯◯ Very low |
| HDL-C | No serious limitations | Very serious Limitations | No serious limitations | No serious limitations | No serious limitations | 174/163 | 5.77 (2.90, 8.64) | 83.5% | ⊕⊕◯◯ Low |
| FBG | No serious limitations | Very serious Limitations | No serious limitations | No serious limitations | Serious Limitations | 214/203 | −18.14 (−29.31, −6.97) | 84.9% | ⊕◯◯◯ Very low |
| Fasting insulin | No serious limitations | No serious limitations | No serious limitations | No serious limitations | No serious limitations | 90/90 | −1.21 (−1.43, −1.00) | 0.0% | ⊕⊕⊕⊕ High |
| HbA1c | No serious limitations | Very serious Limitations | No serious limitations | Serious Limitations | No serious limitations | 139/138 | −0.66 (−1.41, 0.08) | 94.5% | ⊕◯◯◯ Very low |
| HOMA-IR | No serious limitations | No serious limitations | No serious limitations | No serious limitations | No serious limitations | 90/90 | −0.28 (−0.33, −0.23) | 0.0% | ⊕⊕⊕⊕ High |
| SBP | No serious limitations | Very serious Limitations | No serious limitations | No serious limitations | No serious limitations | 112/101 | −7.09 (−12.98, −1.20) | 83.2% | ⊕⊕◯◯ Low |
| DBP | No serious limitations | No serious limitations | No serious limitations | Serious Limitations | No serious limitations | 90/90 | −0.07 (−1.12, 0.97) | 0.0% | ⊕⊕⊕◯ Moderate |
| CRP | No serious limitations | Very serious Limitations | No serious limitations | No serious limitations | No serious limitations | 153/126 | −1.29 (−2.15, −0.44) | 87.0% | ⊕⊕◯◯ Low |
| IL-6 | No serious limitations | No serious limitations | No serious limitations | No serious limitations | No serious limitations | 100/72 | −2.78 (−3.76, −1.79) | 0.0% | ⊕⊕⊕⊕ High |
| TNF-α | No serious limitations | Very serious Limitations | No serious limitations | Serious Limitations | No serious limitations | 61/61 | −3.09 (−8.75, 2.57) | 99.1% | ⊕◯◯◯ Very low |
| Body weight | No serious limitations | No serious limitations | No serious limitations | Serious Limitations | Serious Limitations | 126/114 | −0.51 (−1.85, 0.82) | 0.0% | ⊕⊕◯◯ Low |
| BMI | No serious limitations | No serious limitations | No serious limitations | Serious Limitations | No serious limitations | 188/176 | −0.35 (−0.76, 0.04) | 29.0% | ⊕⊕⊕◯ Moderate |
| WC | No serious limitations | Serious Limitations | No serious limitations | Serious Limitations | No serious limitations | 126/114 | −1.32 (−3.89, 1.23) | 67.4% | ⊕⊕◯◯ Low |
| FM | No serious limitations | No serious limitations | No serious limitations | Serious Limitations | No serious limitations | 86/74 | −0.86 (−1.95, 0.23) | 4.3% | ⊕⊕⊕◯ Moderate |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ashtary-Larky, D.; Rezaei Kelishadi, M.; Bagheri, R.; Moosavian, S.P.; Wong, A.; Davoodi, S.H.; Khalili, P.; Dutheil, F.; Suzuki, K.; Asbaghi, O. The Effects of Nano-Curcumin Supplementation on Risk Factors for Cardiovascular Disease: A GRADE-Assessed Systematic Review and Meta-Analysis of Clinical Trials. Antioxidants 2021, 10, 1015. https://doi.org/10.3390/antiox10071015
Ashtary-Larky D, Rezaei Kelishadi M, Bagheri R, Moosavian SP, Wong A, Davoodi SH, Khalili P, Dutheil F, Suzuki K, Asbaghi O. The Effects of Nano-Curcumin Supplementation on Risk Factors for Cardiovascular Disease: A GRADE-Assessed Systematic Review and Meta-Analysis of Clinical Trials. Antioxidants. 2021; 10(7):1015. https://doi.org/10.3390/antiox10071015
Chicago/Turabian StyleAshtary-Larky, Damoon, Mahnaz Rezaei Kelishadi, Reza Bagheri, Seyedeh Parisa Moosavian, Alexei Wong, Sayed Hossein Davoodi, Pardis Khalili, Frédéric Dutheil, Katsuhiko Suzuki, and Omid Asbaghi. 2021. "The Effects of Nano-Curcumin Supplementation on Risk Factors for Cardiovascular Disease: A GRADE-Assessed Systematic Review and Meta-Analysis of Clinical Trials" Antioxidants 10, no. 7: 1015. https://doi.org/10.3390/antiox10071015
APA StyleAshtary-Larky, D., Rezaei Kelishadi, M., Bagheri, R., Moosavian, S. P., Wong, A., Davoodi, S. H., Khalili, P., Dutheil, F., Suzuki, K., & Asbaghi, O. (2021). The Effects of Nano-Curcumin Supplementation on Risk Factors for Cardiovascular Disease: A GRADE-Assessed Systematic Review and Meta-Analysis of Clinical Trials. Antioxidants, 10(7), 1015. https://doi.org/10.3390/antiox10071015










