Spasticity Management in Disorders of Consciousness
Abstract
1. Introduction
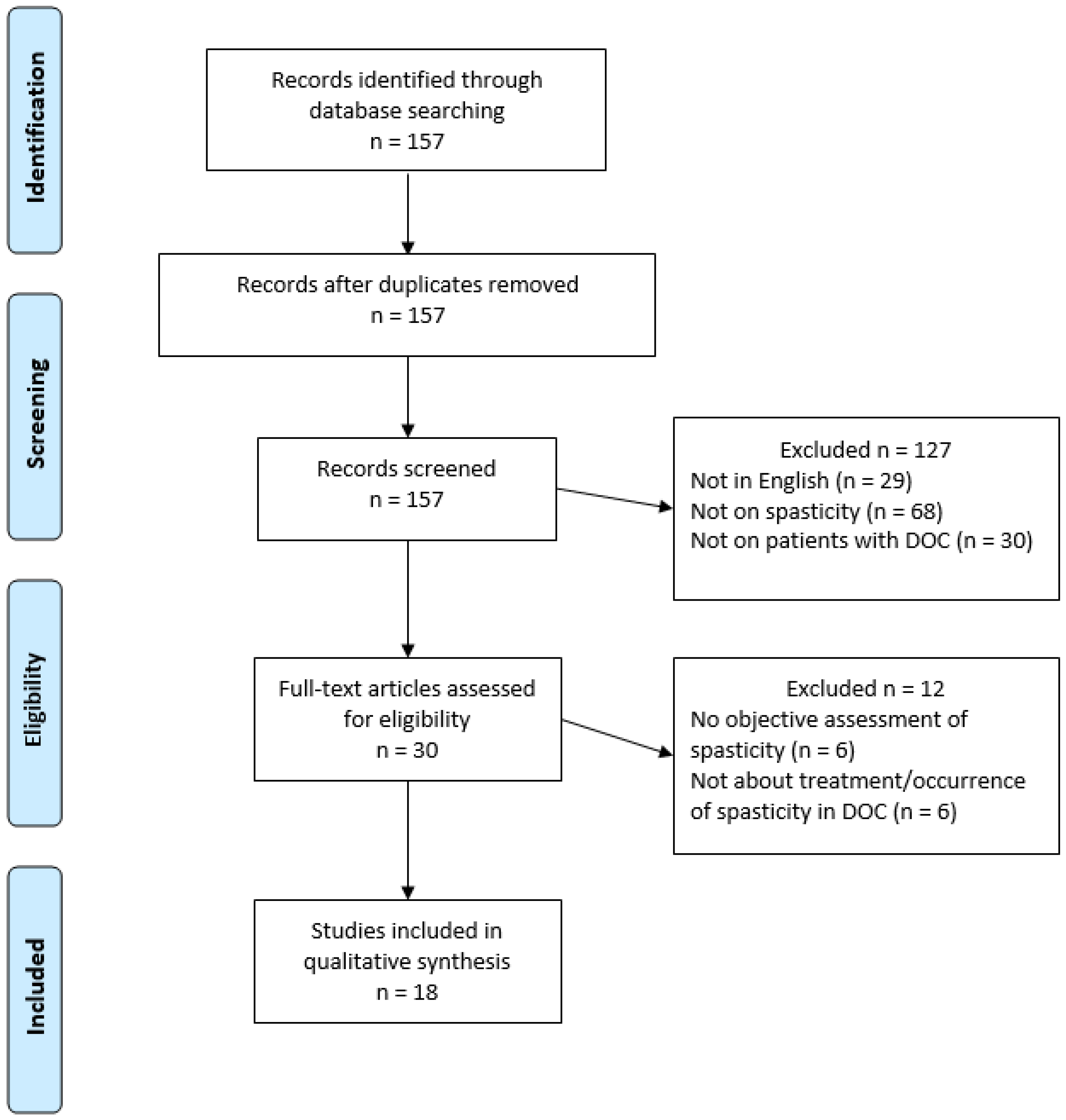
2. Materials and Methods
3. Results
3.1. Occurrence of Spasticity in DOC Patients
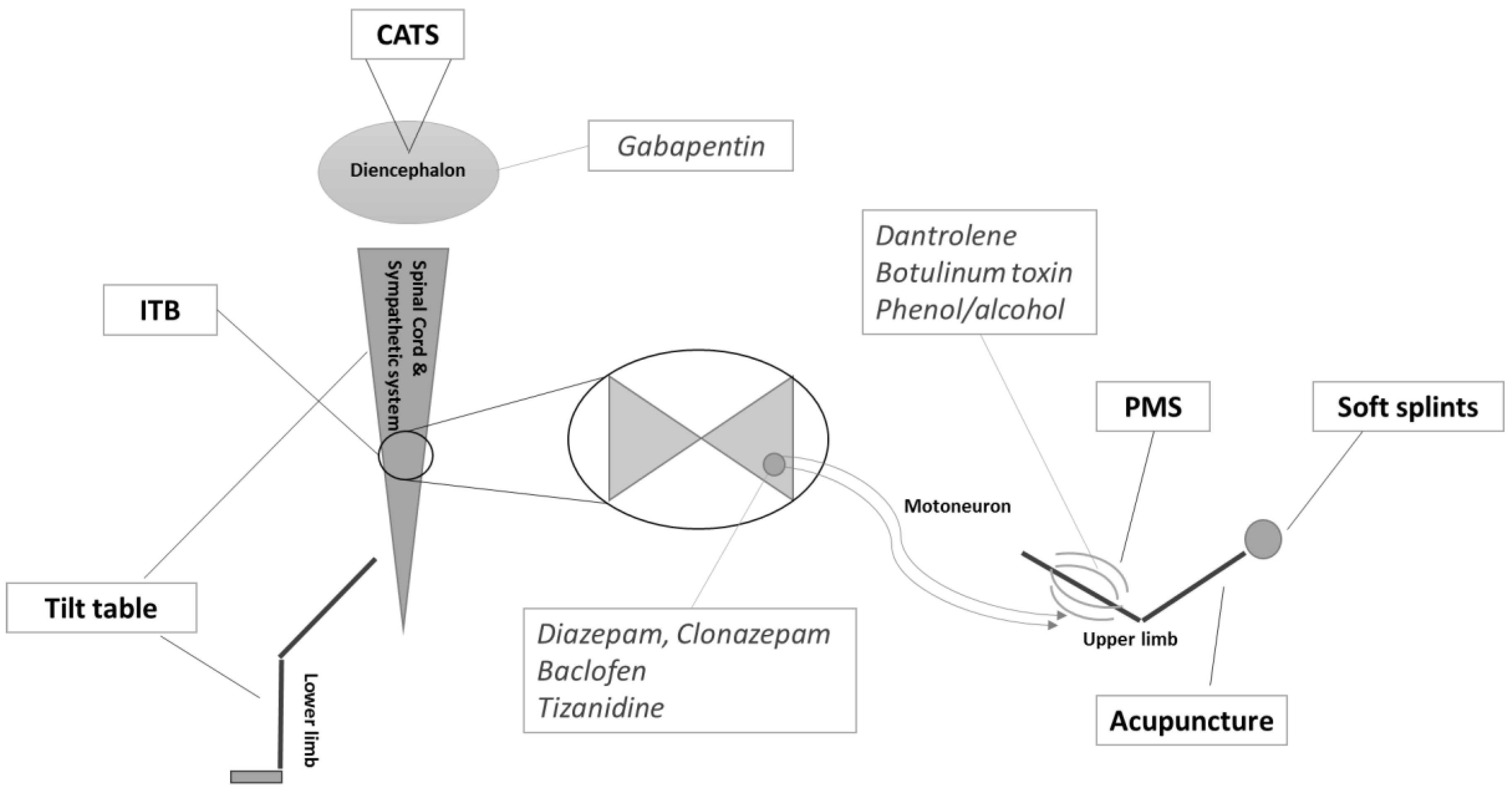
3.2. Treatments Targetting Spasticity in DOC Patients
3.3. Treatments with Spasticity as a Secondary Outcome in DOC Patients
4. Discussion
5. Conclusion
Acknowledgments
Conflicts of Interest
References
- Laureys, S.; Celesia, G.G.; Cohadon, F.; Lavrijsen, J.; Leon-Carrion, J.; Sannita, W.G.; Sazbon, L.; Schmutzhard, E.; von Wild, K.R.; Zeman, A.; et al. Unresponsive wakefulness syndrome: A new name for the vegetative state or apallic syndrome. BMC Med. 2010, 8, 68. [Google Scholar] [CrossRef] [PubMed]
- Giacino, J.T.; Ashwal, S.; Childs, N.; Cranford, R.; Jennett, B.; Katz, D.I.; Kelly, J.P.; Rosenberg, J.H.; Whyte, J.; Zafonte, R.D.; et al. The minimally conscious state: Definition and diagnostic criteria. Neurology 2002, 58, 349–353. [Google Scholar] [CrossRef] [PubMed]
- Thibaut, A.; Chatelle, C.; Wannez, S.; Deltombe, T.; Stender, J.; Schnakers, C.; Laureys, S.; Gosseries, O. Spasticity in disorders of consciousness: A behavioral study. Eur. J. Phys. Rehabil. Med. 2015, 51, 389–397. [Google Scholar] [PubMed]
- Lance, J.W. Spasticity: Disorders Motor Control. Symposium Synopsis; Feldman, R.G., Young, R.P., Koella, W.P., Eds.; Year Book Medical Publishers: Miami, FL, USA, 1980. [Google Scholar]
- Dietz, V.; Sinkjaer, T. Spastic movement disorder: Impaired reflex function and altered muscle mechanics. Lancet Neurol. 2007, 6, 725–733. [Google Scholar] [CrossRef]
- Burke, D.; Wissel, J.; Donnan, G.A. Pathophysiology of spasticity in stroke. Neurology 2013, 80 (Suppl. S2), S20–S26. [Google Scholar] [CrossRef] [PubMed]
- Gracies, J.M. Pathophysiology of spastic paresis. I: Paresis and soft tissue changes. Muscle Nerve 2005, 31, 535–551. [Google Scholar] [CrossRef] [PubMed]
- Wissel, J.; Schelosky, L.D.; Scott, J.; Christe, W.; Faiss, J.H.; Mueller, J. Early development of spasticity following stroke: A prospective, observational trial. J. Neurol. 2010, 257, 1067–1072. [Google Scholar] [CrossRef] [PubMed]
- McClelland, S.; Bethoux, F.A.; Boulis, N.M.; Sutliff, M.H.; Stough, D.K.; Schwetz, K.M.; Gogol, D.M.; Harrison, M.; Pioro, E.P. Intrathecal baclofen for spasticity-related pain in amyotrophic lateral sclerosis: Efficacy and factors associated with pain relief. Muscle Nerve 2008, 37, 396–398. [Google Scholar] [CrossRef] [PubMed]
- Shiel, A.; Gelling, L.; Wilson, B.; Coleman, M.; Pickard, J. Difficulties in diagnosing the vegetative state. Br. J. Neurosurg. 2004, 18, 5–7. [Google Scholar] [CrossRef] [PubMed]
- Giacino, J.T.; Whyte, J.; Bagiella, E.; Kalmar, K.; Childs, N.; Khademi, A.; Eifert, B.; Long, D.; Katz, D.I.; Cho, S.; et al. Placebo-controlled trial of amantadine for severe traumatic brain injury. N. Engl. J. Med. 2012, 366, 819–826. [Google Scholar] [CrossRef] [PubMed]
- Thibaut, A.; Bruno, M.-A.; Ledoux, D.; Demertzi, A.; Laureys, S. tDCS in patients with disorders of consciousness: Sham-controlled randomized double-blind study. Neurology 2014, 82, 1112–1128. [Google Scholar] [CrossRef] [PubMed]
- Monti, M.M.; Schnakers, C.; Korb, A.S.; Bystritsky, A.; Vespa, P.M. Non-Invasive Ultrasonic Thalamic Stimulation in Disorders of Consciousness after Severe Brain Injury: A First-in-Man Report. Brain Stimul. 2016, 9, 940–941. [Google Scholar] [CrossRef] [PubMed]
- Burchiel, K.J.; Hsu, F.P.K. Pain and Spasticity After Spinal Cord Injury Mechanisms and Treatment. Spine 2001, 26, 146–160. [Google Scholar] [CrossRef]
- Ward, A.B. A summary of spasticity management—A treatment algorithm. Eur. J. Neurol. 2002, 9, 48–52. [Google Scholar] [CrossRef] [PubMed]
- Chatelle, C.; De Val, M.D.; Catano, A.; Chaskis, C.; Seeldrayers, P.; Laureys, S.; Biston, P.; Schnakers, C. Is the Nociception Coma Scale-Revised a Useful Clinical Tool for Managing Pain in Patients with Disorders of Consciousness? Clin. J. Pain. 2016, 32, 321–326. [Google Scholar] [CrossRef] [PubMed]
- Nakase-Richardson, R.; McNamee, S.; Howe, L.L.; Massengale, J.; Peterson, M.; Barnett, S.D.; Harris, O.; McCarthy, M.; Tran, J.; Scott, S.; et al. Descriptive characteristics and rehabilitation outcomes in active duty military personnel and veterans with disorders of consciousness with combat- and noncombat-related brain injury. Arch. Phys. Med. Rehabil. 2013, 94, 1861–1869. [Google Scholar] [CrossRef] [PubMed]
- Ganesh, S.; Guernon, A.; Chalcraft, L.; Harton, B.; Smith, B.; Louise-Bender Pape, T. Medical comorbidities in disorders of consciousness patients and their association with functional outcomes. Arch. Phys. Med. Rehabil. 2013, 94, 1899–1907. [Google Scholar] [CrossRef] [PubMed]
- Thibaut, A.; Deltombe, T.; Wannez, S.; Gosseries, O.; Ziegler, E.; Dieni, C.; Deroy, M.; Laureys, S. Impact of soft splints on upper limb spasticity in chronic patients with disorders of consciousness: A randomized, single-blind, controlled trial. Brain Inj. 2015, 29, 830–836. [Google Scholar] [CrossRef] [PubMed]
- Matsumoto-Miyazaki, J.; Asano, Y.; Ikegame, Y.; Kawasaki, T.; Nomura, Y.; Shinoda, J. Acupuncture Reduces Excitability of Spinal Motor Neurons in Patients with Spastic Muscle Overactivity and Chronic Disorder of Consciousness Following Traumatic Brain Injury. J. Altern. Complement. Med. 2016, 22, 895–902. [Google Scholar] [CrossRef] [PubMed]
- Shrestha, P.; Malla, H.; Pant, B.; Taira, T. Intrathecal baclofen therapy in severe head injury, first time in Nepal, a technique suitable for underdeveloped countries. Asian J. Neurosurg. 2011, 6, 49–51. [Google Scholar] [PubMed]
- Francois, B.; Vacher, P.; Roustan, J.; Salle, J.Y.; Vidal, J.; Moreau, J.J.; Vignon, P. Intrathecal baclofen after traumatic brain injury: Early treatment using a new technique to prevent spasticity. J. Trauma—Inj. Infect. Crit. Care 2001, 50, 158–161. [Google Scholar] [CrossRef]
- Leong, B. The vegetative and minimally conscious states in children: Spasticity, muscle contracture and issues for physiotherapy treatment. Brain Inj. 2002, 16, 217–230. [Google Scholar] [CrossRef] [PubMed]
- Leong, B. Critical review of passive muscle stretch: Implications for the treatment of children in vegetative and minimally conscious states. Brain Inj. 2002, 16, 169–183. [Google Scholar] [CrossRef] [PubMed]
- Becker, R.; Alberti, O.; Bauer, B.L. Continuous intrathecal baclofen infusion in severe spasticity after traumatic or hypoxic brain injury. J. Neurol. 1997, 244, 160–166. [Google Scholar] [CrossRef] [PubMed]
- Lehmkuhl, L.D.; Thoi, L.L.; Baize, C.; Kelley, C.J.; Krawczyk, L.; Bontke, C.F. Multimodality treatment of joint contractures in patients with severe brain injury: Cost, effectiveness, and integration of therapies in the application of serial/inhibitive casts. J. Head Trauma Rehabil. 1990, 5, 23–42. [Google Scholar] [CrossRef]
- Magrassi, L.; Maggioni, G.; Pistarini, C.; Di Perri, C.; Bastianello, S.; Zippo, A.G.; Iotti, G.A.; Biella, G.E.; Imberti, R. Results of a prospective study (CATS) on the effects of thalamic stimulation in minimally conscious and vegetative state patients. J. Neurosurg. Am. Assoc. Neurol. Surg. 2016, 125, 972–981. [Google Scholar] [CrossRef] [PubMed]
- Krewer, C.; Luther, M.; Koenig, E.; Müller, F. Tilt Table Therapies for Patients with Severe Disorders of Consciousness: A Randomized, Controlled Trial. PLoS ONE 2015, 10, e0143180. [Google Scholar] [CrossRef] [PubMed]
- Margetis, K.; Korfias, S.I.; Gatzonis, S.; Boutos, N.; Stranjalis, G.; Boviatsis, E.; Sakas, D.E. Intrathecal baclofen associated with improvement of consciousness disorders in spasticity patients. Neuromodulation 2014, 17, 699–704. [Google Scholar] [CrossRef] [PubMed]
- Al-Khodairy, A.T.; Wicky, G.; Nicolo, D.; Vuadens, P. Influence of intrathecal baclofen on the level of consciousness and mental functions after extremely severe traumatic brain injury: Brief report. Brain Inj. 2015, 29, 527–532. [Google Scholar] [CrossRef] [PubMed]
- Oyama, H.; Kito, A.; Maki, H.; Hattori, K.; Tanahashi, K. Consciousness Recovery Induced by Intrathecal Baclofen Administration After Subarachnoid Hemorrhage. Neurol. Med. Chir. 2010, 50, 386–390. [Google Scholar] [CrossRef]
- Taira, T. Intrathecal administration of GABA agonists in the vegetative state. Prog. Brain Res. 2009, 177, 317–328. [Google Scholar] [PubMed]
- Sara, M.; Pistoia, F.; Mura, E.; Onorati, P.; Govoni, S. Intrathecal baclofen in patients with persistent vegetative state: 2 hypotheses. Arch. Phys. Med. Rehabil. 2009, 90, 1245–1249. [Google Scholar] [CrossRef] [PubMed]
- Mazaux, J.M.; De Sèze, M.; Joseph, P.A.; Barat, M. Early rehabilitation after severe brain injury: A French perspective. J. Rehabil. Med. 2001, 33, 99–109. [Google Scholar] [PubMed]
- Bobath, B. The very early treatment of cerebral palsy. Dev. Med. Child Neurol. 1967, 9, 373–390. [Google Scholar] [CrossRef] [PubMed]
- Pistoia, F.; Sacco, S.; Sarà, M.; Franceschini, M.; Carolei, A. Intrathecal Baclofen: Effects on Spasticity, Pain, and Consciousness in Disorders of Consciousness and Locked-in Syndrome. Curr. Pain Headache Rep. 2015, 19, 466. [Google Scholar] [CrossRef] [PubMed]
- Thibaut, A.; Chatelle, C.; Ziegler, E.; Bruno, M.-A.; Laureys, S.; Gosseries, O. Spasticity after stroke: Physiology, assessment and treatment. Brain Inj. 2013, 27, 1093–1105. [Google Scholar] [CrossRef] [PubMed]
| Authors | Study Type | n | Intervention | Results |
|---|---|---|---|---|
| Occurrence of Spasticity in DOC Patients | ||||
| Thibaut et al., 2014 [3] | Prospective | 65 | / | 89% showed spasticity (MAS ≥ 1) |
| Nakase-Richardson, 2013 [17] | Prospective | 122 | / | 70% showed spasticity (requiring oral medications, injections or surgical procedure) |
| Ganesh et al., 2013 [18] | Prospective | 68 | / | 57% showed spasticity |
| Treatments targeting spasticity in DOC patients | ||||
| Thibaut et al., 2015 [19] | Randomized controlled trial | 17 | Soft splints applied to the hand for 30 min | Significant decrease (p = 0.014) in the MAS scores (3.5 to 2.5) of the finger flexor muscles |
| Mastumoto-Miyazaki et al., 2016 [20] | Randomized controlled trial | 11 | Japanese style acupuncture on 6 points for 10 min | Significant decrease in F/M ratio (p < 0.001) of the abductor pollicis brevis |
| Shrestha et al., 2011 [21] | Case report | 1 | ITB injections of 50 µg daily for 2 weeks then 100 µg daily for 3 weeks through epidural catheter | Significant decrease of spasticity (subjective report). Patients discharged 2.5 months later, could walk with support |
| Francois et al., 2001 [22] | Case report | 4 | ITB injections of 25 µg/mL continuously through intrathecal catheter and then pump | Decrease in MAS score (4.5 to 3.5 for upper limbs and 4.5 to 2 for lower limbs, on average). |
| Leong, 2002 [23] | Review | / | / | / |
| Leong, 2002 [24] | Systematic review | 17 studies | Passive muscle stretch | Limited evidence |
| Treatments with spasticity as secondary outcome | ||||
| Magrassi et al., 2016 [27] | Clinical trial | 3 | Implantation of bilateral thalamic electrodes | Decrease in spasticity and myoclonus (Unified Myoclonus Rating Scale Section 2 and Section 3: decrease of >25 points) |
| Krewer et al., 2015 [28] | Randomized controlled trial | 50 | Tilt table therapy (with our without integrated stepping device) 10 × 1 h | No significant differences (8.5% of all MAS values showed improvement, 19.7% showed worsening and 71.8% showed no difference) |
| Margetis et al., 2014 [29] | Open-label | 8 | ITB pump | Decrease in MAS scores from 3.4 to 1, on average |
| Al-Khodairy et al., 2015 [30] | Case report | 2 | ITB pump | Decrease in MAS scores (minimum 2 points) |
| Oyama et al., 2010 [31] | Case report | 2 | ITB pump (50 µg/day) | Decrease in MAS scores (minimum 1 point) |
| Taira, 2009 [21] | Case report | 2 | ITB through lumbar puncture | Effective control of the spasticity |
| Sara et al., 2009 [36] | Case report | 5 | ITB pump (100 µg/day) | Decrease in MAS scores (1 point, on average) |
| Mazaux et al., 2001 [34] | Review | / | / | Good agreement exists among clinicians about prevention of orthopedic complications and treatment for spasticity. However, little consensus exists concerning treatment of non-pyramidal hypertonia and spasms. |
| Pistoia et al., 2015 [36] | Review | / | / | Although the current indication of ITB is the management of severe spasticity, its potential use in speeding the recovery of consciousness merits further investigation. |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martens, G.; Laureys, S.; Thibaut, A. Spasticity Management in Disorders of Consciousness. Brain Sci. 2017, 7, 162. https://doi.org/10.3390/brainsci7120162
Martens G, Laureys S, Thibaut A. Spasticity Management in Disorders of Consciousness. Brain Sciences. 2017; 7(12):162. https://doi.org/10.3390/brainsci7120162
Chicago/Turabian StyleMartens, Géraldine, Steven Laureys, and Aurore Thibaut. 2017. "Spasticity Management in Disorders of Consciousness" Brain Sciences 7, no. 12: 162. https://doi.org/10.3390/brainsci7120162
APA StyleMartens, G., Laureys, S., & Thibaut, A. (2017). Spasticity Management in Disorders of Consciousness. Brain Sciences, 7(12), 162. https://doi.org/10.3390/brainsci7120162





