Differential Associations Between Distinct Components of Cognitive and Physical Function in Middle-Aged and Older Adults
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Instruments
2.2.1. Cognitive Functions
2.2.2. Physical Function
2.3. Procedure
2.4. Data Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sprague, B.N.; Phillips, C.B.; Ross, L.A. Age-varying relationships between physical function and cognition in older adulthood. J. Gerontol. Ser. B 2019, 74, 772–784. [Google Scholar] [CrossRef]
- Blumen, H.M.; Buchman, A.S. Adapting the reserve and resilience framework for motor and other aging phenotypes. Neurobiol. Aging 2023, 131, 224–225. [Google Scholar] [CrossRef]
- Holtzer, R.; Verghese, J.; Xue, X.; Lipton, R.B. Cognitive processes related to gait velocity: Results from the Einstein Aging Study. Neuropsychology 2006, 20, 215. [Google Scholar] [CrossRef] [PubMed]
- Sunderaraman, P.; Maidan, I.; Kozlovski, T.; Apa, Z.; Mirelman, A.; Hausdorff, J.M.; Stern, Y. Differential associations between distinct components of cognitive function and mobility: Implications for understanding aging, turning and dual-task walking. Front. Aging Neurosci. 2019, 11, 166. [Google Scholar] [CrossRef]
- Baltes, P.B.; Lindenberger, U. Emergence of a powerful connection between sensory and cognitive functions across the adult life span: A new window to the study of cognitive aging? Psychol. Aging 1997, 12, 12. [Google Scholar] [CrossRef]
- Blumen, H.M.; Holtzer, R.; Brown, L.L.; Gazes, Y.; Verghese, J. Behavioral and neural correlates of imagined walking and walking-while-talking in the elderly. Hum. Brain Mapp. 2014, 35, 4090–4104. [Google Scholar] [CrossRef]
- Tripathi, S.; Verghese, J.; Blumen, H.M. Gray matter volume covariance networks associated with dual-task cost during walking-while-talking. Hum. Brain Mapp. 2019, 40, 2229–2240. [Google Scholar] [CrossRef]
- Montero-Odasso, M.; Verghese, J.; Beauchet, O.; Hausdorff, J.M. Gait and cognition: A complementary approach to understanding brain function and the risk of falling. J. Am. Geriatr. Soc. 2012, 60, 2127–2136. [Google Scholar] [CrossRef]
- Buracchio, T.; Dodge, H.H.; Howieson, D.; Wasserman, D.; Kaye, J. The trajectory of gait speed preceding mild cognitive impairment. Arch. Neurol. 2010, 67, 980–986. [Google Scholar] [CrossRef] [PubMed]
- Morris, R.; Lord, S.; Bunce, J.; Burn, D.; Rochester, L. Gait and cognition: Mapping the global and discrete relationships in ageing and neurodegenerative disease. Neurosci. Biobehav. Rev. 2016, 64, 326–345. [Google Scholar] [CrossRef] [PubMed]
- Verghese, J.; Robbins, M.; Holtzer, R.; Zimmerman, M.; Wang, C.; Xue, X.; Lipton, R.B. Gait dysfunction in mild cognitive impairment syndromes. J. Am. Geriatr. Soc. 2008, 56, 1244–1251. [Google Scholar] [CrossRef]
- Skillbäck, T.; Blennow, K.; Zetterberg, H.; Skoog, J.; Rydén, L.; Wetterberg, H.; Guo, X.; Sacuiu, S.; Mielke, M.M.; Zettergren, A.; et al. Slowing gait speed precedes cognitive decline by several years. Alzheimer’s Dement. 2022, 18, 1667–1676. [Google Scholar] [CrossRef]
- Ayan, C.; Cancela, J.M.; Gutiérrez, A.; Prieto, I. Influence of the cognitive impairment level on the performance of the Timed “Up & Go” Test (TUG) in elderly institutionalized people. Arch. Gerontol. Geriatr. 2013, 56, 44–49. [Google Scholar] [CrossRef] [PubMed]
- de Oliveira Silva, F.; Ferreira, J.V.; Placido, J.; Chagas, D.; Praxedes, J.; Guimaraes, C.; Batista, L.A.; Marinho, V.; Laks, J.; Deslandes, A.C. Stages of mild cognitive impairment and Alzheimer’s disease can be differentiated by declines in timed up and go test: A systematic review and meta-analysis. Arch. Gerontol. Geriatr. 2019, 85, 103941. [Google Scholar] [CrossRef]
- Ibrahim, A.; Singh, D.K.A.; Shahar, S. ‘Timed Up and Go’test: Age, gender and cognitive impairment stratified normative values of older adults. PLoS ONE 2017, 12, e0185641. [Google Scholar] [CrossRef] [PubMed]
- Párraga-Montilla, J.A.; Pozuelo-Carrascosa, D.P.; Carmona-Torres, J.M.; Laredo-Aguilera, J.A.; Cobo-Cuenca, A.I.; Latorre-Román, P.Á. Gait performance as an indicator of cognitive deficit in older people. Int. J. Environ. Res. Public Health 2021, 18, 3428. [Google Scholar] [CrossRef]
- Clouston, S.A.; Brewster, P.; Kuh, D.; Richards, M.; Cooper, R.; Hardy, R.; Rubin, M.S.; Hofer, S.M. The dynamic relationship between physical function and cognition in longitudinal aging cohorts. Epidemiol. Rev. 2013, 35, 33–50. [Google Scholar] [CrossRef]
- Verghese, J.; Wang, C.; Lipton, R.B.; Holtzer, R.; Xue, X. Quantitative gait dysfunction and risk of cognitive decline and dementia. J. Neurol. Neurosurg. Psychiatry 2007, 78, 929–935. [Google Scholar] [CrossRef]
- Benedet, M.J.; Alejandre, M.A. Test de Aprendizaje Verbal España-Complutense; [TAVEC: Spain-Complutense Verbal Learning Test]; TEA Ediciones: Madrid, Spain, 1998. [Google Scholar]
- Kaplan, E.F.; Goodglas, H.; Waintraub, S. The Boston Naming Test, 2nd ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 1983. [Google Scholar]
- Williams, B.W.; Mack, W.; Henderson, V.W. Boston naming test in Alzheimer’s disease. Neuropsychologia 1989, 27, 1073–1079. [Google Scholar] [CrossRef] [PubMed]
- Reitan, R.M.; Wolfson, D. The Halstead–Reitan neuropsychological test battery. In Theory and Clinical Interpretation, 2nd ed.; Neuropsychology Press: Tucson, AZ, USA, 1993; pp. 9–20. [Google Scholar]
- Facal, D.; Juncos-Rabadán, O.; Pereiro, A.X.; Lojo-Seoane, C. Working memory span in mild cognitive impairment. Influence of processing speed and cognitive reserve. Int. Psychogeriatr. 2014, 26, 615–625. [Google Scholar] [CrossRef]
- Carral, J.M.C.; Ayán, C.; Sturzinger, L.; Gonzalez, G. Relationships between body mass index and static and dynamic balance in active and inactive older adults. J. Geriatr. Phys. Ther. 2019, 42, E85–E90. [Google Scholar] [CrossRef] [PubMed]
- da Silva, L.P.G.; de Araújo, M.D.G.R.; dos Santos Costa, A.; de Sousa Pedrosa, B.C.; da SIlva, K.K.D.; dos Santos, T.M. Inertial sensor and Timed Up and Go test in elderly women with bone demineralization: A reliability and agreement study. Rev. Bras. Atividade Fís. Saúde 2020, 25, 1–7. [Google Scholar] [CrossRef]
- Posada-Ordax, J.; Cosin-Matamoros, J.; Losa-Iglesias, M.E.; Becerro-de-Bengoa-Vallejo, R.; Esteban-Gonzalo, L.; Martin-Villa, C.; Calvo-Lobo, C.; Rodriguez-Sanz, D. Accuracy and repeatability of spatiotemporal gait parameters measured with an inertial measurement unit. J. Clin. Med. 2021, 10, 1804. [Google Scholar] [CrossRef]
- Weiss, A.; Mirelman, A.; Giladi, N.; Barnes, L.; Bennett, D.; Buchman, A.; Hausdorff, J.M. Transition between TUG turn to sit subtasks: Is timing everything? J. Am. Med. Dir. Assoc. 2016, 17, 864.e9–864.e15. [Google Scholar] [CrossRef]
- Alley, D.E.; Shardell, M.D.; Peters, K.W.; McLean, R.R.; Dam, T.T.L.; Kenny, A.M.; Fragala, M.S.; Harris, T.B.; Kiel, D.P.; Guralnik, J.M.; et al. Grip strength cutpoints for the identification of clinically relevant weakness. J. Gerontol. Ser. A Biomed. Sci. Med. Sci. 2014, 69, 559–566. [Google Scholar] [CrossRef]
- Ruiz Comellas, A.; Pera, G.; Baena Díez, J.M.; Mundet Tudurí, X.; Alzamora Sas, T.; Elosua, R.; Torán Monserrat, P.; Heras, A.; Forés Raurell, R.; Fusté Gamisans, M.; et al. Validación de una versión reducida en español del cuestionario de actividad física en el tiempo libre de Minnesota (VREM) [Validation of a Spanish Short Version of the Minnesota Leisure Time Physical Activity Questionnaire (VREM)]. Rev. Esp. Salud Pública 2012, 86, 495–508. [Google Scholar]
- Asperholm, M.; Högman, N.; Rafi, J.; Herlitz, A. What did you do yesterday? A meta-analysis of sex differences in episodic memory. Psychol. Bull. 2019, 145, 785–821. [Google Scholar] [CrossRef]
- Nonnekes, J.; Post, E.; Imbalzano, G.; Bloem, B.R. Gait changes with aging: An early warning sign for underlying pathology. J. Neurol. 2025, 272, 257. [Google Scholar] [CrossRef]
- Wu, T.; Hallett, M. The influence of normal human ageing on automatic movements. J. Physiol. 2005, 562, 605–615. [Google Scholar] [CrossRef] [PubMed]
- Giovannoli, J.; Martella, D.; Casagrande, M. Executive functioning during verbal fluency tasks in bilinguals: A systematic review. Int. J. Lang. Commun. Disord. 2023, 58, 1316–1334. [Google Scholar] [CrossRef]
- Whiteside, D.M.; Kealey, T.; Semla, M.; Luu, H.; Rice, L.; Basso, M.R.; Roper, B. Verbal fluency: Language or executive function measure? Appl. Neuropsychol. Adult 2016, 23, 29–34. [Google Scholar] [CrossRef] [PubMed]
- Brandt, T.; Schautzer, F.; Hamilton, D.A.; Brüning, R.; Markowitsch, H.J.; Kalla, R.; Darlington, C.; Smith, P.; Strupp, M. Vestibular loss causes hippocampal atrophy and impaired spatial memory in humans. Brain 2005, 128, 2732–2741. [Google Scholar] [CrossRef]
- Maguire, E.A.; Burke, T.; Phillips, J.; Staunton, H. Topographical disorientation following unilateral temporal lobe lesions in humans. Neuropsychologia 1996, 34, 993–1001. [Google Scholar] [CrossRef]
- Maguire, E.A.; Gadian, D.G.; Johnsrude, I.S.; Good, C.D.; Ashburner, J.; Frackowiak, R.S.; Frith, C.D. Navigation-related structural change in the hippocampi of taxi drivers. Proc. Natl. Acad. Sci. USA 2000, 97, 4398–4403. [Google Scholar] [CrossRef]
- Griesbauer, E.M.; Manley, E.; Wiener, J.M.; Spiers, H.J. London taxi drivers: A review of neurocognitive studies and an exploration of how they build their cognitive map of London. Hippocampus 2022, 32, 3–20. [Google Scholar] [CrossRef]
- Sternäng, O.; Reynolds, C.A.; Finkel, D.; Ernsth-Bravell, M.; Pedersen, N.L.; Dahl Aslan, A.K. Grip strength and cognitive abilities: Associations in old age. J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 2016, 71, 841–848. [Google Scholar] [CrossRef]
- Sui, S.X.; Hendy, A.M.; Teo, W.P.; Moran, J.T.; Nuzum, N.D.; Pasco, J.A. A review of the measurement of the neurology of gait in cognitive dysfunction or dementia, focusing on the application of fNIRS during dual-task gait assessment. Brain Sci. 2022, 12, 968. [Google Scholar] [CrossRef] [PubMed]
- Latino, F.; Tafuri, F. Physical activity and cognitive functioning. Medicina 2024, 60, 216. [Google Scholar] [CrossRef] [PubMed]
| Mean | Standard Deviation | Range | |
|---|---|---|---|
| CVLT total immediate recall | 54.15 | 10.37 | 25–76 |
| CVLT short-delay free recall | 11.40 | 3.33 | 2–16 |
| CVLT long-delay free recall | 12.08 | 3.05 | 2–16 |
| Boston Naming Test total score | 54.05 | 5.77 | 33–60 |
| Semantic fluency score | 20.78 | 6.16 | 6–37 |
| Phonological fluency score | 15.59 | 5.20 | 1–32 |
| Trail making test—form A | 45.22 | 20.82 | 15–180 |
| Trail making test—form B | 107.27 | 55.88 | 39–300 |
| Counting span task—total items recalled | 35.43 | 12.07 | 12–62 |
| Timed-Up and Go—total time | 10.89 | 3.22 | 5.56–26.95 |
| Timed-Up and Go—standing up time | 1.70 | 0.82 | 0.66–9.26 |
| Timed-Up and Go—turning time | 1.42 | 0.57 | 0.35–3.50 |
| Timed-Up and Go—sitting back down time | 2.01 | 1.19 | 0.14–6.72 |
| Grip strength (Kg) | 24.95 | 8.35 | 4.20–54.40 |
| Self-reported physical activity (METS-min/14 days) | 12,016.67 | 7031.16 | 880.11–38,453.14 |
| Age Group | |||
|---|---|---|---|
| Middle Aged | Older | Mann–Whitney U | |
| CVLT total immediate recall | 59.33 (8.01) | 49.79 (10.15) | 4258.00 ** |
| CVLT short-delay free recall | 13.21 (2.36) | 9.88 (3.26) | 3658.50 ** |
| CVLT long-delay free recall | 13.55 (2.07) | 10.85 (3.20) | 4370.50 ** |
| Boston Naming Test total score | 56.69 (3.43) | 51.83 (6.38) | 4424.00 ** |
| Semantic fluency score | 24.24 (5.43) | 17.88 (5.19) | 3563.50 ** |
| Phonological fluency score | 17.93 (4.97) | 13.61 (4.54) | 4611.50 ** |
| Trail making test—form A | 36.75 (18.09) | 52.35 (20.33) | 14,007.50 ** |
| Trail making test—form B | 76.48 (29.74) | 133.17 (59.56) | 14,363.50 ** |
| Counting span task—total items recalled | 40.36 (11.42) | 31.29 (11.03) | 4780.00 ** |
| Timed-Up and Go—total time | 10.07 (2.65) | 11.58 (3.49) | 11,189.00 ** |
| Timed-Up and Go—standing up time | 1.54 (0.66) | 1.82 (0.91) | 11,158.00 ** |
| Timed-Up and Go—turning time | 1.38 (0.52) | 1.46 (0.62) | 9215.50 |
| Timed-Up and Go—sitting back down time | 1.80 (1.12) | 2.19 (1.21) | 10,421.00 * |
| Grip strength (Kg) | 25.88 (8.69) | 24.17 (8.01) | 7730.00 |
| Self-reported physical activity (METS-min/14 days) | 11,510.61 (6840.57) | 12,442.45 (7183.49) | 954,750 |
| Sex | |||
|---|---|---|---|
| Female | Male | Mann–Whitney U | |
| CVLT total immediate recall | 55.75 (9.72) | 49.17 (10.80) | 4204.50 ** |
| CVLT short-delay free recall | 11.90 (3.04) | 9.85 (3.70) | 4426.00 ** |
| CVLT long-delay free recall | 12.52 (2.75) | 10.72 (3.54) | 4628.00 ** |
| Boston Naming Test total score | 53.96 (5.85) | 54.34 (5.55) | 6676.00 |
| Semantic fluency score | 20.91 (6.33) | 20.41 (5.67) | 6298.00 |
| Phonological fluency score | 15.82 (5.16) | 14.86 (5.29) | 5995.00 |
| Trail making test—form A | 45.86 (21.24) | 43.25 (19.46) | 6032.00 |
| Trail making test—form B | 106.67 (54.68) | 109.14 (59.86) | 6684.00 |
| Counting span task—total items recalled | 35.73 (11.89) | 34.52 (12.67) | 6250.50 |
| Timed-Up and Go—total time | 10.74 (3.32) | 11.33 (2.86) | 7562.00 |
| Timed-Up and Go—standing up time | 1.70 (0.88) | 1.68 (0.59) | 6928.50 |
| Timed-Up and Go—turning time | 1.41 (0.56) | 1.47 (0.62) | 7026.50 |
| Timed-Up and Go—sitting back down time | 1.98 (1.20) | 2.12 (1.13) | 7231.00 |
| Grip strength (Kg) | 21.63 (5.39) | 35.28 (7.47) | 12,408.50 ** |
| Self-reported physical activity (METS-min/14 days) | 12,351.07 (7022.44) | 10,977.45 (7010.32) | 5768.00 |
| Timed-Up and Go—Total Time | Timed-Up and Go—Stand Up Time | Timed-Up and Go—Turning Time | Timed-Up and Go—Siting Back Down Time | Grip Strength | Self-Reported Physical Activity | |
|---|---|---|---|---|---|---|
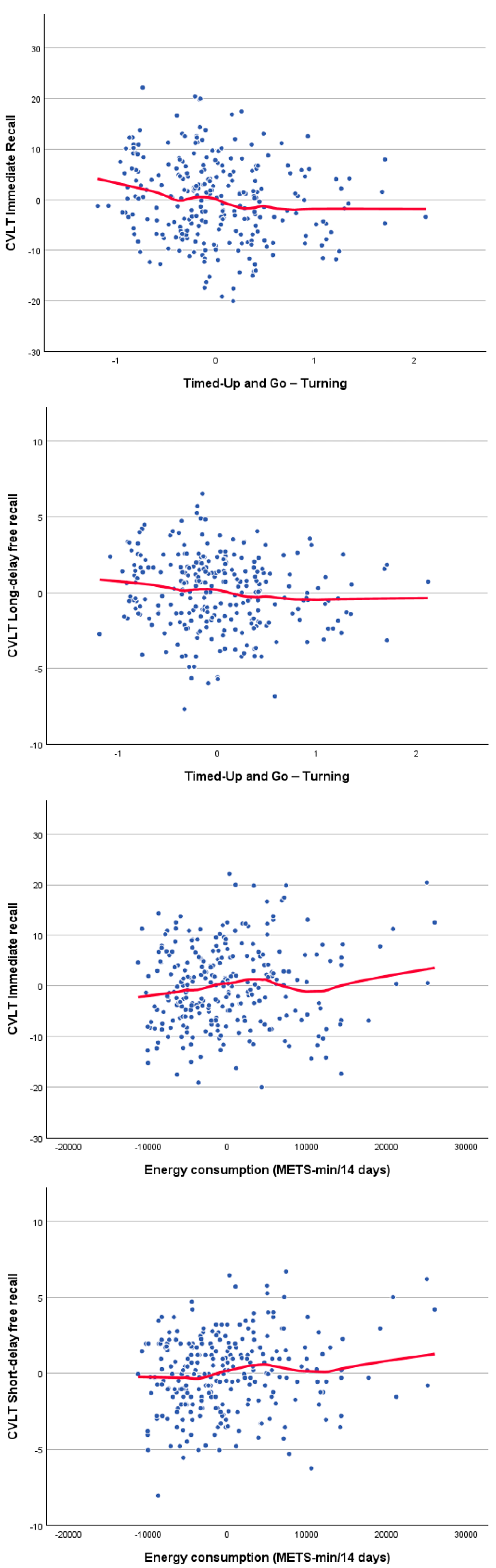
| CVLT total immediate recall | −0.05 | −0.06 | −0.15 * | −0.02 | 0.09 | 0.13 * |
| CVLT short-delay free recall | 0.03 | 0.06 | −0.10 | 0.07 | 0.04 | 0.14 * |
| CVLT long-delay free recall | 0.07 | 0.10 | −0.13 * | 0.09 | 0.07 | 0.12 |
| Boston Naming Test total score | −0.01 | −0.04 | −0.11 | −0.01 | 0.09 | −0.02 |
| Semantic fluency score | −0.01 | −0.03 | −0.07 | −0.01 | −0.03 | 0.03 |
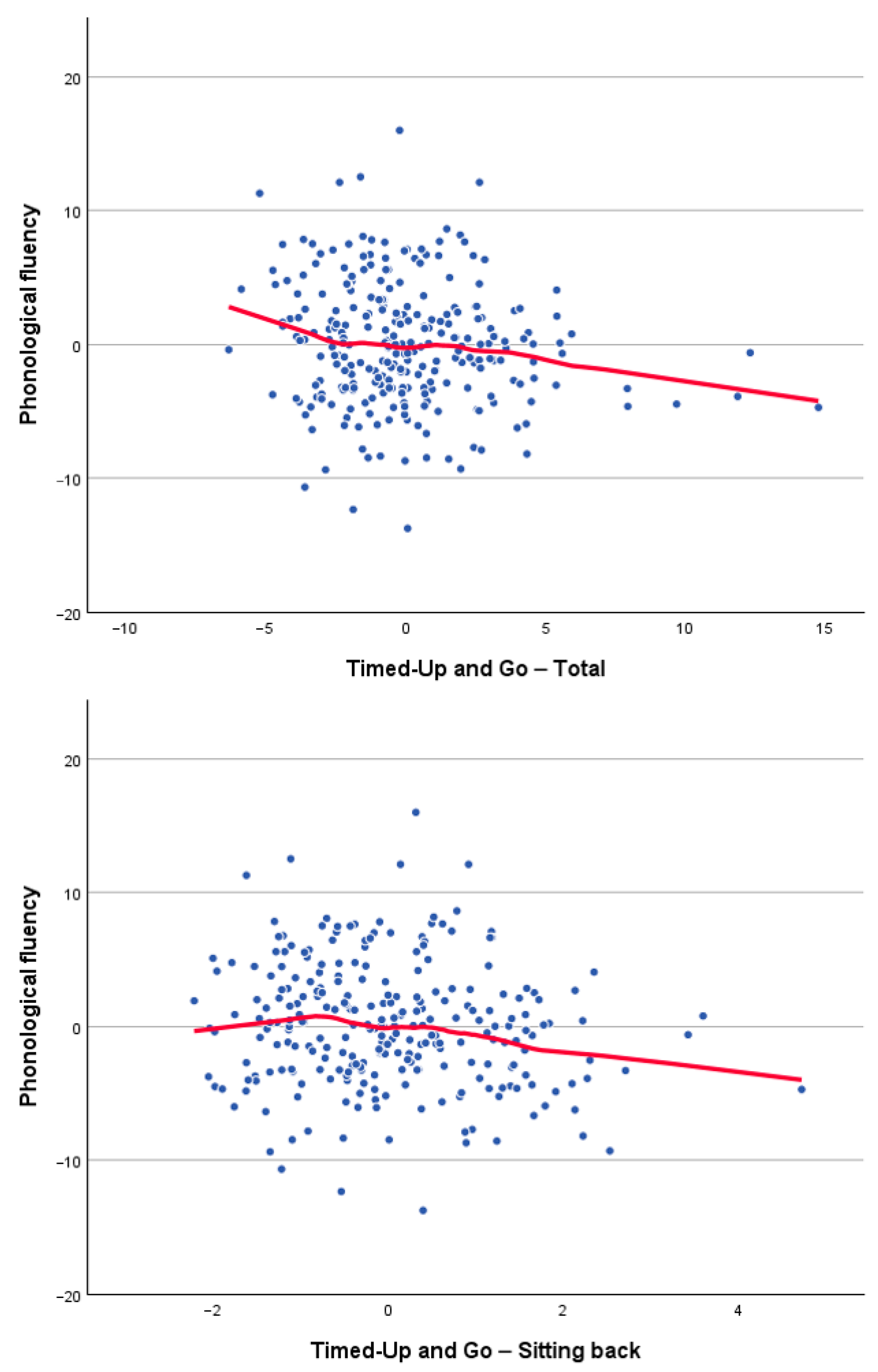
| Phonological fluency score | −0.12 * | −0.12 | −0.03 | −0.12 * | 0.04 | 0.07 |
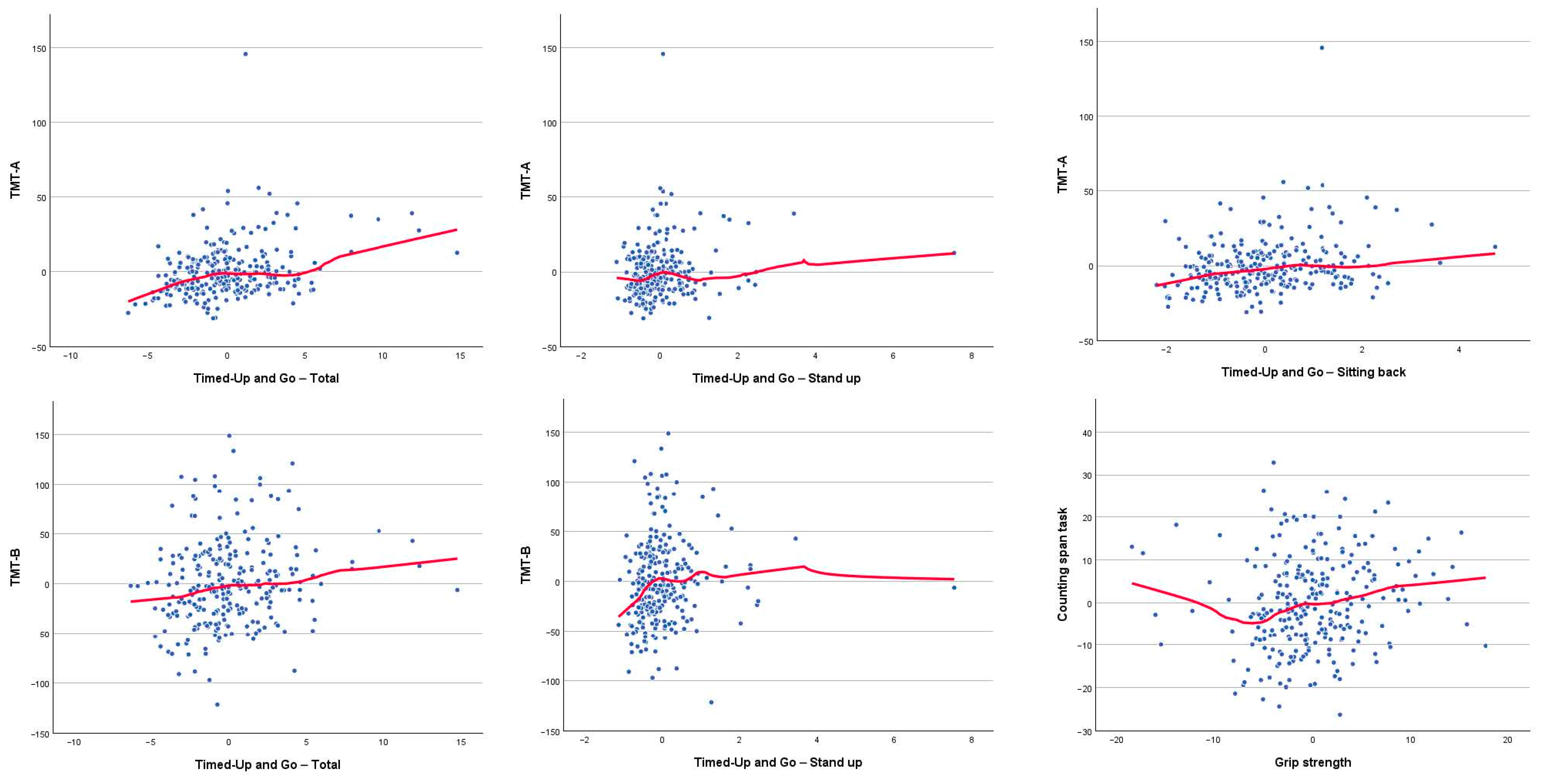
| Trail making test—form A | 0.22 ** | 0.15 * | 0.10 | 0.20 ** | −0.07 | −0.05 |
| Trail making test—form B | 0.12 * | 0.16 ** | 0.10 | 0.09 | −0.10 | −0.05 |
| Counting span task—total items recalled | −0.09 | −0.07 | −0.07 | −0.12 | 0.14 * | 0.04 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.
Share and Cite
Facal, D.; Picón, E.; Blumen, H.M.; Lojo-Seoane, C.; Nieto-Vieites, A.; Stern, Y.; Pereiro, A.X. Differential Associations Between Distinct Components of Cognitive and Physical Function in Middle-Aged and Older Adults. Brain Sci. 2026, 16, 40. https://doi.org/10.3390/brainsci16010040
Facal D, Picón E, Blumen HM, Lojo-Seoane C, Nieto-Vieites A, Stern Y, Pereiro AX. Differential Associations Between Distinct Components of Cognitive and Physical Function in Middle-Aged and Older Adults. Brain Sciences. 2026; 16(1):40. https://doi.org/10.3390/brainsci16010040
Chicago/Turabian StyleFacal, David, Eduardo Picón, Helena M. Blumen, Cristina Lojo-Seoane, Ana Nieto-Vieites, Yaakov Stern, and Arturo X. Pereiro. 2026. "Differential Associations Between Distinct Components of Cognitive and Physical Function in Middle-Aged and Older Adults" Brain Sciences 16, no. 1: 40. https://doi.org/10.3390/brainsci16010040
APA StyleFacal, D., Picón, E., Blumen, H. M., Lojo-Seoane, C., Nieto-Vieites, A., Stern, Y., & Pereiro, A. X. (2026). Differential Associations Between Distinct Components of Cognitive and Physical Function in Middle-Aged and Older Adults. Brain Sciences, 16(1), 40. https://doi.org/10.3390/brainsci16010040






