Communication Abilities, Assessment Procedures, and Intervention Approaches in Rett Syndrome: A Narrative Review
Abstract
1. Introduction
1.1. Diagnostic Criteria for Rett Syndrome
1.2. Rett Syndrome and Communication Characteristics
1.3. Purpose of the Present Review
- Categorize the communication abilities of individuals with RTT participating in research into verbal and nonverbal skills.
- Indicate possible speech and language assessment procedures for identifying the communication abilities of research participants and clinical clients with RTT.
- Identify potential intervention approaches for SLPs and other professionals involved in assessing, planning, and implementing interventions to address communication deficits in individuals with RTT.
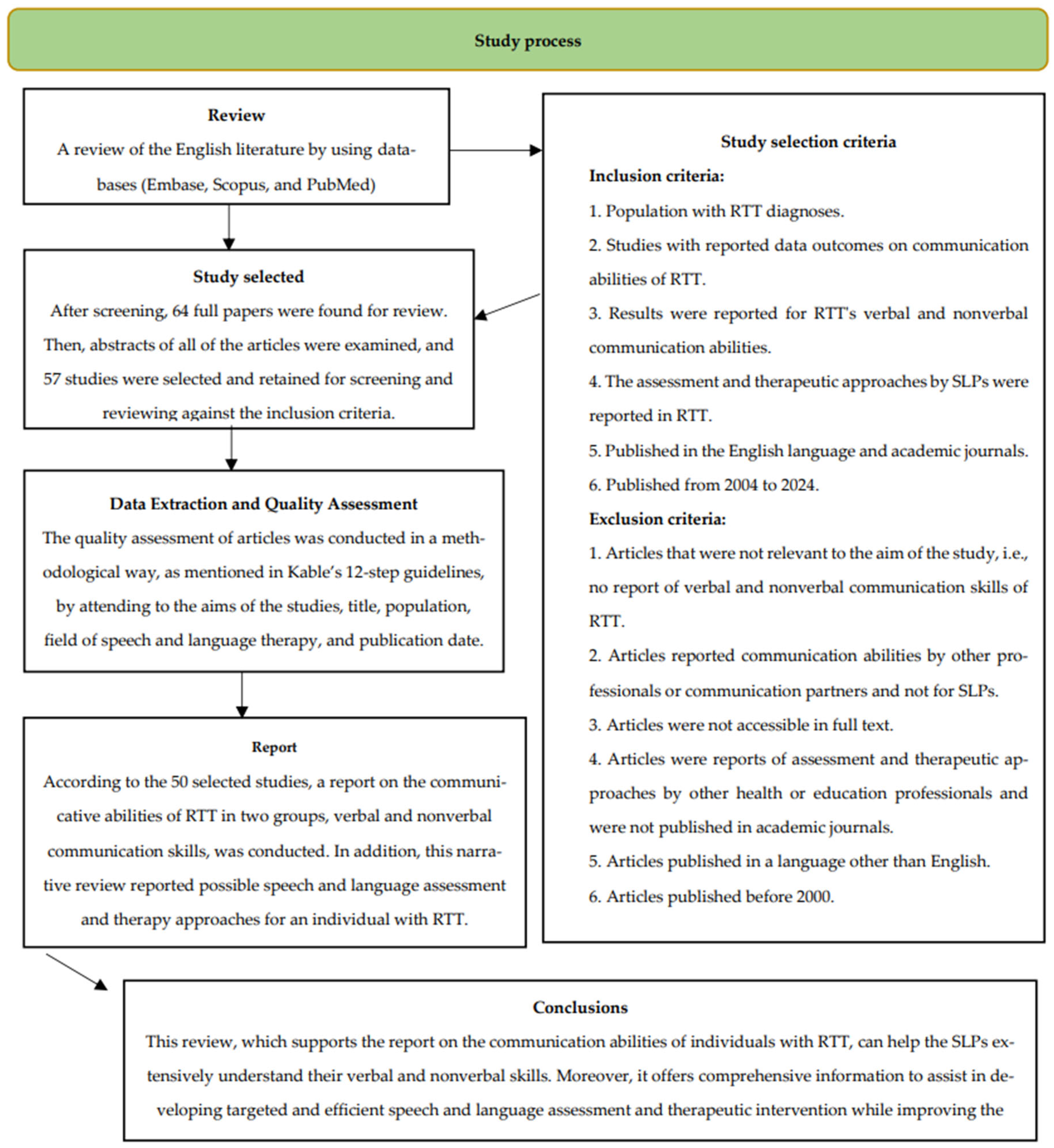
2. Materials and Methods
2.1. Search Strategy
2.2. Study Selection Criteria
- Population with RTT diagnosis;
- All the types of studies with reported data outcomes on the communication abilities of RTT;
- The findings focused exclusively on the verbal and nonverbal communication abilities of individuals with Rett syndrome, without imposing restrictions based on participant characteristics;
- The assessment and intervention approaches implemented by SLPs and other healthcare professionals in individuals with RTT were documented;
- Published in peer-reviewed academic journals available in the English language;
- They were published from 2004 to 2024.
- Articles irrelevant to the study’s aim that did not report the verbal and nonverbal communication skills of individuals with RTT;
- Articles reported communication abilities assessed by other non-SLP professionals or communication partners;
- Articles were inaccessible to the authors in full text;
- Articles reported assessment and intervention approaches by other health or education professionals or were not published in peer-reviewed journals;
- Articles were published in a language other than English;
- Articles published before 2004.
2.3. Data Extraction and Quality Assessment
3. Results
3.1. Sample Characteristics
3.2. Verbal Communication Abilities
3.3. Non Verbal Communication Abilities
3.4. Speech and Language Assessment Procedure
3.5. Speech and Language Intervention Approaches
4. Discussion
4.1. Communication Abilities of Individuals with RTT (Verbal and Nonverbal)
4.2. Speech and Language Assessment Procedures
4.3. Intervention Approaches for SLPs and Other Professionals
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Results | ||||||
|---|---|---|---|---|---|---|
| Authors | Sample [Age] | Purpose of the Study | Study Design | Communication Skills | Assessment of Communication Skills | Intervention of Communication Skills |
| Cianfaglione et al. [45] | 42 individuals with RTT [4 to 47 years, and at follow-up was 7 to 48 years] | Gained a UK national sample of people with RTT across the age range and (1) conduct a cross-sectional comparison of age groups and (2) undertake a longitudinal follow-up. | Research study | Preverbal and pre-intentional level matches their cognitive skill bundle, inhibiting speech intelligibility, body and gestural engagements and expressing unwillingness and displeasure can often happen nonverbally, and receptive abilities are judged alongside mental age | VABS and RSBQ | NA |
| Roche et al. [15] | 23 studies: 13 studies on ASD, 8 studies on RTT, and 2 studies on FXS [0–24 months] | Evaluated early vocal behaviors present in the first two years of life for individuals later diagnosed with ASD, RTT, or FXS. | Systematic analysis on the early development of vocalizations in children later diagnosed with ASD, RTT, or FXS | Inhibited learning ability, decreased mental lexicon development, and verbal communication skills being closely linked to RTTs’ cognitive skills | IPCA | NA |
| Townend et al. [19] | 67 families who have individuals with RTT [3 years 6 months to 60 years 6 months] | A brief report on families’ experiences of eye gaze technology as one form of AAC for individuals with RTT and the advice, training, and support they receive about this. | Research study/online survey relating to communication skills and families’ experiences of communication support | Using eye gaze technology to express their communication abilities | Eye gaze technology | NA |
| Sigafoos et al. [30] | Eight studies that involved 41 individuals with RTT [2.7 years to 36 years] | Reviewed studies that aimed to determine whether behaviors, such as body movements, vocalizations, eye gaze, and facial expressions, served a communicative function for individuals with RTT. | Systematic analysis | Eye pointing/eye gaze, body movements, leading, clapping, reaching, pushing away items, tantrums/screaming | VABS, PPVT-3, Ordinal Scales of Psychological Development, behavioral observations, and interviews | NA |
| Fabio et al. [20] | 20 children (10 individuals with RTT and 10 control girls, matched on mental age) [6 and 21 years] | Analyzed attention and communication abilities in RTT. | Research study | Joint attention, requesting, pointing at the object, and reaching for toys that were out of reach | VABS and behavioral observations | NA |
| Elefant and Wigram [39] | Seven girls with RTT [from 4 to 10 years] | Presented results of a research study examining learning ability in individuals with RTT. | Research study | Choice making and learning ability | NA | Choice-making through eye gaze, nose pointing, or with their hand, according to their preference song and ability |
| Einspieler and Marschik [8] | NA [infants during their first 2 months of life up to 3 years] | This review sheds light on atypical neurofunctions and potential behavioral biomarkers before the onset of the regression of RTT. | Review study | Eye contact, responsive smile, reaction to being called by name, cooing, vocalizations, babbling, index finger pointing, gestures, body movement, proto-words, and two-word combinations | NA | NA |
| Segawa and Nomura [42] | 51 articles with individuals with RTT [NA] | NA | Review study | Avoidance of social interaction | NA | NA |
| Urbanowicz et al. [61] | 16 parents who have individuals with RTT [from 2.3 to 33.7] | Investigated the communicative use of eye gaze and gestures in females with RTT. | Research study | Eye pointing, assigning a point to each feature, the ability to make choices, requesting attention, facial expressions, and social interactions | Interview/several questions about expressive and receptive communication | NA |
| Fabio et al. [22] | A girl with RTT [21 years old] | Investigated the possibility of training communication abilities in people with RTT. | Case study | Cognitive and communicative delays | NA | Training reading–writing abilities |
| Wandin et al. [44] | Nine individuals with RTT [15 to 52 years] | Aimed to (a) develop a tool for assessing visual attention in individuals with RTT using AAC with a communication partner during naturalistic interactions in clinical settings and (b) explored aspects of the tool’s reliability, validity, and utility. | Research study | Limited speech, no intelligible words, and word approximations used inconsistently | AVAI tool | NA |
| Marschik et al. [47] | An individual with RTT [The participant was longitudinally observed from birth to 11 years of age] | Assessed various aspects of speech and language and communicative functions of an individual with the preserved speech variant of RTT to describe her developmental profile over 11 years. | Case study | Hand stereotypies (such as rubbing and washing-like hand movements), as well as hand-to-mouth and hand-to-tongue stereotypies, morphosyntactic and socio-pragmatic limitations, and dysfluency of speech, caused mainly by immediate echolalia | Audio–video recordings of spontaneous speech, picture book reading, storytelling (five stories) and daily routines, parental diaries, and checklists: (i) the Austrian Rett survey; (ii) the Austrian adaptation of the MB-CDIs, a checklist to assess early socio-communicative functions, early gestures, vocabulary, and grammar; (iii) IPCA, AWST-R, TROG-D, SET-K, and the PADLD. | NA |
| Ahonniska-Assa et al. [9] | 17 girls with RTT [3 years and 4 months to 12 years and 2 months] | Investigated whether eye-tracking technology in forced-choice tasks can enable children with very severe motor and speech impairments to respond consistently, allowing a more reliable evaluation of their language comprehension. | Research study | Inconsistent imitation and social skills | Eye-tracking technology and PPVT-4 | NA |
| Castelli et al. [51] | Nine individuals with RTT [5 to 19 years old] | Investigated Theory of Mind capacities with RTT, which is similar to autism yet with more significant impairments. | Research study | Prelinguistic behaviors | Non-verbal false-belief task | NA |
| Sigafoos et al. [29] | Nine studies, 31 participants with RTT [2 years and 7 months to 17 years] | Reviewed communication intervention studies involving people with RTT. | Systematic analysis | Imitative speech, requesting, naming/commenting, and various receptive language skills | NA | Early intensive behavioral intervention |
| Hagberg [50] | NA | Reviewed presentation and clinical diagnosis of RTT at various ages and stages. | Review study | Eye communication or facial expressions as a prominent feature in most individuals with RTT | NA | NA |
| Didden et al. [34] | 120 children and adults (girls) with RTT [5 to 55 years] | Assessed the forms and functions of prelinguistic communicative behaviors for 120 children and adults with RTT using the IPCA. | Research study | Eye gaze, laughing, smiling, vocalization, approaching a person, and distancing from a person | IPCA | NA |
| Marschik et al. [41] | Six individuals with RTT [aged 7 to 24 months] | Contributed new findings related to the pre-regression verbal development of females with a variant of RTT. | Research study | Babbling, (proto-)words and (proto-)word combinations, and nonverbal skills | Spontaneous speech analyses and additional parental report | NA |
| Djukic et al. [53] | 37 Individuals with RTT and 34 typical development girls [2 to 31 years] | Examined the use of eye tracking technology, which is a technique uniquely suited for studying cognition in RTT. | Research study | Using eye gaze to communicate their desires, greet, point, request, and refuse | NA | NA |
| Kaufmann et al. [54] | 80 individuals with RTT [1.6 to 14.9 years] | Examined the social impairments in RTT, the characteristics, and the relationship with clinical severity. | Research study | Pointing at or reaching for an object and requesting | SSI, a measure of autistic behavior suited for individuals with severe communication and motor impairment, RSBQ, VABS, and RSSS | NA |
| Hetzroni et al. [56] | Three individuals with RTT [8 to 10 years] | Investigated whether the use of assistive technology would assist in the ability to identify symbols of individuals with RTT. | Research study | Body movements for making choices, attention, and eye gaze movement | Observations of classroom activities and informal teacher and parent interviews | NA |
| Marschik et al. [21] | 15 young individuals with RTT [first 2 years] | Aimed at shedding light on pre-regression development in RTT by focusing on early speech and language development using a video database. | Research study | Cooing, babbling, (proto-)words, word combinations and vocalization atypicalities | NA | NA |
| Fabio et al. [59] | 28 Participants with RTT [4 to 22 years] | Examined the effects of cognitive rehabilitation with eye-tracker technology on attention, choice behaviors, and language over 2 years in patients with RTT. | Research study | Eye pointing, choice making, gestures, and body movements | NA | Cognitive rehabilitation |
| Skotko et al. [60] | Four individuals with RTT and their mothers [3.6 to 7 years old] | Described evidence and intervention strategies for parents, educators, and researchers who seek to enhance communication and literacy in individuals with RTT. | Research study | Attention and vocalizations | NA | Parent–child storybook interactions |
| Smeets et al. [52] | Two girls with RTT [9 and 11.5 years] | Discussed the clinical aspects with special emphasis on the behavioral phenotype and reviewed current perspectives in clinical management alongside perspectives on altering gene expression. | Review study | Dyspraxia, attention, and eye pointing | NA | NA |
| Barnes et al. [63] | 74 individuals with RTT [2 and 11 years] | Examined the profiles of anxious behavior in individuals with RTT, with a focus on identifying the instrument with the best psychometric properties in this population. | Research study | NA | RSBQ, ADAMS, ABC-C, VABS-II, and CHQ | NA |
| Byiers and Symons [62] | NA [NA] | NA | Commentary study | NA | Eye-tracking technology | NA |
| Cass et al. [58] | 87 individuals with RTT [2 years 1 month to 44 years 10 months] | Presented systematic data from a multidisciplinary clinical assessment of a large series of females with RTT. | Research study | Eye pointing, understanding cause and effect, making choices, and using words with and without meaning | NA | NA |
| Sigafoos et al. [13] | 16 studies that involved 100 participants with RTT [NA] | Identified and summarized 16 communication intervention studies for individuals with RTT. | Systematic–narrative review | NA | NA | AAC device, graphic symbols, or activated microswitches/speech-generating devices to request preferred items, music therapy, eye tracking technology, and transcranial stimulation |
| Lotan and Ben-Zeev [33] | NA [NA] | Presented the basic understanding of common characteristics typical of this disorder and the variants from the classical expression of RTT. | Review study | Express a few words or partial vocabulary | NA | AAC |
| Koppenhaver et al. [75] | 6 individuals with RTT [6 to 7 years old] | Explored the impact of resting hand splints, light-tech augmentative communication systems, such as voice-output devices and symbols, and very basic parent training on the symbolic communication and labelling behaviors of six individuals with RTT. | Research study | NA | NA | Picture communication symbols, single-message Big-Mack, a multi-message four in-line cheap talk, a variety of stands made from PVC pipe |
| Ibrahim et al. [86] | Five children with speech and physical impairments [6 to 9 years] | Examined how children and school staff interact in task-oriented events when speech SGDs are not present or focal. | Research study | NA | NA | AAC |
| Fabio et al. [64] | Three individuals with RTT [aged 29, 30, and 31 years old] | Examined the neurophysiological and cognitive effects of tDCS in three individuals with RTT with chronic language impairments. | Research study | NA | VABS and RARS | tDCS and cognitive empowerment |
| Lamb et al. [70] | 396 caregivers who have individuals with RTT [1.6 to 50 years] | Investigated factors related to family functioning and adaptation in caregivers of individuals with RTT. | Research study | NA | PSOC, WCC-R, FAM-III, and PAS | PMT and CET intervention |
| Byiers et al. [71] | Three individuals with RTT [ages 15 to 47 years] | Examined the effectiveness of functional assessment and functional communication training methods for teaching three children with classic RTT novel communicative behaviors. | Research study | NA | Functional assessment | Functional communication training |
| Stahlhut et al. [74] | 40 participants (parents, care assistants, professionals from schools, and professionals at day centers of RTT) [NA] | Explored facilitators and barriers to “uptime” (non-sedentary) activities in Danish girls and women with RTT as perceived by parents and professionals using focus groups. | Research study | NA | NA | Eye gaze computer |
| Lim et al. [72] | 62 articles with communication skills of children’ RTT [from 9 to 60 years] | Summarized existing interventions and their outcomes in RTT rehabilitation and identified gaps in the literature. | Scoping review | NA | NA | Communication interventions to improve choice-making, communicative language, and social communication abilities |
| Wandin, Lindberg and Sonnander [87] | Three women with RTT [aged 27, 29, and 31 years] | Examined the effect of a communication intervention package on expressive communication and visual attention in individuals with RTT. | Case studies | Visual attention | NA | ALM using responsive partner strategies and a gaze-controlled device |
| Wandin et al., 2015 [73] | 320 SLPs of RTT [NA] | Investigated communication intervention that SLPs provide to people with RTT. | Research study | NA | NA | AAC and communication aids |
| Loffler and Gordon [80] | NA [NA] | NA | Review study | NA | NA | Eye-tracking technology |
| Sandberg et al. [40] | Eight individuals with RTT [11 to 36 years] | Investigated the interrelationships between communication, cognition, and autistic features in young women with one of two variants of RTT complex disorders. | Research study | Loss and reappearance of verbal speech abilities, joint attention, and intentional communication | Video recordings, observations, and VABS | NA |
| Kolb et al. [69] | Three individuals with RTT [1.75 to 29 years old] | Systematically replicated the training procedures to teach three individuals with RTT to use AAC to make requests through caregiver coaching by researchers via telehealth. | Research study | NA | SDA | AAC in the form of manually activated single-message microswitches, eye-gaze device, mind training |
| Neul et al. [88] | 925 caregivers who have individuals with RTT [From less than 1 year to over 40 years] | Determined the top concerns in RTT and RTT-related disorders. | Research study | Communication difficulties and physical inability to coordinate hand movements for communication | CGI-S and the RTT CSS | NA |
| Percy et al. [57] | NA [from 2 to 47 years for clinical studies using the Rett Syndrome Behavior Questionnaire, and the phase 3 LAVENDER study, aged 5 to 20 years] | Reviewed the RSBQ and its utilization in the assessment of symptoms associated with RTT. | Review study | Eye pointing and vocalizations | RSBQ | Eye gaze device, switches, and iPad |
| Vilvarajan et al. [48] | 103 girls with RTT [aged less than 18 years] | Comprehensive review of the clinical features, comorbidities, and multidisciplinary management of a well-characterized cohort of females with classical RTT. | Research study | Single words or short phrases, body language, eye gaze, gestures, and vocalizations | NA | NA |
| Romano, Lotan and Fabio [49] | 195 girls and women with RTT [3 to 40 years] | Evaluated the severity level of girls and women with RTT living in Italy and Israel, two countries with different approaches to caring for people with complex disabilities. | Research study | Spatial and temporal orientation, memory, verbal communication skills, non-verbal communication through facial expressions, ability to maintain eye contact and shared attention, and the presence of responsive smiling | RARS | NA |
| Portnova et al. [65] | 32 Individuals with RTT and 41 typically developing girls [1.9 to 17.1 and 2.58 to 17.98] | Combined clinical, qualitative, and experimental/quantitative approaches to the resting EEG analysis in a search for the EEG characteristics that are linked with RTT symptoms. | Research study | Pleasure and displeasure sounds, and representational gestures | VABS, PDMS-2, and PLS-5 | NA |
| Fabio et al. [55] | 28 young and women with RTT [4 to 22 years] | Examined the effects of motor training on attention, reaching skills, and stereotypies in patients with RTT. | Research study | Attention, reaching skills, and stereotypies | VABS and RARS | Intervention in motor abilities and cognitive intervention |
| Wandin, Lindberg and Sonnander [46] | Three adults with RTT [27, 29 and 31 years old] | Explored and describe a trained communication partner’s use of responsive strategies in dyadic interaction with adults with RTT. | Research study | Eye gaze, body movements, and simple hand movements | RAACS | Gaze-controlled device |
| Unholz-Bowden et al. [66] | Three individuals with RTT [3, 5 and 19 years old] | Investigated the use of high- and low-tech AAC modalities by three individuals with RTT given similar instruction for using both modalities. | Research study | Gestures, requesting, pointing, and eye gaze | NA | High- and low-tech AAC instruments |
| Girtler et al. [89] | Three individuals with RTT [3, 5 and 19 years old] | Evaluated the effects of systematic individualized instruction procedures on the page-linking skills of individuals with RTT. | Research study | Gestures, laughing, crying, and vocalizations | IPCA and SDA | AAC |
| Xavier et al. [90] | 14 girls with RTT and 11 girls with typical development [7–13 years and 3–4 years] | Evaluated the receptive vocabulary of individuals with RTT using eye-tracking technology and examined how these objective measures compared with parents’ perceptions of their daughters’ language abilities. | Research study | NA | Kerr Scale, a parental questionnaire on communication skills, the Peabody Picture Vocabulary Test (PPVT-4), and eye-tracking equipment | NA |
| Passaro et al. [91] | A narrative review NA [NA] | Evaluated studies conducted on the use of ETT to improve cognitive abilities in girls with RTT and to examine its potential application. | Review | NA | Eye tracking technology | NA |
| Neul et al. [67] | 187 females with RTT [5 to 20 years old] | Evaluated the efficacy of trofinetide in communication of individuals with RTT. | Research study | Inability to communicate or make choices | The caregiver-rated CSBS-DP-IT social composite score and RTT-specific clinician rating scales related to discrete aspects of communication (RTT-COMC and RTT-VCOM) | NA |
| Lee et al., 2024 [28] | A case study with a female and a Narrative review with RTT [22 years old] | Evaluated the impact of AAC devices on communication outcomes and quality of life in individuals with RTT through a case report and narrative review. | Research study | NA | AAC | AAC |
| Voniati et al., 2024 [92] | Scoping Review with 7 articles with a total of 381 participants with RTT [NA] | Aimed to provide an overview of the identification of communication abilities in children with RTT in their daily routine from the perspectives of communication partners who interact with individuals diagnosed with RTT. | Scoping review | Eye gaze, expressing pleasure, requesting desired items, making choices, vocalizations, pointing, interaction, and strong receptive skills | Functional Ability Checklist, Functional Independence Measure for Children Communication and Symbolic Behavior Scales Developmental Profile Infant–Toddler Checklist, MacArthur–Bates Communicative Development Inventories and sections of the Vineland Adaptive Behavior Scales, Second Edition, the Assessment of Visual Attention in Interaction tool, the Child Participation in Family Activities questionnaire, the Clinical Severity Score and Hoffer Ambulation Scale | NA |
| Voniati et al., 2023 [43] | Narrative Review: 19 articles with individuals with RTT [NA] | Aimed to support the clinical work of speech–language pathologists (SLPs) while assessing the communication aptitudes of children with RTT. | Review | NA | Medical and developmental intake, functional assessment, Mullen scales, IPCA, PPVT, Vineland Adaptive Behavior Scales, a communication matrix, and AAC assessment | NA |
Appendix B
| SANRA Criterion | Score (0–2) | Justification for Scoring |
|---|---|---|
| 1. Importance for the readership | 2 | The introduction contains all the elements to explain the significance of the communication deficits of individuals with RTT. |
| 2. Stated aims or research questions | 2 | The aims of the study are stated clearly in the abstract and Section 1.2 with main research questions and subobjectives. |
| 3. Description of the literature search | 2 | A transparent, structured search is described. The databases, keywords, Boolean, date range, inclusion/exclusion criteria, and the use of Kable’s 12-step method are noted. |
| 4. Referencing | 2 | Up-to-date, relevant, and peer-reviewed references (n = 91) were used from Databases. |
| 5. Scientific reasoning | 2 | The discussion was developed by making a synthesis of the findings across all studies and discussed supported with citations and any possible evidence. |
| 6. Appropriate presentation of data | 2 | The results were described by domain (verbal, nonverbal, assessment, intervention) and presented by a table in the Appendix A. |
| Total Score | 12 |
References
- Chahil, G.; Bollu, P.C. Rett Syndrome. 2018. Available online: https://europepmc.org/books/NBK482252/figure/article-28490.image.f1/?report=objectonly (accessed on 23 June 2025).[Green Version]
- Amir, R.E.; Van den Veyver, I.B.; Wan, M.; Tran, C.Q.; Francke, U.; Zoghbi, H.Y. Rett syndrome is caused by mutations in X-linked MECP2, encoding methyl-CpG-binding protein 2. Nat. Genet. 1999, 23, 185–188. [Google Scholar] [CrossRef] [PubMed]
- Neul, J.L.; Kaufmann, W.E.; Glaze, D.G.; Christodoulou, J.; Clarke, A.J.; Bahi-Buisson, N.; Leonard, H.; Bailey, M.E.S.; Schanen, N.C.; Zappella, M.; et al. Rett syndrome: Revised diagnostic criteria and nomenclature. Ann. Neurol. 2010, 68, 944–950. [Google Scholar] [CrossRef] [PubMed]
- Poleg, T.; Hadar, N.; Heimer, G.; Dolgin, V.; Aminov, I.; Safran, A.; Agam, N.; Jean, M.M.; Freund, O.; Kaur, S.; et al. Unraveling MECP2 structural variants in previously elusive Rett syndrome cases through IGV interpretation. NPJ Genom. Med. 2025, 10, 23. [Google Scholar] [CrossRef] [PubMed]
- Byun, C.K.; Lee, J.S.; Lim, B.C.; Kim, K.J.; Hwang, Y.S.; Chae, J.H. FOXG1 mutation is a low-incidence genetic cause in atypical Rett syndrome. Child Neurol. Open 2015, 2, 2329048X14568151. [Google Scholar] [CrossRef] [PubMed]
- Weaving, L.S.; Christodoulou, J.; Williamson, S.L.; Friend, K.L.; McKenzie, O.L.D.; Archer, H.; Evans, J.; Clarke, A.; Pelka, G.J.; Tam, P.P.; et al. Mutations of CDKL5 cause a severe neurodevelopmental disorder with infantile spasms and mental retardation. Am. J. Hum. Genet. 2004, 75, 1079–1093. [Google Scholar] [CrossRef] [PubMed]
- Asuncion, R.; Ramani, P. Rett Syndrome; [Updated 27 March 2025]; StatPearls Publishing: Treasure Island, FL, USA, 2025. Available online: https://www.ncbi.nlm.nih.gov/books/NBK482252/ (accessed on 23 June 2025).[Green Version]
- Einspieler, C.; Marschik, P.B. Regression in Rett syndrome: Developmental pathways to its onset. Neurosci. Biobehav. Rev. 2019, 98, 320–332. [Google Scholar] [CrossRef] [PubMed]
- Ahonniska-Assa, J.; Polack, O.; Saraf, E.; Wine, J.; Silberg, T.; Nissenkorn, A.; Ben-Zeev, B. Assessing cognitive functioning in females with Rett syndrome by eye-tracking methodology. Eur. J. Paediatr. Neurol. 2018, 22, 39–45. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Bao, X.; Zhang, J.; Zhao, Y.; Cao, G.; Pan, H.; Zhang, J.; Wei, L.; Wu, X. Molecular characteristics of Chinese patients with Rett syndrome. Eur. J. Med. Genet. 2012, 55, 677–681. [Google Scholar] [CrossRef] [PubMed]
- Tarquinio, D.C.; Hou, W.; Neul, J.L.; Berkmen, G.K.; Drummond, J.; Aronoff, E.; Harris, J.; Lane, J.B.; Kaufmann, W.E.; Motil, K.J.; et al. The course of awake breathing disturbances across the lifespan in Rett syndrome. Brain Dev. 2018, 40, 515–529. [Google Scholar] [CrossRef] [PubMed]
- Sigafoos, J.; O’Reilly, M.F.; Ledbetter-Cho, K.; Lim, N.; Lancioni, G.E.; Marschik, P.B. Addressing sequelae of developmental regression associated with developmental disabilities: A systematic review of behavioral and educational intervention studies. Neurosci. Biobehav. Rev. 2019, 96, 56–71. [Google Scholar] [CrossRef] [PubMed]
- Sigafoos, J.; Roche, L.; O’Reilly, M.F.; Lancioni, G.E.; Marschik, P.B. Updated systematic-narrative review on communication intervention in Rett Syndrome: 2010–2022. Augment. Altern. Commun. 2023, 39, 241–255. [Google Scholar] [CrossRef] [PubMed]
- Hornof, A.; Whitman, H.; Sutherland, M.; Gerendasy, S.; McGrenere, J. Designing for the” Universe of One” Personalized Interactive Media Systems for People with the Severe Cognitive Impairment Associated with Rett Syndrome. In Proceedings of the 2017 CHI Conference on Human Factors in Computing Systems, Denver, CO, USA, 6–11 May 2017; pp. 2137–2148. [Google Scholar][Green Version]
- Roche, L.; Zhang, D.; Bartl-Pokorny, K.D.; Pokorny, F.B.; Schuller, B.W.; Esposito, G.; Bölte, S.; Roeyers, H.; Poustka, L.; Gugatschka, M.; et al. Early vocal development in autism spectrum disorder, Rett syndrome, and fragile X syndrome: Insights from studies using retrospective video analysis. Adv. Neurodev. Disord. 2018, 2, 49–61. [Google Scholar] [CrossRef] [PubMed]
- Jian, L.; Nagarajan, L.; De Klerk, N.; Ravine, D.; Bower, C.; Anderson, A.; Williamson, S.; Christodoulou, J.; Leonard, H. Predictors of seizure onset in Rett syndrome. J. Pediatr. 2006, 149, 542–547. [Google Scholar] [CrossRef] [PubMed]
- Neul, J.L.; Lane, J.B.; Lee, H.S.; Geerts, S.; Barrish, J.O.; Annese, F.; Baggett, L.M.; Barnes, K.; ASkinner, S.; Motil, K.J.; et al. Developmental delay in Rett syndrome: Data from the natural history study. J. Neurodev. Disord. 2014, 6, 20. [Google Scholar] [CrossRef] [PubMed]
- Brunetti, S.; Lumsden, D.E. Rett Syndrome as a movement and motor disorder—A narrative review. Eur. J. Paediatr. Neurol. 2020, 28, 29–37. [Google Scholar] [CrossRef] [PubMed]
- Townend, G.S.; Marschik, P.B.; Smeets, E.; Van de Berg, R.; van den Berg, M.; Curfs, L.M.G. Eye gaze technology as a form of augmentative and alternative communication for individuals with Rett syndrome: Experiences of families in The Netherlands. J. Dev. Phys. Disabil. 2016, 28, 101–112. [Google Scholar] [CrossRef] [PubMed]
- Fabio, R.A.; Giannatiempo, S.; Caprì, T. Attention and identification of the same and the similar visual stimuli in Rett Syndrome. Life Span. Disabil. 2019, 22, 113–127. [Google Scholar]
- Marschik, P.B.; Kaufmann, W.E.; Sigafoos, J.; Wolin, T.; Zhang, D.; Bartl-Pokorny, K.D.; Pini, G.; Zappella, M.; Tager-Flusberg, H.; Einspieler, C.; et al. Changing the perspective on early development of Rett syndrome. Res. Dev. Disabil. 2013, 34, 1236–1239. [Google Scholar] [CrossRef] [PubMed]
- Fabio, R.A.; Castelli, I.; Marchetti, A.; Antonietti, A. Training communication abilities in Rett Syndrome through reading and writing. Front. Psychol. 2013, 4, 66589. [Google Scholar] [CrossRef] [PubMed]
- Bartolotta, T.E.; Zipp, G.P.; Simpkins, S.D.; Glazewski, B. Communication skills in girls with Rett syndrome. Focus Autism Other Dev. Disabl. 2011, 26, 15–24. [Google Scholar] [CrossRef]
- Bartl-Pokorny, K.D.; Marschik, P.B.; Sigafoos, J.; Tager-Flusberg, H.; Kaufmann, W.E.; Grossmann, T.; Einspieler, C. Early socio-communicative forms and functions in typical Rett syndrome. Res. Dev. Disabil. 2013, 34, 3133–3138. [Google Scholar] [CrossRef] [PubMed]
- Cianfaglione, R.; Clarke, A.; Kerr, M.; Hastings, R.P.; Oliver, C.; Moss, J.; Heald, M.; Felce, D. A national survey of Rett syndrome: Behavioural characteristics. J. Neurodev. Disord. 2015, 7, 11. [Google Scholar] [CrossRef] [PubMed]
- Rozensztrauch, A.; Sebzda, A.; Śmigiel, R. Clinical presentation of Rett syndrome in relation to quality of life and family functioning. J. Int. Med. Res. 2021, 49, 03000605211007714. [Google Scholar] [CrossRef] [PubMed]
- Townend, G.S.; Bartolotta, T.E.; Urbanowicz, A.; Wandin, H.; Curfs, L.M.G. Development of consensus-based guidelines for managing communication of individuals with Rett syndrome. Augment. Altern. Commun. 2020, 36, 71–81. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Lee, J.; Abu-Daoud, M.; Al-Ajlouni, Y.A. Assistive Communication Devices in Rett Syndrome: A Case Report and Narrative Review. BioMed 2024, 4, 146–155. [Google Scholar] [CrossRef]
- Sigafoos, J.; Green, V.A.; Schlosser, R.; O’eilly, M.F.; Lancioni, G.E.; Rispoli, M.; Lang, R. Communication intervention in Rett syndrome: A systematic review. Res. Autism Spectr. Disord. 2009, 3, 304–318. [Google Scholar] [CrossRef]
- Sigafoos, J.; Kagohara, D.; van der Meer, L.; Green, V.A.; O’Reilly, M.F.; Lancioni, G.E.; Lang, R.; Rispoli, M.; Zisimopoulos, D. Communication assessment for individuals with Rett syndrome: A systematic review. Res. Autism Spectr. Disord. 2011, 5, 692–700. [Google Scholar] [CrossRef]
- Einspieler, C.; Kerr, A.M.; Prechtl, H.F.R. Is the early development of girls with Rett disorder really normal? Pediatr. Res. 2005, 57, 696–700. [Google Scholar] [CrossRef] [PubMed]
- Lotan, M. Rett syndrome. Guidelines for individual intervention. Sci. World J. 2006, 6, 1504–1516. [Google Scholar] [CrossRef] [PubMed]
- Lotan, M.; Ben-Zeev, B. Rett syndrome. A review with emphasis on clinical characteristics and intervention. Sci. World J. 2006, 6, 1517–1541. [Google Scholar] [CrossRef] [PubMed]
- Didden, R.; Korzilius, H.; Smeets, E.; Green, V.A.; Lang, R.; Lancioni, G.E.; Curfs, L.M. Communication in individuals with Rett syndrome: An assessment of forms and functions. J. Dev. Phys. Disabil. 2010, 22, 105–118. [Google Scholar] [CrossRef] [PubMed]
- Sukhera, J. Narrative reviews: Flexible, rigorous, and practical. J. Grad. Med. Educ. 2022, 14, 414–417. [Google Scholar] [CrossRef] [PubMed]
- Kable, A.K.; Pich, J.; Maslin-Prothero, S.E. A structured approach to documenting a search strategy for publication: A 12 step guideline for authors. Nurse Educ. Today 2012, 32, 878–886. [Google Scholar] [CrossRef] [PubMed]
- Baethge, C.; Goldbeck-Wood, S.; Mertens, S. SANRA—A scale for the quality assessment of narrative review articles. Res. Integr. Peer Rev. 2019, 4, 5. [Google Scholar] [CrossRef] [PubMed]
- Baethge, C.; Mertens, S.; Goldbeck-Wood, S. Development of a quality score for the assessment of non-systematic review articles (SANRA). In Proceedings of the Poster, Seventh International Congress on Peer Review and Biomedical Publication, Chicago, IL, USA, 8–10 September 2013. [Google Scholar]
- Elefant, C.; Wigram, T. Learning ability in children with Rett syndrome. Brain Dev. 2005, 27, S97–S101. [Google Scholar] [CrossRef] [PubMed]
- Sandberg, A.D.; Ehlers, S.; Hagberg, B.; Gillberg, C. The Rett syndrome complex: Communicative functions in relation to developmental level and autistic features. Autism 2000, 4, 249–267. [Google Scholar] [CrossRef]
- Marschik, P.B.; Pini, G.; Bartl-Pokorny, K.D.; Duckworth, M.; Gugatschka, M.; Vollmann, R.; Zappella, M.; Einspieler, C. Early speech–language development in females with Rett syndrome: Focusing on the preserved speech variant. Dev. Med. Child. Neurol. 2012, 54, 451–456. [Google Scholar] [CrossRef] [PubMed]
- Segawa, M.; Nomura, Y. Rett syndrome. Curr. Opin. Neurol. 2005, 18, 97–104. [Google Scholar] [CrossRef] [PubMed]
- Voniati, L.; Papaleontiou, A.; Georgiou, R.; Tafiadis, D. Identifying key aspects of the communicative capabilities of children with Rett syndrome. Neurosci. Res. Notes 2023, 6, 175. [Google Scholar] [CrossRef]
- Wandin, H.; Lindberg, P.; Sonnander, K. Development of a tool to assess visual attention in Rett syn-drome: A pilot study. Augment. Altern. Commun. 2020, 36, 118–127. [Google Scholar] [CrossRef] [PubMed]
- Cianfaglione, R.; Clarke, A.; Kerr, M.; Hastings, R.P.; Oliver, C.; Felce, D. Ageing in Rett syndrome. J. Intellect. Disabil. Res. 2016, 60, 182–190. [Google Scholar] [CrossRef] [PubMed]
- Wandin, H.; Lindberg, P.; Sonnander, K. A trained communication partner’s use of responsive strategies in aided communication with three adults with Rett syndrome: A case report. Front. Psychol. 2022, 13, 989319. [Google Scholar] [CrossRef] [PubMed]
- Marschik, P.B.; Vollmann, R.; Bartl-Pokorny, K.D.; Green, V.A.; van der Meer, L.; Wolin, T.; Einspieler, C. Develop-mental profile of speech-language and communicative functions in an individual with the Preserved Speech Variant of Rett syndrome. Dev. Neurorehabil 2014, 17, 284–290. [Google Scholar] [CrossRef] [PubMed]
- Vilvarajan, S.; McDonald, M.; Douglas, L.; Newham, J.; Kirkland, R.; Tzannes, G.; Tay, D.; Christodoulou, J.; Thompson, S.; Ellaway, C. Multidisciplinary Management of Rett Syndrome: Twenty Years’ Experience. Genes 2023, 14, 1607. [Google Scholar] [CrossRef] [PubMed]
- Romano, A.; Lotan, M.; Fabio, R.A. A Severity Comparison between Italian and Israeli Rett Syndrome Cohorts. Diagnostics 2023, 13, 3390. [Google Scholar] [CrossRef] [PubMed]
- Hagberg, B. Clinical manifestations and stages of Rett syndrome. Ment. Retard. Dev. Disabil. Res. Rev. 2002, 8, 61–65. [Google Scholar] [CrossRef] [PubMed]
- Castelli, I.; Antonietti, A.; Fabio, R.A.; Lucchini, B.; Marchetti, A. Do rett syndrome persons possess theory of mind? Some evidence from not-treated girls. Life Span. Disabil. 2013, 16, 157–168. [Google Scholar]
- Smeets, E.E.J.; Pelc, K.; Dan, B. Rett syndrome. Mol. Syndromol. 2012, 2, 113–127. [Google Scholar] [CrossRef] [PubMed]
- Djukic, A.; Rose, S.A.; Jankowski, J.J.; Feldman, J.F. Rett syndrome: Recognition of facial expression and its relation to scanning patterns. Pediatr. Neurol. 2014, 51, 650–656. [Google Scholar] [CrossRef] [PubMed]
- Kaufmann, W.E.; Tierney, E.; Rohde, C.A.; Suarez-Pedraza, M.C.; Clarke, M.A.; Salorio, C.F.; Bibat, G.; Bukelis, I.; Naram, D.; Lanham, D.C.; et al. Social impairments in Rett syndrome: Characteristics and relationship with clinical severity. J. Intellect. Disabil. Res. 2012, 56, 233–247. [Google Scholar] [CrossRef] [PubMed]
- Fabio, R.A.; Giannatiempo, S.; Caprì, T.; Semino, M. Repeated Motor Training on Attention Reaching Skills and Stereotypies in Rett Syndrome. Mov. Disord. Clin. Pract. 2022, 9, 637–646. [Google Scholar] [CrossRef] [PubMed]
- Hetzroni, O.; Rubin, C.; Konkol, O. The use of assistive technology for symbol identification by children with Rett syndrome. J. Intellect. Dev. Disabil. 2002, 27, 57–71. [Google Scholar] [CrossRef]
- Percy, A.K.; Neul, J.L.; Benke, T.A.; Marsh, E.D.; Glaze, D.G. A review of the Rett Syndrome Behaviour Questionnaire and its utilization in the assessment of symptoms associated with Rett syndrome. Front. Pediatr. 2023, 11, 1229553. [Google Scholar] [CrossRef] [PubMed]
- Cass, H.; Reilly, S.; Owen, L.; Wisbeach, A.; Weekes, L.; Slonims, V.; Wigram, T.; Charman, T. Findings from a multidisciplinary clinical case series of females with Rett syndrome. Dev. Med. Child. Neurol. 2003, 45, 325–337. [Google Scholar] [CrossRef] [PubMed]
- Fabio, R.A.; Giannatiempo, S.; Semino, M.; Caprì, T. Longitudinal cognitive rehabilitation applied with eye-tracker for patients with Rett Syndrome. Res. Dev. Disabil. 2021, 111, 103891. [Google Scholar] [CrossRef] [PubMed]
- Skotko, B.G.; Koppenhaver, D.A.; Erickson, K.A. Parent reading behaviors and communication outcomes in girls with Rett syndrome. Except. Child. 2004, 70, 145–166. [Google Scholar] [CrossRef]
- Urbanowicz, A.; Downs, J.; Girdler, S.; Ciccone, N.; Leonard, H. An exploration of the use of eye gaze and gestures in females with Rett syndrome. J. Speech Lang. Hear. Res. 2016, 59, 1373–1383. [Google Scholar] [CrossRef] [PubMed]
- Byiers, B.; Symons, F. The need for unbiased cognitive assessment in Rett syndrome: Is eye tracking the answer? Dev. Med. Child. Neurol. 2013, 55, 301. [Google Scholar] [CrossRef] [PubMed]
- Barnes, K.V.; Coughlin, F.R.; O’Leary, H.M.; Bruck, N.; Bazin, G.A.; Beinecke, E.B.; Walco, A.C.; Cantwell, N.G.; Kaufmann, W.E. Anxiety-like behavior in Rett syndrome: Characteristics and assessment by anxiety scales. J. Neurodev. Disord. 2015, 7, 30. [Google Scholar] [CrossRef] [PubMed]
- Fabio, R.A.; Gangemi, A.; Capri, T.; Budden, S.; Falzone, A. Neurophysiological and cognitive effects of Transcranial Direct Current Stimulation in three girls with Rett Syndrome with chronic language impairments. Res. Dev. Disabil. 2018, 76, 76–87. [Google Scholar] [CrossRef] [PubMed]
- Portnova, G.; Neklyudova, A.; Voinova, V.; Sysoeva, O. Clinical EEG of Rett syndrome: Group analysis supplemented with longitudinal case report. J. Pers. Med. 2022, 12, 1973. [Google Scholar] [CrossRef] [PubMed]
- Unholz-Bowden, E.K.; Girtler, S.N.; Shipchandler, A.; Kolb, R.L.; McComas, J.J. Use of augmentative and alternative communication by individuals with rett syndrome part 2: High-tech and low-tech modalities. J. Dev. Phys. Disabil. 2024, 36, 147–167. [Google Scholar] [CrossRef] [PubMed]
- Neul, J.L.; Percy, A.K.; Benke, T.A.; Berry-Kravis, E.M.; Glaze, D.G.; Peters, S.U.; Marsh, E.D.; An, D.; Bishop, K.M.; Youakim, J.M. Trofinetide treatment demonstrates a benefit over placebo for the ability to communicate in Rett syndrome. Pediatr. Neurol. 2024, 152, 63–72. [Google Scholar] [CrossRef] [PubMed]
- Urbanowicz, A.; Ciccone, N.; Girdler, S.; Leonard, H.; Downs, J. Choice making in Rett syndrome: A descriptive study using video data. Disabil. Rehabil. 2018, 40, 813–819. [Google Scholar] [CrossRef] [PubMed]
- Kolb, R.L.; McComas, J.J.; Girtler, S.N.; Simacek, J.; Dimian, A.F.; Unholz-Bowden, E.K.; Shipchandler, A.K. Teaching requesting to individuals with Rett syndrome using alternative augmentative communication (AAC) through caregiver coaching via telehealth. J. Dev. Phys. Disabil. 2023, 35, 1063–1090. [Google Scholar] [CrossRef] [PubMed]
- Lamb, A.E.; Biesecker, B.B.; Umstead, K.L.; Muratori, M.; Biesecker, L.G.; Erby, L.H. Family functioning mediates adaptation in caregivers of individuals with Rett syndrome. Patient Educ. Couns. 2016, 99, 1873–1879. [Google Scholar] [CrossRef] [PubMed]
- Byiers, B.J.; Dimian, A.; Symons, F.J. Functional communication training in Rett syndrome: A preliminary study. Am. J. Intellect. Dev. Disabil. 2014, 119, 340–350. [Google Scholar] [CrossRef] [PubMed]
- Lim, J.; Greenspoon, D.; Hunt, A.; McAdam, L. Rehabilitation interventions in Rett syndrome: A scoping review. Dev. Med. Child. Neurol. 2020, 62, 906–916. [Google Scholar] [CrossRef] [PubMed]
- Wandin, H.; Lindberg, P.; Sonnander, K. Communication intervention in Rett syndrome: A survey of speech language pathologists in Swedish health services. Disabil. Rehabil. 2015, 37, 1324–1333. [Google Scholar] [CrossRef] [PubMed]
- Stahlhut, M.; Esbensen, B.A.; Larsen, J.L.; Bisgaard, A.M.; Downs, J.; Nordmark, E. Facilitators and Barriers of Participation in “Uptime” Activities in Girls and Women with Rett Syndrome: Perspectives from Parents and Professionals. Qual. Health Res. 2019, 29, 609–619. [Google Scholar] [CrossRef] [PubMed]
- Koppenhaver, D.; Erickson, K.; Harris, B.; McLellan, J.; Skotko, B.; Newton, R. Storybook-based communication intervention for girls with Rett syndrome and their mothers. Disabil. Rehabil. 2001, 23, 149–159. [Google Scholar] [PubMed]
- Sigafoos, J.; Woodyatt, G.; Keen, D.; Tait, K.; Tucker, M.; Roberts-Pennell, D.; Pittendreigh, N. Identifying potential communicative acts in children with developmental and physical disabilities. Commun. Disord. Q. 2000, 21, 77–86. [Google Scholar] [CrossRef]
- Sigafoos, J.; O’Reilly, M.F.; Lancioni, G.E.; Zhang, D.; Marschik, P.B. The Inventory of Potential Communicative Acts (IPCA): Narrative review of reliability, validity, and clinical utility. Evid. Based Commun. Assess. Interv. 2022, 16, 105–122. [Google Scholar] [CrossRef]
- Coplan, J. Early Language Milestone Scale: Examiner’s Manual. PRO-ED. 1993. Available online: https://www.aucd.org/uploads/itacresourcefiles/ELM.PDF (accessed on 23 June 2025).
- Lewis, M. Early Language Milestone Scale. In Encyclopedia of Autism Spectrum Disorders; Springer: New York, NY, USA, 2013; pp. 1032–1033. [Google Scholar]
- Loffler, G.; Gordon, G.E. Cognitive function in Rett syndrome: Profoundly impaired or near normal? Eur. J. Paediatr. Neurol. 2018, 22, 2–3. [Google Scholar] [CrossRef] [PubMed]
- Levine, J.; Hakim, F.; Kooy, R.F.; Gozes, I. Vineland adaptive behavior scale in a cohort of four ADNP syndrome patients implicates age-dependent developmental delays with increased impact of activities of daily living. J. Mol. Neurosci. 2022, 72, 1531–1546. [Google Scholar] [CrossRef] [PubMed]
- Perry, A.; Flanagan, H.E.; Dunn Geier, J.; Freeman, N.L. Brief report: The Vineland Adaptive Behavior Scales in young children with autism spectrum disorders at different cognitive levels. J. Autism Dev. Disord. 2009, 39, 1066–1078. [Google Scholar] [CrossRef] [PubMed]
- Salomon-Estebanez, M.; Mohamed, Z.; Michaelidou, M.; Collins, H.; Rigby, L.; Skae, M.; Padidela, R.; Rust, S.; Dunne, M.; Cosgrove, K. Vineland adaptive behavior scales to identify neurodevelopmental problems in children with Congenital Hyperinsulinism (CHI). Orphanet J. Rare Dis. 2017, 12, 96. [Google Scholar] [CrossRef] [PubMed]
- Hedrick, D.L.; Prather, E.M.; Tobin, A.R. Sequenced Inventory of Communication Development; University of Washington Press: Washington, DC, USA, 1975. [Google Scholar]
- Thompson, L.A.; Plomin, R. The sequenced inventory of communication development: An adoption study of two and three-year olds. Int. J. Behav. Dev. 1988, 11, 219–231. [Google Scholar] [CrossRef]
- Ibrahim, S.B.; Vasalou, A.; Clarke, M. Design opportunities for AAC and children with severe speech and physical impairments. In Proceedings of the 2018 CHI Conference on Human Factors in Computing Systems, Montreal, QC, Canada, 21–26 April 2018; pp. 1–13. [Google Scholar]
- Wandin, H.; Lindberg, P.; Sonnander, K. Aided language modelling, responsive communication and eye-gaze technology as communication intervention for adults with Rett syndrome: Three experimental single case studies. Disabil. Rehabil. Assist. Technol. 2023, 18, 1011–1025. [Google Scholar] [CrossRef] [PubMed]
- Neul, J.L.; Benke, T.A.; Marsh, E.D.; Suter, B.; Silveira, L.; Fu, C.; Peters, S.U.; Percy, A.K.; for the Rett syndrome Natural History Study Group; Skinner, S.A.; et al. Top caregiver concerns in Rett syndrome and related disorders: Data from the US natural history study. J. Neurodev. Disord. 2023, 15, 33. [Google Scholar] [CrossRef] [PubMed]
- Girtler, S.N.; Unholz-Bowden, E.K.; Shipchandler, A.; Kolb, R.L.; McComas, J.J. Use of Augmentative and Alternative Communication by Individuals with Rett Syndrome Part 1: Page-Linking. J. Dev. Phys. Disabil. 2024, 36, 125–145. [Google Scholar] [CrossRef] [PubMed]
- Xavier, J.S.; Orsati, F.T.; Laurence, P.G.; Barbosa, L.K.; Gouveia, A.S.; D’ANtino, M.E.F.; Lukasova, K.; Macedo, E.C.; Schwartzman, J.S. Insights into Rett Syndrome girls’ receptive vocabulary through eye movements and parental perception. Eur. J. Paediatr. Neurol. 2024, 51, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Passaro, A.; Zullo, A.; Di Gioia, M.; Curcio, E.; Stasolla, F. A Narrative Review on the Use of Eye-Tracking in Rett Syndrome: Implications for Diagnosis and Treatment. OBM Genet. 2024, 8, 250. [Google Scholar] [CrossRef]
- Voniati, L.; Georgiou, R.; Papaleontiou, A.; Tsapara, A.; Papadopoulos, A.; Tafiadis, D. Scoping Review of Communication Abilities of Children with Rett Syndrome in Daily Routine: A Communication Partners’ Perspectives. Adv. Neurodev. Disord. 2024, 9, 185–194. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Voniati, L.; Papadopoulos, A.; Ziavra, N.; Tafiadis, D. Communication Abilities, Assessment Procedures, and Intervention Approaches in Rett Syndrome: A Narrative Review. Brain Sci. 2025, 15, 753. https://doi.org/10.3390/brainsci15070753
Voniati L, Papadopoulos A, Ziavra N, Tafiadis D. Communication Abilities, Assessment Procedures, and Intervention Approaches in Rett Syndrome: A Narrative Review. Brain Sciences. 2025; 15(7):753. https://doi.org/10.3390/brainsci15070753
Chicago/Turabian StyleVoniati, Louiza, Angelos Papadopoulos, Nafsika Ziavra, and Dionysios Tafiadis. 2025. "Communication Abilities, Assessment Procedures, and Intervention Approaches in Rett Syndrome: A Narrative Review" Brain Sciences 15, no. 7: 753. https://doi.org/10.3390/brainsci15070753
APA StyleVoniati, L., Papadopoulos, A., Ziavra, N., & Tafiadis, D. (2025). Communication Abilities, Assessment Procedures, and Intervention Approaches in Rett Syndrome: A Narrative Review. Brain Sciences, 15(7), 753. https://doi.org/10.3390/brainsci15070753








