Effect of Safinamide on Non-Motor Symptoms and Quality of Life in Parkinson’s Disease Patients According to Sex, Age, Disease Duration and Levodopa Equivalent Daily Dose
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Analysis
2.2. Standard Protocol Approvals, Registrations, and Patient Consents
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AEs | adverse events |
| H&Y | Hoen & Yahr |
| DD | disease duration |
| LEDD | levodopa equivalent daily dose |
| NMS | non-motor symptoms |
| NMSS | Non-Motor Symptoms Scale |
| PD | Parkinson’s disease |
| PDQ-39SI | 39-item Parkinson’s Disease Quality of Life Questionnaire Summary Index |
| QoL | quality of life |
References
- Willis, A.W.; Roberts, E.; Beck, J.C.; Fiske, B.; Ross, W.; Savica, R.; Van Den Eeden, S.K.; Tanner, C.M.; Marras, C.; Alcalay, R.; et al. Incidence of Parkinson disease in North America. NPJ Park. Dis. 2022, 8, 170. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, M.J.; Okun, M.S. Diagnosis and Treatment of Parkinson Disease: A Review. JAMA 2020, 323, 548–560. [Google Scholar] [CrossRef]
- Barone, P.; Antonini, A.; Colosimo, C.; Marconi, R.; Morgante, L.; Avarello, T.P.; Bottacchi, E.; Cannas, A.; Ceravolo, G.; Ceravolo, R.; et al. The PRIAMO study: A multicenter assessment of nonmotor symptoms and their impact on quality of life in Parkinson’s disease. Mov. Disord. 2009, 24, 1641–1649. [Google Scholar] [CrossRef]
- Martinez-Martin, P.; Rodriguez-Blazquez, C.; Kurtis, M.M.; Chaudhuri, K.R.; NMSS Validation Group. The impact of non-motor symptoms on health-related quality of life of patients with Parkinson’s disease. Mov. Disord. 2011, 26, 399–406. [Google Scholar] [CrossRef]
- Santos García, D.; de Deus Fonticoba, T.; Suárez Castro, E.; Borrué, C.; Mata, M.; Solano Vila, B.; Cots Foraster, A.; Álvarez Sauco, M.; Rodríguez Pérez, A.B.; Vela, L.; et al. Non-motor symptoms burden, mood, and gait problems are the most significant factors contributing to a poor quality of life in non-demented Parkinson’s disease patients: Results from the COPPADIS Study Cohort. Park. Relat. Disord. 2019, 66, 151–157. [Google Scholar] [CrossRef]
- Santos-García, D.; de la Fuente-Fernández, R. Impact of non-motor symptoms on health-related and perceived quality of life in Parkinson’s disease. J. Neurol. Sci. 2013, 332, 136–140. [Google Scholar] [CrossRef] [PubMed]
- Bloem, B.R.; Okun, M.S.; Klein, C. Parkinson’s disease. Lancet 2021, 397, 2284–2303. [Google Scholar] [CrossRef] [PubMed]
- Fox, S.H.; Katzenschlager, R.; Lim, S.-Y.; Barton, B.; de Bie, R.M.A.; Seppi, K.; Coelho, M.; Sampaio, C.; Movement Disorder Society Evidence-Based Medicine Committee. International Parkinson and movement disorder society evidence-based medicine review: Update on treatments for the motor symptoms of Parkinson’s disease. Mov. Disord. 2018, 33, 1248–1266. [Google Scholar] [CrossRef]
- Simuni, T.; Okun, M.S. Adjunctive Therapies in Parkinson Disease-Have We Made Meaningful Progress? JAMA Neurol. 2022, 79, 119–120. [Google Scholar] [CrossRef]
- Stocchi, F.; Vacca, L.; Radicati, F.G. How to optimize the treatment of early stage Parkinson’s disease. Transl. Neurodegener. 2015, 4, 4. [Google Scholar] [CrossRef]
- Fabbri, M.; Rosa, M.M.; Abreu, D.; Ferreira, J.J. Clinical pharmacology review of safinamide for the treatment of Parkinson’s disease. Neurodegener. Dis. Manag. 2015, 5, 481–496. [Google Scholar] [CrossRef] [PubMed]
- Abbruzzese, G.; Kulisevsky, J.; Bergmans, B.; Gomez-Esteban, J.C.; Kägi, G.; Raw, J.; Stefani, A.; Warnecke, T.; Jost, W.H.; the SYNAPSES Study Investigators Group. A European Observational Study to Evaluate the Safety and the Effectiveness of Safinamide in Routine Clinical Practice: The SYNAPSES Trial1. J. Park. Dis. 2021, 11, 187–198. [Google Scholar] [CrossRef]
- Borgohain, R.; Szasz, J.; Stanzione, P.; Meshram, C.; Bhatt, M.; Chirilineau, D.; Stocchi, F.; Lucini, V.; Giuliani, R.; Forrest, E.; et al. Randomized trial of safinamide add-on to levodopa in Parkinson’s disease with motor fluctuations. Mov. Disord. 2014, 29, 229–237. [Google Scholar] [CrossRef] [PubMed]
- Borgohain, R.; Szasz, J.; Stanzione, P.; Meshram, C.; Bhatt, M.H.; Chirilineau, D.; Stocchi, F.; Lucini, V.; Giuliani, R.; Forrest, E.; et al. Two-year, randomized, controlled study of safinamide as add-on to levodopa in mid to late Parkinson’s disease. Mov. Disord. 2014, 29, 1273–1280. [Google Scholar] [CrossRef] [PubMed]
- Stocchi, F.; Torti, M. Adjuvant therapies for Parkinson’s disease: Critical evaluation of safinamide. Drug Des. Dev. Ther. 2016, 10, 609–618. [Google Scholar] [CrossRef]
- Espinoza-Vinces, C.; Villino-Rodríguez, R.; Atorrasagasti-Villar, A.; Martí-Andrés, G.; Luquin, M.-R. Impact of Safinamide on Patient-Reported Outcomes in Parkinson’s Disease. Patient Relat. Outcome Meas. 2023, 14, 285–295. [Google Scholar] [CrossRef]
- Stocchi, F.; Antonini, A.; Berg, D.; Bergmans, B.; Jost, W.; Katzenschlager, R.; Kulisevsky, J.; Odin, P.; Valldeoriola, F.; Chaudhuri, K.R. Safinamide in the treatment pathway of Parkinson’s Disease: A European Delphi Consensus. NPJ Park. Dis. 2022, 8, 17. [Google Scholar] [CrossRef]
- Blair, H.A.; Dhillon, S. Safinamide: A Review in Parkinson’s Disease. CNS Drugs 2017, 31, 169–176. [Google Scholar] [CrossRef]
- Cattaneo, C.; Jost, W.H.; Bonizzoni, E. Long-Term Efficacy of Safinamide on Symptoms Severity and Quality of Life in Fluctuating Parkinson’s Disease Patients. J. Park. Dis. 2020, 10, 89–97. [Google Scholar] [CrossRef]
- Bianchi, M.L.E.; Riboldazzi, G.; Mauri, M.; Versino, M. Efficacy of safinamide on non-motor symptoms in a cohort of patients affected by idiopathic Parkinson’s disease. Neurol. Sci. 2019, 40, 275–279. [Google Scholar] [CrossRef]
- Santos García, D.; Labandeira Guerra, C.; Yáñez Baña, R.; Cimas Hernando, M.I.; Cabo Lopez, I.; Paz Gonalez, J.M.; Alonso Losada, M.G.; Gonzalez Palmas, M.J.; Martinez Miro, C. Safinamide Improves Non-Motor Symptoms Burden in Parkinson’s Disease: An Open-Label Prospective Study. Brain Sci. 2021, 11, 316. [Google Scholar] [CrossRef] [PubMed]
- Santos García, D.; Yáñez Baña, R.; Labandeira Guerra, C.; Cimas Hernando, M.I.; Cabo López, I.; Paz González, J.M.; Alonso Losada, M.G.; Gonzalez Palmás, M.J.; Cores Bartolomé, C.; Martínez Miró, C. Pain Improvement in Parkinson’s Disease Patients Treated with Safinamide: Results from the SAFINONMOTOR Study. J. Pers. Med. 2021, 11, 798. [Google Scholar] [CrossRef]
- Labandeira, C.M.; Alonso Losada, M.G.; Yáñez Baña, R.; Hernando, M.I.C.; López, I.C.; González, J.M.P.; Palmás, M.J.G.; Miró, C.M.; García, D.S. Effectiveness of Safinamide over Mood in Parkinson’s Disease Patients: Secondary Analysis of the Open-label Study SAFINONMOTOR. Adv. Ther. 2021, 38, 5398–5411. [Google Scholar] [CrossRef] [PubMed]
- Santos García, D.; Cabo López, I.; Labandeira Guerra, C.; Yanez Bana, R.; Cimas Hernando, M.I.; Paz Gonzalez, J.M.; Alonso Losada, M.G.; Gonzalez Palmas, M.J.; Cores Bartolome, C.; Martinez Miro, C. Safinamide improves sleep and daytime sleepiness in Parkinson’s disease: Results from the SAFINONMOTOR study. Neurol Sci. 2022, 43, 2537–2544. [Google Scholar] [CrossRef] [PubMed]
- Daniel, S.E.; Lees, A.J. Parkinson’s Disease Society Brain Bank, London: Overview and research. J. Neural Transm. Suppl. 1993, 39, 165–172. [Google Scholar]
- Dubois, B.; Burn, D.; Goetz, C.; Aarsland, D.; Brown, R.G.; Broe, G.A.; Dickson, D.; Duyckaerts, C.; Cummings, J.; Gauthier, S.; et al. Diagnostic procedures for Parkinson’s disease dementia: Recommendations from the movement disorder society task force. Mov. Disord. 2007, 22, 2314–2324. [Google Scholar] [CrossRef]
- Chaudhuri, K.R.; Martinez-Martin, P.; Brown, R.G.; Sethi, K.; Stocchi, F.; Odin, P.; Ondo, W.; Abe, K.; MacPhee, G.; MacMahon, D.; et al. The metric properties of a novel non-motor symptoms scale for Parkinson’s disease: Results from an international pilot study. Mov. Disord. 2007, 22, 1901–1911. [Google Scholar] [CrossRef]
- Jenkinson, C.; Fitzpatrick, R.; Peto, V.; Greenhall, R.; Hyman, N. The Parkinson’s Disease Questionnaire (PDQ-39): Development and validation of a Parkinson’s disease summary index score. Age Ageing 1997, 26, 353–357. [Google Scholar] [CrossRef]
- Virameteekul, S.; Phokaewvarangkul, O.; Bhidayasiri, R. Profiling the most elderly Parkinson’s disease patients: Does age or disease duration matter? PLoS ONE 2021, 162, e0261302. [Google Scholar] [CrossRef]
- Peretz, C.; Chillag-Talmor, O.; Linn, S.; Gurevich, T.; El-Ad, B.; Silverman, B.; Friedman, N.; Giladi, N. Parkinson’s disease patients first treated at age 75 years or older: A comparative study. Park. Relat. Disord. 2013, 20, 69–74. [Google Scholar] [CrossRef]
- Dahodwala, N.; Pettit, A.R.; Jahnke, J.; Li, P.; Ladage, V.P.; Kandukuri, P.L.; Zamudio, J.; Jalundhwala, Y.J.; Doshi, J.A. Use of a medication-based algorithm to identify advanced Parkinson’s disease in administrative claims data: Associations with claims-based indicators of disease severity. Clin. Park. Relat. Disord. 2020, 3, 100046. [Google Scholar] [CrossRef] [PubMed]
- Schade, S.; Mollenhauer, B.; Trenkwalder, C. Levodopa Equivalent Dose Conversion Factors: An Updated Proposal Including Opicapone and Safinamide. Mov. Disord. Clin. Pract. 2020, 7, 343–345. [Google Scholar] [CrossRef]
- Sharaf, J.; Williams, K.-A.D.; Tariq, M.; Acharekar, M.V.; Saldivia, S.E.G.; Unnikrishnan, S.; Chavarria, Y.Y.; Akindele, A.O.; Jalkh, A.P.; Eastmond, A.K.; et al. The Efficacy of Safinamide in the Management of Parkinson’s Disease: A Systematic Review. Cureus 2022, 14, e29118. [Google Scholar] [CrossRef] [PubMed]
- Plastino, M.; Gorgone, G.; Fava, A.; Ettore, M.; Iannacchero, R.; Scarfone, R.; Vaccaro, A.; De Bartolo, M.; Bosco, D. Effects of safinamide on REM sleep behavior disorder in Parkinson disease: A randomized, longitudinal, cross-over pilot study. J. Clin. Neurosci. 2021, 91, 306–312. [Google Scholar] [CrossRef] [PubMed]
- Qureshi, A.R.; Rana, A.Q.; Malik, S.H.; Rizvi, S.F.H.; Akhter, S.; Vannabouathong, C.; Sarfraz, Z.; Rana, R. Comprehensive Examination of Therapies for Pain in Parkinson’s Disease: A Systematic Review and Meta-Analysis. Neuroepidemiology 2018, 51, 190–206. [Google Scholar] [CrossRef]
- Nishikawa, N.; Hatano, T.; Nishioka, K.; Ueno, S.-I.; Saiki, S.; Nakamura, R.; Yoritaka, A.; Ogawa, T.; Shimo, Y.; Sako, W.; et al. Safinamide as adjunctive therapy to levodopa monotherapy for patients with Parkinson’s disease with wearing-off: The Japanese observational J-SILVER study. J. Neurol. Sci. 2024, 461, 123051. [Google Scholar] [CrossRef]
- Rinaldi, D.; Bianchini, E.; Sforza, M.; Alborghetti, M.; Galli, S.; Salvetti, M.; Giovannelli, M.; Pontieri, F.E. The tolerability, safety and efficacy of safinamide in elderly Parkinson’s disease patients: A retrospective study. Aging Clin. Exp. Res. 2021, 33, 1689–1692. [Google Scholar] [CrossRef]
- Monaco, M.R.L.; Petracca, M.; Vetrano, D.L.; Di Stasio, E.; Fusco, D.; Ricciardi, D.; Laudisio, A.; Zuccalà, G.; Onder, G.; Bentivoglio, A.R. Safinamide as an adjunct therapy in older patients with Parkinson’s disease: A retrospective study. Aging Clin. Exp. Res. 2020, 32, 1369–1373. [Google Scholar] [CrossRef]
- Kulisevsky, J.; Esquivel, A.; Freire-Álvarez, E.; Gomez-Esteban, J.C.; Legarda-Ramirez, I.; Avilés, A.; Mata-Álvarez-Satullano, M.; SYNAPSES Study Investigators Group. A European observational study to evaluate the safety and the effectiveness of safinamide in routine clinical practice: Post-hoc analysis of the Spanish study population. Rev. Neurol. 2023, 77, S1. [Google Scholar]
- Peña, E.; Borrué, C.; Mata, M.; Martínez-Castrillo, J.C.; Alonso-Canovas, A.; Chico, J.L.; López-Manzanares, L.; Llanero, M.; Herreros-Rodríguez, J.; Esquivel, A.; et al. Impact of SAfinamide on Depressive Symptoms in Parkinson’s Disease Patients (SADness-PD Study): A Multicenter Retrospective Study. Brain Sci. 2021, 11, 232. [Google Scholar] [CrossRef]
- Liguori, C.; Stefani, A.; Ruffini, R.; Mercuri, N.B.; Pierantozzi, M. Safinamide effect on sleep disturbances and daytime sleepiness in motor fluctuating Parkinson’s disease patients: A validated questionnaires-controlled study. Park. Relat. Disord. 2018, 57, 80–81. [Google Scholar] [CrossRef] [PubMed]
- Geroin, C.; Di Vico, I.A.; Squintani, G.; Segatti, A.; Bovi, T.; Tinazzi, M. Effects of safinamide on pain in Parkinson’s disease with motor fluctuations: An exploratory study. J. Neural Transm. 2020, 127, 1143–1152. [Google Scholar] [CrossRef]
- Santos-García, D.; Laguna, A.; Hernández-Vara, J.; Fonticoba, T.d.D.; Bartolomé, C.C.; Painceiras, M.J.F.; Íñiguez-Alvarado, M.C.; Díaz, I.G.; Jesús, S.; Boungiorno, M.T.; et al. Sex Differences in Motor and Non-Motor Symptoms among Spanish Patients with Parkinson’s Disease. J. Clin. Med. 2023, 12, 1329. [Google Scholar] [CrossRef] [PubMed]
- Gómez-López, A.; Sánchez-Sánchez, A.; Natera-Villalba, E.; Ros-Castelló, V.; Beltrán-Corbellini, Á.; Fanjul-Arbós, S.; Moreno, I.P.; Moreno, J.L.L.-S.; Castrillo, J.C.M.; Alonso-Canovas, A. SURINPARK: Safinamide for Urinary Symptoms in Parkinson’s Disease. Brain Sci. 2021, 11, 57. [Google Scholar] [CrossRef]
- De Micco, R.; Satolli, S.; Siciliano, M.; De Mase, A.; Giordano, A.; Tedeschi, G.; Tessitore, A. Effects of safinamide on non-motor, cognitive, and behavioral symptoms in fluctuating Parkinson’s disease patients: A prospective longitudinal study. Neurol. Sci. 2022, 43, 357–364. [Google Scholar] [CrossRef]
- Pellecchia, M.T.; Picillo, M.; Russillo, M.C.; De Pandis, M.F.; Bonizzoni, E.; Marjanovic, I.; Cattaneo, C. Efficacy of Safinamide and Gender Differences During Routine Clinical Practice. Front. Neurol. 2021, 12, 756304. [Google Scholar] [CrossRef] [PubMed]
- Cattaneo, C.; Jost, W.H. Pain in Parkinson’s Disease: Pathophysiology, Classification and Treatment. J. Integr. Neurosci. 2023, 22, 132. [Google Scholar] [CrossRef]
- Beiske, A.G.; Loge, J.H.; Rønningen, A.; Svensson, E. Pain in Parkinson’s disease: Prevalence and characteristics. Pain 2009, 141, 173–177. [Google Scholar] [CrossRef]
- Cattaneo, C.; Kulisevsky, J.; Tubazio, V.; Castellani, P. Long-term Efficacy of Safinamide on Parkinson’s Disease Chronic Pain. Adv. Ther. 2018, 35, 515–522. [Google Scholar] [CrossRef]
- Stocchi, F.; Borgohain, R.; Onofrj, M.; Schapira, A.H.; Bhatt, M.; Lucini, V.; Giuliani, R.; Anand, R.; Study 015 Investigators. A randomized, double-blind, placebo-controlled trial of safinamide as add-on therapy in early Parkinson’s disease patients. Mov. Disord. 2012, 27, 106–112. [Google Scholar] [CrossRef]
- Cattaneo, C.; Barone, P.; Bonizzoni, E.; Sardina, M. Effects of Safinamide on Pain in Fluctuating Parkinson’s Disease Patients: A Post-Hoc Analysis. J. Park. Dis. 2017, 7, 95–101. [Google Scholar] [CrossRef] [PubMed]
- Cattaneo, C.; Sardina, M.; Bonizzoni, E. Safinamide as Add-On Therapy to Levodopa in Mid- to Late-Stage Parkinson’s Disease Fluctuating Patients: Post hoc Analyses of Studies 016 and SETTLE. J. Park. Dis. 2016, 6, 165–173. [Google Scholar] [CrossRef]
- Tsuboi, Y.; Hattori, N.; Yamamoto, A.; Sasagawa, Y.; Nomoto, M.; ME2125-4 Study Group. Long-term safety and efficacy of safinamide as add-on therapy in levodopa-treated Japanese patients with Parkinson’s disease with wearing-off: Results of an open-label study. J. Neurol. Sci. 2020, 416, 117012. [Google Scholar] [CrossRef]
- Hayes, M.T. Parkinson’s Disease and Parkinsonism. Am. J. Med. 2019, 132, 802–807. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Martin, P.; Pecurariu, C.F.; Odin, P.; Hilten, J.J.; Antonini, A.; Rojo-Abuin, J.M.; Borges, V.; Trenkwalder, C.; Aarsland, D.; Brooks, D.J.; et al. Gender-related differences in the burden of non-motor symptoms in Parkinson’s disease. J. Neurol. 2012, 259, 1639–1647. [Google Scholar] [CrossRef]
- Pellecchia, M.T.; Picillo, M.; Russillo, M.C.; Andreozzi, V.; Oliveros, C.; Cattaneo, C. The effects of safinamide according to gender in Chinese parkinsonian patients. Sci. Rep. 2023, 13, 20632. [Google Scholar] [CrossRef]
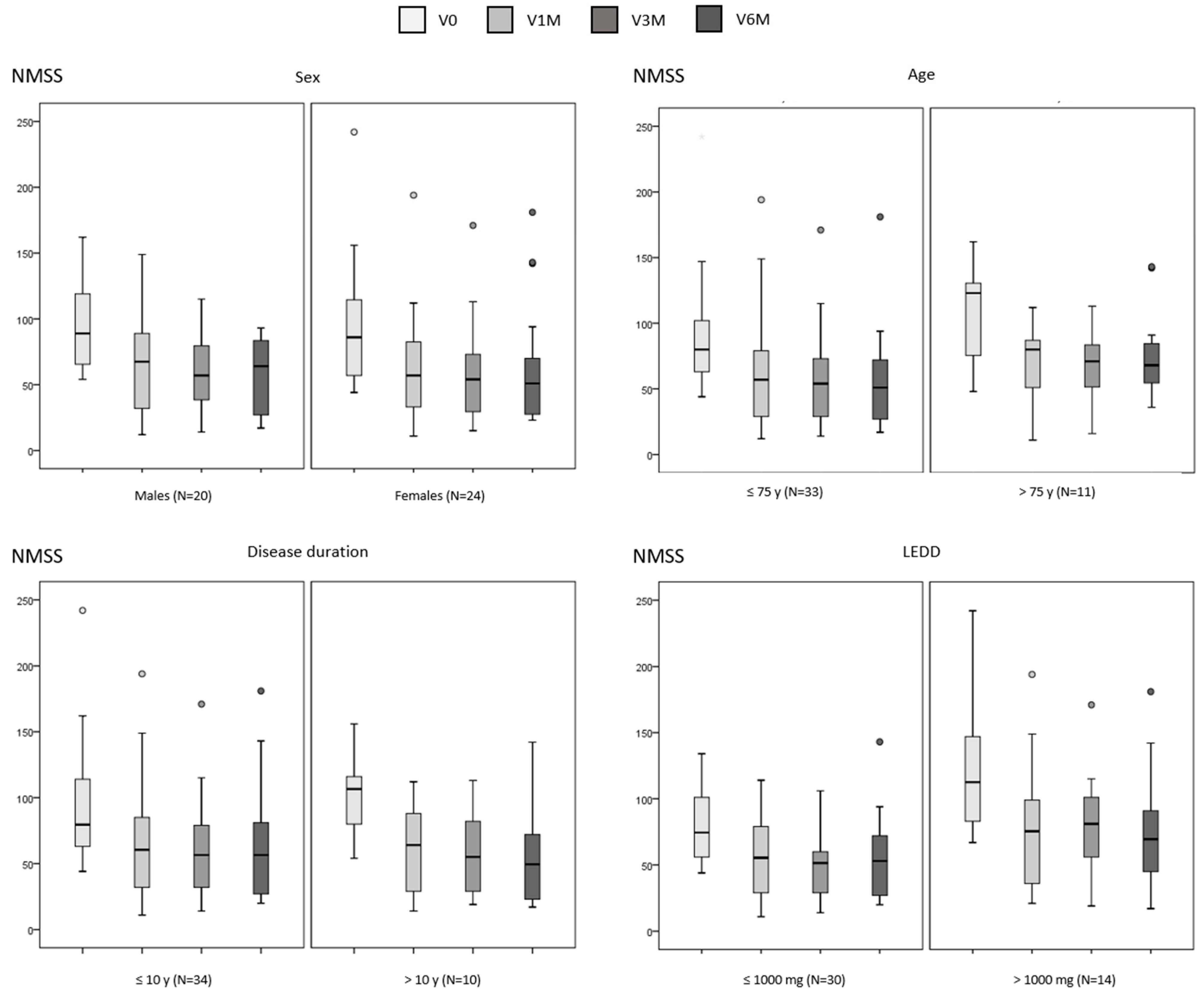
| At V0 | At V6M | Cohen’s d | p a | p b | p c | |
|---|---|---|---|---|---|---|
| Sex | 0.629 | 0.494 | ||||
| Males (N = 20) | 93.6 ± 32.4 | 59.4 ± 27.7 | −1.8 | <0.0001 | ||
| Females (N = 24) | 93.6 ± 45.2 | 60.4 ± 41.5 | −1.3 | 0.001 | ||
| Age | 0.069 | 0.050 | ||||
| ≤75 y (N = 33) | 88.6 ± 38.9 | 54.2 ± 34 | −1.9 | <0.0001 | ||
| >75 y (N = 11) | 108.7 ± 38.6 | 77.2 ± 35.6 | −1.0 | 0.040 | ||
| Disease duration | 0.353 | 0.268 | ||||
| ≤10 y (N = 34) | 90.7 ± 41.1 | 61.6 ± 35.5 | −1.4 | <0.0001 | ||
| >10 y (N = 10) | 102 ± 35.1 | 55.2 ± 38.7 | −1.9 | 0.015 | ||
| LEDD | 0.004 | 0.425 | ||||
| ≤1000 mg (N = 30) | 80.9 ± 28.1 | 53.6 ± 28.2 | −1.4 | <0.0001 | ||
| >1000 mg (N = 14) | 121.3 ± 49 | 68.2 ± 43.1 | −1.7 | 0.002 |
| Males (N = 20) | Females (N = 24) | ≤75 y Old (N = 33) | >75 y Old (N = 11) | ≤10 y DD (N = 34) | >10 y DD (N = 10) | ≤1000 mg LEDD (N = 30) | >1000 mg LEDD (N = 14) | |
|---|---|---|---|---|---|---|---|---|
| Cardiovascular | ||||||||
| At V0 | 8.8 ± 12.1 | 8.7 ± 11.4 | 7.5 ± 11.1 | 12.5 ± 12.9 | 9.3 ± 11.1 | 6.7 ± 13.4 | 8.9 ± 11.3 | 8.3 ± 12.6 |
| At V6M | 8.8 ± 12.3 | 5 ± 9.7 | 3.8 ± 7.5 | 15.5 ± 14.9 | 7.3 ± 11.1 | 4.6 ± 10.5 | 7.1 ± 11.4 | 5.9 ± 10.2 |
| Cohen’s d | 0.0 | −0.4 | −0.4 | 0.3 | −0.2 | −0.2 | −0.2 | −0.3 |
| p value | 0.838 | 0.244 | 0.077 | 0.552 | 0.298 | 0.785 | 0.385 | 0.483 |
| Sleep/fatigue | ||||||||
| At V0 | 34.9 ± 16 | 34 ± 23.7 | 35.3 ± 20.4 | 31.8 ± 21 | 34.9 ± 19.7 | 32.7 ± 23.6 | 31.3 ± 16.8 | 41.2 ± 25.9 |
| At V6M | 19.2 ± 15.2 | 26.5 ± 19.9 | 21.3 ± 16.4 | 28.6 ± 22.4 | 23.8 ± 19.4 | 21 ± 13.4 | 23.9 ± 19.5 | 21.6 ± 15.3 |
| Cohen’s d | −1.6 | −0.4 | −1.0 | −0.2 | −0.7 | −0.6 | −0.5 | −1.0 |
| p value | <0.0001 | 0.253 | 0.001 | 0.755 | 0.008 | 0.126 | 0.045 | 0.023 |
| Mood/apathy | ||||||||
| At V0 | 26.3 ± 11.5 | 36.3 ± 30 | 30.5 ± 27.8 | 35.3 ± 24.6 | 27.2 ± 26.5 | 47.3 ± 22.4 | 25 ± 22.7 | 46 ± 30.1 |
| At V6M | 11.5 ± 12.9 | 17 ± 23.8 | 12.7 ± 19.6 | 19.9 ± 19.6 | 14.2 ± 20.6 | 15.4 ± 16.9 | 11.3 ± 13.6 | 21.3 ± 28.1 |
| Cohen’s d | −1.5 | −1.2 | −1.4 | −1.1 | −1.2 | −2.2 | −1.2 | −1.6 |
| p value | 0.001 | <0.0001 | <0.0001 | 0.040 | <0.0001 | 0.005 | <0.0001 | 0.004 |
| Perceptual symptoms | ||||||||
| At V0 | 3.9 ± 7.8 | 3.4 ± 7.3 | 3.7 ± 6.5 | 3.2 ± 9.9 | 4.3 ± 8.3 | 1.4 ± 2.6 | 2.7 ± 6.6 | 5.6 ± 8.8 |
| At V6M | 4.6 ± 7.9 | 1.4 ± 2.7 | 2.8 ± 6.1 | 2.8 ± 5.4 | 2.9 ± 5.6 | 2.5 ± 6.9 | 2.3 ± 4.9 | 3.9 ± 7.7 |
| Cohen’s d | 0.1 | −0.4 | −0.1 | −0.1 | −0.2 | 0.19 | −0.1 | −0.2 |
| p value | 0.866 | 0.301 | 0.336 | 0.989 | 0.432 | 0.891 | 0.759 | 0.475 |
| Attention/memory | ||||||||
| At V0 | 20.6 ± 17.6 | 14 ± 17.4 | 16.4 ± 15.9 | 18.7 ± 22.7 | 15.2 ± 17.4 | 23.1 ± 17.9 | 13.2 ± 15.4 | 25 ± 19.9 |
| At V6M | 14 ± 17.1 | 12.7 ± 19.4 | 11.1 ± 12.3 | 19.9 ± 29.5 | 11.5 ± 17.3 | 19.4 ± 20.6 | 9.6 ± 15.2 | 21.2 ± 21.9 |
| Cohen’s d | −0.9 | −0.1 | −0.7 | 0.1 | −0.6 | −0.3 | −0.5 | −0.3 |
| p value | 0.010 | 0.482 | 0.006 | 0.858 | 0.020 | 0.553 | 0.032 | 0.373 |
| Gastrointestinal symptoms | ||||||||
| At V0 | 19.9 ± 17.6 | 17.4 ± 16.6 | 16.1 ± 15.8 | 25.8 ± 18.8 | 19.3 ± 17.5 | 15.6 ± 15.2 | 17.9 ± 16.1 | 19.6 ± 19.2 |
| At V6M | 11.9 ± 11.4 | 14.1 ± 14.7 | 10.5 ± 11.7 | 20.9 ± 14.9 | 14.6 ± 12.9 | 8.1 ± 13.3 | 11.8 ± 12 | 16.1 ± 15.5 |
| Cohen’s d | −1.0 | −0.3 | −0.6 | −0.4 | −0.5 | −0.5 | −0.7 | −0.3 |
| p value | 0.019 | 0.148 | 0.027 | 0.090 | 0.042 | 0.108 | 0.014 | 0.278 |
| Urinary symptoms | ||||||||
| At V0 | 45 ± 29.3 | 42.7 ± 30.7 | 40.3 ± 26.3 | 54 ± 37.9 | 44.8 ± 29.6 | 40 ± 31.8 | 37.5 ± 26.4 | 57.1 ± 33.1 |
| At V6M | 37.2 ± 25.4 | 25.1 ± 21.6 | 29.9 ± 25.7 | 32.5 18.6 | 33.6 ± 25.2 | 20.6 ± 16.6 | 28.3 ± 20.9 | 35.5 ± 29.8 |
| Cohen’s d | −0.4 | −1.1 | −0.6 | −1.2 | −0.7 | −0.8 | −0.6 | −1.1 |
| p value | 0.251 | <0.0001 | 0.034 | 0.021 | 0.012 | 0.086 | 0.031 | 0.039 |
| Sexual dysfunction | ||||||||
| At V0 | 40.2 ± 36.4 | 19.4 ± 33.8 | 23.4 ± 31.8 | 45.4 ± 44.3 | 31.5 ± 37.7 | 20 ± 30.1 | 24 ± 31.1 | 39.3 ± 44.7 |
| At V6M | 32.1 ± 33.9 | 17.2 ± 32.9 | 20.4 ± 32.3 | 39.8 ± 34.4 | 27.6 ± 34.7 | 17.5 ± 29.8 | 18.6 ± 26.7 | 39.6 ± 42.5 |
| Cohen’s d | −0.3 | −0.2 | −0.1 | −0.2 | −0.1 | −0.3 | −0.2 | 0.0 |
| p value | 0.672 | 0.812 | 0.823 | 0.888 | 0.875 | 0.565 | 0.639 | 0.799 |
| Miscellaneous | ||||||||
| At V0 | 29.2 ± 21 | 34.5 ± 21.1 | 30.6 ± 21.1 | 36.3 ± 21 | 30.2 ± 18 | 38.3 ± 29.4 | 29.9 ± 19 | 36.8 ± 24.1 |
| At V6M | 16 ± 12.1 | 21.4 ± 15.3 | 19.5 ± 14.7 | 17.4 ± 12.3 | 18.7 ± 11.6 | 19.8 ± 21.1 | 18.9 ± 11.4 | 19.1 ± 19 |
| Cohen’s d | −1.2 | −1.1 | −1.1 | −1.4 | −1.0 | −1.6 | −1.0 | −1.6 |
| p value | 0.002 | 0.002 | <0.0001 | 0.013 | <0.0001 | 0.012 | 0.001 | 0.003 |
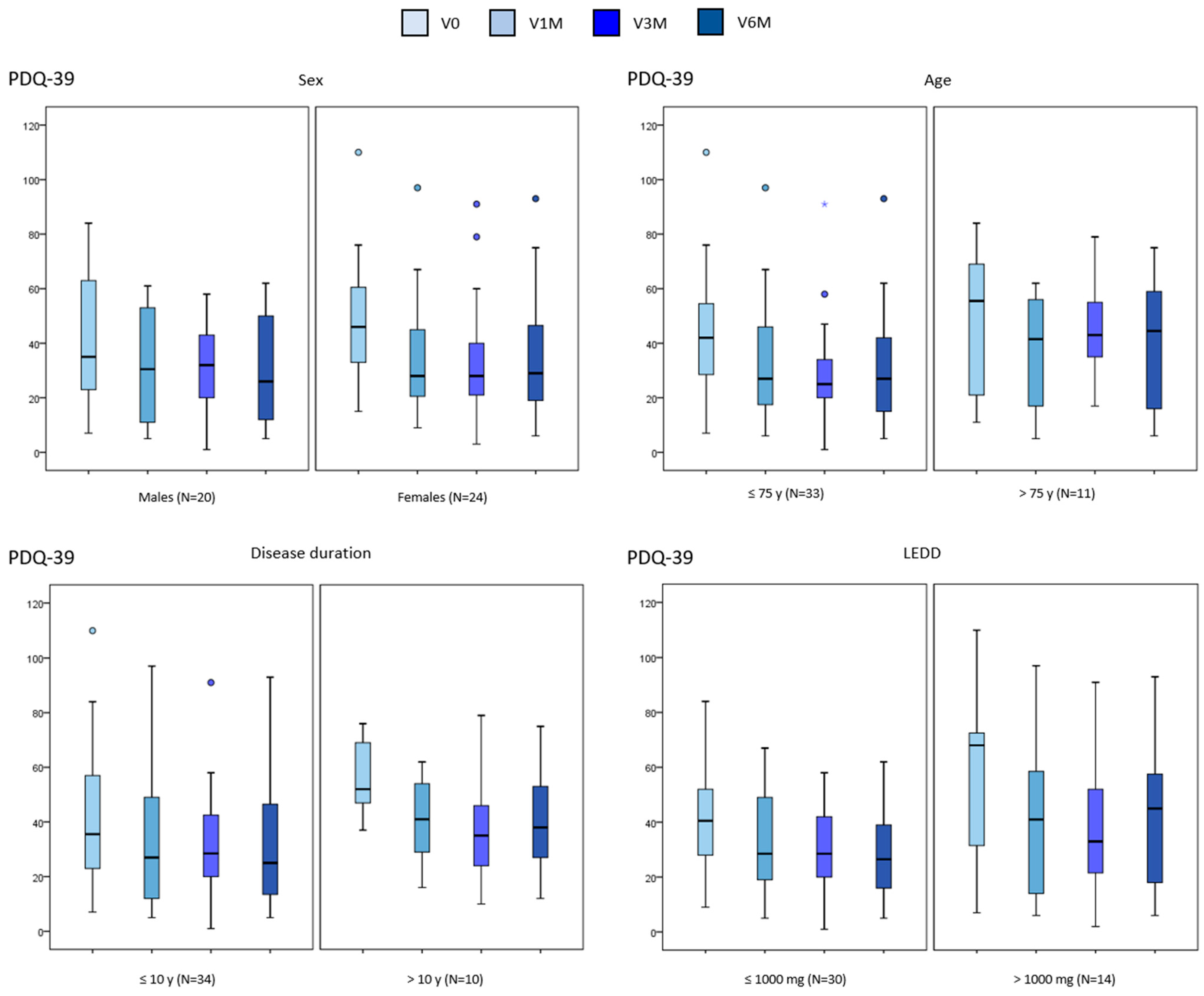
| At V0 | At V6M | Cohen’s d | p a | p b | p c | |
|---|---|---|---|---|---|---|
| Sex | 0.202 | 0.741 | ||||
| Males (N = 20) | 39.1 ± 23.3 | 32.4 ± 20.2 | −0.5 | 0.080 | ||
| Females (N = 24) | 48.3 ± 22.1 | 34.5 ± 22.7 | −1.4 | <0.0001 | ||
| Age | 0.632 | 0.124 | ||||
| ≤75 y (N = 33) | 43.2 ± 22.2 | 30.4 ± 19.8 | −1.4 | <0.0001 | ||
| >75 y (N = 11) | 46.7 ± 25.6 | 42.4 ± 24 | −0.3 | 0.306 | ||
| Disease duration | 0.009 | 0.105 | ||||
| ≤10 y (N = 34) | 40.3 ± 23.5 | 31.2 ± 21.5 | −0.8 | 0.002 | ||
| >10 y (N = 10) | 57.9 ± 14.2 | 42.1 ± 19.9 | −2.1 | 0.011 | ||
| LEDD | 0.391 | 0.265 | ||||
| ≤1000 mg (N = 30) | 40.9.9 ± 18.5 | 29.1 ± 17.1 | −1.1 | <0.0001 | ||
| >1000 mg (N = 14) | 50.6 ± 31.8 | 41.9 ± 26.8 | −0.6 | 0.119 |
| Males (N = 20) | Females (N = 24) | ≤75 y Old (N = 33) | >75 y Old (N = 11) | ≤10 y DD (N = 34) | >10 y DD (N = 10) | ≤1000 mg LEDD (N = 30) | >1000 mg LEDD (N = 14) | |
|---|---|---|---|---|---|---|---|---|
| Mobility | ||||||||
| At V0 | 22.3 ± 30.3 | 42.5 ± 27.6 | 31.4 ± 25.9 | 38.9 ± 28.2 | 28.3 ± 25.7 | 50.3 ± 21.9 | 30.5 ± 20.7 | 39.3 ± 35.7 |
| At V6M | 23.5 ± 22.8 | 33.8 ± 29.4 | 23.5 ± 22.7 | 45.9 ± 32.1 | 25.9 ± 25.6 | 40 ± 29.5 | 24.3 ± 20.4 | 39.2 ± 35.9 |
| Cohen’s d | 0.1 | −0.6 | −0.7 | 0.5 | −0.2 | −0.9 | −0.5 | 0.0 |
| p value | 0.584 | 0.017 | 0.004 | 0.592 | 0.184 | 0.074 | 0.021 | 0.574 |
| Activities of daily living | ||||||||
| At V0 | 24.6 ± 23.4 | 27.6 ± 22.1 | 25.3 ± 21.9 | 29.2 ± 24.9 | 22.4 ± 20.2 | 39.2 ± 25.9 | 23.1 ± 21.8 | 33 ± 23.2 |
| At V6M | 18.3 ± 18.1 | 17.4 ± 18.2 | 14.9 ± 15.6 | 26.5 ± 22.2 | 14.8 ± 15.4 | 27.9 ± 22.9 | 15.2 ± 15.3 | 23.2 ± 22.3 |
| Cohen’s d | −0.5 | −0.8 | −0.9 | −0.2 | −0.6 | −0.8 | −0.6 | −0.8 |
| p value | 0.244 | 0.019 | 0.002 | 0.964 | 0.047 | 0.114 | 0.119 | 0.073 |
| Emotional well-being | ||||||||
| At V0 | 31.4 ± 23.4 | 48.4 ± 27 | 40.4 ± 26.9 | 42.4 ± 27.1 | 38.6 ± 26.6 | 48.3 ± 26.7 | 39.4 ± 24.2 | 44.2 ± 32.3 |
| At V6M | 22.1 ± 20.9 | 29.8 ± 24.4 | 24.6 ± 24.1 | 31.4 ± 19.6 | 26.6 ± 23.3 | 25.4 ± 23 | 23.1 ± 20.2 | 33.3 ± 27.7 |
| Cohen’s d | −0.8 | −1.3 | −1.1 | −1.0 | −0.9 | −1.9 | −1.1 | −1.1 |
| p value | 0.040 | <0.0001 | <0.0001 | 0.052 | 0.002 | 0.008 | <0.0001 | 0.022 |
| Stigmatization | ||||||||
| At V0 | 21.7 ± 25.4 | 9.1 ± 10.9 | 13.9 ± 18.8 | 17 ± 22.4 | 14.4 ± 18.9 | 15.6 ± 22.4 | 15.4 ± 18.7 | 12.9 ± 21.9 |
| At V6M | 11.9 ± 16.1 | 4.2 ± 8.9 | 6.8 ± 12 | 10.2 ± 16.3 | 6.4 ± 12.3 | 11.8 ± 15.4 | 9.6 ± 14.4 | 3.6 ± 8.7 |
| Cohen’s d | −0.6 | −0.5 | −0.5 | −0.9 | −0.6 | −0.3 | −0.6 | −0.5 |
| p value | 0.070 | 0.107 | 0.057 | 0.063 | 0.011 | 0.492 | 0.024 | 0.207 |
| Social support | ||||||||
| At V0 | 7.5 ± 8.7 | 4.5 ± 10.7 | 5.2 ± 9.1 | 7.6 ± 12 | 4.5 ± 8.9 | 10 ± 12.3 | 5 ± 9.7 | 7.7 ± 10.5 |
| At V6M | 3.3 ± 11.3 | 3.8 ± 193.9 | 4.3 ± 14.4 | 1.5 ± 3.8 | 2.2 ± 8.8 | 8.3 ± 21.1 | 4.4 ± 14.9 | 1.8 ± 4.8 |
| Cohen’s d | −0.4 | −0.1 | −0.1 | −0.7 | −0.3 | −0.2 | −0.1 | −0.7 |
| p value | 0.121 | 0.752 | 0.651 | 0.131 | 0.181 | 0.750 | 0.643 | 0.111 |
| Cognition | ||||||||
| At V0 | 27.9 ± 20.9 | 22.1 ± 16.9 | 26.2 ± 19.7 | 20.4 ± 16.1 | 25.4 ± 20.5 | 22.5 ± 12.6 | 23.1 ± 15.1 | 28.4 ± 25.9 |
| At V6M | 28.4 ± 25.3 | 19.8 ± 19.5 | 24.4 ± 22 | 21.6 ± 24.9 | 22.9 ± 21.6 | 26.2 ± 26.3 | 19.4 ± 19 | 33 ± 27.1 |
| Cohen’s d | 0.0 | −0.2 | −0.1 | 0.1 | −0.2 | 0.2 | −0.3 | 0.3 |
| p value | 0.909 | 0.158 | 0.165 | 0.893 | 0.295 | 0.918 | 0.193 | 0.929 |
| Communication | ||||||||
| At V0 | 25.9 ± 27.1 | 7.6 ± 10.9 | 15.6 ± 22.4 | 15.9 ± 19.9 | 15.9 ± 21.7 | 15 ± 25.4 | 14.7 ± 21.5 | 17.9 ± 22.3 |
| At V6M | 18.2 ± 17.5 | 6.3 ± 9.9 | 12.4 ± 15 | 11.4 16.3 | 12.7 ± 15.8 | 10 ± 13.9 | 9.2 ± 11.8 | 18.4 ± 19.6 |
| Cohen’s d | −0.3 | −0.2 | −0.2 | −0.3 | −0.2 | −0.5 | −0.4 | 0.1 |
| p value | 0.278 | 0.497 | 0.399 | 0.344 | 0.367 | 0.380 | 0.090 | 0.980 |
| Pain and discomfort | ||||||||
| At V0 | 37.2 ± 26.6 | 48.3 ± 27.7 | 43.5 ± 27.2 | 43.2 ± 29.3 | 44.2 ± 26.9 | 40.8 ± 30.3 | 42.8 ± 22.8 | 44.8 ± 37 |
| At V6M | 27.9 ± 20.9 | 37.8 ± 18.2 | 34.8 ± 19.4 | 28.8 ± 21.5 | 33.3 ± 19.8 | 33.3 ± 21.1 | 32.5 ± 19.6 | 35.1 ± 21.2 |
| Cohen’s d | −0.6 | −0.5 | −0.5 | −1.0 | −0.6 | −0.3 | −0.7 | −0.4 |
| p value | 0.070 | 0.080 | 0.076 | 0.043 | 0.019 | 0.362 | 0.016 | 0.307 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Solleiro Vidal, Á.; Yáñez Baña, R.; Labandeira Guerra, C.; Cimas Hernando, M.I.; Cabo López, I.; Paz González, J.M.; Alonso Losada, M.G.; Santos García, D. Effect of Safinamide on Non-Motor Symptoms and Quality of Life in Parkinson’s Disease Patients According to Sex, Age, Disease Duration and Levodopa Equivalent Daily Dose. Brain Sci. 2025, 15, 666. https://doi.org/10.3390/brainsci15070666
Solleiro Vidal Á, Yáñez Baña R, Labandeira Guerra C, Cimas Hernando MI, Cabo López I, Paz González JM, Alonso Losada MG, Santos García D. Effect of Safinamide on Non-Motor Symptoms and Quality of Life in Parkinson’s Disease Patients According to Sex, Age, Disease Duration and Levodopa Equivalent Daily Dose. Brain Sciences. 2025; 15(7):666. https://doi.org/10.3390/brainsci15070666
Chicago/Turabian StyleSolleiro Vidal, Ángela, Rosa Yáñez Baña, Carmen Labandeira Guerra, Maria Icíar Cimas Hernando, Iria Cabo López, Jose Manuel Paz González, Maria Gema Alonso Losada, and Diego Santos García. 2025. "Effect of Safinamide on Non-Motor Symptoms and Quality of Life in Parkinson’s Disease Patients According to Sex, Age, Disease Duration and Levodopa Equivalent Daily Dose" Brain Sciences 15, no. 7: 666. https://doi.org/10.3390/brainsci15070666
APA StyleSolleiro Vidal, Á., Yáñez Baña, R., Labandeira Guerra, C., Cimas Hernando, M. I., Cabo López, I., Paz González, J. M., Alonso Losada, M. G., & Santos García, D. (2025). Effect of Safinamide on Non-Motor Symptoms and Quality of Life in Parkinson’s Disease Patients According to Sex, Age, Disease Duration and Levodopa Equivalent Daily Dose. Brain Sciences, 15(7), 666. https://doi.org/10.3390/brainsci15070666






