Eye Tracking in Parkinson’s Disease: A Review of Oculomotor Markers and Clinical Applications
Abstract
1. Introduction
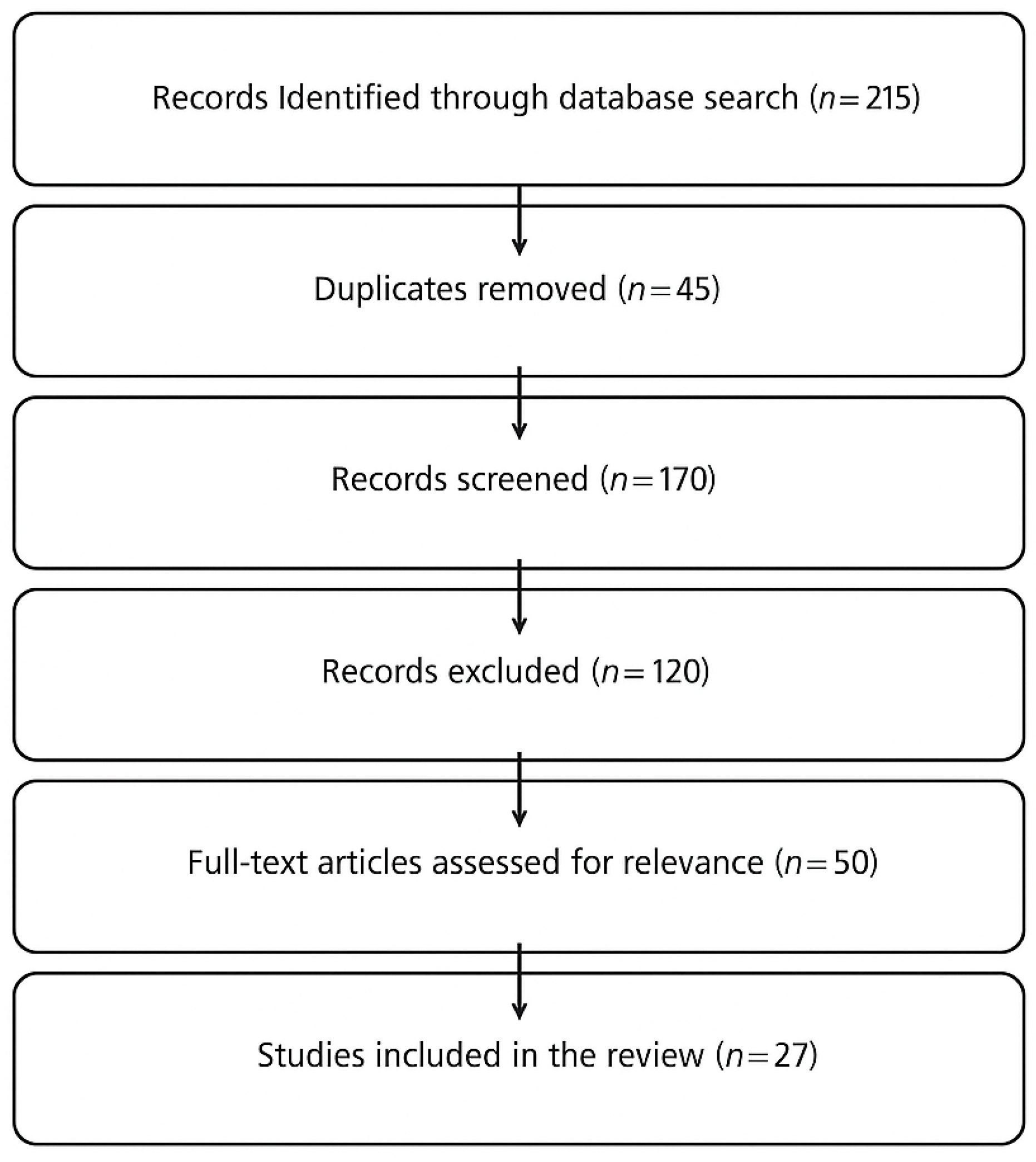
2. Methods
3. Results
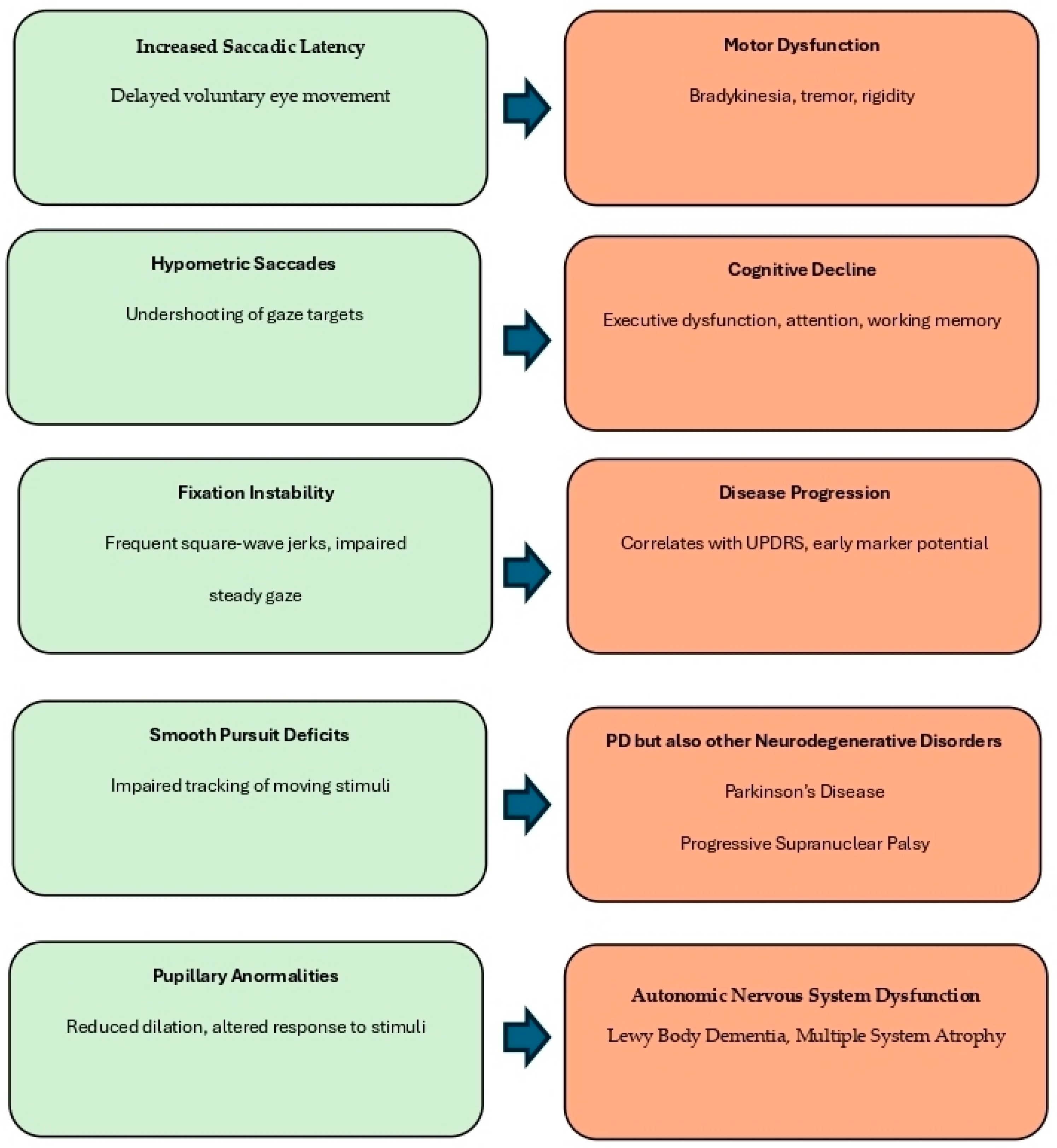
3.1. Eye Movement Abnormalities in Parkinson’s Disease
3.1.1. Saccadic Dysfunction in PD
3.1.2. Fixation Instability and Microsaccadic Intrusions
3.1.3. Smooth Pursuit and Convergence Deficits
3.1.4. Pupillary Abnormalities and Cognitive Correlates
3.2. Eye Tracking as a Diagnostic and Monitoring Tool in PD
3.2.1. Correlation Between Eye Movements and Progression in Parkinson’s Disease
3.2.2. Machine Learning Applications for Automated Diagnosis
3.3. The Role of Eye Tracking in Cognitive Assessment
3.3.1. Eye Movements and Executive Function in PD
3.3.2. Visual Search and Reading Impairments
3.4. Implications for Early Diagnosis and Clinical Interventions
3.4.1. Potential for Early Diagnosis and Disease Monitoring
3.4.2. Integration of Eye Tracking in PD Rehabilitation
| Thematic Area | Autors | Year | Sample | Objective | Methods | Results | Key Findings | |
|---|---|---|---|---|---|---|---|---|
| 1 | Smooth Pursuiit Deficits | Tanabe, J., Tregellas, J., Miller, D., Ross, R. G., & Freedman, R. | 2002 [34] | PD patients (N = 48, 26 M/22 F) | Study brain activation during smooth pursuit | Neuroimaging smooth pursuit tasks | Disrupted pursuit control mechanisms | Neurophysiological basis of pursuit deficits |
| 2 | Fixation Instability | Shaikh, A.G., Xu-Wilson, M., Grill, S., & Zee D. S. | 2011 [16] | PD patients (N = 40, 22 M/18 F) | Investigate ‘staircase’ square-wave jerks in early PD | Oculomotor testinf | Increased square-wave jerks in early PD | Fixation instability as an early PD marker |
| 3 | Fixation instability | Marx, S., Respondek, G., Stamaleou, M., Dowiasch, S., Stoll, J., Bremmer, F., & Einhäuser, W. | 2012 [32] | PD patients (N = 50, 30 M/20 F) | Differentiate PSP from PD using fixation analysis | Mobile eye.tracking | Distinct fixation instability patterns in PSP vs PD | Eye-tracking helps differentitate neurodegenerative disorders |
| 4 | Pupillary abnormalities | Wang, C.A., & Munoz, D. P. | 2015 [39] | PD patients (N = 52, 30 M/22 F) | Analyze cognitive modulation of pupil size | Pupillometry and neurocognitive tasks | Dysregulates autonomic control | Pupillary changes correlate with cognitive decline |
| 5 | Reading and Visual Impairments | Ekker, M. S., Janssen, S., Seppi, K., Poewe, W., de Vries, N. M., Theelen, T., & Bloem, B. R. | 2017 [54] | PD patients (N = 50, 27 M/23 F) | Analyze ocular disorders in PD | Comprensive visual assessments | High prevalence of visual deficits | Ocular disorders often overlooked in PD |
| 6 | Fixation Instability | Wong, O. W., Chan, A. Y., Wong, A., Lau, C. K., Yeung, J. H., Mok, V. C., ... & Chan, S. | 2018 [25] | PD patients (N = 40, 20 M/20 F) | Examine eye movement parameters and cognitive function | Eye-tracking with cognitive assessments | Fixation instability correlates with cognitive decline | Oculomotor measures predict neurocognitive impairment |
| 7 | Eye-tracking in PD Cognitive Assessment | Luke, S. G., Darowski, E. S., & Gale, S. D. | 2018 [49] | PD patients (N = 40, 20 M/20 F) | Predict cognitive impairments through eye traking | Eye movement tasks | Correlation between eye movements and cognitive decline | Early cognitive impairment detection |
| 8 | Reading and Visual Impairments | Jehangir, N., Yu, C. Y., Song, J., Shariati, M. A., Binder, S., Beyer, J., ... & Liao, Y. J. | 2018 [52] | PD patients (N = 42, 22 M/20 F) | Examine reading difficulties in PD | Saccadic analysis during reading | Slower saccadic reading | Reading impairments linked to oculomotor dysfunction |
| 9 | Saccadic Dysfunction | Stuart, S., Lawson, R. A., Yarnall, A. J., Nell, J., Alcock, L., Duncan, G. W., ... & ICICLE-PD study group. | 2019 [8] | PD patients (N = 75, 40 M/35 F) | Examine pro-saccades as predictor of cognitive decline | Saccadic eye-trackinng tasks | Prolonged saccadic latency predicts cognitive decline | Saccadic metrics correlate with executive dysfunction |
| 10 | Reading and Visual Impairments | Stock, L., Krüger-Zechlin, C., Deeb, Z., Timmermann, L., & Waldthaler, J. | 2020 [53] | PD patients (N = 45, 22 M/23 F) | Investigate reading impairments in PD | Naturalistic reading tasks with eye-tracking | PD patients show reduced reading fluency | Reading difficulties linked to cognitive dysfunction |
| 11 | Pupillary Abnormalities | Kahya, M., Lyons, K. E., Pahwa, R., Akinwuntan, A. E., He, J., & Devos, H. | 2021 [38] | PD patients (N = 50, 30 M/20 F) | Investigate pupillary responses to postural demands | Pupillometry and balance tasks | Abnormal pupillary reflex during postural adjustments | Pupil size linked to autonomic dysfunction |
| 12 | Fixation Instability | Tsitsi, P., Benfatto, M. N., Seimyr, G. Ö., Larsson, O., Svenningsson, P., & Markaki, I. | 2021 [14] | PD patients (N = 55, 28 M/27 F) | Analyze fixation duration and pupil size as PD diagnostic tools | Pupillometry and eye-tracking | Shorter fixation duration, smaller pupils | Oculomotor markers for PD diagnosis |
| 13 | Pupillary abnormalities | Tsitsi, P., Benfatto, M. N., Seimyr, G. Ö., Larsson, O., Svenningsson, P., & Markaki, I. | 2021 [14] | PD patients (N = 55, 28 M/27 F) | Investigate pupil size changes in PD | Eye-tracking and pupillometry | Reduce pupil dilatation in PD | Potential biomarker for cognitive decline |
| 14 | AI in PD diagnosis | Mei, J., Desrosiers, C., & Frasnelli, J. | 2021 [43] | PD patients (N = 85, 50 M/35 F) | Review of machine learning for PD diagnosis | Literature review | Various AI models effective in PD classification | Potential for AI in automated diagnostics |
| 15 | Motor-Ocular Function | Fasano, A., Mazzoni, A., & Falotico, E. | 2022 [37] | PD patients (N = 70, 40 M/30 F) | Asses reaching and grasping movements in PD | Oculomotor and motor coordination tests | Impaired visuomotor integration | Oculomotor deficits affect daily function |
| 16 | Saccadic Dysfunction | Kassavetis, P., Kaski, D., Anderson, T., & Hallett, M. | 2022 [4] | PD patients (N = 50, 30 M/20 F) | Investigate eye movement disorders in PD | Clinical observation eye-tracking analysis | Hypometric saccades, increased latency | Saccadic impairments serve as early biomarkers |
| 17 | Smooth Pursuit Deficits | Fooken, J., Patel, P., Jones, C. B., McKeown, M. J., & Spering, M. | 2022 [20] | PD patients (N = 60, 35 M/25 F) | Assess smoth pursuit impairments | Eye-tracking | Reduced pursuit gain, increased compensatory saccades | Deficits in motion tracking |
| 18 | Saccadic Dysfunction | Waldthaler, J., Vinding, M. C., Eriksson, A., Svenningsson, P., & Lundqvist, D. | 2022 [21] | PD patients (N = 45, 25 M/20 F) | Examine neural correlates of impaired response inhibition | EEG and antisaccade tasks | Altered brain activity during saccade inhibition | Deficits in executive function |
| 19 | Saccadic Dysfunction | Fooken, J., Patel, P., Jones, C. B., McKeown, M. J., & Spering, M. | 2022 [20] | PD patients (N = 60, 35 M/25 F) | Assess stimulus and task-specific preservation of ete movemets | Eye-tracking and neurocognitive assessments | Selective preservation of saccades in PD | Task-dependent variability in eye movements |
| 20 | AI in PD Diagnosis | Przybyszewski, A. W., Śledzianowski, A., Chudzik, A., Szlufik, S., & Koziorowski, D. | 2023 [44] | PD patients (N = 90, 48 M/42 F) | Use machine learning to analyze eye movements in neurodegeneration | AI-based classification models | High accuracy in distinguishing PD from other disorders | Machine Learning improves PD diagnostic |
| 21 | Pupillary Abnormalities | Sun, Y. R., Beylergil, S. B., Gupta, P., Ghasia, F. F., & Shaikh, A. G. | 2023 [11] | PD patients (N = 60, 33 M/27 F) | Analyze pupillary responses in PD | Pupillometry assessments | Reduced pupil dilatation linked to cognitive impairment | Potential biomarker for neurodegeneration |
| 22 | Smooth Pursuit Deficits | Swart, E. K., & Sikkema-de Jong, M. T. | 2023 [33] | PD patients (N = 55, 28 M/27 F) | Examine effects of dopamine levels on smooth pursuit | Pharmacological eye-tracking | Dopamine modulates smooth pursuit accuracy | Dopaminergic treatment improves eye tracking |
| 23 | Saccadic Dysfunction | Riek, H. C., Brien, D. C., Coe, B. C., Huang, J., Perkins, J. E., Yep, R., & Munoz, D. P. | 2023 [15] | PD patients (N = 55, 28 M/27 F) | Examine antisaccade behavior across neurodegenerative diases | Antisaccade eye-tracking tasks | Increased error rates in antisaccade tasks | Executive dysfunction correlates with saccadic impairments |
| 24 | VR- based Rehabilitation | Daniol, M., Hemmerling, D., Sikora, J., Jemiolo, P., Wodzinski, M., & Wojcik-Pedziwiatr, M. | 2024 [12] | PD patients (N = 30, 18 M/12 F) | Assess VR applications in PD neurorehabilitation | Mixed reality and eye tracking | Improved visual search and spatial awareness | VR enhances motor-cognitive coordination |
| 25 | Ai in PD Diagnosis | Chudzik, A., Śledzianowski, A., & Przybyszewski, A. W. | 2024 [10] | PD patients (N = 100, 55 M/45 F) | Assess AI and digital biomarkers in early PD detection | Machine learning analysis of eye-tracking data | High accuracy in early diagnosis | AI enhances diagnostic precision |
| 26 | Fixation Instability | Antoniades, C. A., & Spering, M. | 2024 [28] | PD patients (N = 60, 32 M/28 F) | Investigate neurophysiological mechanisms of fixation instability | Eye tracking with neural recordings | Abnormal inhibitory control of fixational eye movements | Fixation instability as a biomarker for PD |
| 27 | Pupillary Abnormalities | Gibbs, M. C., Huxley, J., Readman, M. R., Polden, M., Bredemeyer, O., Crawford, T. J., & Antoniades, C. A. | 2024 [6] | PD patients (N = 58, 31 M/27 F) | Analyze naturalistic eye movement tasks in PD | Pupillometry and real-word eye tracking | Reduced pupil dilation and impaired gaze control | Naturlistic tasks improve PD assessment |
| 28 | Ai in PD Diagnosis | Liao, X., Yao, J., Tang, H., Xing, Y., Zhao, X., Nie, D., ... & Li, G. | 2024 [2] | PD patients (N = 100, 55 M/45 F) | Use AI-driven eye movement analysis for early PD detection | Machine learning on eye-tracking data | High predictive accuracy for early PD | AI-based eye-tracking enhances diagnostic precision |
| 29 | Motor-Ocular Function | Barbieri, F. A., Polastri, P. F., Barela, J. A., Bonnet, C. T., Brito, M. B., & Rodrigues, S. T. | 2024 [31] | PD patients (N = 45, 26 M/19 F) | Investigate coupling of eye movements and postural stability | Eye tracking with balance assessments | PD patients compensate gaze instability with postural adjustments | Eye movement analisys informs fall risk assessment |
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zhang, J.; Zhang, B.; Ren, Q.; Zhong, Q.; Li, Y.; Liu, G.; Ma, X.; Zhao, C. Eye movement especially vertical oculomotor impairment as an aid to assess Parkinson’s disease. Neurol. Sci. 2020, 42, 2337–2345. [Google Scholar] [PubMed]
- Liao, X.; Yao, J.; Tang, H.; Xing, Y.; Zhao, X.; Nie, D.; Luan, P.; Li, G. Deciphering Parkinson’s Disease through Eye Movements: A Promising Tool for Early Diagnosis in the Face of Cognitive Impairment. Int. J. Clin. Pract. 2024, 1, 557923. [Google Scholar]
- Bloem, B.R.; Okun, M.S.; Klein, C. Parkinson’s disease. Lancet 2021, 397, 2284–2303. [Google Scholar] [PubMed]
- Kassavetis, P.; Kaski, D.; Anderson, T.; Hallett, M. Eye Movement Disorders in Movement Disorders. Mov. Disord. Clin. Pract. 2022, 9, 284–295. [Google Scholar] [CrossRef]
- Terao, Y.; Fukuda, H.; Yugeta, A.; Hikosaka, O.; Nomura, Y.; Segawa, M.; Ugawa, Y. Initiation and inhibitory control of saccades with the progression of Parkinson’s disease—Changes in three major drives converging on the superior colliculus. Neuropsychologia 2011, 49, 1794–1806. [Google Scholar] [CrossRef]
- Gibbs, M.C.; Huxley, J.; Readman, M.R.; Polden, M.; Bredemeyer, O.; Crawford, T.J.; Antoniades, C.A. Naturalistic Eye Movement Tasks in Parkinson’s Disease: A Systematic Review. J. Park Dis. 2024, 14, 1369–1386. [Google Scholar]
- Ştefănescu, E.; Strilciuc, Ş.; Chelaru, V.F.; Chira, D.; Mureşanu, D. Eye tracking assessment of Parkinson’s disease: A clinical retrospective analysis. J. Med. Life 2024, 17, 360–367. [Google Scholar]
- Stuart, S.; Lawson, R.A.; Yarnall, A.J.; Nell, J.; Alcock, L.; Duncan, G.W.; Khoo, T.K.; Barker, R.A.; Rochester, L.; Burn, D.J. Pro-Saccades Predict Cognitive Decline in Parkinson’s Disease: ICICLE-PD. Mov. Disord. 2019, 34, 1690–1698. [Google Scholar]
- Bek, J.; Gowen, E.; Vogt, S.; Crawford, T.J.; Poliakoff, E. Observation and imitation of object-directed hand movements in Parkinson’s disease. Sci. Rep. 2023, 13, 18749. [Google Scholar]
- Chudzik, A.; Śledzianowski, A.; Przybyszewski, A.W. Machine Learning and Digital Biomarkers Can Detect Early Stages of Neurodegenerative Diseases. Sensors 2024, 24, 1572. [Google Scholar] [CrossRef]
- Sun, Y.R.; Beylergil, S.B.; Gupta, P.; Ghasia, F.F.; Shaikh, A.G. Monitoring eye movement in patients with Parkinson’s disease: What can it tell us? Eye Brain 2023, 15, 101–112. [Google Scholar] [PubMed]
- Daniol, M.; Hemmerling, D.; Sikora, J.; Jemiolo, P.; Wodzinski, M.; Wojcik-Pedziwiatr, M. Eye-Tracking in Mixed Reality for Diagnosis of Neurodegenerative Diseases. arXiv 2024, arXiv:2404.12984. [Google Scholar]
- Orlosky, J.; Itoh, Y.; Ranchet, M.; Kiyokawa, K.; Morgan, J.; Devos, H. Emulation of physician tasks in eye-tracked virtual reality for remote diagnosis of neurodegenerative disease. IEEE Trans. Vis. Comput. Graph. 2017, 23, 1302–1311. [Google Scholar] [CrossRef]
- Tsitsi, P.; Benfatto, M.N.; Seimyr, G.Ö.; Larsson, O.; Svenningsson, P.; Markaki, I. Fixation Duration and Pupil Size as Diagnostic Tools in Parkinson’s Disease. J. Park. Dis. 2021, 11, 865–875. [Google Scholar] [CrossRef]
- Riek, H.C.; Brien, D.C.; Coe, B.C.; Huang, J.; Perkins, J.E.; Yep, R.; McLaughlin, P.M.; Orange, J.B.; Peltsch, A.J.; Roberts, A.C.; et al. Cognitive correlates of antisaccade behaviour across multiple neurodegenerative diseases. Brain. Commun. 2023, 5, fcad049. [Google Scholar]
- Shaikh, A.G.; Xu-Wilson, M.; Grill, S.; Zee, D.S. ‘Staircase’ square-wave jerks in early Parkinson’s disease. Br. J. Ophthalmol. 2011, 95, 705–709. [Google Scholar] [CrossRef]
- Rivaud-Péchoux, S.; Vidailhet, M.; Gallouedec, G.; Litvan, I.; Gaymard, B.; Pierrot-Deseilligny, C. Longitudinal ocular motor study in corticobasal degeneration and progressive supranuclear palsy. Neurology 2000, 54, 1029–1032. [Google Scholar] [CrossRef]
- MacAskill, M.R.; Anderson, T.J. Eye movements in neurodegenerative diseases. Curr. Opin. Neurol. 2016, 29, 61–68. [Google Scholar]
- Railo, H.; Olkoniemi, H.; Eeronheimo, E.; Pääkkönen, O.; Joutsa, J.; Kaasinen, V. Dopamine and eye movement control in Parkinson’s disease: Deficits in corollary discharge signals? PeerJ 2018, 6, 6038. [Google Scholar] [CrossRef]
- Fooken, J.; Patel, P.; Jones, C.B.; McKeown, M.J.; Spering, M. Preservation of Eye Movements in Parkinson’s Disease Is Stimulus- and Task-Specific. J. Neurosci. 2021, 42, 487–499. [Google Scholar] [CrossRef]
- Waldthaler, J.; Vinding, M.C.; Eriksson, A.; Svenningsson, P.; Lundqvist, D. Neural correlates of impaired response inhibition in the antisaccade task in Parkinson’s disease. Behav. Brain. Res. 2022, 422, 113763. [Google Scholar]
- Jiang, M.; Liu, Y.; Cao, Y.; Xia, S.; Teng, F.; Zhao, W.; Lin, Y.; Liu, W. Diagnosis of Parkinson’s disease by eliciting trait-specific eye movements in multi-visual tasks. J. Transl. Med. 2025, 23, 1. [Google Scholar]
- Hindle, J.V.; Martyr, A.; Clare, L. Cognitive reserve in Parkinson’s disease: A systematic review and meta-analysis. Parkinsonism Relat. Disord. 2014, 20, 1–7. [Google Scholar] [PubMed]
- Archibald, N.K.; Hutton, S.B.; Clarke, M.P.; Mosimann, U.P.; Burn, D.J. Visual exploration in Parkinson’s disease and Parkinson’s disease dementia. Brain 2013, 136, 739–750. [Google Scholar] [PubMed]
- Wong, O.W.; Chan, A.Y.; Wong, A.; Lau, C.K.; Yeung, J.H.; Mok, V.C.; Lam, L.C.; Chan, S. Eye movement parameters and cognitive functions in Parkinson’s disease patients without dementia. Parkinsonism Relat. Disord. 2018, 52, 43–48. [Google Scholar]
- Pretegiani, E.; Optican, L.M. Eye Movements in Parkinson’s Disease and Inherited Parkinsonian Syndromes. Front. Neurol. 2017, 8, 592. [Google Scholar]
- George, S.; Rey, N.L.; Tyson, T.; Esquibel, C.; Meyerdirk, L.; Schulz, E.; Pierce, S.; Burmeister, A.R.; Madaj, Z.; Steiner, J.A.; et al. Microglia affect α-synuclein cell-to-cell transfer in a mouse model of Parkinson’s disease. Mol. Neurodegener. 2019, 14, 34. [Google Scholar]
- Antoniades, C.A.; Spering, M. Eye movements in Parkinson’s disease: From neurophysiological mechanisms to diagnostic tools. Trends Neurosci. 2024, 47, 71–83. [Google Scholar]
- Wark, H.A.C.; Garell, P.C.; Walker, A.L.; Basso, M.A. A case report on fixation instability in Parkinson’s disease with bilateral deep brain stimulation implants. J. Neurol. Neurosurg. Psychiatry 2008, 79, 443–447. [Google Scholar]
- Krauzlis, R.J.; Goffart, L.; Hafed, Z.M. Neuronal control of fixation and fixational eye movements. Philos. Trans. R. Soc. B Biol. Sci. 2017, 372, 20160205. [Google Scholar]
- Barbieri, F.A.; Polastri, P.F.; Barela, J.A.; Bonnet, C.T.; Brito, M.B.; Rodrigues, S.T. People with Parkinson’s disease are able to couple eye movements and postural sway to improve stability. Biomechanics 2024, 4, 460–472. [Google Scholar] [CrossRef]
- Marx, S.; Respondek, G.; Stamelou, M.; Dowiasch, S.; Stoll, J.; Bremmer, F.; Oertel, W.H.; Höglinger, G.U.; Einhäuser, W. Validation of mobile eye-tracking as novel and efficient means for differentiating progressive supranuclear palsy from Parkinson’s disease. Front. Behav. Neurosci. 2012, 6, 88. [Google Scholar]
- Swart, E.K.; Sikkema-de Jong, M.T. The effects of increased dopamine levels on attentional control during reading and reading comprehension. Curr. Psychol. 2023, 42, 11009–11025. [Google Scholar]
- Tanabe, J.; Tregellas, J.; Miller, D.; Ross, R.G.; Freedman, R. Brain activation during smooth-pursuit eye movements. Neuroimage 2002, 17, 1315–1324. [Google Scholar]
- Reilly, J.L.; Lencer, R.; Bishop, J.R.; Keedy, S.; Sweeney, J.A. Pharmacological treatment effects on eye movement control. Brain Cogn. 2008, 68, 415–435. [Google Scholar]
- Caroline, Y.Y.; Lee, T.; Shariati, M.A.; Santini, V.; Poston, K.; Liao, Y.J. Abnormal eye movement behavior during reading in Parkinson’s disease. Parkinsonism Relat. Disord. 2016, 32, 130–132. [Google Scholar]
- Fasano, A.; Mazzoni, A.; Falotico, E. Reaching and grasping movements in Parkinson’s disease: A review. J. Park. Dis. 2022, 12, 1083–1113. [Google Scholar]
- Kahya, M.; Lyons, K.E.; Pahwa, R.; Akinwuntan, A.E.; He, J.; Devos, H. Pupillary response to postural demand in Parkinson’s disease. Front. Bioeng. Biotechnol. 2021, 9, 617028. [Google Scholar]
- Wang, C.A.; Munoz, D.P. A circuit for pupil orienting responses: Implications for cognitive modulation of pupil size. Curr. Opin. Neurobiol. 2015, 33, 134–140. [Google Scholar]
- Tabashum, T.; Zaffer, A.; Yousefzai, R.; Colletta, K.; Jost, M.B.; Park, Y.; Chawla, J.; Gaynes, B.; Albert, M.V.; Xiao, T. Detection of Parkinson’s disease through automated pupil tracking of the post-illumination pupillary response. Front. Med. 2021, 8, 645293. [Google Scholar]
- Smith, C.; Malek, N.; Grosset, K.; Cullen, B.; Gentleman, S.; Grosset, D.G. Neuropathology of dementia in patients with Parkinson’s disease: A systematic review of autopsy studies. J. Neurol. Neurosurg. Psychiatry 2019, 90, 1234–1243. [Google Scholar] [CrossRef] [PubMed]
- Bredemeyer, O.; Huxley, J.; Antoniades, C.A. Oculomotor deficits in Parkinson’s disease: Increasing sensitivity using multivariate approaches. Front. Digit. Health 2022, 4, 939677. [Google Scholar] [CrossRef] [PubMed]
- Mei, J.; Desrosiers, C.; Frasnelli, J. Machine learning for the diagnosis of Parkinson’s disease: A review of literature. Front. Aging Neurosci. 2021, 13, 633752. [Google Scholar] [CrossRef] [PubMed]
- Przybyszewski, A.W.; Śledzianowski, A.; Chudzik, A.; Szlufik, S.; Koziorowski, D. Machine learning and eye movements give insights into neurodegenerative disease mechanisms. Sensors 2023, 23, 2145. [Google Scholar] [CrossRef]
- Wu, P.; Cao, B.; Liang, Z.; Wu, M. The advantages of artificial intelligence-based gait assessment in detecting, predicting, and managing Parkinson’s disease. Front. Aging Neurosci. 2023, 15, 11913. [Google Scholar] [CrossRef]
- Abdollahi, S.; Safa, R. Machine learning and AI for advancing Parkinson’s disease diagnosis: Exploring promising applications. Big Data Comput. Vis. 2024, 4, 12–21. [Google Scholar]
- Godoy Junior, C.A.; Miele, F.; Mäkitie, L.; Fiorenzato, E.; Koivu, M.; Bakker, L.J.; Groot, C.U.; Redekop, W.K.; van Deen, W.K. Attitudes Toward the Adoption of Remote Patient Monitoring and Artificial Intelligence in Parkinson’s Disease Management: Perspectives of Patients and Neurologists. Patient Cent. Outcomes Res. 2024, 17, 275–285. [Google Scholar] [CrossRef]
- Tsitsi, P. Studies on Eye Movements in Parkinson’s Disease. Doctoral Thesis, Karolinska Institutet, Stockholm, Sweden, 2022. Available online: https://hdl.handle.net/10616/48040 (accessed on 4 January 2025).
- Luke, S.G.; Darowski, E.S.; Gale, S.D. Predicting eye-movement characteristics across multiple tasks from working memory and executive control. Mem. Cognit. 2018, 46, 826–839. [Google Scholar] [CrossRef]
- Lavermicocca, V. New Applications of Neurofeedback Techniques for Cognitive Rehabilitation in Parkinson’s Disease. Ph.D. Thesis, Università degli Studi di Trieste, Trieste, Italy, 2015. Available online: http://hdl.handle.net/10077/11018 (accessed on 7 January 2025).
- Gavelin, H.M.; Domellöf, M.E.; Leung, I.; Neely, A.S.; Launder, N.H.; Nategh, L.; Finke, C.; Lampit, A. Computerized cognitive training in Parkinson’s disease: A systematic review and meta-analysis. Ageing Res. Rev. 2022, 80, 101671. [Google Scholar] [CrossRef]
- Jehangir, N.; Yu, C.Y.; Song, J.; Shariati, M.A.; Binder, S.; Beyer, J.; Santini, V.; Poston, K.; Liao, Y.J. Slower saccadic reading in Parkinson’s disease. PLoS ONE 2018, 13, e0191005. [Google Scholar] [CrossRef]
- Stock, L.; Krüger-Zechlin, C.; Deeb, Z.; Timmermann, L.; Waldthaler, J. Natural reading in Parkinson’s disease with and without mild cognitive impairment. Front. Aging Neurosci. 2020, 12, 120. [Google Scholar]
- Ekker, M.S.; Janssen, S.; Seppi, K.; Poewe, W.; de Vries, N.M.; Theelen, T.; Nonnekes, J.; Bloem, B.R. Ocular and visual disorders in Parkinson’s disease: Common but frequently overlooked. Parkinsonism Relat. Disord. 2017, 40, 1–10. [Google Scholar] [PubMed]
- Abasi, A.; Hoseinabadi, R.; Raji, P.; Friedman, J.H.; Hadian, M.R. Evaluating Oculomotor Tests before and after Vestibular Rehabilitation in Patients with Parkinson’s Disease: A Pilot Pre-Post Study. Park. Dis. 2022, 2022, 6913691. [Google Scholar]
- Kelton, C.; Wei, Z.; Ahn, S.; Balasubramanian, A.; Das, S.R.; Samaras, D.; Zelinsky, G. Reading Detection in Real-Time. In Proceedings of the 11th ACM Symposium on Eye Tracking Research & Applications, New York, NY, USA, 25–28 June 2019; pp. 1–5. [Google Scholar]
- Tosti, B.; Corrado, S.; Mancone, S.; Di Libero, T.; Rodio, A.; Andrade, A.; Diotaiuti, P. Integrated use of biofeedback and neurofeedback techniques in treating pathological conditions and improving performance: A narrative review. Front. Neurosci. 2024, 18, 1358481. [Google Scholar]
- D'Ermo, A.; Di Libero, T.; Langiano, E.; Tosti, B.; Corrado, S.; Diotaiuti, P.; Rodio, A. Exergames in neurocognitive disease management in elderly: A narrative review of therapeutic benefits and applications. J. Gerontol. Geriatr. 2024, 72, 204–214. [Google Scholar]
- Di Libero, T.; Langiano, E.; Carissimo, C.; Ferrara, M.; Diotaiuti, P.; Rodio, A. Technological support for people with Parkinson’s disease: A narrative review. J. Gerontol. Geriatr. 2023, 87–101. [Google Scholar] [CrossRef]
- Di Libero, T.; Carissimo, C.; Guerra, F.; Zagaglia, A.; Diotaiuti, P.; Langiano, E. On the benefits of wearable devices for Parkinson’s disease. Clin. Ter. 2022, 173, 50–53. [Google Scholar]
- da Cruz, W.M.; D’Oliveira, A.; Dominski, F.H.; Diotaiuti, P.; Andrade, A. Mental health of older people in social isolation: The role of physical activity at home during the COVID-19 pandemic. Sport Sci. Health 2022, 18, 597–602. [Google Scholar] [CrossRef]
- Tsitsi, P.; Nilsson, M.; Seimyr, G.Ö.; Larsson, O.; Svenningsson, P.; Markaki, I. Reading Alterations in Parkinson’s Disease Indicate Worse Cognitive Status. Mov. Disord. Clin. Pract. 2023, 10, 579–585. [Google Scholar]
- Lukos, J.R.; Anholt, R.V.; Carpenter, R.H.; Fisk, J.D.; Fernandez-Ruiz, J.; Scherberger, H.; Santello, M. Parkinson’s disease patients show impaired corrective grasp control and eye–hand coupling when reaching to grasp virtual objects. Neuroscience 2013, 254, 205–221. [Google Scholar] [CrossRef]
- Zhou, M.-X.; Chen, Y.; Fu, H.-C.; Qian, C.; Shen, X.; Li, Z.-Z.; Xu, C.-H. Oculomotor impairments in de novo Parkinson’s disease. Front. Aging Neurosci. 2022, 14, 985679. [Google Scholar]
- Brien, D.C.; Munoz, D.P.; Riek, H.C. Classification and staging of Parkinson’s disease using video-based eye tracking. Parkinsonism Relat. Disord. 2023, 110, 105316. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Diotaiuti, P.; Marotta, G.; Di Siena, F.; Vitiello, S.; Di Prinzio, F.; Rodio, A.; Di Libero, T.; Falese, L.; Mancone, S. Eye Tracking in Parkinson’s Disease: A Review of Oculomotor Markers and Clinical Applications. Brain Sci. 2025, 15, 362. https://doi.org/10.3390/brainsci15040362
Diotaiuti P, Marotta G, Di Siena F, Vitiello S, Di Prinzio F, Rodio A, Di Libero T, Falese L, Mancone S. Eye Tracking in Parkinson’s Disease: A Review of Oculomotor Markers and Clinical Applications. Brain Sciences. 2025; 15(4):362. https://doi.org/10.3390/brainsci15040362
Chicago/Turabian StyleDiotaiuti, Pierluigi, Giulio Marotta, Francesco Di Siena, Salvatore Vitiello, Francesco Di Prinzio, Angelo Rodio, Tommaso Di Libero, Lavinia Falese, and Stefania Mancone. 2025. "Eye Tracking in Parkinson’s Disease: A Review of Oculomotor Markers and Clinical Applications" Brain Sciences 15, no. 4: 362. https://doi.org/10.3390/brainsci15040362
APA StyleDiotaiuti, P., Marotta, G., Di Siena, F., Vitiello, S., Di Prinzio, F., Rodio, A., Di Libero, T., Falese, L., & Mancone, S. (2025). Eye Tracking in Parkinson’s Disease: A Review of Oculomotor Markers and Clinical Applications. Brain Sciences, 15(4), 362. https://doi.org/10.3390/brainsci15040362








