Clinical and Epidemiological Characteristics of Patients with Functional Stroke Mimics: A Case–Control Study from Southern Portugal
Abstract
1. Introduction
2. Materials and Methods
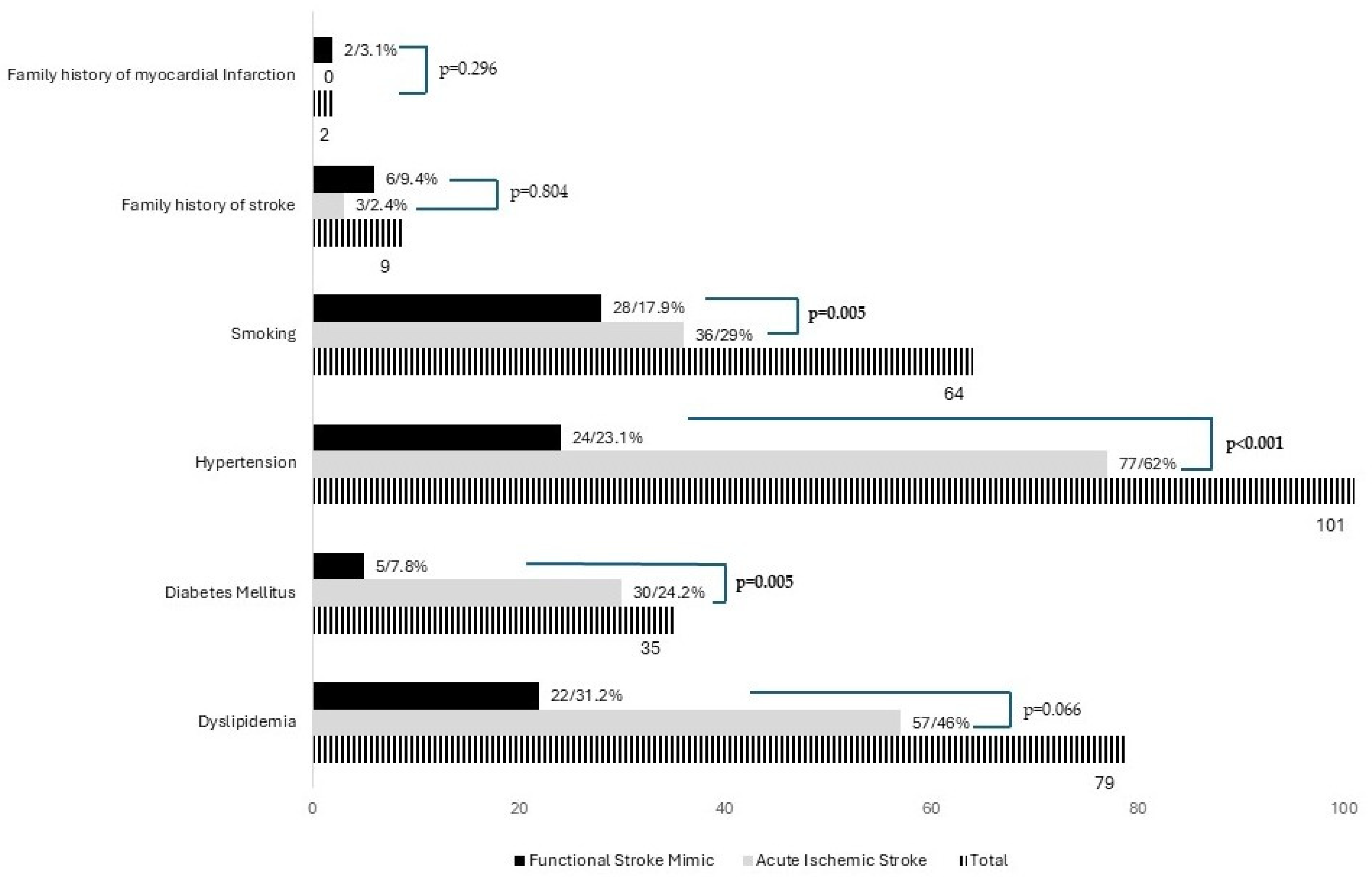
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Finkelstein, S.A.; Cortel-LeBlanc, M.A.; Cortel-LeBlanc, A.; Stone, J. Functional neurological disorder in the emergency department. Acad. Emerg. Med. 2021, 28, 685–696. [Google Scholar] [CrossRef] [PubMed]
- Hallett, M.; Aybek, S.; Dworetzky, B.A.; McWhirter, L.; Staab, J.P.; Stone, J. Functional neurological disorder: New subtypes and shared mechanisms. Lancet Neurol. 2022, 21, 537–550. [Google Scholar] [CrossRef] [PubMed]
- Zinkstok, S.M.; Engelter, S.T.; Gensicke, H.; Lyrer, P.A.; Ringleb, P.A.; Artto, V.; Putaala, J.; Haapaniemi, E.; Tatlisumak, T.; Chen, Y.; et al. Safety of thrombolysis in stroke mimics: Results from a multicenter cohort study. Stroke 2013, 44, 1080–1084. [Google Scholar] [CrossRef] [PubMed]
- Bennett, K.; Diamond, C.; Hoeritzauer, I.; Gardiner, P.; McWhirter, L.; Carson, A.; Stone, J. A practical review of functional neurological disorder (FND) for the general physician. Clin. Med. 2021, 21, 28–36. [Google Scholar] [CrossRef]
- HBuck, B.; Akhtar, N.; Alrohimi, A.; Khan, K.; Shuaib, A. Stroke mimics: Incidence, aetiology, clinical features and treatment. Ann. Med. 2021, 53, 420–436. [Google Scholar] [CrossRef]
- Rochmah, T.N.; Rahmawati, I.T.; Dahlui, M.; Budiarto, W.; Bilqis, N. Economic Burden of Stroke Disease: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 7552. [Google Scholar] [CrossRef] [PubMed]
- Naghavi, M.; Abajobir, A.A.; Abbafati, C.; Abbas, K.M.; Abd-Allah, F.; Abera, S.F.; Aboyans, V.; Adetokunboh, O.; Afshin, A.; Agrawal, A.; et al. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980-2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017, 390, 1151–1210. [Google Scholar] [CrossRef]
- Morotti, A.; Poli, L.; Costa, P. Acute Stroke. Semin. Neurol. 2019, 39, 61–72. [Google Scholar] [CrossRef]
- Boehme, A.K.; Esenwa, C.; Elkind, M.S. Stroke Risk Factors, Genetics, and Prevention. Circ. Res. 2017, 120, 472–495. [Google Scholar] [CrossRef] [PubMed]
- Kuriakose, D.; Xiao, Z. Pathophysiology and Treatment of Stroke: Present Status and Future Perspectives. Int. J. Mol. Sci. 2020, 21, 7609. [Google Scholar] [CrossRef] [PubMed]
- Jones, A.T.; O’Connell, N.K.; David, A.S. Epidemiology of functional stroke mimic patients: A systematic review and meta-analysis. Eur. J. Neurol. 2020, 27, 18–26. [Google Scholar] [CrossRef]
- Popkirov, S.; Stone, J.; Buchan, A.M. Functional Neurological Disorder: A Common and Treatable Stroke Mimic. Stroke 2020, 51, 1629–1635. [Google Scholar] [CrossRef] [PubMed]
- Wilkins, S.S.; Bourke, P.; Salam, A.; Akhtar, N.; D’Souza, A.; Kamran, S.; Bhutta, Z.; Shuaib, A. Functional Stroke Mimics: Incidence and Characteristics at a Primary Stroke Center in the Middle East. Psychosom. Med. 2018, 80, 416–421. [Google Scholar] [CrossRef] [PubMed]
- Caruso, P.; Radin, Y.; Mancinelli, L.; Quagliotto, M.; Lombardo, T.; Pavan, S.; Catalan, M.; Clarici, A.; Bulfon, M.; Benussi, A.; et al. Clinical characteristics and management of functional neurological disorders (FND) mimicking stroke in emergency settings: A functional stroke mimic cases. Front. Neurol. 2024, 15, 1461320. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.S.; Caplan, L.R. Clinical Stroke Syndromes. Front. Neurol. Neurosci. 2016, 40, 72–92. [Google Scholar] [CrossRef] [PubMed]
- Kühne Escolà, J.; Bozkurt, B.; Brune, B.; Chae, W.H.; Milles, L.S.; Pommeranz, D.; Brune, L.; Dammann, P.; Sure, U.; Deuschl, C.; et al. Frequency and Characteristics of Non-Neurological and Neurological Stroke Mimics in the Emergency Department. J. Clin. Med. 2023, 12, 7067. [Google Scholar] [CrossRef]
- Nzwalo, H.; Nogueira, J.; Félix, C.; Guilherme, P.; Baptista, A.; Figueiredo, T.; Ferreira, F.; Marreiros, A.; Thomassen, L.; Logallo, N. Incidence and case-fatality from spontaneous intracerebral hemorrhage in a southern region of Portugal. J. Neurol. Sci. 2017, 380, 74–78. [Google Scholar] [CrossRef] [PubMed]
- Caruso, P.; Bellavita, G.; Furlanis, G.; Ridolfi, M.; Naccarato, M.; Manganotti, P. Functional neurological disorders miming a stroke: Management in the acute phase. Clin. Neurol. Neurosurg. 2020, 196, 105840. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Khunte, M.; Colasurdo, M.; Chaturvedi, S.; Malhotra, A.; Gandhi, D. Mediators of sex-specific differences in rates of stroke mimics among patients treated with intravenous thrombolysis: A nationwide analysis of 174,995 patients. J. Stroke Cerebrovasc. Dis. 2024, 33, 108021. [Google Scholar] [CrossRef] [PubMed]
- Lidstone, S.C.; Costa-Parke, M.; Robinson, E.J.; Ercoli, T.; Stone, J. Functional movement disorder gender, age and phenotype study: A systematic review and individual patient meta-analysis of 4905 cases. J. Neurol. Neurosurg. Psychiatry 2022, 93, 609–616. [Google Scholar] [CrossRef] [PubMed]
- Altemus, M.; Sarvaiya, N.; Neill Epperson, C. Sex differences in anxiety and depression clinical perspectives. Front. Neuroendocrinol. 2014, 35, 320–330. [Google Scholar] [CrossRef] [PubMed]
- Galdas, P.M.; Cheater, F.; Marshall, P. Men and health help-seeking behaviour: Literature review. J. Adv. Nurs. 2005, 49, 616–623. [Google Scholar] [CrossRef] [PubMed]
- Keynejad, R.C.; Frodl, T.; Kanaan, R.; Pariante, C.; Reuber, M.; Nicholson, T.R. Stress and functional neurological disorders: Mechanistic insights. J. Neurol. Neurosurg. Psychiatry 2019, 90, 813–821. [Google Scholar] [CrossRef] [PubMed]
- Pagonabarraga, J.; Álamo, C.; Castellanos, M.; Díaz, S.; Manzano, S. Depression in Major Neurodegenerative Diseases and Strokes: A Critical Review of Similarities and Differences among Neurological Disorders. Brain Sci. 2023, 13, 318. [Google Scholar] [CrossRef] [PubMed]
- Mavroudis, I.; Kazis, D.; Kamal, F.Z.; Gurzu, I.L.; Ciobica, A.; Pădurariu, M.; Novac, B.; Iordache, A. Understanding Functional Neurological Disorder: Recent Insights and Diagnostic Challenges. Int. J. Mol. Sci. 2024, 25, 4470. [Google Scholar] [CrossRef]
- Chora, J.R.; Alves, A.C.; Mariano, C.; Rato, Q.; Antunes, M.; Bourbon, M. Portuguese Lipid Study (e_LIPID). J. Clin. Med. 2024, 13, 6965. [Google Scholar] [CrossRef]
- Botelho, A.; Rios, J.; Fidalgo, A.P.; Ferreira, E.; Nzwalo, H. Organizational Factors Determining Access to Reperfusion Therapies in Ischemic Stroke-Systematic Literature Review. Int. J. Environ. Res. Public Health 2022, 19, 16357. [Google Scholar] [CrossRef] [PubMed]
- Edlow, B.L.; Hurwitz, S.; Edlow, J.A. Diagnosis of DWI-negative acute ischemic stroke: A meta-analysis. Neurology 2017, 89, 256–262. [Google Scholar] [CrossRef]
- Li, Q.; Zhao, L.; Chan, C.L.; Zhang, Y.; Tong, S.W.; Zhang, X.; Ho, J.W.K.; Jiao, Y.; Rainer, T.H. Multi-Level Biomarkers for Early Diagnosis of Ischaemic Stroke: A Systematic Review and Meta-Analysis. Int. J. Mol. Sci. 2023, 24, 13821. [Google Scholar] [CrossRef] [PubMed]

| Characteristics | Total | AIS (n = 124) | FSM (n = 64) | p-Value |
|---|---|---|---|---|
| NIHSS Score | 0.225 | |||
| Minor ≤ 5 | 50 | 32 (25.8%) | 18 (28.1%) | |
| Moderate 5–15 | 43 | 26 (20.9%) | 17 (26.6%) | |
| Severe ≥ 16 | 13 | 10 (8%) | 3 (4.7%) | |
| Motor or sensorial aphasia | 67 | 48 (38.7%) | 19 (29.6%) | 0.294 |
| Transcortical Aphasia | 28 | 26 (20.9%) | 2 (3.1%) | 0.014 |
| Apraxias | 9 | 8 (6.4%) | 1 (1.6%) | 0.080 |
| Vertigo | 15 | 9 (7.2%) | 6 (9.4%) | 0.821 |
| Dysarthria | 62 | 42 (33.9%) | 20 (31.2%) | 0.740 |
| Headache | 38 | 19 (15.3%) | 19 (29.7%) | 0.078 |
| Gait abnormality | 52 | 42 (33.9%) | 10 (15.6%) | 0.004 |
| Hemiparesis | 183 | 122 (98.4%) | 61 (95.3%) | 0.306 |
| Hemianopsia | 31 | 22 (17.7%) | 9 (5.7%) | 0.420 |
| Cranial nerve abnormalities | 74 | 54 (43.5%) | 20 (31.2%) | 0.042 |
| Hemihypoesthesia | 139 | 85 (67.7%) | 54 (84.4%) | 0.066 |
| Characteristics | Total (n = 188) | AIS (n = 124) | FSM (n = 64) | p-Value |
|---|---|---|---|---|
| Prior history of psychiatric disease | ||||
| Generalized Anxiety Disorder | 14 | 4 (3.2%) | 10 (15.6%) | 0.005 |
| Major Depressive Disorder | 21 | 8 (6.4%) | 13 (20.3%) | 0.01 |
| Post-traumatic stress disorder | 2 | 2 (1.6%) | 0 (0.0%) | 0.28 |
| Panic Disorder | 3 | 2 (1.6%) | 1 (1.6%) | 0.91 |
| Bipolar Disorder | 1 | 0 (0.0%) | 1 (1.6%) | 0.19 |
| Prior to event use of drugs | ||||
| Antidepressants | 25 | 14 (11.3%) | 11 (17.2%) | 0.230 |
| Previous use of antithrombotics | 22 | 20 (16.1%) | 2 (3.1%) | 0.007 |
| Oral contraceptive medication | 5 | 1 (0.8%) | 4 (6.2%) | 0.025 |
| Antihypertensive drugs | 93 | 73 (58.9%) | 20 (31.2%) | <0.001 |
| Illicit drugs | 5 | 3 (2.4%) | 2 (3.1%) | 0.817 |
| Characteristics | Total (n = 188) | AIS (n = 124) | FSM (n = 64) | p-Value |
|---|---|---|---|---|
| HDL | 125 | 85 (68.5%) | 40 (62.5%) | 0.515 |
| Normal (≥60 mg/dL) | 20 | 13 (10.5%) | 7 (10.9%) | |
| Moderate Risk (40–59 mg/dL) | 40 | 30 (24.1%) | 10 (15.6%) | |
| High Risk (Men: <40 mg/dL: Women: <50 mg/dL) | 65 | 42 (33.9%) | 23 (35.9%) | |
| LDL | 153 | 102 (82.3%) | 51 (79.7%) | 0.969 |
| Normal (<100 mg/dL) | 62 | 42 (33.9%) | 20 (31.2) | |
| Moderate Risk (100–159 mg/dL) | 64 | 42 (33.9%) | 22 (34.3%) | |
| High Risk (>159 mg/dL) | 27 | 18 (14.5%) | 9 (14%) | |
| Total Cholesterol | 155 | 104 (67.1%) | 51 (79.7%) | 0.450 |
| Normal (<200 mg/dL) | 106 | 70 (83.9%) | 36 (56.2%) | |
| Moderate Risk (200–239 mg/dL) | 26 | 20 (16.1%) | 6 (9.4%) | |
| High Risk (≥240 mg/dL) | 23 | 14 (11.3%) | 9 (14%) | |
| Blood Glucose (Median mg/dL, IQR) b | 111.0 (41.0) | 114 (91.9) | 102 (30.0) | 0.216 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Domingos, M.; Silva, V.H.; Schuh, S.; Correia, H.; Palma, P.; Pedro, J.P.; Nova, B.V.; Marreiros, A.; Félix, A.C.; Nzwalo, H. Clinical and Epidemiological Characteristics of Patients with Functional Stroke Mimics: A Case–Control Study from Southern Portugal. Brain Sci. 2025, 15, 163. https://doi.org/10.3390/brainsci15020163
Domingos M, Silva VH, Schuh S, Correia H, Palma P, Pedro JP, Nova BV, Marreiros A, Félix AC, Nzwalo H. Clinical and Epidemiological Characteristics of Patients with Functional Stroke Mimics: A Case–Control Study from Southern Portugal. Brain Sciences. 2025; 15(2):163. https://doi.org/10.3390/brainsci15020163
Chicago/Turabian StyleDomingos, Miguel, Vítor Hugo Silva, Sara Schuh, Helena Correia, Pedro Palma, João Pedroso Pedro, Bruno Vila Nova, Ana Marreiros, Ana Catarina Félix, and Hipólito Nzwalo. 2025. "Clinical and Epidemiological Characteristics of Patients with Functional Stroke Mimics: A Case–Control Study from Southern Portugal" Brain Sciences 15, no. 2: 163. https://doi.org/10.3390/brainsci15020163
APA StyleDomingos, M., Silva, V. H., Schuh, S., Correia, H., Palma, P., Pedro, J. P., Nova, B. V., Marreiros, A., Félix, A. C., & Nzwalo, H. (2025). Clinical and Epidemiological Characteristics of Patients with Functional Stroke Mimics: A Case–Control Study from Southern Portugal. Brain Sciences, 15(2), 163. https://doi.org/10.3390/brainsci15020163








