Context Is Medicine: Integrating the Exposome into Neurorehabilitation
Abstract
1. Introduction
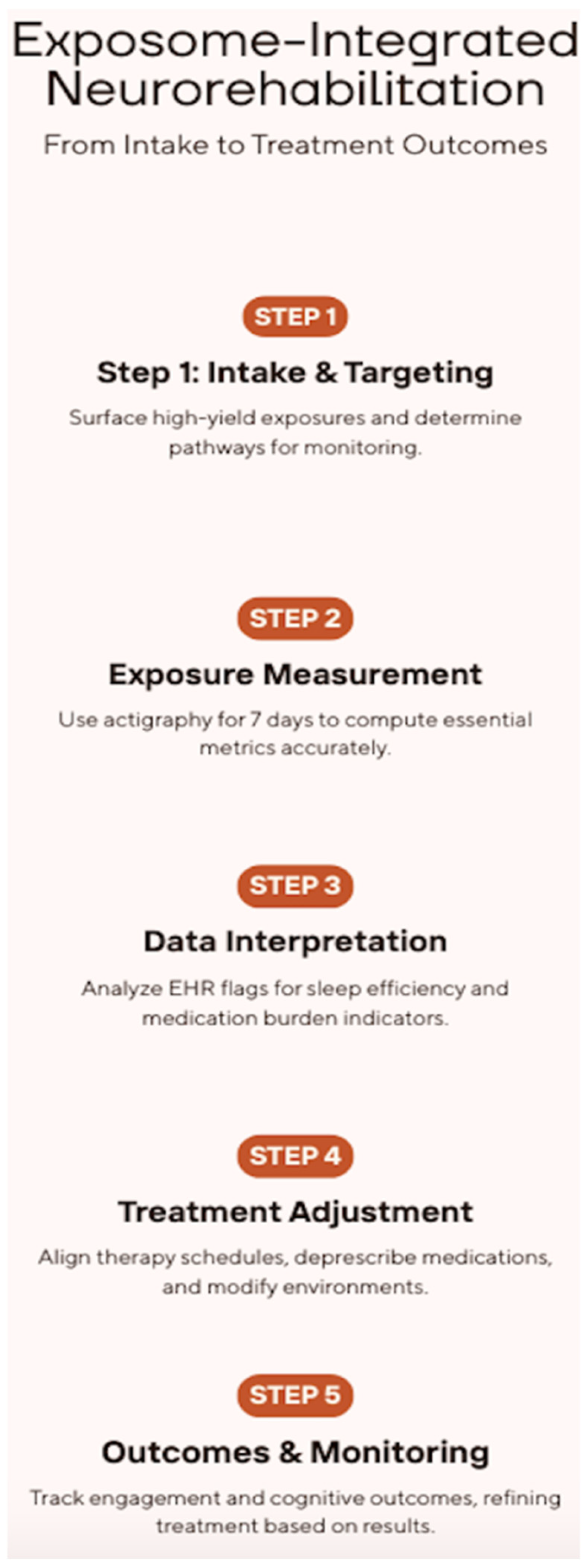
2. Exposome-Informed Neurorehabilitation: Concept, Clinical Levers, and Implementation
2.1. From Concept to Clinic: A Pragmatic Exposome for Neurorehabilitation
2.2. Actionable Exemplars: Sleep–Circadian Alignment and Anticholinergic Burden
2.3. Measurement-to-Action, Service Design, and an Evaluative Agenda
3. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wild, C.P. Complementing the genome with an “exposome”: The outstanding challenge of environmental exposure measurement in molecular epidemiology. Cancer Epidemiol. Biomark. Prev. 2005, 14, 1847–1850. [Google Scholar] [CrossRef] [PubMed]
- Wild, C.P. The exposome: From concept to utility. Int. J. Epidemiol. 2012, 41, 24–32. [Google Scholar] [CrossRef] [PubMed]
- Rappaport, S.M. Implications of the exposome for exposure science. J. Expo. Sci. Environ. Epidemiol. 2011, 21, 5–9. [Google Scholar] [CrossRef] [PubMed]
- Vermeulen, R.; Schymanski, E.L.; Barabási, A.-L.; Miller, G.W. The exposome and health: Where chemistry meets biology. Science 2020, 367, 392–396. [Google Scholar] [CrossRef]
- Tononi, G.; Cirelli, C. Sleep and the price of plasticity: From synaptic and cellular homeostasis to memory consolidation and integration. Neuron 2014, 81, 12–34. [Google Scholar] [CrossRef]
- Morgenthaler, T.; Alessi, C.; Friedman, L.; Owens, J.; Kapur, V.; Boehlecke, B.; Brown, T.; Chesson, A., Jr.; Coleman, J.; Lee-Chiong, T.; et al. Practice parameters for the use of actigraphy in the assessment of sleep and sleep disorders: An update for 2007. Sleep 2007, 30, 519–529. [Google Scholar] [CrossRef]
- Smith, M.T.; McCrae, C.S.; Cheung, J.; Martin, J.L.; Harrod, C.G.; Heald, J.L.; Carden, K.A. Use of Actigraphy for the Evaluation of Sleep Disorders and Circadian Rhythm Sleep-Wake Disorders: An American Academy of Sleep Medicine Systematic Review, Meta-Analysis, and GRADE Assessment. J. Clin. Sleep Med. 2018, 14, 1209–1230. [Google Scholar] [CrossRef]
- Dallere, S.; Rasà, D.M.; Pavarino, G.; Schellino, R.; Vercelli, A.; Boido, M. The exposome from neurodevelopment to neurodegeneration: A narrative review. Neurosci. Biobehav. Rev. 2025, 176, 106247. [Google Scholar] [CrossRef]
- Sakowski, S.A.; Koubek, E.J.; Chen, K.S.; Goutman, S.A.; Feldman, E.L. Role of the Exposome in Neurodegenerative Disease: Recent Insights and Future Directions. Ann. Neurol. 2024, 95, 635–652. [Google Scholar] [CrossRef]
- Li, J.; Somers, V.K.; Lopez-Jimenez, F.; Di, J.; Covassin, N. Demographic characteristics associated with circadian rest-activity rhythm patterns: A cross-sectional study. Int. J. Behav. Nutr. Phys. Act. 2021, 18, 107. [Google Scholar] [CrossRef]
- Lutz, N.D.; Harkotte, M.; Born, J. Sleep’s contribution to memory formation. Physiol. Rev. 2026, 106, 363–483. [Google Scholar] [CrossRef] [PubMed]
- Lyons, L.C.; Vanrobaeys, Y.; Abel, T. Sleep and memory: The impact of sleep deprivation on transcription, translational control, and protein synthesis in the brain. J. Neurochem. 2023, 166, 24–46. [Google Scholar] [CrossRef] [PubMed]
- Kunnath, A.J.; Gifford, R.H.; Wallace, M.T. Cholinergic modulation of sensory perception and plasticity. Neurosci. Biobehav. Rev. 2023, 152, 105323. [Google Scholar] [CrossRef] [PubMed]
- Reallon, E.; Gervais, F.; Moutet, C.; Dauphinot, V.; Desnavailles, P.; Novais, T.; Krolak-Salmon, P.; Garnier-Crussard, A.; Mouchoux, C.; MEMORA Group. Impact of cumulative exposure to anticholinergic and sedative drugs on cognition in older adults: A memory clinic cohort study. Alzheimer’s Res. Ther. 2024, 16, 163. [Google Scholar] [CrossRef]
- Coupland, C.A.C.; Hill, T.; Dening, T.; Morriss, R.; Moore, M.; Hippisley-Cox, J. Anticholinergic Drug Exposure and the Risk of Dementia: A Nested Case-Control Study. JAMA Intern. Med. 2019, 179, 1084–1093. [Google Scholar] [CrossRef]
- Reid, K.J. Assessment of Circadian Rhythms. Neurol. Clin. 2019, 37, 505–526. [Google Scholar] [CrossRef]
- Khatiwada, P.; Yang, B.; Lin, J.C.; Blobel, B. Patient-Generated Health Data (PGHD): Understanding, Requirements, Challenges, and Existing Techniques for Data Security and Privacy. J. Pers. Med. 2024, 14, 282. [Google Scholar] [CrossRef]
- Lau, S.C.L.; Connor, L.T.; Skidmore, E.R. Associations of Circadian Rest-Activity Rhythms with Affect and Cognition in Community-Dwelling Stroke Survivors: An Ambulatory Assessment Study. Neurorehabilit. Neural Repair 2024, 38, 197–206. [Google Scholar] [CrossRef]
- Ruxton, K.; Woodman, R.J.; Mangoni, A.A. Drugs with anticholinergic effects and cognitive impairment, falls and all-cause mortality in older adults: A systematic review and meta-analysis. Br. J. Clin. Pharmacol. 2015, 80, 209–220. [Google Scholar] [CrossRef]
- Chen, M.; Tan, X.; Padman, R. Social determinants of health in electronic health records and their impact on analysis and risk prediction: A systematic review. J. Am. Med. Inform. Assoc. 2020, 27, 1764–1773. [Google Scholar] [CrossRef]
- Lutz, N.D.; Martínez-Albert, E.; Friedrich, H.; Born, J.; Besedovsky, L. Sleep shapes the associative structure underlying pattern completion in multielement event memory. Proc. Natl. Acad. Sci. USA 2024, 121, e2314423121. [Google Scholar] [CrossRef]
- Thiel, C.M.; Friston, K.J.; Dolan, R.J. Cholinergic modulation of experience-dependent plasticity in human auditory cortex. Neuron 2002, 35, 567–574. [Google Scholar] [CrossRef] [PubMed]
- Shi, Q.; Warren, L.; Saposnik, G.; Macdermid, J.C. Confusion assessment method: A systematic review and meta-analysis of diagnostic accuracy. Neuropsychiatr. Dis. Treat. 2013, 9, 1359–1370. [Google Scholar] [CrossRef] [PubMed]
- Tieges, Z.; Maclullich, A.M.J.; Anand, A.; Brookes, C.; Cassarino, M.; O’Connor, M.; Ryan, D.; Saller, T.; Arora, R.C.; Chang, Y.; et al. Diagnostic accuracy of the 4AT for delirium detection in older adults: Systematic review and meta-analysis. Age Ageing 2021, 50, 733–743. [Google Scholar] [CrossRef] [PubMed]
- Morse, A.M.; Bender, E. Sleep in Hospitalized Patients. Clocks Sleep 2019, 1, 151–165. [Google Scholar] [CrossRef]
- Salahudeen, M.S.; Duffull, S.B.; Nishtala, P.S. Anticholinergic burden quantified by anticholinergic risk scales and adverse outcomes in older people: A systematic review. BMC Geriatr. 2015, 15, 31. [Google Scholar] [CrossRef]
- Stewart, C.; Taylor-Rowan, M.; Soiza, R.L.; Quinn, T.J.; Loke, Y.K.; Myint, P.K. Anticholinergic burden measures and older people’s falls risk: A systematic prognostic review. Ther. Adv. Drug Saf. 2021, 12, 20420986211016645. [Google Scholar] [CrossRef]
- van der Meer, H.G.; Taxis, K.; Teichert, M.; Griens, F.; Pont, L.G.; Wouters, H. Anticholinergic and sedative medication use in older community-dwelling people: A national population study in the Netherlands. Pharmacoepidemiol. Drug Saf. 2019, 28, 315–321. [Google Scholar] [CrossRef]
- Feinstein, J.A.; Feudtner, C.; Kempe, A.; Orth, L.E. Anticholinergic Medications and Parent-Reported Anticholinergic Symptoms in Neurologically Impaired Children. J. Pain. Symptom Manag. 2023, 65, e109–e114. [Google Scholar] [CrossRef]
- Van Someren, E.J. Actigraphic monitoring of movement and rest-activity rhythms in aging, Alzheimer’s disease, and Parkinson’s disease. IEEE Trans. Rehabil. Eng. 1997, 5, 394–398. [Google Scholar] [CrossRef]
- Bellelli, G.; Morandi, A.; Davis, D.H.; Mazzola, P.; Turco, R.; Gentile, S.; Ryan, T.; Cash, H.; Guerini, F.; Torpilliesi, T.; et al. Validation of the 4AT, a new instrument for rapid delirium screening: A study in 234 hospitalised older people. Age Ageing 2014, 43, 496–502. [Google Scholar] [CrossRef]
- Basagni, B.; Malloggi, S.; Polito, C.; Pellicciari, L.; Campagnini, S.; Pancani, S.; Mannini, A.; Gemignani, P.; Salvadori, E.; Marignani, S.; et al. MoCA Domain-Specific Pattern of Cognitive Impairment in Stroke Patients Attending Intensive Inpatient Rehabilitation: A Prospective Study. Behav. Sci. 2024, 14, 42. [Google Scholar] [CrossRef] [PubMed]
- Secchi, A.; Mamayusupova, H.; Sami, S.; Maidment, I.; Coulton, S.; Myint, P.K.; Fox, C. A novel Artificial Intelligence-based tool to assess anticholinergic burden: A survey. Age Ageing 2022, 51, afac196. [Google Scholar] [CrossRef] [PubMed]
- Gray, S.L.; Anderson, M.L.; Dublin, S.; Hanlon, J.T.; Hubbard, R.; Walker, R.; Yu, O.; Crane, P.K.; Larson, E.B. Cumulative use of strong anticholinergics and incident dementia: A prospective cohort study. JAMA Intern. Med. 2015, 175, 401–407. [Google Scholar] [CrossRef] [PubMed]
- Jamsen, K.M.; Gnjidic, D.; Hilmer, S.N.; Ilomäki, J.; Le Couteur, D.G.; Blyth, F.M.; Handelsman, D.J.; Naganathan, V.; Waite, L.M.; Cumming, R.G.; et al. Drug Burden Index and change in cognition over time in community-dwelling older men: The CHAMP study. Ann. Med. 2017, 49, 157–164. [Google Scholar] [CrossRef]
- Nevins, P.; Ryan, M.; Davis-Plourde, K.; Ouyang, Y.; Pereira Macedo, J.A.; Meng, C.; Tong, G.; Wang, X.; Ortiz-Reyes, L.; Caille, A.; et al. Adherence to key recommendations for design and analysis of stepped-wedge cluster randomized trials: A review of trials published 2016–2022. Clin. Trials 2024, 21, 199–210. [Google Scholar] [CrossRef]
- Mitchell, J.A.; Quante, M.; Godbole, S.; James, P.; Hipp, J.A.; Marinac, C.R.; Mariani, S.; Cespedes Feliciano, E.M.; Glanz, K.; Laden, F.; et al. Variation in actigraphy-estimated rest-activity patterns by demographic factors. Chronobiol. Int. 2017, 34, 1042–1056. [Google Scholar] [CrossRef]
- Danilevicz, I.M.; Vidil, S.; Landré, B.; Dugravot, A.; van Hees, V.T.; Sabia, S. Reliable measures of rest-activity rhythm fragmentation: How many days are needed? Eur. Rev. Aging Phys. Act. 2024, 21, 29. [Google Scholar] [CrossRef]
- Ancoli-Israel, S.; Cole, R.; Alessi, C.; Chambers, M.; Moorcroft, W.; Pollak, C.P. The role of actigraphy in the study of sleep and circadian rhythms. Sleep 2003, 26, 342–392. [Google Scholar] [CrossRef]
- Hilmer, S.N.; Mager, D.E.; Simonsick, E.M.; Cao, Y.; Ling, S.M.; Windham, B.G.; Harris, T.B.; Hanlon, J.T.; Rubin, S.M.; Shorr, R.I.; et al. A drug burden index to define the functional burden of medications in older people. Arch. Intern. Med. 2007, 167, 781–787. [Google Scholar] [CrossRef]
- Weng, J.K.; Virk, R.; Kaiser, K.; Hoffman, K.E.; Goodman, C.R.; Mitchell, M.; Shaitelman, S.; Schlembach, P.; Reed, V.; Wu, C.F.; et al. Automated, Real-Time Integration of Biometric Data From Wearable Devices with Electronic Medical Records: A Feasibility Study. JCO Clin. Cancer Inform. 2024, 8, e2400040. [Google Scholar] [CrossRef] [PubMed]
- Schubert, M.; Schürch, R.; Boettger, S.; Garcia Nuñez, D.; Schwarz, U.; Bettex, D.; Jenewein, J.; Bogdanovic, J.; Staehli, M.L.; Spirig, R.; et al. A hospital-wide evaluation of delirium prevalence and outcomes in acute care patients—A cohort study. BMC Health Serv. Res. 2018, 18, 550. [Google Scholar] [CrossRef] [PubMed]
- Thein, M.Z.A.; Pereira, J.V.; Nitchingham, A.; Caplan, G.A. A call to action for delirium research: Meta-analysis and regression of delirium associated mortality. BMC Geriatr. 2020, 20, 325. [Google Scholar] [CrossRef] [PubMed]
- Li, F.; Wang, R. Stepped Wedge Cluster Randomized Trials: A Methodological Overview. World Neurosurg. 2022, 161, 323–330. [Google Scholar] [CrossRef]
- Hemming, K.; Taljaard, M. Reflection on modern methods: When is a stepped-wedge cluster randomized trial a good study design choice? Int. J. Epidemiol. 2020, 49, 1043–1052. [Google Scholar] [CrossRef]
- Keogh, R.H.; Gran, J.M.; Seaman, S.R.; Davies, G.; Vansteelandt, S. Causal inference in survival analysis using longitudinal observational data: Sequential trials and marginal structural models. Stat. Med. 2023, 42, 2191–2225. [Google Scholar] [CrossRef]
- Shinozaki, T.; Suzuki, E. Understanding Marginal Structural Models for Time-Varying Exposures: Pitfalls and Tips. J. Epidemiol. 2020, 30, 377–389. [Google Scholar] [CrossRef]
- Stahl, S.T.; Skidmore, E.; Kringle, E.; Shih, M.; Baum, C.; Hammel, J.; Krafty, R.; Covassin, N.; Li, J.; Smagula, S.F. Rest-Activity Rhythm Characteristics Associated with Depression Symptoms in Stroke Survivors. Arch. Phys. Med. Rehabil. 2023, 104, 1203–1208. [Google Scholar] [CrossRef]
- Liang, H.W.; Wu, C.H.; Lin, C.; Chang, H.C.; Lin, Y.H.; Chen, S.Y.; Hsu, W.C. Rest-Activity Rhythm Differences in Acute Rehabilitation Between Poststroke Patients and Non-Brain Disease Controls: Comparative Study. J. Med. Internet Res. 2024, 26, e49530. [Google Scholar] [CrossRef]
- Prabhu, D.F.; Gurupur, V.; Stone, A.; Trader, E. Integrating Artificial Intelligence, Electronic Health Records, and Wearables for Predictive, Patient-Centered Decision Support in Healthcare. Healthcare 2025, 13, 2753. [Google Scholar] [CrossRef]
- Wallace, D.A.; Johnson, D.A.; Redline, S.; Sofer, T.; Kossowsky, J. Rest-activity rhythms across the lifespan: Cross-sectional findings from the US representative National Health and Nutrition Examination Survey. Sleep 2023, 46, zsad220. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Calabrò, R.S. Context Is Medicine: Integrating the Exposome into Neurorehabilitation. Brain Sci. 2025, 15, 1198. https://doi.org/10.3390/brainsci15111198
Calabrò RS. Context Is Medicine: Integrating the Exposome into Neurorehabilitation. Brain Sciences. 2025; 15(11):1198. https://doi.org/10.3390/brainsci15111198
Chicago/Turabian StyleCalabrò, Rocco Salvatore. 2025. "Context Is Medicine: Integrating the Exposome into Neurorehabilitation" Brain Sciences 15, no. 11: 1198. https://doi.org/10.3390/brainsci15111198
APA StyleCalabrò, R. S. (2025). Context Is Medicine: Integrating the Exposome into Neurorehabilitation. Brain Sciences, 15(11), 1198. https://doi.org/10.3390/brainsci15111198





