Valuable Prognostic Role of Disability, Pain, Anxiety, and Depression Scales in Instrumented Lumbar Spine Surgery for Degenerative Pathology: The SAP-LD Study
Abstract
1. Introduction
2. Methods
2.1. Study Design and Participants
2.2. Data Collection
- 1.
- Oswestry Disability Index (ODI): A condition-specific measure of functional disability related to back pain, consisting of 10 sections scored from 0 to 5, with higher scores indicating greater disability. The Italian validated version was used [16].
- 2.
- 36-Item Short Form Health Survey (SF-36): A generic health-related quality of life measure comprising eight subscales: Physical Functioning, Role-Physical, Bodily Pain, General Health, Vitality, Social Functioning, Role-Emotional, and Mental Health. Scores range from 0 to 100, with higher scores indicating better health status. The Italian validated version was used (A178) [17].
- 3.
- Pain Catastrophizing Scale (PCS): A 13-item questionnaire assessing catastrophic thinking related to pain experiences, with three subscales: rumination, magnification, and helplessness. Scores range from 0 to 52, with higher scores indicating greater catastrophizing [18].
- 4.
- Hospital Anxiety and Depression Scale (HADS): A 14-item scale designed to detect anxiety and depression in patients with physical health problems, with separate subscales for anxiety (HADS-A) and depression (HADS-D). Scores range from 0 to 21 for each subscale, with scores ≥ 8 indicating clinically significant symptoms (Zi19) [19].
- 5.
- Visual Analogue Scale (VAS): A unidimensional measure of pain intensity, consisting of a 10 cm line with endpoints labeled “no pain” (0) and “worst possible pain” (10).
2.3. Surgical Procedure
2.4. Follow-Up and Outcome Assessment
2.5. Statistical Analysis
3. Results
3.1. Demographic and Baseline Characteristics
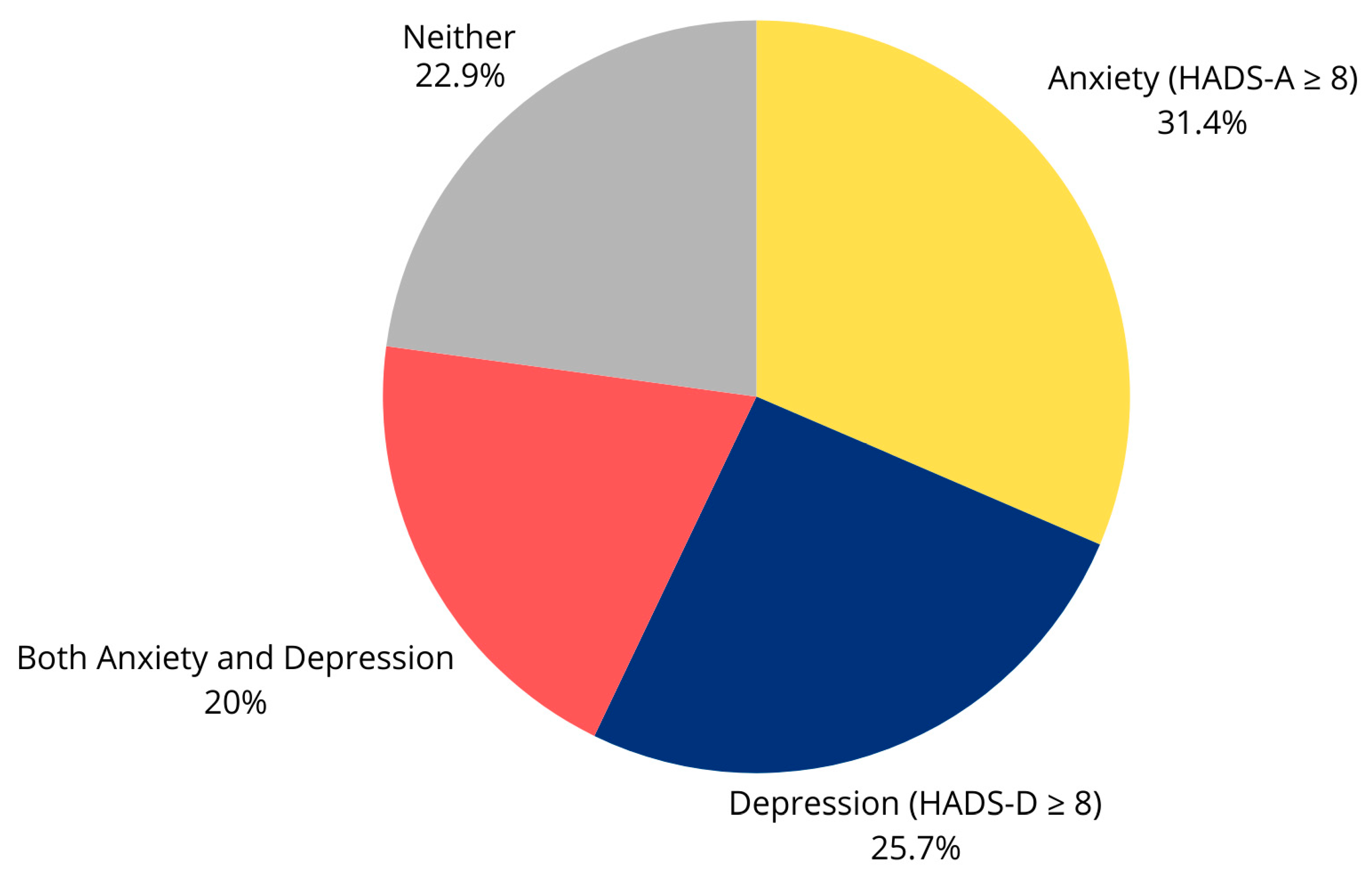
3.2. Preoperative Psychological Assessment
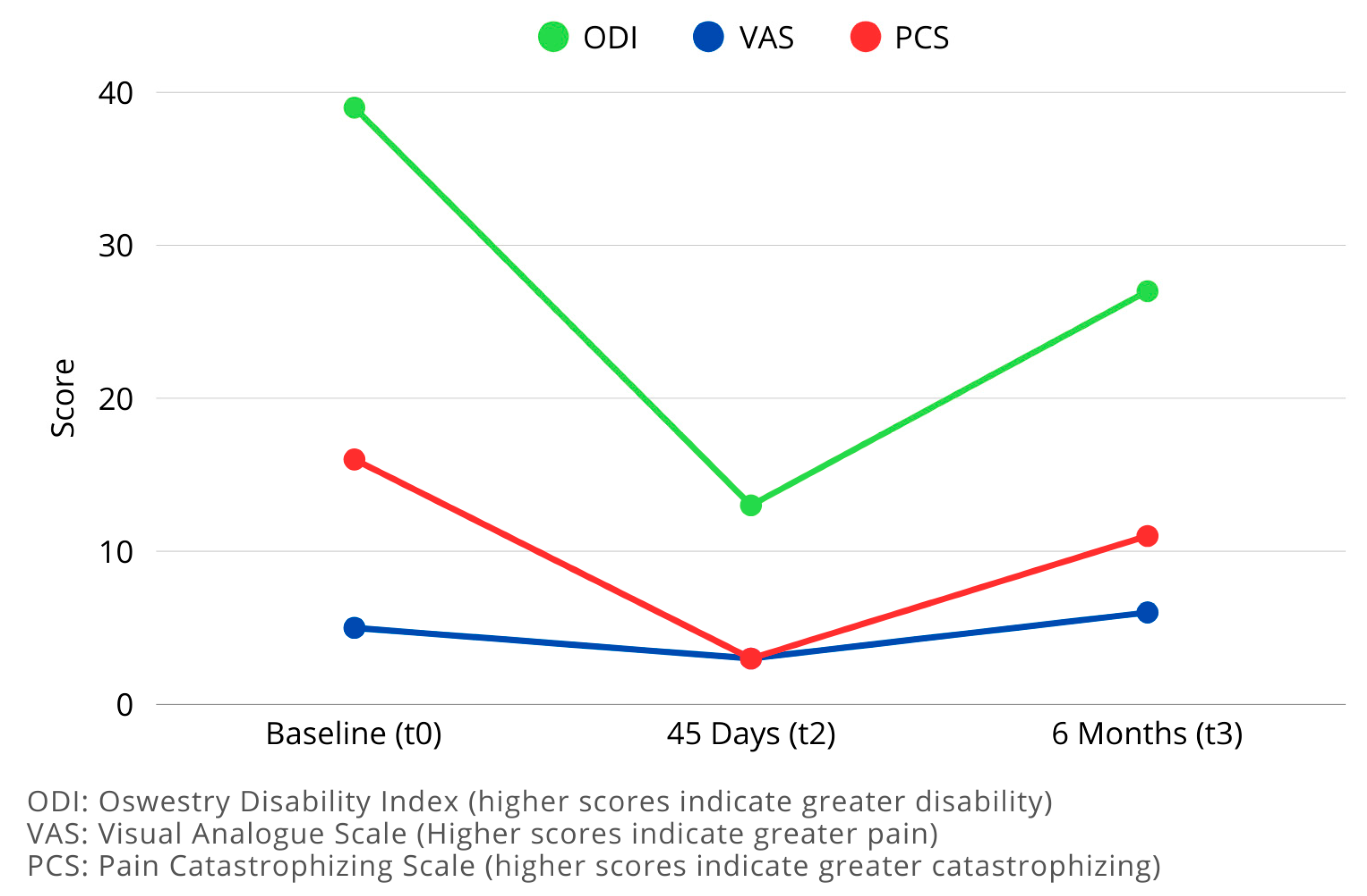
3.3. Longitudinal Changes in Outcome Measures
3.3.1. Disability (ODI)
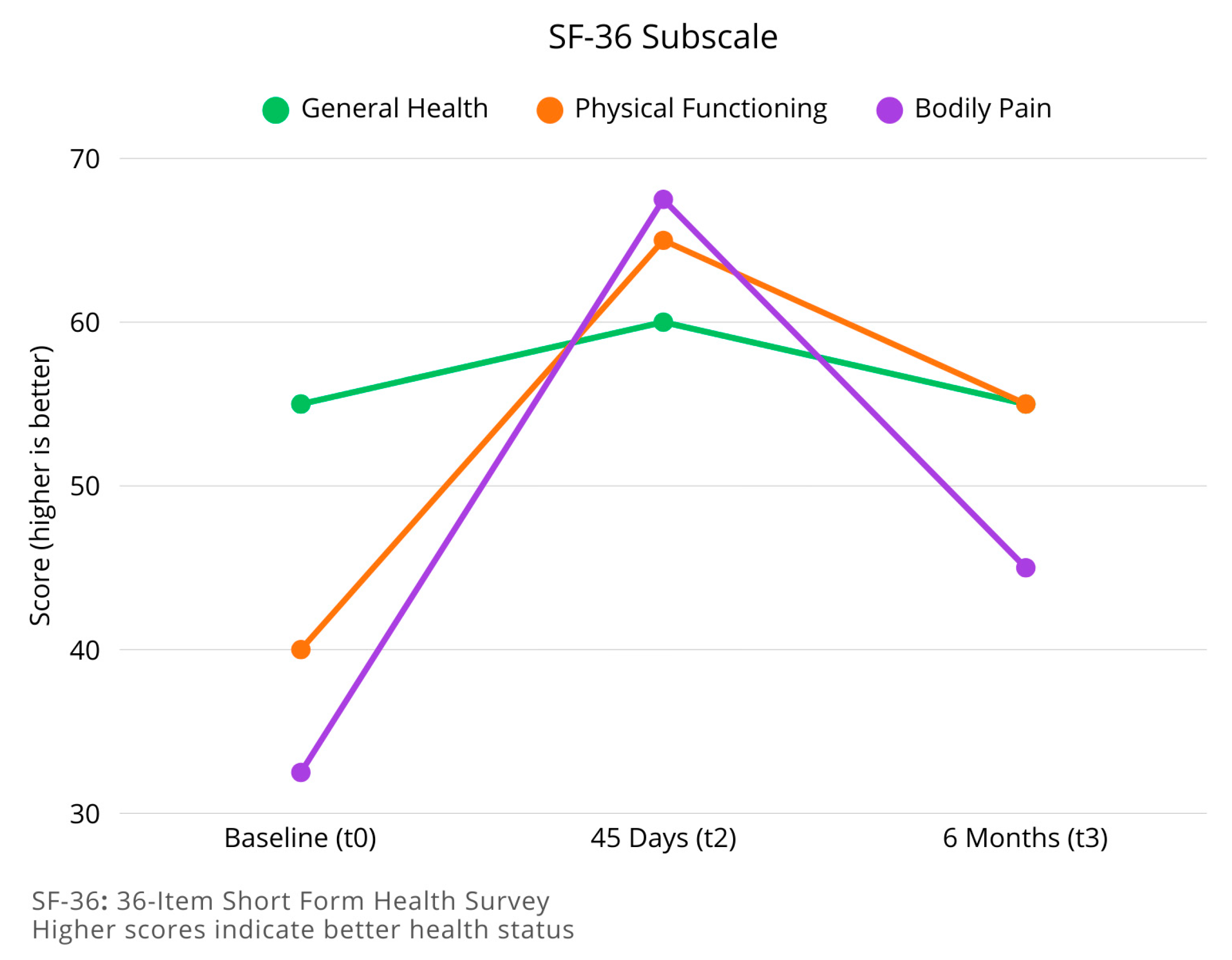
3.3.2. Health-Related Quality of Life (SF-36)
3.3.3. Pain Catastrophizing (PCS)
3.3.4. Pain Intensity (VAS)
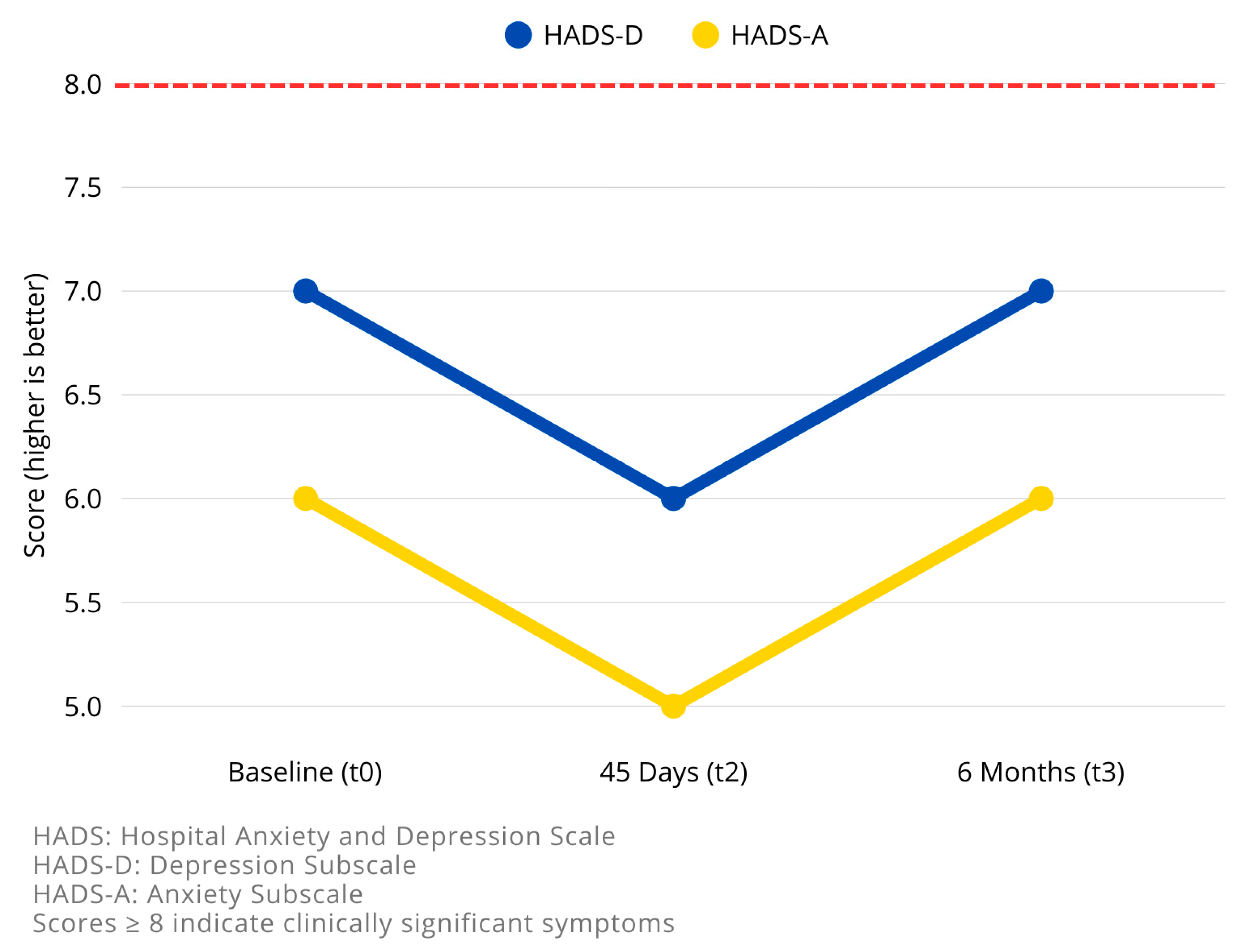
3.3.5. Anxiety and Depression (HADS)
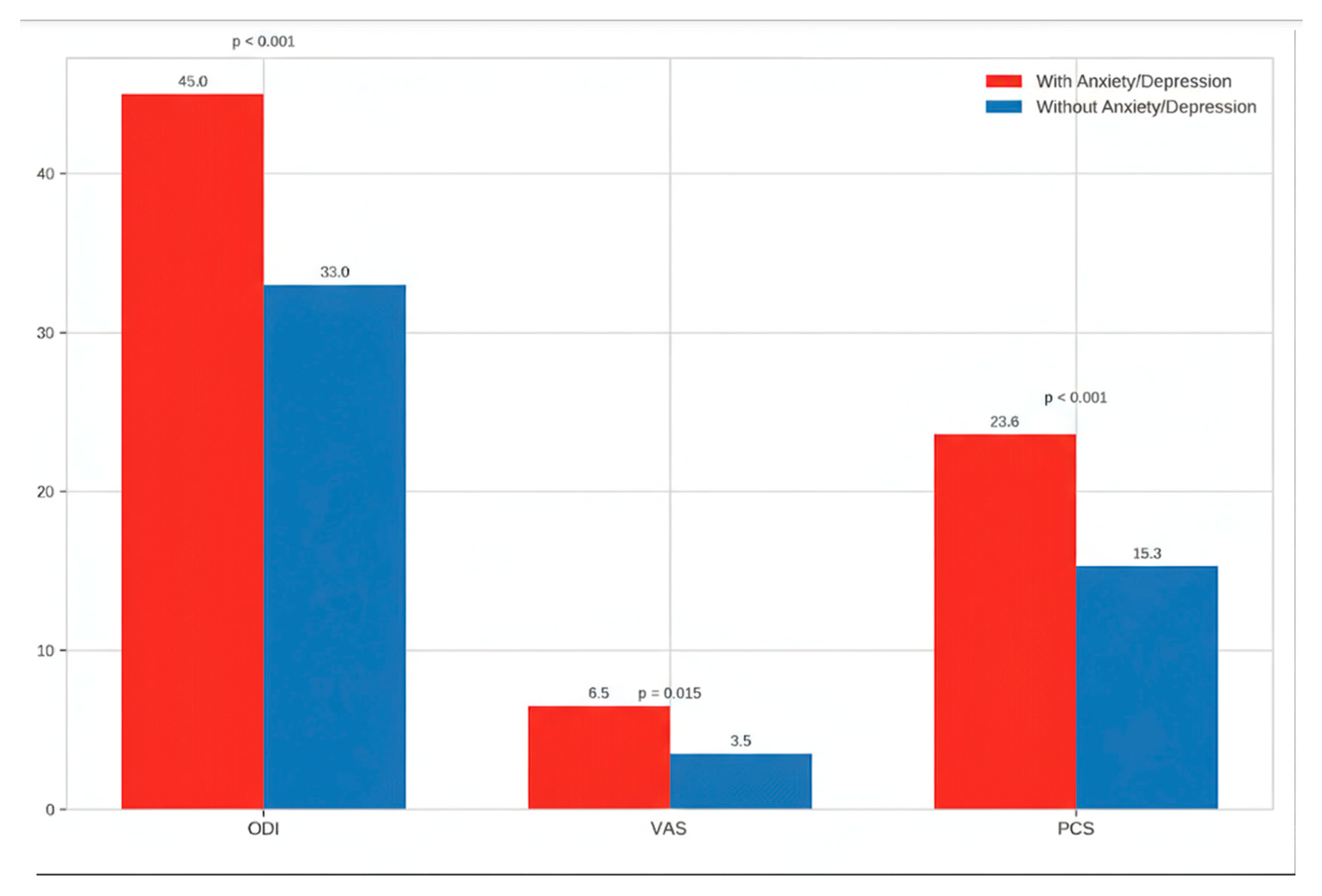
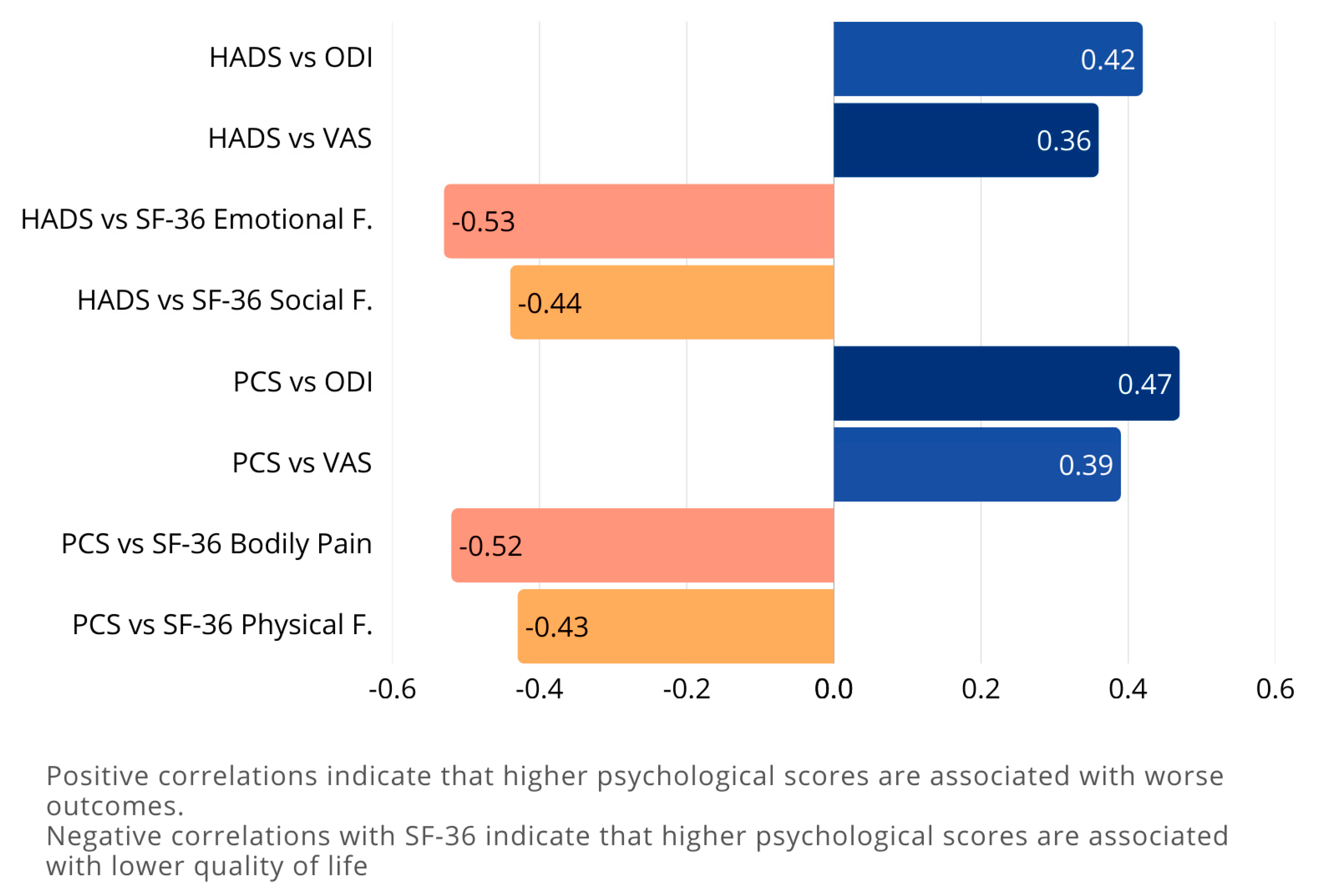
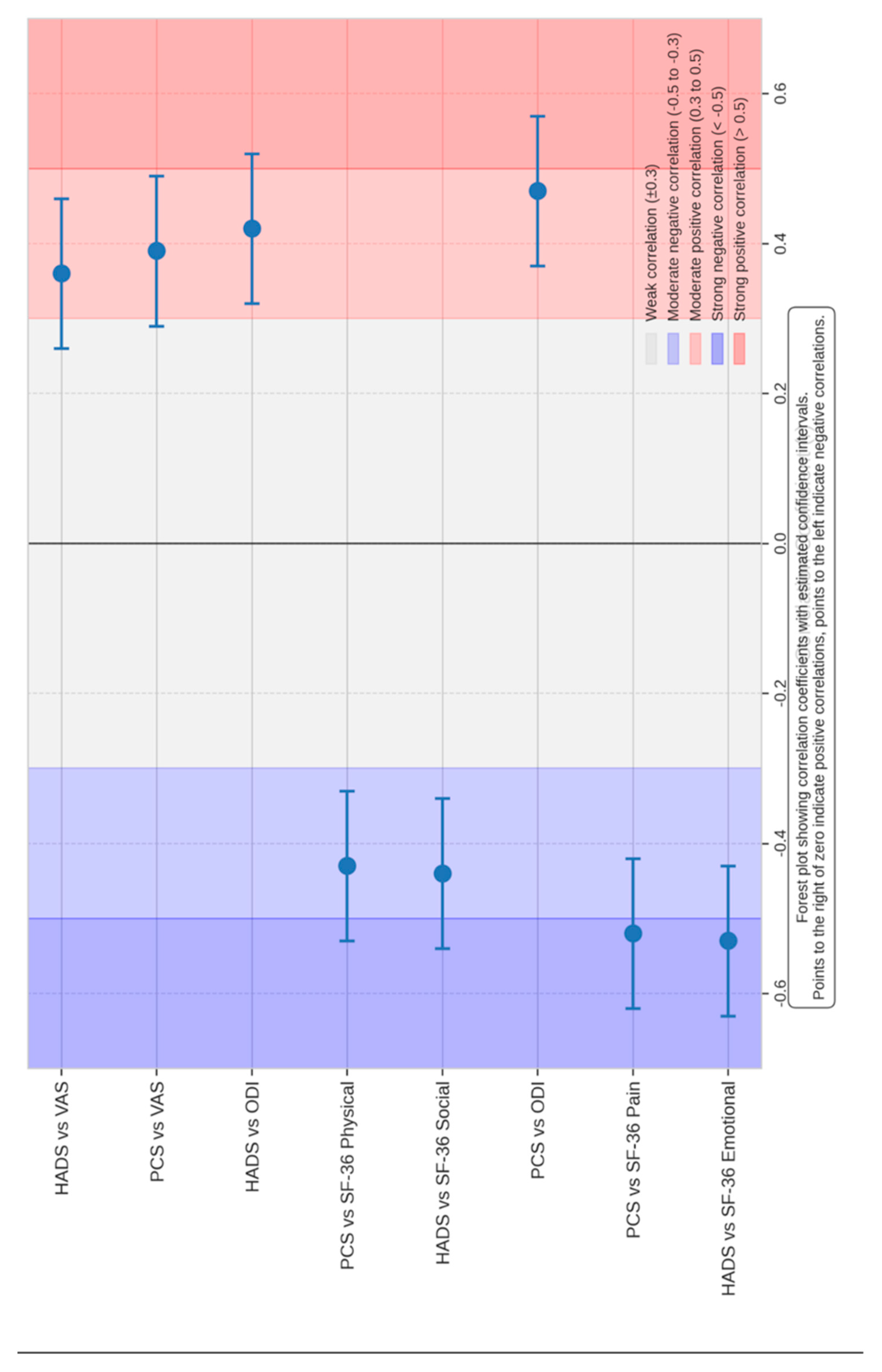
3.4. Correlation Between Psychological Factors and Outcomes
3.4.1. Higher HADS Scores at Baseline Are Associated with:
- Higher ODI scores (increased disability) at all time points (r = 0.42, p = 0.002)
- Higher VAS scores (increased pain) at all time points (r = 0.36, p = 0.015)
- Lower scores on SF-36 subscales, particularly Emotional Well-being (r = −0.53, p = 0.00023) and Social Functioning (r = −0.44, p = 0.002)
3.4.2. Higher PCS Scores at Baseline Are Associated with:
- Higher ODI scores at all time points (r = 0.47, p = 0.001)
- Higher VAS scores at all time points (r = 0.39, p = 0.008)
- Lower scores on SF-36 subscales, particularly Pain (r = −0.52, p = 0.00023) and Physical Functioning (r = −0.43, p = 0.04254)
3.5. Multivariate Analysis
4. Discussion
4.1. Impact of Preoperative Psychological Health
4.2. Efficacy of Surgical Intervention and Postoperative Management
4.3. Prognostic Value of Preoperative Psychological Assessment
4.4. Implications for Clinical Practice and the Multidisciplinary Approach
4.5. Comparison with Recent Literature
4.6. Future Directions and Emerging Concepts
4.7. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ravindra, V.M.; Senglaub, S.S.; Rattani, A.; Dewan, M.C.; Härtl, R.; Bisson, E.; Park, K.B.; Shrime, M.G. Degenerative Lumbar Spine Disease: Estimating Global Incidence and Worldwide Volume. Glob. Spine J 2018, 8, 784–794. [Google Scholar] [CrossRef]
- GBD 2021 Low Back Pain Collaborators. Global, Regional, and National Burden of Low Back Pain, 1990–2020, Its Attributable Risk Factors, and Projections to 2050: A Systematic Analysis of the Global Burden of Disease Study 2021. Lancet Rheumatol 2023, 5, e316–e329. [Google Scholar] [CrossRef] [PubMed]
- Deyo, R.A.; Mirza, S.K.; Martin, B.I.; Kreuter, W.; Goodman, D.C.; Jarvik, J.G. Trends, Major Medical Complications, and Charges Associated with Surgery for Lumbar Spinal Stenosis in Older Adults. JAMA 2010, 303, 1259–1265. [Google Scholar] [CrossRef] [PubMed]
- Katz, J.N.; Zimmerman, Z.E.; Mass, H.; Makhni, M.C. Diagnosis and Management of Lumbar Spinal Stenosis: A Review. JAMA 2022, 327, 1688–1699. [Google Scholar] [CrossRef] [PubMed]
- Mannion, A.F.; Brox, J.I.; Fairbank, J.C.T. Comparison of Spinal Fusion and Nonoperative Treatment in Patients with Chronic Low Back Pain: Long-Term Follow-up of Three Randomized Controlled Trials. Spine J. 2013, 13, 1438–1448. [Google Scholar] [CrossRef]
- Mirza, S.K.; Deyo, R.A. Systematic Review of Randomized Trials Comparing Lumbar Fusion Surgery to Nonoperative Care for Treatment of Chronic Back Pain. Spine 2007, 32, 816–823. [Google Scholar] [CrossRef]
- Adogwa, O.; Parker, S.L.; Shau, D.N.; Mendenhall, S.K.; Aaronson, O.S.; Cheng, J.S.; Devin, C.J.; McGirt, M.J. Preoperative Zung Depression Scale Predicts Outcome after Revision Lumbar Surgery for Adjacent Segment Disease, Recurrent Stenosis, and Pseudarthrosis. Spine J. 2012, 12, 179–185. [Google Scholar] [CrossRef]
- Amaral, V.; Marchi, L.; Martim, H.; Amaral, R.; Nogueira-Neto, J.; Pierro, E.; Oliveira, L.; Coutinho, E.; Marcelino, F.; Faulhaber, N.; et al. Influence of Psychosocial Distress in the Results of Elective Lumbar Spine Surgery. J. Spine Surg. 2017, 3, 371–378. [Google Scholar] [CrossRef]
- Skolasky, R.L.; Wegener, S.T.; Maggard, A.M.; Riley, L.H. The Impact of Reduction of Pain after Lumbar Spine Surgery: The Relationship between Changes in Pain and Physical Function and Disability. Spine 2014, 39, 1426–1432. [Google Scholar] [CrossRef]
- Held, U.; Burgstaller, J.M.; Deforth, M.; Steurer, J.; Pichierri, G.; Wertli, M.M. Association between Depression and Anxiety on Symptom and Function after Surgery for Lumbar Spinal Stenosis. Sci. Rep. 2022, 12, 2821. [Google Scholar] [CrossRef]
- Sullivan, M.J.; Thorn, B.; Haythornthwaite, J.A.; Keefe, F.; Martin, M.; Bradley, L.A.; Lefebvre, J.C. Theoretical Perspectives on the Relation between Catastrophizing and Pain. Clin. J. Pain 2001, 17, 52–64. [Google Scholar] [CrossRef] [PubMed]
- Wertli, M.M.; Rasmussen-Barr, E.; Weiser, S.; Bachmann, L.M.; Brunner, F. The Role of Fear Avoidance Beliefs as a Prognostic Factor for Outcome in Patients with Nonspecific Low Back Pain: A Systematic Review. Spine J. 2014, 14, 816–836.e4. [Google Scholar] [CrossRef] [PubMed]
- Block, A.R.; Gatchel, R.J.; Deardorff, W.W.; Guyer, R.D. The Psychology of Spine Surgery; American Psychological Association: Washington, DC, USA, 2003; ISBN 978-1-55798-997-0. [Google Scholar]
- Faye, E.R.; Ball, J.R.; Mills, E.S.; Wang, J.; Hah, R.J.; Alluri, R.K. The Role of Psychosocial Screening in Patient Selection for Spine Surgery: A Review. Int. J. Spine Surg. 2023, 17, 309–317. [Google Scholar] [CrossRef]
- Archer, K.R.; Devin, C.J.; Vanston, S.W.; Koyama, T.; Phillips, S.E.; Mathis, S.L.; George, S.Z.; McGirt, M.J.; Spengler, D.M.; Aaronson, O.S.; et al. Cognitive-Behavioral-Based Physical Therapy for Patients With Chronic Pain Undergoing Lumbar Spine Surgery: A Randomized Controlled Trial. J. Pain 2016, 17, 76–89. [Google Scholar] [CrossRef] [PubMed]
- Monticone, M.; Baiardi, P.; Ferrari, S.; Foti, C.; Mugnai, R.; Pillastrini, P.; Vanti, C.; Zanoli, G. Development of the Italian Version of the Oswestry Disability Index (ODI-I): A Cross-Cultural Adaptation, Reliability, and Validity Study. Spine 2009, 34, 2090–2095. [Google Scholar] [CrossRef]
- Apolone, G.; Mosconi, P. The Italian SF-36 Health Survey: Translation, Validation and Norming. J. Clin. Epidemiol. 1998, 51, 1025–1036. [Google Scholar] [CrossRef]
- Sullivan, M.J.L.; Bishop, S.R.; Pivik, J. The Pain Catastrophizing Scale: Development and Validation. Psychol. Assess. 1995, 7, 524–532. [Google Scholar] [CrossRef]
- Zigmond, A.S.; Snaith, R.P. The Hospital Anxiety and Depression Scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef]
- Parker, S.L.; Mendenhall, S.K.; Shau, D.N.; Adogwa, O.; Anderson, W.N.; Devin, C.J.; McGirt, M.J. Minimum Clinically Important Difference in Pain, Disability, and Quality of Life after Neural Decompression and Fusion for Same-Level Recurrent Lumbar Stenosis: Understanding Clinical versus Statistical Significance. J. Neurosurg. Spine 2012, 16, 471–478. [Google Scholar] [CrossRef]
- Djurasovic, M.; Glassman, S.D.; Dimar, J.R.; Howard, J.M.; Bratcher, K.R.; Carreon, L.Y. Does Fusion Status Correlate with Patient Outcomes in Lumbar Spinal Fusion? Spine 2011, 36, 404–409. [Google Scholar] [CrossRef] [PubMed]
- Petrucci, G.; Papalia, G.F.; Ambrosio, L.; Russo, F.; Marchetti, A.; De Marinis, M.G.; Vadala, G.; Papalia, R.; Denaro, V. The Influence of Psychological Factors on Postoperative Clinical Outcomes in Patients Undergoing Lumbar Spine Surgery: A Systematic Review and Meta-Analysis. Eur. Spine J. 2025, 34, 1409–1419. [Google Scholar] [CrossRef]
- Wu, R.; Gao, P.; Liu, S.; Yang, Q.; Wang, J.; Liang, F.; Chen, Y.; Yang, L. Anxiety and Depression as Risk Factors for Postoperative Complications and Pain in Lumbar Spine Surgery: A National Database Study. J. Orthop. Surg. 2024, 32, 10225536241280190. [Google Scholar] [CrossRef]
- Namiranian, K.; Norris, E.J.; Jolissaint, J.G.; Patel, J.B.; Lombardi, C.M. Impact of Multidisciplinary Spine Conferences on Surgical Planning and Perioperative Care in Elective Lumbar Spine Surgeries. Asian Spine J. 2018, 12, 854–861. [Google Scholar] [CrossRef]
- Yanamadala, V.; Kim, Y.; Buchlak, Q.D.; Wright, A.K.; Babington, J.; Friedman, A.; Mecklenburg, R.S.; Farrokhi, F.; Leveque, J.-C.; Sethi, R.K. Multidisciplinary Evaluation Leads to the Decreased Utilization of Lumbar Spine Fusion: An Observational Cohort Pilot Study. Spine 2017, 42, E1016–E1023. [Google Scholar] [CrossRef]
- Strøm, J.; Bjerrum, M.B.; Nielsen, C.V.; Thisted, C.N.; Nielsen, T.L.; Laursen, M.; Jørgensen, L.B. Anxiety and Depression in Spine Surgery—A Systematic Integrative Review. Spine J. 2018, 18, 1272–1285. [Google Scholar] [CrossRef]
- Carreon, L.Y.; Jespersen, A.B.; Støttrup, C.C.; Hansen, K.H.; Andersen, M.O. Is the Hospital Anxiety and Depression Scale Associated With Outcomes After Lumbar Spine Surgery? Glob. Spine J. 2020, 10, 266–271. [Google Scholar] [CrossRef] [PubMed]
- Netto, M.B.; Barranco, A.B.S.; deOliveira, K.W.K.; Petronilho, F. Influence of Anxiety and Depression Symptoms on the Quality of Life in Patients Undergoing Lumbar Spine Surgery. Rev. Bras. Ortop. 2018, 53, 38–44. [Google Scholar] [CrossRef]
- Rahman, R.; Ibaseta, A.; Reidler, J.S.; Andrade, N.S.; Skolasky, R.L.; Riley, L.H.; Cohen, D.B.; Sciubba, D.M.; Kebaish, K.M.; Neuman, B.J. Changes in Patients’ Depression and Anxiety Associated with Changes in Patient-Reported Outcomes after Spine Surgery. J. Neurosurg. 2020, 32, 871–890. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, J.P.; Casqueiro, M.; Andrade, J.P.; Reizinho, C. Does Preoperative Physical Therapy/Prehabilitation Affect Outcome or Complications after Surgery for Lumbar Disc Herniation? A Systematic Review. Brain Spine 2025, 5, 104386. [Google Scholar] [CrossRef] [PubMed]
- Parrish, J.M.; Jenkins, N.W.; Parrish, M.S.; Cha, E.D.K.; Lynch, C.P.; Massel, D.H.; Hrynewycz, N.M.; Mohan, S.; Geoghegan, C.E.; Jadczak, C.N.; et al. The Influence of Cognitive Behavioral Therapy on Lumbar Spine Surgery Outcomes: A Systematic Review and Meta-Analysis. Eur. Spine J. 2021, 30, 1365–1379. [Google Scholar] [CrossRef]
- Anheyer, D.; Haller, H.; Barth, J.; Lauche, R.; Dobos, G.; Cramer, H. Mindfulness-Based Stress Reduction for Treating Low Back Pain: A Systematic Review and Meta-Analysis. Ann. Intern. Med. 2017, 166, 799–807. [Google Scholar] [CrossRef] [PubMed]
- Cherkin, D.C.; Sherman, K.J.; Balderson, B.H.; Cook, A.J.; Anderson, M.L.; Hawkes, R.J.; Hansen, K.E.; Turner, J.A. Effect of Mindfulness-Based Stress Reduction vs Cognitive Behavioral Therapy or Usual Care on Back Pain and Functional Limitations in Adults With Chronic Low Back Pain: A Randomized Clinical Trial. JAMA 2016, 315, 1240–1249. [Google Scholar] [CrossRef] [PubMed]
- Hughes, L.S.; Clark, J.; Colclough, J.A.; Dale, E.; McMillan, D. Acceptance and Commitment Therapy (ACT) for Chronic Pain: A Systematic Review and Meta-Analyses. Clin. J. Pain 2017, 33, 552–568. [Google Scholar] [CrossRef] [PubMed]
- Veehof, M.M.; Oskam, M.-J.; Schreurs, K.M.G.; Bohlmeijer, E.T. Acceptance-Based Interventions for the Treatment of Chronic Pain: A Systematic Review and Meta-Analysis. Pain 2011, 152, 533–542. [Google Scholar] [CrossRef]
- Feingold, D.; Brill, S.; Goor-Aryeh, I.; Delayahu, Y.; Lev-Ran, S. Depression and Anxiety among Chronic Pain Patients Receiving Prescription Opioids and Medical Marijuana. J. Affect. Disord. 2017, 218, 1–7. [Google Scholar] [CrossRef]
- Sturgeon, J.A.; Zautra, A.J. Resilience: A New Paradigm for Adaptation to Chronic Pain. Curr. Pain Headache Rep. 2010, 14, 105–112. [Google Scholar] [CrossRef]
- Robinson, A.; Husband, A.K.; Slight, R.D.; Slight, S.P. Digital Technology to Support Lifestyle and Health Behaviour Changes in Surgical Patients: Systematic Review. BJS Open 2021, 5, zraa009. [Google Scholar] [CrossRef]
- Thurnheer, S.E.; Gravestock, I.; Pichierri, G.; Steurer, J.; Burgstaller, J.M. Benefits of Mobile Apps in Pain Management: Systematic Review. JMIR Mhealth Uhealth 2018, 6, e11231. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | Value |
|---|---|
| Demographic Data | |
| Total patients, n | 70 |
| Gender, n (%) | |
| Female | 38 (54.3%) |
| Male | 32 (45.7%) |
| Age, years, mean (range) | 61 (23–81) |
| Educational level, n (%) | |
| Primary | 14 (20.0%) |
| Secondary | 31 (44.3%) |
| Tertiary | 25 (35.7%) |
| Employment status, n (%) | |
| Employed | 35 (50.0%) |
| Retired/Not working | 35 (50.0%) |
| Clinical Data | |
| Diagnosis, n (%) | |
| Lumbar spinal stenosis | 30 (42.9%) |
| Degenerative spondylolisthesis | 22 (31.4%) |
| Disk herniation with instability | 18 (25.7%) |
| Duration of symptoms, months, mean ± SD | 18.3 ± 12.6 |
| Prior conservative treatment ≥6 months, n (%) | 46 (65.7%) |
| Preoperative Psychological Assessment | |
| HADS-Anxiety score, mean ± SD | 6.8 ± 3.5 |
| HADS-Depression score, mean ± SD | 6.2 ± 3.3 |
| Clinically significant anxiety (HADS-A ≥ 8), n (%) | 22 (31.4%) |
| Clinically significant depression (HADS-D ≥ 8), n (%) | 18 (25.7%) |
| Both anxiety and depression, n (%) | 14 (20.0%) |
| Neither | 16 (22.9%) |
| Pain Catastrophizing Scale score, mean ± SD | 18.4 ± 9.7 |
| Measure | With Psychological Distress * | Without Psychological Distress | p-Value |
|---|---|---|---|
| Number of patients, n (%) | 26 (37.1%) | 44 (62.9%) | - |
| Pain Catastrophizing Scale, mean ± SD | 23.6 ± 10.2 | 15.3 ± 8.1 | <0.001 |
| Visual Analog Scale, median (IQR) | 7.0 (6.0–8.0) | 4.0 (3.0–5.0) | <0.001 |
| Oswestry Disability Index, median (IQR) | 52.0 (44.0–64.0) | 32.0 (24.0–40.0) | <0.001 |
| SF-36 Physical Functioning, median (IQR) | 30.0 (20.0–40.0) | 45.0 (35.0–60.0) | 0.002 |
| SF-36 Bodily Pain, median (IQR) | 22.5 (10.0–32.5) | 45.0 (32.5–55.0) | <0.001 |
| SF-36 General Health, median (IQR) | 40.0 (30.0–55.0) | 65.0 (50.0–75.0) | <0.001 |
| SF-36 Social Functioning, median (IQR) | 50.0 (37.5–62.5) | 75.0 (62.5–87.5) | <0.001 |
| SF-36 Emotional Well-being, median (IQR) | 48.0 (36.0–56.0) | 72.0 (60.0–80.0) | <0.001 |
| Measure | Baseline (t0) | 45 Days Post-Op (t2) | 6 Months Post-Op (t3) | p-Value t0 vs. t2 | p-Value t0 vs. t3 | p-Value t2 vs. t3 |
|---|---|---|---|---|---|---|
| Disability and Pain | ||||||
| Oswestry Disability Index, median | 39.00 | 13.00 | 27.00 | 0.00023 * | 0.042 * | 1.00 |
| Visual Analog Scale, median | 5.00 | 3.00 | 6.00 | 0.0007 * | 1.00 | 0.22 |
| Psychological Measures | ||||||
| Pain Catastrophizing Scale, median | 16.00 | 3.00 | 11.00 | 0.0084 * | 1.00 | 0.19 |
| HADS-Anxiety, median | 7.00 | 6.00 | 7.00 | 0.15 | 0.59 | 0.78 |
| HADS-Depression, median | 6.00 | 5.00 | 6.00 | 0.17 | 1.00 | 1.00 |
| SF-36 Health Survey Subscales | ||||||
| General Health, median | 55.00 | 60.00 | 55.00 | 0.12 | 1.00 | 1.00 |
| Physical Functioning, median | 40.00 | 65.00 | 55.00 | 0.00013 * | 0.09 | 1.00 |
| Bodily Pain, median | 32.50 | 67.50 | 45.00 | 0.00012 * | 0.36 | 1.00 |
| Emotional Well-being, median | 60.00 | 68.00 | 65.00 | 0.5 | 1.00 | 1.00 |
| Social Functioning, median | 50.00 | 75.00 | 62.50 | 0.001 * | 0.45 | 0.91 |
| Limitations due to Physical Health, median | 25.00 | 50.00 | 25.00 | 0.43 | 0.17 | 0.61 |
| Limitations due to Emotional Problems, median | 33.33 | 66.67 | 33.33 | 0.017 * | 0.54 | 1.00 |
| Energy & Fatigue, median | 45.00 | 55.00 | 45.00 | 0.058 | 1.00 | 1.00 |
| Health Change, median | 25.00 | 75.00 | 50.00 | 0.00002 * | 0.034 * | 1.00 |
| Preoperative Measure | Outcome Measure | Correlation Coefficient (r) | p-Value |
|---|---|---|---|
| HADS Total Score | |||
| Oswestry Disability Index | 0.42 | 0.002 * | |
| Visual Analog Scale | 0.36 | 0.015 * | |
| SF-36 Emotional Well-being | −0.53 | <0.001 * | |
| SF-36 Social Functioning | −0.44 | 0.002 * | |
| Pain Catastrophizing Scale | |||
| Oswestry Disability Index | 0.47 | 0.001 * | |
| Visual Analog Scale | 0.39 | 0.008 * | |
| SF-36 Bodily Pain | −0.52 | <0.001 * | |
| SF-36 Physical Functioning | −0.43 | 0.003 * | |
| Outcome | Predictor | Coefficient (β) | 95% CI | p-Value |
|---|---|---|---|---|
| Changes in ODI | ||||
| Change from t0 to t2 | −26.4 | −31.8 to −21.0 | <0.001 * | |
| Change from t2 to t3 | 14.2 | −1.6 to 30.0 | 0.079 | |
| Changes in VAS | ||||
| Change from t0 to t2 | −2.1 | −2.8 to −1.4 | <0.001 * | |
| Change from t2 to t3 | 3.0 | 1.1 to 4.9 | 0.003 * | |
| Impact of Preoperative Psychological Factors on 6-Month ODI | ||||
| HADS-Anxiety (per point increase) | 1.8 | 0.7 to 2.9 | 0.002 * | |
| Pain Catastrophizing Scale (per point increase) | 0.9 | 0.4 to 1.4 | 0.001 * | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Simonini, A.; Panciani, P.P.; Bergomi, R.; Saraceno, G.; Brembilla, C.; Capo, G.; Montemurro, N.; Rossi, C.; Agosti, E.; Gritti, L.; et al. Valuable Prognostic Role of Disability, Pain, Anxiety, and Depression Scales in Instrumented Lumbar Spine Surgery for Degenerative Pathology: The SAP-LD Study. Brain Sci. 2025, 15, 1035. https://doi.org/10.3390/brainsci15101035
Simonini A, Panciani PP, Bergomi R, Saraceno G, Brembilla C, Capo G, Montemurro N, Rossi C, Agosti E, Gritti L, et al. Valuable Prognostic Role of Disability, Pain, Anxiety, and Depression Scales in Instrumented Lumbar Spine Surgery for Degenerative Pathology: The SAP-LD Study. Brain Sciences. 2025; 15(10):1035. https://doi.org/10.3390/brainsci15101035
Chicago/Turabian StyleSimonini, Anita, Pier Paolo Panciani, Riccardo Bergomi, Giorgio Saraceno, Carlo Brembilla, Gabriele Capo, Nicola Montemurro, Claudio Rossi, Edoardo Agosti, Linda Gritti, and et al. 2025. "Valuable Prognostic Role of Disability, Pain, Anxiety, and Depression Scales in Instrumented Lumbar Spine Surgery for Degenerative Pathology: The SAP-LD Study" Brain Sciences 15, no. 10: 1035. https://doi.org/10.3390/brainsci15101035
APA StyleSimonini, A., Panciani, P. P., Bergomi, R., Saraceno, G., Brembilla, C., Capo, G., Montemurro, N., Rossi, C., Agosti, E., Gritti, L., Salierno, G., Fontanella, M. M., & Zanin, L. (2025). Valuable Prognostic Role of Disability, Pain, Anxiety, and Depression Scales in Instrumented Lumbar Spine Surgery for Degenerative Pathology: The SAP-LD Study. Brain Sciences, 15(10), 1035. https://doi.org/10.3390/brainsci15101035









