Abstract
Background: Symptomatic intracranial hemorrhage (sICH) is the most dreaded complication after reperfusion therapy for acute ischemic stroke. We performed a meta-analysis of randomized controlled trials to estimate and compare risks of sICH after mechanical thrombectomy (MT) depending on the location of the large vessel occlusion, concomitant use of intravenous thrombolysis, timing of treatment, and core size. Methods: Randomized controlled trials were included, following a comprehensive search of different databases from inception to 1 March 2024. Random-effect models in a meta-analysis were employed to obtain the pooled risk ratios (RRs) and their corresponding 95% confidence intervals (95% CI) for sICH with MT, and were then compared to other reperfusion treatment regimens, including best medical treatment and intravenous thrombolysis (IVT). Results: MT in the anterior circulation was associated with a significantly higher risk of sICH as compared with no-MT (RR: 1.46; 95%CI: 1.03–2.07; p = 0.037). The risk of sICH was comparable between the MT and MT+IVT groups (RR: 0.77; 95%CI: 0.57–1.03; p = 0.079). There was no difference in sICH risk with MT as compared with no-MT within 6 h of last known well (RR: 1.14; 95%CI: 0.78–1.66; p = 0.485) and beyond that time (RR: 1.29; 95%CI: 0.80–2.08; p = 0.252); the risk of sICH was also comparable between MT conducted within 6 h of last known well and MT conducted beyond that time (p = 0.512). The sICH risk for MT in the posterior circulation (RR: 7.48; 95%CI: 2.27–24.61) was significantly higher than for MT in the anterior circulation (RR: 1.18; 95%CI: 0.90–1.56) (p = 0.003). MT was also associated with a significantly higher sICH risk than no-MT among patients with large core strokes (RR: 1.71; 95%CI: 1.09–2.66, p = 0.018). Conclusions: When evaluating cumulative evidence from randomized controlled trials, the risk of sICH is increased after MT compared with patients not treated with MT. Yet, the difference is largely driven by the greater risk of sICH in patients treated with MT for posterior circulation occlusions and, to a lesser degree, large core strokes. Concomitant use of intravenous thrombolysis and the use of MT in the extended therapeutic window do not raise the risk of sICH.
1. Introduction
Stroke is a sudden disruption in blood flow to the brain, leading to brain cell damage and potential long-term disabilities such as paralysis, speech problems, and cognitive impairment. It is a leading cause of death and disability worldwide, with around 15 million people affected each year. Key risk factors include high blood pressure, smoking, diabetes, obesity, and physical inactivity. Stroke outcomes can range from partial recovery to permanent disability or death [1,2,3]. Post-stroke care focuses on rehabilitation through physical, speech, and occupational therapy, along with medication to prevent recurrence and manage underlying health conditions. Reperfusion therapy (via mechanical thrombectomy (MT), intravenous thrombolytics (IVT), or a combination of both) is a successful treatment for acute ischemic stroke (AIS). Researchers usually differentiate between anterior and posterior circulation strokes in terms of management and prognosis due to differences in the characteristics and risks of MT and IVT in both populations. Prior research has conclusively demonstrated that MT improves outcomes in patients with large vessel occlusion (LVO) in the anterior circulation [4,5]. However, MT also increases the risk of symptomatic intracranial hemorrhage (sICH) [6,7] and sICH after reperfusion therapy raises the likelihood of poor functional outcomes and mortality [8]. Estimates show that sICH occurs in 2–14% of cases after MT [9,10,11,12]. Accurate identification of patients at high risk of sICH could assist in making treatment decisions and tailoring appropriate monitoring regimens after the intervention [13].
The efficacy of MT for basilar artery occlusions, which is a rare but serious stroke event resulting from an occlusion affecting the basilar artery, had been controversial until recent trials and a meta-analysis demonstrated better functional outcomes after MT versus medical management in selected patients [14]. Nevertheless, the sICH rate was higher among patients with basilar artery occlusion treated with MT than in the medical management group [14]. How the risk of sICH after MT for basilar artery occlusion compares with the MT for anterior circulation occlusion remains largely unknown.
Previous meta-analyses have compared the risk of sICH after MT alone versus medical management [15], or MT alone versus MT+IVT [16,17,18,19]. Yet no previous meta-analysis has comprehensively compared the risk of sICH across various cohorts of patients treated with MT, not just with and without IVT, but also anterior versus posterior circulation occlusions, extended time window, and large versus small core strokes. Therefore, we conducted a meta-analysis of randomized controlled trials to estimate the risks of sICH following MT compared to the best medical therapy (BMT, including IVT and other standard care practices and procedures) across these various patient groups.
2. Methods
2.1. Search and Screening
A systematic literature review of the English language literature was undertaken on 1 March 2024, according to the PRISMA standards for undertaking systematic reviews (although no protocol was established for conducting this review and, therefore, no registration number can be provided), and included a comprehensive search on PubMed, Embase, Web of Science, and Scopus from inception [20]. For each database, various combinations of potential keywords and/or MeSH phrases were employed to achieve this objective. The following keywords and MeSH phrases were included: “stroke”, “cerebral infarction”, “endovascular”, “thrombectomy”, “intracranial hemorrhage”, “sICH”, “ICH”, “hemorrhage”, and others. A full list of the exact search terms used for each database can be seen in Supplementary Table S1. In addition, we conducted a thorough manual check of the references cited in the included publications to ensure that no relevant papers were overlooked.
We included the randomized clinical trials (including post hoc analyses) that fulfilled the following criteria: (1) adult patients with acute ischemic stroke who had emergency treatment with MT, (2) sICH confirmed by subsequent imaging (no restrictions were made regarding the definition of sICH and the definitions of each trial will be presented as reported), and (3) comparative outcomes reported based on MT versus no-MT or MT versus MT+IVT. Concomitant anterior and posterior circulation strokes were included. Duplicates among the different databases were removed and the remaining articles were organized for screening according to the prespecified criteria. The abstracts were screened separately to identify the appropriate patient population and then thoroughly analyzed to determine if they met the criteria for inclusion. At least two reviewers also conducted full-text, blind evaluations of all possible studies, and final appropriateness for inclusion into the meta-analysis was confirmed by all authors.
2.2. Data Extraction and Outcomes
After performing a preliminary extraction, an extraction sheet was generated and the extraction was carried out by two authors. The extracted data comprised trial characteristics (name, year of publication, and country), stroke location, the definition of interventions of each population, age, gender, NIHSS and ASPECTS scores at baseline, the definition of sICH, the rates of good functional outcome at 90 days (mRS 0–2), 90-day mortality and successful recanalization, and door-to-puncture time. The main outcome of this analysis was the rates of sICH after MT. We also compared the risks of sICH for (1) anterior versus posterior circulation occlusions, (2) direct MT versus MT preceded by IVT, (3) conventional (≤6 h) versus extended (>6 h) therapeutic time window, and (4) core size large (ASPECTS < 6) versus not large (ASPECTS ≥ 6). Following the extraction process, a thorough revision of the retrieved data was conducted by a third author to ensure the absence of any previous errors.
2.3. Risk of Bias Assessment
The risk of bias in the included trials was assessed via the “Cochrane RoB 2: a revised tool for assessing risk of bias” [21]. Two reviewers evaluated all papers blindly. They assessed the quality of each study and resolved any disagreements with the help of a third author, if necessary.
2.4. Statistical Analysis
The package “meta” was utilized to perform a pairwise meta-analysis to obtain the pooled risk ratios (RRs) and their corresponding 95% confidence intervals (95% CI). The meta-analysis utilized a random-effects model due to the presence of methodological heterogeneity that contradicted the common effect assumption and because there were more than five trials included in the analysis. The pooled effect sizes were deemed heterogeneous if the I2 value exceeded 50% and/or the p-value was less than 0.05, as determined by the Q-statistic. A sensitivity analysis was also conducted by removing trials investigating large core occlusions to exclude any potential of increasing sICH risk.
3. Results
3.1. Search Results
The comprehensive search strategy adopted in this meta-analysis yielded 2851 citations, of which 542 duplicates were removed. Following this, 2195 articles were excluded after meeting the exclusion criteria when screened via title/abstract. Accordingly, 114 articles were screened for eligibility via a full-text assessment, which resulted in the final inclusion of 31 relevant trials that were eligible for data synthesis (Supplementary Figure S1).
3.2. Characteristics and Quality Assessment
The data from 30 trials were extracted [11,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50], in addition to the sICH rates data that were obtained from one unpublished trial (TESLA trial). These included 27 trials of anterior circulation stroke and 4 trials of posterior circulation stroke. Data on infarct core and reperfusion timing after stroke onset could be extracted from the 27 trials investigating anterior circulation strokes, including 6 that investigated large core occlusions and 9 with patients having reperfusion timing beyond 6 h from stroke onset (i.e., time of last known well). A further 8 trials compared MT versus MT+IVT, while 19 trials investigated MT versus no-MT (BMT only). The definition of sICH among the included trials was not consistent. The definition of sICH was parenchymal hemorrhage type 2 associated with an increase of ≥4 points in the NIHSS score or leading to death (SITS-MOST) in most of the included trials. The exact definition used in each trial is presented in Supplementary Table S2. Other characteristics of the included studies, including patients’ age, gender, baseline NIHSS, baseline ASPECTS, mRS score at 90 days, and other treatment outcomes are presented in Table 1. RoB assessment demonstrated that almost all trials had a low risk of bias, except for one trial that had a high risk of bias arising from the randomization process and another that had some concerns due to deviation from the intended intervention. The complete presentation of RoB assessment domains, excluding the one unpublished trial, is shown in Supplementary Figures S1 and S2.

Table 1.
Characteristics of the included trials.
Table 1.
Characteristics of the included trials.
| Trial | Country | Location | Design | Group 1 | Group2 | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Age | Male | Location | NIHSS | ASPECTS | mRS (0–2 90 Day) | 90-Day Mortality | Successful Recanalization | Door to Puncture | Total | Age | Male | Location | NIHSS | ASPECTS | mRS | 90-day Mortality | Successful Recanalization | Door to Puncture | |||||
| DIRECT-MT [22] | China | A | RCT | 327 | 69 [61–76] | 189 | ic-ICA: 112/320, M1: 161/320, M2: 42/320 | 17 [12–21] | 9 [7–10] | 119 | 58 | 243/306 | 84 [67–105] | 329 | 18–60: 66; 60–80: 183; >80: 43 | 160 | ic-ICA: 114/326, M1: 178/326, M2: 33/326 | 17 [14–22] | 9 [7–10] | 121 | 62 | 267/316 | 85.5 [70–115] | |
| RESILIENT [23] | Brazil | A | RCT | 11 | 65 [54–77] | 60 | left hemisphere: 64 | 18 [14–21] | 8 [7–9] | 39 | 27 | 91 | 170 [132–213] | 111 | 67 [53–73] | 57 | 63 | 18 [14–21] | 8 [7–9] | 22 | 33 | - | 161 [115–219] | |
| THERAPY [24] | USA and Germany | A | RCT | 43 | 67 (11) | 27 | left hemisphere: 33; ic-ICA: 18, M1: 31, M2: 6 | 17 [13–22] | 7.5 [6–9] | 19/50 | 12% | 30/43 | - | 62 | 70 (10) | 27 | left hemisphere: 31; ic-ICA: 12, M1: 36, M2: 5 | 18 [ 14–22] | 8 [7–9] | 14/46 | 23.90% | 102 [80–154] | ||
| DAWN [26] | USA | A | RCT | 107 | 69.4 (14.1) | 42 | ic-ICA: 22, M1: 83, M2: 2 | 17 [13–21] | - | 49% | 20 | 90 | 109 [76–150] | 99 | 70.7 (13.2) | 51 | ic-ICA: 19, M1: 77, M2: 3 | 17 [14–21] | - | 13% | 18 | - | - | |
| RESCUE-Japan LIMIT [25] | Japan | A | RCT | 100 | 76.6 (10) | 55 | ic-ICA: 47, M1: 74, M2: 0; Tandem+M1: 20 | 22 [18–26] | 3 [3–4] | 14 | 18 | 86 | 254 [165–479] | 102 | 75.7 (10.2) | 58 | ic-ICA: 49, M1: 70, M2: 3; Tandem+M1: 20 | 22 [17–26] | 4 [3–4] | 8 | 24 | - | - | |
| RESCUE BT [27] | China | A | RCT | 483 | 67 [57–75] | 294 | ic-ICA: 98, M1: 310, M2: 77 | 16 [12–19] | 8 [7–9] | 219 | 84 | 439 | 398 [246–618] | 462 | 68 [58–74] | 263 | ic-ICA: 96, M1: 305, M2: 62 | 16 [12–20] | 8 [7–9] | 228 | 82 | 427 | 400 [272–627] | |
| CHOICE [28] | Spain | A | RCT | 52 | 73 [69–67] | 28 | ic-ICA: 4, M1: 20, M2: 28 | 14 [10–20] | 10 [8–10] | 33 | 8 | 52 | 356 [260–635] | 61 | 73 [71–76] | 33 | ic-ICA: 7, M1: 19, M2: 33 | 14 [8–20] | 9 [9–10] | 41 | 5 | 61 | 315 [218–680] | |
| SELECT2 [29] | United States, Canada, Europe, Australia, and New Zealand | A | RCT | 178 | 66 [58–75] | 107 | ic-ICA: 80, M1: 91, M2: 7 | 19 [15–23] | 4 [3–5] | 4 [3–6] | 68 | 142 | 109 [76–138] | 174 | 67 [58–75] | 100 | ic-ICA: 66, M1: 100, M2: 8 | 19 [15–22] | 4 [4–5] | 5 [4–6] | 71 | - | - | |
| SWIFT PRIME [30] | United States and Europe | A | RCT | 98 | 65 (12.5) | 54 | ic-ICA: 17, M1: 62, M2: 13 | 17 [13–20] | 9 [8–10] | 59/98 | 9% | 83% | 224 [165–275] | 97 | 66.3 (11.3) | 45 | ic-ICA: 15, M1: 72, M2: 6 | 17 [13–19] | 9 [7–10] | 33/93 | 12% | 40% | - | |
| SKIP [31] | Japan | A | RCT | 101 | 74 [67–80] | 56 | ic-ICA: 41, M1: 19, M2: 41 | 19 [13–23] | 7 [6–9] | 60 | 8 | 91 | - | 103 | 76 [67–80] | 72 | ic-ICA: 36, M1: 18, M2: 49 | 17 [12–22] | 8 [6–9] | 59 | 9 | 96 | - | |
| ATTENTION [32] | China | P | RCT | 226 | 66 (11.1) | 149 | VA-V4: 20, PBA: 69, MBA: 62, DBA: 74 | 24 [15–35] | 9 [8–10] | 75 | 83 | 208/223 | 5.6 [3.5–7.5] | 114 | 67.3 (10.2) | 82 | VA-V4: 6, PBA: 39, MBA: 29, DBA: 40 | 24 [14–35] | 10 [8–10] | 12 | 63 | - | - | |
| DEVT [34] | China | A | RCT | 115 | 70 [60–77] | 66 | ic-ICA: 18, M1: 95, M2: 3 | 16 [12–20] | 8 [7–9] | 63 | 20 | 113 | 200 [155–247] | 117 | 70 [60–78] | 66 | ic-ICA: 17, M1: 99, M2: 2 | 16 [13–20] | 8 [7–9] | 55 | 21 | 117 | 210 [179–255] | |
| DIRECT-SAFE [33] | Australia, New Zealand, China, and Vietnam | A | RCT | 148 | 70 [61–78] | 78 | ic-ICA: 33, M1: 80, M2: 21, BA: 11, Tandem-ec: 27, ic-ASD: 6 | 15 [11–20] | 10 [9–10] | 80/146 | 22 | 127/ 143 | 87 [56–113]; n:145 | 147 | 69 [60–79] | 88 | ic-ICA: 31, M1: 83, M2: 23, BA: 8, Tandem-ec: 20, ic-ASD: 8 | 15 [10–20] | 10 [9–10] | 89/147 | 24 | 130/146 | 101 [75–127]; n:147 | |
| TO-ACT [35] | Netherlands, China, and Portugal | A | RCT | 33 | 43 [33–50] | 10 | cerebral venous thrombosis | 12 [7–20] | - | 12 mo: 28/33 | 6 mo: 4/33 | 22 (79%) | - | 34 | 38 [23–48] | 7 | cerebral venous thrombosis | 12 [5–20] | - | 12 mo: 28/34 | 6 mo: 1/33 | 15 (52%) | - | |
| Huu An, 2022 [36] | Vietnam | A | RCT | 30 | 66.5 [59–78.5] | 21 | ICA: 33.3, M1: 60, M2: 6.7 | 12 [10–14] | 7 [7–8] | 60% | 3.30% | 90% | 69.5 [51–84] | 30 | 64 [58.75–74] | 18 | ICA: 40, M1: 50, M2: 10 | 13 [11–17.25] | 7 [7–8] | 60% | 6.70% | 86.70% | 73.0 [63.25–86] | |
| THRACE [11] | France | A | RCT | 200 | 62.8 (13.0) | 115 | intracranial internal carotid artery, the M1 segment of the middle cerebral artery, or the superior third of the basilar artery | 18 [15–21] | - | 53% | 12% | - | - | 202 | 62.8 (14.4) | 102 | intracranial internal carotid artery, the M1 segment of the middle cerebral artery, or the superior third of the basilar artery | 17 [13–21] | - | 42.10% | 13% | - | - | |
| DEFUSE 3 [37] | USA | A | RCT | 92 | 70 [59–79] | 46 | ICA: 35%, MCA: 65% | 16 [10–20] | 8 [7–9] | 3 [1–4] | 13 (14) | 65/83 (78) | 0:59 (0:39–1:27) | 90 | 71 [59–80] | 44 | ICA: 40%, MCA: 60% | 16 [12–21] | 8 [7–9] | 4 [3–6] | 23 (26) | 14/77 (18) | - | |
| IMS 3 [38] | United States, Canada, Australia, and Europe | A | RCT | 434 | 69 (23–89) | 218 | Left hemisphere: 224 (51.6), Right hemisphere: 197 (45.4), Brain stem or cerebellum: 10 (2.3), Unknown or multiple locations: 3 (0.7) | 17 [7–40] | 247 (56.9) | 99.80% | 19.10% | - | - | 222 | 68 (23–84) | 122 | Left hemisphere: 106 (47.7), Right hemisphere: 109 (49.1), Brain stem or cerebellum: 4 (1.8), Unknown or multiple locations: 3 (1.4) | 16 [8–30] | 131 (59.0) | 100 | 21.60% | - | - | |
| EXTEND-IA [39] | Australia and New Zealand | A | RCT | 35 | 68.6 (12.3) | 17 | ICA: 31%, MCA: 69% | 17 [13–20] | - | 1 [0–3] | - | 94% | - | 35 | 70.2 (11.8) | 17 | ICA: 31%, MCA: 69% | 13 [9–19] | - | 3 [1 to 5] | - | 43% | - | |
| SYNTHESIS Expansion [40] | Italy | A | RCT | 181 | 66 (11) | 106 | Anterior circulation: 88%, Posterior circulation: 10% | 13 [9–17] | - | - | - | - | - | 181 | 67 (11) | 103 | Anterior circulation: 94%, Posterior circulation: 6% | 13 [9–18] | - | - | - | - | - | |
| ESCAPE [41] | Canada, USA, South Korea, Ireland, UK | A | RCT | 165 | 71 [60.81] | 79 | ICA: 27.6, M1: 68.1, M2: 3.7 | 16 [13–20] | 9 [8–10] | 53% | 10.40% | 72.40% | - | 150 | 70 [60–81] | 71 | ICA: 26.5, M1: 71.4, M2: 2.0 | 17 [12–20] | 9 [8–10] | 29.30% | 19% | - | - | |
| REVASCAT [42] | Spain | A | RCT | 103 | 65.7 (11.3) | 55 | ICA: 25.5, M1: 64.7, M2: 9.8 | 17.0 [14.0–20.0] | 7.0 [6.0–9.0] | 43.7 | - | - | 269 [201–340] | 103 | 67.2 (9.5) | 54 | ICA: 26.7, M1: 64.4, M2: 7.9 | 17.0 (12.0–19.0) | 8.0 [6.0–9.0] | 28.2 | - | - | - | |
| BASICS [43] | Netherlands, Brazil, Germany, France, Italy, Switzerland, Czech republic | P | RCT | 154 | 66.8 (13.1) | 100 | - | 21 | - | 35.1 | 38.30% | - | 4.4 [3.3–6.2] | 146 | 67.2 (11.9) | 96 | - | 22 | - | 30.1 | 43.20% | - | - | |
| MR CLEAN–NO IV [45] | Netherlands | A | RCT | 273 | 72 [62–80] | 161 | ICA: 25, M1: 57.4, M2: 16.5 | 16 [10–20] | 9 [8–10] | 49.1 | 20.5 | 78.2 | 63 [50–78] | 266 | 69 [61–77] | 144 | ICA: 18.8, M1: 65.4, M2: 15 | 16 [10–20] | 9 [8–10] | 51.1 | 15.8 | 84.7 | 64 [51–78] | |
| BAOCHE [44] | China | P | RCT | 102 | 64.2 (9.6) | 80 | Basilar-artery occlusion | 20 [15–29] | 8 [7–10] | 39 | 31 | - | 153 [99–235] | 88 | 63.7 (9.8) | 79 | Basilar-artery occlusion | 19 [12–30] | 8 [7–10] | 14 | 42 | - | - | |
| ANGEL-ASPECT [46] | China | A | RCT | 230 | 68 [61–73] | 135 | ICA: 36.1, M1: 63, M2: 0.9 | 16 [13–20] | 3 [3–4] | 30 | 21.70% | - | - | 225 | 67 [59–73] | 144 | ICA: 36, M1: 63.1, M2: 0.9 | 15 [12–19] | 3 [3–4] | 11.6 | 20% | - | - | |
| MR RESCUE [47] | USA | A | RCT | 64 | Penumbral: 66.4 (13.2) NonPenumbral: 61.6 (12) | 30 | ICA: Penumbral: 18 NonPenumbral: 23, M1: Penumbral: 53 NonPenumbral: 70, M2: Penumbral: 29 NonPenumbral: 7 | Penumbral: 16 [12–18] NonPenumbral: 19 [17–22] | - | Penumbral: 21 NonPenumbral: 17 | - | - | - | 54 | Penumbral: 65.8 (16.9) NonPenumbral: 69.4 (15.9) | 27 | ICA: Penumbral: 15 NonPenumbral: 10, M1: Penumbral: 68 NonPenumbral: 80, M2: Penumbral: 18 NonPenumbral: 10 | Penumbral: 16 [11–18] NonPenumbral: 20.5 [17–23] | - | Penumbral: 26 NonPenumbral: 10 | - | - | - | |
| TENSION [48] | Canada and Europe | A | RCT | 128 | 73 [65–81] | 59 | ICA: 41/125, M1: 83, M2: 0, MCA+ACA: 1, tandem: 8 | 19 [16–22] | - | 4 [3–6] | 40.00% | 104 | 4.2 [3.4–5.9] | 125 | 74 [64–80] | 51 | ICA: 37/127, M1: 88, M2: 1, MCA+ACA: 1, tandem: 7 | 18 [15–22] | - | 6 [4–6] | 51% | - | - | |
| BEST [49] | China | P | RCT | 66 | 62 (50−74) | 48 | Vertebral artery V4 segment: 7; Basilar artery: 59 | 32 (18–38) | 8 (7–9) | 22 | 22 | 45 | 114 (66–150) | 65 | 68 (57−74) | 52 | Vertebral artery V4 segment: 5; Basilar artery: 60 | 26 (13–37) | 8 (7–9) | 18 | 25 | 9 | 111·5 (65–160) | |
| LASTE [50] | France, Spain, and the United States | A | RCT | 159 | 73 (66–79) | 82 | ICA: 69; M1 MCA: 88; Other: 2 | 21 (18–24) | 2 (1–3) | 4 (3–6) | 57/158 (36.1) | 48 (31.8) | 66 (45 to 97) | 165 | 74 (65–80) | 88 (53.3) | ICA: 74; M1 MCA: 91 | 21 (18–24) | 2 (1–3) | 6 (4–6) | 91/164 (55.5) | - | ||
A: Anterior circulation occlusions; P: posterior circulation occlusions; RCT: randomized controlled trial.
3.3. sICH Risk in the Anterior Circulation
3.3.1. Effect of Treatment Type
MT was associated with a significantly higher sICH risk than no-MT (RR: 1.46; 95%CI: 1.03–2.07; p = 0.037), with no significant heterogeneity (I2 = 24%; p = 0.168). The risk was comparable between the MT versus MT+IVT groups (RR: 0.77; 95%CI: 0.57–1.03; p = 0.079), indicating that IVT administration with MT does not further increase the risk of sICH (Figure 1).
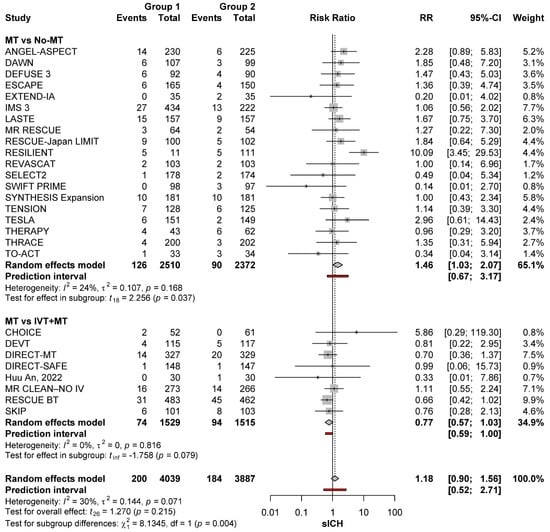
Figure 1.
sICH risk with the different reperfusion regimens among patients with anterior circulation occlusions [11,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50].
3.3.2. Effect of Timing
Time from last known well did not affect the risk of sICH. As compared with no-MT, the risk of sICH after MT was not increased regardless of whether time from last known well was within 6 h (RR: 1.14; 95%CI: 0.78–1.66; p = 0.485) or beyond 6 h (RR: 1.29; 95%CI: 0.80–2.08; p = 0.252)]. The risk of sICH was also similar when comparing MT conducted within 6 h versus MT conducted after 6 h (p = 0.215) (Figure 2).
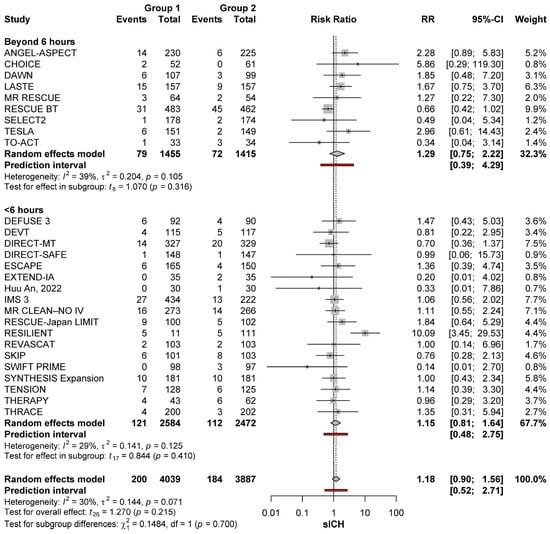
Figure 2.
sICH risk with MT (group 1) and no-MT (group 2) based on timing from stroke onset in the anterior circulation [11,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50].
3.3.3. Effect of Core Size
MT was associated with a significantly higher sICH risk than no-MT among patients with large core strokes (RR: 1.71; 95%CI: 1.09–2.66, p = 0.018), with no significant heterogeneity (I2 = 0%; p = 0.782). Conversely, in non-large core patients there was no difference in sICH risk between MT and no-MT groups (RR: 1.06; 95%CI: 0.76–1.49; p = 0.702), with no significant heterogeneity across studies (I2 = 33%; p = 0.072). However, when comparing sICH risks after MT for large core strokes versus MT for non-large core strokes, the difference was not significant (p = 0.089) (Figure 3).
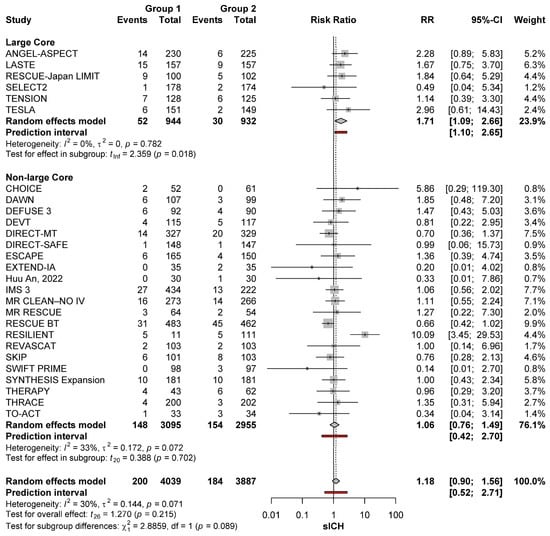
Figure 3.
sICH risk with MT (group 1) and no-MT (group 2) in large and non-large core occlusions of the anterior circulation [11,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50].
3.4. Sensitivity Analysis
After the exclusion of large core trials, the sICH risk did not differ between patients treated with MT and no-MT (RR: 1.30; 95%CI: 0.75–2.24; p = 0.313) and between MT and MT+IVT (RR: 0.77; 95%CI: 0.57–1.03; p = 0.079) (Figure 4).
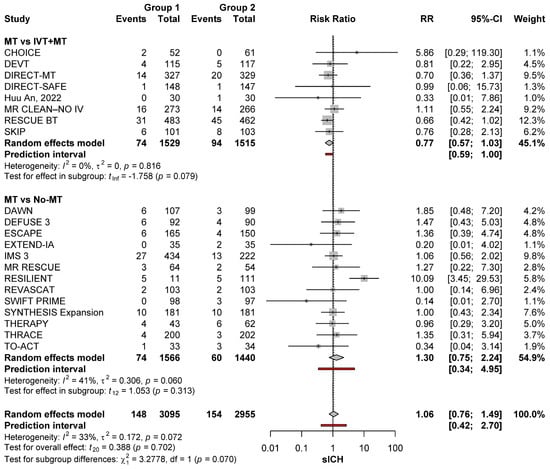
Figure 4.
sICH risk with the different reperfusion regimens among patients with anterior circulation occlusions after removing large core occlusions [11,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50].
After the exclusion of large core trials, time from last known well did not affect the risk of sICH. Compared with no-MT, the risk of sICH after MT was not increased regardless of whether time from last known well was within 6 h (RR: 1.11; 95%CI: 0.74–1.67; p = 0.590) or beyond that time (RR: 0.88; 95%CI: 0.38–2.04; p = 0.691). The risk of sICH was also similar when comparing MT conducted within 6 h versus MT conducted after 6 h (p = 0.512) (Figure 5).
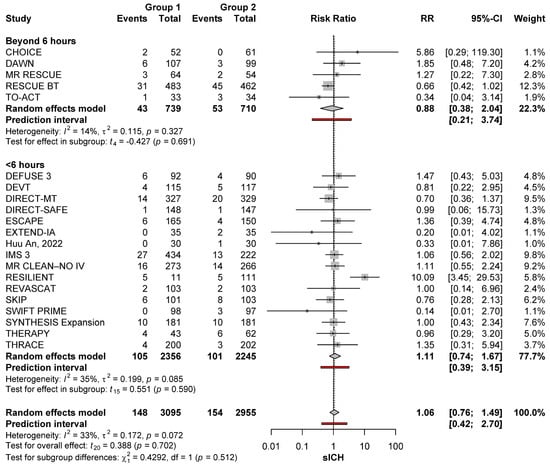
Figure 5.
sICH risk with MT (group 1) and no-MT (group 2) based on timing from stroke onset in the anterior circulation after removing large core occlusions [11,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50].
3.5. sICH in Anterior Versus Posterior Circulation Stroke
The risk of sICH was greater with MT than no-MT for posterior circulation occlusion (RR: 7.48; 95%CI: 2.27–24.61). No significant heterogeneity was noted (I2 = 0%; p = 0.955). On the other hand, the risk with MT was comparable to that of no-MT in patients with anterior circulation occlusions (RR: 1.18; 95%CI: 0.90–1.56), with no significant heterogeneity (I2 = 30%; p = 0.071). When comparing the sICH risk after MT for anterior versus posterior circulation occlusions, the risk was significantly higher among patients with posterior circulation occlusions (p = 0.003) (Figure 6). Sensitivity analysis removing the large core trials made this risk difference larger (RR: 7.48; 95%CI: 2.27–24.61 versus 1.06; 95%CI: 0.76–1.49; p = 0.002) (Figure 6).
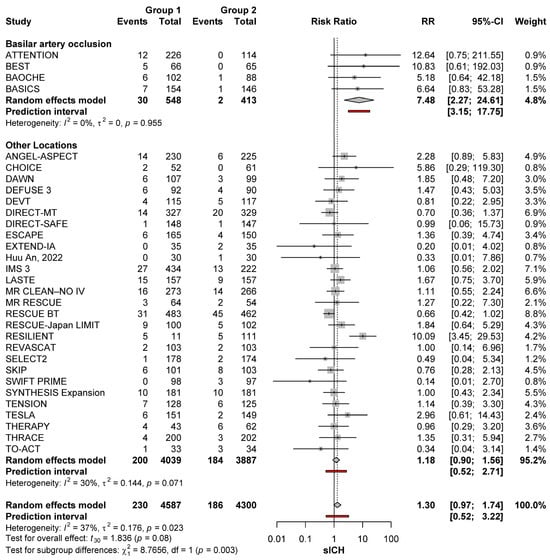
Figure 6.
sICH risk with MT (group 1) and no-MT (group 2) in posterior occlusions and other locations [11,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50].
4. Discussion
The current meta-analysis was aimed at summarizing the information on sICH from RCTs in various cohorts of patients treated with MT. MT has been associated with sICH as a potential adverse event despite the advantages correlated with recanalization and enhanced patient outcomes. The results show that the risk of sICH with MT is higher than no-MT, particularly for patients with posterior circulation occlusions, and to a lesser degree for patients with large core. Meanwhile, the risk of sICH is not increased when MT is combined with IVT or when MT is conducted after 6 h from last known well.
Data on anterior circulation strokes are much more extensive, allowing for adequate evaluation of sICH in subgroups of patients. Our analysis demonstrated that patients with anterior circulation stroke undergoing MT had a significantly higher risk of sICH than no-MT patients. Administration of IVT with MT does not increase the risk of sICH compared to MT alone, in agreement with previous meta-analyses [51,52], supporting the safety of bridge therapy for patients with anterior circulation large vessel occlusions [22,23,27,30,42]. Additionally, the timing of when MT is conducted does not have any major effect on sICH risk. Our meta-analysis showed that the risk of sICH was comparable when MT was conducted within the first 6 h after stroke onset versus in the extended therapeutic window.
We found that MT was associated with increased risk of sICH in patients with large core strokes, but not in patients with smaller core. In fact, the impact of core size on sICH risk may be underestimated. When interpreting the risk of sICH in patients with large core strokes, it is crucial to remember that even large parenchymal hemorrhages may not be categorized as symptomatic because of a ceiling effect on the NIHSS (i.e., patients with very high NIHSS strokes at baseline may not have a sufficient numerical increase in the NIHSS score for the ICH to be called symptomatic even if large and associated with major mass effects). This is a caveat to be considered when comparing the rates of sICH between strokes with large and non-large cores.
Our finding that the risk of sICH after MT is higher in patients with posterior circulation strokes as compared to strokes in the anterior circulation deserves a careful interpretation. Hemorrhage in posterior circulation strokes becomes symptomatic more often; even small hemorrhages in the brainstem or thalamus can cause major neurological decline. Meanwhile, cerebellar infarctions with hemorrhagic conversion from reperfusion injury can cause major deterioration from mass effect causing obstructive hydrocephalus or brainstem compression. Also, in practice, delayed diagnosis and treatment are more common in patients with ischemia affecting the posterior circulation. In such cases, MT may be attempted as a last resort intervention despite the presence of established infarction in areas where bleeding can be life-threatening. Also, most trials of posterior circulation stroke included patients with a medium-to-high severity only (NIHSS of 10 or more) [32,43,44], due to prior evidence suggesting that MT might not be beneficial in patients with mild posterior circulation strokes [43,53,54,55,56]. Further research to refine the prediction of sICH after MT for posterior circulation stroke would be useful, but the risk of sICH should not dissuade clinicians from pursuing MT in patients with severe deficits from a basilar artery occlusion.
The current meta-analysis has several strengths, particularly the evaluation of sICH risk related to MT in different patient groups and clinical scenarios. These multiple comparisons allowed us to identify groups of patients (basilar occlusion, large core, and others) with higher risk of sICH after MT. This meta-analysis also has limitations. sICH was reported in almost all trials as a secondary outcome without clear adjustments for potential confounders. The definitions of sICH among trials were not consistent. The number of trials investigating posterior-circulation stroke was relatively small, which restricted our ability to perform sub-analyses as we did for anterior circulation stroke (i.e., investigating the impact of treatment type, timing, and infarct core on risk of sICH). Furthermore, three of the four posterior circulation trials were conducted in China, which questions the generalizability of our findings to patients from other backgrounds.
5. Conclusions
Overall, the risk of sICH is increased after MT compared with patients not treated with MT, but the difference is largely driven by a greater risk of sICH in patients undergoing MT for basilar artery occlusions and in those presenting with large core strokes. The concomitant use of IVT and MT in the extended therapeutic window does not raise the risk of sICH. These findings shed light on the need to develop more personalized management practices for stroke patients, via enhancing the diagnostic efficacy and providing more precise recanalization approaches with a minimal risk associated with sICH development. Further research to refine the prediction of sICH after MT for posterior circulation stroke would be useful, but the risk of sICH should not dissuade clinicians from pursuing MT in patients with higher risks of sICH, as previously elaborated.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/brainsci15010063/s1, Table S1: Search strategy and results of the different databases. Table S2: Definitions of Groups 1 and 2 of each trial together with sICH rates and definitions. Figure S1: PRISMA flow chart. Figure S2: Risk of bias domains for all included trials. Figure S3: The overall risk of bias for all trials.
Author Contributions
Conceptualization, A.R. (Abdullah Reda) and S.G.; methodology, A.R. (Abdullah Reda), A.H., S.G., H.S.M., T.A.P., M.M., R.K., D.F.K. and A.R. (Alejandro Rabinstein); software, S.G.; validation, A.R. (Abdullah Reda), A.H., S.G., H.S.M., T.A.P., M.M., R.K., D.F.K. and A.R. (Alejandro Rabinstein); formal analysis, S.G.; investigation, A.R. (Abdullah Reda), A.H., S.G., H.S.M., T.A.P., M.M., R.K., D.F.K. and A.R. (Alejandro Rabinstein); resources, A.R. (Abdullah Reda), A.H., S.G., H.S.M., T.A.P. and M.M.; data curation, S.G., H.S.M. and T.A.P.; writing—original draft preparation, A.R. (Abdullah Reda), A.H., S.G., H.S.M., T.A.P., M.M., R.K., D.F.K. and A.R. (Alejandro Rabinstein); writing—review and editing, A.R. (Abdullah Reda), A.H., S.G., H.S.M., T.A.P., M.M., R.K., D.F.K. and A.R. (Alejandro Rabinstein); visualization, A.R. (Abdullah Reda), S.G. and A.R. (Alejandro Rabinstein); supervision, D.F.K. and A.R. (Alejandro Rabinstein); project administration, A.R (Alejandro Rabinstein). All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Data Availability Statement
The data are not publicly available due to privacy.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Li, J.; Zhong, Q.; Yuan, S.; Zhu, F. Global burden of stroke attributable to high systolic blood pressure in 204 countries and territories, 1990-2019. Front. Cardiovasc. Med. 2024, 11, 1339910. [Google Scholar] [CrossRef] [PubMed]
- Wu, S.; Liu, M. Global burden of stroke: Dynamic estimates to inform action. Lancet Neurol. 2024, 23, 952–953. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Lu, H.; Yang, C. Global, regional, and national burden of stroke from 1990 to 2019: A temporal trend analysis based on the Global Burden of Disease Study 2019. Int. J. Stroke 2024, 19, 686–694. [Google Scholar] [CrossRef] [PubMed]
- Jovin, T.G.; Nogueira, R.G.; Lansberg, M.G.; Demchuk, A.M.; Martins, S.O.; Mocco, J.; Ribo, M.; Jadhav, A.P.; Ortega-Gutierrez, S.; Hill, M.D.; et al. Thrombectomy for anterior circulation stroke beyond 6 h from time last known well (AURORA): A systematic review and individual patient data meta-analysis. Lancet 2022, 399, 249–258. [Google Scholar] [CrossRef]
- Goyal, M.; Menon, B.K.; van Zwam, W.H.; Dippel, D.W.; Mitchell, P.J.; Demchuk, A.M.; Dávalos, A.; Majoie, C.B.; van der Lugt, A.; de Miquel, M.A.; et al. Endovascular thrombectomy after large-vessel ischaemic stroke: A meta-analysis of individual patient data from five randomised trials. Lancet 2016, 387, 1723–1731. [Google Scholar] [CrossRef]
- Jansen, I.G.H.; Mulder, M.; Goldhoorn, R.B. Endovascular treatment for acute ischaemic stroke in routine clinical practice: Prospective, observational cohort study (MR CLEAN Registry). BMJ (Clin. Res. Ed.) 2018, 360, k949. [Google Scholar] [CrossRef]
- Wardlaw, J.M.; Murray, V.; Berge, E.; Del Zoppo, G.J. Thrombolysis for acute ischaemic stroke. Cochrane Database Syst. Rev. 2014, 2014, CD000213. [Google Scholar] [CrossRef]
- Maïer, B.; Desilles, J.P.; Mazighi, M. Intracranial Hemorrhage After Reperfusion Therapies in Acute Ischemic Stroke Patients. Front. Neurol. 2020, 11, 599908. [Google Scholar] [CrossRef]
- Chen, Y.; Zhou, S.; Yang, S.; Mofatteh, M.; Hu, Y.; Wei, H.; Lai, Y.; Zeng, Z.; Yang, Y.; Yu, J.; et al. Developing and predicting of early mortality after endovascular thrombectomy in patients with acute ischemic stroke. Front. Neurosci. 2022, 16, 1034472. [Google Scholar] [CrossRef]
- Neuberger, U.; Kickingereder, P.; Schönenberger, S.; Schieber, S.; Ringleb, P.A.; Bendszus, M.; Pfaff, J.; Möhlenbruch, M.A. Risk factors of intracranial hemorrhage after mechanical thrombectomy of anterior circulation ischemic stroke. Neuroradiology 2019, 61, 461–469. [Google Scholar] [CrossRef]
- Bracard, S.; Ducrocq, X.; Mas, J.L.; Soudant, M.; Oppenheim, C.; Moulin, T.; Guillemin, F. Mechanical thrombectomy after intravenous alteplase versus alteplase alone after stroke (THRACE): A randomised controlled trial. Lancet. Neurol. 2016, 15, 1138–1147. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Xie, Y.; Wang, H.; Yang, D.; Jiang, T.; Yuan, K.; Gong, P.; Xu, P.; Li, Y.; Chen, J.; et al. Symptomatic Intracranial Hemorrhage After Mechanical Thrombectomy in Chinese Ischemic Stroke Patients: The ASIAN Score. Stroke 2020, 51, 2690–2696. [Google Scholar] [CrossRef] [PubMed]
- Yaghi, S.; Willey, J.Z.; Cucchiara, B.; Goldstein, J.N.; Gonzales, N.R.; Khatri, P.; Kim, L.J.; Mayer, S.A.; Sheth, K.N.; Schwamm, L.H. Treatment and Outcome of Hemorrhagic Transformation After Intravenous Alteplase in Acute Ischemic Stroke: A Scientific Statement for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke 2017, 48, e343–e361. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Chen, S.; Bao, Q.; Yang, M.; Li, J. Real-world safety and efficacy endovascular treatment versus standard medical treatment for basilar artery occlusion: A systematic review and meta-analysis. Clin. Neurol. Neurosurg. 2024, 236, 108096. [Google Scholar] [CrossRef]
- Pressman, E.; Goldman, H.; Wang, C.; Mhaskar, R.; Guerrero, W.R.; Mokin, M.; Vakharia, K. A meta-analysis and systematic review of endovascular thrombectomy versus medical management for acute basilar artery occlusion. Clin. Neurol. Neurosurg. 2023, 234, 107986. [Google Scholar] [CrossRef]
- Du, H.; Lei, H.; Ambler, G.; Fang, S.; He, R.; Yuan, Q.; Werring, D.J.; Liu, N. Intravenous Thrombolysis Before Mechanical Thrombectomy for Acute Ischemic Stroke: A Meta-Analysis. J. Am. Heart Assoc. 2021, 10, e022303. [Google Scholar] [CrossRef]
- Morsi, R.Z.; Zhang, Y.; Carrión-Penagos, J.; Desai, H.; Tannous, E.; Kothari, S.; Khamis, A.; Darzi, A.J.; Tarabichi, A.; Bastin, R.; et al. Endovascular Thrombectomy With or Without Thrombolysis for Stroke: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Neurohospitalist 2024, 14, 23–33. [Google Scholar] [CrossRef]
- Trifan, G.; Biller, J.; Testai, F.D. Mechanical Thrombectomy vs Bridging Therapy for Anterior Circulation Large Vessel Occlusion Stroke: Systematic Review and Meta-analysis. Neurology 2022, 98, e1361–e1373. [Google Scholar] [CrossRef]
- Wang, X.; Ye, Z.; Busse, J.W.; Hill, M.D.; Smith, E.E.; Guyatt, G.H.; Prasad, K.; Lindsay, M.P.; Yang, H.; Zhang, Y.; et al. Endovascular thrombectomy with or without intravenous alteplase for acute ischemic stroke due to large vessel occlusion: A systematic review and meta-analysis of randomized trials. Stroke Vasc. Neurol. 2022, 7, 510–517. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Med. 2009, 6, e1000100. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ (Clin. Res. Ed.) 2019, 366, l4898. [Google Scholar] [CrossRef] [PubMed]
- Yang, P.; Zhang, Y.; Zhang, L.; Zhang, Y.; Treurniet, K.M.; Chen, W.; Peng, Y.; Han, H.; Wang, J.; Wang, S.; et al. Endovascular Thrombectomy with or without Intravenous Alteplase in Acute Stroke. N. Engl. J. Med. 2020, 382, 1981–1993. [Google Scholar] [CrossRef] [PubMed]
- Martins, S.O.; Mont’Alverne, F.; Rebello, L.C.; Abud, D.G.; Silva, G.S.; Lima, F.O.; Parente, B.S.M.; Nakiri, G.S.; Faria, M.B.; Frudit, M.E.; et al. Thrombectomy for Stroke in the Public Health Care System of Brazil. N. Engl. J. Med. 2020, 382, 2316–2326. [Google Scholar] [CrossRef] [PubMed]
- Mocco, J.; Zaidat, O.O.; von Kummer, R.; Yoo, A.J.; Gupta, R.; Lopes, D.; Frei, D.; Shownkeen, H.; Budzik, R.; Ajani, Z.A.; et al. Aspiration Thrombectomy After Intravenous Alteplase Versus Intravenous Alteplase Alone. Stroke 2016, 47, 2331–2338. [Google Scholar] [CrossRef]
- Yoshimura, S.; Sakai, N.; Yamagami, H.; Uchida, K.; Beppu, M.; Toyoda, K.; Matsumaru, Y.; Matsumoto, Y.; Kimura, K.; Takeuchi, M.; et al. Endovascular Therapy for Acute Stroke with a Large Ischemic Region. N. Engl. J. Med. 2022, 386, 1303–1313. [Google Scholar] [CrossRef]
- Nogueira, R.G.; Jadhav, A.P.; Haussen, D.C.; Bonafe, A.; Budzik, R.F.; Bhuva, P.; Yavagal, D.R.; Ribo, M.; Cognard, C.; Hanel, R.A.; et al. Thrombectomy 6 to 24 Hours after Stroke with a Mismatch between Deficit and Infarct. N. Engl. J. Med. 2017, 378, 11–21. [Google Scholar] [CrossRef]
- Investigators, R.B.T. Effect of Intravenous Tirofiban vs Placebo Before Endovascular Thrombectomy on Functional Outcomes in Large Vessel Occlusion Stroke: The RESCUE BT Randomized Clinical Trial. JAMA 2022, 328, 543–553. [Google Scholar] [CrossRef]
- Renú, A.; Millán, M.; San Román, L.; Blasco, J.; Martí-Fàbregas, J.; Terceño, M.; Amaro, S.; Serena, J.; Urra, X.; Laredo, C.; et al. Effect of Intra-arterial Alteplase vs Placebo Following Successful Thrombectomy on Functional Outcomes in Patients With Large Vessel Occlusion Acute Ischemic Stroke: The CHOICE Randomized Clinical Trial. JAMA 2022, 327, 826–835. [Google Scholar] [CrossRef]
- Sarraj, A.; Hassan, A.E.; Abraham, M.G.; Ortega-Gutierrez, S.; Kasner, S.E.; Hussain, M.S.; Chen, M.; Blackburn, S.; Sitton, C.W.; Churilov, L.; et al. Trial of Endovascular Thrombectomy for Large Ischemic Strokes. N. Engl. J. Med. 2023, 388, 1259–1271. [Google Scholar] [CrossRef]
- Saver, J.L.; Goyal, M.; Bonafe, A.; Diener, H.-C.; Levy, E.I.; Pereira, V.M.; Albers, G.W.; Cognard, C.; Cohen, D.J.; Hacke, W.; et al. Stent-Retriever Thrombectomy after Intravenous t-PA vs. t-PA Alone in Stroke. N. Engl. J. Med. 2015, 372, 2285–2295. [Google Scholar] [CrossRef]
- Suzuki, K.; Matsumaru, Y.; Takeuchi, M.; Morimoto, M.; Kanazawa, R.; Takayama, Y.; Kamiya, Y.; Shigeta, K.; Okubo, S.; Hayakawa, M.; et al. Effect of Mechanical Thrombectomy Without vs With Intravenous Thrombolysis on Functional Outcome Among Patients With Acute Ischemic Stroke: The SKIP Randomized Clinical Trial. JAMA 2021, 325, 244–253. [Google Scholar] [CrossRef] [PubMed]
- Tao, C.; Nogueira, R.G.; Zhu, Y.; Sun, J.; Han, H.; Yuan, G.; Wen, C.; Zhou, P.; Chen, W.; Zeng, G.; et al. Trial of Endovascular Treatment of Acute Basilar-Artery Occlusion. N. Engl. J. Med. 2022, 387, 1361–1372. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, P.J.; Yan, B.; Churilov, L.; Dowling, R.J.; Bush, S.J.; Bivard, A.; Huo, X.C.; Wang, G.; Zhang, S.Y.; Ton, M.D.; et al. Endovascular thrombectomy versus standard bridging thrombolytic with endovascular thrombectomy within 4·5 h of stroke onset: An open-label, blinded-endpoint, randomised non-inferiority trial. Lancet 2022, 400, 116–125. [Google Scholar] [CrossRef] [PubMed]
- Zi, W.; Qiu, Z.; Li, F.; Sang, H.; Wu, D.; Luo, W.; Liu, S.; Yuan, J.; Song, J.; Shi, Z.; et al. Effect of Endovascular Treatment Alone vs Intravenous Alteplase Plus Endovascular Treatment on Functional Independence in Patients With Acute Ischemic Stroke: The DEVT Randomized Clinical Trial. JAMA 2021, 325, 234–243. [Google Scholar] [CrossRef]
- Coutinho, J.M.; Zuurbier, S.M.; Bousser, M.G.; Ji, X.; Canhão, P.; Roos, Y.B.; Crassard, I.; Nunes, A.P.; Uyttenboogaart, M.; Chen, J.; et al. Effect of Endovascular Treatment With Medical Management vs Standard Care on Severe Cerebral Venous Thrombosis: The TO-ACT Randomized Clinical Trial. JAMA Neurol. 2020, 77, 966–973. [Google Scholar] [CrossRef]
- Huu An, N.; Dang Luu, V.; Duy Ton, M.; Anh Tuan, T.; Quang Anh, N.; Hoang Kien, L.; Tat Thien, N.; Viet Phuong, D.; Minh Duc, N. Thrombectomy Alone versus Bridging Therapy in Acute Ischemic Stroke: Preliminary Results of an Experimental Trial. La. Clin. Ter. 2022, 173, 107–114. [Google Scholar] [CrossRef]
- Albers, G.W.; Marks, M.P.; Kemp, S.; Christensen, S.; Tsai, J.P.; Ortega-Gutierrez, S.; McTaggart, R.A.; Torbey, M.T.; Kim-Tenser, M.; Leslie-Mazwi, T.; et al. Thrombectomy for Stroke at 6 to 16 Hours with Selection by Perfusion Imaging. N. Engl. J. Med. 2018, 378, 708–718. [Google Scholar] [CrossRef]
- Broderick, J.P.; Palesch, Y.Y.; Demchuk, A.M.; Yeatts, S.D.; Khatri, P.; Hill, M.D.; Jauch, E.C.; Jovin, T.G.; Yan, B.; Silver, F.L.; et al. Endovascular Therapy after Intravenous t-PA versus t-PA Alone for Stroke. N. Engl. J. Med. 2013, 368, 893–903. [Google Scholar] [CrossRef]
- Campbell, B.C.V.; Mitchell, P.J.; Kleinig, T.J.; Dewey, H.M.; Churilov, L.; Yassi, N.; Yan, B.; Dowling, R.J.; Parsons, M.W.; Oxley, T.J.; et al. Endovascular Therapy for Ischemic Stroke with Perfusion-Imaging Selection. N. Engl. J. Med. 2015, 372, 1009–1018. [Google Scholar] [CrossRef]
- Ciccone, A.; Valvassori, L.; Nichelatti, M.; Sgoifo, A.; Ponzio, M.; Sterzi, R.; Boccardi, E. Endovascular Treatment for Acute Ischemic Stroke. N. Engl. J. Med. 2013, 368, 904–913. [Google Scholar] [CrossRef]
- Goyal, M.; Demchuk, A.M.; Menon, B.K.; Eesa, M.; Rempel, J.L.; Thornton, J.; Roy, D.; Jovin, T.G.; Willinsky, R.A.; Sapkota, B.L.; et al. Randomized Assessment of Rapid Endovascular Treatment of Ischemic Stroke. N. Engl. J. Med. 2015, 372, 1019–1030. [Google Scholar] [CrossRef] [PubMed]
- Jovin, T.G.; Chamorro, A.; Cobo, E.; de Miquel, M.A.; Molina, C.A.; Rovira, A.; San Román, L.; Serena, J.; Abilleira, S.; Ribó, M.; et al. Thrombectomy within 8 Hours after Symptom Onset in Ischemic Stroke. N. Engl. J. Med. 2015, 372, 2296–2306. [Google Scholar] [CrossRef] [PubMed]
- Langezaal, L.C.M.; van der Hoeven, E.J.R.J.; Mont’Alverne, F.J.A.; de Carvalho, J.J.F.; Lima, F.O.; Dippel, D.W.J.; van der Lugt, A.; Lo, R.T.H.; Boiten, J.; Lycklama à Nijeholt, G.J.; et al. Endovascular Therapy for Stroke Due to Basilar-Artery Occlusion. N. Engl. J. Med. 2021, 384, 1910–1920. [Google Scholar] [CrossRef] [PubMed]
- Jovin, T.G.; Li, C.; Wu, L.; Wu, C.; Chen, J.; Jiang, C.; Shi, Z.; Gao, Z.; Song, C.; Chen, W.; et al. Trial of Thrombectomy 6 to 24 Hours after Stroke Due to Basilar-Artery Occlusion. N. Engl. J. Med. 2022, 387, 1373–1384. [Google Scholar] [CrossRef]
- LeCouffe, N.E.; Kappelhof, M.; Treurniet, K.M.; Rinkel, L.A.; Bruggeman, A.E.; Berkhemer, O.A.; Wolff, L.; van Voorst, H.; Tolhuisen, M.L.; Dippel, D.W.J.; et al. A Randomized Trial of Intravenous Alteplase before Endovascular Treatment for Stroke. N. Engl. J. Med. 2021, 385, 1833–1844. [Google Scholar] [CrossRef]
- Huo, X.; Ma, G.; Tong, X.; Zhang, X.; Pan, Y.; Nguyen, T.N.; Yuan, G.; Han, H.; Chen, W.; Wei, M.; et al. Trial of Endovascular Therapy for Acute Ischemic Stroke with Large Infarct. N. Engl. J. Med. 2023, 388, 1272–1283. [Google Scholar] [CrossRef]
- Kidwell, C.S.; Jahan, R.; Gornbein, J.; Alger, J.R.; Nenov, V.; Ajani, Z.; Feng, L.; Meyer, B.C.; Olson, S.; Schwamm, L.H.; et al. A Trial of Imaging Selection and Endovascular Treatment for Ischemic Stroke. N. Engl. J. Med. 2013, 368, 914–923. [Google Scholar] [CrossRef]
- Bendszus, M.; Fiehler, J.; Subtil, F.; Bonekamp, S.; Aamodt, A.H.; Fuentes, B.; Gizewski, E.R.; Hill, M.D.; Krajina, A.; Pierot, L.; et al. Endovascular thrombectomy for acute ischaemic stroke with established large infarct: Multicentre, open-label, randomised trial. Lancet 2023, 402, 1753–1763. [Google Scholar] [CrossRef]
- Liu, X.; Dai, Q.; Ye, R.; Zi, W.; Liu, Y.; Wang, H.; Zhu, W.; Ma, M.; Yin, Q.; Li, M.; et al. Endovascular treatment versus standard medical treatment for vertebrobasilar artery occlusion (BEST): An open-label, randomised controlled trial. Lancet Neurol. 2020, 19, 115–122. [Google Scholar] [CrossRef]
- Costalat, V.; Jovin, T.G.; Albucher, J.F.; Cognard, C.; Henon, H.; Nouri, N.; Gory, B.; Richard, S.; Marnat, G.; Sibon, I.; et al. Trial of Thrombectomy for Stroke with a Large Infarct of Unrestricted Size. N. Engl. J. Med. 2024, 390, 1677–1689. [Google Scholar] [CrossRef]
- Majoie, C.B.; Cavalcante, F.; Gralla, J.; Yang, P.; Kaesmacher, J.; Treurniet, K.M.; Kappelhof, M.; Yan, B.; Suzuki, K.; Zhang, Y.; et al. Value of intravenous thrombolysis in endovascular treatment for large-vessel anterior circulation stroke: Individual participant data meta-analysis of six randomised trials. Lancet 2023, 402, 965–974. [Google Scholar] [CrossRef] [PubMed]
- Panigrahi, B.; Thakur Hameer, S.; Bhatia, R.; Haldar, P.; Sharma, A.; Srivastava, M.V.P. Effect of endovascular therapy in large anterior circulation ischaemic strokes: A systematic review and meta-analysis of randomised controlled trials. Eur. Stroke J. 2023, 8, 932–941. [Google Scholar] [CrossRef] [PubMed]
- Tao, C.; Qureshi, A.I.; Yin, Y.; Li, J.; Li, R.; Xu, P.; Sun, J.; Liao, G.; Yue, X.; Shi, H.; et al. Endovascular Treatment Versus Best Medical Management in Acute Basilar Artery Occlusion Strokes: Results From the ATTENTION Multicenter Registry. Circulation 2022, 146, 6–17. [Google Scholar] [CrossRef] [PubMed]
- Schonewille, W.J.; Wijman, C.A.; Michel, P.; Rueckert, C.M.; Weimar, C.; Mattle, H.P.; Engelter, S.T.; Tanne, D.; Muir, K.W.; Molina, C.A.; et al. Treatment and outcomes of acute basilar artery occlusion in the Basilar Artery International Cooperation Study (BASICS): A prospective registry study. Lancet Neurol. 2009, 8, 724–730. [Google Scholar] [CrossRef] [PubMed]
- Goyal, N.; Tsivgoulis, G.; Malhotra, K.; Ishfaq, M.F.; Pandhi, A.; Frohler, M.T.; Spiotta, A.M.; Anadani, M.; Psychogios, M.; Maus, V.; et al. Medical Management vs Mechanical Thrombectomy for Mild Strokes: An International Multicenter Study and Systematic Review and Meta-analysis. JAMA Neurol. 2020, 77, 16–24. [Google Scholar] [CrossRef]
- Hou, X.; Feng, X.; Wang, H.; Li, Q. Mechanical Thrombectomy for Mild Acute Ischemic Stroke with Large-Vessel Occlusion: A Systematic Review and Meta-Analysis. Cerebrovasc. Dis. 2022, 51, 615–622. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).