Virtual Reality-Based Interventions to Improve Balance in Patients with Traumatic Brain Injury: A Scoping Review
Abstract
1. Introduction
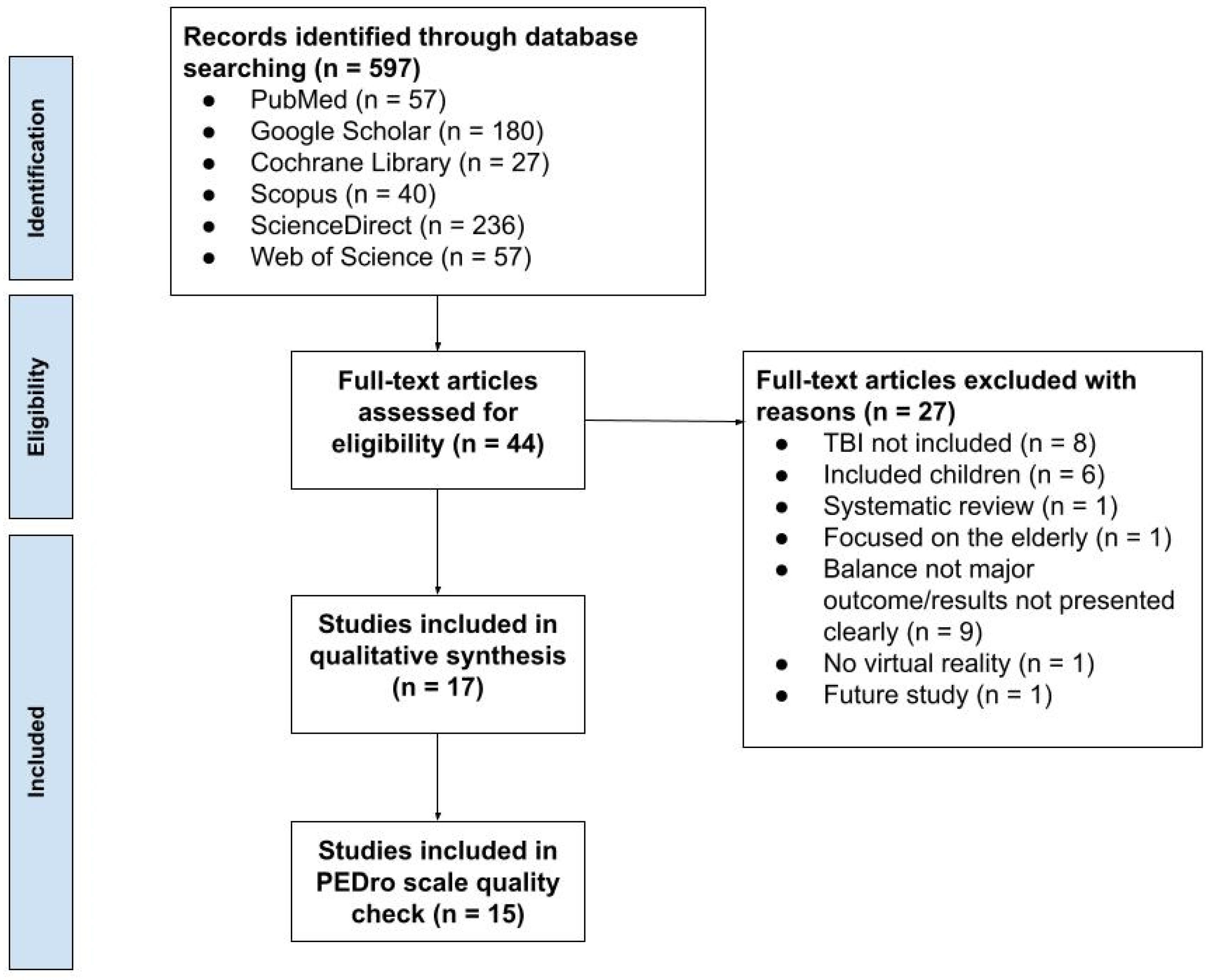
2. Materials and Methods
3. Results
3.1. Risk of Bias Analysis
3.2. Randomized Controlled Trials
3.3. Single-Arm Experimental Study
3.4. Retrospective Studies
3.5. Case Studies
3.6. Feasibility/Usability Study
3.7. Cohort Study
3.8. Diagnostic (Validation) Studies
| Title | Author | Date Published | Score |
|---|---|---|---|
| Feasibility of virtual reality and treadmill training in traumatic brain injury: a randomized controlled pilot trial [24] | Tefertiller et al. | 2022 | 8 |
| Sensorimotor conflict tests in an immersive virtual environment reveal subclinical impairments in mild traumatic brain injury [25] | Rao et al. | 2020 | 5 |
| Results From a Randomized Controlled Trial to Address Balance Deficits After Traumatic Brain Injury [26] | Tefertiller et al. | 2019 | 8 |
| Assessing subacute mild traumatic brain injury with a portable virtual reality balance device [27] | Wright et al. | 2016 | 5 |
| Differential Sensitivity Between a Virtual Reality Balance Module and Clinically Used Concussion Balance Modalities [28] | Teel et al. | 2016 | 4 |
| Visual-vestibular processing deficits in mild traumatic brain injury [29] | Wright et al. | 2017 | 4 |
| Advanced virtual reality-based rehabilitation of balance and gait in clinical practice [32] | Porras et al. | 2019 | 3 |
| History of Mild Traumatic Brain Injury Affects Static Balance under Complex Multisensory Manipulations [33] | Wright et al. | 2022 | 5 |
| Expanding Clinical Assessment for Traumatic Brain Injury and Comorbid Post-Traumatic Stress Disorder: A Retrospective Analysis of Virtual Environment Tasks in the Computer-Assisted Rehabilitation Environment [34] | Onakomaiya et al. | 2017 | 5 |
| Healthy Active Duty Military with Lifetime Experience of Mild Traumatic Brain Injury Exhibits Subtle Deficits in Sensory Reactivity and Sensory Integration During Static Balance [35] | Wright et al. | 2018 | 3 |
| Contextual sensory integration training via head mounted display for individuals with vestibular disorders: a feasibility study [36] | Lubetzky et al. | 2022 | 3 |
| Sensorimotor training for injury prevention in collegiate soccer players: An experimental study [37] | Reneker et al. | 2019 | 3 |
| The effects of video game therapy on balance and attention in chronic ambulatory traumatic brain injury: an exploratory study [38] | Straudi et al. | 2017 | 7 |
| Effects of Balance Training Using a Virtual Reality Program in Hemiplegic Patients [39] | Jung-Ah Kwon, Yoon-Kyum Shin, Deok-Ju Kim, Sung-Rae Cho | 2022 | 5 |
| Towards defining biomarkers to evaluate concussions using virtual reality and a moving platform (BioVRSea) [40] | Jacob et al. | 2022 | 4 |
| (a) | |||||||||||||
| Sr. No | Study Duration | VR System | Outcomes | Participant Groups | |||||||||
| [24] | 1 baseline; 12 training sessions over 4 weeks (after 2 weeks of baseline); 1 post-treatment assessment (within 1 week of final training session), follow up assessment (after 4 weeks of final training session) | Motek C-Mill™ treadmill (Non-Immersive) | Assessment | Metric | Virtual Reality + Treadmill Training N = 10 | Treadmill Training N = 11 | Standard of Care N = 10 | ||||||
| Community Balance and Mobility Scale | Mean (SD) | B | PT | F* | B | PT | F* | B | PT | F* | |||
| 33.1 (21.3) | 39.0 (24.6) | 39.0 (24.2) | 27.4 (25.1) | 32.5 (27.7) | 35.9 (28.5) | 31.6 (21.5) | 37.8 (25.6) | 41.2 (25.6) | |||||
| 10 Meter Walk Test (Speed, meters/second | Mean (SD) | 1.09 (0.45) | 1.21 (0.49) | 1.14 (0.38) | 1.05 (0.50) | 1.12 (0.47) | 1.11 (0.45) | 0.99 (0.44) | 1.03 (0.46) | 1.02 (0.38) | |||
| 6 Minute Walk Test (Distance, meters) | Mean (SD) | 344.0 (122.4) | 377.4 (151.8) | 398.2 (138.5) | 359.2 (157.1) | 397.3 (180.7) | 402.9 (166.4) | 343.7 (149.2) | 374.5 (151.3) | 378.3 (154.4) | |||
| Timed Up and Go Test (Time, seconds) | Mean (SD) | 16.4 (14.6) | 14.3 (10.4) | 13.4 (7.0) | 17.7 (13.3) | 17.2 (13.3) | 16.6 (13.7) | 21.5 (30.1) | 17.5 (21.3) | 19.9 (26.4) | |||
| Physical Activity Enjoyment Scale | Mean (SD) | 105.3 (16.2) | 113.9 (12.7) | N/A | 111.7 (14.5) | 112.9 (16.1) | N/A | 103.9 (17.3) | 103.3 (19.8) | N/A | |||
| [25] | 3–4 training sessions/week (30 min) for 12 weeks; 1 follow-up on week 24 | X-Box Kinect (Non-Immersive) | Outcomes | TBI (VR Group) | TBI (Home Exercise Program Group) | ||||||||
| Assessment | Metric | 6 weeks* | 12 weeks* | 24 weeks* | 6 weeks* | 12 weeks* | 24 weeks* | ||||||
| Community Balance and Mobility Scale | Mean Estimate | 5.19 | 7.73 | 8.60 | 5.49 | 7.87 | 8.73 | ||||||
| SE | 1.31 | 1.66 | 1.39 | 1.31 | 1.66 | 1.37 | |||||||
| 95% CI | 2.57–7.81 | 4.41–11.05 | 5.81–11.38 | 2.87–8.11 | 4.55–11.19 | 5.99–11.48 | |||||||
| p Value | 0.0002 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | |||||||
| Balance Evaluation System Test (BESTest) Changes from Baseline | Mean Estimate | 3.90 | 5.27 | 6.80 | 3.89 | 5.36 | 5.89 | ||||||
| SE | 1.31 | 1.69 | 1.44 | 1.31 | 1.69 | 1.42 | |||||||
| 95% CI | 1.28–6.52 | 1.89–8.65 | 3.92–9.68 | 1.27–6.51 | 1.99–8.74 | 3.05–8.74 | |||||||
| p Value | 0.0042 | 0.0028 | <0.0001 | 0.0043 | 0.0023 | 0.0001 | |||||||
| Activities-Specific Balance Confidence Scale (ABC) | Mean Estimate | 3.30 | 1.62 | 3.75 | 0.65 | 2.60 | 2.45 | ||||||
| SE | 1.76 | 1.64 | 1.91 | 1.75 | 1.64 | 1.64 | |||||||
| 95% CI | −0.23 to 6.82 | −1.66 to 4.90 | −0.08 to 7.57 | −2.86 to 4.16 | −0.67 to 5.88 | −0.67 to 5.88 | |||||||
| p Value | 0.0663 | 0.3271 | 0.0550 | 0.7138 | 0.1171 | 0.1171 | |||||||
| Participation Assessment with Recombined Tools-Objective (PART-O) | Mean Estimate | 0.00 | 0.02 | 0.07 | 0.08 | 0.04 | 0.04 | ||||||
| SE | =0.05 | 0.05 | 0.07 | 0.05 | 0.05 | 0.07 | |||||||
| 95% CI | −0.11 to 0.10 | −0.09 to 0.13 | −0.08 to 0.21 | −0.03 to 0.19 | −0.07 to 0.14 | −0.11 to 0.18 | |||||||
| p Value | 0.9523 | 0.7023 | 0.3676 | 0.1494 | 0.4977 | 0.6204 | |||||||
| [26] | 3 sessions/week for 6 weeks (1 h) | Xbox 360 Kinect (Non-Immersive) | Outcomes | TBI (VGT) | TBI (BPT) | ||||||||
| Assessment | Metric | B** | PT** | B** | PT** | ||||||||
| Community Balance and Mobility Scale | Median (IQR) | 17 (15) | 25 (15.5) | 25 (32) | 25.5 (31.5) | ||||||||
| Unified Balance Scale | (UBS) | 43 (20.5) | 49.5 (20.5) | 49 (18.5) | 51 (20.5) | ||||||||
| Timed up and Go Test | (Time, seconds) | 18.7 (16.1) | 16.4 (9.4) | 14.0 (20.3) | 15.4 (16.2) | ||||||||
| Static balance | ML path length (mm) | EO: 154.9 (56.0) EC: 161.2 (68.3) | EO: 140.7 (83.9) EC: 188.1 (85.0) | EO: 169.5 (539.5) EC: 218.8 (508.3) | EO: 201.0 (128.3) EC: 233.5 (145.8) | ||||||||
| AP path length (mm) | EO: 223.7 (80.9) EC: 312.0 (141.1) | 171.2 (137.6) EC: 311.3 (147.9) | EO: 258.3 (127.6) EC: 332.5 (419.6) | EO: 262.7 (226.1) EC: 321.6 (480.4) | |||||||||
| Sway speed (mm/s) | EO: 15.6 (6.9) EC: 19.2(4.3) | 12.7 (8.6) EC: 19.7 (10.1) | EO: 18.2 (24.4) EC: 22.9 (35.8) | EO: 20.9 (9.8) EC: 23.5 (22.8) | |||||||||
| Tot path length (mm) | EO: 309.5 (137.0) EC: 382.0 (85.6) | 252.1 (170.7) EC: 392.0 (201.6) | EO: 362.0 (486.4) EC: 456.3 (714.3) | EO: 416.3 (194.8) EC: 468.5 (454.5) | |||||||||
| Selective visual attention evaluation (Go/No go task reaction | time (ms) | 569.5 (205) | 557 (179) | 568 (146) | 576 (166) | ||||||||
| (b) | |||||||||||||
| Sr. No | Study Duration | VR System | Outcomes | Participant groups | |||||||||
| [27] | 2 face-to-face sessions per week (45 min. each) for 4 weeks and a home exercise program (HEP) | Headset VR (Oculus Go) (Immersive) | Assessment | Metric | TBI | Non-TBI | |||||||
| B* | PT (after session 8) | B | PT (after session 8) | ||||||||||
| Static balance | Sway score | 88.6 | 93.7 | 88.2 | 91.2 | ||||||||
| p value | N/A | <0.001 | N/A | 0.006 | |||||||||
| (c) | |||||||||||||
| Sr. No | Study Duration | VR System | Outcomes | Participant groups | |||||||||
| [28] | 1 full assessment session (PRE) and 11 tailored training sessions (30–45 min each); Reassessment after session 12 (POST) | Computer Assisted Rehabilitation Environment (CAREN) High-End, the CAREN Base, the V-Gait, the C-Mill (Non-Immersive)) | Assessment | Metric | TBI | ||||||||
| B* | PT (after session 12): | ||||||||||||
| Mini BESTest | mean ± error | 14.83 ± 2.21 | 15.5 ± 2.83 | ||||||||||
| N | 6 | 6 | |||||||||||
| Berg Balance Scale | mean ± error | 26.00 ± 5.94 | 29.00 ± 9.55 | ||||||||||
| N | 5 | 5 | |||||||||||
| 10 Meter Walk Test-DT (10MWT) | (mean ± error) | 0.76 ± 0.14 | 0.75 ± 0.10 | ||||||||||
| N | 5 | 5 | |||||||||||
| Timed Up and Go-DT (TUG) | mean ± error | 18.52 ± 3.21 | 17.16 ± 1.97 | ||||||||||
| N | 5 | 5 | |||||||||||
| Four Square Step Test (FSST) | mean ± error | 19.13 ± 6.32 | 15.36 ± 4.87 | ||||||||||
| N | 2 | 2 | |||||||||||
| [29] | Total 15 training sessions (2x/week for 8 weeks) | Nintendo Wii Fit (Non-Immersive) | Outcomes | TBI, stroke, tumor (Intervention group) | TBI, stroke, tumor (control group) | ||||||||
| Assessment | Metric | B* | PT (after session 15) | B* | PT (after session 15) | ||||||||
| Berg Balance Scale (BBS) | Score | 42.10 +/− 9.36 | 48.10 +/− 7.18 | 47.00 +/− 8.52 | 48.35 +/− 7.71 | ||||||||
| 10-Meter Walk Test (10MWT) Walking Speed (m/s) | Speed (m/s) | Regular speed: 1.54 +/− 0.50 Fast speed: 1.21 +/− 0.50 | Regular speed: 1.29 +/− 0.41 Fast speed: 1.06 +/− 0.40 | Regular speed: 1.30 +/− 0.51 Fast speed: 1.03 +/− 0.38 | Regular Speed: 1.25 ± 0.54 Fast Speed: 0.96 ± 0.32 | ||||||||
| Activity-Specific Balance Confidence (ABC) | Score | 55.95 +/− 22.74 | 69.76 +/− 20.98 | 64.99 ± 29.82 | 66.10 ± 27.87 | ||||||||
| (d) | |||||||||||||
| Sr. No | Study Duration | VR System | Outcomes | Participant groups | |||||||||
| [30] | Baseline phase (12 weeks); Intervention phase (8 weeks); Retention period (4 weeks) | Xbox One® and Kinect® sensor (Microsoft, Redmond WA, USA), 45″ Samsung television (Non-Immersive) | Assessment | Metric | TBI | ||||||||
| B* | I* | R* | |||||||||||
| Limits of Stability (LOS) (end-point excursion (EPE)) | (Mean and SD) | Front: 67.3 (SD = 10.2) Right: 69.4 (SD = 6.1) Back: 74.1 (SD = 5.4) Left: 75.0 (SD = 5.7) | Front: 69.9 (SD = 6.5) Right: 70.5 (SD = 8.6) Back: 84.6 (SD = 13.0) Left: 79.3 (SD = 12.1) | Front: 80.2 (SD = 10.5) Right: 70.0 (SD = 2.9) Back: 78.1 (SD = 9.6) Left: 73.5 (SD = 6.8) | |||||||||
| Limits of Stability (LOS) (maximal excursion (MXE)) | (Mean and SD) | Front: 98.5 (SD = 8.6) Right: 94.2 (SD = 6.9) Back: 100.1 (SD = 7.6) Left: 99.8 (SD = 8.5) | Front: 99.7 (SD = 5.3) Right: 98.7 (SD = 6.3) Back: 108.3 (SD = 7.2) Left: 101.8 (SD = 7.8) | Front: 107.0 (SD = 3.8) Right: 100.4 (SD = 2.9) Back: 106.6 (SD = 10.7) Left: 107.0 (SD = 6.7) | |||||||||
| Limits of Stability (LOS) directional control (DCL) (Mean and SD) | (Mean and SD) | Front: 67.33 (SD = 5.8) Right: 55.02 (SD = 11.3) Back: 50.5 (SD = 8.6) Left: 68.3 (SD = 4.3) | Front: 74.2 (SD = 4.8) Right: 66.8 (SD = 8.6) Back: 59.1 (SD = 3.0) Left: 73.1 (SD = 3.6) | Front: 67.5 (SD = 7.5) Right: 64.2 (SD = 9.4) Back: 60.5 (SD = 10.4) Left: 68.5 (SD = 4.5) | |||||||||
| Functional reach test (FRT) | (Mean and SD) | Condition 1 Both palms: 28.9 (SD = 2.9) Condition 2 Left palm: 37.0 (SD = 2.3) Condition 3 Right palm: 36.6 (SD = 1.9) | Condition 1 Both palms: 28.9 (SD = 1.9) Condition 2 Left palm: 36.8 (SD = 1.0) Condition 3 Right palm: 37.5 (SD = 2.0) | Condition 1 Both palms: 26.9 (SD = 1.6) Condition 2 Left palm: 34.7 (SD = 1.4) Condition 3 Right palm: 36.0 (SD = 2.0) | |||||||||
| Dynamic Gait Index (DGI) | (Mean and SD) | 11.8 (SD = 0.4) | 16.2 (SD = 2.3) | 19 (SD = 0.0) | |||||||||
| [31] | 20 min. of VR-based training and 30 min. of general physical therapy (5×week for 8 weeks) | Treadmill (Quasar Med, Nussdorf am Inn, Germany), Oculus Rift VR device, smart insoles (R-C-SPO-Pedisol250, Pedisol, Korea) (Immersive) | Assessment | Metric | TBI | ||||||||
| Baseline | PT (8 Weeks) | ||||||||||||
| BioRescue | COP and LOS | COP: 35.62 cm LOS: 6625.62 cm2 | COP: 32.67 cm LOS: 7123.52 cm2 | ||||||||||
| Gait Ability | measured by GAITRite | ASL (cm): 32.96 SL (cm): 67.66 ASS (%): 25.67 Cadence (step/second): 72 | ASL (cm): 41.59 SL (cm): 75.12 ASS (%): 32.12 Cadence (step/second): 82 | ||||||||||
| Activity Function | measured by Fugl–Meyer Assessment (FMA) | FMA: 18 | FMA: 23 | ||||||||||
| (e) | |||||||||||||
| Sr. No | Study Duration | VR System | Outcomes | Participant groups | |||||||||
| [32] | Average of 6 sessions (SD = 1.3); Maximum = 8; minimum = 3. | HTC Vive (Immersive) | Assessment | Metric | TBI | ||||||||
| B* | PT* | ||||||||||||
| 8-foot up and go (8FUG) | (Mean) | 6.85 s | 5.94 s | ||||||||||
| Activities-Specific Balance Confidence | (ABC) Scale (%) | Improvement on the ABC scale between B* and PT* was 8.3 (SD = 9.03)% | |||||||||||
| Visual Vertigo Analogue Scale | (VVAS) cm | Improvement on the VVAS scale between B* and PT* was 19.8 (SD = 25.03)cm | |||||||||||
| Cohort study | |||||||||||||
| [33] | One session | Wii Balance Board (WBB), 60 in. (75 cm high × 134 cm wide) television (Non-Immersive) | Postural assessment | COP sway area, p values | TBI | Non-TBI | |||||||
| A significant effect of number of mTBI was found in the postural assessment (p = 0.002). Participants with more than one mTBI produced the greatest COP sway area on DYN-Foam. | Patients with no mTBI history produced greater COP sway area on EC-Foam, EO-Foam, and EO, EC, DYN Firm. | ||||||||||||
| (f) | |||||||||||||
| Sr. No | Study Duration | VR System | Outcomes | Participant groups | |||||||||
| [34] | 1 session; clinical tests = 1.5 h and CAREN = 2 h | Computer-Assisted Rehabilitation Environment (CAREN) system (Non-Immersive) | Assessment | Metric | TBI+ Healthy participants | ||||||||
| Balance Evaluation Systems Test (BESTest) | N/A | Insensitive and non-specific | |||||||||||
| Berg Balance Scale (BBS) | N/A | Insensitive and non-specific | |||||||||||
| Dynamic Gait Index (DGI) | N/A | Insensitive and non-specific | |||||||||||
| High-Level Mobility Assessment Tool (HiMAT) | N/A | Insensitive and non-specific | |||||||||||
| Activities-Specific Balance Confidence (ABC) Scale | N/A | Results not presented clearly | |||||||||||
| Sensorimotor Perturbations (standing and walking) | N/A | Discriminative capabilities: Standing avg. ≈ 0.65 Walking avg. ≈ 0.90 | |||||||||||
| Dix–Hallpike Maneuver | N/A | Results not presented clearly | |||||||||||
| [35] | 1 session | Wii Balance Board and a large flat screen (Non-Immersive) | Assessment | Metric | TBI+ Healthy participants | ||||||||
| Virtual Environment TBI Screen (VETS) COP sway area | Virtual Environment TBI Screen | Accuracy: 91.0% ROC curve with AUC = 0.865, p < 0.001 | |||||||||||
| Neurocom Sensory Organization Test | Accuracy: 84.0% ROC curve with AUC, p = 0.034 | ||||||||||||
| [36] | 1 session | Head Rehab VR System (Non-Immersive) | Assessment | Metric | TBI+ Healthy participants | ||||||||
| The Balance Error Scoring System (BESS) | Sensitivity, Specificity, AUC | Sensitivity: 85.7% Specificity of 87.8% (cutoff score = 8.25). The AUC = 0.862 (95% CI; 0.767–0.958) | |||||||||||
| [37] | 1 session | Wii Balance Board, 60″ (75 cm high × 134 cm wide) television (Non-Immersive) | Assessment | Metric | TBI+ Healthy participants | ||||||||
| DYN-Firm, EO-Foam, EC-Foam, DYN-Foam) | A single forward conditional regression model | Accuracy: 94.4% AUC = 0.998, p < 0.001 Sensitivity: 100% Specificity: 93.1%. | |||||||||||
| Balance Error Scoring System | (BESS) | r = –0.15, p = 0.21 | |||||||||||
| [38] | 1 session | Wii Balance Board [WBB], 60-inch [75 cm high × 134 cm wide] television (Non-Immersive) | Assessment | Metric | TBI+ non-TBI | ||||||||
| Virtual Environment TBI Screening (VETS) | (COP sway area, conditions = EO-Firm, EC-Firm, DYN-Firm, EO-Foam, EC-Foam, DYN-Foam) | The mTBI+ group had greater COP sway area during DYN-Foam than the mTBI- group. Across all VETS conditions, the mTBI1+ group generally had increased COP sway compared to the mTBI1 and mTBI- groups. | |||||||||||
| [39] | 4-week program | Computer-Assisted Rehabilitation Environment (CAREN) system (Non-Immersive) | Assessment | Metric | TBI | ||||||||
| Balance Balls VE | AUC; p value | Balance Balls AUC = 0.618 (p = 0.007). | |||||||||||
| Balance Cubes VE (Static and PM) | AUC; p value | Balance Cubes—Static AUC = 0.664 (p < 0.001). Balance Cubes—PM AUC = 0.688 (p < 0.001). | |||||||||||
| [40] | 1 session | BioVRSea (Immersive) | Assessment | Metric | TBI+ non-TBI | ||||||||
| COP sway area | Accuracy | Using machine learning and combining SCAT5 and BioVRSea parameters can classify concussion and non-concussion with an accuracy of up to 95.5%. | |||||||||||
| Sr. No | Type of Study | Total Studies | TBI Sample Size | Gender (TBI) | Age (TBI) (Mean SD) | |
|---|---|---|---|---|---|---|
| Male | Female | |||||
| 1 | Randomized Controlled Trials | 3 | 115 | 75 | 40 | 41.4 ± 2.77 |
| 2 | One-Arm Experimental Study | 1 | 30 | N/A | N/A | 20.2 ± 1.46 |
| 3 | Retrospective Studies | 2 | 30 | 13 | 18 | 55.4 ± 0.2 |
| 4 | Case Studies | 2 | 2 | 2 | 0 | 47.5 ± 0 |
| 5 | Feasibility/Usability Study | 1 | 2 | N/A | N/A | N/A |
| 6 | Cohort Study | 1 | 14 | N/A | N/A | 25.95 ± 4.48 |
| 7 | Diagnostic (Validation) Studies | 7 | 334 | 220 * | 73 | 39.61 ± 7.0 |
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Georges, A.; Joe, M.D. Traumatic Brain Injury; StatPearls: Treasure Island, FL, USA, 2023. [Google Scholar]
- Traumatic Brain Injury. Available online: https://www.alz.org/alzheimers-dementia/what-is-dementia/related_conditions/traumatic-brain-injury (accessed on 22 August 2023).
- Tenovuo, O.; Diaz-Arrastia, R.; Goldstein, L.E.; Sharp, D.J.; Van Der Naalt, J.; Zasler, N.D. Assessing the Severity of Traumatic Brain Injury—Time for a Change? J. Clin. Med. 2021, 10, 148. [Google Scholar] [CrossRef]
- Holm, L.; Cassidy, J.D.; Carroll, L.; Borg, J. Summary of the WHO Collaborating Centre for Neurotrauma Task Force on Mild Traumatic Brain Injury. J. Rehabil. Med. 2005, 37, 137–141. [Google Scholar] [CrossRef]
- Belanger, H.G.; Curtiss, G.; Demery, J.A.; Lebowitz, B.K.; Vanderploeg, R.D. Factors moderating neuropsychological outcomes following mild traumatic brain injury: A meta-analysis. J. Int. Neuropsychol. Soc. 2005, 11, 215–227. [Google Scholar] [CrossRef]
- Corrigan, J.D.; Cuthbert, J.P.; Harrison-Felix, C.; Whiteneck, G.G.; Bell, J.M.; Miller, A.C.; Coronado, V.G.; Pretz, C.R. US Population Estimates of Health and Social Outcomes 5 Years After Rehabilitation for Traumatic Brain Injury. J. Head Trauma Rehabil. 2014, 29, E1–E9. [Google Scholar] [CrossRef]
- Langlois, J.A.; Rutland-Brown, W.; Wald, M.M. The Epidemiology and Impact of Traumatic Brain Injury: A Brief Overview. J. Head Trauma Rehabil. 2006, 21, 375–378. [Google Scholar] [CrossRef]
- Peterson, M.; Greenwald, B.D. Balance problems after traumatic brain injury. Arch. Phys. Med. Rehabil. 2015, 96, 379–380. [Google Scholar] [CrossRef]
- Basford, J.R.; Chou, L.-S.; Kaufman, K.R.; Brey, R.H.; Walker, A.; Malec, J.F.; Moessner, A.M.; Brown, A.W. An assessment of gait and balance deficits after traumatic brain injury. Arch. Phys. Med. Rehabil. 2003, 84, 343–349. [Google Scholar] [CrossRef]
- Row, J.; Chan, L.; Damiano, D.; Shenouda, C.N.; Collins, J.; Zampieri, C. Balance Assessment in Traumatic Brain Injury: A Comparison of the Sensory Organization and Limits of Stability Tests. J. Neurotrauma 2019, 36, 2435–2442. [Google Scholar] [CrossRef]
- Cuthbert, J.P.; Staniszewski, K.; Hays, K.; Gerber, D.; Natale, A.; O’dell, D. Virtual reality-based therapy for the treatment of balance deficits in patients receiving inpatient rehabilitation for traumatic brain injury. Brain Inj. 2014, 28, 181–188. [Google Scholar] [CrossRef]
- Klatt, B.N.; Carender, W.J.; Lin, C.C.; Alsubaie, S.F.; Kinnaird, C.R.; Sienko, K.H.; Whitney, S.L. A Conceptual Framework for the Progression of Balance Exercises in Persons with Balance and Vestibular Disorders. Phys. Med. Rehabil. Int. 2015, 2, 1044. [Google Scholar]
- Marklund, N.; Bellander, B.; Godbolt, A.K.; Levin, H.; McCrory, P.; Thelin, E.P. Treatments and rehabilitation in the acute and chronic state of traumatic brain injury. J. Intern. Med. 2019, 285, 608–623. [Google Scholar] [CrossRef]
- Chen, J.C.; Shaw, F.Z. Progress in sensorimotor rehabilitative physical therapy programs for stroke patients. World J. Clin. Cases 2014, 2, 316–326. [Google Scholar] [CrossRef]
- Adamovich, S.V.; Fluet, G.G.; Tunik, E.; Merians, A.S. Sensorimotor training in virtual reality: A review. NeuroRehabilitation 2009, 25, 29–44. [Google Scholar] [CrossRef]
- Fusco, A.; Giovannini, S.; Castelli, L.; Coraci, D.; Gatto, D.M.; Reale, G.; Pastorino, R.; Padua, L. Virtual Reality and Lower Limb Rehabilitation: Effects on Motor and Cognitive Outcome—A Crossover Pilot Study. J. Clin. Med. 2022, 11, 2300. [Google Scholar] [CrossRef]
- Rizzo, A.A.; Schultheis, M.; Kerns, K.A.; Mateer, C. Analysis of assets for virtual reality applications in neuropsychology. Neuropsychol. Rehabil. 2004, 14, 207–239. [Google Scholar] [CrossRef]
- aples-Keller, J.L.; Bunnell, B.E.; Kim, S.-J.B.; Rothbaum, B.O. The Use of Virtual Reality Technology in the Treatment of Anxiety and Other Psychiatric Disorders. Harv. Rev. Psychiatry 2017, 25, 103–113. [Google Scholar] [CrossRef]
- Rizzo, A.; Kim, G. A SWOT Analysis of the Field of Virtual Rehabilitation and Therapy. Presence 2005, 14, 119–146. [Google Scholar] [CrossRef]
- Ventura, S.; Brivio, E.; Riva, G.; Baños, R.M. Immersive Versus Non-immersive Experience: Exploring the Feasibility of Memory Assessment Through 360° Technology. Front. Psychol. 2019, 10, 479119. [Google Scholar] [CrossRef]
- Cipresso, P.; Giglioli, I.A.C.; Raya, M.A.; Riva, G. The Past, Present, and Future of Virtual and Augmented Reality Research: A Network and Cluster Analysis of the Literature. Front. Psychol. 2018, 9, 309500. [Google Scholar] [CrossRef]
- Alashram, A.R.; Padua, E.; Annino, G. Virtual reality for balance and mobility rehabilitation following traumatic brain injury: A systematic review of randomized controlled trials. J. Clin. Neurosci. 2022, 105, 115–121. [Google Scholar] [CrossRef]
- Ma, L.L.; Wang, Y.Y.; Yang, Z.H.; Huang, D.; Weng, H.; Zeng, X.T. Methodological quality (risk of bias) assessment tools for primary and secondary medical studies: What are they and which is better? Mil. Med. Res. 2020, 7, 7. [Google Scholar] [CrossRef] [PubMed]
- Tefertiller, C.; Ketchum, J.M.; Bartelt, P.; Peckham, M.; Hays, K. Feasibility of virtual reality and treadmill training in traumatic brain injury: A randomized controlled pilot trial. Brain Inj. 2022, 36, 898–908. [Google Scholar] [CrossRef] [PubMed]
- Tefertiller, C.; Hays, K.; Natale, A.; O’dell, D.; Ketchum, J.; Sevigny, M.; Eagye, C.; Philippus, A.; Harrison-Felix, C. Results From a Randomized Controlled Trial to Address Balance Deficits After Traumatic Brain Injury. Arch. Phys. Med. Rehabil. 2019, 100, 1409–1416. [Google Scholar] [CrossRef] [PubMed]
- Straudi, S.; Severini, G.; Charabati, A.S.; Pavarelli, C.; Gamberini, G.; Scotti, A.; Basaglia, N. The effects of video game therapy on balance and attention in chronic ambulatory traumatic brain injury: An exploratory study. BMC Neurol. 2017, 17, 86. [Google Scholar] [CrossRef] [PubMed]
- Reneker, J.C.; Babl, R.; Pannell, W.C.; Adah, F.; Flowers, M.M.; Curbow-Wilcox, K.; Lirette, S. Sensorimotor training for injury prevention in collegiate soccer players: An experimental study. Phys. Ther. Sport. 2019, 40, 184–192. [Google Scholar] [CrossRef] [PubMed]
- Porras, D.C.; Sharon, H.; Inzelberg, R.; Ziv-Ner, Y.; Zeilig, G.; Plotnik, M. Advanced virtual reality-based rehabilitation of balance and gait in clinical practice. Ther. Adv. Chronic Dis. 2019, 10, 2040622319868379. [Google Scholar]
- Kwon, J.-A.; Shin, Y.-K.; Kim, D.-J.; Cho, S.-R. Effects of Balance Training Using a Virtual Reality Program in Hemiplegic Patients. Int. J. Environ. Res. Public. Health 2022, 19, 2805. [Google Scholar] [CrossRef]
- Chanpimol, S.; Seamon, B.; Hernandez, H.; Harris-Love, M.; Blackman, M.R. Using Xbox kinect motion capture technology to improve clinical rehabilitation outcomes for balance and cardiovascular health in an individual with chronic TBI. Arch. Physiother. 2017, 7, 6. [Google Scholar] [CrossRef]
- Kim, K.H.; Kim, D.H. Improved Balance, Gait, and Lower Limb Motor Function in a 58-Year-Old Man with Right Hemiplegic Traumatic Brain Injury Following Virtual Reality-Based Real-Time Feedback Physical Therapy. Am. J. Case Rep. 2023, 24, e938803. [Google Scholar] [CrossRef]
- Lubetzky, A.V.; Kelly, J.; Wang, Z.; Gospodarek, M.; Fu, G.; Sutera, J.; Hujsak, B.D. Contextual sensory integration training via head mounted display for individuals with vestibular disorders: A feasibility study. Disabil. Rehabil. Assist. Technol. 2022, 17, 74–84. [Google Scholar] [CrossRef]
- Wright, W.G.; Handy, J.D.; Avcu, P.; Ortiz, A.; Haran, F.J.; Doria, M.; Servatius, R.J. Healthy Active Duty Military with Lifetime Experience of Mild Traumatic Brain Injury Exhibits Subtle Deficits in Sensory Reactivity and Sensory Integration During Static Balance. Mil. Med. 2018, 183 (Suppl. S1), 313–320. [Google Scholar] [CrossRef] [PubMed]
- Rao, H.M.; Talkar, T.; Ciccarelli, G.; Nolan, M.; O’Brien, A.; Vergara-Diaz, G.; Sherrill, D.; Zafonte, R.; Palmer, J.S.; Quatieri, T.F.; et al. Sensorimotor conflict tests in an immersive virtual environment reveal subclinical impairments in mild traumatic brain injury. Sci. Rep. 2020, 10, 14773. [Google Scholar] [CrossRef] [PubMed]
- Wright, W.G.; McDevitt, J.; Tierney, R.; Haran, F.J.; Appiah-Kubi, K.O.; Dumont, A. Assessing subacute mild traumatic brain injury with a portable virtual reality balance device. Disabil. Rehabil. 2017, 39, 1564–1572. [Google Scholar] [CrossRef] [PubMed]
- Teel, E.F.; Gay, M.R.; Arnett, P.A.; Slobounov, S.M. Differential Sensitivity Between a Virtual Reality Balance Module and Clinically Used Concussion Balance Modalities. Clin. J. Sport. Med. 2016, 26, 162–166. [Google Scholar] [CrossRef]
- Wright, W.G.; Tierney, R.T.; McDevitt, J. Visual-vestibular processing deficits in mild traumatic brain injury. J. Vestib. Res. 2017, 27, 27–37. [Google Scholar] [CrossRef] [PubMed]
- Wright, W.G.; Handy, J.D.; Haskell, A.; Servatius, L.; Servatius, R.J. History of Mild Traumatic Brain Injury Affects Static Balance under Complex Multisensory Manipulations. J. Neurotrauma 2022, 39, 821–828. [Google Scholar] [CrossRef] [PubMed]
- Onakomaiya, M.M.; Kruger, S.E.; Highland, K.B.; Kodosky, P.N.; Pape, M.M.; Roy, M.J. Expanding Clinical Assessment for Traumatic Brain Injury and Comorbid Post-Traumatic Stress Disorder: A Retrospective Analysis of Virtual Environment Tasks in the Computer-Assisted Rehabilitation Environment. Mil. Med. 2017, 182, 128–136. [Google Scholar] [CrossRef]
- Jacob, D.; Kristensen, I.S.U.; Aubonnet, R.; Recenti, M.; Donisi, L.; Ricciardi, C.; Svansson, H.R.; Agnarsdóttir, S.; Colacino, A.; Jónsdóttir, M.K.; et al. Towards defining biomarkers to evaluate concussions using virtual reality and a moving platform (BioVRSea). Sci. Rep. 2022, 12, 8996. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hernan, G.; Ingale, N.; Somayaji, S.; Veerubhotla, A. Virtual Reality-Based Interventions to Improve Balance in Patients with Traumatic Brain Injury: A Scoping Review. Brain Sci. 2024, 14, 429. https://doi.org/10.3390/brainsci14050429
Hernan G, Ingale N, Somayaji S, Veerubhotla A. Virtual Reality-Based Interventions to Improve Balance in Patients with Traumatic Brain Injury: A Scoping Review. Brain Sciences. 2024; 14(5):429. https://doi.org/10.3390/brainsci14050429
Chicago/Turabian StyleHernan, Gabriel, Neha Ingale, Sujith Somayaji, and Akhila Veerubhotla. 2024. "Virtual Reality-Based Interventions to Improve Balance in Patients with Traumatic Brain Injury: A Scoping Review" Brain Sciences 14, no. 5: 429. https://doi.org/10.3390/brainsci14050429
APA StyleHernan, G., Ingale, N., Somayaji, S., & Veerubhotla, A. (2024). Virtual Reality-Based Interventions to Improve Balance in Patients with Traumatic Brain Injury: A Scoping Review. Brain Sciences, 14(5), 429. https://doi.org/10.3390/brainsci14050429





