The Efficacy of Cognitive Remediation Therapy for Anorexia Nervosa: A Systematic Review of Systematic Reviews
Abstract
1. Introduction
2. Materials and Methods
2.1. Literature Search
2.2. Inclusion and Exclusion Criteria
2.3. Selection Process
2.4. Data Extraction
2.5. The Assessment of the Risk of Bias
2.6. Data Analysis and Synthesis
3. Results
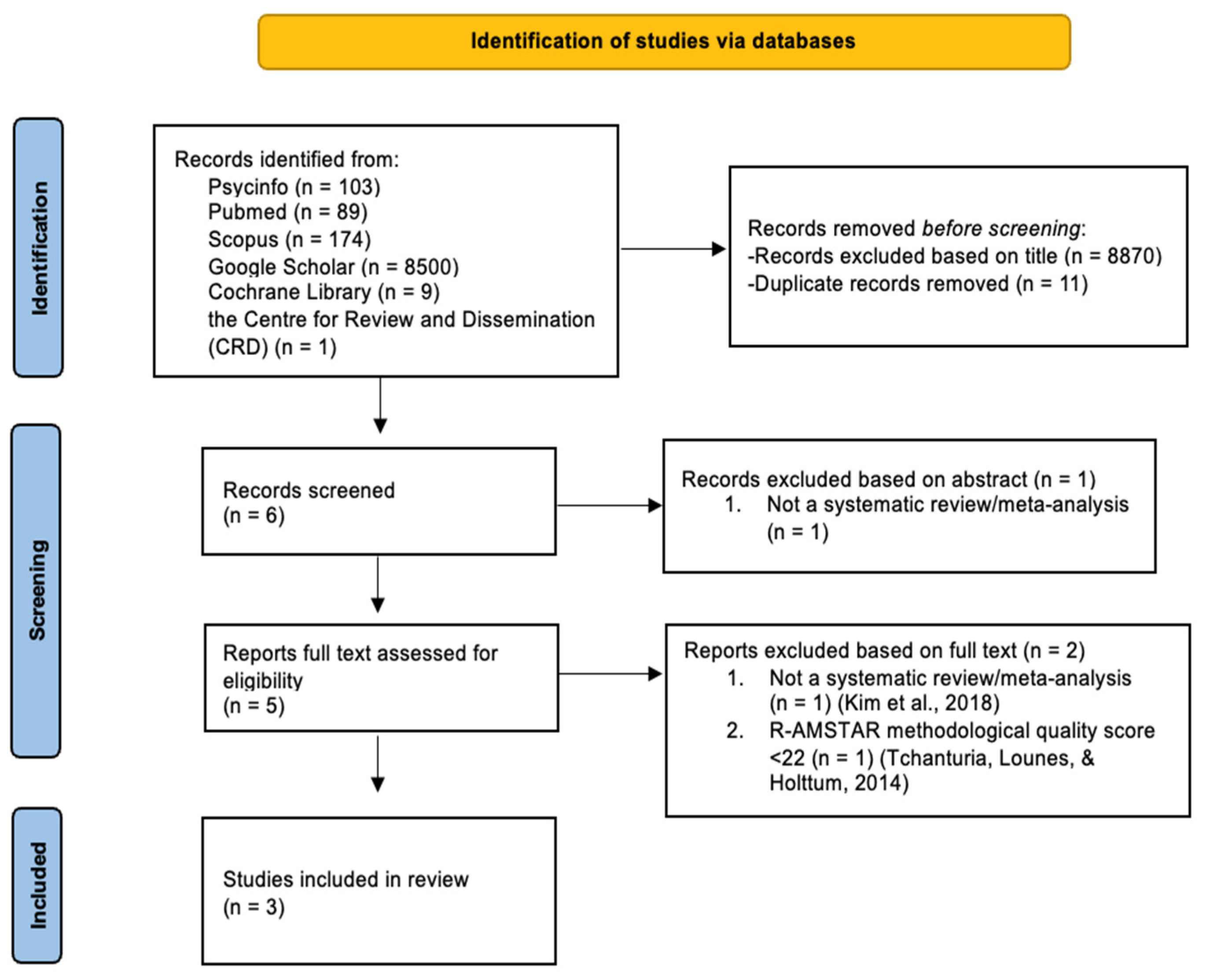
3.1. Study Selection
3.2. The Characteristics of the Included Studies
3.3. The Methodological Quality of Included Reviews
3.4. Single Cases
3.5. Case Series
3.6. Randomized Control Trials (RCTs)
3.7. Qualitative Studies
4. Discussion
5. Strengths and Limitations
6. Suggestions and Implications for Future Research
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. Target Studies Included in Each Selected Systematic Review/Meta-Analysis
| Dahlgren (2014) [38] | Hagan (2020) [20] | Tchanturia (2017) [21] | |
| Abbate-Daga (2012) [53] | X | ||
| Brockmeyer (2013) [40] | X | X | |
| Dahlgren (2013) [46] | X | X | |
| Davies (2005) [63] | X | ||
| Dingemans (2014) [41] | X | X | |
| Easter (2011) [52] | X | ||
| Genders (2010) [58] | X | ||
| Giombini (2016) [29] | X | ||
| Giombini (2017) [29] | X | ||
| Harrison (2018) [28] | X | ||
| Herbrich (2017) [42] | X | X | |
| Lask (2013) [62] | X | ||
| Lock (2013) [43] | X | X | |
| Lock (2018) [59] | X | ||
| Pitt (2010) [56] | X | ||
| Pretorius (2007) [64] | X | ||
| Pretorius (2012) [44] | X | X | |
| Sproch (2019) [26] | X | ||
| Steinglass (2014) [45] | X | X | |
| Tchanturia (2006) [65] | X | ||
| Tchanturia (2007) [57] | X | ||
| Tchanturia (2008) [54] | X | ||
| van Noort (2015) [47] | X | ||
| van Noort (2016) [66] | X | ||
| van Passel (2020) [61] | X | ||
| Whitney (2008) [51] | X | ||
| Wood (2011) [49] | X | ||
| Zuchova (2013) [50] | X |
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5; American Psychiatric Association: Washington, DC, USA, 2013; Volume 5. [Google Scholar]
- van Eeden, A.E.; van Hoeken, D.; Hoek, H.W. Incidence, prevalence and mortality of anorexia nervosa and bulimia nervosa. Curr. Opin. Psychiatry 2021, 34, 515–524. [Google Scholar] [CrossRef] [PubMed]
- Godier, L.R.; Park, R.J. Compulsivity in anorexia nervosa: A transdiagnostic concept. Front. Psychol. 2014, 5, 778. [Google Scholar] [CrossRef] [PubMed]
- Fairburn, C.G. Evidence-based treatment of anorexia nervosa. Int. J. Eat. Disord. 2005, 37, S26–S30. [Google Scholar] [CrossRef] [PubMed]
- Dejong, H.; Broadbent, H.; Schmidt, U. A systematic review of dropout from treatment in outpatients with anorexia nervosa. Int. J. Eat. Disord. 2012, 45, 635–647. [Google Scholar] [CrossRef] [PubMed]
- Halmi, K.A.; Agras, W.S.; Crow, S.; Mitchell, J.; Wilson, G.T.; Bryson, S.W.; Kraemer, H.C. Predictors of Treatment Acceptance and Completion in Anorexia Nervosa: Implications for Future Study Designs. Arch. Gen. Psychiatry 2005, 62, 776–781. [Google Scholar] [CrossRef]
- Di Lodovico, L.; Gorwood, P. The relationship between moderate to vigorous physical activity and cognitive rigidity in anorexia nervosa. Psychiatry Res. 2019, 284, 112703. [Google Scholar] [CrossRef]
- Murray, S.B.; Quintana, D.S.; Loeb, K.L.; Griffiths, S.; Le Grange, D. Treatment outcomes for anorexia nervosa: A systematic review and meta-analysis of randomized controlled trials. Psychol. Med. 2019, 49, 535–544. [Google Scholar] [CrossRef]
- Zeeck, A.; Herpertz-Dahlmann, B.; Friederich, H.C.; Brockmeyer, T.; Resmark, G.; Hagenah, U.; Ehrlich, S.; Cuntz, U.; Zipfel, S.; Hartmann, A. Psychotherapeutic Treatment for Anorexia Nervosa: A Systematic Review and Network Meta-Analysis. Front. Psychiatry 2018, 9, 158. [Google Scholar] [CrossRef]
- Miles, S.; Gnatt, I.; Phillipou, A.; Nedeljkovic, M. Cognitive flexibility in acute anorexia nervosa and after recovery: A systematic review. Clin. Psychol. Rev. 2020, 81, 101905. [Google Scholar] [CrossRef]
- Dann, K.M.; Hay, P.; Touyz, S. Are poor set-shifting and central coherence associated with everyday function in anorexia nervosa? A systematic review. J. Eat. Disord. 2021, 9, 40. [Google Scholar] [CrossRef]
- Fuglset, T.S. Is set-shifting and central coherence in anorexia nervosa influenced by body mass index, anxiety or depression? A systematic review. BMC Psychiatry 2021, 21, 137. [Google Scholar] [CrossRef] [PubMed]
- Keegan, E.; Tchanturia, K.; Wade, T.D. Central coherence and set-shifting between nonunderweight eating disorders and anorexia nervosa: A systematic review and meta-analysis. Int. J. Eat. Disord. 2020, 54, 229–243. [Google Scholar] [CrossRef] [PubMed]
- Brockmeyer, T.; Febry, H.; Leiteritz-Rausch, A.; Wünsch-Leiteritz, W.; Leiteritz, A.; Friederich, H.-C. Cognitive flexibility, central coherence, and quality of life in anorexia nervosa. J. Eat. Disord. 2022, 10, 22. [Google Scholar] [CrossRef] [PubMed]
- Solmi, M.; Wade, T.D.; Byrne, S.; Del Giovane, C.; Fairburn, C.G.; Ostinelli, E.G.; De Crescenzo, F.; Johnson, C.; Schmidt, U.; Treasure, J.; et al. Comparative efficacy and acceptability of psychological interventions for the treatment of adult outpatients with anorexia nervosa: A systematic review and network meta-analysis. Lancet Psychiatry 2021, 8, 215–224. [Google Scholar] [CrossRef] [PubMed]
- Williams, R.; Smith, M.; Wright, D. Anorexia: A literature review of young people’s experiences of hospital treatment. Nurs. Child. Young-People 2020, 33, 10–17. [Google Scholar] [CrossRef]
- Fuglset, T.S. Set-shifting, central coherence and decision-making in individuals recovered from anorexia nervosa: A systematic review. J. Eat. Disord. 2019, 7, 22. [Google Scholar] [CrossRef]
- Tenconi, E.; Collantoni, E.; Meregalli, V.; Bonello, E.; Zanetti, T.; Veronese, A.; Meneguzzo, P.; Favaro, A. Clinical and Cognitive Functioning Changes After Partial Hospitalization in Patients with Anorexia Nervosa. Front. Psychiatry 2021, 12, 653506. [Google Scholar] [CrossRef]
- Tchanturia, K.; Harrison, A.; Davies, H.; Roberts, M.; Oldershaw, A.; Nakazato, M.; Stahl, D.; Morris, R.; Schmidt, U.; Treasure, J. Cognitive Flexibility and Clinical Severity in Eating Disorders. PLoS ONE 2011, 6, e20462. [Google Scholar] [CrossRef]
- Hagan, K.E.; Christensen, K.A.; Forbush, K.T. A preliminary systematic review and meta-analysis of randomized-controlled trials of cognitive remediation therapy for anorexia nervosa. Eat. Behav. 2020, 37, 101391. [Google Scholar] [CrossRef]
- Tchanturia, K.; Giombini, L.; Leppanen, J.; Kinnaird, E. Evidence for Cognitive Remediation Therapy in Young People with Anorexia Nervosa: Systematic Review and Meta-analysis of the Literature. Eur. Eat Disord. Rev. 2017, 25, 227–236. [Google Scholar] [CrossRef]
- Tchanturia, K.; Davies, H.; Reeder, C.; Wykes, T. Cognitive Remediation Programme for Anorexia Nervosa: A Manual for Practitioners; NHS Foundation Trust: London, UK, 2008. [Google Scholar]
- Dandil, Y.; Baillie, C.; Tchanturia, K. Cognitive Remediation Therapy as a Feasible Treatment for a Young Person with Anorexia Nervosa and Autism Spectrum Disorder Comorbidity: A Case Study. Clin. Case Stud. 2019, 19, 115–132. [Google Scholar] [CrossRef]
- Herbrich-Bowe, L.; Bentz, L.K.; Correll, C.U.; Kappel, V.; van Noort, B.M. Randomized controlled trial of cognitive remediation therapy in adolescent inpatients with anorexia nervosa: Neuropsychological outcomes. Eur. Eat. Disord. Rev. 2022, 30, 772–786. [Google Scholar] [CrossRef] [PubMed]
- Brockmeyer, T.; Schmidt, H.; Leiteritz-Rausch, A.; Zimmermann, J.; Wünsch-Leiteritz, W.; Leiteritz, A.; Friederich, H.-C. Cognitive remediation therapy in anorexia nervosa—A randomized clinical trial. J. Consult. Clin. Psychol. 2021, 89, 805–815. [Google Scholar] [CrossRef] [PubMed]
- Sproch, L.E.; Anderson, K.P.; Sherman, M.F.; Crawford, S.F.; Brandt, H.A. A randomized controlled trial of group cognitive remediation therapy for anorexia nervosa: Effects on set-shifting tasks for inpatient adults and adolescents. Int. J. Eat. Disord. 2019, 52, 1004–1014. [Google Scholar] [CrossRef]
- Alvarado-Sánchez, N.; Alvarez-Rayón, G.; Mancilla-Díaz, J.M. Cognitive remediation therapy in Mexico as a treatment for Anorexia Nervosa: A case study. Eat. Disord. 2019, 27, 230–252. [Google Scholar] [CrossRef] [PubMed]
- Harrison, A.; Stavri, P.; Ormond, L.; McEnemy, F.; Akyol, D.; Qureshi, A.; Al-Khairulla, H. Cognitive remediation therapy for adolescent inpatients with severe and complex anorexia nervosa: A treatment trial. Eur. Eat. Disord. Rev. 2018, 26, 230–240. [Google Scholar] [CrossRef]
- Giombini, L.; Moynihan, J.; Turco, M.; Nesbitt, S. Evaluation of individual cognitive remediation therapy (CRT) for the treatment of young people with anorexia nervosa. Eat. Weight Disord. 2017, 22, 667–673. [Google Scholar] [CrossRef]
- Tchanturia, K.; Larsson, E.; Brown, A. Benefits of group cognitive remediation therapy in anorexia nervosa: Case series. Neuropsychiatrie 2016, 30, 42–49. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; A Akl, E.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Huang, X.; Lin, J.; Demner-Fushman, D. Evaluation of PICO as a knowledge representation for clinical questions. AMIA Annu. Symp. Proc. 2006, 2006, 359–363. [Google Scholar]
- Kung, J.; Chiappelli, F.; Cajulis, O.O.; Avezova, R.; Kossan, G.; Chew, L.; Maida, C.A. From Systematic Reviews to Clinical Recommendations for Evidence-Based Health Care: Validation of Revised Assessment of Multiple Systematic Reviews (R-AMSTAR) for Grading of Clinical Relevance. Open Dent. J. 2010, 4, 84–91. [Google Scholar] [CrossRef] [PubMed]
- Smith, V.; Devane, D.; Begley, C.M.; Clarke, M. Methodology in conducting a systematic review of systematic reviews of healthcare interventions. BMC Med. Res. Methodol. 2011, 11, 15. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Prisma Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Int. J. Surg. 2010, 8, 336–341. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.J.; Bahk, Y.-C.; Oh, H.; Lee, W.-H.; Lee, J.-S.; Choi, K.-H. Current Status of Cognitive Remediation for Psychiatric Disorders: A Review. Front. Psychiatry 2018, 9, 461. [Google Scholar] [CrossRef] [PubMed]
- Tchanturia, K.; Lounes, N.; Holttum, S. Cognitive Remediation in Anorexia Nervosa and Related Conditions: A Systematic Review. Eur. Eat. Disord. Rev. 2014, 22, 454–462. [Google Scholar] [CrossRef] [PubMed]
- Lindvall Dahlgren, C.; Ro, O. A systematic review of cognitive remediation therapy for anorexia nervosa—Development, current state and implications for future research and clinical practice. J. Eat Disord. 2014, 2, 26. [Google Scholar] [CrossRef] [PubMed]
- Sorgente, A.; Pietrabissa, G.; Manzoni, G.M.; Re, F.; Simpson, S.; Perona, S.; Rossi, A.; Cattivelli, R.; Innamorati, M.; Jackson, J.B.; et al. Web-Based Interventions for Weight Loss or Weight Loss Maintenance in Overweight and Obese People: A Systematic Review of Systematic Reviews. J. Med. Internet Res. 2017, 19, e229. [Google Scholar] [CrossRef] [PubMed]
- Brockmeyer, T.; Ingenerf, K.; Walther, S.; Wild, B.; Hartmann, M.; Herzog, W.; Bents, H.; Friederich, H. Training cognitive flexibility in patients with anorexia nervosa: A pilot randomized controlled trial of cognitive remediation therapy. Int. J. Eat. Disord. 2013, 47, 24–31. [Google Scholar] [CrossRef]
- Dingemans, A.E.; Danner, U.N.; Donker, J.M.; Aardoom, J.J.; Van Meer, F.; Tobias, K.; Van Elburg, A.A.; Van Furth, E.F. The effectiveness of cognitive remediation therapy in patients with a severe or enduring eating disorder: A randomized controlled trial. Psychother. Psychosom. 2014, 83, 29–36. [Google Scholar] [CrossRef]
- Herbrich, L.; van Noort, B.; Pfeiffer, E.; Lehmkuhl, U.; Winter, S.; Kappel, V. Follow-up Assessment of Cognitive Remediation Therapy in Adolescent Anorexia Nervosa: A Pilot Study. Eur. Eat. Disord. Rev. 2017, 25, 104–113. [Google Scholar] [CrossRef]
- Lock, J.; Agras, W.S.; Fitzpatrick, K.K.; Bryson, S.W.; Jo, B.; Tchanturia, K. Is outpatient cognitive remediation therapy feasible to use in randomized clinical trials for anorexia nervosa? Int. J. Eat. Disord. 2013, 46, 567–575. [Google Scholar] [CrossRef] [PubMed]
- Pretorius, N.; Dimmer, M.; Power, E.; Eisler, I.; Simic, M.; Tchanturia, K. Evaluation of a Cognitive Remediation Therapy Group for Adolescents with Anorexia Nervosa: Pilot Study. Eur. Eat. Disord. Rev. 2012, 20, 321–325. [Google Scholar] [CrossRef] [PubMed]
- Steinglass, J.E.; Albano, A.M.; Simpson, H.B.; Wang, Y.; Zou, J.; Attia, E.; Walsh, B.T. Confronting fear using exposure and response prevention for anorexia nervosa: A randomized controlled pilot study. Int. J. Eat Disord. 2014, 47, 174–180. [Google Scholar] [CrossRef] [PubMed]
- Dahlgren, C.L.; Lask, B.; Landrø, N.I.; Rø, Ø. Neuropsychological functioning in adolescents with anorexia nervosa before and after cognitive remediation therapy: A feasibility trial. Int. J. Eat Disord. 2013, 46, 576–581. [Google Scholar] [CrossRef] [PubMed]
- van Noort, B.M.; Pfeiffer, E.; Lehmkuhl, U.; Kappel, V. Cognitive Remediation Therapy for Children with Anorexia Nervosa. Z. Kinder Jugendpsychiatr Psychother. 2015, 43, 351–355. [Google Scholar] [CrossRef]
- Asch, M.; Esteves, J.; De Hautecloque, D.; Bargiacchi, A.; Le Heuzey, M.F.; Mouren, M.C.; Doyen, C. Cognitive remediation therapy for children and adolescents with anorexia nervosa in France: An exploratory study. Encephale 2014, 40, 240–246. [Google Scholar] [CrossRef]
- Wood, L.; Al-Khairulla, H.; Lask, B. Group cognitive remediation therapy for adolescents with anorexia nervosa. Clin. Child Psychol. Psychiatry 2011, 16, 225–231. [Google Scholar] [CrossRef]
- Zuchova, S.; Erler, T.; Papezova, H. Group cognitive remediation therapy for adult anorexia nervosa inpatients: First experiences. Eat. Weight Disord. 2013, 18, 269–273. [Google Scholar] [CrossRef]
- Whitney, J.; Easter, A.; Tchanturia, K. Service users’ feedback on cognitive training in the treatment of anorexia nervosa: A qualitative study. Int. J. Eat. Disord. 2008, 41, 542–550. [Google Scholar] [CrossRef]
- Easter, A.; Tchanturia, K. Therapists’ experiences of Cognitive Remediation Therapy for anorexia nervosa: Implications for working with adolescents. Clin. Child Psychol. Psychiatry 2011, 16, 233–246. [Google Scholar] [CrossRef]
- Abbate-Daga, G.; Buzzichelli, S.; Marzola, E.; Amianto, F.; Fassino, S. Effectiveness of cognitive remediation therapy (CRT) in anorexia nervosa: A case series. J. Clin. Exp. Neuropsychol. 2012, 34, 1009–1015. [Google Scholar] [CrossRef] [PubMed]
- Tchanturia, K.; Davies, H.; Lopez, C.; Schmidt, U.; Treasure, J.; Wykes, T. Letter to the Editor: Neuropsychological task performance before and after cognitive remediation in anorexia nervosa: A pilot case-series. Psychol. Med. 2008, 38, 1371–1373. [Google Scholar] [CrossRef] [PubMed]
- Dahlgren, C.L.; Lask, B.; Landrø, N.I.; Rø, Ø. Developing and evaluating cognitive remediation therapy (CRT) for adolescents with anorexia nervosa: A feasibility study. Clin. Child Psychol. Psychiatry 2013, 19, 476–487. [Google Scholar] [CrossRef]
- Pitt, S.; Lewis, R.; Morgan, S.; Woodward, D. Cognitive remediation therapy in an outpatient setting: A case series. Eat. Weight. Disord. Stud. Anorex. Bulim. Obes. 2010, 15, e281–e286. [Google Scholar] [CrossRef] [PubMed]
- Tchanturia, K.; Davies, H.; Campbell, I.C. Cognitive remediation therapy for patients with anorexia nervosa: Preliminary findings. Ann. Gen. Psychiatry 2007, 6, 14. [Google Scholar] [CrossRef] [PubMed]
- Genders, R.; Tchanturia, K. Cognitive Remediation Therapy (CRT) for anorexia in group format: A pilot study. Eat. Weight. Disord. Stud. Anorex. Bulim. Obes. 2010, 15, e234–e239. [Google Scholar] [CrossRef]
- Lock, J.; Fitzpatrick, K.K.; Agras, W.S.; Weinbach, N.; Jo, B. Feasibility study combining art therapy or cognitive remediation therapy with family-based treatment for adolescent anorexia nervosa. Eur. Eat. Disord. Rev. 2018, 26, 62–68. [Google Scholar] [CrossRef]
- Giombini, L.; Nesbitt, S.; Waples, L.; Finazzi, E.; Easter, A.; Tchanturia, K. Young people’s experience of individual cognitive remediation therapy (CRT) in an inpatient eating disorder service: A qualitative study. Eat. Weight Disord. 2018, 23, 499–505. [Google Scholar] [CrossRef]
- van Passel, B.; Danner, U.N.; Dingemans, A.E.; Aarts, E.; Sternheim, L.C.; Becker, E.S.; van Elburg, A.A.; van Furth, E.F.; Hendriks, G.J.; Cath, D.C. Cognitive Remediation Therapy Does Not Enhance Treatment Effect in Obsessive-Compulsive Disorder and Anorexia Nervosa: A Randomized Controlled Trial. Psychother. Psychosom. 2020, 89, 228–241. [Google Scholar] [CrossRef]
- Lask, B.; Roberts, A. Family cognitive remediation therapy for anorexia nervosa. Clin. Child Psychol. Psychiatry 2013, 20, 207–217. [Google Scholar] [CrossRef]
- Davies, H.; Tchanturia, K. Cognitive remediation therapy as an intervention for acute anorexia nervosa: A case report. Eur. Eat. Disord. Rev. 2005, 13, 311–316. [Google Scholar] [CrossRef]
- Pretorius, N.; Tchanturia, K. Anorexia nervosa: How people think and how we address it in cognitive remediation therapy. Therapy 2007, 4, 423–432. [Google Scholar] [CrossRef]
- Tchanturia, K.; Whitney, J.; Treasure, J. Can cognitive exercises help treat anorexia nervosa? Eat. Weight. Disord. 2006, 11, e112–e116. [Google Scholar] [CrossRef] [PubMed]
- van Noort, B.M.; Kraus, M.K.A.; Pfeiffer, E.; Lehmkuhl, U.; Kappel, V. Neuropsychological and behavioural short-term effects of cognitive remediation therapy in adolescent anorexia nervosa: A pilot study. Eur. Eat. Disord. Rev. 2016, 24, 69–74. [Google Scholar] [CrossRef]
| First Author (Year) | Country | Aim of the Review | Included Studies | Study Design | Sample Size (n) | Age (Year): Mean (SD) or Range | Women: n or % |
|---|---|---|---|---|---|---|---|
| Dahlgren (2014) [38] | UK | To systematically review studies of CRT for AN and to discuss findings with references to clinical practice and future research | 21 | Single or multiple case studies and RCT | 362 | 12–62 | 355 |
| Hagan (2020) [20] | USA | To determine the effect of CRT for AN in comparison with control treatments in RCTs on neuropsychological deficits at the end of the treatment and to assess the effect of CRT for AN on dropout, related eating disorders, and other psychological outcomes at the end of the treatment | 9 | RCT | 303 | 22.67 (0.37) | 93.9% |
| Tchanturia (2017) [21] | UK | To evaluate the evidence about the efficacy of CRT in children and adolescents with AN | 9 | Single or multiple case studies and qualitative assessments | 367 | 14.97 (0.65) | NR |
| First Author (Year) | N° of Sessions | Frequency of Sessions | Format | Clinical Outcome (Measure) | Psychological Outcome (Measure) | Neuropsychological Outcome (Measure) | |
| Dahlgren (2014) [38] | Between 4 and 30 session | From 1 to 3 times per week | Individual, groups, or systemic | BMI; Calorie intake | Depression; Patients’ experience with CRT; Treatment acceptance | Cognitive flexibility; Cognitive set-shifting; Perfectionism; Rigidity; Reflexive skills; Impulse regulation; Visuospatial memory; Working memory; Verbal fluency; Global information processing; Brixton & CatBat tasks; Executive function (BRIEF-SR) | |
| Hagan (2020) [20] | Between 6 and 36 sessions | From 1 to 3 times per week | Individual or groups | BMI; Range, frequency, and severity of behaviors associated with ED (EDE/EDEQ); Calories consumed during meal | Depression (BDI and DIKJ); Quality of life (EDQoL); Anxiety (STAI(C)-T), ED (ChEDEQ and YBC-EDS); Obsessive and compulsive symptoms (CY-BOCS) | Global processing ability, visuospatial ability, and visuospatial memory (RCFT); Executive functions (D-KEFS CWIT); Cognitive control related to the updating, representation, and maintenance of frequently changing task rules | |
| Tchanturia (2017) [21] | Between 8 and 10 sessions | NR | Individual or groups | NR | Identification and quantification of adaptation patterns (CWT); Aspects of personality and cognitive impairment (GEFT); Motivation (Motivational Ruler); Satisfaction (Satisfaction Questionnaire) | Global processing ability, visuospatial ability, and visuospatial memory (RCFT); Attention (TMT-4); Executive functions (BRIEF-SR, Tower Test, and D-KEFS); Neuropsychological functioning in AN (The Ravello Profile); Cognitive flexibility (CFS) | |
| First Author (Year) | Item 1 | Item 2 | Item 3 | Item 4 | Item 5 | Item 6 | Item 7 | Item 8 | Item 9 | Item 10 | Item 11 | Total Score |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Dahlgren (2014) [38] | 2 | 1 | 4 | 3 | 4 | 4 | 1 | 1 | 1 | 1 | 3 | 25 |
| Hagan (2020) [20] | 2 | 4 | 4 | 2 | 2 | 4 | 3 | 3 | 2 | 3 | 3 | 32 |
| Tchanturia (2014) [37] | 2 | 1 | 4 | 3 | 1 | 4 | 1 | 1 | 1 | 1 | 2 | 21 |
| Tchanturia (2017) [21] | 2 | 3 | 4 | 1 | 2 | 4 | 1 | 1 | 3 | 3 | 1 | 25 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marchesi, G.; Cammisuli, D.M.; Semonella, M.; Castelnuovo, G.; Pietrabissa, G. The Efficacy of Cognitive Remediation Therapy for Anorexia Nervosa: A Systematic Review of Systematic Reviews. Brain Sci. 2024, 14, 118. https://doi.org/10.3390/brainsci14020118
Marchesi G, Cammisuli DM, Semonella M, Castelnuovo G, Pietrabissa G. The Efficacy of Cognitive Remediation Therapy for Anorexia Nervosa: A Systematic Review of Systematic Reviews. Brain Sciences. 2024; 14(2):118. https://doi.org/10.3390/brainsci14020118
Chicago/Turabian StyleMarchesi, Gloria, Davide Maria Cammisuli, Michelle Semonella, Gianluca Castelnuovo, and Giada Pietrabissa. 2024. "The Efficacy of Cognitive Remediation Therapy for Anorexia Nervosa: A Systematic Review of Systematic Reviews" Brain Sciences 14, no. 2: 118. https://doi.org/10.3390/brainsci14020118
APA StyleMarchesi, G., Cammisuli, D. M., Semonella, M., Castelnuovo, G., & Pietrabissa, G. (2024). The Efficacy of Cognitive Remediation Therapy for Anorexia Nervosa: A Systematic Review of Systematic Reviews. Brain Sciences, 14(2), 118. https://doi.org/10.3390/brainsci14020118