Brain Health Indicators Following Acute Neuro-Exergaming: Biomarker and Cognition in Mild Cognitive Impairment (MCI) after Pedal-n-Play (iPACES)
Abstract
1. Introduction
1.1. Dementia Epidemic and Mild Cognitive Impairment (MCI)
1.2. Physical Exercise and Cognition Change
1.3. Cognitive Training and Cognitive Decline
1.4. Mental and Physical Exercise Combination (Interactive/Neuro-Exergaming) and Cognitive Decline
1.5. Single-Bout Exercise Intervention and Cognitive Performance
1.6. Neurobiological Mechanism and Markers of Cognitive Changes
1.7. A Priori Hypotheses
- Executive function will improve after a single-bout intervention of interactive neuro-exergaming [17].
- Improvements in cognition will be correlated with changes in the salivary biomarkers as follows:
- MCI participants will experience a greater improvement in cognitive performance than normative older adults [103].
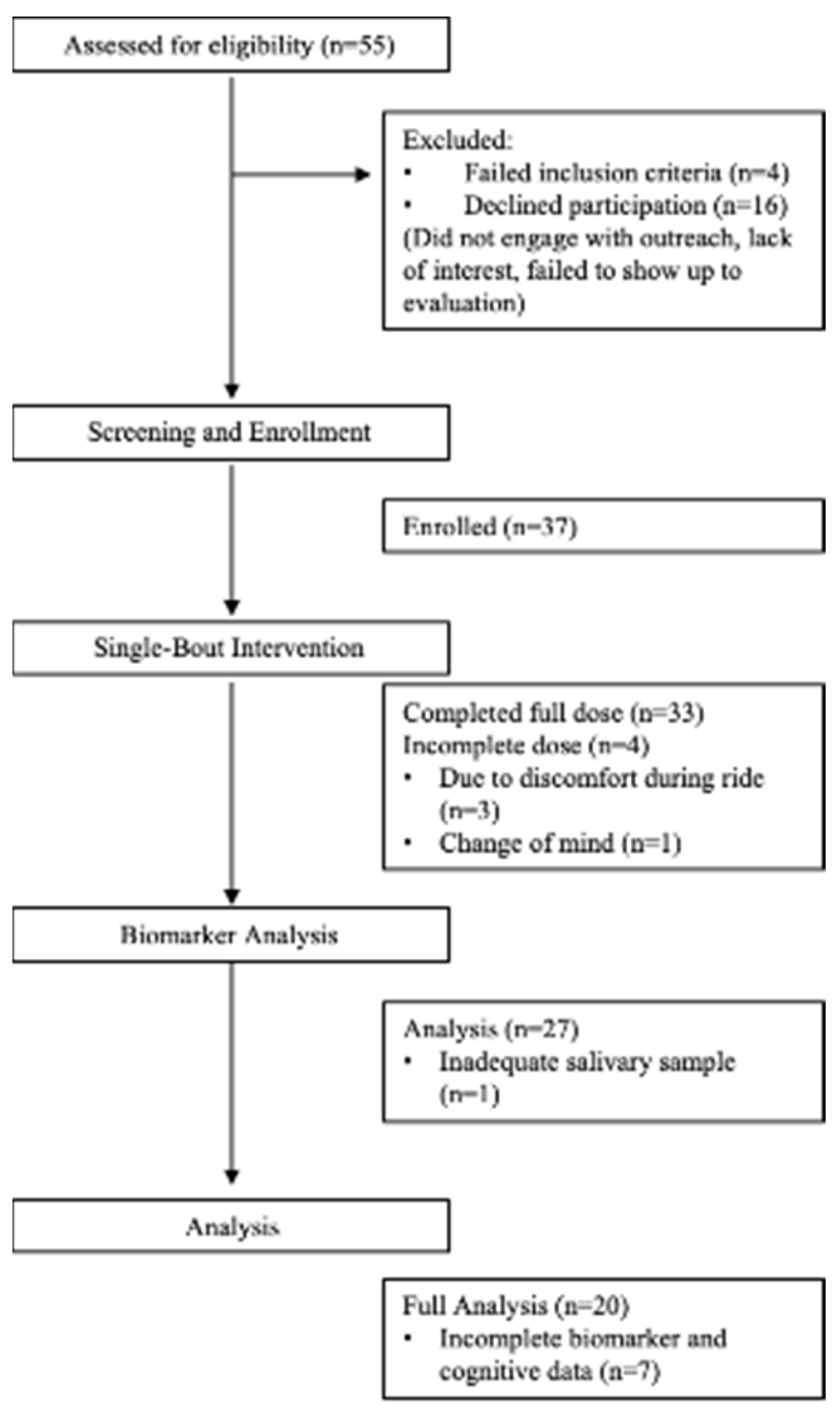
2. Materials and Methods
2.1. Participants
2.2. Procedures
2.3. Measures
2.3.1. Neuropsychological Evaluation
2.3.2. Cognitive Measures
2.3.3. Biological Measures
2.4. Intervention
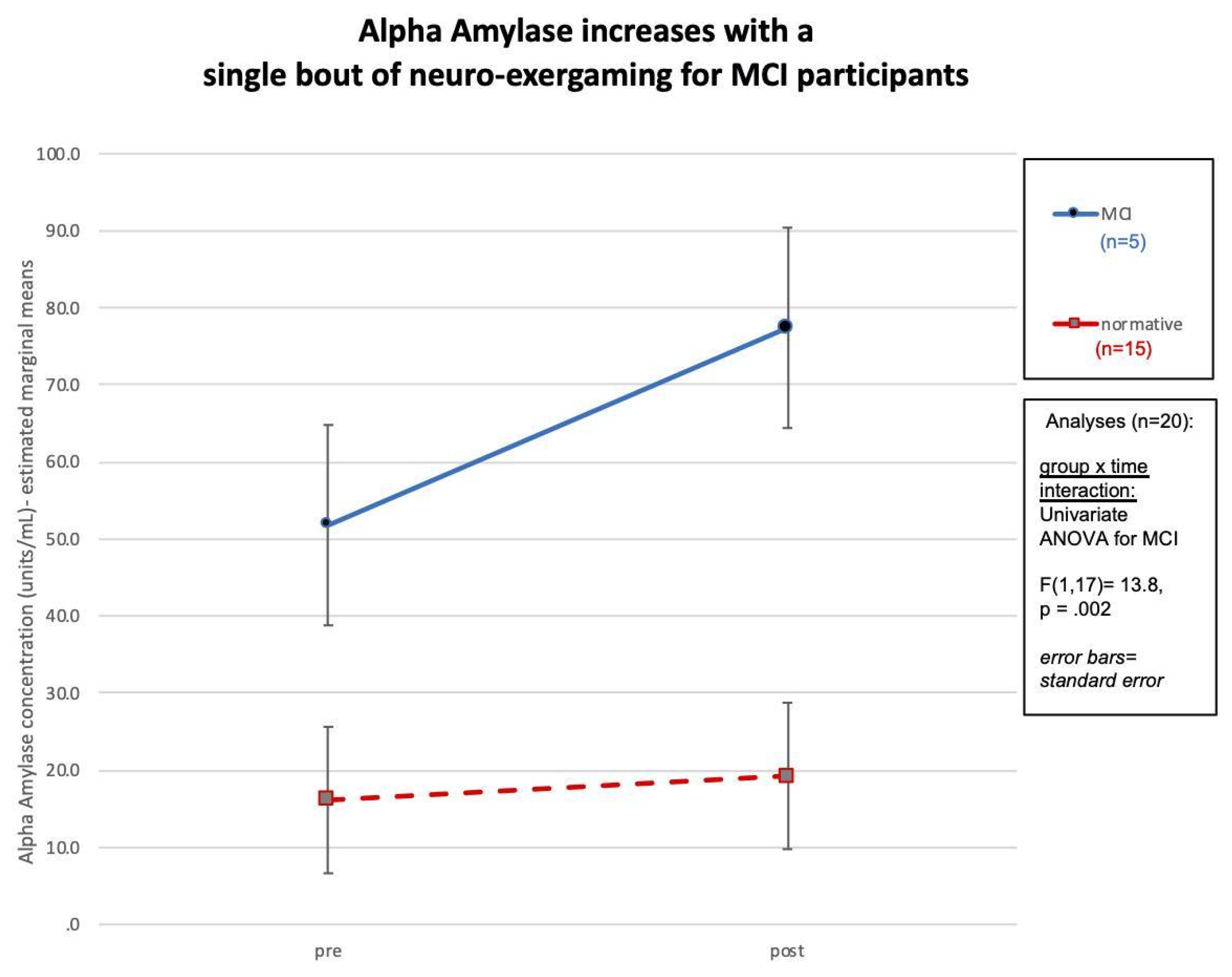
3. Results
Description of Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kirova, A.-M.; Bays, R.B.; Lagalwar, S. Working Memory and Executive Function Decline across Normal Aging, Mild Cognitive Impairment, and Alzheimer’s Disease. BioMed Res. Int. 2015, 2015, 748212. [Google Scholar] [CrossRef] [PubMed]
- Nichols, E.; Steinmetz, J.D.; Vollset, S.E.; Fukutaki, K.; Chalek, J.; Abd-Allah, F.; Abdoli, A.; Abualhasan, A.; Abu-Gharbieh, E.; Akram, T.T.; et al. Estimation of the Global Prevalence of Dementia in 2019 and Forecasted Prevalence in 2050: An Analysis for the Global Burden of Disease Study 2019. Lancet Public Health 2022, 7, e105–e125. [Google Scholar] [CrossRef] [PubMed]
- Hansen, R.A.; Gartlehner, G.; Lohr, K.N.; Kaufer, D.I. Functional Outcomes of Drug Treatment in Alzheimer’s Disease: A Systematic Review and Meta-Analysis. Drugs Aging 2007, 24, 155–167. [Google Scholar] [CrossRef]
- Ahlskog, J.E.; Geda, Y.E.; Graff-Radford, N.R.; Petersen, R.C. Physical Exercise as a Preventive or Disease-Modifying Treatment of Dementia and Brain Aging. Mayo Clin. Proc. 2011, 86, 876–884. [Google Scholar] [CrossRef] [PubMed]
- Schneider, L.S.; Mangialasche, F.; Andreasen, N.; Feldman, H.; Giacobini, E.; Jones, R.; Mantua, V.; Mecocci, P.; Pani, L.; Winblad, B.; et al. Clinical Trials and Late-Stage Drug Development for Alzheimer’s Disease: An Appraisal from 1984 to 2014. J. Intern. Med. 2014, 275, 251–283. [Google Scholar] [CrossRef]
- Korczyn, A.D.; Vakhapova, V. The Prevention of the Dementia Epidemic. J. Neurol. Sci. 2007, 257, 2–4. [Google Scholar] [CrossRef]
- Larson, E.B. Prospects for Delaying the Rising Tide of Worldwide, Late-Life Dementias. Int. Psychogeriatr. 2010, 22, 1196–1202. [Google Scholar] [CrossRef]
- Brookmeyer, R.; Johnson, E.; Ziegler-Graham, K.; Arrighi, H.M. Forecasting the Global Burden of Alzheimer’s Disease. Alzheimer’s Dement. 2007, 3, 186–191. [Google Scholar] [CrossRef]
- Heyn, P.; Abreu, B.C.; Ottenbacher, K.J. The Effects of Exercise Training on Elderly Persons with Cognitive Impairment and Dementia: A Meta-Analysis. Arch. Phys. Med. Rehabil. 2004, 85, 1694–1704. [Google Scholar] [CrossRef]
- Hillman, C.H.; Erickson, K.I.; Kramer, A.F. Be Smart, Exercise Your Heart: Exercise Effects on Brain and Cognition. Nat. Rev. Neurosci. 2008, 9, 58–65. [Google Scholar] [CrossRef]
- World Health Organization. Risk Reduction of Cognitive Decline and Dementia: WHO Guidelines; World Health Organization: Geneva, Switzerland, 2019. [Google Scholar]
- Kramer, A.F.; Colcombe, S. Fitness Effects on the Cognitive Function of Older Adults: A Meta-Analytic Study—Revisited. Perspect. Psychol. Sci. 2018, 13, 213–217. [Google Scholar] [CrossRef]
- Nelson, M.E.; Rejeski, W.J.; Blair, S.N.; Duncan, P.W.; Judge, J.O.; King, A.C.; Macera, C.A.; Castaneda-Sceppa, C. Physical Activity and Public Health in Older Adults: Recommendation from the American College of Sports Medicine and the American Heart Association. Med. Sci. Sport. Exerc. 2007, 39, 1435–1445. [Google Scholar] [CrossRef]
- Read, J.L.; Shortell, S.M. Interactive Games to Promote Behavior Change in Prevention and Treatment. JAMA 2011, 305, 1704. [Google Scholar] [CrossRef]
- Wall, K.; Stark, J.; Schillaci, A.; Saulnier, E.; McLaren, E.; Striegnitz, K.; Cohen, B.; Arciero, P.; Kramer, A.; Anderson-Hanley, C. The Enhanced Interactive Physical and Cognitive Exercise System (iPACESTM v2.0): Pilot Clinical Trial of an In-Home IPad-Based Neuro-Exergame for Mild Cognitive Impairment (MCI). J. Clin. Med. 2018, 7, 249. [Google Scholar] [CrossRef]
- Cui, M.Y.; Lin, Y.; Sheng, J.Y.; Zhang, X.; Cui, R.J. Exercise Intervention Associated with Cognitive Improvement in Alzheimer’s Disease. Neural Plast. 2018, 2018, 9234105. [Google Scholar] [CrossRef]
- Anderson-Hanley, C.; Maloney, M.; Barcelos, N.; Striegnitz, K.; Kramer, A. Neuropsychological Benefits of Neuro-Exergaming for Older Adults: A Pilot Study of an Interactive Physical and Cognitive Exercise System (IPACES). J. Aging Phys. Act. 2017, 25, 73–83. [Google Scholar] [CrossRef] [PubMed]
- Colcombe, S.; Kramer, A.F. Fitness Effects on the Cognitive Function of Older Adults: A Meta-Analytic Study. Psychol. Sci. 2003, 14, 125–130. [Google Scholar] [CrossRef] [PubMed]
- Rathore, A.; Lom, B. The Effects of Chronic and Acute Physical Activity on Working Memory Performance in Healthy Participants: A Systematic Review with Meta-Analysis of Randomized Controlled Trials. Syst. Rev. 2017, 6, 124. [Google Scholar] [CrossRef] [PubMed]
- Biazus-Sehn, L.F.; Schuch, F.B.; Firth, J.; de Souza Stigger, F. Effects of Physical Exercise on Cognitive Function of Older Adults with Mild Cognitive Impairment: A Systematic Review and Meta-Analysis. Arch. Gerontol. Geriatr. 2020, 89, 104048. [Google Scholar] [CrossRef]
- Chen, F.-T.; Etnier, J.L.; Chan, K.-H.; Chiu, P.-K.; Hung, T.-M.; Chang, Y.-K. Effects of Exercise Training Interventions on Executive Function in Older Adults: A Systematic Review and Meta-Analysis. Sport. Med. 2020, 50, 1451–1467. [Google Scholar] [CrossRef]
- Diamond, A.; Ling, D.S. Aerobic-Exercise and Resistance-Training Interventions Have Been among the Least Effective Ways to Improve Executive Functions of Any Method Tried Thus Far. Dev. Cogn. Neurosci. 2019, 37, 100572. [Google Scholar] [CrossRef] [PubMed]
- Gasquoine, P.G.; Chen, P.-Y. Effect of Physical Exercise on Popular Measures of Executive Function in Older, Nonclinical, Participants of Randomized Controlled Trials: A Meta-Analytic Review. Appl. Neuropsychol. Adult 2022, 29, 203–211. [Google Scholar] [CrossRef]
- De Souto Barreto, P.; Demougeot, L.; Vellas, B.; Rolland, Y. Exercise Training for Preventing Dementia, Mild Cognitive Impairment, and Clinically Meaningful Cognitive Decline: A Systematic Review and Meta-Analysis. J. Gerontol. Ser. A 2018, 73, 1504–1511. [Google Scholar] [CrossRef]
- Forbes, D.; Forbes, S.C.; Blake, C.M.; Thiessen, E.J.; Forbes, S. Exercise Programs for People with Dementia. Cochrane Database Syst. Rev. 2015, 2015, CD006489. [Google Scholar] [CrossRef]
- Young, J.; Angevaren, M.; Rusted, J.; Tabet, N. Aerobic Exercise to Improve Cognitive Function in Older People without Known Cognitive Impairment. Cochrane Database Syst. Rev. 2015, 2015, CD005381. [Google Scholar] [CrossRef] [PubMed]
- Kramer, A.F.; Hahn, S.; Cohen, N.J.; Banich, M.T.; McAuley, E.; Harrison, C.R.; Chason, J.; Vakil, E.; Bardell, L.; Boileau, R.A.; et al. Ageing, Fitness and Neurocognitive Function. Nature 1999, 400, 418–419. [Google Scholar] [CrossRef] [PubMed]
- Studenski, S.; Carlson, M.C.; Fillit, H.; Greenough, W.T.; Kramer, A.; Rebok, G.W. From Bedside to Bench: Does Mental and Physical Activity Promote Cognitive Vitality in Late Life? Sci. Aging Knowl. Environ. 2006, 2006, pe21. [Google Scholar] [CrossRef]
- Angevaren, M.; Aufdemkampe, G.; Verhaar, H.J.J.; Aleman, A.; Vanhees, L. Physical Activity and Enhanced Fitness to Improve Cognitive Function in Older People without Known Cognitive Impairment. Cochrane Database Syst. Rev. 2008, 2008, CD005381. [Google Scholar] [CrossRef]
- Baker, L.D.; Frank, L.L.; Foster-Schubert, K.; Green, P.S.; Wilkinson, C.W.; McTiernan, A.; Plymate, S.R.; Fishel, M.A.; Watson, G.S.; Cholerton, B.A.; et al. Effects of Aerobic Exercise on Mild Cognitive Impairment: A Controlled Trial. Arch. Neurol. 2010, 67, 71–79. [Google Scholar] [CrossRef]
- Geda, Y.E.; Roberts, R.O.; Knopman, D.S.; Christianson, T.J.H.; Pankratz, V.S.; Ivnik, R.J.; Boeve, B.F.; Tangalos, E.G.; Petersen, R.C.; Rocca, W.A. Physical Exercise, Aging, and Mild Cognitive Impairment: A Population-Based Study. Arch. Neurol. 2010, 67, 80–86. [Google Scholar] [CrossRef]
- Martin, M.; Clare, L.; Altgassen, A.M.; Cameron, M.H.; Zehnder, F. Cognition-Based Interventions for Healthy Older People and People with Mild Cognitive Impairment. Cochrane Database Syst. Rev. 2011, 2011, CD006220. [Google Scholar] [CrossRef]
- Zheng, G.; Xia, R.; Zhou, W.; Tao, J.; Chen, L. Aerobic Exercise Ameliorates Cognitive Function in Older Adults with Mild Cognitive Impairment: A Systematic Review and Meta-Analysis of Randomised Controlled Trials. Br. J. Sport Med. 2016, 50, 1443–1450. [Google Scholar] [CrossRef]
- Song, D.; Yu, D.S.F.; Li, P.W.C.; Lei, Y. The Effectiveness of Physical Exercise on Cognitive and Psychological Outcomes in Individuals with Mild Cognitive Impairment: A Systematic Review and Meta-Analysis. Int. J. Nurs. Stud. 2018, 79, 155–164. [Google Scholar] [CrossRef]
- Hess, N.C.; Dieberg, G.; McFarlane, J.R.; Smart, N.A. The Effect of Exercise Intervention on Cognitive Performance in Persons at Risk of, or with, Dementia: A Systematic Review and Meta-Analysis. Healthy Aging Res. 2014, 3, 3. [Google Scholar]
- Mistridis, P.; Krumm, S.; Monsch, A.U.; Berres, M.; Taylor, K.I. The 12 Years Preceding Mild Cognitive Impairment Due to Alzheimer’s Disease: The Temporal Emergence of Cognitive Decline. J. Alzheimer’s Dis. 2015, 48, 1095–1107. [Google Scholar] [CrossRef]
- Meng, Q.; Lin, M.-S.; Tzeng, I.-S. Relationship between Exercise and Alzheimer’s Disease: A Narrative Literature Review. Front. Neurosci. 2020, 14, 131. [Google Scholar] [CrossRef]
- Kramer, A.F.; Erickson, K.I. Capitalizing on Cortical Plasticity: Influence of Physical Activity on Cognition and Brain Function. Trends Cogn. Sci. 2007, 11, 342–348. [Google Scholar] [CrossRef]
- Teixeira, C.V.L.; Rezende, T.J.; Weiler, M.; Nogueira, M.H.; Campos, B.M.; Pegoraro, L.F.; Vicentini, J.E.; Scriptore, G.; Cendes, F.; Balthazar, M.L. Relation between Aerobic Fitness and Brain Structures in Amnestic Mild Cognitive Impairment Elderly. Age 2016, 38, 51. [Google Scholar] [CrossRef][Green Version]
- Gates, N.; Fiatarone Singh, M.A.; Sachdev, P.S.; Valenzuela, M. The Effect of Exercise Training on Cognitive Function in Older Adults with Mild Cognitive Impairment: A Meta-Analysis of Randomized Controlled Trials. Am. J. Geriatr. Psychiatry 2013, 21, 1086–1097. [Google Scholar] [CrossRef] [PubMed]
- Ludyga, S.; Gerber, M.; Brand, S.; Holsboer-Trachsler, E.; Pühse, U. Acute Effects of Moderate Aerobic Exercise on Specific Aspects of Executive Function in Different Age and Fitness Groups: A Meta-Analysis: Moderate Exercise and Executive Function. Psychophysiology 2016, 53, 1611–1626. [Google Scholar] [CrossRef]
- Liang, J.-H.; Xu, Y.; Lin, L.; Jia, R.-X.; Zhang, H.-B.; Hang, L. Comparison of Multiple Interventions for Older Adults with Alzheimer Disease or Mild Cognitive Impairment. Medicine 2018, 97, e10744. [Google Scholar] [CrossRef] [PubMed]
- Anderson-Hanley, C.; Arciero, P.J.; Brickman, A.M.; Nimon, J.P.; Okuma, N.; Westen, S.C.; Merz, M.E.; Pence, B.D.; Woods, J.A.; Kramer, A.F.; et al. Exergaming and Older Adult Cognition. Am. J. Prev. Med. 2012, 42, 109–119. [Google Scholar] [CrossRef] [PubMed]
- Anderson-Hanley, C.; Barcelos, N.M.; Zimmerman, E.A.; Gillen, R.W.; Dunnam, M.; Cohen, B.D.; Yerokhin, V.; Miller, K.E.; Hayes, D.J.; Arciero, P.J.; et al. The Aerobic and Cognitive Exercise Study (ACES) for Community-Dwelling Older Adults with or At-Risk for Mild Cognitive Impairment (MCI): Neuropsychological, Neurobiological and Neuroimaging Outcomes of a Randomized Clinical Trial. Front. Aging Neurosci. 2018, 10, 76. [Google Scholar] [CrossRef] [PubMed]
- Cotman, C.W.; Berchtold, N.C.; Christie, L.-A. Exercise Builds Brain Health: Key Roles of Growth Factor Cascades and Inflammation. Trends Neurosci. 2007, 30, 464–472. [Google Scholar] [CrossRef]
- Van Praag, H.; Kempermann, G.; Gage, F.H. Neural Consequences of Environmental Enrichment. Nat. Rev. Neurosci. 2000, 1, 191–198. [Google Scholar] [CrossRef]
- Van Praag, H.; Shubert, T.; Zhao, C.; Gage, F.H. Exercise Enhances Learning and Hippocampal Neurogenesis in Aged Mice. J. Neurosci. 2005, 25, 8680–8685. [Google Scholar] [CrossRef] [PubMed]
- Van Praag, H. Neurogenesis and Exercise: Past and Future Directions. Neuromol. Med. 2008, 10, 128–140. [Google Scholar] [CrossRef]
- Suo, C.; Singh, M.F.; Gates, N.; Wen, W.; Sachdev, P.; Brodaty, H.; Saigal, N.; Wilson, G.C.; Meiklejohn, J.; Singh, N.; et al. Therapeutically Relevant Structural and Functional Mechanisms Triggered by Physical and Cognitive Exercise. Mol. Psychiatry 2016, 21, 1633–1642. [Google Scholar] [CrossRef]
- Kirk-Sanchez, N.; McGough, E. Physical Exercise and Cognitive Performance in the Elderly: Current Perspectives. Clin. Interv. Aging 2013, 9, 51–62. [Google Scholar] [CrossRef]
- Rasmussen, P.; Brassard, P.; Adser, H.; Pedersen, M.V.; Leick, L.; Hart, E.; Secher, N.H.; Pedersen, B.K.; Pilegaard, H. Evidence for a Release of Brain-Derived Neurotrophic Factor from the Brain during Exercise: Brain-Derived Neurotrophic Factor Release during Exercise. Exp. Physiol. 2009, 94, 1062–1069. [Google Scholar] [CrossRef]
- Petersen, R.C.; Lopez, O.; Armstrong, M.J.; Getchius, T.S.D.; Ganguli, M.; Gloss, D.; Gronseth, G.S.; Marson, D.; Pringsheim, T.; Day, G.S.; et al. Practice Guideline Update Summary: Mild Cognitive Impairment: Report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology. Neurology 2018, 90, 126–135. [Google Scholar] [CrossRef]
- Papp, K.V.; Walsh, S.J.; Snyder, P.J. Immediate and Delayed Effects of Cognitive Interventions in Healthy Elderly: A Review of Current Literature and Future Directions. Alzheimer’s Dement. 2009, 5, 50–60. [Google Scholar] [CrossRef]
- Anguera, J.A.; Boccanfuso, J.; Rintoul, J.L.; Al-Hashimi, O.; Faraji, F.; Janowich, J.; Kong, E.; Larraburo, Y.; Rolle, C.; Johnston, E.; et al. Video Game Training Enhances Cognitive Control in Older Adults. Nature 2013, 501, 97–101. [Google Scholar] [CrossRef] [PubMed]
- Li, K.Z.H.; Lindenberger, U.; Freund, A.M.; Baltes, P.B. Walking While Memorizing: Age-Related Differences in Compensatory Behavior. Psychol. Sci. 2001, 12, 230–237. [Google Scholar] [CrossRef]
- Toril, P.; Reales, J.M.; Ballesteros, S. Video Game Training Enhances Cognition of Older Adults: A Meta-Analytic Study. Psychol. Aging 2014, 29, 706–716. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Yu, J.-T.; Wang, H.-F.; Tan, C.-C.; Meng, X.-F.; Tan, L. Non-Pharmacological Interventions for Patients with Mild Cognitive Impairment: A Meta-Analysis of Randomized Controlled Trials of Cognition-Based and Exercise Interventions. J. Alzheimer’s Dis. 2014, 42, 663–678. [Google Scholar] [CrossRef] [PubMed]
- Ballesteros, S.; Prieto, A.; Mayas, J.; Toril, P.; Pita, C.; Ponce de León, L.; Reales, J.M.; Waterworth, J. Brain Training with Non-Action Video Games Enhances Aspects of Cognition in Older Adults: A Randomized Controlled Trial. Front. Aging Neurosci. 2014, 6, 277. [Google Scholar] [CrossRef]
- Bamidis, P.D.; Vivas, A.B.; Styliadis, C.; Frantzidis, C.; Klados, M.; Schlee, W.; Siountas, A.; Papageorgiou, S.G. A Review of Physical and Cognitive Interventions in Aging. Neurosci. Biobehav. Rev. 2014, 44, 206–220. [Google Scholar] [CrossRef]
- Corbett, A.; Owen, A.; Hampshire, A.; Grahn, J.; Stenton, R.; Dajani, S.; Burns, A.; Howard, R.; Williams, N.; Williams, G.; et al. The Effect of an Online Cognitive Training Package in Healthy Older Adults: An Online Randomized Controlled Trial. J. Am. Med. Dir. Assoc. 2015, 16, 990–997. [Google Scholar] [CrossRef]
- Mowszowski, L.; Lampit, A.; Walton, C.C.; Naismith, S.L. Strategy-Based Cognitive Training for Improving Executive Functions in Older Adults: A Systematic Review. Neuropsychol. Rev. 2016, 26, 252–270. [Google Scholar] [CrossRef]
- Bahar-Fuchs, A.; Clare, L.; Woods, B. Cognitive Training and Cognitive Rehabilitation for Persons with Mild to Moderate Dementia of the Alzheimer’s or Vascular Type: A Review. Alzheimers Res. 2013, 5, 35. [Google Scholar] [CrossRef]
- Simons, D.J.; Boot, W.R.; Charness, N.; Gathercole, S.E.; Chabris, C.F.; Hambrick, D.Z.; Stine-Morrow, E.A.L. Do “Brain-Training” Programs Work? Psychol. Sci. Public Interest 2016, 17, 103–186. [Google Scholar] [CrossRef] [PubMed]
- Reijnders, J.; van Heugten, C.; van Boxtel, M. Cognitive Interventions in Healthy Older Adults and People with Mild Cognitive Impairment: A Systematic Review. Ageing Res. Rev. 2013, 12, 263–275. [Google Scholar] [CrossRef] [PubMed]
- Willis, S.L.; Tennstedt, S.L.; Marsiske, M.; Ball, K.; Elias, J.; Koepke, K.M.; Morris, J.N.; Rebok, G.W.; Unverzagt, F.W.; Stoddard, A.M.; et al. Long-Term Effects of Cognitive Training on Everyday Functional Outcomes in Older Adults. JAMA 2006, 296, 2805. [Google Scholar] [CrossRef]
- Karr, J.E.; Areshenkoff, C.N.; Rast, P.; Garcia-Barrera, M.A. An Empirical Comparison of the Therapeutic Benefits of Physical Exercise and Cognitive Training on the Executive Functions of Older Adults: A Meta-Analysis of Controlled Trials. Neuropsychology 2014, 28, 829–845. [Google Scholar] [CrossRef]
- Huntley, J.D.; Gould, R.L.; Liu, K.; Smith, M.; Howard, R.J. Do Cognitive Interventions Improve General Cognition in Dementia? A Meta-Analysis and Meta-Regression. BMJ Open 2015, 5, e005247. [Google Scholar] [CrossRef]
- Owen, A.M.; Hampshire, A.; Grahn, J.A.; Stenton, R.; Dajani, S.; Burns, A.S.; Howard, R.J.; Ballard, C.G. Putting Brain Training to the Test. Nature 2010, 465, 775–778. [Google Scholar] [CrossRef]
- Van Muijden, J.; Band, G.P.H.; Hommel, B. Online Games Training Aging Brains: Limited Transfer to Cognitive Control Functions. Front. Hum. Neurosci. 2012, 6, 221. [Google Scholar] [CrossRef]
- Redick, T.S.; Shipstead, Z.; Harrison, T.L.; Hicks, K.L.; Fried, D.E.; Hambrick, D.Z.; Kane, M.J.; Engle, R.W. No Evidence of Intelligence Improvement after Working Memory Training: A Randomized, Placebo-Controlled Study. J. Exp. Psychol. Gen. 2013, 142, 359–379. [Google Scholar] [CrossRef]
- Boot, W.R.; Kramer, A.F. The Brain-Games Conundrum: Does Cognitive Training Really Sharpen the Mind? Cerebrum 2014, 2014, 15. [Google Scholar]
- Zokaei, N.; MacKellar, C.; Čepukaitytė, G.; Patai, E.Z.; Nobre, A.C. Cognitive Training in the Elderly: Bottlenecks and New Avenues. J. Cogn. Neurosci. 2017, 29, 1473–1482. [Google Scholar] [CrossRef]
- Gheysen, F.; Poppe, L.; DeSmet, A.; Swinnen, S.; Cardon, G.; De Bourdeaudhuij, I.; Chastin, S.; Fias, W. Physical Activity to Improve Cognition in Older Adults: Can Physical Activity Programs Enriched with Cognitive Challenges Enhance the Effects? A Systematic Review and Meta-Analysis. Int. J. Behav. Nutr. Phys. Act 2018, 15, 63. [Google Scholar] [CrossRef]
- Constans, A.; Pin-barre, C.; Temprado, J.-J.; Decherchi, P.; Laurin, J. Influence of Aerobic Training and Combinations of Interventions on Cognition and Neuroplasticity after Stroke. Front. Aging Neurosci. 2016, 8, 164. [Google Scholar] [CrossRef]
- Diamond, A. Effects of Physical Exercise on Executive Functions: Going beyond Simply Moving to Moving with Thought. Ann. Sport. Med. Res. 2015, 2, 1011. [Google Scholar]
- Zhu, X.; Yin, S.; Lang, M.; He, R.; Li, J. The More the Better? A Meta-Analysis on Effects of Combined Cognitive and Physical Intervention on Cognition in Healthy Older Adults. Ageing Res. Rev. 2016, 31, 67–79. [Google Scholar] [CrossRef] [PubMed]
- Geda, Y.E.; Silber, T.C.; Roberts, R.O.; Knopman, D.S.; Christianson, T.J.H.; Pankratz, V.S.; Boeve, B.F.; Tangalos, E.G.; Petersen, R.C. Computer Activities, Physical Exercise, Aging, and Mild Cognitive Impairment: A Population-Based Study. Mayo Clin. Proc. 2012, 87, 437–442. [Google Scholar] [CrossRef] [PubMed]
- Shah, T.; Verdile, G.; Sohrabi, H.; Campbell, A.; Putland, E.; Cheetham, C.; Dhaliwal, S.; Weinborn, M.; Maruff, P.; Darby, D.; et al. A Combination of Physical Activity and Computerized Brain Training Improves Verbal Memory and Increases Cerebral Glucose Metabolism in the Elderly. Transl. Psychiatry 2014, 4, e487. [Google Scholar] [CrossRef]
- Karssemeijer, E.G.A.; Aaronson, J.A.; Bossers, W.J.; Smits, T.; Olde Rikkert, M.G.M.; Kessels, R.P.C. Positive Effects of Combined Cognitive and Physical Exercise Training on Cognitive Function in Older Adults with Mild Cognitive Impairment or Dementia: A Meta-Analysis. Ageing Res. Rev. 2017, 40, 75–83. [Google Scholar] [CrossRef]
- Styliadis, C.; Kartsidis, P.; Paraskevopoulos, E.; Ioannides, A.A.; Bamidis, P.D. Neuroplastic Effects of Combined Computerized Physical and Cognitive Training in Elderly Individuals at Risk for Dementia: An ELORETA Controlled Study on Resting States. Neural Plast. 2015, 2015, 172192. [Google Scholar] [CrossRef]
- Edwards, M.; Loprinzi, P. Experimental Effects of Acute Exercise and Meditation on Parameters of Cognitive Function. J. Clin. Med. 2018, 7, 125. [Google Scholar] [CrossRef] [PubMed]
- Ballesteros, S.; Voelcker-Rehage, C.; Bherer, L. Editorial: Cognitive and Brain Plasticity Induced by Physical Exercise, Cognitive Training, Video Games, and Combined Interventions. Front. Hum. Neurosci. 2018, 12, 169. [Google Scholar] [CrossRef] [PubMed]
- Barnes, D.E.; Santos-Modesitt, W.; Poelke, G.; Kramer, A.F.; Castro, C.; Middleton, L.E.; Yaffe, K. The Mental Activity and Exercise (MAX) Trial. JAMA Intern. Med. 2013, 173, 797. [Google Scholar] [CrossRef]
- Fiatarone Singh, M.A.; Gates, N.; Saigal, N.; Wilson, G.C.; Meiklejohn, J.; Brodaty, H.; Wen, W.; Singh, N.; Baune, B.T.; Suo, C.; et al. The Study of Mental and Resistance Training (SMART) Study—Resistance Training and/or Cognitive Training in Mild Cognitive Impairment: A Randomized, Double-Blind, Double-Sham Controlled Trial. J. Am. Med. Dir. Assoc. 2014, 15, 873–880. [Google Scholar] [CrossRef]
- Law, L.L.F.; Barnett, F.; Yau, M.K.; Gray, M.A. Effects of Combined Cognitive and Exercise Interventions on Cognition in Older Adults with and without Cognitive Impairment: A Systematic Review. Ageing Res. Rev. 2014, 15, 61–75. [Google Scholar] [CrossRef]
- Rahe, J.; Becker, J.; Fink, G.R.; Kessler, J.; Kukolja, J.; Rahn, A.; Rosen, J.B.; Szabados, F.; Wirth, B.; Kalbe, E. Cognitive Training with and without Additional Physical Activity in Healthy Older Adults: Cognitive Effects, Neurobiological Mechanisms, and Prediction of Training Success. Front. Aging Neurosci. 2015, 7, 187. [Google Scholar] [CrossRef] [PubMed]
- Lipardo, D.S.; Aseron, A.M.C.; Kwan, M.M.; Tsang, W.W. Effect of Exercise and Cognitive Training on Falls and Fall-Related Factors in Older Adults with Mild Cognitive Impairment: A Systematic Review. Arch. Phys. Med. Rehabil. 2017, 98, 2079–2096. [Google Scholar] [CrossRef] [PubMed]
- Schaefer, S.; Schumacher, V. The Interplay between Cognitive and Motor Functioning in Healthy Older Adults: Findings from Dual-Task Studies and Suggestions for Intervention. Gerontology 2011, 57, 239–246. [Google Scholar] [CrossRef]
- De Coelho, F.G.M.; Andrade, L.P.; Pedroso, R.V.; Santos-Galduroz, R.F.; Gobbi, S.; Costa, J.L.R.; Gobbi, L.T.B. Multimodal Exercise Intervention Improves Frontal Cognitive Functions and Gait in Alzheimer’s Disease: A Controlled Trial: Exercise, Cognitive Functions and Gait. Geriatr. Gerontol. Int. 2013, 13, 198–203. [Google Scholar] [CrossRef]
- Forte, R.; Boreham, C.; Leite, J.; De Vito, G.; Brennan, L.; Gibney, E.; Pesce, C. Enhancing Cognitive Functioning in the Elderly: Multicomponent vs Resistance Training. Clin. Interv. Aging 2013, 2013, 19–27. [Google Scholar] [CrossRef]
- Theill, N.; Schumacher, V.; Adelsberger, R.; Martin, M.; Jäncke, L. Effects of Simultaneously Performed Cognitive and Physical Training in Older Adults. BMC Neurosci. 2013, 14, 103. [Google Scholar] [CrossRef]
- Bherer, L. Cognitive Plasticity in Older Adults: Effects of Cognitive Training and Physical Exercise: Cognitive Plasticity in Older Adults. Ann. N. Y. Acad. Sci. 2015, 1337, 12682. [Google Scholar] [CrossRef]
- Eggenberger, P.; Wolf, M.; Schumann, M.; de Bruin, E.D. Exergame and Balance Training Modulate Prefrontal Brain Activity during Walking and Enhance Executive Function in Older Adults. Front. Aging Neurosci. 2016, 8, 66. [Google Scholar] [CrossRef]
- Yokoyama, H.; Okazaki, K.; Imai, D.; Yamashina, Y.; Takeda, R.; Naghavi, N.; Ota, A.; Hirasawa, Y.; Miyagawa, T. The Effect of Cognitive-Motor Dual-Task Training on Cognitive Function and Plasma Amyloid β Peptide 42/40 Ratio in Healthy Elderly Persons: A Randomized Controlled Trial. BMC Geriatr. 2015, 15, 60. [Google Scholar] [CrossRef] [PubMed]
- Desjardins-Crepeau, L.; Berryman, N.; Fraser, S.; Vu, T.T.M.; Kergoat, M.-J.; Li, K.; Bosquet, L.; Bherer, L. Effects of Combined Physical and Cognitive Training on Fitness and Neuropsychological Outcomes in Healthy Older Adults. Clin. Interv. Aging 2016, 11, 1287–1299. [Google Scholar] [CrossRef]
- Maillot, P.; Perrot, A.; Hartley, A. Effects of Interactive Physical-Activity Video-Game Training on Physical and Cognitive Function in Older Adults. Psychol. Aging 2012, 27, 589–600. [Google Scholar] [CrossRef]
- González-Palau, F.; Franco, M.; Bamidis, P.; Losada, R.; Parra, E.; Papageorgiou, S.G.; Vivas, A.B. The Effects of a Computer-Based Cognitive and Physical Training Program in a Healthy and Mildly Cognitive Impaired Aging Sample. Aging Ment. Health 2014, 18, 838–846. [Google Scholar] [CrossRef]
- Schoene, D.; Valenzuela, T.; Lord, S.R.; de Bruin, E.D. The Effect of Interactive Cognitive-Motor Training in Reducing Fall Risk in Older People: A Systematic Review. BMC Geriatr. 2014, 14, 107. [Google Scholar] [CrossRef] [PubMed]
- Bamidis, P.D.; Fissler, P.; Papageorgiou, S.G.; Zilidou, V.; Konstantinidis, E.I.; Billis, A.S.; Romanopoulou, E.; Karagianni, M.; Beratis, I.; Tsapanou, A.; et al. Gains in Cognition through Combined Cognitive and Physical Training: The Role of Training Dosage and Severity of Neurocognitive Disorder. Front. Aging Neurosci. 2015, 7, 152. [Google Scholar] [CrossRef]
- Lauenroth, A.; Ioannidis, A.E.; Teichmann, B. Influence of Combined Physical and Cognitive Training on Cognition: A Systematic Review. BMC Geriatr. 2016, 16, 141. [Google Scholar] [CrossRef] [PubMed]
- Wang, P.; Liu, H.-H.; Zhu, X.-T.; Meng, T.; Li, H.-J.; Zuo, X.-N. Action Video Game Training for Healthy Adults: A Meta-Analytic Study. Front. Psychol. 2016, 7, 907. [Google Scholar] [CrossRef]
- Stanmore, E.; Stubbs, B.; Vancampfort, D.; de Bruin, E.D.; Firth, J. The Effect of Active Video Games on Cognitive Functioning in Clinical and Non-Clinical Populations: A Meta-Analysis of Randomized Controlled Trials. Neurosci. Biobehav. Rev. 2017, 78, 34–43. [Google Scholar] [CrossRef] [PubMed]
- Anderson-Hanley, C.; Stark, J.; Wall, K.M.; VanBrakle, M.; Michel, M.; Maloney, M.; Barcelos, N.; Striegnitz, K.; Cohen, B.; Kramer, A.F. The Interactive Physical and Cognitive Exercise System (IPACES™): Effects of a 3-Month in-Home Pilot Clinical Trial for Mild Cognitive Impairment and Caregivers. Clin. Interv. Aging 2018, 13, 1565–1577. [Google Scholar] [CrossRef] [PubMed]
- Bruderer-Hofstetter, M.; Rausch-Osthoff, A.-K.; Meichtry, A.; Münzer, T.; Niedermann, K. Effective Multicomponent Interventions in Comparison to Active Control and No Interventions on Physical Capacity, Cognitive Function and Instrumental Activities of Daily Living in Elderly People with and without Mild Impaired Cognition—A Systematic Review and Network Meta-Analysis. Ageing Res. Rev. 2018, 45, 1–14. [Google Scholar] [CrossRef]
- Joubert, C.; Chainay, H. Aging Brain: The Effect of Combined Cognitive and Physical Training on Cognition as Compared to Cognitive and Physical Training Alone—A Systematic Review. Clin. Interv. Aging 2018, 13, 1267–1301. [Google Scholar] [CrossRef]
- Van het Reve, E.; de Bruin, E.D. Strength-Balance Supplemented with Computerized Cognitive Training to Improve Dual Task Gait and Divided Attention in Older Adults: A Multicenter Randomized-Controlled Trial. BMC Geriatr. 2014, 14, 134. [Google Scholar] [CrossRef] [PubMed]
- Hiyamizu, M.; Morioka, S.; Shomoto, K.; Shimada, T. Effects of Dual Task Balance Training on Dual Task Performance in Elderly People: A Randomized Controlled Trial. Clin. Rehabil. 2012, 26, 58–67. [Google Scholar] [CrossRef]
- Kayama, H.; Okamoto, K.; Nishiguchi, S.; Yamada, M.; Kuroda, T.; Aoyama, T. Effect of a Kinect-Based Exercise Game on Improving Executive Cognitive Performance in Community-Dwelling Elderly: Case Control Study. J. Med. Internet Res. 2014, 16, e61. [Google Scholar] [CrossRef] [PubMed]
- Barcelos, N.; Shah, N.; Cohen, K.; Hogan, M.J.; Mulkerrin, E.; Arciero, P.J.; Cohen, B.D.; Kramer, A.F.; Anderson-Hanley, C. Aerobic and Cognitive Exercise (ACE) Pilot Study for Older Adults: Executive Function Improves with Cognitive Challenge While Exergaming. J. Int. Neuropsychol. Soc. 2015, 21, 768–779. [Google Scholar] [CrossRef]
- Nishiguchi, S.; Yamada, M.; Tanigawa, T.; Sekiyama, K.; Kawagoe, T.; Suzuki, M.; Yoshikawa, S.; Abe, N.; Otsuka, Y.; Nakai, R.; et al. A 12-Week Physical and Cognitive Exercise Program Can Improve Cognitive Function and Neural Efficiency in Community-Dwelling Older Adults: A Randomized Controlled Trial. J. Am. Geriatr. Soc. 2015, 63, 1355–1363. [Google Scholar] [CrossRef]
- León, J.; Ureña, A.; Bolaños, M.J.; Bilbao, A.; Oña, A. A Combination of Physical and Cognitive Exercise Improves Reaction Time in Persons 61–84 Years Old. J. Aging Phys. Act. 2015, 23, 72–77. [Google Scholar] [CrossRef]
- Smith, G.E. Healthy Cognitive Aging and Dementia Prevention. Am. Psychol. 2016, 71, 268–275. [Google Scholar] [CrossRef]
- Barry, G.; Galna, B.; Rochester, L. The Role of Exergaming in Parkinson’s Disease Rehabilitation: A Systematic Review of the Evidence. J. NeuroEng. Rehabil. 2014, 11, 33. [Google Scholar] [CrossRef] [PubMed]
- Chao, Y.-Y.; Scherer, Y.K.; Montgomery, C.A. Effects of Using Nintendo Wii™ Exergames in Older Adults: A Review of the Literature. J. Aging Health 2015, 27, 379–402. [Google Scholar] [CrossRef] [PubMed]
- Ogawa, E.F.; You, T.; Leveille, S.G. Potential Benefits of Exergaming for Cognition and Dual-Task Function in Older Adults: A Systematic Review. J. Aging Phys. Act. 2016, 24, 332–336. [Google Scholar] [CrossRef] [PubMed]
- Zilidou, V.I.; Konstantinidis, E.I.; Romanopoulou, E.D.; Karagianni, M.; Kartsidis, P.; Bamidis, P.D. Investigating the Effectiveness of Physical Training through Exergames: Focus on Balance and Aerobic Protocols. In Proceedings of the 2016 1st International Conference on Technology and Innovation in Sports, Health and Wellbeing (TISHW), Vila Real, Portugal, 1–3 December 2016; IEEE: Piscataway, NJ, USA, 2016; pp. 1–6. [Google Scholar] [CrossRef]
- Fissler, P.; Küster, O.; Schlee, W.; Kolassa, I.-T. Novelty Interventions to Enhance Broad Cognitive Abilities and Prevent Dementia. In Progress in Brain Research; Elsevier: Amsterdam, The Netherlands, 2013; Volume 207, pp. 403–434. [Google Scholar] [CrossRef]
- Chang, Y.K.; Labban, J.D.; Gapin, J.I.; Etnier, J.L. The Effects of Acute Exercise on Cognitive Performance: A Meta-Analysis. Brain Res. 2012, 1453, 87–101. [Google Scholar] [CrossRef]
- Lambourne, K.; Tomporowski, P. The Effect of Exercise-Induced Arousal on Cognitive Task Performance: A Meta-Regression Analysis. Brain Res. 2010, 1341, 12–24. [Google Scholar] [CrossRef]
- Hillman, C.H.; Pontifex, M.B.; Raine, L.B.; Castelli, D.M.; Hall, E.E.; Kramer, A.F. The Effect of Acute Treadmill Walking on Cognitive Control and Academic Achievement in Preadolescent Children. Neuroscience 2009, 159, 1044–1054. [Google Scholar] [CrossRef]
- Nanda, B.; Balde, J.; Manjunatha, S. The Acute Effects of a Single Bout of Moderate-Intensity Aerobic Exercise on Cognitive Functions in Healthy Adult Males. J. Clin. Diagn. Res. JCDR 2013, 7, 1883. [Google Scholar] [CrossRef]
- Kamijo, K.; Hayashi, Y.; Sakai, T.; Yahiro, T.; Tanaka, K.; Nishihira, Y. Acute Effects of Aerobic Exercise on Cognitive Function in Older Adults. J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 2009, 64B, 356–363. [Google Scholar] [CrossRef]
- Li, L.; Men, W.-W.; Chang, Y.-K.; Fan, M.-X.; Ji, L.; Wei, G.-X. Acute Aerobic Exercise Increases Cortical Activity during Working Memory: A Functional MRI Study in Female College Students. PLoS ONE 2014, 9, e99222. [Google Scholar] [CrossRef]
- Loprinzi, P.D.; Roig, M.; Tomporowski, P.D.; Javadi, A.; Kelemen, W.L. Effects of acute exercise on memory: Considerations of exercise intensity, post-exercise recovery period and aerobic endurance. Mem. Cognit. 2023, 51, 1011–1026. [Google Scholar] [CrossRef] [PubMed]
- Labban, J.D.; Etnier, J.L. Effects of acute exercise on long-term memory. Res. Q. Exerc. Sport 2011, 82, 712–721. [Google Scholar] [CrossRef] [PubMed]
- Heath, M.; Shukla, D. A Single Bout of Aerobic Exercise Provides an Immediate “Boost” to Cognitive Flexibility. Front. Psychol. 2020, 11, 1106. [Google Scholar] [CrossRef]
- Tsai, C.-L.; Pai, M.-C.; Ukropec, J.; Ukropcová, B. Distinctive Effects of Aerobic and Resistance Exercise Modes on Neurocognitive and Biochemical Changes in Individuals with Mild Cognitive Impairment. Curr. Alzheimer Res. 2019, 16, 316–332. [Google Scholar] [CrossRef] [PubMed]
- Devenney, K.E.; Guinan, E.M.; Kelly, Á.M.; Mota, B.C.; Walsh, C.; Olde Rikkert, M.; Schneider, S.; Lawlor, B. Acute High-Intensity Aerobic Exercise Affects Brain-Derived Neurotrophic Factor in Mild Cognitive Impairment: A Randomised Controlled Study. BMJ Open Sport Exerc. Med. 2019, 5, e000499. [Google Scholar] [CrossRef]
- Knaepen, K.; Goekint, M.; Heyman, E.M.; Meeusen, R. Neuroplasticity—Exercise-Induced Response of Peripheral Brain-Derived Neurotrophic Factor: A Systematic Review of Experimental Studies in Human Subjects. Sport. Med. 2010, 40, 765–801. [Google Scholar] [CrossRef]
- Leckie, R.L.; Oberlin, L.E.; Voss, M.W.; Prakash, R.S.; Szabo-Reed, A.; Chaddock-Heyman, L.; Phillips, S.M.; Gothe, N.P.; Mailey, E.; Vieira-Potter, V.J.; et al. BDNF Mediates Improvements in Executive Function Following a 1-Year Exercise Intervention. Front. Hum. Neurosci. 2014, 8, 985. [Google Scholar] [CrossRef]
- Vaughan, S.; Wallis, M.; Polit, D.; Steele, M.; Shum, D.; Morris, N. The Effects of Multimodal Exercise on Cognitive and Physical Functioning and Brain-Derived Neurotrophic Factor in Older Women: A Randomised Controlled Trial. Age Ageing 2014, 43, 623–629. [Google Scholar] [CrossRef]
- Dinoff, A.; Herrmann, N.; Swardfager, W.; Liu, C.S.; Sherman, C.; Chan, S.; Lanctôt, K.L. The Effect of Exercise Training on Resting Concentrations of Peripheral Brain-Derived Neurotrophic Factor (BDNF): A Meta-Analysis. PLoS ONE 2016, 11, e0163037. [Google Scholar] [CrossRef]
- Maass, A.; Düzel, S.; Brigadski, T.; Goerke, M.; Becke, A.; Sobieray, U.; Neumann, K.; Lövdén, M.; Lindenberger, U.; Bäckman, L.; et al. Relationships of Peripheral IGF-1, VEGF and BDNF Levels to Exercise-Related Changes in Memory, Hippocampal Perfusion and Volumes in Older Adults. NeuroImage 2016, 131, 142–154. [Google Scholar] [CrossRef]
- Canton-Martínez, E.; Rentería, I.; García-Suárez, P.C.; Moncada-Jiménez, J.; Machado-Parra, J.P.; Lira, F.S.; Johnson, D.K.; Jiménez-Maldonado, A. Concurrent Training Increases Serum Brain-Derived Neurotrophic Factor in Older Adults Regardless of the Exercise Frequency. Front. Aging Neurosci. 2022, 14, 791698. [Google Scholar] [CrossRef]
- De Rondão, C.A.M.; Mota, M.P.; Oliveira, M.M.; Peixoto, F.; Esteves, D. Multicomponent Exercise Program Effects on Fitness and Cognitive Function of Elderlies with Mild Cognitive Impairment: Involvement of Oxidative Stress and BDNF. Front. Aging Neurosci. 2022, 14, 950937. [Google Scholar] [CrossRef] [PubMed]
- Voss, M.W.; Prakash, R.S.; Erickson, K.I.; Basak, C.; Chaddock, L.; Kim, J.S.; Alves, H.; Heo, S.; Szabo, A.N.; White, S.M.; et al. Plasticity of Brain Networks in a Randomized Intervention Trial of Exercise Training in Older Adults. Front. Aging Neurosci. 2010, 2, 32. [Google Scholar] [CrossRef] [PubMed]
- Brown, B.M.; Peiffer, J.J.; Martins, R.N. Multiple Effects of Physical Activity on Molecular and Cognitive Signs of Brain Aging: Can Exercise Slow Neurodegeneration and Delay Alzheimer’s Disease? Mol. Psychiatry 2013, 18, 864–874. [Google Scholar] [CrossRef] [PubMed]
- Phillips, C.; Baktir, M.A.; Srivatsan, M.; Salehi, A. Neuroprotective Effects of Physical Activity on the Brain: A Closer Look at Trophic Factor Signaling. Front. Cell. Neurosci. 2014, 8, 170. [Google Scholar] [CrossRef] [PubMed]
- Rojas Vega, S.; Knicker, A.; Hollmann, W.; Bloch, W.; Strüder, H.K. Effect of Resistance Exercise on Serum Levels of Growth Factors in Humans. Horm. Metab. Res. 2010, 42, 982–986. [Google Scholar] [CrossRef]
- Bellar, D.; Glickman, E.L.; Juvancic-Heltzel, J.; Gunstad, J. Serum Insulin like Growth Factor-1 Is Associated with Working Memory, Executive Function and Selective Attention in a Sample of Healthy, Fit Older Adults. Neuroscience 2011, 178, 133–137. [Google Scholar] [CrossRef]
- Stein, A.M.; da Silva, T.M.V.; de Coelho, F.G.M.; Rueda, A.V.; Camarini, R.; Galduróz, R.F.S. Acute Exercise Increases Circulating IGF-1 in Alzheimer’s Disease Patients, but Not in Older Adults without Dementia. Behav. Brain Res. 2021, 396, 112903. [Google Scholar] [CrossRef]
- Dik, M.G.; Pluijm, S.M.F.; Jonker, C.; Deeg, D.J.H.; Lomecky, M.Z.; Lips, P. Insulin-like Growth Factor I (IGF-I) and Cognitive Decline in Older Persons. Neurobiol. Aging 2003, 24, 573–581. [Google Scholar] [CrossRef]
- Al-Delaimy, W.K.; Von Muhlen, D.; Barrett-Connor, E. Insulinlike Growth Factor-1, Insulinlike Growth Factor Binding Protein-1, and Cognitive Function in Older Men and Women: IGF-1 and Cognitive Function. J. Am. Geriatr. Soc. 2009, 57, 1441–1446. [Google Scholar] [CrossRef]
- Lara, V.P.; Caramelli, P.; Teixeira, A.L.; Barbosa, M.T.; Carmona, K.C.; Carvalho, M.G.; Fernandes, A.P.; Gomes, K.B. High Cortisol Levels Are Associated with Cognitive Impairment No-Dementia (CIND) and Dementia. Clin. Chim. Acta 2013, 423, 18–22. [Google Scholar] [CrossRef] [PubMed]
- Tortosa-Martínez, J.; Manchado, C.; Cortell-Tormo, J.M.; Chulvi-Medrano, I. Exercise, the Diurnal Cycle of Cortisol and Cognitive Impairment in Older Adults. Neurobiol. Stress 2018, 9, 40–47. [Google Scholar] [CrossRef] [PubMed]
- Lupien, S.J.; Maheu, F.; Tu, M.; Fiocco, A.; Schramek, T.E. The Effects of Stress and Stress Hormones on Human Cognition: Implications for the Field of Brain and Cognition. Brain Cogn. 2007, 65, 209–237. [Google Scholar] [CrossRef] [PubMed]
- Wirth, M.; Lange, C.; Huijbers, W. Plasma Cortisol Is Associated with Cerebral Hypometabolism across the Alzheimer’s Disease Spectrum. Neurobiol. Aging 2019, 84, 80–89. [Google Scholar] [CrossRef] [PubMed]
- Kline, S.A.; Mega, M.S. Stress-Induced Neurodegeneration: The Potential for Coping as Neuroprotective Therapy. Am. J. Alzheimers Dis. Other Demen. 2020, 35, 153331752096087. [Google Scholar] [CrossRef]
- Lupien, S.J.; de Leon, M.; de Santi, S.; Convit, A.; Tarshish, C.; Nair, N.P.V.; Thakur, M.; McEwen, B.S.; Hauger, R.L.; Meaney, M.J. Cortisol Levels during Human Aging Predict Hippocampal Atrophy and Memory Deficits. Nat. Neurosci. 1998, 1, 69–73. [Google Scholar] [CrossRef]
- Lupien, S.J.; Nair, N.P.V.; Briére, S.; Maheu, F.; Tu, M.T.; Lemay, Μ.; McEwen, B.S.; Meaney, M.J. Increased Cortisol Levels and Impaired Cognition in Human Aging: Implication for Depression and Dementia in Later Life. Rev. Neurosci. 1999, 10, 117–140. [Google Scholar] [CrossRef] [PubMed]
- Csernansky, J.G.; Dong, H.; Fagan, A.M.; Wang, L.; Xiong, C.; Holtzman, D.M.; Morris, J.C. Plasma Cortisol and Progression of Dementia in Subjects with Alzheimer-Type Dementia. Am. J. Psychiatry 2006, 163, 2164–2169. [Google Scholar] [CrossRef]
- Lara, J.; Cooper, R.; Nissan, J.; Ginty, A.T.; Khaw, K.-T.; Deary, I.J.; Lord, J.M.; Kuh, D.; Mathers, J.C. A Proposed Panel of Biomarkers of Healthy Ageing. BMC Med. 2015, 13, 222. [Google Scholar] [CrossRef]
- Antypa, D.; Basta, M.; Vgontzas, A.; Zaganas, I.; Panagiotakis, S.; Vogiatzi, E.; Kokosali, E.; Simos, P. The Association of Basal Cortisol Levels with Episodic Memory in Older Adults Is Mediated by Executive Function. Neurobiol. Learn. Mem. 2022, 190, 107600. [Google Scholar] [CrossRef]
- Tortosa-Martínez, J.; Clow, A.; Caus-Pertegaz, N.; González-Caballero, G.; Abellán-Miralles, I.; Saenz, M.J. Exercise Increases the Dynamics of Diurnal Cortisol Secretion and Executive Function in People with Amnestic Mild Cognitive Impairment. J. Aging Phys. Act. 2015, 23, 550–558. [Google Scholar] [CrossRef] [PubMed]
- Segal, S.K.; Cotman, C.W.; Cahill, L.F. Exercise-Induced Noradrenergic Activation Enhances Memory Consolidation in Both Normal Aging and Patients with Amnestic Mild Cognitive Impairment. J. Alzheimer’s Dis. 2012, 32, 1011–1018. [Google Scholar] [CrossRef] [PubMed]
- Carson, N.; Leach, L.; Murphy, K.J. A Re-Examination of Montreal Cognitive Assessment (MoCA) Cutoff Scores: Re-Examination of MoCA Cutoff Scores. Int. J. Geriatr. Psychiatry 2018, 33, 379–388. [Google Scholar] [CrossRef] [PubMed]
- Diamond, A. Want to Optimize Executive Functions and Academic Outcomes? Simple, Just Nourish the Human Spirit. Minn. Symp. Child Psychol. Ser. 2014, 37, 205–232. [Google Scholar]
- Strauss, E.; Sherman, E.; Spreen, O. A Compendium of Neuropsychological Tests: Administration, Norms, and Commentary, 3rd ed.; Oxford University Press: Oxford, UK, 2006. [Google Scholar]
- Lee, H.; Baniqued, P.L.; Cosman, J.; Mullen, S.; McAuley, E.; Severson, J.; Kramer, A.F. Examining Cognitive Function across the Lifespan Using a Mobile Application. Comput. Hum. Behav. 2012, 28, 1934–1946. [Google Scholar] [CrossRef]
- Van der Elst, W.; Van Boxtel, M.P.J.; Van Breukelen, G.J.P.; Jolles, J. The Stroop Color-Word Test: Influence of Age, Sex, and Education; and Normative Data for a Large Sample Across the Adult Age Range. Assessment 2006, 13, 62–79. [Google Scholar] [CrossRef]
- Ettenhofer, M.L.; Hambrick, D.Z.; Abeles, N. Reliability and Stability of Executive Functioning in Older Adults. Neuropsychology 2006, 20, 607–613. [Google Scholar] [CrossRef]
- Houx, P.J. Testing Cognitive Function in Elderly Populations: The PROSPER Study. J. Neurol. Neurosurg. Psychiatry 2002, 73, 385–389. [Google Scholar] [CrossRef]
- Lesh, T.A.; Westphal, A.J.; Niendam, T.A.; Yoon, J.H.; Minzenberg, M.J.; Ragland, J.D.; Solomon, M.; Carter, C.S. Proactive and Reactive Cognitive Control and Dorsolateral Prefrontal Cortex Dysfunction in First Episode Schizophrenia. NeuroImage Clin. 2013, 2, 590–599. [Google Scholar] [CrossRef]
- Mohs, R.C.; Knopman, D.; Petersen, R.C.; Ferris, S.H.; Ernesto, C.; Grundman, M.; Sano, M.; Bieliauskas, L.; Geldmacher, D.; Clark, C.; et al. Development of Cognitive Instruments for Use in Clinical Trials of Antidementia Drugs: Additions to the Alzheimer’s Disease Assessment Scale That Broaden Its Scope. The Alzheimer’s Disease Cooperative Study. Alzheimer Dis. Assoc. Disord. 1997, 11 (Suppl. S2), S13–S21. [Google Scholar] [CrossRef]
- Harrison, J.; Minassian, S.L.; Jenkins, L.; Black, R.S.; Koller, M.; Grundman, M. A Neuropsychological Test Battery for Use in Alzheimer Disease Clinical Trials. Arch. Neurol. 2007, 64, 1323. [Google Scholar] [CrossRef] [PubMed]
- Podhorna, J.; Krahnke, T.; Shear, M.; Harrison, J.E. for the Alzheimer’s Disease Neuroimaging Initiative. Alzheimer’s Disease Assessment Scale–Cognitive Subscale Variants in Mild Cognitive Impairment and Mild Alzheimer’s Disease: Change over Time and the Effect of Enrichment Strategies. Alzheimer’s Res. Ther. 2016, 8, 8. [Google Scholar] [CrossRef] [PubMed]
- Nasreddine, Z.S.; Phillips, N.A.; Bédirian, V.; Charbonneau, S.; Whitehead, V.; Collin, I.; Cummings, J.L.; Chertkow, H. The Montreal Cognitive Assessment, MoCA: A Brief Screening Tool for Mild Cognitive Impairment: MOCA: A Brief Screening Tool for MCI. J. Am. Geriatr. Soc. 2005, 53, 695–699. [Google Scholar] [CrossRef] [PubMed]
- McAuley, E.; Mullen, S.P.; Szabo, A.N.; White, S.M.; Wójcicki, T.R.; Mailey, E.L.; Gothe, N.P.; Olson, E.A.; Voss, M.; Erickson, K.; et al. Self-Regulatory Processes and Exercise Adherence in Older Adults. Am. J. Prev. Med. 2011, 41, 284–290. [Google Scholar] [CrossRef] [PubMed]
- Menendez-Gonzalez, M. Routine Lumbar Puncture for the Early Diagnosis of Alzheimer’s Disease. Is It Safe? Front. Aging Neurosci. 2014, 6, 65. [Google Scholar]
- Bermejo-Pareja, F.; Antequera, D.; Vargas, T.; Molina, J.A.; Carro, E. Saliva Levels of Abeta1-42 as Potential Biomarker of Alzheimer’s Disease: A Pilot Study. BMC Neurol. 2010, 10, 108. [Google Scholar] [CrossRef]
- Sabbagh, M.N.; Shi, J.; Lee, M.; Arnold, L.; Al-Hasan, Y.; Heim, J.; McGeer, P. Salivary Beta Amyloid Protein Levels Are Detectable and Differentiate Patients with Alzheimer’s Disease Dementia from Normal Controls: Preliminary Findings. BMC Neurol. 2018, 18, 155. [Google Scholar] [CrossRef]
- Lee, M.; Guo, J.-P.; Kennedy, K.; McGeer, E.G.; McGeer, P.L. A Method for Diagnosing Alzheimer’s Disease Based on Salivary Amyloid-β Protein 42 Levels. J. Alzheimer’s Dis. 2016, 55, 1175–1182. [Google Scholar] [CrossRef]
- McGeer, P.L.; Guo, J.P.; Lee, M.; Kennedy, K.; McGeer, E.G. Alzheimer’s Disease Can Be Spared by Nonsteroidal Anti-Inflammatory Drugs. J. Alzheimer’s Dis. 2018, 62, 1219–1222. [Google Scholar] [CrossRef]
- Sheinerman, K.S.; Toledo, J.B.; Tsivinsky, V.G.; Irwin, D.; Grossman, M.; Weintraub, D.; Hurtig, H.I.; Chen-Plotkin, A.; Wolk, D.A.; McCluskey, L.F.; et al. Circulating Brain-Enriched MicroRNAs as Novel Biomarkers for Detection and Differentiation of Neurodegenerative Diseases. Alzheimer’s Res. Ther. 2017, 9, 89. [Google Scholar] [CrossRef]
- Nath, K.; Puleio, A.; Michielli, M.; Voelm, C.; Alberts, K.; Wall, K.; Duff, A.; Hanley, C.; Rogers, C.; Cohen, B.; et al. Biomarker and cognitive improvements after a single bout of Interactive Cognitive and Physical Exercise (iPACES v2.75): Results of a multi-site pilot study. In Proceedings of the The 33rd Annual Steinmetz Symposium, Schenectady, NY, USA, 22–24 May 2020. [Google Scholar]

| Completed iPACES Single-Bout | Completed Cognitive & Biomarker Data | |||
|---|---|---|---|---|
| (n = 33) | (n = 20) | |||
| Demographics a | X | SD | X | SD |
| Age | 72.8 | 10.7 | 70.5 | 9.0 |
| Education (years) b | 16.1 | 2.4 | 16.3 | 2.5 |
| BMI | 25.9 | 3.3 | 26.0 | 3.2 |
| MoCA Score | 24.7 | 3.0 | 25.3 | 2.6 |
| Gender (% female) | 61% | 65% | ||
| Race (% White) | 98% | 98% | ||
| Retiree Status (% retired) | 82% | 75% | ||
| Marital Status (% married) c | 67% | 80% | ||
| Self-rated physical activity d | 3.0 | 1.4 | 3.1 | 2.5 |
| Past Experience e | 0.0 | 0.0 | ||
| Cycling | 2.5 | 0.9 | 2.5 | 2.5 |
| Computers | 2.8 | 1.0 | 3.1 | 3.1 |
| Videogames | 1.1 | 1.0 | 1.3 | 1.3 |
| Motivation | 2.5 | 0.7 | 2.5 | 2.5 |
| Completed iPACES Single-Bout | Completed Cognitive & Biomarker Data | |||||||
|---|---|---|---|---|---|---|---|---|
| (n = 33) | (n = 20) | |||||||
| Pre | Post | Pre | Post | |||||
| Measure | X | SD | X | SD | X | SD | X | SD |
| Executive Function | ||||||||
| Stroop (Brain Baseline) | ||||||||
| Incongruent % correct | 0.83 | 0.25 | 0.89 | 0.19 | 0.91 | 0.15 | 0.93 | 0.13 |
| Congruent % correct | 0.92 | 0.17 | 0.97 | 0.07 | 0.94 | 0.14 | 0.98 | 0.07 |
| CCII | 0.75 | 0.37 | 0.85 | 0.26 | 0.85 | 0.25 | 0.90 | 0.20 |
| Stroop (Paper) | ||||||||
| Stroop A time | 24.94 | 6.96 | 24.60 | 8.11 | 22.65 | 5.17 | 22.54 | 6.36 |
| Stroop B time | 19.16 | 6.73 | 19.20 | 5.84 | 17.62 | 4.17 | 18.62 | 5.34 |
| Stroop C time | 57.94 | 32.75 | 52.58 | 22.51 | 48.75 | 21.22 | 46.50 | 19.29 |
| ADAS-Cog | ||||||||
| Word List (sum trials correct) | 18.54 | 4.37 | 19.75 | 3.86 | 19.89 | 3.74 | 21.25 | 2.99 |
| Word List (delay correct) | 6.00 | 2.85 | 5.33 | 3.25 | 7.25 | 2.05 | 6.42 | 2.75 |
| Biomarkers | ||||||||
| cortisol | 1.23 | 0.81 | 1.09 | 1.25 | ||||
| IGF-1 | 384.82 | 241.29 | 441.20 | 238.31 | ||||
| alpha-amylase | 37.72 | 68.66 | 33.83 | 45.67 | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nath, K.; Ferguson, I.; Puleio, A.; Wall, K.; Stark, J.; Clark, S.; Story, C.; Cohen, B.; Anderson-Hanley, C. Brain Health Indicators Following Acute Neuro-Exergaming: Biomarker and Cognition in Mild Cognitive Impairment (MCI) after Pedal-n-Play (iPACES). Brain Sci. 2023, 13, 844. https://doi.org/10.3390/brainsci13060844
Nath K, Ferguson I, Puleio A, Wall K, Stark J, Clark S, Story C, Cohen B, Anderson-Hanley C. Brain Health Indicators Following Acute Neuro-Exergaming: Biomarker and Cognition in Mild Cognitive Impairment (MCI) after Pedal-n-Play (iPACES). Brain Sciences. 2023; 13(6):844. https://doi.org/10.3390/brainsci13060844
Chicago/Turabian StyleNath, Kartik, IreLee Ferguson, Alexa Puleio, Kathryn Wall, Jessica Stark, Sean Clark, Craig Story, Brian Cohen, and Cay Anderson-Hanley. 2023. "Brain Health Indicators Following Acute Neuro-Exergaming: Biomarker and Cognition in Mild Cognitive Impairment (MCI) after Pedal-n-Play (iPACES)" Brain Sciences 13, no. 6: 844. https://doi.org/10.3390/brainsci13060844
APA StyleNath, K., Ferguson, I., Puleio, A., Wall, K., Stark, J., Clark, S., Story, C., Cohen, B., & Anderson-Hanley, C. (2023). Brain Health Indicators Following Acute Neuro-Exergaming: Biomarker and Cognition in Mild Cognitive Impairment (MCI) after Pedal-n-Play (iPACES). Brain Sciences, 13(6), 844. https://doi.org/10.3390/brainsci13060844






