Sleep Apnea and Substance Use Disorders Associated with Co-Occurrence of Anxiety Disorder and Depression among U.S. Adults: Findings from the NSDUH 2008–2014
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Measurements
2.2.1. Outcome Measure
2.2.2. Social-Demographic Factors
2.2.3. Chronic Diseases
2.2.4. Substance Use Disorders in the Past Year
2.3. Statistical Analysis
3. Results
3.1. Overall Prevalence of Anxiety and Depression and Comorbidity in the Population
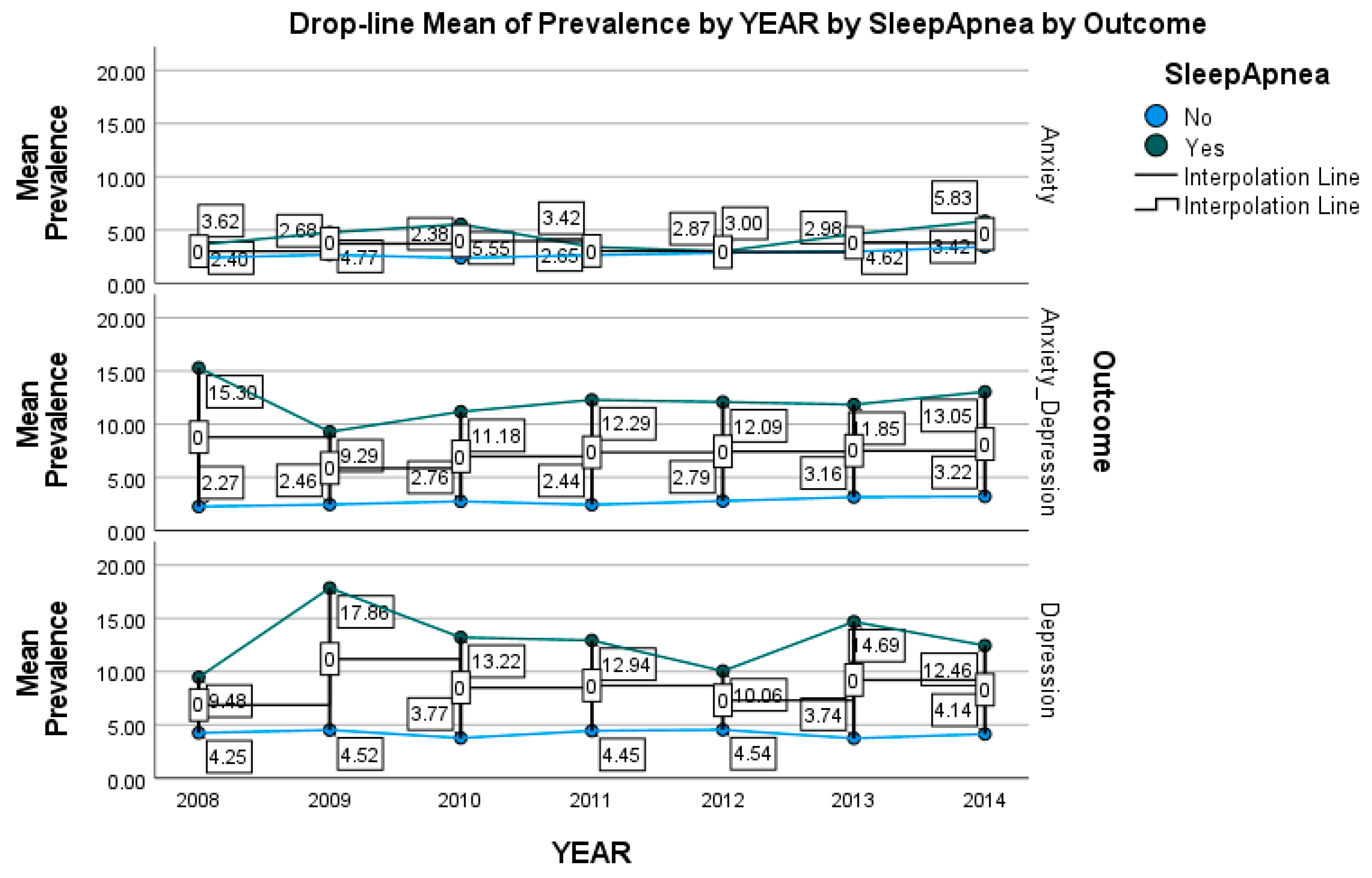
3.2. Prevalence of Anxiety Only, Depression Only, and Their Co-Occurrence by Year
3.3. Prevalence of Anxiety Only, Depression Only, and Their Co-Occurrence across Potential Factors
3.4. Multivariable Logistic Regression Analyses
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Choi, K.W.; Kim, Y.-K.; Jeon, H.J. Comorbid Anxiety and Depression: Clinical and Conceptual Consideration and Transdiagnostic Treatment. In Advances in Experimental Medicine and Biology; Springer: Singapore, 2020; Volume 1191, pp. 219–235. [Google Scholar] [CrossRef]
- Coplan, J.D.; Aaronson, C.J.; Panthangi, V.; Kim, Y. Treating comorbid anxiety and depression: Psychosocial and pharmacological approaches. World J. Psychiatry 2015, 5, 366–378. [Google Scholar] [CrossRef]
- Kalin, N.H. The Critical Relationship Between Anxiety and Depression. Am. J. Psychiatry 2020, 177, 365–367. [Google Scholar] [CrossRef] [PubMed]
- Maron, E.; Nutt, D. Biological markers of generalized anxiety disorder. Dialog. Clin. Neurosci. 2017, 19, 147–158. [Google Scholar] [CrossRef] [PubMed]
- Blanco, C.; Rubio, J.; Wall, M.; Wang, S.; Jiu, C.J.; Kendler, K.S. Risk factors for anxiety disorders: Common and specific effects in a national sample. Depress. Anxiety 2014, 31, 756–764. [Google Scholar] [CrossRef] [PubMed]
- Struijs, S.Y.; de Jong, P.J.; Jeronimus, B.F.; van der Does, W.; Riese, H.; Spinhoven, P. Psychological risk factors and the course of depression and anxiety disorders: A review of 15 years NESDA research. J. Affect. Disord. 2021, 295, 1347–1359. [Google Scholar] [CrossRef] [PubMed]
- Razzak, H.A.; Harbi, A.; Ahli, S. Depression: Prevalence and Associated Risk Factors in the United Arab Emirates. Oman Med. J. 2019, 34, 274–282. [Google Scholar] [CrossRef] [PubMed]
- Kaufmann, C.N.; Susukida, R.; Depp, C.A. Sleep apnea, psychopathology, and mental health care. Sleep Health 2017, 3, 244–249. [Google Scholar] [CrossRef]
- Hobzova, M.; Prasko, J.; Vanek, J.; Ocisková, M.; Genzor, S.; Holubová, M.; Grambal, A.; Latalova, K. Depression and obstructive sleep apnea. Neuro Endocrinol. Lett. 2017, 38, 343–352. [Google Scholar]
- Dempsey, J.A. Central sleep apnea: Misunderstood and mistreated! F1000Research 2019, 8, 981. [Google Scholar] [CrossRef]
- Garbarino, S.; Bardwell, W.A.; Guglielmi, O.; Chiorri, C.; Bonanni, E.; Magnavita, N. Association of Anxiety and Depression in Obstructive Sleep Apnea Patients: A Systematic Review and Meta-Analysis. Behav. Sleep Med. 2020, 18, 35–57. [Google Scholar] [CrossRef]
- Adams, G.C.; McWilliams, L.A.; Wrath, A.J.; Mondal, P.; Harder, J.A.; Skomro, R.; Fenton, M.E. An exploration of adult attachment insecurity and psychiatric symptoms in individuals with obstructive sleep apnea. J. Psychosom. Res. 2019, 123, 109731. [Google Scholar] [CrossRef]
- Gharsalli, H.; Harizi, C.; Zaouche, R.; Sahnoun, I.; Saffar, F.; Maalej, S.; Douik El Gharbi, L. Prevalence of depression and anxiety in obstructive sleep apnea. Tunis Med. 2022, 100, 525–533. [Google Scholar] [PubMed]
- Bierhoff, J.; Haardörfer, R.; Windle, M.; Berg, C.J. Psychological Risk Factors for Alcohol, Cannabis, and Various Tobacco Use among Young Adults: A Longitudinal Analysis. Subst. Use Misuse 2019, 54, 1365–1375. [Google Scholar] [CrossRef] [PubMed]
- Grant, J.E.; Lust, K.; Fridberg, D.J.; King, A.C.; Chamberlain, S.R. E-Cigarette Use (Vaping) is Associated with Illicit Drug Use, Mental Health Problems, and Impulsivity in University Students. Ann. Clin. Psychiatry 2019, 31, 27–35. [Google Scholar] [PubMed]
- Boden, J.M.; Fergusson, D.M. Alcohol and depression. Addiction 2011, 106, 906–914. [Google Scholar] [CrossRef]
- Husky, M.M.; Mazure, C.M.; Paliwal, P.; McKee, S.A. Gender differences in the comorbidity of smoking behavior and major depression. Drug Alcohol Depend. 2008, 93, 176–179. [Google Scholar] [CrossRef] [PubMed]
- Mugisha, J.; Muyinda, H.; Malamba, S.; Kinyanda, E. Major depressive disorder seven years after the conflict in northern Uganda: Burden, risk factors and impact on outcomes (The Wayo-Nero Study). BMC Psychiatry 2015, 15, 48. [Google Scholar] [CrossRef]
- Hassan, A.N. Patients with Alcohol Use Disorder Co-Occurring with Depression and Anxiety Symptoms: Diagnostic and Treatment Initiation Recommendations. J. Clin. Psychiatry 2018, 79, 17ac11999. [Google Scholar] [CrossRef]
- Subramaniam, P.; Rogowska, J.; DiMuzio, J.; Lopez-Larson, M.; McGlade, E.; Yurgelun-Todd, D. Orbitofrontal connectivity is associated with depression and anxiety in marijuana-using adolescents. J. Affect. Disord. 2018, 239, 234–241. [Google Scholar] [CrossRef]
- Onaemo, V.N.; Fawehinmi, T.O.; D’Arcy, C. Comorbid Cannabis Use Disorder with Major Depression and Generalized Anxiety Disorder: A Systematic Review with Meta-analysis of Nationally Representative Epidemiological Surveys. J. Affect. Disord. 2021, 281, 467–475. [Google Scholar] [CrossRef]
- Williams, R.; Farquharson, L.; Rhodes, E.; Dang, M.; Butler, J.; Quirk, A.; Baldwin, D.S.; Crawford, M.J. Impact of Substance Use Disorder on Quality of Inpatient Mental Health Services for People with Anxiety and Depression. J. Dual Diagn. 2021, 17, 80–93. [Google Scholar] [CrossRef] [PubMed]
- Robinson, L.D.; Deane, F.P. Substance Use Disorder and Anxiety, Depression, Eating Disorder, PTSD, and Phobia Comorbidities Among Individuals Attending Residential Substance Use Treatment Settings. J. Dual Diagn. 2022, 18, 165–176. [Google Scholar] [CrossRef] [PubMed]
- Chen, F.; Zou, L.; Dai, Y.; Sun, J.; Chen, C.; Zhang, Y.; Peng, Q.; Zhang, Z.; Xie, Z.; Wu, H.; et al. Prognostic plasma exosomal microRNA biomarkers in patients with substance use disorders presenting comorbid with anxiety and depression. Sci. Rep. 2021, 11, 6271. [Google Scholar] [CrossRef] [PubMed]
- Iqbal, M.N.; Levin, C.J.; Levin, F.R. Treatment for Substance Use Disorder with Co-Occurring Mental Illness. Focus 2019, 17, 88–97. [Google Scholar] [CrossRef] [PubMed]
- Duan, X.; Zheng, M.; Zhao, W.; Huang, J.; Lao, L.; Li, H.; Lu, J.; Chen, W.; Liu, X.; Deng, H. Associations of Depression, Anxiety, and Life Events with the Risk of Obstructive Sleep Apnea Evaluated by Berlin Questionnaire. Front. Med. 2022, 9, 799792. [Google Scholar] [CrossRef]
- Coussement, C.; Heeren, A. Sleep problems as a transdiagnostic hub bridging impaired attention control, generalized anxiety, and depression. J. Affect. Disord. 2022, 296, 305–308. [Google Scholar] [CrossRef]
- Choi, N.G.; DiNitto, D.M.; Marti, C.N. Treatment use, perceived need, and barriers to seeking treatment for substance abuse and mental health problems among older adults compared to younger adults. Drug Alcohol Depend. 2014, 145, 113–120. [Google Scholar] [CrossRef]
- Salas, J.; Scherrer, J.F.; Lustman, P.J.; Schneider, F.D. Racial differences in the association between nonmedical prescription opioid use, abuse/dependence, and major depression. Subst. Abus. 2016, 37, 25–30. [Google Scholar] [CrossRef]
- Pacek, L.R.; Sweitzer, M.M.; McClernon, F.J. Non-cigarette tobacco and poly-tobacco use among persons living with HIV drawn from a nationally representative sample. Drug Alcohol Depend. 2016, 162, 251–255. [Google Scholar] [CrossRef]
- Keith, D.R.; Stanton, C.A.; Gaalema, D.E.; Bunn, J.Y.; Doogan, N.J.; Redner, R.; Kurti, A.N.; Cepeda-Benito, A.; Lopez, A.A.; Morehead, A.L.; et al. Disparities in US Healthcare Provider Screening and Advice for Cessation Across Chronic Medical Conditions and Tobacco Products. J. Gen. Intern. Med. 2017, 32, 974–980. [Google Scholar] [CrossRef]
- Center for Behavioral Health Statistics and Quality. 2008–2014 National Survey on Drug Use and Health Public Use File Codebook; Substance Abuse and Mental Health Services Administration: Rockville, MD, USA, 2009–2015. [Google Scholar]
- Shiffman, S.; Waters, A.J.; Hickcox, M. The Nicotine Dependence Syndrome Scale: A multidimensional measure of nicotine dependence. Nicotine Tob. Res. 2004, 6, 327–348. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th ed.; American Psychiatric Association: Washington, DC, USA, 1994. [Google Scholar]
- Walker, E.R.; Druss, B.G. Cumulative burden of comorbid mental disorders, substance use disorders, chronic medical conditions, and poverty on health among adults in the U.S.A. Psychol. Health Med. 2017, 22, 727–735. [Google Scholar] [CrossRef] [PubMed]
- Faravelli, C.; Scarpato, M.A.; Castellini, G.; Sauro, C.L. Gender differences in depression and anxiety: The role of age. Psychiatry Res. 2013, 210, 1301–1303. [Google Scholar] [CrossRef] [PubMed]
- Kuehner, C. Why is depression more common among women than among men? Lancet Psychiatry 2017, 4, 146–158. [Google Scholar] [CrossRef]
- Malhi, G.S.; Mann, J.J. Depression. Lancet 2018, 392, 2299–2312. [Google Scholar] [CrossRef]
- Hasin, D.S.; Sarvet, A.L.; Meyers, J.L.; Saha, T.D.; Ruan, W.J.; Stohl, M.; Grant, B.F. Epidemiology of Adult DSM-5 Major Depressive Disorder and Its Specifiers in the United States. JAMA Psychiatry 2018, 75, 336–346. [Google Scholar] [CrossRef]
- Ettman, C.K.; Cohen, G.H.; Abdalla, S.M.; Galea, S. Do assets explain the relation between race/ethnicity and probable depression in U.S. adults? PLoS ONE 2020, 15, e0239618. [Google Scholar] [CrossRef]
- LaPierre, T.A. Marital Status and Depressive Symptoms Over Time: Age and Gender Variations. Fam. Relat. 2009, 58, 404–416. [Google Scholar] [CrossRef]
- Recksiedler, C.; Stawski, R.S. Marital Transitions and Depressive Symptoms among Older Adults: Examining Educational Differences. Gerontology 2019, 65, 407–418. [Google Scholar] [CrossRef]
- Sareen, J.; Afifi, T.O.; McMillan, K.A.; Asmundson, G.J.G. Relationship Between Household Income and Mental Disorders: Findings from a Population-Based Longitudinal Study. Arch. Gen. Psychiatry 2011, 68, 419–427. [Google Scholar] [CrossRef]
- Milaneschi, Y.; Simmons, W.K.; Van Rossum, E.F.C.; Penninx, B.W. Depression and obesity: Evidence of shared biological mechanisms. Mol. Psychiatry 2019, 24, 18–33. [Google Scholar] [CrossRef] [PubMed]
- Ye, G.; Baldwin, D.S.; Hou, R. Anxiety in asthma: A systematic review and meta-analysis. Psychol. Med. 2021, 51, 11–20. [Google Scholar] [CrossRef]
- Diaz, S.V.; Brown, L.K. Relationships between obstructive sleep apnea and anxiety. Curr. Opin. Pulm. Med. 2016, 22, 563–569. [Google Scholar] [CrossRef] [PubMed]
- Klumpp, H.; Chang, F.; Bauer, B.W.; Burgess, H.J. Objective and Subjective Sleep Measures Are Related to Suicidal Ideation and Are Transdiagnostic Features of Major Depressive Disorder and Social Anxiety Disorder. Brain Sci. 2023, 13, 288. [Google Scholar] [CrossRef]
- Lai, H.M.X.; Cleary, M.; Sitharthan, T.; Hunt, G.E. Prevalence of comorbid substance use, anxiety and mood disorders in epidemiological surveys, 1990–2014: A systematic review and meta-analysis. Drug Alcohol Depend. 2015, 154, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Sushanthi, S.; Doraikannan, S.; Indiran, M.A. Assessment of anxiety, depression and nicotine dependence among construction workers in Chennai—A cross sectional study. J. Oral Biol. Craniofacial Res. 2022, 12, 263–267. [Google Scholar] [CrossRef]
- El-Sherbiny, N.A.; Elsary, A.Y. Smoking and nicotine dependence in relation to depression, anxiety, and stress in Egyptian adults: A cross-sectional study. J. Family Community Med. 2022, 29, 8–16. [Google Scholar] [CrossRef]
- Andreasen, J.T. Tobacco dependence, anxiety, and depression. Ugeskr Laeger. 2022, 184, V01220038. [Google Scholar]
- Williams, G.C.; Patte, K.A.; Ferro, M.A.; Leatherdale, S.T. Associations between Longitudinal Patterns of Substance Use and Anxiety and Depression Symptoms among a Sample of Canadian Secondary School Students. Int. J. Environ. Res. Public Health 2021, 18, 10468. [Google Scholar] [CrossRef]
- Fluharty, M.; Taylor, A.E.; Grabski, M.; Munafò, M.R. The Association of Cigarette Smoking with Depression and Anxiety: A Systematic Review. Nicotine Tob. Res. 2017, 19, 3–13. [Google Scholar] [CrossRef]
- McKenzie, M.; Jorm, A.F.; Romaniuk, H.; Olsson, C.A.; Patton, G.C. Association of adolescent symptoms of depression and anxiety with alcohol use disorders in young adulthood: Findings from the Victorian Adolescent Health Cohort Study. Med. J. Aust. 2011, 195, S27–S30. [Google Scholar] [CrossRef] [PubMed]
- Brook, J.S.; Zhang, C.; Rubenstone, E.; Primack, B.A.; Brook, D.W. Comorbid trajectories of substance use as predictors of Antisocial Personality Disorder, Major Depressive Episode, and Generalized Anxiety Disorder. Addict. Behav. 2016, 62, 114–121. [Google Scholar] [CrossRef] [PubMed]
- Klein, R.J.; Gyorda, J.A.; Jacobson, N.C. Anxiety, depression, and substance experimentation in childhood. PLoS ONE 2022, 17, e0265239. [Google Scholar] [CrossRef]
- Cioffredi, L.-A.; Kamon, J.; Turner, W. Effects of depression, anxiety and screen use on adolescent substance use. Prev. Med. Rep. 2021, 22, 101362. [Google Scholar] [CrossRef]
- Amendola, S.; Hengartner, M.P.; Ajdacic-Gross, V.; Angst, J.; Rössler, W. Longitudinal reciprocal associations between depression, anxiety, and substance use disorders over three decades of life. J. Affect. Disord. 2022, 302, 315–323. [Google Scholar] [CrossRef] [PubMed]
- Wang, R.; Snieder, H.; Hartman, C.A. Familial co-aggregation and shared heritability between depression, anxiety, obesity and substance use. Transl. Psychiatry 2022, 12, 1–8. [Google Scholar] [CrossRef]
- Harrison, L.; Huges, A. (Eds.) The Validity of Self-Reported Drug Use: Improving the Accuracy of Survey Estimates; NIDA Research Monograph 167, NIH Publication No. 97-4147; National Institute on Drug Use: Rockville, MD, USA, 1997. [Google Scholar]
| Variable | Total | Anxiety | Prevalence (%) (95% CI) | Total | Depression | Prevalence (%) (95% CI) | p-Value |
|---|---|---|---|---|---|---|---|
| Anxiety | |||||||
| No | 248,866 | 11,561 | 4.8 (4.6–4.9) | <0.0001 | |||
| Yes | 9268 | 8142 | 51.8 (50.6–53.0) | ||||
| Depression | |||||||
| No | 245,447 | 8142 | 3.1 (3.0–3.2) | <0.0001 | |||
| Yes | 20,829 | 9268 | 40.4 (39.3–41.5) | ||||
| Overall | 270,227 | 17,410 | 5.9 (5.7–6.0) | 270,227 | 20,829 | 7.5 (7.4–7.7) |
| Variable | Total | Anxiety Only | Prevalence (%) (95% CI) | Depression Only | Prevalence (%) (95% CI) | Co-Occurrence | Prevalence (%) (95% CI) | a p-Value |
|---|---|---|---|---|---|---|---|---|
| Year | ||||||||
| 2008 | 36,910 | 939 | 2.4 (2.1–2.7) | 1630 | 4.4 (4.0–4.8) | 1018 | 2.6 (2.4–2.9) | <0.0001 |
| 2009 | 37,182 | 1029 | 2.7 (2.5–3.0) | 1662 | 4.9 (4.6–5.2) | 1135 | 2.6 (2.4–2.9) | |
| 2010 | 38,343 | 1062 | 2.5 (2.2–2.7) | 1636 | 4.0 (3.7–4.4) | 1288 | 3.0 (2.7–3.2) | |
| 2011 | 38,613 | 1099 | 2.7 (2.4–2.9) | 1717 | 4.7 (4.4–5.1) | 1250 | 2.8 (2.5–3.0) | |
| 2012 | 37,331 | 1190 | 2.9 (2.6–3.2) | 1683 | 4.7 (4.3–5.1) | 1343 | 3.1 (2.9–3.4) | |
| 2013 | 36,834 | 1285 | 3.0 (2.7–3.3) | 1508 | 4.2 (3.8–4.5) | 1489 | 3.5 (3.2–3.8) | |
| 2014 | 41,063 | 1538 | 3.5 (3.3–3.7) | 1725 | 4.5 (4.2–4.7) | 1745 | 3.6 (3.4–3.9) | |
| b p-Value | <0.0001 | 0.0047 | <0.0001 | |||||
| Overall | 270,227 | 8142 | 2.8 (2.7–2.9) | 11,561 | 4.5 (4.4–4.6) | 9268 | 3.0 (2.9–3.1) |
| Variable | Total | Anxiety Only | Prevalence (%) (95% CI) | Depression Only | Prevalence (%) (95% CI) | Co-Occurrence | Prevalence (%) (95% CI) | p-Value |
|---|---|---|---|---|---|---|---|---|
| Sex | ||||||||
| Male | 123,623 | 2606 | 2.0 (1.9–2.1) | 3471 | 3.0 (2.9–3.2) | 2377 | 1.8 (1.7–1.9) | <0.0001 |
| Female | 142,653 | 5536 | 3.6 (3.5–3.8) | 8090 | 5.9 (5.6–6.1) | 6891 | 4.2 (4.0–4.3) | |
| Age group | ||||||||
| 18–25 years | 123,552 | 3657 | 3.0 (2.8–3.1) | 4591 | 3.4 (3.3–3.5) | 4067 | 3.1 (3.0–3.2) | <0.0001 |
| 26–49 years | 98,308 | 3389 | 3.2 (3.1–3.4) | 4649 | 4.4 (4.2–4.6) | 3968 | 3.5 (3.4–3.7) | |
| 50–64 years | 27,400 | 732 | 2.6 (2.3–2.8) | 1714 | 5.9 (5.5–6.3) | 1018 | 3.4 (3.1–3.7) | |
| 65+ years | 17,016 | 364 | 2.2 (1.9–2.4) | 607 | 3.6 (3.2–4.0) | 215 | 1.3 (1.1–1.5) | |
| Race | ||||||||
| White | 167,953 | 6332 | 3.4 (3.3–3.5) | 8507 | 5.2 (5.0–5.3) | 7442 | 3.7 (3.6–3.8) | <0.0001 |
| AA | 32,974 | 508 | 1.6 (1.4–1.8) | 936 | 3.0 (2.7–3.3) | 435 | 1.3 (1.1–1.5) | |
| Asian | 10,525 | 109 | 1.0 (0.6–1.3) | 176 | 1.8 (1.3–2.2) | 101 | 1.1 (0.7–1.5) | |
| Hispanic | 41,981 | 804 | 1.8 (1.6–2.0) | 1319 | 3.3 (3.0–3.7) | 785 | 1.8 (1.6–2.1) | |
| Other | 12,843 | 389 | 2.7 (2.1–3.3) | 623 | 5.1 (4.1–6.2) | 505 | 3.9 (3.3–4.6) | |
| Marital status | ||||||||
| Married | 97,095 | 2791 | 2.5 (2.4–2.7) | 4197 | 4.1 (3.9–4.3) | 2807 | 2.4 (2.3–2.5) | <0.0001 |
| Widowed/divorced/separated | 32,387 | 1204 | 3.2 (2.9–3.5) | 2149 | 6.2 (5.8–6.6) | 1825 | 4.3 (4.1–4.7) | |
| Never married | 136,794 | 4147 | 3.2 (3.0–3.4) | 5215 | 3.9 (3.8–4.1) | 4636 | 3.4 (3.2–3.5) | |
| Income | ||||||||
| Less than USD 20,000 | 66,665 | 2294 | 3.4 (3.1–3.7) | 3329 | 5.6 (5.3–6.0) | 3089 | 4.7 (4.5–4.9) | <0.0001 |
| USD 20,000–49,999 | 90,208 | 2626 | 2.8 (2.6–3.0) | 3904 | 4.6 (4.4–4.8) | 3057 | 3.1 (2.9–3.3) | |
| USD 50,000–74,999 | 42,423 | 1220 | 2.5 (2.3–2.7) | 1737 | 4.4 (4.1–4.8) | 1284 | 2.8 (2.6–3.0) | |
| USD 75,000 or more | 66,980 | 2002 | 2.7 (2.6–2.9) | 2591 | 3.8 (3.6–3.9) | 1838 | 2.2 (2.0–2.3) | |
| Sleep apnea | ||||||||
| No | 260,700 | 7843 | 2.8 (2.7–2.9) | 10,791 | 4.2 (4.1–4.3) | 8396 | 2.7 (2.6–2.8) | <0.0001 |
| Yes | 5550 | 299 | 4.4 (3.7–5.2) | 770 | 12.9 (11.6–14.3) | 872 | 12.2 (10.9–13.5) | |
| IDUD and AUD | ||||||||
| No | 260,910 | 7818 | 2.8 (2.7–2.9) | 11,138 | 4.4 (4.3–4.6) | 8724 | 3.0 (2.9–3.1) | <0.0001 |
| Yes | 5366 | 324 | 6.4 (5.5–7.4) | 423 | 9.4 (8.2–10.7) | 544 | 10.7 (9.0–12.4) | |
| Nicotine dependence | ||||||||
| No | 224,510 | 6070 | 2.5 (2.4–2.6) | 8815 | 4.2 (4.0–4.3) | 6324 | 2.5 (2.4–2.6) | <0.0001 |
| Yes | 41,766 | 2072 | 4.7 (4.4–5.1) | 2746 | 6.5 (6.1–6.9) | 2944 | 6.6 (6.2–6.9) | |
| Asthma | ||||||||
| No | 248,382 | 7461 | 2.8 (2.7–2.9) | 10,480 | 4.4 (4.2–4.5) | 7880 | 2.8 (2.7–2.9) | <0.0001 |
| Yes | 17,772 | 681 | 3.6 (3.1–4.1) | 1081 | 6.6 (6.0–7.2) | 1388 | 7.4 (6.6–8.1) | |
| Bronchitis | ||||||||
| No | 256,713 | 7755 | 2.8 (2.7–2.9) | 10,911 | 4..4 (4.2–4.5) | 8446 | 2.8 (2.7–2.9) | <0.0001 |
| Yes | 9510 | 387 | 3.8 (3.2–4.4) | 650 | 7.4 (6.7–8.1) | 822 | 7.9 (7.1–8.7) | |
| Diabetes | ||||||||
| No | 255,617 | 7917 | 2.9 (2.8–3.0) | 10,870 | 4.4 (4.2–4.5) | 8703 | 3.0 (2.9–3.1) | <0.0001 |
| Yes | 10,606 | 225 | 1.9 (1.6–2.2) | 691 | 6.0 (5.3–6.6) | 565 | 4.1 (3.5–4.7) | |
| Hypertension | ||||||||
| No | 237,705 | 7302 | 2.9 (5.8–3.0) | 9684 | 4.1 (3.9–4.2) | 7723 | 2.7 (2.7–2.8) | <0.0001 |
| Yes | 28,471 | 840 | 2.4 (2.2–2.7) | 1877 | 6.3 (5.9–6.7) | 1545 | 4.3 (4.0–4.6) | |
| Heart disease | ||||||||
| No | 261,172 | 8002 | 4.2 (4.0–4.5) | 11,227 | 4.3 (4.1–4.5) | 8938 | 2.1 (2.0–2.3) | <0.0001 |
| Yes | 5082 | 140 | 2.8 (2.7–2.9) | 334 | 6.4 (5.4–7.4) | 330 | 4.9 (4.1–5.7) |
| Variable | Anxiety Only OR (95% CI) | p-Value | Depression Only OR (95% CI) | p-Value | Co-Occurrence OR (95% CI) | p-Value |
|---|---|---|---|---|---|---|
| Year (ref = 2008) | ||||||
| 2009 | 1.14 (0.98–1.33) | 0.0886 | 1.12 (1.01–1.25) | 0.0313 | 1.02 (0.89–1.17) | 0.7455 |
| 2010 | 1.02 (0.87–1.20) | 0.7665 | 0.91 (0.80–1.04) | 0.1814 | 1.14 (1.01–1.30) | 0.0400 |
| 2011 | 1.13 (0.96–1.33) | 0.1361 | 1.08 (0.97–1.21) | 0.1716 | 1.06 (0.91–1.25) | 0.4341 |
| 2012 | 1.24 (1.04–1.46) | 0.0152 | 1.10 (0.96–1.26) | 0.1565 | 1.26 (1.11–1.43) | 0.0006 |
| 2013 | 1.32 (1.14–1.54) | 0.0003 | 0.97 (0.85–1.11) | 0.6559 | 1.42 (1.25–1.61) | <0.0001 |
| 2014 | 1.56 (1.35–1.79) | <0.0001 | 1.06 (0.95–1.18) | 0.2803 | 1.50 (1.33–1.69) | <0.0001 |
| Sex (ref = male) | 2.13 (1.99–2.29) | <0.0001 | 2.26 (2.11–2.41) | <0.0001 | 2.83 (2.61–3.06) | <0.0001 |
| Age group (ref = 18–34) | ||||||
| 35–49 | 1.30 (1.20–1.40) | <0.0001 | 1.36(1.26–1.47) | <0.0001 | 1.29 (1.19–1.40) | <0.0001 |
| 50–64 | 0.98 (0.85–1.14) | 0.8308 | 1.50 (1.34–1.68) | <0.0001 | 0.91 (0.80–1.03) | 0.1172 |
| 65+ | 0.71 (0.61–0.84) | <0.0001 | 0.68 (0.59–0.80) | <0.0001 | 0.23 (0.19–0.29) | <0.0001 |
| Race (ref = White) | ||||||
| AA | 0.36 (0.31–0.42) | <0.0001 | 0.42 (0.38–0.47) | <0.0001 | 0.20(0.18–0.39) | <0.0001 |
| Hispanic | 0.47 (0.42–0.54) | <0.0001 | 0.61 (0.55–0.68) | <0.0001 | 0.43 (0.38–0.49) | <0.0001 |
| Asian | 0.69 (0.55–0.85) | <0.0001 | 0.86 (0.69–1.07) | <0.0001 | 0.77 (0.63–0.95) | <0.0001 |
| Marital status (ref = married) | ||||||
| Widowed/divorced/separated | 1.20 (1.05–1.37) | 0.0008 | 1.33 (1.23–1.44) | <0.0001 | 1.51 (1.37–1.68) | <0.0001 |
| Never married | 1.28 (1.15–1.43) | <0.0001 | 1.12 (1.03–1.22) | 0.0064 | 1.35 (1.23–1.49) | <0.0001 |
| Income (ref = less than USD 20,000) | ||||||
| USD 20,000–49,999 | 0.81 (0.73–0.89) | <0.0001 | 0.81 (0.73–0.87) | <0.0001 | 0.71 (0.65–0.77) | <0.0001 |
| USD 50,000–74,999 | 0.70 (0.61–0.80) | <0.0001 | 0.74 (0.66–0.84) | <0.0001 | 0.63 (0.55–0.71) | <0.0001 |
| USD 75,000 or more | 0.77 (0.68–0.87) | <0.0001 | 0.63 (0.57–0.70) | <0.0001 | 0.50 (0.44–0.57) | <0.0001 |
| Sleep apnea (ref = no) | 2.44 (2.03–2.94) | <0.0001 | 3.73 (3.27–4.25) | <0.0001 | 5.39 (4.67–6.22) | <0.0001 |
| IDUD and AUD (ref = no) | 2.51 (2.12–2.98) | <0.0001 | 2.99 (2.58–3.47) | <0.0001 | 3.83 (3.17–4.62) | <0.0001 |
| Nicotine dependence (ref = no) | 1.74 (1.60–1.89) | <0.0001 | 1.44 (1.33–1.56) | <0.0001 | 2.07 (1.88–2.27) | <0.0001 |
| Asthma (ref = no) | 1.22 (1.06–1.41) | 0.0079 | 1.28 (1.15–1.42) | <0.0001 | 1.87 (1.64–2.13) | <0.0001 |
| Bronchitis (ref = no) | 1.15 (0.97–1.36) | 0.1134 | 1.27 (1.13–1.43) | <0.0001 | 1.68 (1.48–1.91) | <0.0001 |
| Diabetes (ref = no) | 0.77 (0.64–0.92) | 0.0044 | 1.15 (1.00–1.32) | 0.0448 | 1.19 (0.99–1.42) | 0.0667 |
| Hypertension (ref = no) | 0.99 (0.87–1.12) | 0.8632 | 1.50 (1.38–1.64) | <0.0001 | 1.84 (1.67–2.03) | <0.0001 |
| Heart disease (ref = no) | 1.24 (0.96–1.60) | 0.1045 | 1.30 (1.10–1.55) | 0.0031 | 1.68 (1.36–2.10) | <0.0001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Xu, C.; Acevedo, P.; Wang, L.; Wang, N.; Ozuna, K.; Shafique, S.; Karithara, A.; Padilla, V.; Mao, C.; Xie, X.; et al. Sleep Apnea and Substance Use Disorders Associated with Co-Occurrence of Anxiety Disorder and Depression among U.S. Adults: Findings from the NSDUH 2008–2014. Brain Sci. 2023, 13, 661. https://doi.org/10.3390/brainsci13040661
Xu C, Acevedo P, Wang L, Wang N, Ozuna K, Shafique S, Karithara A, Padilla V, Mao C, Xie X, et al. Sleep Apnea and Substance Use Disorders Associated with Co-Occurrence of Anxiety Disorder and Depression among U.S. Adults: Findings from the NSDUH 2008–2014. Brain Sciences. 2023; 13(4):661. https://doi.org/10.3390/brainsci13040661
Chicago/Turabian StyleXu, Chun, Priscila Acevedo, Liang Wang, Nianyang Wang, Kaysie Ozuna, Saima Shafique, Annu Karithara, Victoria Padilla, Chunxiang Mao, Xin Xie, and et al. 2023. "Sleep Apnea and Substance Use Disorders Associated with Co-Occurrence of Anxiety Disorder and Depression among U.S. Adults: Findings from the NSDUH 2008–2014" Brain Sciences 13, no. 4: 661. https://doi.org/10.3390/brainsci13040661
APA StyleXu, C., Acevedo, P., Wang, L., Wang, N., Ozuna, K., Shafique, S., Karithara, A., Padilla, V., Mao, C., Xie, X., & Wang, K. (2023). Sleep Apnea and Substance Use Disorders Associated with Co-Occurrence of Anxiety Disorder and Depression among U.S. Adults: Findings from the NSDUH 2008–2014. Brain Sciences, 13(4), 661. https://doi.org/10.3390/brainsci13040661







