Paraneoplastic Syndrome Presenting Combined Central and Peripheral Demyelination Associated with Anti-CV2/CRMP5 and Anti-NF186 Antibodies: A Case Report
Abstract
1. Introduction
2. Case Report
3. Discussion
4. Conclusions
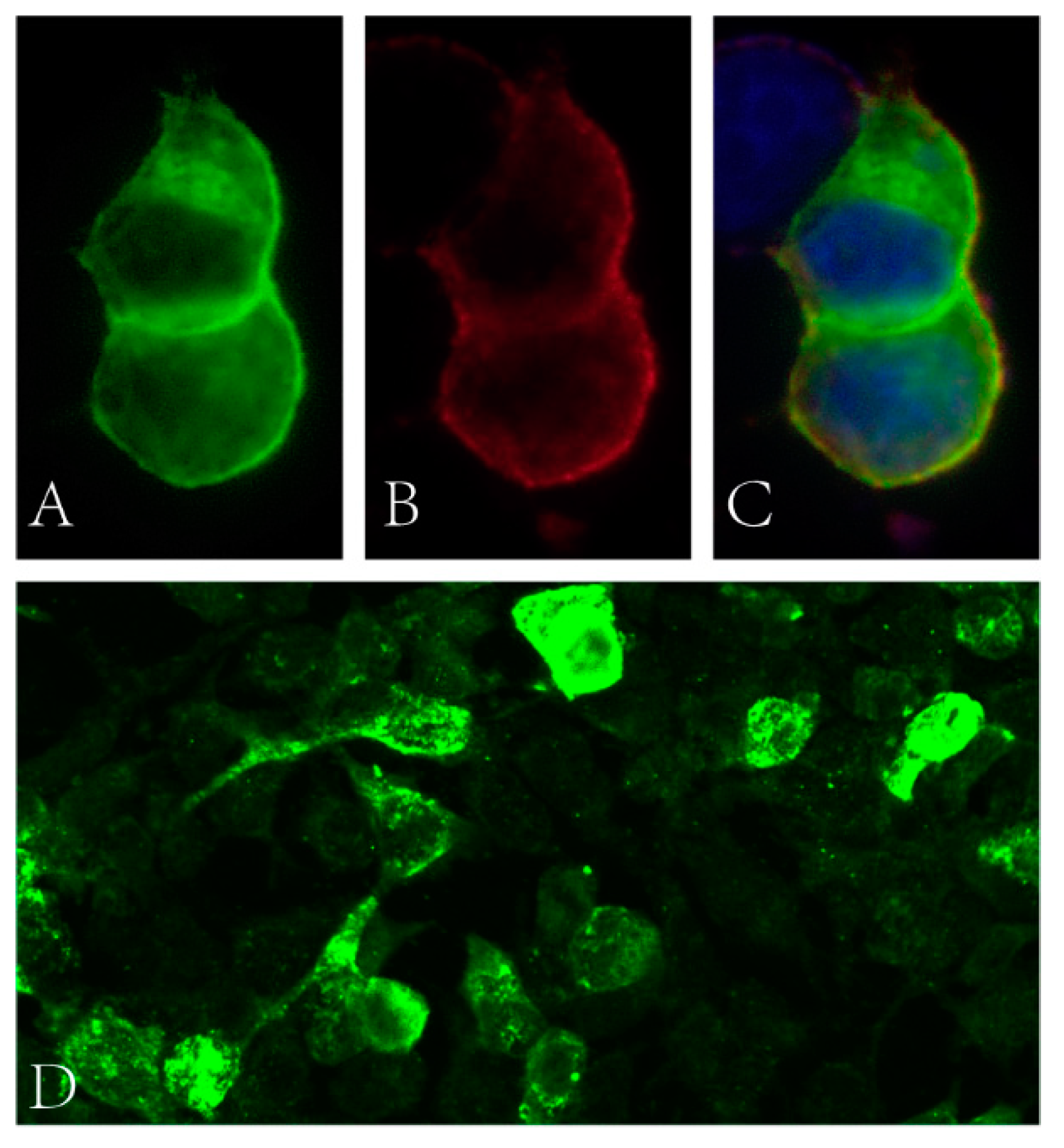
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kamm, C.; Zettl, U.K. Autoimmune disorders affecting both the central and peripheral nervous system. Autoimmun. Rev. 2012, 11, 196–202. [Google Scholar] [CrossRef]
- Darnell, R.B.; Posner, J.B. Paraneoplastic syndromes involving the nervous system. N. Engl. J. Med. 2003, 349, 1543–1554. [Google Scholar] [CrossRef] [PubMed]
- Campetella, L.; Papi, C.; Sabatelli, E.; Marini, S.; Iorio, R. Real-world application of the updated diagnostic criteria for paraneoplastic neurological syndromes. J. Neuroimmunol. 2022, 372, 577972. [Google Scholar] [CrossRef] [PubMed]
- Xie, C.; Wang, Z.; Zhao, N.; Zhu, D.; Zhou, X.; Ding, J.; Wu, Y.; Yu, H.; Guan, Y. From PNS to CNS: Characteristics of anti-neurofascin 186 neuropathy in 16 cases. Neurol. Sci. 2021, 42, 4673–4681. [Google Scholar] [CrossRef] [PubMed]
- Vallat, J.-M.; Mathis, S.; Magy, L.; Bounolleau, P.; Skarzynski, M.; Heitzmann, A.; Manso, C.; Devaux, J.; Uncini, A. Subacute nodopathy with conduction blocks and anti-neurofascin 140/186 antibodies: An ultrastructural study. Brain 2018, 141, e56. [Google Scholar] [CrossRef]
- Burnor, E.; Yang, L.; Zhou, H.; Patterson, K.R.; Quinn, C.; Reilly, M.M.; Rossor, A.; Scherer, S.S.; Lancaster, E. Neurofascin antibodies in autoimmune, genetic, and idiopathic neuropathies. Neurology 2017, 90, e31–e38. [Google Scholar] [CrossRef]
- Delmont, E.; Manso, C.; Querol, L.; Cortese, A.; Berardinelli, A.; Lozza, A.; Belghazi, M.; Malissart, P.; Labauge, P.; Taieb, G.; et al. Autoantibodies to nodal isoforms of neurofascin in chronic inflammatory demyelinating polyneuropathy. Brain 2017, 140, 1851–1858. [Google Scholar] [CrossRef]
- Sundaram, S.; Nair, S.S.; Jaganmohan, D.; Unnikrishnan, G.; Nair, M. Relapsing lumbosacral myeloradiculitis: An unusual presentation of MOG antibody disease. Mult. Scler. J. 2020, 26, 509–511. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.-Q.; Chen, H.; Zhuang, W.-P.; Li, H.-L. The clinical features of combined central and peripheral demyelination in Chinese patients. J. Neuroimmunol. 2018, 317, 32–36. [Google Scholar] [CrossRef]
- Kawamura, N.; Yamasaki, R.; Yonekawa, T.; Matsushita, T.; Kusunoki, S.; Nagayama, S.; Fukuda, Y.; Ogata, H.; Matsuse, D.; Murai, H.; et al. Anti-neurofascin antibody in patients with combined central and peripheral demyelination. Neurology 2013, 81, 714–722. [Google Scholar] [CrossRef]
- Ogata, H.; Matsuse, D.; Yamasaki, R.; Kawamura, N.; Matsushita, T.; Yonekawa, T.; Hirotani, M.; Murai, H.; Kira, J.-I. A nationwide survey of combined central and peripheral demyelination in Japan. J. Neurol. Neurosurg. Psychiatry 2016, 87, 29–36. [Google Scholar] [CrossRef] [PubMed]
- Antoine, J.C.; Honnorat, J.; Camdessanché, J.P.; Magistris, M.; Absi, L.; Mosnier, J.F.; Petiot, P.P.; Kopp, N.; Michel, D. Paraneoplastic anti-cv2 antibodies react with peripheral nerve and are associated with a mixed axonal and demyelinating peripheral neuropathy. Ann. Neurol. 2001, 49, 214–221. [Google Scholar] [CrossRef] [PubMed]
- Siles, A.M.; Martínez-Hernández, E.; Araque, J.; Diaz-Manera, J.; Rojas-García, R.; Gallardo, E.; Illa, I.; Graus, F.; Querol, L. Antibodies against cell adhesion molecules and neural structures in paraneoplastic neuropathies. Ann. Clin. Transl. Neurol. 2018, 5, 559–569. [Google Scholar] [CrossRef]
- Shah, S.; Campo, R.V.D.; Kumar, N.; McKeon, A.; Flanagan, E.P.; Klein, C.; Pittock, S.J.; Dubey, D. Paraneoplastic myeloneuropathies. Neurology 2021, 96, e632–e639. [Google Scholar] [CrossRef]
- Dubey, D.; Lennon, V.A.; Gadoth, A.; Pittock, S.J.; Flanagan, E.P.; Schmeling, J.E.; McKeon, A.; Klein, C.J. Autoimmune CRMP5 neuropathy phenotype and outcome defined from 105 cases. Neurology 2018, 90, e103–e110. [Google Scholar] [CrossRef]
- Thaxton, C.; Pillai, A.M.; Pribisko, A.L.; Dupree, J.L.; Bhat, M.A. Nodes of Ranvier act as barriers to restrict invasion of flanking Paranodal domains in myelinated axons. Neuron 2011, 69, 244–257. [Google Scholar] [CrossRef]
- Feinberg, K.; Eshed-Eisenbach, Y.; Frechter, S.; Amor, V.; Salomon, D.; Sabanay, H.; Dupree, J.L.; Grumet, M.; Brophy, P.J.; Shrager, P.; et al. A glial signal consisting of gliomedin and NrCAM clusters axonal Na+ channels during the formation of nodes of ranvier. Neuron 2010, 65, 490–502. [Google Scholar] [CrossRef]
- Devaux, J.J.; Miura, Y.; Fukami, Y.; Inoue, T.; Manso, C.; Belghazi, M.; Sekiguchi, K.; Kokubun, N.; Ichikawa, H.; Wong, A.H.Y.; et al. Neurofascin-155 IgG4 in chronic inflammatory demyelinating polyneuropathy. Neurology 2016, 86, 800–807. [Google Scholar] [CrossRef]
- Querol, L.; Nogales-Gadea, G.; Rojas-Garcia, R.; Diaz-Manera, J.; Pardo, J.; Ortega-Moreno, A.; Sedano, M.J.; Gallardo, E.; Berciano, J.; Blesa, R.; et al. Neurofascin IgG4 antibodies in CIDP associate with disabling tremor and poor response to IVIg. Neurology 2014, 82, 879–886. [Google Scholar] [CrossRef]
- Fehmi, J.; Davies, A.J.; Walters, J.; Lavin, T.; Keh, R.; Rossor, A.M.; Munteanu, T.; Delanty, N.; Roberts, R.; Bäumer, D.; et al. IgG1 pan-neurofascin antibodies identify a severe yet treatable neuropathy with a high mortality. J. Neurol. Neurosurg. Psychiatry 2021, 92, 1089–1095. [Google Scholar] [CrossRef] [PubMed]
- Stengel, H.; Vural, A.; Brunder, A.-M.; Heinius, A.; Appeltshauser, L.; Fiebig, B.; Giese, F.; Dresel, C.; Papagianni, A.; Birklein, F.; et al. Anti–pan-neurofascin IgG3 as a marker of fulminant autoimmune neuropathy. Neurol. Neuroimmunol. Neuroinflamm. 2019, 6, e603. [Google Scholar] [CrossRef] [PubMed]
- Appeltshauser, L.; Junghof, H.; Messinger, J.; Linke, J.; Haarmann, A.; Ayzenberg, I.; Baka, P.; Dorst, J.; Fisse, A.L.; Grüter, T.; et al. Anti-pan-neurofascin antibodies induce subclass-related complement activation and nodo-paranodal damage. Brain, 2022; online ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Bien, C.G.; Schänzer, A.; Dargvainiene, J.; Dogan-Onugoren, M.; Woermann, F.; Strickler, A. Co-occurrence of antibodies against dipeptidyl-peptidase-like protein-6 and aquaporin-4 during a case of paraneoplastic encephalitis. Clin. Neurol. Neurosurg. 2020, 197, 106093. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, B.; Zhou, L.; Zheng, Y.; Sun, C.; Lin, J. Paraneoplastic Syndrome Presenting Combined Central and Peripheral Demyelination Associated with Anti-CV2/CRMP5 and Anti-NF186 Antibodies: A Case Report. Brain Sci. 2023, 13, 374. https://doi.org/10.3390/brainsci13030374
Liu B, Zhou L, Zheng Y, Sun C, Lin J. Paraneoplastic Syndrome Presenting Combined Central and Peripheral Demyelination Associated with Anti-CV2/CRMP5 and Anti-NF186 Antibodies: A Case Report. Brain Sciences. 2023; 13(3):374. https://doi.org/10.3390/brainsci13030374
Chicago/Turabian StyleLiu, Bingyou, Lei Zhou, Yongsheng Zheng, Chong Sun, and Jie Lin. 2023. "Paraneoplastic Syndrome Presenting Combined Central and Peripheral Demyelination Associated with Anti-CV2/CRMP5 and Anti-NF186 Antibodies: A Case Report" Brain Sciences 13, no. 3: 374. https://doi.org/10.3390/brainsci13030374
APA StyleLiu, B., Zhou, L., Zheng, Y., Sun, C., & Lin, J. (2023). Paraneoplastic Syndrome Presenting Combined Central and Peripheral Demyelination Associated with Anti-CV2/CRMP5 and Anti-NF186 Antibodies: A Case Report. Brain Sciences, 13(3), 374. https://doi.org/10.3390/brainsci13030374





